1 - Prevention of Stroke - A Perspective
Editors: Norris, John W.; Hachinski, Vladimir
Title: Stroke Prevention, 1st Edition
Copyright 2001 Oxford University Press
> Table of Contents > 1 - Prevention of Stroke: A Perspective
1
Prevention of Stroke: A Perspective
John W. Norris
Vladimir Hachinski
Humans have never been healthier. The greatest benefit to humans from the explosion of scientific advances in the twentieth century has been the conquest disease and advancement of health well-being.1 This applies to both the developed and developing worlds. The anguish of childhood death crippling disability and the plagues that decimated the world not so long ago have been greatly reduced, but as people live longer and better, degenerative diseases of the brain and blood vessels exact their toll.
Fifty years ago, cardiovascular disease was almost unknown in the developing world, but with economic growth comes increased life expectancy, so that the traditional risk factors of infection, parasitic disease, and malnutrition are being replaced by obesity, hypertension, and coronary artery disease. People can afford to smoke more, exercise less, and switch from largely vegetarian diets to those rich in animal fats. A global epidemic of cardiovascular disease (and stroke) is predicted to encompass a large part of the world's population that lives in China, India, Indonesia, and the former Soviet Union (Fig. 1.1).2 Conversely, as these diseases increase in the developing world, health education is bringing healthier lifestyles to the Western world, where cardiovascular diseases and stroke are diminishing in incidence.
The incidence and mortality of stroke have declined substantially in the United States (the best-documented country) since the 1920s, reaching an annual rate of
P.2
decline of 5% by the 1970s.3 This decline has slowed in recent decades because of both successful treatment and successful prevention, while computerized tomography (CT) brain scanning is revealing many minor cases of stroke that were previously attributed to other lesions.4
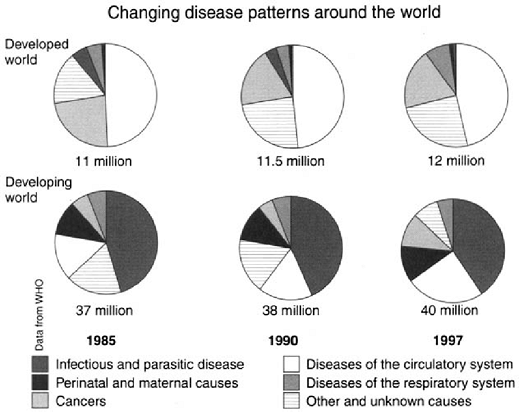 |
FIGURE 1.1. Changing disease patterns around the world. Reprinted with permission from Ref. 2. |
CT scanning partly explains the apparent fall in stroke severity, but a true shift to less severe strokes was documented in the Framingham study. This not due to any change in the proportions of ischemic or hemorrhagic stroke but represented a real increase in patients with minor neurological deficits compared with patients admitted in unconscious states with more devastating lesions. 5
According to epidemiologists, the explanations for these favorable changes can only be found by careful analysis of stroke incidence and fatality,6 but epidemiologic studies often overlook the importance of verifying presence and type of stroke using clinical and brain imaging methods. Data from family physician surveys and death certificates can be of dubious value or frankly misleading.
Primary Prevention of Stroke
Five factors must be considered in the primary prevention of stroke. These include nonmodifiable risk factors, modifiable medical prevention, surgical prevention, and public health strategies.
P.3
Nonmodifiable Risk Factors
Nothing at present can be changed regarding age, sex, or family history, although genetic engineering is likely to play an increasingly major role in all forms of disorders. Males have always suffered the lion's share of vascular disease in the heart, brain, and peripheral blood vessels, the prevalence rises steeply with age. In developing countries, the number of old people (over 60 years) is predicted to increase from 171 million in 1998 to 1.594 billion by 2050.7
The contributions of nurture and nature in stroke incidence remain uncertain, but clear epidemiological evidence indicates that nurture plays the major role. The high prevalence of all forms stroke in Japan (one of the world's hot spots ) declines with westward emigration. The decrease in stroke frequency from Japan through Hawaii to the United States indicates that whatever prognosis the genetic basis provides, it is strongly influenced by lifestyle.3
Modifiable Risk Factors
Details of lifestyle modification and treatable risk factors are presented in later chapters. Major changes in the way people live, exercise, smoke, drink, and eat have had profound effects on the incidence, mortality, and severity of all forms of vascular disease.
