35 - Extended Resection of Bronchial Carcinoma in the Superior Pulmonary Sulcus
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section IX - The Chest Wall > Chapter 43 - Thoracic Outlet Syndrome
Chapter 43
Thoracic Outlet Syndrome
Harold C. Urschel Jr.
Thoracic outlet syndrome (TOS) consists of compression of the subclavian vessels and brachial plexus at the superior aperture of the thorax. It was designated previously according to presumed etiologies such as scalenus anticus, costoclavicular, hyperabduction, cervical rib, and first rib syndromes. The various syndromes are similar, and the specific compression mechanism is often difficult to identify; however, the first rib seems to be a common denominator against which most compressive factors operate.
The symptoms are neurologic, vascular, or mixed, depending on which component is compressed. Occasionally, the pain is atypical in distribution and severity and is experienced predominantly in the chest wall and parascapular area, simulating angina pectoris.
Diagnosis of the nerve compression group can be objectively substantiated by determining the ulnar nerve conduction velocity. In the vascular compression group, diagnosis is usually established clinically, rarely requiring the use of angiography.
The ulnar nerve conduction velocity test (UNCV), as described by Jebsen (1967) and Caldwell and associates (1971), has widened the clinical recognition of this syndrome and has improved diagnosis, selection of treatment, and assessment of therapeutic results.
Physiotherapy to improve posture, strengthen shoulder girdle muscles, and stretch neck muscles is used initially in most cases of thoracic outlet syndrome and is often successful in cases of mild compression. Surgical treatment involves extirpation of the first rib, as initially described by Falconer and Li (1962), usually through the transaxillary approach. The most suitable indication for operative intervention is in cases of severe compression that have not responded to conservative therapy.
ANATOMIC CONSIDERATIONS
The subclavian vessels and brachial plexus traverse the cervicoaxillary canal to reach the upper extremity. The outer border of the first rib divides this canal into a proximal division triangle. This proximal division is composed of the scalene triangle and the space bounded by the clavicle and the first rib (the costoclavicular space). The distal division comprises the axilla. The proximal division is the most critical for neurovascular compression. It is bounded superiorly by the clavicle and the subclavius muscle; inferiorly by the first rib; anteromedially by the border of the sternum, the clavipectoral fascia, and the costocoracoid ligament; and posterolaterally by the scalenus medius muscle and the long thoracic nerve. The scalenus anticus, inserting on the scalene tubercle of the first rib, divides the costoclavicular space into two compartments: an anterior compartment, containing the subclavian vein, and a posterior compartment, containing the subclavian artery and brachial plexus. The axilla, which is the outer division of the cervicoaxillary canal, with its underlying structures, including the pectoralis minor muscle, the coracoid process, and the head of the humerus, is also an area of potential compression.
Compression Factors
Many factors can cause compression of the neurovascular bundle at the thoracic outlet (Fig. 43-1). The basic factor, which was pointed out by Rosati and Lord (1961), is deranged anatomy, to which congenital, traumatic, and atherosclerotic factors may contribute (Table 43-1).
Bony abnormalities are present in approximately 30% of patients, either as a cervical rib, a bifid first rib, fusion of first and second ribs, clavicular deformities, or previous thoracoplasty.
Pathologic changes in the configuration of the cervicoaxillary canal alter the normal functional dynamics and serve as the basis of the clinical maneuvers used in the diagnosis of thoracic outlet syndrome.
DIAGNOSIS
The basic diagnostic consideration for thoracic outlet syndrome includes the history and physical examination,
P.690
radiographs of the chest and cervical spine, neurologic consultation, electromyography, and UNCV. On occasion, a cervical myelogram, coronary angiogram, and venograms may be necessary to establish the diagnosis.
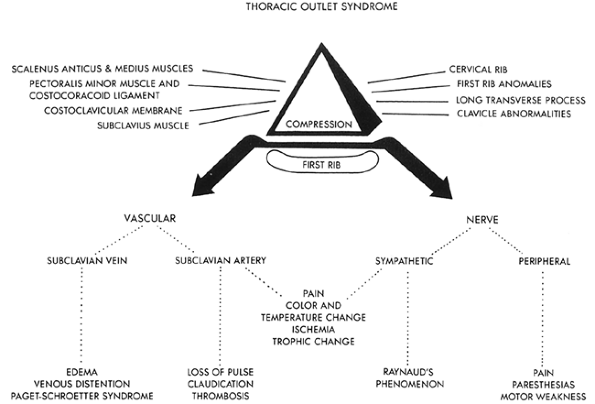 |
Fig. 43-1. Schematic diagram showing the relation of muscle, ligament, and bone abnormalities in the thoracic outlet that may compress neurovascular structures against the first rib. |
Table 43-1. Etiologic Factors in Thoracic Outlet Syndrome | |
|---|---|
|
Signs and Symptoms
The symptoms and signs of thoracic outlet syndrome depend on whether the nerves or blood vessels, or both, are compressed at the thoracic outlet (see Fig. 43-1).
