 | Note: Large images and tables on this page may necessitate printing in landscape mode.
Copyright 2007 The McGraw-Hill Companies. All rights reserved.
Clinician's Pocket Reference > Chapter 15. Imaging Studies >
X-Ray Preparations In general, follow this principle: Obtain plain films before obtaining films that require contrast. Each hospital has its own guidelines for patient preps. Consult the radiology department before ordering any x-ray that requires a prep. Examinations that require no specific bowel preparation are routine CXR, flat and upright abdominal films, cystograms, C-spines, skull series, extremity films, CT scans of the head and chest, and many others. Studies that usually require preps such as enemas, laxatives, or oral contrast agents or those that require that the patient be NPO before the examination include upper GI series, small-bowel follow-through (SBFT), barium enema, IVP, and others. IV contrast studies are discussed below. |
Common X-Ray Studies: Noncontrast Chest Chest X-Ray (Routine): Includes posteroanterior (PA) and lateral chest films. (PA means the film is placed in front of the patient with the beam coming from the back.) Evaluation of pulmonary, cardiac, and mediastinal diseases and traumatic injury. See How to Read a Chest X-Ray, and Figures 15 1 and 15 2. | 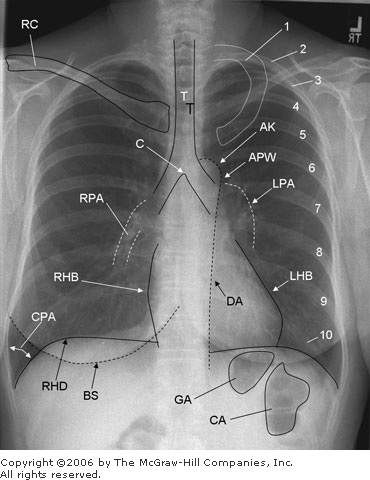 | Structures seen on a posteroanterior (PA) chest x-ray. 1 = first rib; 2 10 = posterior aspect of ribs 2 10; AK = aortic knob; APW = aortopulmonary window, BS = breast shadow (labeled only on right); C = carina; CA = colonic air; CPA = costophrenic angle, DA = descending aorta; GA = gastric air; LHB = left heart border (Note: Most of the left heart border represents the left ventricle; the superior aspect of the left heart border represents the left atrial appendage.); LPA = left pulmonary artery; RC = right clavicle (left clavicle not labeled); RHB = right heart border (Note: The right heart border represents the right atrium.); RHD = right hemidiaphragm (left hemidiaphragm not labeled); RPA = right pulmonary artery; T = tracheal air column. |
|
| 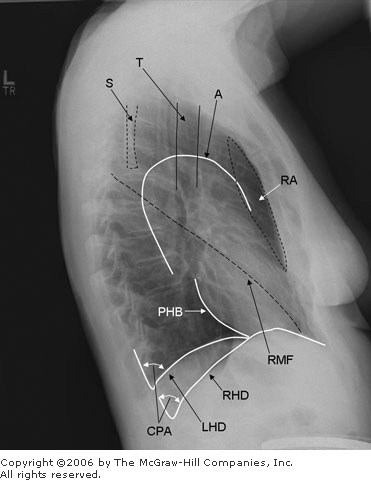 | Structures seen on a lateral chest x-ray. A = aorta; CPA = posterior costophrenic angle; LHD = left hemidiaphragm; PHB = posterior heart border (Note: The posterior heart border represents the left atrium superiorly and left ventricle inferiorly; the anterior heart border is not clearly defined on this film but represents the right ventricle.); RA = retrosternal airspace; RHD = right hemidiaphragm; RMF = right major fissure (left major fissure and minor fissures not well visualized on these films but can occasionally be seen); S = scapula; T = tracheal air column. |
|
Expiratory Chest: Visualization of small pneumothorax Lateral Decubitus Chest: Allows small amounts of pleural effusion or subpulmonic effusion to layer out; as little as 175 mL of pleural fluid can be detected Lordotic Chest: Evaluation of apices and lesions of the right and left upper lobes, TB Portable Chest and AP Films: Imaging of critically ill patients who cannot stand for a routine PA CXR; diagnosis of pneumothorax, pneumonia, and edema; verification of vascular line or tube placement. Not accurate in evaluation of heart or mediastinal size because the standard x-ray is PA (beam from behind), and the AP technique magnifies these structures Rib Details: Delineation of rib abnormalities when plain CXR or bone scan findings suggest fracture or other metastatic lesions Abdominal Abdominal Decubitus: Obtain instead of upright abdominal film for imaging of debilitated patients. Patient's left side is down to show free air outlining the liver and right lateral gutter. Acute Abdominal Series ("Obstruction Series"): Includes flat and upright abdominal films (KUB) and CXR. Initial evaluation of acute abdomen (See KUB.) Cross-Table Lateral Abdominal: Identification of free air in debilitated patients. KUB, Supine and Erect: Short for "kidneys, ureter, and bladder"; also known as flat and upright abdominal, scout film, and flat plate. Useful when the patient complains of abdominal pain or distention, and for initial evaluation of the urinary tract (80% of kidney stones and 20% of gallstones are visualized on KUBs). Look for calcifications, foreign bodies, the gas pattern, psoas shadows, renal and liver