The lay public tends to believe that stroke and heart attack are due to stress. In ancient times, apoplexy was attributed to emotion, sloth, drunkenness, and gluttony. 8 Although there is convincing evidence from many sources that sudden cardiac death can be precipitated by acute emotional events, such as the threat of death, no such relationship has ever been demonstrated in stroke. In ischemic stroke this is hardly surprising, since the commonest cause thrombo embolism from the extracranial arteries or heart.
Attempts to relate the type A personality stroke remain strikingly unsuccessful. The idea that sudden, precipitous rises in blood pressure can produce hemorrhagic stroke is more plausible. It was claimed that this occurred in Israel during the Persian Gulf crisis.9
Fruit and vegetables have been promoted for many years as health foods, in part because of the supposedly protective effects their high potassium content. Epidemiologic studies demonstrated a reduction of both vascular disease and cancer in people with large vegetarian moieties in their diet. The explanation offered was that antioxidant vitamins (beta carotene and vitamins B and C) interfere with oxidative damage to DNA and lipoproteins.10 At present insufficient evidence exists to recommend vitamin supplements, pending the results of ongoing ran domized trials, but it is becoming clear that factors previously considered irrelevant, such as diet and cholesterol, are as important in cerobrovascular in cardiovascular disease.11
P.4
The role of the contraceptive pill as a stroke risk factor has become increasingly controversial in recent years. Early studies using high-dose estrogen (>100 micrograms) and primitive methodology were performed before CT scanning was widely used. Studies in recent years using low-dose pills (<50 micrograms) and carefully performed cohort and case control studies indicate either infinitesimal or no risk increase of either ischemic or hemorrhagic stroke. 12 Moreover, mounting evidence suggests that estrogen replacement therapy protects against ischemic cardiac and cerebral disease. 13
Although hypertension is the major preventable risk factor for all forms of vascular disease, surpassed only by malnutrition and smoking as a cause of death worldwide,14 its control only partly explains the decline in mortality from stroke noted in previous decades and probably accounts for only 15%.15 Nevertheless, observational studies indicate that small reductions in diastolic blood pressure have enormous impact at a population level. It is estimated that 2 mm. average blood pressure reduction would result in a 17% decrease the prevalence of hypertension, a 6% reduction in coronary heart disease, and a 15% stroke.16
Cholesterol has emerged only in recent years as a risk factor for stroke.17 An in-depth analysis of randomized trials published in 1998 concluded that hyperlipidemic patients without previous stroke the use of 3-hydroxy-3-methyl glutaryl co-enzyme A (HMG CoA) reductase inhibitors (which lower blood lipid levels) reduce the subsequent incidence of stroke in these patients.18
In patients with previous coronary heart disease, the picture is much clearer. In the Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) study, where pravastatin was given to patients with prior coronary artery disease, stroke risk was significantly reduced over the seven years of follow-up (p < 0.048).19
One problem in determining the role of cholesterol as a stroke risk factor is its compounding effect with hypertension. Where hypertension is sufficiently controlled to reduce hypertensive strokes, dyslipidemia is unmasked as a stroke risk factor.20
In a pooled study of nearly 125,000 persons in China and Japan, hypertension and cholesterol had no synergistic effect. Lower levels were associated with a lower ischemic stroke rate but a higher rate of hemorrhagic stroke. The author's conclusion was that population-wide changes in eastern Asia, such as lower salt intake, higher potassium intake (fruit), more exercise, less obesity, and wider availability of effective antihypertensive drugs would have a major impact on health.21
New risk factors have emerged in recent years but have not yet assumed an established role, such as the metabolic disturbance of hyperhomocysteinemia. Increases in this amino acid turn raise levels of free radical activation, damaging vascular endothelium. The antidote is to increase levels of folic acid as well as vitamins B-12 and B-6, therapeutic trials are in progress.22
P.5
The gram negative bacterium chlamydia pneumoniae affects most of the population in childhood, but elevated liters of the antibody are found patients with coronary artery disease and, more recently, cerebrovascular disease.23 It is postulated that chronic vascular infection initiates or accelerates atherosclerosis and plaque formation. Evidence so far is inconclusive.