Signs and symptoms of nerve compression occur most frequently, arm pain and paresthesias being present in about 95% of patients and motor weakness in less than 10%. Pain and paresthesias are segmented in 75% of cases, with 90% occurring in the ulnar nerve distribution. Pain is usually insidious in onset and commonly involves the neck, shoulder, arm, and hand.
Compression Tests
Adson or Scalene Test
The Adson or scalene test, described by Adson in 1951, tightens the anterior and middle scalene muscles, thus decreasing the interscalene space and magnifying any preexisting compression of the subclavian artery and brachial plexus. The patient is instructed to (a) take and hold a deep breath, (b) extend his or her neck fully, and (c) turn his or her face toward the side. Obliteration or diminution in the radial pulse suggests compression.
Costoclavicular Test: Military Position
In the costoclavicular test, the shoulders are drawn downward and backward. This maneuver narrows the costoclavicular space by approximating the clavicle to the first rib, thus tending to compress the neurovascular bundle.
P.691
Changes in the radial pulse or production of symptoms indicate compression.
Hyperabduction Test
When the arm is hyperabducted to 180 degrees, the components of the neurovascular bundle are pulled around the pectoralis minor tendon, coracoid process, and head of the humerus. If the radial pulse decreases, compression should be suspected.
Arm Claudication Test (Roos Test)
In the arm claudication test as outlined by Roos and Owens (1966), the shoulders are drawn upward and backward. The arms are raised to the horizontal position with the elbows flexed 90 degrees. With exercises of the hands, numbness or pain is experienced in the hands and forearms if compression is present.
Pseudoangina
In some patients, the pain is atypical, involving the anterior chest wall or the parascapular area, and is termed pseudoangina because it simulates angina pectoris. As presented by me and my associates in 1973, these patients have normal coronary arteriograms and decreased ulnar nerve conduction velocities, strongly suggesting the diagnosis of thoracic outlet syndrome. The usual shoulder, arm, and hand symptoms that might have provided the clue for the diagnosis of thoracic outlet syndrome are initially either absent or minimal compared with the severity of the chest pain. Without a high index of suspicion, the diagnosis of thoracic outlet syndrome is frequently overlooked, and many of these patients become cardiac cripples without an appropriate diagnosis, or develop severe psychological depression when told that their coronary arteries are normal and that they have no significant cause for their pain.
To understand the symptomatic overlap between coronary artery disease and this atypical manifestation of the thoracic outlet syndrome (i.e., pseudoangina), it is necessary to review the neuroanatomy, innervation, and pain pathways of the arm, chest wall, and heart.
At least two types of pain pathways are present in the arm. These are the commonly acknowledged C5 T1 cutaneous more superficial fibers and the T2 T5 afferent spinal fibers, which travel with the sympathetic nerves and transmit deeper painful stimuli from the ulnar, median, and parascapular distribution, as reported by Kuntz (1951). The cell bodies of the two types of afferent neurons are situated in the dorsal root ganglia of the corresponding spinal segments. They synapse in the dorsal gray matter of the spinal cord and the axons of the second-order neurons, cross the midline, and ascend in the spinothalamic tract to the brain.
Compression of the superficial C8 Tl cutaneous afferent fibers elicits stimuli that are transmitted to the brain and recognized as integumentary pain or paresthesias in the ulnar nerve distribution. In contrast, compression of the predominantly deeper sensory fibers elicits impulses that are interpreted by the brain as deep pain originating in the arm or referred to the chest wall.
The pseudoangina experienced in thoracic outlet compression shares with angina pectoris the same dermatomal distribution, in that the heart, arm, and chest wall have afferent fibers convergent on T2 T5 spinal cord segments and cell bodies that are located in the corresponding dorsal root ganglia. Referred pain to the chest wall is a component of both pseudoangina and angina pectoris. Because somatic pain is more common than visceral pain, the brain interprets activity arriving in a given pathway as a pain stimulus in a particular somatic area.
Two theories attempt to explain the mechanism of referred pain from the heart or arm stimuli to the chest wall. The convergence theory holds that somatic and visceral afferents converge on the same spinothalamic neurons; when the same pathway is stimulated by activity in visceral afferents, the signal reaching the brain is the same and the pain is projected to the somatic area. The facilitation effort theory holds that because of subliminal fringe effects, incoming impulses from visceral structures (e.g., heart) lower the threshold of spinothalamic neurons receiving afferents from somatic areas. Thus, minor activity in the pain pathways from the somatic areas (activity that would normally die out in the spinal cord) passes on to the brain and is interpreted as somatic pain rather than pain in the viscera, where the stimulus was initiated.
