5 - The Process and Economics of Heart Failure
Editors: Peacock, W. Frank
Title: Short Stay Management of Heart Failure, 1st Edition
Copyright 2006 Lippincott Williams & Wilkins
> Table of Contents > 5 - The Process and Economics of Heart Failure
5
The Process and Economics of Heart Failure
Sandra Sieck
Introduction
Heart failure (HF) is the only cardiac disease whose incidence and prevalence are increasing, a trend that threatens to impose an exponentially increasing burden on the health care system.1,2 This burden impacts patients, providers, insurers, health care suppliers, and particularly hospitals, where the majority of health care is rendered to those with acute decompensated heart failure (ADHF).
Much progress has been made in the clinical treatment of HF with aggressive pharmacologic and device therapies, but the difficulty in treating these patients effectively while maintaining a healthy balance of economic viability is the goal of the acute care facility. Defining and implementing optimal care that is cost-effective and results in best clinical outcomes, quality of life, and satisfaction of patient and providers has been a challenge to the health care delivery system. As advances in technology add increasing costs to the treatment of HF patients, reimbursements remain limited and place the onus on the acute care facility to ensure the provision of cost-efficient care while maintaining a high of quality of care. As the population ages, the health care system will be forced to develop more innovative approaches to the care and treatment of patients with chronic diseases that are prone to exacerbations resulting in costly health care utilization.
Burden of Disease
HF is responsible for more elderly patient hospitalizations than any other disease1 High readmission rates 20% at 30 days and 50% at 6 months also contribute to the staggering figure: a total of 6.5 million hospital days are expended to treat ADHF.3 Hospital discharges for HF in 2001 were estimated to be approaching 1 million (Figure 5-1). In fact, HF is the most commonly used Medicare diagnosis-related group (DRG).4 The high utilization not only is reflected in the inpatient sector, this diagnosis also accounts for 12 to 15 million office visits annually.5 These utilization figures have continued on an increasing trend over the last 2 decades.
P.40
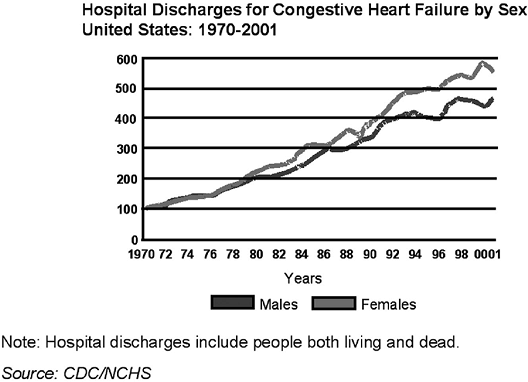 |
FIGURE 5-1 Trends in U.S. hospital discharge rates. From American Heart Association 2004 Statistical Update, p. 24 (Fig. 2). |
HF patients are considerably expensive patients as well and contributed to $25.8 billion in 2004 in direct and indirect costs to the United States.6 Compared with other cardiac conditions, HF accounts for more than 10% of total costs for all cardiovascular conditions (Table 5-1). Although charges for medications, provider fees, and nursing care contribute to these costs, the majority of the expenditures are related to acute hospitalizations (Figure 5-2). These figures substantiate the large health care burden of HF, both clinically and financially. Although these figures represent high-level economic views, the overall burden can easily be translated to the level of the individual hospital.
Current Practices
Currently, the majority of ADHF patients are treated in the inpatient environment. The emergency department (ED) is the point of entry for three out of every four ADHF patients, and 75% to 90% of HF patients presenting to the ED are ultimately admitted to the hospital.7,8 Once admitted to the hospital, the average length of stay (LOS) is 7.0 days.9
After the Balanced Budget Act of 1997 and the Refinement Act of 1999, hospitals began struggling and continue to struggle with the Inpatient Prospective Payment System (IPPS) and the Outpatient Prospective Payment System (OPPS). Most facilities are reimbursed for ADHF patients on a fixed inpatient payment under the DRG system and must operate with optimal efficiency to maintain financial viability.