Medical Prevention
For some years, the media, taking an oversimplified and overdramatic stance, have promoted the daily use of aspirin (usually one 325 mg. tablet) to ward off heart attacks and strokes. More than half the patients attending cardiology stroke prevention clinics have been taking aspirin, often for years before the event. Although two well-documented trials (one in the United States and one in the United Kingdom) of chronic ingestion 350 500 mg/day aspirin in asymptomatic male physicians demonstrated a decrease in ischemic cardiac events, no such effect was seen on stroke.3 Added to these negative results is the chance of gastrointestinal bleeding related to the dose of aspirin, which may prove fatal, especially with increasing age. There is simply no justification for asymptomatic persons to take aspirin daily prevent stroke. Unfortunately, data are scanty for patients with asymptomatic carotid stenosis, but the only published randomized trial showed no stroke prophylactic effect with long-term aspirin ingestion.24
The broadly aggressive approach of treating all types vascular disease (including that of the heart, brain, and limbs), as in some recent antiplatelet trials,25 has proven effective in preventing events other vascular territories patients without symptoms. Cardiologists lagged behind neurologists for years in endorsing the relationship between atrial fibrillation and embolic stroke, but anticoagulant trials in recent years have demonstrated beyond doubt that warfarin considerably reduces the risk of cardioembolic stroke in both symptomatic and asymptomatic patients.26 Unfortunately, many physicians regard anticoagulant therapy as too dangerous in the very old (over 80 years), even though evidence from trials suggests the opposite. Consequently, only a minority of patients (probably less than 25%) receive anticoagulant therapy, though five separate trials have demonstrated a 68% reduction in stroke outcome.26 A search is underway for alternative anticoagulants that do not require the inconvenience and expense of blood monitoring,27 and devices to monitor coagulation parameters in the home are being tested.28
Surgical Prevention
The studies that have probably had greatest effect are the carotid endarterectomy trials for symptomatic patients, because they have fundamentally established guidelines for surgical practice.29 The value of carotid surgery in asymptomatic
P.6
patients and in those undergoing cardiac surgery is more questionnable. A national survey of Canadian neurologists specializing in stroke concluded that there was insufficient evidence to recommend carotid endarterectomy in asymptomatic carotid stenosis, and, further, the authors did not endorse screening even for asymptomatic patients with risk factors for vascular disease.30
The role of carotid surgery for asymptomatic carotid stenosis remains unsettled, and strong lobbies exist both for and against surgical intervention. The definitive trial, the Asymptomatic Carotid Atherosclerosis Study (ACAS),31 which enrolled 1662 patients with >60% stenosis and followed them over 2.7 years, showed an absolute risk reduction for stroke of only 1% annually. Women had scarcely any benefit at all.
To show benefit, carotid endarterectomy trials must demonstrate a minimal combined risk from angiography and surgery. In ACAS, this was 2.3% for stroke and death, with more risk from angiography (1.2%) than surgery (1.1%). Since all data from trials are gathered state-of-the-art procedures, higher risks may mean the benefit will become negligible in practice, where guidelines are blurred or ignored. For instance, in a survey of Toronto teaching hospitals from 1994 to 1996, the stroke and death rate for asymptomatic carotid surgery was 3.8%,32 raising concerns that the relatively low complication rates achieved by ACAS surgeons could not be matched, even in centers with extensive experience outside trial conditions.
There is no obvious solution to this problem. A search for a subgroup of highrisk patients who will benefit from surgical intervention so far has not been fruitful. Attempts to identify these special risk patients have targeted those with rapidly progressing stenoses using ultrasound33 and those with falling cerebral blood flow values.34 To compound this issue, those at highest risk of stroke may also have the highest risk of ischemic heart disease,33 so that the very patients most needing carotid surgery are the ones that most at risk on the operating table.
Angioplasty and stenting have not yet found a clear place in surgical intervention for symptomatic or asymptomatic disease. Preliminary data suggest that these procedures are too hazardous in asymptomatic patients and are only just acceptable in certain high-risk, symptomatic patients.35 The results of current international trials may shed more light.