Vascular Compression
Symptoms of vascular compression in thoracic outlet syndrome, much less common than those of neurologic compression, include coldness, weakness, easy fatigability of the arm and hand, and pain that is usually more diffuse in distribution. Evaluation or exercise may cause pain, paresthesias, and color and temperature changes. Raynaud's phenomenon is occasionally noted. Venous compression is recognized by edema, venous distention, and discoloration of the arm and hand. Thrombosis of the subclavian vein [ effort thrombosis or Paget-Schroetter syndrome (PSS)] is infrequently noted but was described by Lang in 1962.
Objective physical findings, in contrast, are more common in patients with primarily vascular rather than neural compression. Loss or diminution of radial pulse and reproduction of symptoms can be elicited with Adson's test, costoclavicular (military) position, and hyperabduction maneuvers in most patients with vascular compression. Other possible findings are venous distention and edema, trophic changes, Raynaud's phenomenon, temperature changes, subclavian vein thrombosis, and even arterial occlusion and
P.692
claudication. In case of neural compression, the objective neurologic findings, which occur less frequently, consist of hypesthesia, anesthesia, and occasional muscular weakness or atrophy.
Nerve Conduction Velocity
Motor conduction velocities of the ulnar, median, radial, and musculocutaneous nerves can be reliably measured, as described by Jebsen (1967). Caldwell and associates (1971) improved and adapted to clinical use the technique of measuring the UNCV in evaluating patients with thoracic outlet compression. Conduction velocities over proximal and distal segments of the ulnar nerve are determined by recording the action potentials generated in the hypothenar or first dorsal interosseous muscles. The points of stimulation are the supraclavicular fossa, mid-upper arm, area below the elbow, and wrist. The Meditron 201-AD or the TECA B-3 electromyogram including the coaxial cable with three needle or surface electrodes can be used for this examination. The normal average UNCV values are 85 m/s across the thoracic outlet, 55 m/s around the elbow, 59 m/s in the forearm, and 2.5 to 3.5 m/s at the wrist. In patients with thoracic outlet syndrome, the average UNCV value is reduced to 53 m/s across the outlet (range of 32 65 m/s) as reported by me (1972) and my colleagues (1971).
Angiography
Simple clinical observations usually suffice to determine the degree of vascular impairment in the upper extremity, and peripheral angiography is rarely needed. As reported by Lang (1962), bruits in the supra- or infraclavicular spaces suggest stenosis or aneurysm, and absence of pulse denotes total obstruction. In these instances, retrograde or antegrade arteriograms of the subclavian and brachial arterial systems are indicated to demonstrate localized pathologic changes. Using arteriography or phlebography routinely for demonstrating temporary occlusion of the vessels in different arm positions is usually unnecessary and redundant to an adequate clinical examination in most patients and may be associated with some morbidity. The UNCV may be depressed in patients with vascular compression as well as nerve compression.
In instances of venous stenosis or obstruction, as in PSS, ultrasonography or phlebography is indicated to discern the extent of thrombosis to determine the status of collateral venous circulation. After successful thrombolysis, because the stenosis appears localized, attempts have been made to dilate it with a balloon and insert intravascular stents to keep the stenosis open. All have occluded in my and Patel's (2003) experience and in the experience of others, such as that of Sharafuddin and colleagues (2002). Remaining stenosis after successful thrombolysis is related to external compression of the vein by the clavicle, costoclavicular ligament, rib, or scalenus anterior muscle.
Table 43-2. Differential Diagnosis of Nerve Compression | |
|---|---|
|
DIFFERENTIAL DIAGNOSIS
The cardinal rule for the establishment of a thoracic outlet syndrome diagnosis is the elimination of significant coronary artery disease, as well as pulmonary, esophageal, and chest wall etiologies. It is also necessary to differentiate it neurologically from lesions of the cervical spine, brachial plexus, and peripheral nerves (Table 43-2), as well as from arterial and venous phenomena (Table 43-3).
THERAPY
Most patients with neurologic TOS receive physiotherapy before operative intervention. Such therapy must not be the same as given to patients with the cervical syndrome, which often exaggerates the symptoms of thoracic outlet compression. Proper physiotherapy for thoracic outlet compression includes heat massages, active neck exercises, scalenus anticus muscle stretching, strengthening of the upper trapezius muscle and shoulder girdle, and posture instruction. Because sagging of the shoulder girdle, common among middle-aged
P.693
people, is a significant etiologic factor in the spontaneous TOS, many patients with less severe disease benefit from strengthening the shoulder girdle and improving posture. More than half the patients seen in consultation required no surgical procedure but improved significantly with conservative management.
Table 43-3. Differential Diagnosis of Vascular Compression | |
|---|---|
|
Most patients with a nerve conduction value (NCV) above 60 m/s improve with conservative management. Most patients with an NCV below 60 m/s require surgical resection of the first rib and correction of any bony abnormalities.
Physical therapy is not used in patients with PSS or acute arterial insufficiency problems because of the urgency for immediate interventional therapy in both situations. The primary use for physical therapy and conservative management trials is for many neurologic primary or recurrent thoracic outlet syndromes. The exception might rest in a patient who is developing motor deficits and certain other selected situations.
