17. Cannabinoid receptor antagonists - a perspective
Editors: Spanagel, Rainer; Mann, Karl F.
Title: Drugs for Relapse Prevention of Alcoholism, 1st Edition
Copyright 2005 Springer
> Table of Contents > Cannabinoid receptor antagonists: a perspective
Cannabinoid receptor antagonists: a perspective
Mauro A.M. Carai1
Carla Lobina1
Gian Luigi Gessa1, 2
Giancarlo Colombo2
1 Department of Neuroscience, University of Cagliari, Cagliari, Italy
2 C.N.R. Institute of Neuroscience, Section of Cagliari, Viale Diaz 182, 09126 Cagliari, Italy
Introduction
Cannabinoid CB1 receptors are G-protein coupled receptors, located in different brain areas, including the cerebral cortex, hippocampus, basal ganglia, limbic structures and cerebellum (see [1]). Together with their endogenous ligands (anandamide and 2-arachidonyl-glycerol- identified to date), cannabinoid CB1 receptors constitute the so-called endocannabinoid system . When activated, cannabinoid CB1 receptors suppress the neuronal release of different excitatory and inhibitory neurotransmitters, including acetylcholine, noradrenaline, dopamine, serotonin, GABA, glutamate and aspartate (see [1]). As a consequence, cannabinoid CB1 receptors have been implicated in physiological functions such as cognition, control of movement, pain perception, and emotional responses as well as appetite (see [1]).
Furthermore, in recent years, accumulating lines of experimental evidence have suggested the possible involvement of the brain cannabinoid CB1 receptor system in the neural circuitry controlling alcohol intake, including alcohol relapse-like drinking, and alcohol reinforcing properties. Specifically, the acute administration of cannabinoid receptor agonists CP 55,940 and WIN 55,212-2 has been found to stimulate alcohol intake in selectively bred Sardinian alcohol-preferring (sP) rats [2] and enhance the break-point for beer (i.e., an index of the appetitive or motivational properties of alcohol) in Wistar rats [3]. These effects were completely blocked via pre-treatment with the selective cannabinoid CB1 receptor antagonist SR 141716, indicating that they were indeed mediated by the cannabinoid CB1 receptor [2, 3].
Conversely, the administration of SR 141716 has repeatedly been reported to produce opposite effects. Specifically, SR 141716 has been found to:
Reduce voluntary alcohol intake and alcohol preference under the home cage, 2-bottle alcohol versus water choice paradigm in alcohol-experienced C57BL/6 mice [4], sP rats [5] and Wistar rats [6], which may model the maintenance or active drinking phase of human alcoholism;
Suppress the acquisition of alcohol drinking behavior in alcohol-naive sP rats, that is rats which had never consumed alcohol before the start of the experiment [7];
Suppress the alcohol deprivation effect (ADE; a model of alcohol relapses in human alcoholics) in sP rats (see below);
Decrease the oral self-administration of alcohol in unselected rats tested under operant procedures (i.e., experimental paradigms in which rats were trained to press a lever to gain access to alcohol) [8] (see also L. Parsons and G. Koob's contribution to [9]);
Attenuate the appetitive or motivational properties of alcohol, as revealed by a decrease in the probability of the completion of response requirements for alcohol in operant procedures using unselected rats [8, 10] and by the suppression of extinction responding for alcohol (i.e., the maximal amount of work which a rat trained to lever-press for alcohol is willing to perform to obtain alcohol) in sP rats [11].
P.182
In agreement with the above results on the effect of the pharmacological blockade of the cannabinoid CB1 receptor by SR 141716, CB1 receptor knockout mice tested under the 2-bottle choice paradigm displayed significantly lower levels of alcohol preference and consumption in comparison to the wild-type mice ([12, 13, 14 and 15]; see however [16]).
Taken together, these results suggest that the cannabinoid CB1 receptor is one of multiple receptor systems implicated in the mediation of the behavioral responses to alcohol.