Public Health Strategies
Risk factor profiles of potential stroke patients are now well enough established to exert pressure on public health policies aimed at changing lifestyles and screening patients at high risk. To do this, extensive and expensive national campaigns are required to educate not just the public but also physicians. The apparently huge expenditure should be offset by equivalent cost savings from stroke prevention, to say nothing of the reduced toll suffering.
P.7
Screening is ideal in principle, but often poor practice. In a survey of elderly people (>65 years old) for atrial fibrillation in the United Kingdom, 4.7% of 4843 people had atrial fibrillation. Using standard criteria based on published trials, 61% would have benefited from anticoagulation therapy, but in practice only 23% received treatment. The authors concluded that anticoagulants were underused and misdirected. Physicians need to be educated not only concerning anticoagulants but also in the use of hypertensive drugs.
Despite the proven efficacy of drugs to control high blood pressure, compliance is poor, and patients lose enthusiasm, so that even in developed countries many hypertensives remain untreated.36
Public health strategies, including screening for surgical prevention of stroke, are even more complex and uncertain. The spectacular success of carotid endarterectomy in stroke prevention symptomatic patients, following the publication of surgical trials,29 encouraged attempts at repeating these successes in asymptomatic patients. Whether the asymptomatic patient with a 70% carotid stenosis has carotid surgery depends on the individual surgeon, the method of assessing the target artery, patient's preference, hospital, and even country of residence. The ease and safety noninvasive vascular imaging has encouraged the use of this procedure on a massive scale. Screening people in supermarkets or other public areas yields a 5% 6% rate of detectable carotid stenoses, of which at most 1% 2% will be eligible for surgery.37 Some unscrupulous physicians even advertise to the public free carotid doppler examinations on the assumption that a small number will request surgery once carotid lesion is found. Because 67 people with carotid stenoses need to be treated prevent one stroke, the major costs of screening, neurovascular imaging, and surgery, with it's attendant complications, make this strategy impractical.
Secondary Prevention of Stroke
Prevention of further strokes in patients who have already experienced transient ischemic attacks (TIAs) or stroke (secondary prevention) is less effective compared to primary prevention, although patients are more likely follow advice after something happens to them. In a minority of patients, this means a transient ischemic attack, but the vast majority suffer a stroke. The patients at highest risk of having a stroke are those who already have had one. The mainstay of secondary prevention comprises control of risk factors, enhancement protective factors, drug treatment, and other interventions.
Control of Risk Factors
Hypertension remains the most important treatable risk factor for stroke in secondary prevention, as it is in primary prevention. This is true for women and
P.8
men, for systolic and diastolic blood pressure, for ischemic hemorrhagic stroke38 (see Chapter 5). Growing evidence supports a role also for hypertension in cognitive decline; new data suggest that treatment of hypertension may mitigate or prevent this decline.39 In addition, it appears that treatment with the angiotension-converting enzyme inhibitor ramipril in patients who have already had a stroke reduces the risk of by one-third.40
Smoking represents a risk factor for all types of arterial disease (peripheral, coronary, and cerebrovascular) in both primary secondary stroke prevention41 (see Chapter 2). About one-third of individuals still smoke in developed countries and a growing number in the developing world. The WHO has made an antismoking campaign its top priority.
Lipids have long been known as risk factors for coronary disease, but no relationship was established with stroke until recently. Now it is clear that statins decrease the risk of coronary disease, and the evidence suggests a similar fact for stroke prevention. The mechanism remains unclear; it may be lipid lowering, endothelium protection, or both42 (see Chapter 4).
Atrial fibrillation is a serious complication of valvular heart disease. It is an escalating problem in the elderly everywhere, as prevalence of atrial fibrillation doubles every decade. Fortunately warfarin and, to a lesser extent, aspirin are effective in both primary and secondary prevention43 (see Chapter 6).
Homocystinemia is clearly associated with carotid atherosclerosis. What remains to be demonstrated is whether treatment with vitamins will slow, arrest, or reverse the process.41
Many other risk factors have been described. Some are common, such as diabetes, strict treatment of which makes little difference to large vessel disease but prevents small vessel diseases that lead to retinopathy, nephropathy, and neuropathy. Others are rare, such as lupus anticoagulant, and still others uncertain, such as migraine, which may be a marker of increased risk rather than a risk factor itself.