Surgical Approaches
For primary straightforward neurologic TOSs resistant to conservative management, the preferred approach is the transaxillary resection of the first or cervical rib with neurovascular decompression as suggested by Roos in 1966. Because most patients are women, the scar is unobtrusive and difficult to visualize; no major muscles are divided, and the cervical or first rib may be removed directly without retraction of the brachial plexus or blood vessels. The wound, however, is deeper, and more light and magnification are required, and greater experience is necessary, than for other approaches.
The supraclavicular approach is reserved for patients with arterial insufficiency or arterial aneurysm who require bypass therapy. This necessitates a proximal subclavian arterial anastomosis and an infraclavicular brachial or axillary artery anastomosis in most cases. The disadvantage of this is the cosmetic scar being visible in most cases and the necessity of retracting the brachial plexus and blood vessels to remove the first rib. There is a higher incidence of nerve injury in this approach as compared with the transaxillary technique.
Reoperations for recurrent TOS are best accomplished via the high posterior thoracoplasty approach with a muscle-splitting incision of the trapezius and rhomboids. This provides an excellent approach to bone remnants and to the brachial plexus for neurolysis.
Other approaches include the infraclavicular approach and the transthoracic thoracoscopic rib removal as described by Wolf and associates (2000), as well as combined procedures.
Technique of Transaxillary Resection of the First Rib
The patient is placed in the lateral position with the involved extremity abducted to 90 degrees by a traction strap wrapped carefully around the forearm and attached to an overhead pulley. A two-pound weight is used to maintain this position without undue traction. The axilla and forearm are prepared and draped. A transverse incision is made below the axillary hairline between the pectoralis major, and the latissimus dorsi muscles and deepened to the external intercostal fascia. Care should be taken to prevent injury to the intercostobrachial cutaneous nerve, which passes from the chest wall to the subcutaneous tissue in the center of the operative field. The dissection is extended cephalad next to the external intercostal fascia up to the first rib. The bluish vein leads to the neurovascular bundle. Its relationship to the first rib and both scalene muscles is clearly outlined to avoid injury to the neurovascular bundle. The insertion of the scalenus anticus muscle (SM) on the first rib is dissected and the muscle is divided at the tubercle (Fig. 43-2). The first rib is dissected subperiosteally and carefully separated from the underlying pleura to avoid pneumothorax. The rib is then divided at its middle portion, and a triangle of rib is removed with the vertex of the scalene tuberosity. The anterior portion of the rib is dissected away from the vein (Fig. 43-3). The costoclavicular ligament is divided, and the rib is removed from its sternal attachment. The anterior venous compartment is decompressed. The posterior segment of the rib is dissected from
P.694
the subclavian artery and brachial plexus. The scalenus medius muscle should be stripped with a periosteal elevator, being careful to avoid injuring the long thoracic nerve that lies on its posterior margin. The dissection is carried to the articulation with the transverse process of the vertebra and the rib divided (Fig. 43-4). Complete removal of the neck and head of the first rib is achieved using special Urschel pituitary and Urschel-Lexel rongeurs (Fig. 43-5). The eighth cervical and first thoracic nerve roots are carefully preserved. If a cervical rib is present, it is removed at this time, and the seventh cervical nerve root may be visualized. Only the subcutaneous tissues and skin require closure because no large muscles have been divided. Minimal traction is required for exposure and no significant brachial plexus stretching or neuritis has been observed. The patient is encouraged to use the arm normally and can be discharged from the hospital 2 days after the surgical procedure.
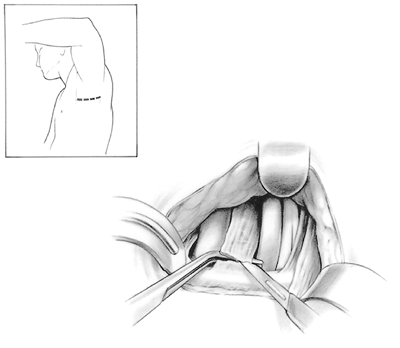 |
Fig. 43-2. Incision: The incision is transaxillary below the hairline, and transverse between the pectoralis major muscle anteriorly and the latissimus dorsi muscle posteriorly (inset). The incision is carried directly to the chest wall without angling up toward the first rib. When the chest wall is encountered, the dissection is carried superiorly to the first rib, identifying the intercostal brachial nerve that exits between the first and second ribs. It is preserved by retracting it anteriorly or posteriorly. (Division produces 6 months to 1 year of paresthesias on the inner surface of the upper arm.) The first rib is dissected subperiosteally with a Shaw-Paulson periosteal elevator and the scalenus anticus muscle identified. A right-angle clamp is placed behind the muscle, being careful not to injure the subclavian artery or vein. The SM is divided near its insertion on the first rib. (This prevents injury to the phrenic nerve, which courses away from the muscle at this level.) |
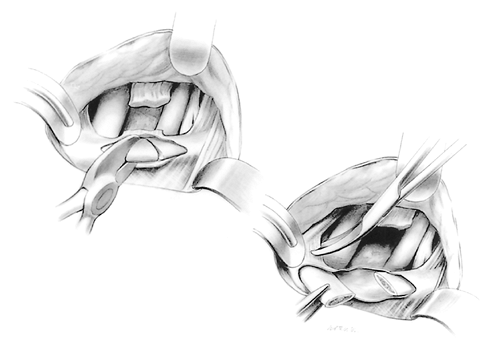 |
Fig. 43-3. Dissection: After dividing the scalenus muscle, the first rib is dissected free subperiosteally and separated from the pleura. A triangular piece of the rib is removed in the avascular area. The vertex of the triangle removed is at the scalene tubercle. The anterior part of the rib is removed by dividing the costoclavicular ligament and resecting the rib subperiosteally back to the costocartilage of the sternum. |
It is preferable to remove the entire first rib, including its head and neck, to prevent future irritation of the plexus from regenerated fibrocartilage.