shadows, flank stripes, the vertebral bodies, and the pelvic bones. On the upright, look for air fluid levels of adynamic ileus and mechanical obstruction and for free air under the diaphragm, which suggests a perforated viscus or recent surgery; however, an upright CXR (especially the lateral view) is often best for spotting pneumoperitoneum. Other Noncontrast X-Rays C-Spine: Usually includes PA, lateral, and oblique films. Evaluation of trauma, neck pain, and neurologic evaluation of the upper extremities. All seven cervical vertebrae must be seen for this study to be acceptable. Add an "open mouth" view to identify odontoid fractures in trauma. DEXA Scan (Dual Energy X-Ray Absorptiometry, Bone Densitometry): Quantification of osteoporosis by measurement of bone mineral density (BMD). Assessment of fracture risk and effect of drugs such as bisphosphonates in osteoporosis. Central DEXA measures BMD in the spine or hip. Results are reported as a T and a Z score. T score shows the amount of bone compared with that of a young adult of the same sex with peak bone mass. A score above 1 is normal, 1 to 2.5 indicates osteopenia, and below 2.5 indicates osteoporosis. Z score reflects the amount of bone compared with an age-matched group. Mammography: Detection of tumors > 5 mm. Two forms are equal in diagnostic quality: - Screen film. Produces standard black and white x-ray with a specially designed mammographic machine; 3 5 % smaller radiation dose
- Digital mammography. Digital images may improve the resolution over film techniques
Sinus Films (Paranasal Sinus Radiographs): Evaluation of sinus trauma, sinusitis, neoplasms, and congenital disorders Skull Films: Detection of fractures and identification of pituitary tumors and congenital anomalies; not generally as useful as other imaging studies Thoracic, Lumbar, Sacral Vertebral Radiography: Evaluation of fractures, dislocations, subluxations, disk disease, and the effects of arthritic and metabolic disorders of the spine |
Common X-Ray Studies: Contrast A visualizing agent is used (such as barium, Gastrografin, or an IV contrast agent). If a GI tract fistula or perforation is suspected, inform the radiologist because the presence of such a lesion can affect the choice of contrast agent (eg, using a water-soluble agent such as Gastrografin rather than barium to prevent "barium peritonitis"). Standard IV contrast media are ionic, potentially nephrotoxic, and may be associated with rare adverse reactions when administered systemically (see following section). The use of nonionic contrast media can limit these side effects. In general, for use of an IV contrast agent, the creatinine must be < 1.8 2.0 mg/dL. Patients with elevated creatinine should be well hydrated to minimize nephrotoxicity. Contrast reactions to IV agents can occur. The overall incidence is 5%. Severe reactions occur in 1/1000 cases, and death due to anaphylaxis occurs in 1/40,000 cases. Reactions can be mild (nausea, vomiting, sneezing, diaphoresis, headache), intermediate (urticaria, angioneurotic edema, wheezing), or severe (cardiovascular collapse, pulmonary edema, shock, laryngeal edema, respiratory arrest). Vagal reactions (hypotension and bradycardia) are another adverse effect. A history of asthma is a risk factor, and a previous reaction to a contrast agent does not necessarily preclude use of IV contrast material (allergy to seafood or iodine is no longer considered an important risk factor). Premedication with two doses of PO methylprednisolone, one 12 h before and the other 2 h before IV contrast injection, as well as oral antihistamines may limit symptoms. For patients with a known history of allergic reaction, a nonionic agent or an alternative imaging technique is recommended. Angiography: A rapid series of films obtained after a bolus contrast injection through a percutaneous catheter. Imaging of aorta, major arteries and branches, tumors, and venous drainage with late "run-off" films. Helical CT scans also generate angiographic images. - Digital subtraction angiography (DSA). Allows reverse negative views and requires less contrast load
- Cardiac angiography. Definitive for diagnosis and assessment of severity of CAD. Significant (> 70% occlusion) stenotic lesions can be seen: 30% involve single vessels, 30% involve two, and 40% involve three vessels.
