42 - Infections of the Chest Wall
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section X - The Diaphragm > Chapter 52 - Formamen of Morgagni Hernia
Chapter 52
Formamen of Morgagni Hernia
Ronald B. Ponn
In 1769, Morgagni first described the rare anterior, retrosternal diaphragmatic defect that now bears his name. He noted this condition in the autopsy of an Italian stonecutter who died from gangrenous colon herniated through an opening beneath the sternocostal junction. Because Napoleon's surgeon, Larrey, described a surgical approach to the pericardial sac through an anterior retrosternal diaphragmatic defect, this area has also been termed the space of Larrey.
ANATOMY
The embryology of the diaphragm is discussed in Chapter 48. Lack of fusion or muscularization of the pleuroperitoneal membrane anteriorly leads to a defect in the costosternal trigones known as the foramen of Morgagni. This triangular space is located between the muscle fibers from the xiphisternum and the costal margin fibers that insert on the central tendon (Fig. 52-1). The internal mammary artery traverses this space to enter the rectus sheath and become the superior epigastric artery. Because the peritoneum is intact, there is usually a true hernia sac. In most cases, the hernia contains only omentum, but the colon is involved occasionally, and the small bowel or stomach rarely. A left-sided defect is less likely to result in herniation because it is protected by the pericardium. The ligamentum teres defines the medial border of the hernia on either side.
INCIDENCE
Clinically evident hernias through the foramen of Morgagni are uncommon at any age. Despite their congenital etiology, they are detected less often in children than in adults. Comer and Clagett (1966) reported 50 patients (7%) with foramen of Morgagni hernias of a total of 750 patients with diaphragmatic hernias of all kinds found over 32 years. Harrington (1948) listed only seven foramen of Morgagni hernias (1.5%) in a series of 430 patients who were operated on for diaphragmatic hernia. Overall, the incidence of Morgagni hernia among all diaphragmatic defects in adults and children is 3% to 4%. For the anatomic reason noted previously, about 90% of the hernias occur on the right, 8% are bilateral, and only 2% are limited to the left. Foramen of Morgagni hernias are detected more often in women than in men and more often in obese people than in those of average or below-average weight.
SYMPTOMS
In a literature review of 132 adult and pediatric cases, Berardi and associates (1997) reported that about one third of patients are asymptomatic. Those with symptoms most frequently describe chronic gastrointestinal complaints, such as crampy pain or constipation from partial intermittent colonic obstruction. Symptoms due to intermittent gastric volvulus or small bowel obstruction are less frequent. Patients often complain only of vague epigastric or substernal fullness or a dull right subcostal discomfort. Complete obstruction, incarceration, or strangulation with necrosis of a hollow viscus contained in a foramen of Morgagni hernia is rare and is associated with an acute or subacute presentation. In the aforementioned series, 12 patients had complete bowel obstruction, and one had gangrenous intestine.
Cardiorespiratory symptoms (mainly dyspnea and palpitations) are less common overall than gastrointestinal complaints. Although children are more often asymptomatic than adolescents and adults, they have about an equal incidence of respiratory and gastrointestinal symptoms.
As with other hernias, conditions that produce prolonged or sudden severe increased intraabdominal pressure can precipitate the onset of or exacerbate existing symptoms due to a foramen of Morgagni hernia. Valases and Sills (1988) reported that exercise and athletic activity may cause the occurrence of symptoms. Ellyson and Parks (1986) reported that trauma could initiate symptoms. Lin and Maginot (1999)
P.773
described a patient who became symptomatic during pregnancy.
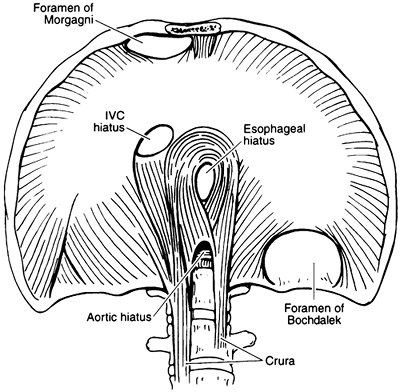 |
Fig. 52-1. Illustration of posterolateral (Bochdalek) and anterior (Morgagni) diaphragmatic hernia. Note location of the latter between muscle fibers from the xiphisternum and from the costal arch that insert on the central tendon. From Naunheim KS: Adult presentation of unusual diaphragmatic hernias. Chest Surg Clin North Am 8:359, 1998. With permission. |
DIAGNOSIS
The diagnosis of a foramen of Morgagni hernia is made by radiography, either prompted by symptoms or performed for unrelated reasons. In very small hernias, Lanuza (1981) described the sign of the cane : a curvilinear accumulation of fat continuous with the properitoneal fat line of the anterior abdominal wall. This sign suggests that a small anterior cardiophrenic mass may be a foramen of Morgagni hernia. More commonly, the standard chest radiograph shows obvious right, left, or bilateral pericardiophrenic abnormalities that are solid or contain air. The usual finding is a rounded opacity at the right cardiophrenic angle. The lateral chest film localizes this density to the anterior retrosternal space (Fig. 52-2). The opacification is generally due to omentum rising through the hernia defect. When the transverse colon, small bowel, or stomach herniates through the defect, an air fluid level may be seen on chest film (Fig. 52-3). In adults, pericardial cyst, prominent fat pad, loculated pneumothorax, bronchial carcinoma in the cardiophrenic region, and atypical mediastinal tumor may mimic the radiographic features of herniation through the foramen of Morgagni.
