1 - Approach to the Patient Health Maintenance
Editors: McPhee, Stephen J.; Papadakis, Maxine A.; Tierney, Lawrence M.
Title: Current Medical Diagnosis & Treatment, 46th Edition
Copyright 2007 McGraw-Hill
> Table of Contents > 4 - Geriatric Medicine
function show_scrollbar() {}
4
Geriatric Medicine
C. Bree Johnston MD
G. Michael Harper MD
C. Seth Landefeld MD
The impressive successes of medicine and public health over the past century have made it possible for elderly persons to live longer and healthier than ever before. Persons over the age of 65 account for about 13% of the population, which will swell to about 20% by 2030 as the baby boomers age. Thus, most physicians will spend a significant portion of their professional lives dealing with older adults' health care.
Older persons are remarkably heterogeneous. Many persons in their 60s are healthy and can expect to live another 30 years or longer. Yet, chronic diseases that will cause disability and ultimately death will develop in nearly all older persons. While age alone is a strong predictor of risk for disease, disability, and death, the health status, prognosis, and preferences of care of persons in their 70s, 80s, and 90s vary widely. Therefore, physicians caring for older adults must have skills in managing multiple comorbidities and wisely guiding the patient in both curative and palliative care.
General Principles of Geriatric Medicine
The following principles are helpful to keep in mind while caring for older adults:
Many disorders are multifactorial in origin.
Diseases often present atypically.
Not all abnormalities require evaluation and treatment.
Complex medication regimens, adherence problems, and polypharmacy are common challenges.
Comorbidities are common in older people, and the diagnostic law of parsimony often does not apply. For example, fever, anemia, and a heart murmur are almost always diagnostic of endocarditis in a younger patient; however, in an older patient, three different explanations a viral illness, colon cancer, and aortic sclerosis might be equally likely than the unifying diagnosis of endocarditis.
Disease presentation is often atypical in elderly patients. A disorder in one organ system may lead to symptoms in another, especially one that is compromised by preexisting disease. Because these organ systems are often the brain, the lower urinary tract, and the cardiovascular or musculoskeletal systems, a limited number of presenting symptoms ie, confusion, falling, incontinence, dizziness, and functional decline predominate irrespective of the underlying disease. Thus, regardless of the presenting symptom in older people, the differential diagnosis is often similar. An 80-year-old person with new falls and confusion could have pneumonia, an acute myocardial infarction, a stroke, or a urinary tract infection. Furthermore, because many geriatric syndromes have multiple causes, multiple targeted interventions may be a more realistic approach than trying to find a cure. For example, dizziness is often multifactorial in older adults. A practitioner who focuses on finding a diagnosis and treatment may become frustrated, while a practitioner who works on multiple problems, such as correcting vision, prescribing physical therapy focused on strength and balance, and reducing sedating medications, might meet with more success.
Many abnormal findings in younger patients are relatively common in older people and may not be responsible for a particular symptom. Such findings may include asymptomatic bacteriuria, premature ventricular contractions, and slowed reaction time. In addition, many older patients with multiple comorbidities may have laboratory abnormalities that, while pathologic, may not be clinically important. A complete workup for a mild anemia of chronic disease in a person with multiple other issues might be burdensome to the patient with little chance of impacting quality of life or longevity. While abnormalities should not be ignored, they can be addressed in order of priority, with the patient's goals (symptom management, desire for longevity) dictating the evaluation strategy.
Many older patients have to manage complex medication regimens, particularly those who have multiple comorbidities. Drug side effects can occur with low doses of drugs that usually produce no side effects in younger people. For instance, a mild anticholinergic agent (eg, diphenhydramine) may cause confusion, loop diuretics may precipitate urinary incontinence, digoxin may induce anorexia even with normal serum levels, and nonprescription sympathomimetics may result in urinary retention in older men with mild prostatic obstruction.
P.52
General Approach to the Older Patient
Therapy in elders should be guided by the estimated life expectancy and the patients' values and goals (Figure 4-1). Interventions that are likely to help elders who are well may differ from those that will benefit elders who are frail. Estimating life expectancy can help a health care provider focus on those issues most likely to be beneficial in a given patient. A mammogram would be appropriate for a healthy older woman with a life expectancy of 12 years, but not for a woman with congestive heart failure and chronic obstructive pulmonary disease with a life expectancy of less than 5 years.
Detecting and treating some conditions produce almost immediate benefit, and those may be useful at any age. These include visual impairment, hearing loss, falls, depression, incontinence, immobility, and pain. Smoking cessation and initiating an exercise program can also produce very rapid benefits, even in the oldest old.
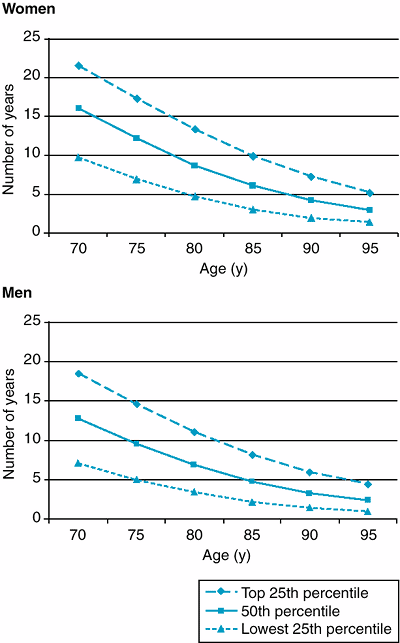 |
Figure 4-1. Median life expectancy of older women and men. (Adapted from Walter LC et al: Screening for colorectal, breast, and cervical cancer in the elderly: a review of the evidence. Am J Med 2005;118:1078. ) |
An awareness of a patient's goals, values, and preferences can help the health care provider focus the patient's visits appropriately. For example, many evaluations and interventions can be avoided in an elderly patient who is interested in receiving symptomatic, but not life prolonging, care.
Certain strategies can make the care of older people in a busy outpatient practice a little more manageable. Such strategies include using brief assessment instruments for common geriatric conditions when appropriate, training nonprovider personnel in administering some of these assessments (hearing screen, vision screen), having portable amplifiers ( pocket talkers ) available, and designing protocols for following up abnormal screening assessments. For example, a medical assistant might perform the simple geriatric screen (Figure 4-2) on all patients older than 75 years, and prompt the provider by having follow up instruments such as the Mini-Mental State Examination (MMSE) and the geriatric depression scale available when the screen was positive.
Many practitioners question which elders should be referred to geriatric care, home care, or team care. The answer depends on the resources of the community, but a good rule of thumb is that if it feels like the patient cannot be treated adequately in the setting where they are receiving care or if the coordination of care is taking so much time that it is detracting from the care of other patients, it may be time to explore a different level of care.
Fried TR et al: Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002;346:1061.
Assessment of Older Adults
Functional Assessment
Functional assessment gauges a patient's ability to manage tasks of self-care, household management, and mobility.
About one-fourth of patients over 65 have impairments in their IADLs (instrumental activities of daily living: transportation, shopping, cooking, using the telephone, managing money, taking medications, housecleaning, laundry) or ADLs (basic activities of daily living: bathing, dressing, eating, transferring from bed to chair, continence, toileting). Half of those persons older than 85 years have these latter impairments. Persons who are unable to perform IADLs independently are far more likely to have dementia than their independent counterparts.
Information about function can be used in a number of ways: (1) as baseline information, (2) as a measure of the patient's need for support services or placement, (3) as an indicator of possible caregiver burden,
P.53
P.54
(4) as a potential marker of specific disease activity, (5) to determine the need for therapeutic interventions, and (6) to indicate prognosis.