P.41
TABLE 5-1 Cardiovascular Disease Costs (in $billion) in the United States | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
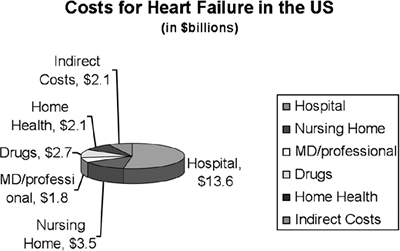 |
FIGURE 5-2 Costs for heart failure in the United States. Data taken from Table 5-1. |
P.42
Placement of the ADHF patient in an inpatient bed can easily consume the average Medicare payment of $4,617 currently reimbursed for DRG 127 under the IPPS. With an average LOS of more than 5 days combined with the break-even point for most hospitals occurring at about 5 days, most hospitals are not adequately reimbursed to cover these costs.10 In a review of 2001 cost data, the average hospital lost $1,288 per ADHF patient.10 Such losses obviously represent a serious impact on a hospital's operation and fiscal stability.
Another unique characteristic of reimbursement under Medicare affects the HF patient who has been recently discharged after an acute admission and is readmitted within 30 days. Nearly 20% of patients discharged from an acute hospitalization for exacerbation of congestive heart failure (CHF) are readmitted within 30 days, and 50% are readmitted within 6 months.11,12 With repeat admissions within a 30-day period, payment is not guaranteed and potential audits could occur. Return visits create burden of proof on the facility with medical necessity to justify the return visit within 30 days. Medicare may not reimburse the hospital, and payment could be vulnerable at the expense of the facility. Because most HF patients are covered under Medicare, many hospitals are faced with a fiscal loss when rendering care to the ADHF patient under the current Medicare DRG reimbursement levels. The relative weight of DRG 127 (HF) is less than DRG 89 Pneumonia. Of course, the current practice patterns regarding inpatient admissions contribute to these fiscal problems. As hospitals are seeing increasingly ill patients, it is becoming more difficult to offset these losses by caring for other conditions. Therefore, acute care facilities are forced to find alternative solutions in providing quality care for ADHF in a fiscally sound manner.
Emergence of the Observation Unit
In general, efforts in health care delivery are moving in the direction of providing more services in the outpatient setting. Care in such settings is commonly less costly and more efficient. As an example, chest pain centers (CPCs) again began to emerge in the late 1990s for patients presenting with chest pain, as a more efficient way of ruling out myocardial infarction in low-risk patient subsets. The method proved not only more logistically efficient but more cost-effective as well.
The Centers for Medicare and Medicaid Services (CMS) have now targeted chest pain, asthma, and HF for efforts to reduce morbidity and mortality through use of intense treatment in nonacute care settings. This strategy, coupled with the positive experiences gained from the CPCs, has led to the emergence of the observation unit (OU), a service provided on-hospital premises, including use of a bed and periodic monitoring by nursing or other staff, which are reasonable and necessary to evaluate an outpatient's condition or determine the need for possible admission as an inpatient. 13
P.43
TABLE 5-2 Utilization of Observation Units | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Use of the OU has dramatically increased over the last few years (Table 5-2). Between 2002 and 2003, there was an 85% increase in OU utilization. Chest pain represented the most common condition seen in an OU, followed by gastrointestinal disorders and asthma.14 ADHF accounted for 5% of OU conditions in 2002 to 2003.
In April 2002, CMS developed a new coding and reimbursement rate for patients who are placed into OU services for these conditions. Ambulatory Patient Classification Code (APC) 0339 was designed to relieve some of the pressures of treating CHF patients aggressively on the front end of the process versus admitting the patients into an acute care setting. This new APC 0339 code is currently reimbursed at $408 pending that the minimal requirements for receiving this payment are met. These requirements include a stay of 8 to 24 hours, up to 48 hours, with appropriate documentation. No consideration for greater than 24 hours was made in regard to the additional OU payment. Also, most diagnostic tests that are performed during the OU stay are billable and reimbursable separately from the OU stay, as deemed medically necessary (Table 5-3).
