Spinal Cord Disorders
Authors: Flaherty, Alice W.; Rost, Natalia S.
Title: Massachusetts General Hospital Handbook of Neurology, The, 2nd Edition
Copyright 2007 Lippincott Williams & Wilkins
> Table of Contents > Adult Neurology > Spinal Cord Disorders
Spinal Cord Disorders
A. Acute cord compression is an emergency
Consider this in any pt with rapidly progressive spinal cord sx, especially of bladder or bowel.
1. Exams: Rectal sensory and motor exam, emergent spinal MRI. Do whole spine if cancer suspected.
2. Rx: Consider dexamethasone 100 mg IV push or the methylprednisolone protocol available in most ERs, stat neurosurgery consult, or XRT. Goal is to prevent progression, although deficit can sometimes reverse if it is of recent onset.
3. Blood pressure: Very labile with cord lesions, especially during pain. Overtreating BP (e.g., with nifedipine) can cause hypotension.
4. Cervical cord contusion: High-dose steroids, hard collar unless cervical instability already ruled out with C-spine x-ray (but do not flex/extend if there is a known cord contusion).
B. Pts with back pain and known cancer
Assume cord compression until proven otherwise. see p. 117 for workup.
P.114
C. Terminology
1. Bone problems: Spondylosis = degeneration. Cervical spondylosis sometimes used as synonym for stenosis. Spondylolisthesis = anterior subluxation. Spondylolysis = isthmic spondylolisthesis.
2. Cord problems: Myelopathy and myelitis are spinal cord damage and inflammation, respectively. Cf. myopathy and myositis, which are muscle conditions.
D. History
Radiation of pain, triggers, numbness, weakness, incontinence, weight loss, IVDA, DM, previous surgery, trauma, litigation, degree of disability, assoc. depression. With neck pain, ask about chest pain, shortness of breath, radiation to jaw.
1. Location: Thoracic level suggests metastases.
2. Character: Burning, electric, aching.
3. Precipitants: Walking, sitting, squatting, leaning forward, coughing, time of day.
4. Bladder changes: Frequency, urgency, sensation during voiding, sexual function.
a. UMN lesion: Bladder stretch reflex is disinhibited and spastic, so small bladder and frequent voids.
b. LMN lesion: Retention, sometimes with retention overflow.
E. Exam
Document exam carefully, especially if pt. going to OR, to record presurgical deficit.
1. Reflexes: Spread, finger flexors, Hoffman's, crossed adductors, clonus, Babinski, abdominals.
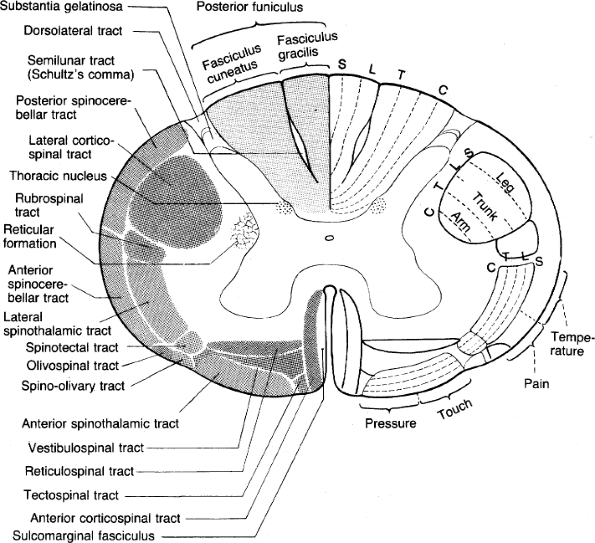
Figure 12. The spinal cord in cross-section. (Reprinted with permission from Duus P. Topical Diagnosis in Neurology. New York: Thieme; 1983: 49.)
2. Straight leg raise (SLR): For L5, S1 irritation. Pain during reverse SLR (extension) suggests L3 or L4 irritation. Pain on palpation, range of motion, posture (anthropoid in stenosis), abdominal reflexes, clonus, pulses, atrophy, fasciculations, caf -au-lait spots, Lhermitte's sign.