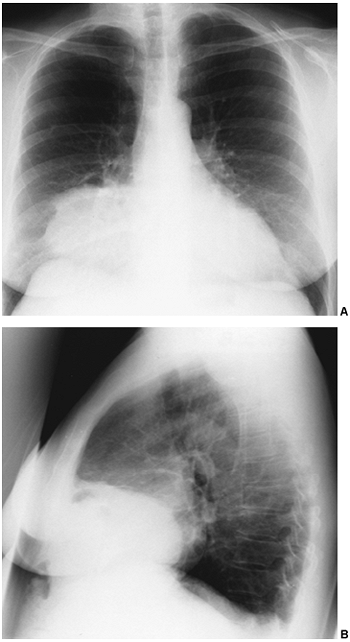 |
Fig. 52-2. A. Posteroanterior radiograph showing a round right pericardiophrenic density. B. Lateral film localizes the opacity to the retrosternal area. |
Contrast studies of the colon or upper gastrointestinal tract can confirm the diagnosis in patients with visceral herniation (Fig. 52-4). Computed tomographic (CT) scan is diagnostic in cases with or without visceral herniation because it demonstrates the presence of fat, a hollow viscus, or both, without the need for gastrointestinal contrast.
P.774
The usual, CT finding is a retrosternal mass of fat density representing herniated omentum (Fig. 52-5) or a combination of omentum and an air-containing viscus (Fig. 52-6). Magnetic resonance (MR) imaging can provide similar information but is usually not required. Although radiographs after induced pneumoperitoneum have been used to outline the hernia sac for definitive diagnosis, this approach is rarely needed.
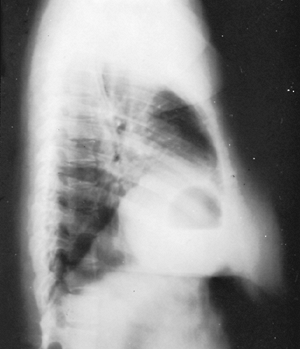 |
Fig. 52-3. Lateral chest radiograph showing a large air-fluid level in a foramen of Morgagni hernia that contained part of the stomach. |
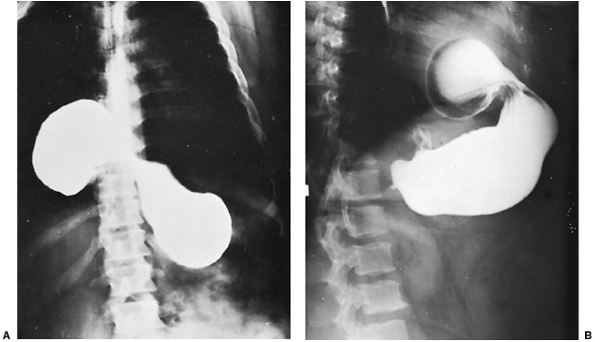 |
Fig. 52-4. Posteroanterior film (A) and lateral view (B) of a barium-filled stomach partially herniated into the chest through a right-sided foramen of Morgagni hernia. |
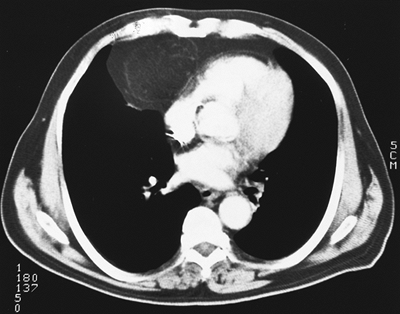 |
Fig. 52-5. Computed tomographic scan showing a right retrosternal mass consisting entirely of fat in herniated omentum. |
SURGICAL REPAIR
The treatment of a foramen of Morgagni hernia is surgical. All symptomatic adults should undergo repair. I agree with most recent reports in also recommending repair in most asymptomatic adults because hernias may enlarge over time and there is a low but definite risk of progression to incarceration and strangulation. Thus, a safe, elective operation can become a potentially high-risk procedure. In some asymptomatic cases, however, it is reasonable to follow
P.775
the patient without repair. This group includes people with only herniated omentum who have comorbidities that increase the risk for operation.