Another benefit of APC 0339 for the hospital is that revisits occurring within 30 days or admissions to the hospital after an OU visit are all reimbursable. There is no restriction to the number of claims that can be submitted for a patient if billed under the APC outpatient system. Also, if a patient is admitted to an OU and then requires an inpatient hospital admission at that same point of contact, there is no penalty. The hospital does not get the APC outpatient reimbursement but instead receives the full DRG inpatient reimbursement.
Cost-Effectiveness of the Ou
The OU provides a location for the provision of intense medical therapy and services under close observation and frequent monitoring of response to treatment. In the ADHERE data registry (a multicenter, observational database of patients discharged from the hospital with a DRG diagnosis of HF), the time to initiation of administration of certain intravenous (IV) medicines specifically directed at acute HF was 1.1 hours if the patient's
P.44
treatment was initiated in the ED, compared with 22 hours if therapy was begun in an inpatient unit.15 The OU has definitive protocols for both treatment and timely adjustments in treatment plans based on the clinical parameters being observed. Such a methodology leads to more intense and timely initiation of therapy. This drastic variation in timing can have remarkable differences in clinical outcomes, as well as a dramatic impact on financial implications (Figure 5-3).
TABLE 5-3 Comparison of Medicare Reimbursements for ADHF Financial Template | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
Treatment of ADHF in an OU has resulted in reduced 30-day readmissions and hospitalizations and decreased LOS if a subsequent hospitalization is required.16 The ADHERE data showed that early initiation of IV vasoactive therapy can reduce the hospital LOS from an average of 7.0 days to 4.5 days.17 Because LOS is the greatest contributor to hospital costs for the ADHF patient, and up to 75% of ADHF cases admitted to an OU can ultimately be discharged directly from the OU, the potential impact on overall hospital utilization can be substantial.10,18
P.45
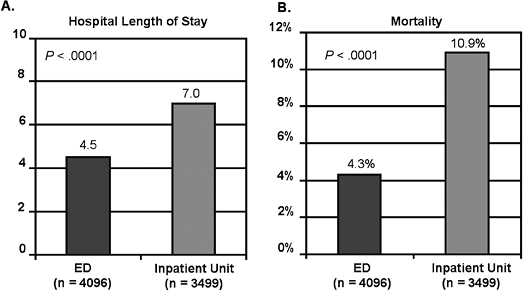 |
FIGURE 5-3 Effect of site initiation of therapy on length of stay and mortality. ED, emergency department. From Emerman CL. Treatment of the acute decompensation of heart failure: efficacy and pharmacoeconomics of early initiation of therapy in the emergency department. Rev Cardiovasc Med 2003;4(Suppl 7):S13 S20. |
In an analysis of The Cleveland Clinic experience using the OU as a venue for treatment of the ADHF patient, they reported positive 90-day outcomes (Table 5-4):19
Revisits were reduced by 44%
ED observation discharges increased by 9%
HF rehospitalizations were reduced by 36%
Observation rehospitalizations were reduced by 39%
The authors believed this impact on outcomes was due to application of testing on presentation to the OU, patient education, and early and aggressive treatment with pharmacologic therapies.
TABLE 5-4 90-Day Utilization Rates in ADHF Related to OU Treatment Venue | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||
The new APC reimbursement coding can also result in better profitability for the acute care facility. By carefully selecting appropriately risk-stratified ADHF patients and placing appropriate resources in the ED that can result in initiation of drug therapies in the 1-hour window,
P.46
hospitals can recognize a positive financial margin per case (Table 5-5). This difference in profitability comes partly from the new CMS reimbursement coding. Although the reimbursement levels for APC 0339 are smaller compared with the DRG reimbursement for a hospitalization, the operational expenses for an OU stay are also smaller. Overhead costs are generally less in the ED or outpatient units when compared with inpatient treatments because of the productivity and turnover rate of the beds. Thus, intense therapy for ADHF that results in a short stay in an OU can actually result in a profit for the hospital facility. However, the ability to show a profit in the ADHF patient still requires a redesign of the current system and attention to an early risk-stratified, protocol-driven process to be successful.