- Cerebral angiography. Evaluation of intra- and extracranial vascular disease, atherosclerosis, aneurysms, and A V malformations. Not used for detection of cerebral structural lesions (use MRI or CT instead)
- Pulmonary angiography. Visualization of emboli, intrinsic or extrinsic vascular abnormalities, A V malformations, and bleeding due to tumors. Most accurate diagnostic procedure for PE but only used if findings on helical CT or lung
 / / scan are not diagnostic scan are not diagnostic - Bronchial angiography. Visualization of bleeding vessels from the systemic circuit. Evaluation of hemoptysis in cases of known bronchiectasis
Barium Enema (BE): Examination of colon and rectum. Indications include diarrhea, crampy abdominal pain, heme-positive stools, change in bowel habits, and unexplained weight loss - Air-contrast BE. Done with the double-contrast technique (air and barium) to better delineate the mucosa. More likely to show polyps than standard BE
- Gastrografin enema. Similar to barium enema, but water-soluble contrast agent is used (clears colon more quickly than barium). If Gastrografin leaks from the GI tract, it is less irritating to the peritoneum (does not cause barium peritonitis). Therapeutic in evaluation of obstipation and colonic volvulus; depicts postop anastomotic leak
Barium Swallow (Esophagogram): Evaluation of swallowing mechanism, esophageal lesions, and abnormal peristalsis Cystogram: Bladder is filled and emptied with a catheter in place; used to evaluate bladder filling defects (tumors, diverticula) and bladder perforation. Can also be done with CT (CT cystogram is more sensitive for perforation with trauma) (see also Voiding Cystourethrography) Enteroclysis: Intubation of the proximal jejunum and rapid infusion of contrast material. Better than an SBFT in evaluation of polyps and obstruction (eg, adhesions, internal hernia); used to evaluate small-bowel sources of chronic bleeding after negative upper and lower endoscopy Endoscopic Retrograde Cholangiopancreatography (ERCP): Contrast material is endoscopically injected into the ampulla of Vater to visualize the common bile and pancreatic ducts for obstruction, stones, and ductal pattern Intravenous Pyelography (IVP): Contrast study of the kidneys and ureters; limited usefulness for evaluating bladder. Indications include flank pain, kidney stones, hematuria, UTI, trauma, and malignancy. Bowel prep helpful but not essential. Creatinine must be < 1.8 mg/dL. Largely replaced by CT urography. Nephrotomograms are images of kidney sections for further definition of the three-dimensional location or nature of renal lesions and stones. Fistulography (Sinogram): Injection of water-soluble contrast medium into any wound or body opening to determine the connection with other structures Hysterosalpinogography (HSG): Evaluation of uterine abnormalities (congenital anomalies, fibroids, adhesions) or tubal abnormalities (occlusion or adhesion), often as part of infertility evaluation. Contraindicated during menses, undiagnosed vaginal bleeding, and acute PID and if pregnancy is suspected. Place the patient in pelvic exam position, insert a speculum, cannulate the uterine os, and inject contrast material. Lymphangiography: Iodinated oil is injected to opacify lymphatics of the leg and the inguinal, pelvic, and retroperitoneal areas. Test of the integrity of the lymphatic system, evaluation for metastatic tumors (eg, testicular) and lymphoma Myelography: Evaluation of subarachnoid space for tumors, herniated disks, and other cause of nerve root injury. Use LP technique to inject contrast material into the subarachnoid space. Oral Cholecystography (OCG): Oral agent is used to visualize gallbladder; generally replaced by ultrasonography Percutaneous Nephrostography: Management of renal obstruction; percutaneous catheter placement through the renal parenchyma and into the collecting system to relieve and evaluate level and cause of obstruction Percutaneous Transhepatic Cholangiography (PTHC): Visualization of biliary tree in patients unable to concentrate contrast medium (bilirubin > 3 mg/dL). Needle inserted percutaneously into dilated biliary duct; contrast material injected. Retrograde Pyelography (RPG): Contrast material injected into the ureters through a cystoscope. Imaging of patients allergic to IV contrast medium or with elevated creatinine, if kidney or ureter cannot be visualized with other imaging techniques, and in the presence of renal mass, ureteral obstruction, or filling defects in the collecting system Retrograde Urethrography (RUG): Visualization of traumatic disruption of the urethra and urethral strictures Small Bowel Follow-Through (SBFT): Usually done after a UGI series. Delayed films show jejunum