Effect of SR 141716 on relapse-like behavior in alcohol-preferring rats
The possible anti-relapse properties of SR 141716 have been tested by investigating its effect on ADE in alcohol-preferring sP rats. ADE is defined as the transient increase in alcohol intake which occurs in several animal species after a period of abstinence from alcohol, and ADE has been proposed to model the loss of control over alcohol and the episodes of alcohol relapse of human alcoholics (see [17, 18]). Notably, ADE is a relevant feature of alcohol drinking behavior of sP rats. Indeed, after a proper period of exposure to alcohol and a subsequent period of alcohol deprivation, sP rats display a pronounced ADE during the first hour of re-access to alcohol [19, 20]. Furthermore, ADE in sP rats is reduced by the anti-relapse agent naltrexone (this laboratory, unpublished observations). These results make sP rats a suitable animal model, with predictive validity for pharmacological investigations on ADE.
In the experiment with SR 141716 [21], adult male sP rats were individually housed and continuously (24 h/day) offered alcohol (10%, v/v) and water under the standard home cage 2-bottle choice paradigm with unlimited access for 4 consecutive weeks. Subsequently, rats were divided into two groups
P.183
(matched for alcohol intake over the last seven days). One group was deprived of alcohol for 15 consecutive days, during which water was the sole fluid available (alcohol-deprived rats). The second group continued to have unlimited access to alcohol and water (alcohol-nondeprived rats), consuming an average of approximately 6 g/kg/day alcohol. At the end of the deprivation phase, rats of both groups (alcohol-deprived and -nondeprived) were further divided into four subgroups (n = 12-13) and acutely and intraperitoneally injected with 0, 0.3, 1 and 3 mg/kg SR 141716, 30 min before lights off. Alcohol was re-presented at lights off and its consumption was recorded 1 h later. Alcohol intake was recorded 60 min later (previous studies have indicated that the time interval of 60 min after alcohol re-presentation is the interval during which ADE is maximal in sP rats [19, 20]). Standard rat chow was available throughout the study.
The results of the study showed that alcohol intake was approximately two times higher in vehicle-treated alcohol-deprived rats than in vehicle-treated alcohol-nondeprived rats, indicative of the development of a robust ADE (Fig. 1). This extra intake of alcohol was, however, eliminated by all doses of SR 141716 (Fig. 1). Indeed, alcohol intake in the alcohol-deprived rat groups treated with all doses of SR 141716 was a) significantly lower than that recorded in alcohol-deprived vehicle-dosed rats, and b) not significantly different from that recorded in the corresponding alcohol-nondeprived SR 141716-treated groups.
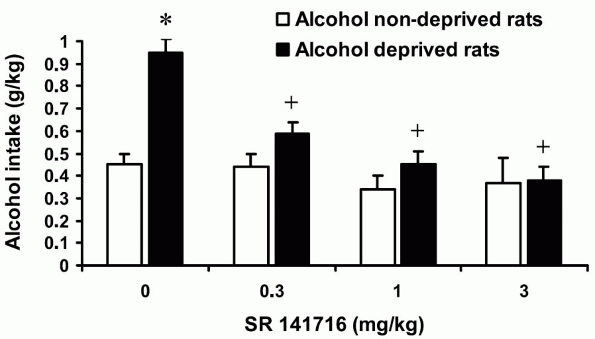 |
Figure 1. Suppressing effect of the cannabinoid CB1 receptor antagonist SR 141716 on the alcohol deprivation effect (ADE) in sP rats with alcohol given under the 2-bottle choice regimen. Each bar is the mean + SEM of n = 12-13. *: P < 0.05 with respect to vehicle-treated alcohol-nondeprived rats; +: P < 0.05 with respect to vehicle-treated alcohol-deprived rats (Newman-Keuls test). Reprinted from Eur J Pharmacol 443: 95-97, 2002, with permission from Elsevier. |
P.184
These results suggest that the cannabinoid CB1 receptor is likely part of a neural substrate mediating ADE. These results, together with the apparent safety and potential use in humans of SR 141716 (Rimonabant) [22], also suggest that SR 141716 should be tested for its ability in preventing alcohol relapse in human alcoholics.