TABLE 5-5 Utilization and Cost Differences Based on Medicare Reimbursement Type | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
Current Medicare DRG reimbursements put extreme pressure on facilities to maintain effective treatment options available to the growing ADHF population. Facilities must explore and evaluate the advantages of using observation services that will allow the placement of traditional technologies and protocols at the point of contact with HF patients versus allowing the patients to be placed into the system only to recognize they could have been effectively identified, risk stratified, and treated more efficiently on the front end of the their presentation.
Clinical Outcomes
Process improvement initiatives appear to be the focus of government and other agencies attempting to reduce morbidity and mortality as well as increase other quality outcomes. With 550,000 new incident HF cases annually, health care delivery systems are seeing a tremendous increase in the number of patients presenting to EDs across the nation. Improved
P.47
disease management and an emphasis on process are critical toward attaining improved clinical outcomes in this set of patients.
Some argue that attempts to increase quality of care are inherently more costly due to the use of more therapeutic and diagnostic interventions. However, the overall impact of high-quality care could reduce total costs by diminishing unnecessary health care utilization that results from inappropriate or inadequate care.
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has created a set of quality performance indicators for HF.20 These indicators include objective measurement of ejection fraction, angiotensin-converting enzyme (ACE) inhibitor treatment if tolerated, provision of complete discharge instructions, and smoking cessation counseling. In an analysis of the ADHERE registry data, only 30% of ADHF patients meet these quality requirements.21 Although OU management has been demonstrated to reduce morbidity and a trend toward reduced mortality, further studies are needed to assess the full impact of OU care on quality measures.22,23
Disease management efforts for HF have demonstrated improved clinical outcomes and quality of care measures in selected populations as shown in the CMS/Premier Project launched in 2003. Clearly, third-party insurers and employers are increasingly seeking methods to merge quality care with cost reductions. Medicare has recently initiated a demonstration project to determine how disease management efforts can affect cost and quality in the senior population. Many health plans are beginning pay-for-performance programs that reward providers and facilities for providing higher quality care. Although quality appears to be the focus of such efforts, there is an underlying belief that such care will also reduce overall costs. Thus, marrying cost and quality is becoming a theme in today's health care environment.
Transtheoretical Y-Model
Hospitals must merge quality and finance to create a viable plan of operation. Although this is a common concept in the business world, it has not yet been incorporated throughout the health care arena. The transtheoretical Y-model is a new approach that allows facilities to closely examine different aspects of operations within their systems.23 It encompasses the concept of health care delivery along a continuum from the point of entry into the system through to discharge. This Y-model can be applied to the overall operations of these systems or to one specific disease, such as HF. By applying variations of the Y-model, in which all focus is on the end points of quality and cost, facilities can recognize ways to turn CHF from a negative contribution margin to one that breaks even or contributes favorably.
Using the transtheoretical Y-model in the health care setting can be compared with an industrial setting. Industrial facilities can examine the
P.48
exact route from raw material to finished product with detailed accuracy. The end product is priced to the market based on the operating costs within the process. If the manufacturing process varies greatly over time, costs of production rise and are passed on in a higher market price. To keep prices down, actions must be taken to get the variances under control. If not, the contribution margin is eroded and eventually could become negative. The objective is to keep the contribution margin at its maximum without compromising quality.
This model can be similarly applied to an ADHF patient routing through the health care delivery setting. Patients receive services within different care units within the acute hospital setting. These care units are analogous to the industrial setting's business units. By understanding how each care unit's operational strategies affect each subsequent care unit from point of entry to discharge, a seamless transfer of patient care in both outpatient and inpatient settings can optimize quality improvement and positive economic value. Without each care unit providing vital information to others in this holistic approach, moving patients efficiently through the system is challenged.
