133 - Replacement of the Esophagus with Colon
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume II > The Mediastinum > Section XXV - Anatomy > Chapter 156 - Mediastinal Parathyroids
Chapter 156
Mediastinal Parathyroids
Thomas W. Shields
The two pairs of parathyroid glands derive from the endoderm of the third and fourth pharyngeal pouches bilaterally (Fig. 156-1). Hamilton and Mossman (1972) also presented evidence that the fifth pharyngeal pouch may fuse with the fourth pouch to form the so-called caudal pharyngeal complex and that parathyroid IV arises from the dorsal portion of this complex. The possible importance of this observation is discussed in this chapter.
NUMBER OF PARATHYROID GLANDS
In an autopsy study of 527 specimens, Gilmour and Martin (1937) noted that the normal number of four glands was identified in 80%, whereas in the remaining 20%, a lesser or greater number of glands was found. In 73 specimens (14%), three glands were found in 69 and only two glands in 6 specimens. Because the weight of the individually identified glands in these specimens fell within the norm, however, Gilmour and Martin surmised that the decrease in number resulted from not identifying the missing gland or glands rather than from a true abnormality in the normal number. In a subsequent report, however, Gilmour (1938) noted that because of studies by R ssle (1938), B ttiger and Wernstedt (1927), and Gilmour (1937) of 16 embryos in which thorough serial microscopic sections were made and which did not identify four glands in all specimens, it may be that less than four glands are present in some individuals.
The presence of supernumerary glands, however, was definitely established in 6% of the specimens: five glands in 31 (5.8%) and six glands in 2 specimens (0.3%). A greater number of glands have been even more rarely identified. Scholz and associates (1973) at the Mayo Clinic noted that when a supernumerary gland or glands was present in association with a normal number of glands in the neck, 14 of 15 were found in the mediastinum. Russell and associates (1982) reported that two thirds of the supernumerary glands in their selected series of 15 patients were located in the mediastinum: three were associated with the aorta or great vessels, and seven were within the mediastinal portion of the thymus. By extrapolating the data presented by Russell and associates (1981) of 2,770 operations for hyperparathyroidism, the incidence of a mediastinal location of one of the normal four glands is only 1%. This extrapolation essentially agrees with the data of Wang (1976), who reported that 2% of people may have one parathyroid gland in the mediastinal portion of the thymus within 3 to 4 cm of the sternal notch.
MEDIASTINAL LOCATIONS
The explanation for a mediastinal position of a gland is that, embryologically, the parathyroids III remain associated with or even imbedded in the cephalic tip of the thymic lobes as they migrate caudally. Their descent usually stops in the neck adjacent to the lower pole of the thyroid. However, Gilmour (1938) found 19 of 792 parathyroids III (2.4%) 3 cm or more below the lower poles of the thyroid gland: 1.4% at 3 cm, 0.9% at 4 cm, and 0.1% at 6 cm. The more distal of such glands or a supernumerary gland may be carried down into the prevascular (anterior) compartment of the mediastinum along with the thymus.
Retropharyngeal (Low Cervical) Area
The originally lower parathyroids IV become cephalad in position relative to the original upper parathyroids III. Because parathyroids IV arise in close association with the postbranchial bodies that emerge with the thyroid primordium, these glands (parathyroids IV) remain in contact with the upper posterior aspects of the thyroid lobes. When parathyroids IV assume an ectopic position, they remain in the visceral compartment of the neck. With caudad descent, an ectopic gland may come to lie in the posterior aspect of the superior portion of the visceral compartment of the mediastinum adjacent or dorsal to the trachea or even the esophagus and dorsal to the recurrent nerves. In a dissection of 160 postmortem subjects, Wang (1976) found 1%
P.2358
of parathyroid glands IV behind the lower pharynx or esophagus in the visceral compartment of the neck near the thoracic inlet. Gilmour (1938) found 46 parathyroids IV (5.8%) in a more posterior plane than that of the lower pole of the thyroid and in the same plane as the esophagus, and nine (1.1%) opposite the lower pole of thyroid behind the esophagus, which agrees with Wang's findings. When a parathyroid gland IV descends below the thoracic inlet, it lies in the retrotracheal portion of the visceral compartment. According to Nathaniels and associates (1970), such glands are often attached by a large vascular pedicle that ascends to the inferior thyroid vessels in the neck.
 |
Fig. 156-1. Schematic representation of 104 missing parathyroid glands reported by Wang; 34 glands were found in the low retrotracheal space. From Wang CA: Parathyroid reexploration, a clinical and pathological study of 112 cases. Ann Surg 186:140, 1977. With permission. |
In reviewing a series of 112 patients who underwent reoperation for primary hyperparathyroidism, however, Wang (1977) found the missing gland in the retrotracheal space in 34 patients (38%; see Fig. 156-1). Most of these obviously represented an enlarged parathyroid IV gland that was originally located higher but that had descended into this abnormal location. Thompson and associates (1982) recorded a similar incidence of enlarged parathyroids IV in this location (Fig. 156-2).