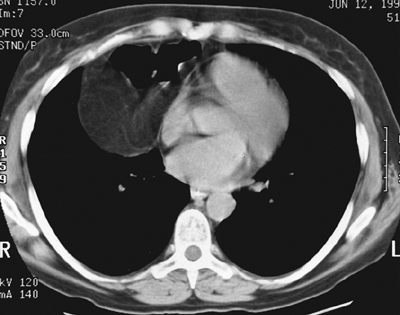 |
Fig. 52-6. Computed tomographic scan showing a right retrosternal hernia containing both omentum and transverse colon. |
Repair is generally performed transabdominally through an upper midline, subcostal, or paramedian incision. A midline approach allows easy access to both sides in the event that bilateral hernias are encountered. Adhesions are taken down, and the contents of the hernia are reduced into the peritoneal cavity. The margins of the hernia sac are identified, and the sac is generally resected. As in all types of hernia surgery, a tension-free closure is required to prevent recurrence. For small defects that can be closed primarily, repair of the muscular defect is performed with heavy (0-gauge) interrupted, nonabsorbable mattress sutures. It is usually necessary to pull the diaphragm up to the posterior part of the sternum and to the posterior rectus sheath (Fig. 52-7). Prosthetic patches are used to close larger defects. In many patients, it is not necessary to enter the chest or to drain the pleural space.
Occasionally, a foramen of Morgagni hernia is encountered during a thoracotomy performed for an undiagnosed mediastinal mass or other indication. Once identified, the sac is opened and explored, and the contents are reduced into the peritoneal cavity. Primary or prosthetic patch repair of the defect can often be performed in a manner similar to the transabdominal technique. In some cases, adequate repair requires passing the sutures around a rib anteriorly or through the sternal periosteum.
Experience is increasing with minimally invasive approaches to the treatment of foramen of Morgagni hernias. Laparoscopy is used most commonly, as reported by Kuster (1992) and Orita (1997) and their colleagues, as well as Fernandez-Cebrian and De Oteyza (1996), among others. Hussong and associates (1997) reported success with a thoracoscopic approach.
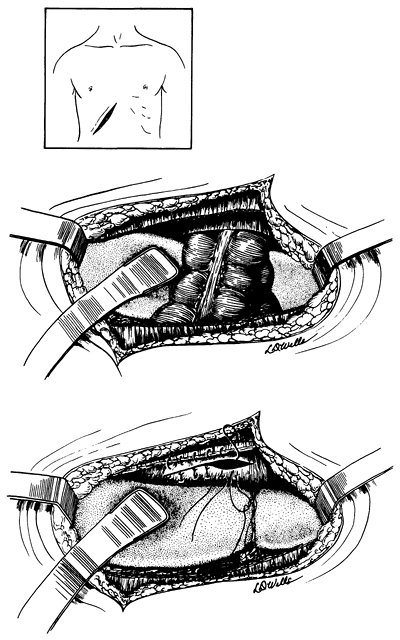 |
Fig. 52-7. Technique of closure of a foramen of Morgagni hernia by an open transabdominal approach. From Shields TW: The diaphragm. In Nora P (ed): Operative Surgery: Principles and Techniques. Philadelphia: Lea Febiger, 1972. With permission. |
The results of surgical repair of foramen of Morgagni hernias are excellent. Operative mortality and morbidity are low, especially for elective repair. There were five deaths (3.8%), involving one child and four adults, in the series of 132 patients reviewed by Berardi and co-workers (1997). Of paramount importance is that all five deaths occurred in patients with strangulated bowel. Although there are no reliable data on recurrence rates, individual reports of recurrences are rare. Follow-up is limited, but the results of endoscopic repair so far appear to be excellent.
REFERENCES
Berardi RS, et al: An update on the surgical aspects of Morgagni's hernia. Surgical Rounds, Sept. 1997, pp. 370 376.
Comer TP, Clagett OT: Surgical treatment of hernia of the foramen of Morgagni. J Thorac Cardiovasc Surg 52:461, 1966.
P.776
Ellyson JH, Parks SN: Hernia of Morgagni in trauma patients. J Trauma 26:569, 1986.
Fernandez-Cebrian JM, De Oteyza JP: Laparoscopic repair of hernia of foramen of Morgagni. J Laparoendosc Surg 6:61, 1996.
Harrington SW: Various types of diaphragmatic hernia treated surgically. Surg Gynecol Obstet 86:735, 1948.
Hussong RL, Landreneau RJ, Cole FH: Diagnosis and repair of a Morgagni hernia with video-assisted thoracic surgery. Ann Thorac Surg 63:1474, 1997.
Kuster GGR, Kline LE, Garzo G: Diaphragmatic hernia through the foramen of Morgagni: laparoscopic repair. J Laparosc Surg 2:93, 1992.
Lanuza A: The sign of the cane: a new radiological sign for the diagnosis of small Morgagni hernias. Radiology 101:293, 1981.
Lin JC, Maginot AE: Postpartum incarcerated Morgagni's hernia: an unusual presentation of Morgagni's hernia. Surgical Rounds, Feb. 1999, pp. 70 72.
Naunheim KS: Adult presentation of unusual diaphragmatic hernias. Chest Surg Clin North Am 8:359, 1998.
Orita M, et al: Laparoscopic repair of a diaphragmatic hernia through the foramen of Morgagni. Surg Endosc 11:668, 1997.
Shields TW: The diaphragm. In Nora P (ed): Operative Surgery: Principles and Techniques. Philadelphia: Lea & Febiger, 1972.
Valases C, Sills C: Case report: anterior diaphragmatic hernia (hernia of Morgagni). N J Med 85:603, 1988.
EAN: 2147483647
Pages: 203