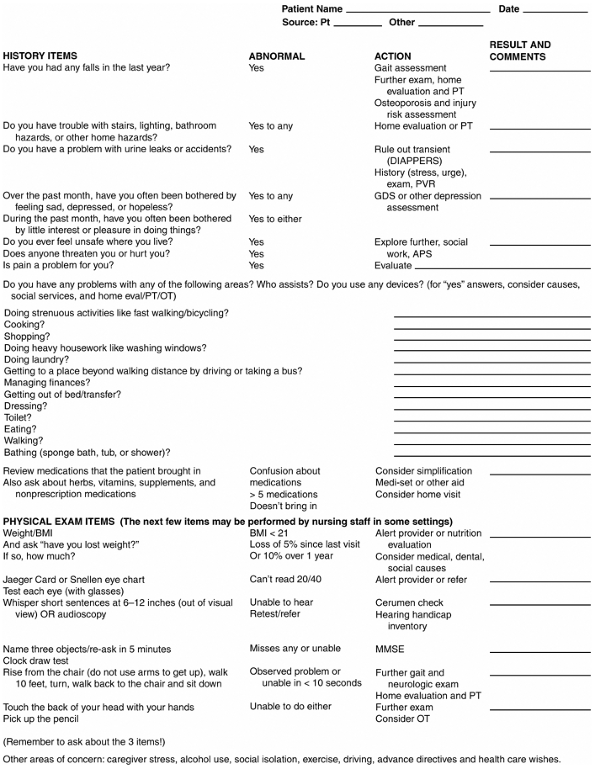 |
Figure 4-2. Simple geriatric screen. PT = physical therapy; DIAPPERS = delirium, infection, atrophic urethritis or vaginitis, pharmaceuticals, psychological factors, excess urinary output, restricted mobility, stool impaction; PVR = postvoid residual; GDS = Geriatric Depression Screen; APS = Adult Protective Services; OT = occupational therapy; BMI = body mass index; MMSE = Mini-Mental State Exam. (Modified from Lachs M et al: A simple procedure for general screening for functional disability in elderly patients. Ann Intern Med 1990;112:699 andMoore AA et al: Screening for common problems in ambulatory elderly: clinical confirmation of a screening instrument. Am J Med 1996;100:438. ) |
In general, persons who need help only with IADLs can usually live independently with minimal supports, such as financial services (eg, a representative payee) or a chore worker. If institutional care is needed, residential care, board-and-care, or assisted living is usually sufficient. While many persons who need help with ADLs may require a nursing home level of care, most live at home with caregivers and other community services (eg, day care).
Screening for Vision Impairment
An appreciable minority of elders have severe visual loss. Visual impairment is an independent risk factor for falls; it also has a significant impact on quality of life. Although administering direct visual testing with a Snellen chart or Jaeger card in most primary care settings is relatively easy, the prevalence of serious eye disease and visual impairment in elders is sufficient to warrant a complete eye examination by an ophthalmologist or optometrist annually or biannually for most elders. Many patients with visual loss benefit from a referral to a low vision program, and primary care practitioners should not assume that an ophthalmologist or optometrist will automatically make this referral.
Screening for Hearing Impairment
Over one-third of persons over age 65 and half of those over age 85 have some hearing loss. This deficit is correlated with social isolation and depression. Although the optimal screening method for hearing loss in older adults is undetermined, the whispered voice test is easy to perform and has sensitivities and specificities ranging from 70% to 100%. To determine the degree to which the impairment interferes with functioning, the provider may ask if the patient becomes frustrated when conversing with family members, is embarrassed when meeting new people, has difficulty listening to the radio or watching TV, or has problems understanding conversations in noisy restaurants. Caregivers or family members often have important information on the impact of hearing loss on the patient's social interactions.
Compliance with hearing amplification can be a challenge because of the stigma associated with hearing aid use as well as the cost of such devices, which are not paid for under most Medicare plans. High compliance rates can be achieved with a proactive approach such as the use of loaner aids for low-income persons. In addition to standard hearing aids, other devices are available. For example, portable amplifiers are small radio-sized units with earphones attached; they can be purchased inexpensively at many electronics stores and are well accepted by many patients. Special telephones, amplifiers for the television, and many other devices are available to aid the person with hearing loss.
Screening for Falls & Gait Impairment
Falls are the leading cause of nonfatal injuries in older persons, and their complications are the leading cause of death from injury in persons over age 65. Hip fractures are common precursors to functional impairment, nursing home placement, and death. Furthermore, fear of falling may lead some elders to restrict their activities. About one-third of people over 65 fall each year, and the frequency increases markedly with advancing age.
Every older person should be asked about falls; many will not volunteer such information. Clinicians should ask about home hazards that might be remediable. A thorough gait assessment should be performed in all older people. Gait and balance can be readily assessed by the Up and Go Test, in which the patient is asked to stand up from a sitting position without use of hands, walk 10 feet, turn around, walk back, and sit down. Patients who take less than 10 seconds are usually normal, patients who take longer than 30 seconds tend to need assistance with many mobility tasks, and those in between tend to vary widely with respect to gait, balance, and function. The ability to recognize common patterns of gait disorders is an extremely useful clinical skill to develop. Examples of gait abnormalities and their causes are listed in Table 4-1.
Screening for Cognitive Impairment
The prevalence of dementia doubles every 5 years after age 60, so that by age 85 about 30 50% of individuals have some degree of impairment. Patients with mild or early dementia frequently remain undiagnosed because their social graces are retained.
Although there is no consensus at present on whether older patients should be screened for dementia, the benefits of early detection include identification of potentially reversible causes, planning for the future (including advance directives), providing support and counseling for the caregiver, modification of interventions for other diseases as appropriate (eg, simplifying drug regimens, minimizing anticholinergic drug use), and beginning acetylcholinesterase inhibitor drugs.
The combination of a clock drawing task with a three-item word recall is fairly quick to administer. Although a number of different methods for administering and scoring the clock draw test have been described, the authors of this chapter favor the approach of pre-drawing a four inch circle on a sheet of paper and instructing the patient to draw a clock with the time set at 10 minutes after 11. Scores are classified as normal, almost normal, or abnormal. When a patient is able to draw a clock normally and can remember all 3 objects, dementia is unlikely. When a patient fails this simple screen, further cognitive evaluation with
P.55
the MMSE (see Figure 25-1), neuropsychological testing, or other instruments is warranted.
Table 4-1. Evaluation of gait abnormalities. | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Borson S et al: The Mini-Cog as a screen for dementia: Validation in a population based sample. J Am Geriatr Soc 2003; 51:1451.
Screening for Incontinence
Incontinence in older adults is common, and interventions can improve most patients. Many patients fail to tell their providers about it. A simple question about involuntary leakage of urine is a reasonable screen: Do you have a problem with urine leaks or accidents?
Screening for Depression
Although major depressive disorder has a slightly lower prevalence in older adults than in younger populations, depressive symptoms are actually more common. Its prevalence in ill and hospitalized elders is particularly high. A simple two-question screen (Figure 4-2) has shown 96% sensitivity for detecting major depression in a general population and may have even higher sensitivity in those over age 65. Positive responses can be followed up with more comprehensive, structured interviews, eg, Yesavage's Geriatric Depression Scale (Table 4-2).
Assessment of Decision-Making Capacity
It is common for a cognitively impaired elder to face a serious medical decision and for the clinicians involved in his care to ascertain whether the capacity exists to make the choice. There are five components of a thorough assessment: (1) ability to express a choice; (2) understanding relevant information about the risks and benefits of planned therapy and the alternatives, including no treatment; (3) comprehension of the problem and its consequences; and (4) ability to reason; and (5) consistency. A patient's choice should follow rationally from an understanding of the consequences.
Cultural sensitivity must be used in applying these five components to people of various cultural backgrounds. In performing such assessments, it is to be remembered that decision-making capacity varies over time: A delirious patient may regain his capacity after an infection is treated, and so reassessments are often appropriate. Furthermore, the capacity to make a decision is a function of the decision in question. A mildly demented woman may lack the capacity to consent to coronary artery bypass grafting yet retain the capacity
P.56
to designate a surrogate decision maker or allow removal of a suspicious nevus.
Table 4-2. Yesavage's Geriatric Depression Scale (short form). | ||
|---|---|---|
|
Caregiver Issues
Most elders with functional impairment live in the community with the help of an informal caregiver, most commonly a spouse or daughter. The health and well-being of the patient and caregiver are closely linked. High levels of functional dependency place an enormous burden on a caregiver, and may result in caregiver burnout, depression, morbidity, and even increased mortality.
An older patient's need for nursing home placement is often better predicted from assessment of the caregiver characteristics and stress than the severity of the patient's illness. Therefore, part of caring for a frail elder involves paying attention to the well-being of the caregiver. The older patient who is also a caregiver is at risk for depression and should be screened for it. For the stressed caregiver, a social worker may help identify programs such as caregiver support groups, respite programs, adult day care, or hired home health aides.