Results
The clinical results of first rib resections in properly selected patients are good in 85%, fair in 10%, and poor in 5%. A good result is indicated by complete relief of symptoms,
P.695
a fair result by improvement with some residual or recurrent mild symptoms, and a poor result by no change from the preoperative status.
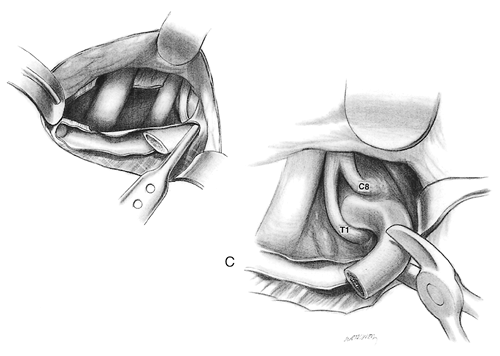 |
Fig. 43-4. Posterior rib dissection: The posterior part of the rib is dissected subperiosteally to the transverse process, where it is divided using a pair of rib shears. The rib may be resected posteriorly using an Urschel-Leksell reinforced rongeur. Care is taken to avoid injury to the C8 and T1 nerve roots as the scalenus medius muscle is dissected from the rib. |
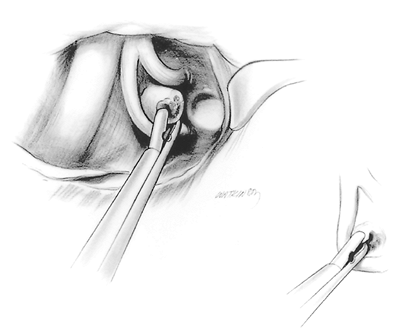 |
Fig. 43-5. Head and neck rib portion removal: After visualizing the transverse process articulation, the head and neck of the rib are removed using an Urschel reinforced pituitary rongeur. It is important to remove the complete head and neck of the rib so as to minimize regeneration. Care is taken not to injure the T1 nerve root below or the C8 nerve root above. Following complete removal of the first rib, neurolysis of C7, C8, and T1 nerve roots as well as the middle and lower trunks of the brachial plexus is performed. A video thoracoscope is used for this purpose because of its magnification and light. The scalenus medius and scalenus anticus muscles are resected up into the neck so that they will not reattach to Sibson's fascia or the pleura. |
Uniform improvement of symptoms is usually obtained in patients with primarily vascular compression.
In patients with predominantly nerve compression, however, two groups with different rates of improvement are observed. The first group includes patients with a spontaneous onset, the classic manifestations of ulnar neuralgia, and elicitation of pulse diminution, in which an average preoperative UNCV is reduced to 53 m/s. Ninety-five percent of patients in this group are improved by first rib resection.
In the second group are patients with a traumatic onset, with or without atypical pain distribution, who may or may not have shown pulse changes by compression tests and in whom the average preoperative UNCV was only reduced to 60 m/second. Surgical intervention is carried out in such patients as a therapeutic trial after prolonged conservative therapy has failed. Although many patients in the second group are improved, the fair and poor results mostly occur in these patients as noted by me and Razzuk (1998).
The UNCV and clinical status are highly correlated. Patients with good postoperative results have a preoperative average UNCV of 51 m/s and show return to a normal average of 72 m/s after operation. In those who have fair results, the preoperative UNCV averages 60 m/s and increases to an average of only 63 m/s after the operation. In the poor result group, no appreciable change occurs in the postoperative from the preoperative values. In fact, the average conduction time was only 58 m/s.
No hospital mortality has been directly related to this procedure. Postoperative morbidity after the transaxillary approach includes clinically inconsequential pneumothorax in 15%, hematoma in 1%, and infection in 0.1%. No significant nerve injury occurred.
