The Esophagus
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume II > The Esophagus > Section XXIII - Benign Esophageal Disease > Chapter 140 - Inflammatory Diseases of the Esophagus
Chapter 140
Inflammatory Diseases of the Esophagus
Arvydas D. Vanagunas
Robert M. Craig
As pointed out by Baehr and McDonald (1994), esophageal infections are predominantly due to diminished host defense, the use of antibiotics, or a structural abnormality of the esophagus, such as a stricture. Infections with herpes simplex virus (HSV) and Candida species infection occur rarely in the immunocompetent individual. Acquired immunodeficiency syndrome (AIDS) and immunosuppression for transplantation and treatment of malignant disease are responsible for the increased importance of benign inflammatory diseases of the esophagus. Common and uncommon opportunistic infections of the esophagus in immunocompromised patients are outlined in Table 140-1. The aggressive use of protease inhibitors to suppress human immunodeficiency virus (HIV) replication and the routine use of antiviral prophylaxis in transplant recipients has actually resulted in an overall reduction in opportunistic infections of the esophagus during the past several years. Esophagitis related to gastroesophageal reflux is discussed in Chapter 143, and irradiation damage to the esophagus is considered in Chapters 109 and 110.
CANDIDA ESOPHAGITIS
With AIDS and immunosuppression for transplantation has come an increase in fungal and viral infections of the esophagus. The most common infection that occurs in patients with AIDS is Candida esophagitis, and its presence establishes the diagnosis of AIDS in patients who have a positive serum HIV antibody. Candida esophagitis can also occur in patients who are not immunosuppressed, but there are usually predisposing factors, as pointed out by Fazio (1983) and Kodsi (1976) and their colleagues. Kodsi and associates (1976) noted that most esophagitis with normal immune status occurs in elderly patients. Other factors associated with the development of Candida esophagitis in immunocompetent patients include malnutrition, alcoholism, lymphoproliferative disease, cancer, and head and neck irradiation. The use of antibiotics as well as inhaled and systemic corticosteroids can also allow the development of Candida esophagitis. Usually, the infection resolves spontaneously with discontinuation of the antibiotic or the corticosteroid. Rarely, diabetic patients develop Candida esophagitis spontaneously. Frick (1988) and Winston (1979) and their colleagues noted that whereas Candida esophagitis is quite common in patients with AIDS, it occurs less commonly in patients who undergo transplantation and immunosuppression, and the risk is less than 5% in transplant recipients given prophylactic antifungal therapy. Larner and Lendrum (1992) described a patient with esophageal candidiasis secondary to omeprazole use, presumably a result of diminished acid production in the stomach, which allows colonization in the stomach followed by esophageal infection.
Most immunocompetent patients with Candida esophagitis respond to the elimination of a predisposing antibiotic or corticosteroid. Agents such as clotrimazole and nystatin mouthwash are effective for oral candidiasis and as prophylaxis against esophageal infection but are generally less effective than oral azoles. Azoles (ketoconazole, fluconazole, and itraconazole) are the agents of first choice in treating Candida esophagitis, and Barbaro and colleagues (1996) demonstrated in a randomized controlled trial that fluconazole, 100 to 200 mg daily, is the superior agent in patients with AIDS. Ketoconazole is generally less effective than the other azoles, and Laine and colleagues (1992) suggested that the inefficacy of ketoconazole may be attributed to the necessity of an acid pH in the stomach for optimal ketoconazole absorption and the increased frequency of hypochlorhydria in patients with AIDS.
Often, the esophagitis is so severe that the entire esophagus is filled with a pseudomembranous exudative infiltrate. The infection can invade the esophageal wall and can produce systemic candidiasis. The patient should receive intravenous amphotericin B if there is not a rapid response to fluconazole. In general, the use of amphotericin B requires hospitalization. Once the patient has been shown to tolerate the medication well, he or she can be discharged to receive intermittent therapy intravenously at home. Amphotericin B is an effective agent but its severe side effect profile, including
P.2141
renal toxicity, is problematic. Low dose of intravenous amphotericin B (10 to 20 mg daily) for a total dose in the range of 100 to 200 mg may be effective in curing Candida esophagitis. Lipid-based formulations of amphotericin B are currently available that decrease the nephrotoxicity risk without compromising antifungal effects. Villanueva and colleagues (2001) described the effectiveness of a new echinocandin drug, caspofungin, as a less toxic alternative to amphotericin B in azole-resistant patients. This drug was approved in 2001 under the name Cancidas for patients who do not tolerate amphotericin B antifungal therapy.