Elder Abuse
It is helpful to observe and talk with every older person alone for at least part of a visit in order to question directly about possible abuse and neglect (Table 4-3). Clues to the possibility of elder abuse include behavioral changes in the presence of the caregiver, delays between injuries and sought treatment, inconsistencies between an observed injury and associated explanation, lack of appropriate clothing or hygiene, and not filling prescriptions.
Functional Screening Instrument
Figure 4-2 gives a simple functional screening list. In addition to ADL and IADL assessment, it looks for evidence of health problems that affect function: sensory impairment, limited upper extremity range of motion, mobility, falls, weight loss, incontinence, depressed mood, and cognitive impairment.
Table 4-3. Questions that may elicit a history of elder abuse. | |
|---|---|
|
Standard functional screening measures may not be useful in capturing subtle impairments in highly functional independent elders. One technique for these patients is to identify and regularly ask about a target activity, such as playing bridge, bowling, or working outside the home. If the patient begins to have trouble with or discontinues such an advanced activity of daily living, it may indicate early impairment, such as dementia, incontinence, or worsening hearing loss, which additional gentle questioning or assessment may uncover.
Selected Preventive Measures in Geriatric Practice
Exercise
Inactive elders are at greater risk for becoming functionally dependent than their more physically active counterparts. Higher levels of physical activity are associated with reduced risks of future disability, disease-related morbidity, and mortality. Even sedentary elders should be urged to increase their level of physical activity. By writing out an exercise prescription, a provider demonstrates the importance of the activity and may improve compliance. Components that have been demonstrated to improve outcomes in elders include strength training (isolated muscle group contractions), endurance training (walking, cycling, swimming), and balance (tai chi, dance). Ideally, the patient should aim for a total of 30 60 minutes of activity daily. Recent data suggests that even short spurts of activity throughout the day are beneficial. The greatest increase in benefit is experienced by those going from a completely sedentary lifestyle to participating in some physical activity.
Gill TM et al: A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med 2002;347:1068.
Gill TM et al: Exercise stress testing for older persons starting an exercise program. JAMA 2000;284:2591.
Manson JE et al: Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med 2002;347:716.
Hypertension
Treatment of hypertension is of substantial benefit in older adults, and the absolute benefit of treatment may be greater in older than in younger patients. The role of aggressive antihypertensive therapy in the persons over age 85 is still being debated. Treatment of hypertension and isolated systolic hypertension reduces the incidence of strokes, heart failure, and cardiovascular events but not overall mortality in this age group. Lifestyle modifications (weight loss for overweight patients, alcohol and sodium limitation, increased aerobic physical activity) are reasonable to recommend for all hypertensive patients for whom treatment is appropriate. For those who require pharmacologic
P.57
treatment, thiazides are the drugs of choice unless a comorbid condition makes another choice preferable.
Cancer Screening
The authors of this chapter recommend against routinely screening elderly men for prostate cancer, since there is no evidence that the practice prolongs life, and the burdens of treatment can be considerable. An older woman is likely to benefit from breast cancer screening until her life expectancy falls below 5 10 years (Figure 4-1). Screening for colon cancer can be stopped when a patient's life expectancy is less than 5 10 years. Cervical cancer is uncommon in older women, and screening can usually be discontinued at age 65 if the woman has had a history of regular screening and normal Pap smears.
Walter LC et al: Screening for colorectal, breast, and cervical cancer in the elderly: a review of the evidence. Am J Med 2005;118:1078.
Immunizations
Individuals over age 65 and health care workers who are in contact with them should receive annual influenza vaccinations. Although data from randomized controlled trials are scarce, observational studies suggest that flu vaccination decreases mortality and pneumonia in elders. Similarly, persons over 65 should receive at least one pneumococcal immunization; some experts recommend revaccination in those over 75 or with severe chronic disease and who were vaccinated more than 5 years previously, although data are lacking. The Centers for Disease Control and Prevention recommends primary vaccination for tetanus and diphtheria (Td) in elders who are previously unvaccinated. The historical recommendation has been to give booster doses of Td every 10 years. An alternative approach is to give a single booster dose of Td at midlife (age 50 years) to those who have received full pediatric immunizations (see Chapter 30).
Ppd for Congregate Living
Older adults are a significant reservoir of tuberculosis, both primary and reactivation. The disease develops in over 20% of elderly patients who live in nursing homes. Long-term care facilities should routinely perform a tuberculin skin test (PPD) on all entering patients, using the two-step approach in which a second dose is administered to persons whose first was negative. If the second reaction is also negative, the patient is uninfected or anergic; if positive, a boosted response is likely, signifying a tuberculin reactor but not a recent converter. Whether these reactors need treatment is controversial, but their positive-PPD status should be noted. Prophylaxis and treatment regimens are described in Chapter 9. Skin testing is repeated annually in congregate settings or if an active case is identified in the group.
Common Problems of the Frail Older Person
Dementia
![]() Essentials of Diagnosis
Essentials of Diagnosis
Progressive impairment of intellectual function, including loss of short-term memory.
Deficits in at least one other area, including aphasia, apraxia, agnosia, or a disturbance in executive functioning.
Deficit severe enough to cause impairment of function.
Psychiatric manifestations common.
Not delirious.
Alzheimer's disease is most common cause, followed by vascular dementia and dementia with Lewy bodies.
Older individuals experience occasional difficulty retrieving items from memory (usually manifested as word-finding complaints) and experience a slowing in their rate of information processing. By contrast, dementia is an acquired persistent and progressive impairment in intellectual function, with compromise of memory and at least one other cognitive domain. The diagnosis of dementia requires a significant decline in function that is severe enough to interfere with work or social life.
Intellectual impairments in older patients are frequently the result of two other syndromes, each of which frequently coexists with dementia: depression and delirium. Depression is a common concomitant of dementia, but it can also masquerade as dementia. Moreover, a patient with depression and cognitive impairment whose intellectual function improves with treatment of the mood disorder has an almost fivefold greater risk of suffering irreversible dementia later in life. Delirium, characterized by acute confusion, occurs much more commonly in patients with underlying dementia.
General Considerations
Alzheimer's disease is the eighth leading cause of death in the United States and sixth leading cause among the elderly. It has a prevalence that doubles every 5 years in the older population, reaching 30 50% at age 85. Women suffer disproportionately, both as patients (even after age adjustment) and as caregivers. Alzheimer's disease accounts for roughly two-thirds of cases in the
P.58
United States, with vascular dementia (either alone or combined with Alzheimer's disease) accounting for much of the rest. Risk factors for Alzheimer's disease are older age, family history, lower education level, and female gender. Some epidemiologic studies suggest that head injury, hypertension, higher homocysteine levels, and higher low-density lipoprotein (LDL) cholesterol levels are risk factors for dementia, while nonsteroidal anti-inflammatory drug (NSAID) use, HMG-CoA reductase inhibitor use, moderate alcohol intake, and strong social supports may decrease the risk. However, these studies of risk factors for dementia do not provide an adequate basis for treatment recommendations. Risk factors for vascular dementia are those for stroke, ie, older age, male sex, black race, hypertension, cigarette use, previous myocardial infarction, atrial fibrillation, diabetes, and hyperlipidemia.
Causes of potentially reversible cognitive impairment include drug effect, depression, thyroid disease, vitamin B12 deficiency, hypercalcemia, subdural hematoma, HIV infection, and normal-pressure hydrocephalus. The prevalence of fully reversible dementias is well under 5%, and the correction of these suspected causes leads only to partial improvement in most cases.
Clinical Features
Demented patients have memory impairment and at least one or more of the following: language impairment (initially just word finding; later, difficulty following a conversation; finally, mutism), apraxia (inability to perform previously learned tasks, such as cutting a loaf of bread, despite intact sensory and motor function), agnosia (inability to recognize objects), and impaired executive function (poor abstraction, mental flexibility, planning, and judgment). Alzheimer's disease typically presents with early problems in memory and visuospatial abilities (eg, becoming lost in familiar surroundings, inability to copy a geometric design on paper), yet social graces may be retained despite advanced cognitive decline. Personality changes and behavioral difficulties (wandering, inappropriate sexual behavior, agitation) may develop as the disease progresses. Hallucinations are not typically observed except in moderate-to-severe dementia. End-stage disease is characterized by near-mutism; inability to sit up, hold up the head, or track objects with the eyes; difficulty with eating and swallowing; weight loss; bowel or bladder incontinence; and recurrent respiratory or urinary infections.