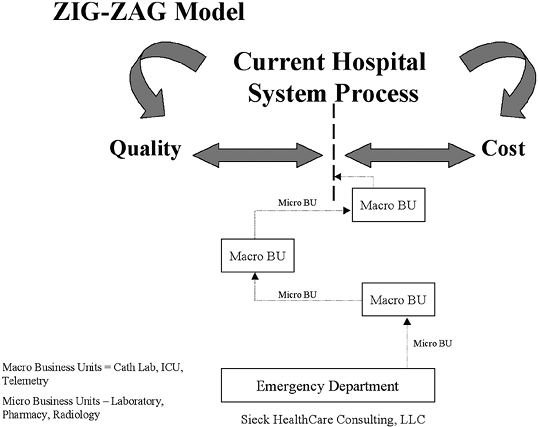 |
FIGURE 5-4 The zig-zag model of care. BU, business unit; ICU, intensive care unit. From Sieck S. Cost effectiveness of chest pain units. Cardiol Clin 2005;23(4):598. |
The current processes in health care delivery to the ADHF patient are more characteristic of a zig-zag model (Figure 5-4). An ADHF patient enters through the ED and receives treatments and evaluations through
P.49
multiple disconnected service sectors or care units (known as business units in the commercial sector). These care units are represented by nursing, electrocardiogram (ECG) department, radiology department, pharmacy, laboratory, and so forth. Each of the care units is viewed and acts as a single independent business unit from the standpoint of the hospital. The outputs of these care units' activities are collated by the provider, usually once the patient has been admitted to the acute hospital bed. It is then, at the back end of the process, that care treatment plans are decided on. The zig-zag model is a disconnected and fragmented model.
The transtheoretical Y-model represents a different approach and provides a template to facilities on optimizing covering costs of care by placing the proper resources at the front end of the point-of-care entry. This concept begins at the point of entry and ends at discharge and marries a clinical and financial strategy that meets quality indicators while producing desirable profit margins. Beginning in the ED, this concept emphasizes an efficient, rapid assessment and action centered on a seamless integration of ancillary services, such as the laboratory, diagnostic imaging, and skilled nursing, while understanding the economic impacts on decisions made as the patient is directed through the system.
Using this template can impact quality, costs, efficiency, and clinical outcomes. This model provides a more accurate breakdown on the exact volume by International Classification of Disease, Ninth Revision (ICD-9) codes instead of the inpatient DRG to give a more accurate picture of the number of patients that are passing through the outpatient door within a system. With this analysis and the proper guidance, facilities can target this and other diseases more effectively. Patients who require an inpatient admission are properly admitted, and those who could be effectively treated in the outpatient setting are treated and properly released. The placement of more critical patients in the inpatient acute care setting impacts the case mix index positively because the patients are simply sicker and require more resources.
Creating a new care delivery system for the ADHF patient that is based on the transtheoretical Y-model can positively impact the contribution margins when ADHF patients are carefully identified, risk stratified, and given appropriate early treatment during the interaction (Figure 5-5). This model emphasizes a multidisciplinary team approach to align the care units that affect an ADHF patient's progress through the current system. The emphasis is on front-end compliance that sets up the pathway the patient will follow (Figure 5-6). A patient is not arbitrarily admitted to an inpatient bed, treated, and then discharged. A decision is made upfront on the most ideal care venue for the risk-stratified patient to be admitted to and undergo tailored treatment. It also initiates the financial pathway with identified markers throughout the patient interaction that allows facilities to know the ramifications of making random decisions versus following a protocol designed to emphasize quality while optimizing economic results. The transtheoretical Y-model places an emphasis on
P.50
P.51
process improvement while targeting the end points of quality and contribution margin (Figure 5-7).