Protective Factors
Good exercise, diet, and drink are powerful protective factors against stroke, along with estrogen replacement for postmenopausal women. Exercise in moderation seems to be good for everything from maintaining health preventing and treating virtually all ailments. A diet rich in fruit and vegetables, hence high in potassium, seems to protect not only the heart, but the brain.44 A drink or two a day may keep the stroke doctor away, although much needs to be clarified regarding the precise role of the ethanol molecule and its various vehicles45 (see Chapter 3). Despite controversy, estrogen replacement therapy for postmenopausal women seems to protect against cardiovascular disease46 (see Chapter 8).
P.9
Interventions
The value of carotid endarterectomy in symptomatic patients with stenosis >70% has been established beyond a reasonable doubt, providing that it can be done within well defined limits of perioperative complications47 (see Chapter 12). Angioplasty and stenting are gaining ground as promising techniques, with overall complication rates approaching those of carotid endarterectomy48 (see Chapter 13). However, the role of carotid endarterectomy in secondary prevention is both clear and durable, whereas experience with angioplasty stenting is brief and controversial. The time has come for a direct comparison. Otherwise, the procedures will fall into a quandary similar to that that clouds the role of angioplasty in peripheral vascular disease almost three decades after it was first attempted.
Drug Therapy
Antiplatelet agents have proven to be effective in decreasing the risk of further stroke after a transient ischemic attack or minor stroke. Aspirin remains the drug of choice, although the right dose continues to be debated49 (see Chapter 10). Ticlopidine, clopidogrel, and dipyridamole may offer better alternatives50 (see Chapter 11).
The only clear role of anticoagulants in secondary prevention is in reducing the risk of recurrent cardiac embolism43,51 (see Chapters 6 and 9). Aspirin decreases the risk of a recurrent stroke, but whether it prevents cardiac embolism or reduces the risk of other strokes to which the patient is prone remains uncertain.
Prevention: Policy and Practice
Stroke poses such a ubiquitous threat of death and disability that an urgent plan of stroke prevention is needed worldwide. Eighty percent of deaths occur in the poor countries of the world, and the number will rise as some most populous countries witness a doubling in the number of their elderly. A hierarchy of values various interventions for stroke must be clarified52 (see Chapter 14).
The challenges are formidable. Even in developed countries, where costs not insuperable, highly effective measures are seldom implemented to their fullest53 (see Chapter 7). Only a fraction of the people who should receive anticoagulant treatment are getting it, and only one in five American hypertensives has his or her blood pressure controlled.54
An intervention can be overused or misused as well underused. This is exemplified by carotid endarterectomy, the best documented surgical procedure for stroke prevention55 (see Chapter 16).
P.10
Translating the results of clinical trials into clinical practice has major limitations56 (see Chapter 15). Patients in clinical trials are selected, receive extraordinary care, and are seldom representative of the general population. Although we have made evidence-based medicine an ideal, there will never be enough evidence from clinical trials to address all pressing health problems. While the results of clinical trials provide the best odds that a particular treatment will benefit patients, they do not directly address whether a particular patient will respond to a specific intervention. More research is needed into the basis of individualizing therapy and the best strategies for acquiring applying knowledge.
As usual, the ideal clashes with affordable57 (see Chapter 17). Not all measures have equal value, and no method is acceptable to all. Eventually, some common measure of value for invested money may emerge, such as disability adjusted life years (DALY) lost, to judge what each society or individual can or wants to afford. This may vary widely, given the great diversity in wealth, priorities, and cultures. Even so, different cultures can make decisions better in reference to a common currency.