Subcortical dementias (eg, the dementia of Parkinson's disease, and some cases of vascular dementia) are characterized by psychomotor slowing, reduced attention, early loss of executive function, and personality changes, and benefit from cuing-in tests of memory.
Dementia with Lewy bodies may be confused with delirium, as fluctuating cognitive impairment is frequently observed. Rigidity and bradykinesia are the primary signs, and tremor is rare. Response to dopaminergic agonist therapy is poor. Complex visual hallucinations typically of people or animals may be an early feature that can help distinguish dementia with Lewy bodies from Alzheimer's disease. These patients demonstrate a hypersensitivity to neuroleptic therapy, and attempts to treat the hallucinations may lead to marked worsening of extrapyramidal symptoms.
Frontotemporal dementias are a group of diseases that include Pick's disease, dementia associated with amyotrophic lateral sclerosis, and others. Patients manifest personality change (euphoria, disinhibition, apathy) and compulsive behaviors (often peculiar eating habits or hyperorality). In contrast to Alzheimer's disease, visuospatial function is relatively preserved.
Dementia in association with motor findings, such as extrapyramidal features or ataxia, may represent a less common disorder (eg, progressive supranuclear palsy, corticobasal ganglionic degeneration, olivopontocerebellar atrophy).
Differential Diagnosis
In addition to depression and delirium, apparent cognitive impairment in older adults may be the result of drug effects or uncorrected sensory deficits; these problems more often exacerbate dementia than mimic it.
Many medications have been associated with diminished mentation in older patients. Anticholinergic agents, hypnotics, neuroleptics, and opioids are well-established causes, but NSAIDs, antihistamines (including H2-antagonists), and corticosteroids have been implicated as well.
An elderly patient with intact cognition but with severe impairments in vision or hearing commonly becomes confused in an unfamiliar medical setting and consequently may be falsely labeled as demented. Cognitive testing is best performed after optimal correction of the sensory deficits.
Diagnosis
Historical questions in an evaluation for dementia include those directed at the rate of progression of the deficits, their nature (including any personality or behavioral change), motor problems, risk factors for HIV, family history, medication list, functional disabilities, and degree of social support.
The neurologic examination emphasizes assessment of mental status (see Figure 25-1) but should also include evaluation for deficits related to previous strokes, parkinsonism, or peripheral neuropathy. The remainder of the physical examination should focus on identifying comorbid conditions that may aggravate the individual's disability.
Laboratory studies for most patients are intended to uncover treatable causes of cognitive impairment and include a complete blood count, electrolytes, calcium, creatinine, glucose, thyroid-stimulating hormone (TSH), and vitamin B12 levels. HIV testing, RPR (rapid plasma reagin) test, heavy metal screen, and liver function tests may be informative in selected patients but should not be considered part of routine testing.
P.59
Although consensus is lacking with respect to which patients benefit from head CT or MRI, those who are younger and those who have focal neurologic symptoms or signs, seizures, gait abnormalities, and an acute or subacute onset are most likely to yield positive findings.
Referral for neuropsychological testing may be helpful in the following circumstances: to distinguish dementia from depression, to diagnose dementia in persons of very poor education or very high premorbid intellect, and to aid diagnosis when impairment is mild.
Treatment
Soon after diagnosis, patients and families should be made aware of the Alzheimer's Association as well as the wealth of helpful publications available for advice in coping with behavioral problems, financial worries, and other matters. Caregiver support, education, and counseling can prevent or delay nursing home placement. Education includes the manifestations and natural history of dementia as well as the availability of local support services such as respite care. Even under the best of circumstances, caregiver stress can be substantial.
Because demented patients have greatly diminished cognitive reserve, they are at high risk for experiencing acute cognitive or functional decline in the setting of new medical illness. Consequently, fragile cognitive status may be best maintained by ensuring that comorbid diseases such as congestive heart failure and infections are detected and treated.
Most experts recommend considering a trial of acetylcholinesterase inhibitors (eg, donepezil, galantamine, rivastigmine) in most patients with mild to moderate Alzheimer's disease. These medications produce statistically significant but modest improvements in cognitive function. Acetylcholinesterase inhibitors may also benefit patients with vascular dementia or dementia with Lewy bodies. Starting doses, respectively, of donepezil, galantamine, and rivastigmine, are 5 mg orally once daily (maximum 10 mg once daily), 4 mg orally twice daily (maximum 12 mg twice daily), and 1.5 mg orally twice daily (maximum 6 mg twice daily). The doses are increased gradually as tolerated. The most bothersome side effects include diarrhea, nausea, anorexia, and weight loss.
Evidence from a recent long-term randomized controlled trial of donepezil versus placebo in community-dwelling patients with Alzheimer's disease confirmed the modest cognitive improvement seen in previous trials but found no difference in the rates of institutionalization or progression of disability at 3 years between the two groups. Some experts have been concerned that stopping these drugs may lead to irreversible worsening, but this trial did not substantiate this concern. Therefore, in those patients who have had no apparent benefit, experience side effects or for whom the financial outlay is a burden, the authors of this chapter recommend a trial of discontinuation.
In clinical trials, patients with more advanced disease have been shown to have statistical benefit from the use of memantine, a N-methyl-d-aspartate (NMDA) antagonist, with or without concomitant use of an acetylcholinesterase inhibitor. Long-term and meaningful functional outcomes have yet to be demonstrated.
Other agents have been studied. Ginkgo biloba has shown mixed results in clinical trials. Vitamin E demonstrated some efficacy in one randomized controlled trial, but the results are difficult to interpret. Estrogen and NSAIDs have shown no benefits in randomized trials.
Behavioral problems in demented patients are often best managed with a nonpharmacologic approach. Initially, it should be established that the problem is not unrecognized delirium, pain, urinary obstruction, or fecal impaction. It also helps to inquire whether the caregiver or institutional staff can tolerate the behavior, as it is often easier to find ways to accommodate to the behavior than to modify it. If not, the caregiver is asked to keep a brief, informal journal in which the behavior is described along with antecedent events and consequences. Recurring precipitants of the behavior are often found to be present or it may be that the behavior is rewarded for example, by increased attention. Caregivers are taught to use simple language when communicating with the patient, to break down activities into simple component tasks, and to use a distract, not confront approach when the patient seems disturbed by a troublesome issue. Additional steps to address behavioral problems include the discontinuation of all medications except those considered absolutely necessary and correction, if possible, of sensory deficits.
There is no clear consensus about a pharmacologic approach to treatment of behavioral problems in patients who have not benefited from nonpharmacologic therapies. The target symptoms depression, anxiety, psychosis may suggest which class of medications might be most helpful in a given patient. Patients with depressive symptoms may show improvement with antidepressant therapy.
The efficacy of acetylcholinesterase inhibitors for behavioral disturbances in Alzheimer's dementia is still undetermined, but a meta-analysis suggested that they may exert a modest benefit on neuropsychiatric outcomes. Patients with dementia with Lewy bodies have shown clinically significant improvement in behavioral symptoms when treated with rivastigmine. Neuroleptics are commonly used for behavioral disturbances, but the literature on their efficacy is mixed. One review suggested that haloperidol may be modestly useful in reducing aggression but not agitation in dementia and that it is associated with significant adverse effects. The newer atypical agents (risperidone, olanzapine, quetiapine, aripiprazole, clozapine, ziprasidone) are reported to be better tolerated than older agents, but they are considerably more expensive. The US Food and Drug Administration recently issued a public health advisory warning that these agents, when used to treat elderly demented patients with behavioral disturbances, increased the mortality rates 1.6 1.7 times compared
P.60
with placebo. A separate meta-analysis reached similar conclusions and also found a nonstatistically significant trend toward increased mortality with haloperidol. Because of limited efficacy data and safety concerns, caution should be used when prescribing neuroleptic agents for treating behavioral disturbances in dementia. When the choice is made to use these agents, starting and target dosages should be much lower than those used in schizophrenia (eg, haloperidol, 0.5 2 mg orally; risperidone, 0.25 2 mg orally). Federal regulations require that if antipsychotic agents are used in treatment of a nursing home patient, drug reduction efforts must be made at least every 6 months.