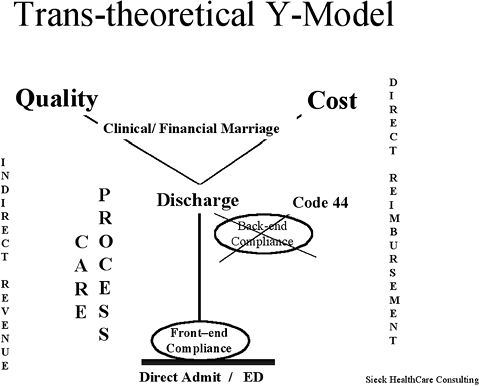 |
FIGURE 5-5 The transtheoretical Y-model. ED, emergency department. From Sieck S.Cost effectiveness of chest pain units. Cardiol Clin 2005;23(4):597. |
 |
FIGURE 5-6 Use of transtheoretical Y-model to maximize cost-efficiency. ED, emergency department; JCAHO, Joint Commission on Accreditation of Healthcare Organizations. From Sieck S.Cost effectiveness of chest pain units. Cardiol Clin 2005;23(4):597. |
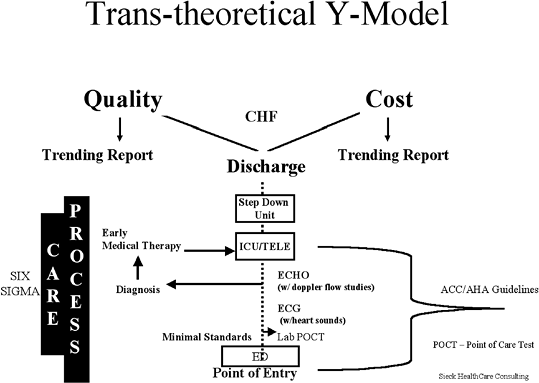 |
FIGURE 5-7 Quality and cost impact of the transtheoretical Y-model. ACC/AHA, American College of Cardiology/American Hospital Association CHF, congestive heart failure; ECG, electrocardiogram; ED, emergency department; ICU, intensive care unit. From Sieck S. Cost effectiveness of chest pain centers Cardiol Clin 2005;23(4):597. |
This variation of the model was recently used successfully at a southern medical center for an initiative on acute coronary syndrome (ACS). Prior to the initiative the hospital had a zig-zag model of care. Patients entered through the ED and were admitted to the acute care bed, and laboratory tests were completed and treatment initiated several hours into the process. With initiation of the Y-model, stratification was performed and appropriate therapy initiated in the ED with point-of-care testing in a patient-centric improvement effort. The new design resulted in improvements in turnaround time for therapy, reduced LOS, enhanced patient placement in the most appropriate bed venue [e.g., critical care unit (CCU), telemetry, or clinical decision unit], and improved patient satisfaction.
Improvements demonstrated in the ACS redesign can be translated to the ADHF setting. Similar to the ACS patient, not every ADHF patient absolutely requires a CCU or OU bed. Similarly, not all ADHF patients are candidates for the OU. Point-of-entry triaging to the most appropriate care unit where an individualized treatment plan is rendered allows a facility to better merge quality care with positive financial outcomes.
P.52
Conclusions
Health care delivery systems must explore innovative strategies and health care redesign to provide cost-effective quality treatment to ADHF patients. Inconsistent and inefficient treatments contribute to poor clinical and economic outcomes. CMS is shifting patients from inpatient to outpatient services in an attempt to relieve the inpatient burden placed on hospital services while simultaneously alleviating the economic problems encountered when treating this unique class of patients. These forces create fiscal and logistic challenges for the hospital, which can ultimately impact the institution's survival.
The transtheoretical Y-model offers a solution that is focused mainly on process improvement techniques and the economic impacts these changes can have on the hospital system. The core of the model is based on merging quality and finance. Although financial aspects of care play a vital role in this model, economics cannot be considered a higher priority than clinical outcomes. The model treats these two parameters as equally important to the successful implementation of a redesigned care process for the ADHF patient population.