3. FABER (Flex-ABduct-Extend-Rotate): Put ankle on opposite knee; rotate knee towards exam table. Positive for hip dz and mechanical low back pain, but not for disc dz.
4. Hysterical back pain: If pain on simulated axial loading (push top of head), or if cannot tolerate straight leg raise, but can sit/put socks on.
5. Bowel/bladder: Prostate, bulbocavernosus (finger in rectum, pull on penis or bladder catheter), cremaster, anal wink, percuss bladder, measure postvoid residual (if residual >100 cc, leave catheter in). Any abnormality may be indication for emergent MRI.
6. Sensory lesions: Look for sensory level, dissociation of sensory modalities. Pinprick is lost first (vs. peripheral nerve injury, where light touch is lost first). See Sensory Loss, p. 111.
P.115
F. DDx
1. Conus medullaris vs. cauda equina compression: The former is a cord lesion, the latter peripheral nerve. However, prognosis is similar, and sx often overlap.
Table 32. Distinguishing conus and cauda syndromes.
Conus Medullaris Cauda Equina Onset Sudden, bilateral Gradual, unilateral Pain Mild, bilateral Severe, radicular Bladder/bowel Severe, early Late Sensory loss Symmetric, saddle distribution. Asymmetric Touch vs. pain Touch/pain dissociation No dissociation Motor loss Mild, symmetric Marked asymmetric atrophy Fasciculations Common Rare Reflexes Lose ankle but not knee jerk May lose knee jerk too 2. Cortical vs. spinal or peripheral lesion: Former has slow mvts., latter has fast but weak mvts.
3. Disc herniation vs. spinal stenosis:
a. Provocation: Both worse with coughing, Valsalva. Stenosis worse with walking, better with leaning forward ( anthropoid posture).
b. Reflexes: Stenosis causes brisk reflexes, toes can be up. Disc herniation causes dropped reflexes.
4. Central cord syndrome: Arms weaker than legs, pain and temperature sensation worse than dorsal column modalities vibration and proprioception. LMN signs in some segments. Later, UMN signs below the lesion. Anterior spinal artery infarct can do this. (Relative preservation of dorsal column modalities of vibration and proprioception.)
5. Cervical cord contusion: Usually after hyperextension with underlying stenosis or instability.
6. Paraparesis: Consider spinal stenosis or mass, falx meningioma, spinal ischemia, thyrotoxic paralysis. Check orthostatic BPs.
7. Onc: Pain worse lying/at night. Weakness usually legs first; not clear why there is usually sacral sparing. Position/vibration sense very sensitive for compression. Occasionally ataxia. Consider leptomeningeal metastases, q.v. p. 124; lumbosacral plexopathy in pelvic cancer. Most spine tumors compress rather than invade.
a. Leptomeningeal tumors: See Tumors of Brain p. 120.
b. Extradural (55%):
1) Metastases: Common. Consider lung, breast, prostate, lymphoma, kidney.
2) Primary: Rare. Chordomas, neurofibromas, osteoid osteomas, osteoblastomas, aneurysmal bone cysts, vertebral hemangiomas.
c. Intradural extramedullary (40%): Schwannomas, meningiomas, neurofibromas, lipomas.
d. Intramedullary (5%): Astrocytomas (30%), ependymomas (30%), miscellaneous.
8. Ortho: Compression fracture, ankylosing spondylitis (get plain films of sacral joint; HLA B-27 Ag), Paget's dz.
9. Other: Epidural abscess, osteomyelitis, vasculitis, transverse myelitis, spondylitis, aortic dissection, cord embolus, bleed, Guillain-Barr , CIPD, schistosomiasis .
P.116
G. Tests
1. Spine MR: Useless if metal in back (e.g., previous surgery), but hip replacements are usually okay. Consider pain premedication. 24% of asymptomatic pts have bulging disc; 4% have stenosis.
a. Screening sagittal view of whole spine: If you suspect metastasis (30% have second met).
b. Contrast: If you suspect leptomeningeal dz or myelitis or if there was previous surgery and you need to tell scar from disc.