Anecdotal data suggest that some patients improve with agents such as mood stabilizers or trazodone, but randomized trials show mixed results. In one trial, haloperidol, trazodone, behavioral management techniques, and placebo produced comparable if modest reductions in agitation in patients with dementia.
Prognosis
Life expectancy after a diagnosis of Alzheimer's disease is typically 3 15 years; it may be shorter than previously reported. Other neurodegenerative dementias, such as dementia with Lewy bodies, show more rapid decline.
Courtney C et al: Long-term donepezil treatment in 565 patients with Alzheimer's disease (AD2000): randomised double-blind trial. Lancet 2004;363:2105.
Lonergan E et al: Haloperidol for agitation in dementia. Cochrane Database Syst Rev 2002;(2):CD002852.
Schneider LS et al: Risk of death with atypical antipsychotic drug treatment for dementia; meta-analysis of randomized placebo controlled trials. JAMA 2005;294:1934.
Trinh NH et al: Efficacy of cholinesterase inhibitors in the treatment of neuropsychiatric symptoms and functional impairment in Alzheimer disease: a meta-analysis. JAMA 2003; 289:210.
Wilkinson D et al: Donepezil in vascular dementia: a randomized placebo controlled trial. Neurology 2003;61:479.
Depression
Geriatric patients with depression are more likely than younger ones to have somatic complaints, less likely to report depressed mood or feelings of guilt, and more likely to experience delusions.
Depressive syndromes that arise late in life are heterogeneous, and a significant number may represent persons with neurodegenerative disorders (eg, dementia). Consequently, close follow-up of a newly diagnosed patient, with frequent assessment of mental status and neurologic examination, may disclose an additional or alternative diagnosis.
Depression in older adults is associated with disability, increased rates of hospitalization and nursing home admission, and higher mortality. Medical illness and disability more common in older adults are risk factors for depression. In particular, stroke and Parkinson's disease appear to predispose to depression. Suicide is most common in older men. Although the presence of comorbid medical illnesses and cognitive disorders may interfere with diagnosis, use of the Geriatric Depression Scale (see Table 4-2) with candidate cases may provide the data needed to make a treatment decision.
Elderly patients with depressive symptoms should be questioned about medication use, as many drugs (benzodiazepines, cimetidine, corticosteroids, and clonidine, to name a few) may contribute to the clinical picture. Similarly, several medical problems can cause fatigue, lethargy, or hypoactive delirium, all of which may be mistaken for depression. Laboratory requests should include a complete blood count; liver, thyroid, and renal function tests; and serum calcium. The workup to exclude an organic explanation calls for urinalysis and an electrocardiogram.
Choice of antidepressant agent in elders is usually based on side effect profile and cost. In general, fluoxetine is avoided because of its long duration of action and tricyclic antidepressants are avoided because of their high anticholinergic side effects. Regardless of the drug chosen, many experts recommend starting elders at a relatively low dose, titrating to full dose slowly, and continuing for a longer trial (at least 9 weeks) before trying a different medication. Cognitive behavioral therapy can improve outcomes alone or in combination with medication therapy. Depressed elders may do better with a collaborative care model than with usual care.
Unutzer J et al: Collaborative care management of late life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288:2836.
Delirium
![]() Essentials of Diagnosis
Essentials of Diagnosis
Rapid onset and fluctuating course.
Primary deficit in attention rather than memory.
May be hypoactive or hyperactive.
Dementia frequently coexists.
Delirium is an acute, fluctuating disturbance of consciousness, associated with a change in cognition or the development of perceptual disturbances (see also Chapter 25). It is the pathophysiologic consequence of an underlying general medical condition such as infection, coronary ischemia, hypoxemia, or metabolic derangement. Delirium persists in up to 25% of patients and is associated with worse clinical outcomes (higher in-hospital and postdischarge mortality,
P.61
longer lengths of stay, greater probability of placement in a nursing facility).
Although the acutely agitated, sundowning elderly patient often comes to mind when considering delirium, many episodes are more subtle. Such quiet, or hypoactive, delirium may only be suspected if one notices new cognitive slowing or inattention.
Cognitive impairment is an important risk factor for delirium. Approximately 25% of delirious patients are demented, and 40% of demented hospitalized patients are delirious. Other risk factors are male sex, severe illness, hip fracture, fever or hypothermia, hypotension, malnutrition, polypharmacy and use of psychoactive medications, sensory impairment, use of restraints, use of intravenous lines or urinary catheters, metabolic disorders, depression, and alcoholism.
Assessment
A key component of a delirium workup is review of medications because a large number of drugs, the addition of a new drug, or the discontinuation of a medication known to cause withdrawal symptoms are all associated with the development of delirium. Laboratory evaluation of most patients should include a complete blood count, electrolytes, blood urea nitrogen (BUN) and serum creatinine, glucose, calcium, albumin, liver function studies, urinalysis, and electrocardiography. In selected cases, serum magnesium, serum drug levels, arterial blood gas measurements, blood cultures, chest radiography, and urinary toxin screens may be helpful.
Management
Prevention is the best approach. Measures include improving cognition (frequent reorientation, activities), sleep (massage, noise reduction), mobility, vision (visual aids and adaptive equipment), hearing (portable amplifiers, cerumen disimpaction), and hydration status (volume repletion). Management of established episodes of delirium is supportive, entailing treatment of the underlying cause, eliminating unnecessary medications, and avoidance of restraints. Antipsychotic agents (such as haloperidol, 0.5 1 mg, or quetiapine, 25 mg, at bedtime or twice daily) are considered the medication of choice when drug treatment of delirium is necessary. In emergency situations, starting haloperidol at 0.5 mg by mouth or intramuscularly and repeating every 30 minutes until the agitation is controlled may be necessary, but such treatment is often followed by prolonged sedation or other complications. Other medications (eg, trazadone, donepezil, mood stabilizers) have also been used, but clinical trials that support these approaches are lacking.
Most episodes of delirium clear in a matter of days after correction of the precipitant, but some patients suffer episodes of longer duration. These individuals merit closer follow-up for the development of dementia if not already diagnosed.
Cole MG et al: Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial. CMAJ 2002;167:753.
Inouye SK et al: A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999; 340:669.
Kalisvaart KJ et al: Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc 2005;53:1658.
Marcantonio ER et al: Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc 2001;49:516.
Immobility
Although common in older people, reduced mobility is never normal and is often treatable if its causes are identified. It is an important cause of hospital-induced functional decline. Among hospitalized medical patients over 70, about 10% experience a decline in their ability to perform ADLs, much of which results from preventable reductions in mobility.
The hazards of bed rest in older adults are multiple, serious, quick to develop, and slow to reverse. Deconditioning of the cardiovascular system occurs within days and involves fluid shifts, decreased cardiac output, decreased peak oxygen uptake, and increased resting heart rate. More striking changes occur in skeletal muscle, with loss of contractile velocity and strength. Pressure sores are a third serious complication; mechanical pressure, moisture, friction, and shearing forces all predispose to their development. Thrombophlebitis and pulmonary embolism are additional serious risks. Within days after being confined to bed, the risk of postural hypotension, falls, skin breakdown, and pulmonary embolism rises rapidly in the older patient. Moreover, recovery from these changes usually takes weeks to months.
Common causes of immobility are weakness, stiffness, pain, dizziness, and comorbid illness. Weakness may result from disuse of muscles, malnutrition, electrolyte disturbances, anemia, neurologic disorders, or myopathies. The most common cause of stiffness in older adults is osteoarthritis, but Parkinson's disease and inflammatory arthritides such as rheumatoid arthritis also are possible in this age group, and drugs such as haloperidol may also contribute. Polymyalgia rheumatica should be strongly considered in older patients with pain and stiffness, particularly of the pelvic and shoulder girdle, associated with systemic symptoms (see Chapter 20).
Pain, whether from bone (eg, osteoporosis, osteomalacia, Paget's disease, metastatic bone cancer, trauma), joints (eg, osteoarthritis, rheumatoid arthritis, hip fractures, gout), bursae, or muscle (polymyalgia rheumatica, intermittent claudication, or pseudoclaudication ), may immobilize the patient. Painful foot problems are common as well and include plantar warts, ulcerations, bunions, corns, and ingrown and overgrown toenails. Poorly fitting shoes are a frequent cause of these disorders.