Conclusions
Any discussion of the feasibility and costs primary stroke prevention must factor in cost savings. Lifetime costs (as compared to acute care costs) are at least twice as high most quoted figures. A study in the United States in 1997 estimated costs, depending on the type of stroke, at between $90 and $230 thousand per patient, based on 1990 data.58 In one Canadian study, costs plummeted from Can$27,500 in 1993 to Can$10,000 1997, reflecting more than medical factors, such as earlier hospital discharge and a shift of burden to family and social services.59,60
A meaningful attack on significant risk factors can occur only after accurate evaluation of epidemiologic data. People at high risk of stroke due to blood pressure need treatment, but treatment at lower levels of hypertension has progressively less influence on disease trends. Nevertheless, resources must be mobilized worldwide to combat the rising epidemic of vascular disease. One should also bear in mind a note of caution concerning the ethical dimension health promotion sounded by the Irish epidemiologist McCormick: Health promotion falls far short of meeting the ethical imperatives for screening procedures. General practitioners would do better to encourage people live lives of modified hedonism, so that they may enjoy to the full, the only life they are likely have .61
It is known that most risk factors are not thresholds, but gradients. This applies to hypertension as well lipid and homocysteine levels. This implies that there are different cost benefit ratios at different ends of the spectrum and calls for more sophisticated analyses about the effects of treatment.
P.11
Protective factors are emerging as important contributors of individual resistance to disease and its recurrence. Although much has been learned, more needs to be discovered. If all known risk factors for stroke were abolished today, only about half of all strokes would be prevented53 (see Chapter 7). Much more research is needed into the interaction of the environment and genetics, not only in disease development, but in disease protection and individual response to treatment.
References
1. Porter R. The Greatest Benefit to Mankind. London: Harper Collins, 1997.
2. Husten L. Global epidemic of cardiovascular disease predicted. Lancet 1998;352:1530.
3. Bronner LL, Kanter DS, Manson JE. Primary prevention of stroke. N Engl J Med 1995;333:1392 1400.
4. Broderick JP, Phillips SJ, Whisnant et al. Incidence rates of stroke in the eighties. Stroke 1989;20:577 582
5. Wolf PA, D'Agostino RB, O'Neal MA, et al. Secular trends in stroke incidence and mortality. Stroke 1992;23:1551 1555.
6. Bonita R, Broad JB, Beaglehole R. Changes in stroke incidence and case-fatality Auckland, New Zealand, 1981 91. Lancet 1993;342:1470 1473.
7. The hidden epidemic of cardiovascular disease. Lancet 1998;352:1795 (editorial).
8. Schneck MJ. Is psychological stress a risk factor for cerebrovascular disease? Neuroepidemiology 1997;16:174 179.
9. Kleinman Y, Korn-Lubetzki I, Eliashiv S, Abramsky O, Eliakim M. High frequency of hemorrhagic strokes in Jerusalem during the Persian Gulf War. Neurology 1992;42: 2225 2226.
10. Greenberg ER, Sporn MB. Antioxidant vitamins, cancer, and cardiovascular disease. N Engl J Med 1996;334:1189 1190.
11. Gorelick PB. Stroke Prevention: Windows of opportunity and failed expectations? Neuroepidemiology 1997;16:163 173.
12. Schwartz SM, Petitti DB, Siscovick DS, et al. Stroke and use of low-dose oral contraceptives in young women. Stroke 1998;29:2277 2284.
13. Gurwitz D. Oestrogen replacement therapy in postmenopausal women. Lancet 1999;353:674.
14. Murray CJLM, Lopez AD. Evidence-based health policy lessons from the Global Burden of Disease Study. Science 1996;274:740 743.
15. Bonita R, Beaglehole R. Increased treatment of hypertension does not explain the decline in stroke mortality in the United States, 1970 1980. Hypertension 1989; 13 (suppl l):I-69-I-73.
16. Cook NR, Cohen J, Hebert PR, et al. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med 1995; 155: 701 709.
17. Gorelick PB, Schneck M, Bergland LF, Feinberg W, Goldstone J. Status of lipids as a risk factor for stroke. Neuroepidemiology 1997;16:107 115.
18. The long-term intervention with pravastatin in ischemic disease (LIPID) study group. N Engl J Med 1998;339:1349 1357.
19. Bucher HC, Griffith LE, Guyatt GH. Effective HMGcoA reductase inhibitors on stroke. Ann Intern Med 1998; 128:89 95.
20. Spence JD. Statins for prevention of stroke. Lancet 1998;352:909.
P.12
21. Eastern Stroke and Coronary Heart Disease Collaboration Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. Lancet 1998;352:1801 1807.
22. Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N EnglJ Med 1998;328: 1042 1050.