2. X-rays: Get C-spine if recent neck trauma. Consider flexion-extension C-spine films, especially if transient quadriparesis after a neck injury or if there is A-P pain. Lumbosacral x-rays are usually useless except if spine may be unstable; then get flexion-extension films.
3. CT myelogram: If MRI contraindicated, previous back surgery, suspected dural AV fistula, CSF leak or obstruction.
4. LP: Can show high prot. below cord comp, because of pooling.
5. Bone scan: Not useful except as screen for infection or metastases all over. Rarely positive if plain films and ESR nl. Does not show myeloma.
6. Blood: Consider ESR, UBJ, SIEP, PSA, CA125, CEA.
7. CSF: Avoid LPs, as risk of deterioration in
8. EMG: If need to distinguish radiculopathy (nl nerve conduction velocity, but F-wave abnormal) from peripheral neurop. Denervation changes after disc occur 1-2 wk in paraspinous muscles; 2-5 wk in leg. Polyphasic renervation potentials start ~10 wk.
H. Rx of noncancer spinal pain
NSAIDS, gabapentin, duloxetine, nortriptyline, soft collar or back brace, physical therapy; consider surgery if myelopathy. Bed rest rarely helps.
P.117
1. Disc herniation:
a. Home neck traction: Kit available in surgical supply stores. 10-20 min qd, facing door, 6-8 lb in sandbag. Head should be pulled 15 degrees forwards, not back. Pressure on both occiput and mandible. Should not hurt.
2. Spinal stenosis: NSAIDS, physical therapy, surgery. Pt may tolerate bicycling more than other forms of exercise.
I. Rx of spine pain in a pt with cancer
Assume spinal cord compression until proven otherwise.
1. Neurological deficit on exam:
a. Dexamethasone: 100 mg IV bolus.
b. Emergent MRI or myelogram: Multiple lesions are common, so request longitudinal scout of entire spine. For MRI appearance of spinal cord tumors, see p. 189.
1) Tumor and > 80% stenosis: Give emergent XRT, consider surgery. Continue dexamethasone 96 mg qd; taper as tolerated.
2) Tumor and <80% stenosis: Nonemergent XRT surgery.
3) No tumor: Symptomatic rx.
2. No neuro deficit: Get plain spine films.
a. If abnormal x-ray with >50% collapse of a vertebral body or pedicle erosion, get emergent MRI and proceed as above.
b. If normal x-ray: Get nonemergent MRI.
3. Acute cord compression rx in cancer:
a. Dexamethasone: 100 mg bolus, then 24 mg q6h. In breast cancer and lymphoma, steroids kill tumor, as well as decrease edema and pain.
b. Neurosurgery consult: Emergent.
1) Indications: Decompression, tissue diagnosis, displaced bone or ligament, unstable spine, or relapse at previously irradiated site. May reverse paraplegia.
2) Relative contraindications: Very radiosensitive tumor (myeloma, lymphoma), total paralysis >24 h. Laminectomy no better than radiation. Anterior decompression and stabilization beneficial, but most pts are poor surgical candidates.
c. Radiation therapy within 12 h: See below. After XRT, 80% of pts. who could walk before can still walk, <50% if paraparetic before, <10% if paraplegic before.
4. Nonemergent cord compression rx in cancer:
a. Dexamethasone: 10 mg q6h.
b. Radiation therapy:
1) Dose limit: 300 rad fractions 10, i.e., 3000 rads. Higher dose causes transverse myelitis. Need to simulate and plan field carefully if window may overlap previous radiation therapy area.
2) Contraindications:
a) Bone compression: If bone, not tumor, is compressing cord, pt needs surgery, not radiation therapy.
b) Radio-resistant tumor: E.g., thyroid cancer, renal cancer, sarcoma.
c) Previous XRT in same region: Unless pts have only a few months to live, XRT twice in same field will cause paralysis.
c. Chemotherapy:
1) Prostate metastases: Start flutamide several days before Lupron; latter has temporary agonist effect and can cause swelling with acute cord compression.
2) Lymphoma.
P.118
EAN: 2147483647
Pages: 109