P.62
Imbalance and fear of falling are major causes of immobilization. Imbalance often results from several causes concurrently, including neurologic disorders (eg, stroke, cervical myelopathy, peripheral neuropathy due to diabetes or alcohol, and vestibulocerebellar abnormalities), orthostatic or postprandial hypotension, or drugs (eg, diuretics, antihypertensives, sedatives, neuroleptics, and antidepressants). It may also occur following prolonged bed rest.
Psychological conditions such as severe anxiety or depression may contribute to immobilization.
Prevention & Treatment
When immobilization cannot be avoided, several measures can be used to minimize its consequences. Adequate nutrition should be ensured, and the skin over pressure points should be inspected frequently; if the patient is unable to shift position, staff should do so every 2 hours. To minimize cardiovascular deconditioning, patients should be positioned as close to the upright position as possible, several times daily. To reduce the risks of contracture and weakness, range of motion exercises should be started immediately and isometric and isotonic exercises performed while the patient is in bed. Whenever possible, patients should assist with their own positioning, transferring, and self-care. As long as the patient remains immobilized, pharmacologic (eg, low-dose heparin) or nonpharmacologic means (eg, graduated compression stockings) should be used to reduce the risk of thrombosis if that is consistent with the patient's goals of care.
Avoiding restraints and discontinuing invasive devices (intravenous lines, urinary catheters) may increase an elderly patient's prospects for early mobility. Once this becomes feasible, graduated ambulation should begin. Advice from a physical therapist is often helpful. Installing handrails, lowering the bed, and providing chairs of proper height with arms and rubber skid guards may make the patient safely mobile in the home. A properly fitted cane or walker may also be useful.
If pain is contributing to immobility, it should be addressed (see section below on analgesics). If depression is preventing a patient from participating in physical therapy, it may prove necessary to start with a short course of stimulant medication (eg, methylphenidate; see Chapter 25), at least until a more traditional antidepressant has had time to take effect.
van Baar ME et al: Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee. Arthritis Rheum 1999;42:1361.
Falls & Gait Disorders
Thirty percent of community-dwelling elderly persons fall each year, including half of people over age 80. About 1% of falls result in hip fracture, and hip fracture is associated with significant increases in functional dependence, morbidity, and mortality. Fear of falling may contribute to loss of independence and other negative health effects. Falls are thought to be a contributing factor to almost half of nursing home admissions. Nonetheless, falls are not inevitable or untreatable.
Causes of Falls
Balance and ambulation require a complex interplay of cognitive, neuromuscular, and cardiovascular function. With age, balance becomes impaired and postural sway increases. This predisposes the older person to a fall when challenged by an additional insult to any of these systems.
A fall may be the clinical manifestation of an occult problem, such as pneumonia or myocardial infarction, but much more commonly falls are due to the interaction between an impaired patient and an environmental risk factor. While a warped floorboard may pose little problem for a vigorous, cognitively intact person, it may be sufficient to precipitate a fall and hip fracture in the patient with impaired vision, balance, muscle tone, or cognition. Thus, falls in older people are rarely due to a single cause, and effective intervention entails a comprehensive assessment of the patient's intrinsic deficits (usually diseases and medications), the activity engaged in at the time of the fall, and environmental obstacles.
Intrinsic deficits are those that impair sensory input, judgment, blood pressure regulation, reaction time, and balance and gait. Dizziness may be closely related to the deficits associated with falls and gait abnormalities. While it may be impossible to isolate a sole cause or a cure for falls, gait abnormalities, or dizziness, it is often possible to identify and ameliorate some of the underlying contributory conditions and improve the patient's overall function.
As for most geriatric conditions, medications and alcohol use are among the most common, significant, and reversible causes of falling. Benzodiazepines, sedative-hypnotics, antidepressants, neuroleptics, and the use of four or more medications simultaneously have been associated with an increased fall risk. Other often overlooked but treatable contributors include postprandial hypotension (which peaks 30 60 minutes after a meal), insomnia, urinary urgency, and peripheral edema (which can burden impaired leg strength and gait because of the additional weight).
Since most falls occur in or around the home, a visit by a visiting nurse, physical therapist, or health care provider reaps substantial benefits in identifying environmental obstacles and is generally reimbursed by third-party payers, including Medicare. Insufficient lighting is an underappreciated factor in many cases. In addition to the number and location of lamps, noting their wattage is also important; because of a loss of contrast sensitivity, older people often need twice the wattage to maximize visual acuity. Replacement of 60-watt bulbs with 100-watt bulbs may be cost-effective.
P.63
Complications of Falls
The most common fractures resulting from falls are of the wrist, hip, and vertebrae. There is a high mortality rate (approximately 20% in 1 year) in elderly women with hip fractures, particularly if they were debilitated prior to the time of the fracture.
Fear of falling again is a common, serious, but treatable factor in the elderly person's loss of confidence and independence. Referral to a physical therapist for gait training with special devices is often all that is required.
Chronic subdural hematoma is an easily overlooked complication of falls that must be considered in any elderly patient presenting with new neurologic symptoms or signs, particularly obtundation. Headache is uncommonly present. In many cases there is no history of trauma.
Patients who are unable to get up from a fall are at risk for dehydration, electrolyte imbalance, pressure sores, rhabdomyolysis, and hypothermia.
Prevention & Management
The risk of falling and consequent injury, disability, and potential institutionalization can be reduced by modifying those factors outlined in Table 4-4. Emphasis is placed on treating all contributory medical conditions, minimizing environmental hazards, and reducing the number of medications particularly those that induce parkinsonism, orthostasis (eg, -blockers, calcium channel blockers, nitrates, antiparkinsonism agents, antipsychotics, tricyclic antidepressants), peripheral edema, and confusion. Also important are strength, balance, and gait training as well as steps to improve bone density (with calcium and vitamin D supplementation in most older adults and other medications as indicated). There is some evidence that vitamin D may help prevent falls.
Table 4-4. Fall risk factors and targeted interventions. | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Assistive devices, such as canes and walkers, are useful for many older adults but are often used incorrectly. Canes should be used on the good side. The height of walkers and canes should generally be about the level of the wrist. Physical therapists are invaluable in assessing the need for an assistive device, selecting the best device, and training a patient in its correct use.
Patients with repeated falls are often reassured by the availability of phones at floor level, a portable phone, or a lightweight radio call system. Their therapy should also include training in techniques for arising after a fall. Use of an anatomically designed external hip protector reduces hip fracture risk in frail older people but is often poorly tolerated.
Bischoff-Ferrari HA et al: Effect of Vitamin D on falls: a meta-analysis. JAMA 2004;291:1999.
Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc 2001;49:664.
Tinetti ME: Clinical practice. Preventing falls in elderly persons. N Engl J Med 2003;348:42.
Urinary Incontinence
![]() Essentials of Diagnosis
Essentials of Diagnosis
Involuntary loss of urine.
Stress incontinence presents with leakage of urine upon coughing, sneezing, or standing.
Urge incontinence presents with symptoms of urgency and inability to delay urination.
Overflow incontinence may have variable presentation.
Classification
Because continence requires adequate mobility, mentation, motivation, and manual dexterity, problems outside the bladder often result in geriatric incontinence. In general, the authors of this chapter find it useful to differentiate between transient or potentially reversible causes of incontinence and more established causes.
P.64
A. Transient Causes
Use of the mnemonic DIAPPERS may be helpful in remembering the categories of transient incontinence.
1. Delirium
A clouded sensorium impedes recognition of both the need to void and the location of the nearest toilet. Delirium is the most common cause of incontinence in hospitalized patients; once it clears, incontinence usually resolves.
2. Infection
Symptomatic urinary tract infection commonly causes or contributes to urgency and incontinence. Asymptomatic bacteriuria does not.
3. Atrophic urethritis or vaginitis
Because it usually coexists with atrophic vaginitis, atrophic urethritis can be diagnosed presumptively by the presence of vaginal mucosal telangiectasia, petechiae, erosions, erythema, or friability. Urethral inflammation, if symptomatic, may contribute to incontinence in some women.