PAGET-SCHROETTER SYNDROME
Effort thrombosis of the axillary-subclavian vein, or PSS, usually occurs as a result of unusual or excessive use of the arm in addition to the presence of one or more comprehensive elements in the thoracic outlet that I and Razzuk discussed in our two reports (1991, 2000).
Sir James Paget, in 1875 in London, and von Schroetter, in 1884 in Vienna, independently described this syndrome of thrombosis of the axillary-subclavian vein. The word effort was added to thrombosis because of the frequent association with exertion producing either direct or indirect compression of the vein. The thrombosis results from trauma or unusual occupations requiring repetitive muscular activity, as have been observed in professional athletics, Linotype operators, painters, and beauticians. Cold and traumatic factors, such as carrying skis over the shoulder, tend to increase the proclivity for thrombosis. Elements of increased thrombogenicity also increase the incidence of this problem and exacerbates its symptoms on a long-term basis. At surgery, all PSS patients have demonstrated lateral insertion of the costoclavicular ligament on the first rib or beyond.
Adams and DeWeese (1971) reported long-term results in patients treated conservatively with elevation and warfarin. They noted a 12% incidence of pulmonary embolism. Development of occasional venous distention occurred in 18%, and late residual arm symptoms of swelling, pain, and superficial thrombophlebitis were noted in 68% of patients (i.e., deep venous thrombosis with postphlebitic syndrome). One patient had phlegmasia cerulea dolens.
The natural history of PSS suggests moderate morbidity with conservative treatment alone as recorded by Machleder (1993). Bypass with vein or other conduits has not been very successful. Causes other than TOS must be treated individually. Intermittent obstruction of the subclavian vein can lead to thrombosis, and decompression should be used prophylactically.
For years, patients with effort thrombosis were treated with anticoagulants and conservative exercises; if recurrent symptoms developed when they returned to work, they were considered candidates for first rib resection. Use of thrombolytic agents with early surgical decompression of the neurovascular compression has reduced morbidity, such as a postphlebitic
P.696
syndrome, and the necessity for thrombectomy. In 67 patients seen by me and Razzuk (1991, 2000) over a 25-year period, the patients were initially treated with heparin sodium and then warfarin sodium (Coumadin, DuPont Pharma, Wilmington, DE, U.S.A.). Recurrent symptoms developed in 54 (80.5%) of these patients after they returned to work, necessitating transaxillary first rib resection to relieve symptoms. Over 600 patients with PSS subsequently have been treated with early thrombolytic therapy and prompt first rib resection with excellent results. This is by far the best management, as I and Patel (2003) have recorded.
RECURRENT THORACIC OUTLET SYNDROME
Extirpation of the first rib offers relief of symptoms in patients with TOS that is not improved by physiotherapy. Ten percent of surgically treated patients develop variable degrees of shoulder, arm, neck, and hand pain, as well as paresthesias. These are usually mild and short lasting and usually respond well to a brief course of physiotherapy and muscle relaxants. In 1.6% of patients, however, symptoms persist, become progressively more severe, and often involve a wider area of distribution because of entrapment of the intermediate trunk in addition to the lower trunk and C8 and T1 nerve roots. Symptoms may recur from 1 month to 10 years after an initial rib resection. However, most recurrence is within the first 3 months, as I and my colleagues (1976) have noted. Symptoms consist of aching or burning pain, often associated with paresthesia, involving the neck, shoulder, parascapular area, anterior chest wall, arm, and hand. Vascular lesions are uncommon and consist of causalgia minor and infected false aneurysms.
Two distinct groups of patients require reoperation. Pseudorecurrences happen in patients who never had relief of symptoms after the initial operation. Cases can be separated etiologically as follows: (a) the second rib was mistakenly resected instead of the first, (b) the first rib was resected, leaving a cervical rib, (c) a cervical rib was resected leaving an abnormal first rib, or (d) a second rib was resected leaving a rudimentary first rib. The second group includes patients whose symptoms were relieved after the initial operation but who developed recurrence because a significant piece of the first rib was left in place at the initial operation and a small subgroup who had complete resection of the first rib but demonstrated excessive scar formation involving the brachial plexus, as described by me and Razzuk (1986).
Physiotherapy should be instituted in most patients with symptoms of neurovascular compression after first rib resection. (This may not be necessary for pure vascular recurrence.) If symptoms persist and conduction velocity remains below normal, reoperation is indicated.
Reoperation for recurrent TOS is performed through the high posterior thoracoplasty approach described by Clagett (1962) to provide better exposure of the nerve roots and brachial plexus, thereby reducing the danger of injury to these structures as well as providing adequate exposure of the subclavian artery and vein. It also provides a wider field for easy resection of any bony abnormalities or fibrous bands and allows extensive neurolysis of the nerve roots and brachial plexus, which are not always accessible through the limited exposure of the transaxillary approach. I (1987) believe that the anterior or supraclavicular approach is inadequate for reoperation.