Table 140-1. Opportunistic Pathogens of the Esophagus in Immunocompromised Patients | |
|---|---|
|
Diagnosis
Oral candidiasis (thrush) may be seen with Candida esophagitis, but its absence does not exclude infection of the esophagus. Diagnosis of Candida esophagitis is established by upper endoscopy with cytologic and tissue analysis (Fig. 140-1). Endoscopy is the diagnostic procedure of choice, although antifungal empiric therapy when thrush is present is an acceptable approach. Endoscopy should be considered if symptoms do not resolve rapidly. The endoscopic appearance may range from a few white plaques to confluent, thick, yellowish exudate coating the mucosa and encroaching on the esophageal lumen (Fig. 140-1). Brandt and colleagues (1993) described a technique involving the blind passage of a cytology brush transnasally. This technique is quite sensitive for the diagnosis of Candida but less reliable for HSV or cytomegalovirus (CMV) esophagitis. Patients with infectious esophagitis usually have odynophagia and often have dysphagia. Usually, esophageal candidiasis remains localized in the esophagus without systemic dissemination.
Chronic mucocutaneous candidiasis is a rare illness affecting the patient's T cells. The mouth, larynx, skin, and nails usually are involved with the infection. Often, esophagitis ensues as part of the generalized process.
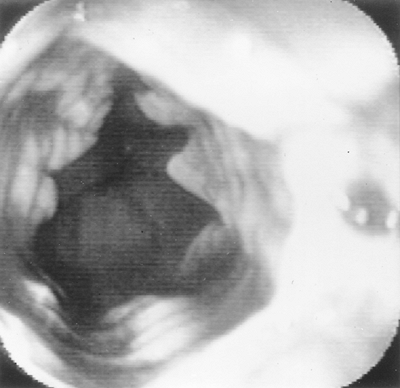 |
Fig. 140-1. Candida esophagitis in a patient with acquired immunodeficiency syndrome. |
Radiographic Features
Patients with Candida esophagitis have large intramural defects owing to the pseudomembranous process. In addition, intramural pseudodiverticulosis sometimes is evident (Fig. 140-2). Glick (1994) points out that Candida esophagitis can mimic viral esophagitis radiographically, thus necessitating endoscopic clarification.
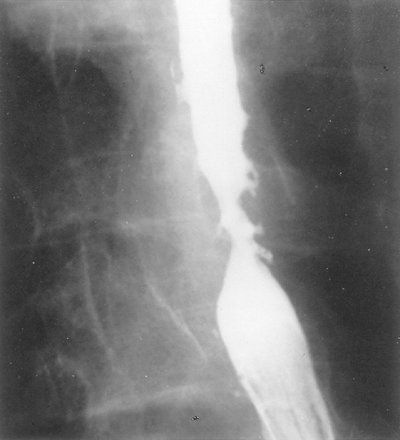 |
Fig. 140-2. Esophagram shows pseudodiverticulosis in a patient with Candida esophagitis. |
P.2142
OTHER FUNGAL DISEASES
Rarely, other fungal diseases can affect the esophagus, especially in patients with AIDS. Fungi typically spread to the esophagus by contiguous spread from lymph nodes in the mediastinum or by vascular dissemination, although primary esophageal infection can occur. The presentations mimic other opportunistic esophageal infections, with odynophagia as the primary symptom. Long fibrosing esophageal strictures or fistulae should raise clinical suspicion of an atypical fungal infection. Torulopsis glabrata esophagitis was described by Mukherjee (2000). Fortunately, it is a rare complication in AIDS because it is quite resistant to therapy. An unusual finding of actinomycosis of the esophagus with resulting esophagobronchial fistula was reported by Vinson and Sutherland (1926) in an immune-depressed patient. Aspergillosis, blastomycosis, mucormycosis, and histoplasmosis infections of the esophagus have been described.
VIRAL ESOPHAGITIS
As Momin and Chandrasekaar (1995) and Brodt (1997) and Hibberd (1995) and their associates observed, the incidence of viral esophagitis has generally been decreasing. As protease inhibitors have decreased viral replication in patients with AIDS and prophylaxis against HSV infection, the use of cytomegalovirus (CMV)-negative blood products and organs and preemptive ganciclovir have been become standard in transplant recipients. Viral infections of the esophagus are more common in bone marrow transplant recipients than in solid-organ transplant recipients because of the more profound immunosuppression. In general, the incidence of CMV and HSV esophagitis is similar after organ transplantation, and coinfections have been described. In AIDS patients, CMV esophagitis is much more common than HSV esophagitis. As noted by Ramanathan and associates (2000), herpetic ulcers of the esophagus can also occur in healthy individuals, usually as a consequence of primary infection or reactivation. Patients with HSV often have more odynophagia then those with Candida esophagitis. Instead of the pseudomembranous process seen on endoscopy, isolated, multiple, shallow ulcerations (Fig.140-3) or vesicles are present. Deep or longitudinal ulcers should suggest CMV esophagitis. Rattner and co workers (1985) reported that in rare circumstances, HSV esophagitis has presented with massive gastrointestinal hemorrhage.