Effect of the combination of SR 141716 plus naloxone on relapse-like behavior in alcohol-preferring rats
Recent clinical surveys suggest that positive therapeutic outcomes in the treatment of alcohol relapse may be achieved by using a combination of drugs. For example, a recent, double-blind placebo-controlled study demonstrated that the combination of naltrexone and acamprosate tended to be more effective than the single application of either drug in the prevention of alcohol relapse in alcoholics [23]. Following this line of thought, this laboratory recently tested the hypothesis that a combination of SR 141716 with the opioid receptor antagonist naloxone would result in a potentiation of the reducing effect of each single drug on ADE in alcohol-preferring sP rats.
The procedure employed in this experiment was similar to that used in the study testing SR 141716 alone (see above). Specifically, adult male sP rats were singly housed and continuously (24 h/day) offered alcohol (10%, v/v) and water under the home cage 2-bottle regimen for 8 consecutive weeks. After the initial period of access to alcohol and water, rats were divided into two groups matched for similar daily alcohol consumption and preference over the last 7 days. One group was deprived of alcohol for 14 consecutive days, during which water was the sole fluid available (alcohol-deprived rats). The second group continued to have unlimited access to alcohol and water (alcohol-nondeprived rats). At the end of the deprivation phase, rats of both groups were divided into four subgroups (n = 16), matched for body weight, and acutely treated with: a) SR 141716 vehicle plus naloxone vehicle; b) 0.05 mg/kg SR 141716 plus naloxone vehicle; c) SR 141716 vehicle plus 0.01 mg/kg naloxone; d) 0.05 mg/kg SR 141716 plus 0.01 mg/kg naloxone. The SR 141716 and naloxone doses were chosen so as to be ineffective when given alone. Drugs were administered intraperitoneally 30 min before alcohol presentation (which coincided with lights off). Alcohol was re-presented at lights off. Alcohol intake was recorded 60 min later. Standard rat chow was available throughout the study.
As expected, after alcohol re-presentation, alcohol intake was higher by approximately 50% in control alcohol-deprived rats as compared to control alcohol-nondeprived rats (Fig. 2), indicating the development of ADE. When given alone, neither 0.05 mg/kg SR 141716 nor 0.01 mg/kg naloxone affected the extra amount of alcohol intake, which constitutes ADE. In contrast, their combination reduced ADE by approximately 30% (Fig. 2).
These results are in close agreement with those of recent studies, demonstrating that SR 141716 and the opioid receptor antagonist naltrexone synergistically
P.185
reduce the break-point for alcohol in unselected rats [24] as well as acquisition of alcohol drinking behavior in alcohol-preferring sP rats (this laboratory, unpublished observations), providing further support to the hypothesized existence of functional interactions between the cannabinoid and opioid receptor systems in relation to alcohol drinking behavior [2, 25]. Accordingly, previous work has demonstrated that the stimulating effects of cannabinoids and morphine on alcohol intake were blocked by both SR 141716 and naloxone [2, 25]. Finally, the extension to food intake of the synergistic reducing effect of SR 141716 and naloxone in rats [26, 27] suggests that the functional relationship between cannabinoid and opioid receptor systems pertains not only to alcohol intake but to different ingestive behaviors as well.