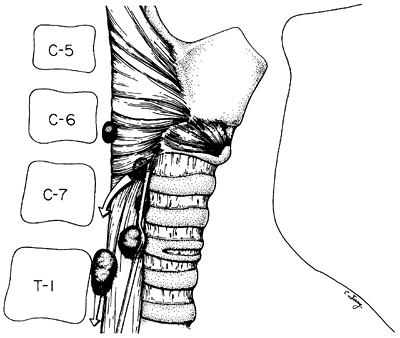 |
Fig. 156-2. Common abnormal location (found 36% to 39% of the time) of superior (upper) parathyroid gland adenomas. From Thompson NW, Eckhauser FE, Harneas JK: The anatomy of primary hyperparathyroidism. Surgery 92:814, 1982. With permission. |
Anterior Compartment
In Wang's (1977) very selected series of 112 reoperations for hyperparathyroidism, 21 mediastinal parathyroids III (19%) were located in the anterior compartment (Fig. 156-3; see Fig. 156-1). Although most parathyroid glands located in the anterior compartment are found in or associated closely with the thymus gland, the remaining few that are found behind the thymus actually may be located in the pretracheal portion of the visceral compartment, as defined in Chapter 154.
In a series of hyperparathyroid patients, Thompson (1982) and Russell (1981) and their associates found an approximately 1% to 2% incidence of anterior mediastinal parathyroids, which agrees with the various anatomic studies summarized by Thompson and associates (1982) (Fig. 156-4). Although the blood supply to the normally located parathyroid III gland is from the inferior thyroid vessels, when one of these glands is in the anterior compartment of the mediastinum, according to Doppman and co-workers (1977), its blood supply may arise directly from the internal mammary artery. The incidence of this variation is unknown.
Visceral (Middle) Compartment
Parathyroid tissue has been reported to occur in the aortopulmonary window and in close proximity to the right pulmonary artery near the tracheal bifurcation by McHenry (1988) and Curley (1988) and their associates, among others (see Chapter 193). The translocation of parathyroid tissue
P.2359
to these areas in the visceral (middle) compartment of the mediastinum may occur in a manner such as the translocation of thymic tissue to these areas during descent of the heart (see Chapter 155) and thus may derive from a parathyroid III. However, Curley and associates (1988) suggest it is more likely that such tissue arises from a dislocated parathyroid IV. Gilmour (1937) noted that in the 3-mm embryo, parathyroid IV is in close contact with the pericardium and thus that some of the tissue may retain this relationship and develop in the visceral compartment. Curley and associates (1988), however, believe it is more likely that parathyroid IV tissue in the visceral compartment is the result of its embryologic association with the sixth branchial artery in the 7.5- to 11-mm embryo, as Hamilton and Mossman (1972) point out. Curley and associates (1988) believe that if the parathyroid IV component fragments from the dorsal portion of the caudal pharyngeal complex (a fusion of the fourth and fifth pharyngeal pouches) during this time, such parathyroid tissue may remain near the developing right pulmonary artery. Which of these speculations is correct remains unsettled. Nonetheless, the possibility of an ectopic parathyroid adenoma in the visceral compartment must be recognized and appropriate steps taken for its identification when necessary. In addition to these locations of ectopic parathyroid tissue from one of the inferior (parathyroid III) glands in the anterior area of the visceral compartment (pretracheal area), some of these may progress posteriorly into the retrotracheal compartment as well. However, most parathyroid tissue found in the retrotracheal area derives from displaced or dislocated superior (parathyroid IV) glands that have descended retrotracheally into the mediastinum. As Thompson and colleagues (1982) have stated (among many other surgeons), this retrotracheal mediastinal area must be investigated whenever a superior gland cannot be identified in the neck.
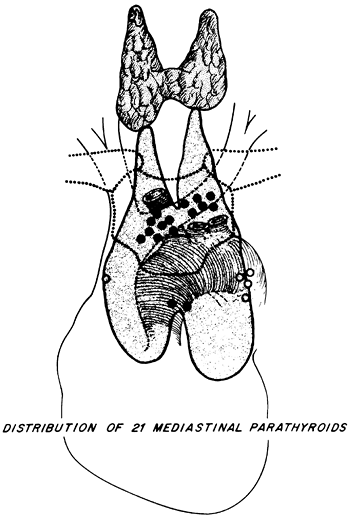 |
Fig. 156-3. Distribution of sites of 21 mediastinal parathyroid glands. Solid dots indicate glands within the thymus (incidence of 16%). Open dots indicate those behind the thymus or anterior to the great vessels or the bronchus (incidence of 33%). From Wang CA: Parathyroid reexploration, a clinical and pathological study of 112 cases. Ann Surg 186:140, 1977. With permission. |
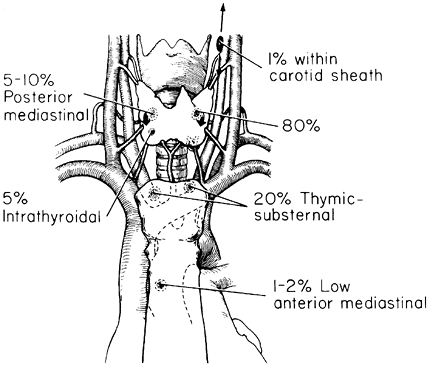 |
Fig. 156-4. Normal and ectopic location of normal parathyroid glands as summarized from anatomic studies. From Thompson NW, Eckhauser FE, Harneas JK: The anatomy of primary hyperparathyroidism. Surgery 92:814, 1982. With permission. |
HISTOPATHOLOGY OF MEDIASTINAL PARATHYROIDS
Normal parathyroid glands are rarely encountered surgically in the mediastinum, although Jaretzki and Wolff (1988) reported the identification of parathyroid tissue in 17 of 50 patients undergoing a maximal mediastinal thymectomy. As a rule, however, when parathyroid tissue is identified, it usually represents a functioning adenoma, rarely a hyperplastic gland, or even more infrequently an adenocarcinoma (see Chapter 193) or a rare mediastinal parathyroid cyst (see Chapter 197).