4. Pharmaceuticals
Drugs are one of the most common causes of transient incontinence. Typical offending agents include potent diuretics, anticholinergics, psychotropics, opioid analgesics, -blockers (in women), -agonists (in men), and calcium channel blockers.
5. Psychological factors
Severe depression with psychomotor retardation may impede the ability or motivation to reach a toilet.
6. Excess urinary output
Excess urinary output may also overwhelm the ability of an older person to reach a toilet in time. In addition to diuretics, common causes include excess fluid intake; metabolic abnormalities (eg, hyperglycemia, hypercalcemia, diabetes insipidus); and disorders associated with peripheral edema, with its associated heavy nocturia when previously dependent legs assume a horizontal position in bed. Edema may be due to heart failure, venous insufficiency, malnutrition, cirrhosis, and use of calcium channel blockers or NSAIDs.
7. Restricted mobility
(See Immobility section, above.) If mobility cannot be improved, access to a urinal or commode (eg, at the bedside) may improve continence.
8. Stool impaction
This is a common cause of urinary incontinence in hospitalized or immobile patients. Although the mechanism is still unknown, a clinical clue to its presence is the onset of both urinary and fecal incontinence. Disimpaction restores urinary continence.
B. Established Causes
Causes of established incontinence should be addressed after the transient causes have been uncovered and managed appropriately.
1. Detrusor overactivity (urge incontinence)
Detrusor overactivity refers to uninhibited bladder contractions that cause leakage. It is the most common cause of established geriatric incontinence, accounting for two-thirds of cases, and is usually idiopathic. Women will complain of urinary leakage after the onset of an intense urge to urinate that cannot be forestalled. In men the symptoms are similar, but detrusor overactivity commonly coexists with urethral obstruction from benign prostatic hyperplasia. Because detrusor overactivity also may be due to bladder stones or tumor, the abrupt onset of otherwise unexplained urge incontinence especially if accompanied by perineal or suprapubic discomfort or sterile hematuria should be investigated by cystoscopy and cytologic examination of a urine specimen.
2. Urethral incompetence (stress incontinence)
Urethral incompetence is the second most common cause of established urinary incontinence in older women. Urinary incontinence is most commonly seen in men after radical prostatectomy. Stress incontinence is characterized by instantaneous leakage of urine in response to a stress maneuver. It commonly coexists with detrusor overactivity. Typically, urinary loss occurs with laughing, coughing, or lifting heavy objects. Leakage is worse or occurs only during the day, unless another abnormality (eg, detrusor overactivity) is also present. To test for stress incontinence, have the patient relax her perineum and cough vigorously (a single cough) while standing with a full bladder. Instantaneous leakage indicates stress incontinence if urinary retention has been excluded by postvoiding residual determination using ultrasound. A delay of several seconds or persistent leakage suggests that the problem is instead caused by an uninhibited bladder contraction induced by coughing.
3. Urethral obstruction
Urethral obstruction (due to prostatic enlargement, urethral stricture, bladder neck contracture, or prostatic cancer) is a common cause of established incontinence in older men but is rare in older women. It can present as dribbling incontinence after voiding, urge incontinence due to detrusor overactivity (which coexists in two-thirds of cases), or overflow incontinence due to urinary retention. Renal ultrasound is required to exclude hydronephrosis in men whose postvoiding residual urine exceeds 150 mL.
4. Detrusor underactivity (overflow incontinence)
Detrusor underactivity is the least common cause of incontinence. It may be idiopathic or due to sacral lower motor nerve dysfunction ( neurogenic bladder ). When it causes incontinence, detrusor underactivity is associated with urinary frequency, nocturia, and frequent leakage of small amounts. The elevated postvoiding residual urine (generally over 450 mL) distinguishes it from detrusor overactivity and stress incontinence, but only urodynamic testing differentiates it from urethral obstruction in men. Such testing usually is not required in women, in whom obstruction is rarely present.
Treatment
A. Transient Causes
Each identified transient cause should be treated regardless of whether an established cause coexists. For
P.65
patients with urinary retention induced by an anticholinergic agent, discontinuation of the drug should first be considered. If this is not feasible, substituting a less anticholinergic agent (eg, sertraline instead of desipramine for depression) may be useful.
B. Established Causes
1. Detrusor overactivity
The cornerstone of treatment is behavioral therapy. Patients are instructed to void every 1 2 hours while awake. Once daytime continence is restored, the interval is increased by 30 minutes until the interval is 4 5 hours. Most patients who become continent during the day on this regimen become continent at night as well. For patients who are unable to manage on their own, caregivers should ask whether they need to void at suitable intervals.
Pelvic floor exercises, behavioral approaches, and biofeedback can be extremely helpful in training cognitively intact, motivated patients. Results superior to those achieved with use of bladder relaxants are possible.
If behavioral approaches prove insufficient, drug therapy with oxybutynin (2.5 5 mg three or four times daily), long-acting oxybutynin (5 15 mg daily), tolterodine (1 2 mg twice daily), or long-acting tolterodine (2 4 mg daily) appear modestly effective at reducing episodes of incontinence in some patients. All of these agents can produce delirium, dry mouth, or urinary retention; long-acting preparations may be better tolerated. In men with both benign prostatic hyperplasia and detrusor overactivity, a postvoiding residual or urodynamic testing should be done if prescription of a bladder relaxant is planned in order to avoid precipitating urinary retention. In refractory cases, where intermittent catheterization is feasible, the provider may choose intentionally to induce urinary retention with a bladder relaxant and have the patient empty the bladder three or four times daily. Clean but not sterile technique is required.
2. Urethral incompetence (stress incontinence)
Although a last resort, surgery is the most effective treatment for stress incontinence, resulting in a cure rate of 75 85% even in older women. For women who wish to avoid surgery and who can employ them indefinitely, pelvic muscle exercises are effective for mild to moderate stress incontinence; they can be combined, if necessary, with biofeedback, electrical stimulation, or vaginal cones. Pelvic floor exercises can be taught during bimanual vaginal examination or by asking the patient to try to contract the muscle that they use to stop the flow of urine. It is often necessary to perform 30 60 exercises daily for 6 weeks before significant improvement will be noticed. Pessaries or vaginal cones may be helpful in some women but should be prescribed by practitioners who are experienced with using these modalities.
Drug therapy is limited. There is no evidence that topical or oral estrogens are helpful, although some experts prescribe a trial of topical estrogen in women with symptomatic atrophic urethritis. -Agonists, such as pseudoephedrine, may have modest efficacy but are often poorly tolerated. Some new agents are under investigation.
3. Urethral obstruction
Surgical decompression is the most effective treatment for obstruction, especially in the setting of urinary retention. A variety of newer, less invasive techniques make decompression feasible even for frail men. For the nonoperative candidate with urinary retention, intermittent or indwelling catheterization is used. For a man with prostatic obstruction who does not require or desire immediate surgery, treatment with -blocking agents (eg, terazosin, 1 10 mg daily; prazosin, 1 5 mg orally twice daily; tamsulosin, 0.4 0.8 mg daily) can improve symptoms and delay obstruction. Finasteride, 5 mg daily, can also improve outcomes and provides additional benefits to an -blocking agent. However, finasteride may carry a risk of increasing high-grade prostate cancer.
4. Detrusor underactivity
For the patient with a poorly contractile bladder, augmented voiding techniques (eg, double voiding, suprapubic pressure) often prove effective. If further emptying is needed, intermittent or indwelling catheterization is the only option. Antibiotics should be used only for symptomatic upper urinary tract infection or as prophylaxis against recurrent symptomatic infections in a patient using intermittent catheterization; they should not be used as prophylaxis with an indwelling catheter.
Assessment and treatment of urinary incontinence. Scientific Committee of the First International Consultation on Incontinence. Lancet 2000;355:2153.
Weight Loss & Malnutrition
Undernutrition affects substantial numbers of elderly persons and often precedes hospitalization for failure to thrive. The degree of unintended weight loss that deserves evaluation is not agreed upon, although a reasonable threshold is loss of 5% of body weight in 1 month or 10% of body weight in 6 months. Commonly overlooked causes of weight loss in elders include dental problems or poorly fitting dentures, new functional decline with loss of ability to shop or prepare meals, worsening dementia, occult depression, or lack of caregiver support.