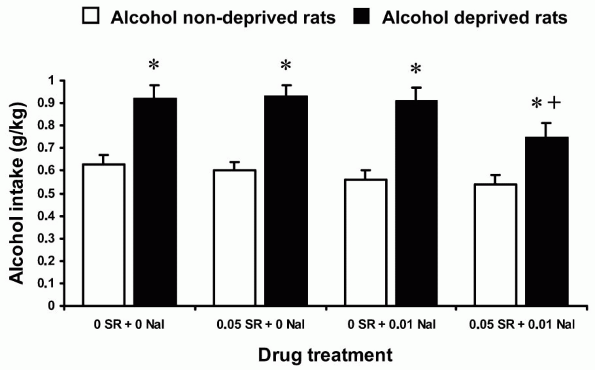 |
Figure 2. Reducing effect of the combination of the cannabinoid CB1 receptor antagonist SR 141716, and the opioid receptor antagonist naloxone, on the alcohol deprivation effect (ADE) in sP rats with alcohol given under the 2-bottle choice regimen. Each bar is the mean + SEM of n = 16. *: P < 0.05 with respect to alcohol-nondeprived rats treated with the corresponding doses of SR 141716 and naloxone; +: P < 0.05 with respect to alcohol-deprived rats treated with SR 141716 vehicle plus naloxone vehicle (Newman-Keuls test). |
The possible generalization to human alcoholics of the reducing effect of the combination of SR 141716 and naloxone on alcohol relapse-like drinking in sP rats would indicate a new therapeutic strategy.
References
1 Iversen L (2003) Cannabis and the brain. Brain 126: 1252-1270
2 Colombo G, Serra S, Brunetti G, Gomez R, Melis S, Vacca G, Carai MAM, Gessa GL (2002) Stimulation of voluntary ethanol intake by cannabinoid receptor agonists in ethanol-preferring sP rats. Psychopharmacology 159: 181-187
P.186
3 Gallate JE, Saharov T, Mallet PE, McGregor IS (1999) Increased motivation for beer in rats following administration of a cannabinoid CB1 receptor agonist. Eur J Pharmacol 370: 233-240
4 Arnone M, Maruani J, Chaperon F, Thi bot M-E, Poncelet M, Soubri P, Le Fur G (1997) Selective inhibition of sucrose and alcohol intake by SR 141716, an antagonist of central cannabinoid (CB1) receptors. Psychopharmacology 132: 104-106
5 Colombo G, Agabio R, F M, Guano L, Lobina C, Loche A, Reali R, Gessa GL (1998) Reduction of voluntary ethanol intake in ethanol-preferring sP rats by the cannabinoid antagonist SR 141716. Alcohol Alcoholism 33: 126-130
6 Lallemand F, Soubri PH, De Witte PH (2001) Effects of CB1 cannabinoid receptor blockade on ethanol preference after chronic ethanol administration. Alcohol Clin Exp Res 25: 1317-1323
7 Serra S, Carai MAM, Brunetti G, Gomez R, Melis S, Vacca G, Colombo G, Gessa GL (2001) The cannabinoid receptor antagonist SR 141716 prevents acquisition of drinking behaviour in alcohol-preferring rats. Eur J Pharmacol 430: 369-371
8 Freedland CS, Sharpe AL, Samson HH, Porrino LJ (2001) Effects of SR 1417161A on alcohol and sucrose self-administration. Alcohol Clin Exp Res 25: 277-282
9 Hungund BL, Basavarajappa BS, Vadasz C, Kunos G, Rodriguez de Fonseca F, Colombo G, Serra S, Parsons L, Koob GF (2002) Ethanol, endocannabinoids, and the cannabinoidergic signaling system. Alcohol Clin Exp Res 26: 565-574
10 Gallate JE, McGregor IS (1999) The motivation for beer in rats: effects of ritanserin, naloxone and SR 141716. Psychopharmacology 142: 302-308
11 Colombo G, Vacca G, Serra S, Carai MAM, Gessa GL (2004) Suppressing effect of the cannabinoid CB1 receptor antagonist, SR 141716, on alcohol's motivational properties in alcohol-preferring rats. Eur J Pharmacol 498: 119-123
12 Hungund BL, Szakall I, Adam A, Basavarajappa BS, Vadasz C (2003) Cannabinoid CB1 receptor knockout exhibit markedly reduced voluntary alcohol consumption and lack alcohol-induced dopamine release in the nucleus accumbens. J Neurochem 84: 698-704