and ileum. Evaluation of diarrhea, abdominal cramps, malabsorption, and UGI bleeding T-Tube Cholangiography: Contrast injection into T-tube placed in the common bile duct after gallbladder or bile duct surgery. Evaluation of degree of swelling, find residual stones, and evaluate patency of bile duct drainage Upper GI (UGI) Series: Includes esophagography and imaging of stomach and duodenum. Visualization of ulcers, masses, hiatal hernia and to evaluate heme-positive stools and upper abdominal pain Venography, Peripheral: Contrast material is injected into a small foot or ankle vein for evaluation of patency of deep veins of leg and calf and detection of filling defect or outline of a thrombus. Noninvasive exams for DVT, such as Doppler ultrasonography and compression ultrasonography; highly sensitive (> 90%) for proximal thrombi. Has largely replaced contrast venography. Voiding Cystourethrography (VCUG): Bladder is filled with contrast material through a catheter, then catheter is removed, and the patient voids. Diagnosis of vesicoureteral reflux, examination of urethral valves, and evaluation of UTI |
Ultrasonography Abdominal: Gallbladder (95% sensitivity in diagnosis of stones), cholecystitis, biliary tree obstruction, pancreas (pseudocyst, tumor, pancreatitis), aorta (aneurysm), kidneys (obstruction, tumor, cyst), abscesses, ascites Echocardiography - M-mode. Valve mobility, chamber size, pericardial effusions, septal size
- Two-dimensional. Valvular vegetations, septal defects, wall motion, chamber size, pericardial effusion, valve motion, wall thickness
- Doppler. Cross-valvular pressure gradients, blood flow patterns, and valve orifice areas in work-up of cardiac valvular disease
Endovaginal: Diagnosis of abnormalities of uterus and ovaries Pelvic: (Note: A full bladder is desirable) - Pregnancy. Fetal dating (biparietal diameters); diagnosis of multiple gestations; determination of intrauterine growth retardation, hydrocephalus, and hydronephrosis; localization of placenta
- Gynecologic. Ovarian and uterine masses (eg, tumors, cysts, fibroids), ectopic pregnancy, abscesses
Thyroid: Thyroid nodules (cyst versus solid) and direct biopsy. Ultrasonographic findings alone cannot be used to differentiate benign from malignant lesions. Transrectal: Rectal wall and prostate abnormalities, prostate needle biopsy in diagnosis of prostate cancer, drainage of pelvic and prostatic abscesses Other: Testicular and scrotal masses (eg, hydrocele versus tumor), intraoperative determination of bladder emptying |
Computed Tomography (CT) Performed with or without contrast agent. Administration of a dilute oral contrast agent (eg, Tomocat) before abdominal or pelvic scans helps delineate the bowel. IV contrast is used to obtain vascular and tissue enhancement for some CT scans; check the creatinine level to determine the suitability of IV contrast administration. Any body part can be scanned depending on the indications, but CT is most helpful in evaluating the brain, lung, mediastinum, retroperitoneum (pancreas, kidney, nodes, aorta), and liver and to a lesser extent pelvis, colon, and bone. In CT density, measurements called Hounsfield units are used to differentiate cysts, lipomas, hemochromatosis, vascular (enhancing) and avascular (nonenhancing) lesions. In Hounsfield units, bone is +1000, water is 0, fat is 1000, and other tissues fall within this scale, depending on the machine settings. Metal and barium can cause distortion of the image. Abdominal CT: Imaging of all intraabdominal and retroperitoneal organs and define disease processes. Accurate for abscesses, but ultrasonography may show smaller collections adjacent to the liver, spleen, or bladder. Surgical clips or undiluted barium in the gut can cause artifacts. An IV contrast usually is given, so check creatinine level. Oral contrast helps identify the bowel; give the oral contrast agent at least 45 minutes before imaging. Chest CT: Depicts 40% more nodules than whole-lung tomograms, which show 20% more nodules than plain CXR. Although calcifications suggest benign disease (eg, granuloma), no definite density value can reliably separate malignant from benign lesions. Useful in differentiating hilar adenopathy from vascular structures seen on plain CXR, especially when contrast-enhanced images are obtained. High-resolution images are useful for characterizing interstitial lung disease. PE-protocol scans are obtained with contrast enhancement on spiral scanners (see Spiral [Helical] CT); this protocol frequently includes CT venography of the lower pelvis and legs. Head CT: Evaluation of tumors, subdural and epidural hematomas, A V malformations, hydrocephalus, and sinus and temporal bone abnormalities. Initial test of choice for