Useful laboratory and radiologic studies include complete blood count, serum chemistries (including glucose, TSH, creatinine, calcium), urinalysis, and chest film. These studies are intended to uncover an occult metabolic or neoplastic cause but are not exhaustive.
Oral nutritional supplements of 200 1000 kcal/d can increase weight and improve outcomes in malnourished elders. Megestrol acetate as an appetite stimulant has not been shown to increase body mass or lengthen life in the elderly population. For those who have lost the ability to feed themselves, assiduous
P.66
hand feeding may allow maintenance of weight. Although artificial nutrition and hydration ( tube feeding ) may seem a more convenient alternative, it deprives the patient of the taste and texture of food as well as the social milieu typically associated with mealtime; before this option is chosen, the patient or his or her surrogate will wish to review the benefits and burdens of the treatment in light of overall goals of care. If the patient makes repeated attempts to pull out the tube during a trial of artificial nutrition, the treatment burden becomes substantial, and the utility of tube feeding should be reconsidered. Although commonly used, there is no evidence that tube feeding prolongs life in patients with end-stage dementia.
Failure to thrive is a syndrome lacking a consensus definition but generally representing a constellation of weight loss, weakness, and progressive functional decline. The label is typically applied when some triggering event loss of social support, a bout of depression or pneumonia, the addition of a new medication pulls a struggling elderly person below the threshold of successful independent living. Ideally, use of the preventive measures recommended earlier in this chapter will reduce the patient's chances of reaching this stage of frailty.
Finucane TE et al: Tube feeding in patients with advanced dementia: a review of the evidence. JAMA 1999;282:1365.
Milne AC et al: Meta-analysis: Protein and energy supplementation in older people. Ann Intern Med 2006;144:37.
Pressure Ulcers
![]() Essentials of Diagnosis
Essentials of Diagnosis
Examine at-risk patients daily.
Blanchable hyperemia (stage I).
Extension through epidermis (stage II).
Full thickness skin loss (stage III).
Full thickness wounds with extension into muscle, bone, or supporting structures (stage IV).
If eschar overlies the wound, staging cannot be done.
General Considerations
The majority of pressure ulcers develop during a hospital stay for an acute illness. Incident rates range from 3% to 30% and vary according to patient characteristics. The primary risk factor for pressure ulcers is immobility. Other contributing risk factors include reduced sensory perception, moisture (urinary and fecal incontinence), poor nutritional status, and friction and shear forces.
A number of risk assessment instruments including the Braden Scale and the Norton score can be used to assess the risk of developing pressure ulcers; both have reasonable performance characteristics. These instruments can be used to identify the highest risk patients who might benefit most from scarce resources such as mattresses that reduce or relieve pressure.
Prevention
Pressure ulcers are often used as an indicator of quality of care; whether or not high quality preventive measures can eliminate pressure ulcers entirely is controversial. Mainstays of preventive therapy include promoting mobility and turning and repositioning immobile patients every 2 hours. For moderate- to high-risk patients, surfaces that reduce tissue pressure beyond a standard mattress but not to < 32 mm Hg (eg, air-fluid beds and low air loss beds) appear to be superior to standard mattresses. The literature comparing specific products is sparse and inconclusive.
Treatment
Treatment is aimed toward removing necrotic debris and maintaining a moist wound bed that will promote healing and formation of granulation tissue. The type of dressing that is recommended depends on the location and depth of the wound, whether necrotic tissue or dead space is present, and the amount of exudate (Table 4-5). Pressure-reducing devices (eg, air-fluid beds and
P.67
low air loss beds) are associated with improved healing rates. Although poor nutritional status is a risk factor for the development of pressure ulcers, the results of trials of nutritional supplementation in the treatment of pressure ulcers have been disappointing.
Table 4-5. Treatment of pressure ulcers. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Practitioners can become easily overwhelmed by the array of products available for treatment of established pressure ulcers. Most institutions should designate a wound care expert or wound care team to select a streamlined wound care product line that has simple guidelines.
Complications
Pressure ulcers are associated with increased mortality rates, although a causal link has not been proven. Complications include pain, cellulitis, osteomyelitis, systemic sepsis, and prolongation of lengths of stay in the inpatient or nursing home setting.
Pharmacotherapy & Polypharmacy
There are several reasons for the greater incidence of iatrogenic drug reactions in the elderly population, the most important of which is the high number of medications that are taken by elders, especially those with multiple comorbidities. Drug metabolism is often impaired in this group, due to a decrease in glomerular filtration rate as well as reduced hepatic clearance. The latter is due to decreased activity of microsomal enzymes and reduced hepatic perfusion with aging. The volume of distribution of drugs is also affected. Since older adults have a decrease in total body water and a relative increase in body fat, water-soluble drugs become more concentrated and fat-soluble drugs have longer half-lives. Serum albumin levels decrease, especially in acutely ill patients, with reduction in protein binding of some drugs (eg, warfarin, phenytoin), leaving more free (active) drug available.
Older individuals often have varying responses to a given serum drug level. Thus, they are more sensitive to some drugs (eg, opioids) and less sensitive to others (eg, -blocking agents).
Precautions in Administering Drugs
The symptom requiring treatment may be due to another drug, leading to a prescribing cascade, in which adverse drug effects are attributed to new medical conditions, in time resulting in prescription of still more medications.
Nonpharmacologic interventions can often be a first-line alternative to drugs (eg, mild hypertension or type 2 diabetes mellitus). Pharmacotherapy is not necessarily indicated in some common clinical situations. In asymptomatic bacteriuria, for example, antibiotics need not be given unless the disorder is associated with obstructive uropathy, other anatomic abnormalities, or stones. Ankle edema is often due to venous insufficiency, drugs (NSAIDs, calcium channel blockers), malnutrition, or inactivity in chair-bound patients and need not be treated with diuretics unless associated with heart failure. Leg elevation in the evening or fitted pressure-gradient stockings are often helpful.
Therapy is begun with less than the usual adult dosage and the dosage increased slowly, consistent with its pharmacokinetics in older patients. However, age-related changes in drug distribution and clearance are variable among individuals, and some require full doses. After determining acceptable measures of success and toxicity, the dose is increased until one or the other is reached.
Despite the importance of beginning new drugs in a slow, measured fashion, all too often an inadequate trial is permitted (in terms of duration of course, or ultimate dose) before they are discontinued. Angiotensin-converting enzyme inhibitors and antidepressants, in particular, are frequently stopped before therapeutic dosages are reached.
Steps are taken to improve adherence to the prescribed medical regimen. The following increase the odds of nonadherence: The patient lives alone; uses more than one pharmacy or provider; is prescribed medications with multiple daily doses; has a drug regimen that is changed frequently; is prescribed a large number of drugs; has difficulty reaching a pharmacy; and has poor cognition, vision, or dexterity. When possible, the provider should keep the dosing schedule simple, the number of pills low, and the medication changes infrequent.
The patient or caregiver is asked to bring in all medications at each visit for reinforcing instructions regarding reasons for drug use, dosage, frequency of administration, and possible adverse effects.
Although serum drug levels may be useful for monitoring certain drugs with narrow therapeutic windows (eg, digoxin), toxicity can still occur even with normal therapeutic levels of many drugs. The risk of toxicity goes up with the number of medications prescribed. Certain combinations of medications (eg, warfarin and many types of antibiotics, digoxin and clarithromycin, angiotensin-converting enzyme inhibitors and NSAIDs) are particularly likely to cause drug-drug interactions, and should be watched carefully.
Trials of individual drug discontinuation should be considered (including sedative-hypnotics, digoxin, proton pump inhibitors, NSAIDs) when the original indication is unclear, the goals of care have changed, or the patient might be experiencing side effects.
The Medicare prescription drug benefit in the United States certainly helps many elders with burdensome prescription drug costs. However, it is unclear how successful the program will be overall. Its benefits are complex and difficult to understand, particularly for those elders with limited cognition, literacy, and Internet access. Information is available at http://www.medicare.gov.
EAN: 2147483647
Pages: 49
- Challenging the Unpredictable: Changeable Order Management Systems
- The Second Wave ERP Market: An Australian Viewpoint
- Context Management of ERP Processes in Virtual Communities
- Distributed Data Warehouse for Geo-spatial Services
- Relevance and Micro-Relevance for the Professional as Determinants of IT-Diffusion and IT-Use in Healthcare