The basic elements of reoperation include: (a) resection of persistent or recurrent bony remnants of either a cervical or the first rib, (b) neurolysis of the brachial plexus and nerve root, and (c) dorsal sympathectomy. Sympathectomy removes the TI, T2, and T3 thoracic ganglia. The surgeon should avoid damaging the C8 ganglion (upper aspect of the stellate ganglion), which produces Horner's syndrome. The sympathectomy provides relief of major and minor causalgia and alleviates the paresthesias in the supraclavicular and interclavicular areas. The incidence of postsympathetic syndrome has been negligible in this group of patients. The use of a nerve stimulator to differentiate scar from nerve root is cardinal in avoiding damage in reoperation.
The technique of the operation includes a high thoracoplasty incision, extending from 3 cm above the angle of the scapula, halfway between the angle of the scapula and the spinal processes, and caudad 5 cm from the angle of the scapula. The trapezius and rhomboid muscles are split the length of the incision. The scapula is retracted from the chest wall by incising the latissimus dorsi over the fourth rib. The posterior superior serratus muscle is divided, and the sacrospinalis muscle is retracted medially. The first rib remnant and cervical rib remnant, if present, are located and removed subperiosteally. After the rib remnants have been resected, the regenerated periosteum is extirpated. In my experience, most regenerated ribs occur from the end of an unresected segment of rib rather than from the periosteum, although the latter is possible. As I have stressed, at the initial operation it is important to remove the first rib totally to reduce the incidence of bony regeneration in all patients with primarily nerve compression and pain symptoms.
If excessive scarring is present after removal of any rib remnant, it may be prudent to perform the sympathectomy initially. This involves resection of a 1-in (2.5-cm) segment of the second rib posteriorly to locate the sympathetic ganglion. In that way, the first thoracic nerve may be easier to locate beneath rather than through the scar.
Neurolysis of the nerve root and brachial plexus is performed using a nerve stimulator. Neurolysis is carried down to but not into the nerve sheath. It is extended peripherally over the brachial plexus as far as any scar persists. Excessive neurolysis is not indicated, and opening of the nerve sheath may produce more scar than it relieves. To minimize excessive scarring, efforts in the initial operation for thoracic outlet syndrome should include complete extirpation of the first rib; avoidance of hematomas by adequate drainage, either by catheter or by opening the pleura; and avoidance of infection.
P.697
The subclavian artery and vein are released if symptoms mandate. The scalenus medius muscle is d brided. The dorsal sympathectomy is completed via extrapleural dissection. Meticulous hemostasis is affected, and a large Jackson-Pratt catheter drain is placed in the area of the brachial plexus, but not touching it. This drain is brought out through the subscapular space through a stab wound into the axilla. Methylprednisolone acetate (Depo-Medrol, Pharmacia & Upjohn, Peapack, NJ, U.S.A.), 80 mg, is left in the area of the nerve plexus, although the patient is not given systemic steroids unless keloid formation has previously occurred. Hyaluronic acid is left in the area of neurolysis to minimize recurrent scarring. The wound is closed in layers with interrupted heavy Vicryl sutures to provide adequate strength, and the arm is kept in a sling and should be used carefully for the first 3 months. Range-of-motion exercises are prescribed to prevent shoulder limitation. However, overactivity is contraindicated because it may result in excessive scar formation.
When the problem is vascular, involving false or mycotic aneurysms, special techniques for reoperation are used. A bypass graft is interposed from the innominate or carotid artery proximally, through a separate tunnel distally, to the brachial artery. Usually, the saphenous vein is used, although other conduits may be selected. The arteries feeding and leaving the infected aneurysm are ligated. At a subsequent stage, the aneurysm is resected through a transaxillary approach with no fear of bleeding or ischemia of the arm.
Special instruments have been devised to provide adequate resection through the transaxillary or posterior route. These include a modified strengthened pituitary rongeur and a modified Leksell double-action rongeur for first rib removal without danger to the nerve root. The sympathectomy relieves chest wall pain that mimics angina pectoris, esophageal disease, or even a lung tumor by denervating the deep fibers that travel with the arteries and bone.
Results of reoperation have been excellent if an accurate diagnosis was established and the proper procedure was executed. Follow-up of more than 2,000 patients has ranged from 6 months to 35 years. All patients improved initially after reoperation: in 79%, improvement was maintained for more than 5 years. Fourteen percent of patients developed symptoms that were easily managed with physiotherapy. Seven percent of patients required a second reoperation, in every instance because of rescarring. No deaths occurred, and only one case of significant infection requiring drainage was recorded.
REFERENCES
Adams JT, DeWeese JA: Effort thrombosis of the axillary and subclavian veins. J Trauma 11:923, 1971.
Adson AW: Cervical ribs: symptoms, differential diagnosis for section of the scalenus anticus muscle. J Int Coll Surg 16:546, 1951.