trauma; may be superior to MRI in detection of hemorrhage within first 24 48 h Mediastinal CT: Masses, nodes, ectopic parathyroid tissue Neck CT: Work-up of neck masses, abscesses, and other diseases of the throat and trachea Pelvic CT: Staging and diagnosis of bladder, prostate, rectal, and gynecologic carcinoma; diagnosis of appendicitis, diverticulitis, and complications of pregnancy Retroperitoneal CT: Evaluation of pancreatitis; pancreatic masses; nodal metastasis from colon, prostate, renal, and testicular tumors; adrenal masses (> 3 cm suggests carcinoma); psoas mass; aortic aneurysm, retroperitoneal hemorrhage Spinal CT: MRI generally preferred over CT. However, rare conditions, contraindication to MRI, and artifact from metal may make the CT the preferred test. |
Spiral (Helical) CT Spiral technique can be used for any type of CT. It minimizes motion artifact and allows capture of a bolus of contrast material at peak levels in the region being scanned. Conventional CT is too slow to capture this peak flow. From a practical standpoint, almost all newer CT scanners have multidetector rows for acquisition of multiple (4, 8, 16) spiral scans at one time. These scanners provide higher-resolution images than do older units. Contrast-enhanced spiral CT scans allow detailed 3D reconstruction and angiographic evaluation (aortic, renal, peripheral, carotid, CNS, cardiac). Bony structures can also be visualized without contrast administration. The term spiral or helical is derived from the fact that the tube spins around the patient while the table moves. Spiral CT can compensate for "streak" artifact due to implanted metallic devices. Diagnosis of PE, pretransplantation angiography, evaluation of flank pain, detection of kidney stones (largely replacing emergency IVP), and rapid evaluation of trauma. Coronary CT angiography is used to evaluate common causes of acute chest pain and other cardiac indications. It requires a 64-slice scanner that acquires up to 192 images of the heart per second. Calcium scoring is an emerging technology for evaluation of coronary artery disease. |
Magnetic Resonance Imaging (MRI) How MRI Works Measurements of the magnetic movements of atomic nuclei are used to delineate tissues. When placed in a strong magnetic field, nuclei, such as hydrogen, resonate and emit radio signals when pulsed with radio waves. A defined sequence of magnetic pulses and interval pauses produces measured changes in the magnetic vectors of the tissue, which results in an MR image. T1, or longitudinal relaxation time, is the measurement of magnetic vector changes in the z-axis during the relaxation pause. T2, or transverse relaxation time, is the magnetic vector changes in the x-axis and the y-axis. Each tissue, normal or pathologic, has unique T1 and T2 for a given MRI field strength. In general T1 > T2. T1 = 0.1 2 s and T2 = 0.03 0.6 s. The inherent tissue differences between various T1 and T2 values give the visual contrast seen between tissues on the MR image. An image is T1-weighted if it depends on the differences in T1 measurements for visual contrast and T2-weighted if it depends on T2 measurements. The oldest, most common pulse sequence is called spin echo (SE). Partial saturation (PS) and inversion recovery (IR) are variations of the traditional SE sequence. A gradient echo technique now is used to obtain tissue contrast similar to that obtained with older SE methods. MR images are obtained in the transverse, sagittal, oblique, and coronal views. MRI Contrast: Gadolinium (gadopentetic dimeglumine) is an ionic contrast agent that acts as a paramagnetic agent and enhances vessels and lesions of abnormal vascularity. How to Read MR Images SE T1-Weighted Images: Provide good anatomic planes because of the wide variance in T1 values among normal tissues. - Brightest (high signal intensity): Fat
- Dark or black: Pathologic tissues, tumor or inflammation, fluid collections
- Black (low signal intensity): Respiratory tract, GI tract, calcified bone and tissues, blood vessels, heart chambers, and pericardial effusions
SE T2-Weighted Images: Pathologic lesions prolong T2 measurements, and normal tissues have a very small range of T2 values. T2-weighted images depict pathologic lesions best and normal tissue anatomy not as well. Tumor surrounded by fat may be lost on T2-weighted images. - Brightest: Fat and fluid collections
- Bright: Pheochromocytoma
When to Use MRI MRI provides better soft-tissue contrast than CT. MRI also is better than CT for imaging of the brain, spinal cord, musculoskeletal soft tissues, and areas of high CT bony artifact. However, spiral CT may overcome some of these disadvantages. Advantages - No ionizing radiation
- Display of vascular anatomy without contrast