P.2360
Briefly, the histopathology of a parathyroid adenoma may be noted. As stated by Marchevsky and Kaneko (1992), the adenoma is usually a single, enlarged, well-encapsulated nodule. Histologically, it is composed of trabeculae, solid nests, and microacini lined by chief cells, oncocytic cells, clear cells, or all three. A rim of normal parathyroid tissue often can be seen in adjacent tissue external to the capsule. Microcysts may be present. Castleman and Mallory (1935) found microcysts in 50% of normal parathyroid glands in necropsy cases of individuals past puberty. Black and Watts (1949) found microcysts of 100 m or more in 42% of specimens. The histologic features of true parathyroid cysts and cystic adenomas are presented in Chapter 197 and discussed in greater detail by this author and Immerman (1999) in their collective review of parathyroid cysts that had appeared in the world literature up to 1999.
REFERENCES
Black BM, Watts CF: Cysts of parathyroid origin: report of two cases and study of the incidence and pathogenesis of cysts in parathyroid glands. Surgery 25:941, 1949.
B ttiger E, Wernstedt W: Todlich verlaufender fall von Spasmophilic bei einem Brusthinde mit Arnomalien der Thymus und der Parathyreoideae. Acta Paediatr 6: 373, 1927.
Castleman B, Mallory TB: The pathology of the parathyroid glands in hyperparathyroidism. Am J Pathol 11:1, 1935.
Curley IR, et al: The challenge of the middle mediastinal parathyroid. World J Surg 12: 818, 1988.
Doppman JL, et al: The blood supply of mediastinal parathyroid adenomas. Ann Surg 185: 488, 1977.
Gilmour JR: The embryology of the parathyroid glands, the thymus and certain associated rudiments. J Pathol 45: 507, 1937.
Gilmour JR: The gross anatomy of the parathyroid glands. J Pathol 46: 133, 1938.
Gilmour JR, Martin WJ: The weight of the parathyroid glands. J Pathol Bacteriol 44: 431, 1937.
Hamilton WJ, Mossman HW: Human Embryology. 4th Ed. Cambridge: W Heffner & Sons, 1972, pp. 228 290, 291 376.
Jaretzki A III, Wolff M: Maximal thymectomy for myasthenia gravis. Surgical anatomy and operative techniques. J Thorac Cardiovasc Surg 96:711, 1988.
Marchevsky AM, Kaneko M: Endocrine and salivary gland lesions of the mediastinum. In Marchevsky AM, Kaneko M (eds): Surgical Pathology of the Mediastinum. 2nd Ed. New York: Raven Press, 1992, p. 196.
McHenry C, et al: Resection of parathyroid tumor in the aorticopulmonary window without prior neck exploration. Surgery 104: 1090, 1988.
Nathaniels EK, Nathaniels AM, Wang CA: Mediastinal parathyroid tumors: a clinical and pathological study of 48 cases. Ann Surg 171:165, 1970.
R ssle R: Quoted by Gilmour JR: The gross anatomy of the parathyroid glands. J Pathol 46: 133, 1938.
Russell CF, Grant CS, van Heerden JA: Hyperfunctioning supernumerary parathyroid glands. An occasional cause of hyperparathyroidism. Mayo Clin Proc 57: 121, 1982.
Russell CF, et al: Mediastinal parathyroid tumors: experience with 38 tumors requiring mediastinotomy for removal. Ann Surg 193: 805, 1981.
Scholz DA, et al: Mediastinal hyperfunctioning parathyroid tumors: review of 14 cases. Ann Surg 178:173, 1973.
Shields TW, Immerman SC: Mediastinal parathyroid cysts revisited. Ann Thorac Surg 67:581, 1999.
Thompson NW, Eckhauser FE, Harness JK: The anatomy of primary hyperparathyroidism. Surgery 92: 814, 1982.
Wang CA: The anatomic basis of parathyroid surgery. Ann Surg 183: 271, 1976.
Wang CA: Parathyroid reexploration. A clinical and pathological study of 112 cases. Ann Surg 186: 140, 1977.
EAN: 2147483647
Pages: 203