References
1. Peacock WF, Albert NM. Observation unit management of heart failure. Emerg Med Clin North Am 2001;19:209 232.
2. Massie BM, Shah NB. Evolving trends in epidemiologic factors of heart failure: rationale for preventative strategies and comprehensive disease management. Am Heart J 1997;133:703 712.
3. Aghababian RV. Acutely decompensated heart failure: opportunities to improve care and outcomes in the emergency department. Rev Cardiovasc Med 2002;3[Suppl 4]:S3 S9.
4. Massie BM, Shah NB. Evolving trends in epidemiologic factors of heart failure: rationale for preventative strategies and comprehensive disease management. Am Heart J 1997;133:703 712.
5. O'Connell JB, Bristow M. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Transplant 1993;13:S107 S112.
6. AHA, ASA. Heart disease and stroke statistics 2004 update. Available at: http://www.americanheart.org/downloadable/heart/1072969766940Sstats2004Update.pdf (accessed September 13, 2004).
7. The Acute Decompensated Heart Failure National Registry (ADHERE): Opportunities to Improve Care of Patients Hospitalized with Acute Decompensated Heart Failure. Data on file January 2004.
8. Graff L, Orledge J, Radford MJ, et al. Correlation of the Agency for Health care Policy and Research congestive heart failure admission guideline with mortality: peer review organization voluntary hospital association initiative to decrease events (PROVIDE) for congestive heart failure. Ann Emerg Med 1999;34:429 437.
9. Emerman CL. Treatment of the acute decompensation of heart failure: efficacy and pharmacoeconomics of early initiation of therapy in the emergency department. Rev Cardiovasc Med 2003;4:S13 S20.
10. Peacock WF. Heart failure management in the emergency department observation unit. Prog Cardiovasc Dis 2004;46:465 485.
P.53
11. Aghababian RV. Acutely decompensated heart failure: opportunities to improve care and outcomes in the emergency department. Rev Cardiovasc Med 2002;3[Suppl 4]:S3 S9.
12. Jong P, Vowinckel E, Liv PP, et al. Prognosis and determinants of survival in patients newly hospitalized for heart failure: a population-based study. Arch Intern Med 2002;162:1689 1694.
13. Medicare Observation Status Reference. Volume, Issue IV, Jan 3, 2003.
14. Mace SE, Graff L, Mikhail M, et al. A national survey of observation units. Am J Emerg Med 2003;21:529 533.
15. Fonarow GC, for the ADHERE Scientific Advisory Committee. The Acute Decompensated Heart Failure Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure. Rev Cardiovasc Med 2003;4:S21 S30.
16. Peacock WF, Remer EE, Aponte J, et al. Effective observation unit treatment of decompensated heart failure. Congest Heart Fail 2002;8:68 73.
17. Peacock WF, Emerman CL, Costanzo MR, et al. Early initiation of IV vasoactive therapy improves heart failure outcome: an analysis from the ADHERE registry database. Ann Emerg Med 2003;42:526.
18. Peacock WF, Albert NM. Patient outcome and costs following an acute heart failure (HF) management program in an emergency department (ED) observation unit (OU) [abstract 240]. J Heart Lung Transplant 1999;18:92.
19. Peacock F. Management of acute decompensated heart failure in the emergency department. J Am Coll Cardiol 2003;4:336A.
20. www.jcaho.org
21. Fonarow GC, for the ADHERE Scientific Advisory Committee. The Acute Decompensated Heart Failure Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure. Rev Cardiovasc Med 2003;4:S21 S30.
22. Peacock WF. Acute emergency department management of heart failure. Heart Failure Rev 2003;8:335 338.
23. Sieck S. Cost effectiveness of chest pain units. Cardiol Clin 2005; 23(4):589 599, ix.
EAN: 2147483647
Pages: 18