- Visualization of linear structures: spine and spinal cord, aorta, vena cava
- Visualization of posterior fossa and other difficult-to-see CT areas
- High-contrast soft-tissue images
Disadvantages - Claustrophobia because of confining magnet; open MRI systems may help, but some may have more motion artifact
- Longer scanning time, resulting in motion artifacts
- Inability to image critically ill patients who need life support equipment
- Metallic foreign bodies (eg, pacemakers, shrapnel, CNS vascular clips, metallic eye fragments, and cochlear implants) are contraindications
Uses of MRI MRI is sensitive to motion artifact; anxious or agitated patients may have to be sedated for acquisition of optimal images. Intramuscular glucagon can be used to suppress intestinal peristalsis on abdominal studies. If the presence of metallic eye fragments is likely, obtain screening CT scans of the orbits before MRI. MRI is generally contraindicated in patients with intracranial aneurysm clips, intraocular metallic fragments, and pacemakers. Dental fillings and dental prostheses have not been a problem. Abdomen: Detection of adrenal lesions, tumor staging (renal, GI, pelvic), evaluation of abdominal masses, examination of almost all intraabdominal organs and retroperitoneal structures, and differentiation of benign adenoma from metastasis Chest: Evaluation of mediastinal masses, differentiation of nodes from vessels, detection of cardiac disease, tumor staging, detection of aortic dissection or aneurysm Head: Analysis of all intracranial lesions, identification of demyelinating diseases; some conditions, including acute trauma, are better evaluated with CT (see Spiral [Helical] CT). Magnetic resonance spectroscopy MRS may increase the sensitivity of diagnosis of many neurologic diseases by providing a biochemical "fingerprint" of tissues in the brain. Performed in conjunction with MRI equipped with MRS capability. Differentiation of causes of dementia, tumors, MS, and many other conditions. Musculoskeletal System: Detection of bone tumors and bone and soft-tissue infection, evaluation of joint spaces (unless a prosthesis is in place), marrow disorders, aseptic necrosis of femoral head Pelvis: Evaluation of all pelvic organs in male and female patients, differentiation of endometrium from myoma and adenomyosis, diagnosis of congenital uterine anomalies (eg, bicornuate, septate). Endorectal surface coil allows enhanced imaging of structures such as the prostate. Spine: Diagnosis of diseases of the spinal column (eg, herniated disk, tumors) |
Nuclear Scans The following are the more commonly used nuclear scans and their purposes. Most are contraindicated in pregnancy; check with your nuclear medicine department. Adrenal Scan: Localization of pheochromocytoma when MRI or CT findings are equivocal. Performed with labeled MIBG; patient must return for imaging several days after MIBG administration. Bleeding Scan: Detection of source of GI tract bleeding. - Technetium-99m (99mTc) Sulfur Colloid Scan. Detection of bleeding of 0.05 0.1 mL/min.
- Technetium-99m (99mTc)-Labeled Red Cell Scan. Same as sulfur colloid scan, but may be superior for localizing intermittent bleeding
Bone Scan: Metastatic work-ups (cancers most likely to go to bone: prostate, breast, kidney, thyroid, lung); evaluation of delayed union of fractures, osteomyelitis, avascular necrosis of femoral head; evaluation for hip prosthesis; differentiation of pathologic and traumatic fractures Brain Scan: Metastatic work-up, determination of blood flow (in brain death or atherosclerotic disease), evaluation of space-occupying lesions (tumor, hematoma, abscess, AV malformation), encephalitis Cardiac Scans: Diagnosis of MI, stress testing, measurement of ejection fractions and cardiac output, diagnosis of ventricular aneurysms - Thallium-201 (201Tl). Measurement of myocardial perfusion by uptake of 201Tl by normal myocardium. Normal myocardium appears hot, and ischemic or infarcted areas cold. AMI (< 12 h) seen as a hotspot, old MI (scar) seen as cold on both resting and exercise scans. Ischemia is cold on exercise scan and returns to normal after rest.
- Technetium-99m (99mTc) Pyrophosphate. Recently damaged myocardium concentrates 99mTc pyrophosphate, producing a myocardial hotspot. Most sensitive 24 72 h after AMI
- Technetium-99m (99mTc) Ventriculogram. 99mTc-labeled serum albumin or RBCs are used. Shows abnormal wall motion, cardiac shunt, size and function of heart chambers, cardiac output, and ejection fraction. Another form of this study is a MUGA scan, in which data collected are synchronized to an ECG and used to produce a "moving picture" of cardiac function. Performed with patient at rest or during exercise stress test.