23. Fagerberg B, Gnarpe J, H, et al. Chlamydia pneumoniae but not cytomegalovirus antibodies are associated with future risk of stroke and cardiovascular disease. Stroke 1999;30:299 305.
24. Cote R, Battista RN, Abrahamowicz M, et al. Lack of effect aspirin in asymptomatic patients with carotid bruits and substantial carotid narrowing. Ann Intern Med. 1995;123:649 655.
25. CAPRIE Steering Committee. A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996;348:1329 1339.
26. Albers GW. Atrial fibrillation and stroke three new studies, three remaining questions. Arch Intern Med 1994;154:1443 1448.
27. Fihn SD. Aiming for safe anticoagulation. N Engl J Med 1995;333:54 55.
28. Hirsh J, Weitz JI. New antithrombotic agents. Lancet 1999;353:1431 1436.
29. Barnett HIM, Eliasziw M, Meldrum HE. Drugs and surgery in the prevention of ischemic stroke. N Engl J Med 1995;332:238 248.
30. Perry JR, Szalai JP, Morris JW. Consensus against both endarterectomy and routine screening for asymptomatic carotid artery stenosis. Arch Neurol 1997;54:25 28.
31. Executive committee for the asymptomatic carotid atherosclerosis study. JAMA 1995; 273:1421 1428.
32. Smurawska LT, Bowyer B, Rowed D, Maggisano R, Oh P, Morris JW. Changing practice and costs of carotid endarterectomy in Toronto, Canada. Stroke 1998; 29: 2014 2017.
33. Chambers BR, Morris JW. Outcome in patients with asymptomatic neck bruits. N Engl J Med 1986; 315:860 865.
34. Frey JL. Asymptomatic carotid stenosis: Surgery's the answer, but that's not the question. Ann Neur 1996; 39:3:405 406.
35. Norris JW, Nadareishvili ZG, Rowed DW, Bowyer B, Magigisano R. Are the hazards of carotid stenting unacceptably high? Neurology 1999;52(suppl):A269.
36. Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistance with treatment for hypertension in actual practice. CMAJ 1999;160(l):31 37.
37. O'Leary DH, Polak JF, Krournal RA, et al. Distribution and correlates of sonographically detected carotid artery disease in the Cardiovascular Health Study. Stroke 1991;23:1752 1760.
38. Taylor TN, David PH, Torner JC, Holmes J, Meyer JW, Jacobson ME Lifetime cost of stroke in the United States. Stroke 1996;27:1459 1466.
39. Forette F, Stewx M-L, Staessen JA, et al. Prevention of dementia in randomized, doubleblind, placebo controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 1998;352:1347 1351.
40. The Heart Outcomes Prevention Evaluations Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J of Med 2000;342:145 153.
41. Sacco, chapter 2, this volume.
42. Adams, chapter 4, this volume.
43. Sherman, chapter 6, this volume.
44. Joshipura, KJ, Ascherio A, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Hennekens CH, et al. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA 1999;282(13): 1233 1239.
P.13
45. Orgogozo, chapter 3, this volume.
46. Petitti, chapter 8, this volume.
47. Barnett, chapter 12, this volume.
48. Brown, chapter 13, this volume.
49. Bornstein, chapter 10, this volume.
50. Easton, chapter 11, this volume.
51. Bogousslavsky, chapter 9, this volume.
52. Bonita, chapter 14, this volume.
53. Gorelick, chapter 7, this volume.
54. Wolf PA. Prevention of stroke. Stroke 1998;352(suppl):15 18.
55. Feasby, chapter 16, this volume.
56. Donnan, chapter 15, this volume.
57. Hankey, chapter 17, this volume.
58. Taylor TN, David PH, Tomer JC, et al. Lifetime costs of stroke in the United States. Stroke 1996;27:1459 1466.
59. Smurawska LT, Alexandrov AV, Bladin CF, Norris JW. Cost of acute stroke care in Toronto, Canada. Stroke 1994;25:1628 1631.
60. Tran C, Nadareishvili Z, Smurawska L, Oh PIT, Norris JW. Decreasing costs of stroke hospitalization in Toronto. Stroke 1999;30:185 186.
61. McCormick J. Health promotion: the ethical dimension. Lancet 1994;344:390 391.
EAN: 2147483647
Pages: 23