Caldwell JW, Crane CR, Krussen EM: Nerve conduction studies: an aid in the diagnosis of the thoracic outlet syndrome. South Med J 64:210, 1971.
Clagett OT: Presidential address: research and prosearch. J Thorac Cardiovasc Surg 44:153, 1962.
Falconer MA, Li FWP: Resection of the first rib in costoclavicular compression of the brachial plexus. Lancet 1:59, 1962.
Jebsen RH: Motor conduction velocities in the median and ulnar nerves. Arch Phys Med Rehab 48:185, 1967.
Kuntz A: Afferent innervation of peripheral blood vessels through sympathetic trunks. South Med J 44:673, 1951.
Lang EK: Roentgenographic diagnosis of the neurovascular compression syndromes. Radiology 79:58, 1962.
Machleder HI: Evaluation of a new treatment strategy for Paget-Schroetter syndrome: spontaneous thrombosis of the axillary-subclavian vein. J Vasc Surg 17:305, 1993.
Paget J: Clinical Lectures and Essays. London: Longmans Green, 1875.
Roos DB: Transaxillary approach for first rib resection to relieve thoracic outlet syndrome. Ann Surg 163:354, 1966.
Roos DB, Owens JC: Thoracic outlet syndrome. Arch Surg 93:71, 1966.
Rosati LM, Lord JW: Neurovascular compression syndrome of the shoulder girdle. In Modern Surgical Monographs. New York: Grune & Stratton, 1961, p. 168.
Sharafuddin MJ, Sun S, Hoballah JJ: Endovascular management of venous thrombotic diseases of the upper torso and extremities. J Vasc Interv Radiol 13:975, 2002.
Urschel HC Jr: Management of the thoracic outlet syndrome. N Engl J Med 286:1140, 1972.
Urschel HC Jr: Thoracic outlet syndrome: reoperation. In Grillo HC, Eschapasse H (eds): International Trends in General Thoracic Surgery: Major Challenges. Vol. 2. Philadelphia: WB Saunders, 1987, p. 374.
Urschel HC Jr, Patel AN: Paget Schroetter syndrome therapy: failure of intravenous stents. Ann Thorac Surg 5:1693, 2003.
Urschel HC Jr, Razzuk MA: The failed operation for thoracic outlet syndrome: the difficulty of diagnosis and management. Ann Thorac Surg 42:523, 1986.
Urschel HC Jr, Razzuk MA: Improved management of the Paget-Schroetter syndrome secondary to thoracic outlet compression. Ann Thorac Surg 52:1217, 1991.
Urschel HC Jr, Razzuk MA: Neurovascular compression in the thoracic outlet: changing management over 50 years. Ann Thorac Surg 228:609, 1998.
Urschel HC Jr, Razzuk MA: Paget-Schroetter syndrome: what is the best management? Ann Thorac Surg 69:1693, 2000.
Urschel HC Jr, et al: Objective diagnosis (ulnar nerve conduction velocity) and current therapy of the thoracic outlet syndrome. Ann Thorac Surg 12:608, 1971.
Urschel HC Jr, et al: Thoracic outlet syndrome masquerading as coronary artery disease (pseudoangina). Ann Thorac Surg 16:239, 1973.
Urschel HC Jr, et al: Reoperation for recurrent thoracic outlet syndrome. Ann Thoracic Surg 21:19, 1976.
von Schroetter L: Erkrankugnan der Gefasse. In Nathaogel R (ed): Handuch der Pathologic und Therapie. Vienna: Holder, 1884.
Wolf RK, Craword AH, Hann B: Thoracoscopic first rib resection for thoracic outlet syndrome. In Yim AP, et al (eds): Minimal Access Cardiothoracic Surgery. Philadelphia: WB Saunders, 2000, p. 328.
Reading References
Adson AW, Coffey JR: Cervical rib: a method of anterior approach for relief of symptoms by division of the scalenus anticus. Ann Surg 85:839, 1927.
Aziz S, Strachley CJ, Whelan TJ Jr: Effort-related axillosubclavian vein thrombosis. A new theory of pathogenesis and a plea for direct surgical intervention. Am J Surg 152:57, 1986.
Molina JE: Surgery for effort thrombosis of the subclavian vein. J Thorac Cardiovasc Surg 103:341, 1992.
Rob CG, Standover A: Arterial occlusion complicating thoracic outlet compression syndrome. BMJ 2:709, 1958.
Roos DB: Experience with first rib resection for thoracic outlet syndrome. Ann Surg 173:429, 1971.
Telford ED, Mottershead S: Pressure at the cervicobrachial junction. J Bone Joint Surg Am 30:249, 1948.
Urschel HC Jr, Paulson DL, McNamara JJ: Thoracic outlet syndrome. Am Thorac Surg 61:1, 1968.
EAN: 2147483647
Pages: 203