Gallium Scan: Location of abscesses (5 10 d old) and chronic inflammatory lesions, lymphoma staging and follow-up for disease detection, diagnosis of lung cancer, melanoma, other neoplasms Hepatobiliary Scan (HIDA-Scan, BIDA-Scan): Differential diagnosis of biliary obstruction (when bilirubin > 1.5 mg/dL and < 7 mg/dL), acute cholecystitis, biliary atresia; not good for stones unless cystic duct is completely occluded and acute cholecystitis is present Indium-111 (111in) Octreotide (OctreoScan): Imaging of tumors with somatostatin receptors (pheochromocytoma, gastrinomas, insulinomas, small-cell lung cancer) Iodine-125 (125I) Fibrinogen Scanning: Detection of venous thrombosis in the lower extremities. Patient is scanned several hours and several days after injection of tracer. Identification of clots at or below knees. False-positives with varicosities, cellulitis, incisions, arthritis, hematomas, and recent venography. Tracer availability is a problem. Liver Spleen Scan: Estimating organ size; evaluation of parenchymal disease (eg, hepatitis), abscess, cysts, primary and secondary tumors Lung Scan ( / / Scan): Scan): With CXR, evaluation of PE. Normal scan excludes PE; indeterminate scan necessitates further study with pulmonary angiography; clear perfusion deficit coupled with a normal ventilation is highly suggestive of PE. Shows evidence of pulmonary disease, COPD, and emphysema Renal Scans: Agents are generally classified as functional tracers or morphologic tracers. - Iodine-131 (131I) Hippuran. Evaluation of function in renal insufficiency; visualization is poor, and radiation dose can be high
- Technetium-99m (99mTc) Glucoheptonate. Combination renal cortical imaging and renal function; evaluation of overall function but can be used to determine vascular flow and visualize renal parenchyma and collecting system
- Technetium-99m (99mTc) DMSA (dimercaptosuccinic acid). Renal cortical imaging only
- Technetium-99m (99mTc) DTPA (diethylenetriamine pentaacetic acid). Renal function; renal blood flow studies, estimation of GFR, evaluation of collecting system
- Technetium-99m (99mTc) Mercaptoacetyltriglycine (MAG3). Renal function; imaging of the parenchyma within minutes of injection and with low radiation dose. May eventually replace all other renal agents.
Single-Photon Emission CT (SPECT): Multiple nuclear images are sequentially displayed as in CT; can be applied to many nuclear scans. Strontium-89 (89Sr)(Metastron): Palliative therapy for multiple painful bony metastasis (eg, prostate or breast cancer). Because agent is a pure beta emitter, radioactivity remains in the body, so no special precautions (other than blood and urine) are needed. Thyroid Scan: Most often technetium-99m pertechnetate. Evaluation of nodules (solitary cold nodules require a tissue diagnosis because 25% are cancerous). Scan patterns in correlation with lab tests may help diagnose hyperfunctioning adenoma, Plummer and Graves diseases, multinodular goiter; localization of ectopic thyroid tissues (especially after thyroidectomy for cancer); identification of superior mediastinal thyroid masses |
Positron Emission Tomography (PET) PET involves injection of a positron-emitting tracer that is attached to a metabolically active molecule and accumulates in areas of increased metabolic activity. Tomographic images localize the tracer within the body. PET is often performed with CT or MRI, and the functional information obtained with PET scan is correlated with the precise anatomic detail obtained from CT or MRI. The most commonly used PET tracer is 18-fluoro-deoxyglucose (18-FDG). Fluorine-18 decays by positron emission. The positron emitters used in PET generally have a short half-life. The half-life of 18F is 110 min. This short half-life results in a low dose to the patient but means that a cyclotron must be available to produce the agent a short time before it is to be used. Clinical applications of PET are: - Cancer: Because malignant tissue has a higher metabolic rate than benign tissue, PET tracers of glucose metabolism are selectively concentrated in living tumor. PET depicts small foci of cancer that may be missed with conventional CT or MRI. PET can also be used to differentiate live tumors from treated dead tissue and fibrosis. Any metabolically active tissue will "light up," however. Areas of inflammation can cause false-positive results. The tumors most commonly imaged with PET include colorectal cancer, lung cancer, brain cancer, breast cancer, lymphoma, and melanoma. PET can be used in both diagnosis and staging of these cancers.