13 Poncelet M, Maruani J, Calassi R, Soubri P (2003) Overeating, alcohol and sucrose consumption decrease in CB1 receptor deleted mice. Neurosci Lett 343: 216-218
14 Wang L, Liu J, Harvey-White J, Zimmer A, Kunos G (2003) Endocannabinoid signaling via cannabinoid receptor 1 is involved in ethanol preference and its age-dependent decline in mice. Proc Natl Acad Sci USA 100: 1393-1398
15 Naassila M, Pierrefiche O, Ledent C, Daoust M (2004) Decreased alcohol self-administration and increased alcohol sensitivity and withdrawal in CB1 receptor knockout mice. Neuropharmacology 46: 243-253
16 Racz I, Bilkei-Gorzo A, Toth ZE, Michel K, Palkovits M, Zimmer A (2003) A critical role for the cannabinoid CB1 receptors in alcohol dependence and stress-stimulated ethanol drinking. J Neurosci 23: 2453-2458
17 Boening JA-L, Lesch OM, Spanagel R, Wolffgramm J, Narita M, Sinclair D, Mason BJ, Wiesbeck GA (2001) Pharmacological relapse prevention in alcohol dependence: from animal models to clinical trials. Alcohol Clin Exp Res 25: 127S-131S
18 McBride WJ, Le A-D, Noronha A (2002) Central nervous system mechanisms in alcohol relapse. Alcohol Clin Exp Res 26: 280-286
19 Agabio R, Carai MAM, Lobina C, Pani M, Reali R, Vacca G, Gessa GL, Colombo G (2000) Development of short-lasting alcohol deprivation effect (ADE) in Sardinian alcohol-preferring rats. Alcohol 21: 59-62
20 Serra S, Brunetti G, Vacca G, Lobina C, Carai MAM, Gessa GL, Colombo G (2003) Stable preference for high ethanol concentrations after alcohol deprivation in Sardinian alcohol-preferring (sP) rats. Alcohol 29: 101-108
21 Serra S, Brunetti G, Pani M, Vacca G, Carai MAM, Gessa GL, Colombo G (2002) Blockade by the cannabinoid CB1 receptor antagonist, SR 141716, of alcohol deprivation effect in alcohol-preferring rats. Eur J Pharmacol 443: 95-97
22 Le Fur G, Arnone M, Rinaldi-Carmona M, Barth F, Heshmati H (2001) SR 141716, a selective antagonist of CB1 receptors and obesity. Abstract book, 2001 Meeting of the International Cannabinoid Research Society, San Lorenzo de El Escorial, Spain, 101
23 Kiefer F, Jahn H, Tarnasker T, Helwig H, Briken P, Holbach R, Kampf P, Stracke R, Baehr M, Naber D et al. (2003) Comparing and combining naltrexone and acamprosate in relapse prevention of alcoholism. A double-blind, placebo-controlled study. Arch Gen Psychiatry 60: 92-99
P.187
24 Gallate JE, Mallet PE, McGregor IS (2004) Combined low dose treatment with opioid and cannabinoid receptor antagonists synergistically reduces the motivation to consume alcohol in rats. Psychopharmacology 173: 210-216
25 Vacca G, Serra S, Brunetti G, Carai MAM, Gessa GL, Colombo G (2002) Boosting effect of morphine on alcohol drinking is suppressed not only by naloxone but also by the cannabinoid CB1 receptor antagonist, SR 141716. Eur J Pharmacol 445: 55-59
26 Kirkham TC, Williams CM (2001) Synergistic effect of opioid and cannabinoid antagonists on food intake. Psychopharmacology 153: 267-270
27 Rowland NE, Mukherjee M, Robertson K (2001) Effects of the cannabinoid receptor antagonist SR 141716, alone and in combination with dexfenfluramine or naloxone, on food intake in rats. Psychopharmacology 159: 111-116
EAN: 2147483647
Pages: 26