- Neurologic Imaging: Localization of specific functions and definition of functional neuroanatomy. Localization of epileptogenic foci in patients with seizures; diagnosis of various brain disorders, including dementia, depression, and schizophrenia.
- Cardiac Imaging: Definition of myocardial viability; findings complementary to anatomic information obtained with cardiac angiography, may be used in treatment planning.
|
How to Read a Chest X-Ray A CXR is a basic part of the evaluation of an ill patient. Understanding the basic principles of CXR interpretation is considered a key learning step for all physicians. Determine the Adequacy of the Film - Inspiration: Diaphragm below ribs 8 10 posteriorly and 5 6 anteriorly
- Rotation: Clavicles are equidistant from the spinous processes
- Penetration: Disk spaces are seen, but bony details of spine cannot be seen
PA Film The film is in front of the patient, and the x-ray beam passes from back (posterior) to front (anterior). The following structures are shown in Figure 15 1. Soft Tissues: Check for symmetry, swelling, loss of tissue planes, and subcutaneous air. Skeletal Structures: Examine the clavicles, scapulas, vertebrae, sternum, and ribs. Look for symmetry. In a good x-ray, the clavicles are symmetrical. Check for osteolytic or osteoblastic lesions, fractures, and arthritic changes. Look for rib-notching. Diaphragm: Sides should be equal and slightly rounded, although the left is usually slightly lower by one rib interspace. Costophrenic angles should be clear and sharp. Blunting suggests scarring or fluid. It takes about 100 200 mL of pleural fluid to cause blunting. Check below the diaphragm for the gas pattern and free air. A unilateral high diaphragm suggests paralysis (from nerve damage, trauma, or an abscess), eventration, or loss of lung volume on that side because of atelectasis or pneumothorax. A low, flat diaphragm suggests COPD. Mediastinum and Heart: The aortic knob should be visible and distinct. Widening of the mediastinum is seen with traumatic disruption of the thoracic aorta. In children, do not mistake the normally prominent thymus for widening. Mediastinal masses can be associated with Hodgkin disease and other lymphomas. The trachea should be in a straight line with a sharp carina. Tracheal deviation suggests a mass (tumor), goiter, unilateral loss of lung volume (collapse), or tension pneumothorax. The heart should be less than one-half the width of the chest wall on a PA film. If greater than one half, consider the presence of CHF or pericardial fluid. Hilum: The left hilum should be up to 2 3 cm higher than the right. Vessels are seen. Look for any masses, nodes, or calcifications. Lung Fields: Note the presence of any shadows from CVP lines, NG tubes, pulmonary artery catheters, etc. The fields should be clear with normal lung markings all the way to the periphery. The vessels should taper to become almost invisible at the periphery. Vessels in the lower lung should be larger than those in the upper lung. A reversal of this difference (called cephalization) suggests pulmonary venous hypertension and heart failure. Kerley B lines, small linear densities found usually at the lateral base of the lung, are associated with CHF. Check the margins carefully; look for pleural thickening or calcification, masses, and pneumothorax. If the lungs appear hyperlucent with a relatively small heart and flattening of the diaphragms, COPD is likely. Thin, plate-like linear densities are associated with atelectasis. To locate a lesion, do not forget to check a lateral film and remember the "silhouette sign." Obliteration of all or part of a heart border means the lesion is anterior in the chest and lies in the right middle lobe, lingula, or anterior segment of the upper lobe. A radiopacity that overlaps the heart but does not obliterate the heart border is posterior and lies in the lower lobes. Examine carefully for the following: | | 1. Coin lesions: Caused by granulomas (50% of cases and usually calcified and caused by histoplasmosis, 25%; TB, 20%, or coccidioidomycosis, 20%; varies with locale); primary carcinoma (25%), hamartoma (< 10%), and metastatic disease (< 5%) 2. Cavitary lesions: Caused by abscess, cancer, TB, coccidioidomycosis, Wegener granulomatosus 3. Infiltrates: Two major types | | a. Interstitial Pattern. "Reticular." Caused by granulomatous infections, miliary TB, coccidioidomycosis, pneumoconiosis, sarcoidosis, CHF. "Honeycombing" represents end-stage fibrosis caused by sarcoid, RA, and pneumoconiosis. b. Alveolar Pattern. Diffuse, quick progression and regression. "Butterfly" pattern or air bronchograms. Caused by PE, pneumonia, hemorrhage, or PE associated with CHF. |
|
Lateral Film Examine the structures shown in Figure 15 2. Check for 3D location of lesions. Pay close attention to retrosternal clear space, costophrenic angles, and the path of aorta. |
| |  |