Endoscopic sampling of the esophagus is required for diagnosis. HSV infection is limited to the squamous mucosa, and histology of the epithelial cells lining the margin of ulcers will reveal a fairly typical cytopathic effect. Cytologic specimens show the typical viral intranuclear eosinophilic inclusion bodies (Cowdry type A bodies). Wilcox and colleagues (1996) documented that 10 biopsy samples taken at the edge of esophageal ulcers may be needed to diagnose HSV esophagitis accurately. Genereau and colleagues (1996) reviewed a large experience with HSV esophagitis in AIDS and noted that infected patients were quite advanced and profoundly immunosuppressed, with average CD4 counts of 15 cells/mm3. The overwhelming majority of patients complained of odynophagia or chest pain, and extraesophageal herpes was found in only 38%. Mirra (1982) and McDonald (1985) and their associates observed that patients with AIDS frequently have two or more coexisting infections, which is distinctly unusual in other patient groups.
 |
Fig. 140-3. Superficial ulceration evident endoscopically in a patient with acquired human immunodeficiency syndrome. hsv, herpes simplex virus. |
HSV generally responds to acyclovir therapy (200 mg orally five times daily). Often, higher doses must be used in patients with AIDS, but the drug is generally quite well tolerated. Similar to Candida esophagitis, HSV esophagitis in the AIDS patient usually is not eradicated, but rather is only suppressed with acyclovir, and long-term prophylaxis may be needed in some patients. Valacyclovir, a prodrug of acyclovir, and famciclovir are also available and have some advantage in that they can be administered three times daily with equal efficacy to acyclovir. Unfortunately, some resistant forms of HSV have been described by Ehrlich and colleagues (1989) in patients with AIDS, making therapy more problematic.
In contrast to HSV, CMV esophagitis is very unusual in the normal host. The ulcerations are often larger than those seen with HSV (Fig. 140-4), commonly are variable in size, and often extend longitudinally down the esophagus. Patients with CMV esophagitis also have severe odynophagia and dysphagia. Diagnosis is established by cytologic or tissue sampling during upper endoscopy. Unlike HSV, which infects epithelial cells, the cytopathic effect of CMV is in
P.2143
endothelial and mesenchymal cells located in the base of the ulcer. The typical inclusions from CMV are quite large and typically intranuclear. The inclusions may be atypical, and cytologic diagnosis may need to be confirmed by immunohistochemical staining. Viral culture may increase the yield in diagnosis but can be falsely positive in some patients. CMV retinitis may accompany CMV esophagitis in AIDS patients, and ophthalmologic evaluation is appropriate.
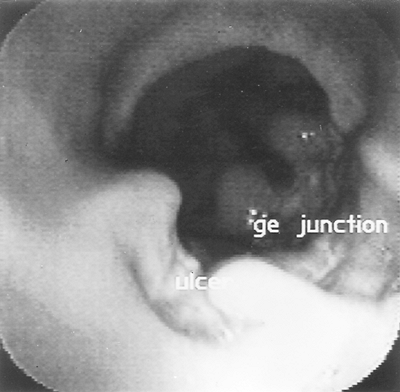 |
Fig. 140-4. Deep ulceration from cytomegalovirus in the distal esophagus of a patient with acquired immunodeficiency syndrome. ge, gastroesophageal. |
Ganciclovir is the treatment of choice and should be instituted, but its oral bioavailability is poor, and it needs to be administered intravenously. Wilcox and associates (1995) demonstrated ganciclovir to be effective in 77% of AIDS patients with CMV esophagitis. A 2 to 4 week treatment course is usually adequate in AIDS patients, but transplant recipients may need a prolonged course until the dosage of immunosuppressive agents can be reduced. Chronic use of ganciclovir may not be well tolerated, and bone marrow suppression is the main side effect. Foscarnet seems equivalent in efficacy to ganciclovir but is potentially toxic. Reversible renal failure and multiple electrolyte abnormalities, as well as a higher cost, make foscarnet a second-line therapy. Making therapy more difficult, resistance to foscarnet and ganciclovir has been reported in some patients with CMV infection. Cidofovir has had some efficacy in the treatment of CMV retinitis, but it use in CMV esophagitis is limited, and the agent is nephrotoxic. It should be noted that all currently used drugs are virostatic and not viricidal, and Wilcox and colleagues (1996) noted that the risk for relapse is 50% in patients with AIDS. Prophylactic ganciclovir has been effective in many high risk transplant recipients who are CMV seropositive or CMV seronegative and receive a CMV seropositive organ or blood product. Ganciclovir has been beneficial in the prevention of CMV retinitis in AIDS patients, but there is no experience in CMV esophagitis.
Human immunodeficiency virus (HIV) can probably invade the esophagus and produce esophagitis in its own right. Some patients negative for CMV, HSV, and Candida have been shown to have severe esophagitis with deep discrete esophageal ulcers. These idiopathic esophageal ulcers may be seen in up to 40% of patients with AIDS, typically in later stages of the disease when CD4 counts are below 100 cells/mm3. Biopsy of ulcerations seen in these patients has demonstrated the HIV glycoprotein 24, and in situ hybridization techniques have demonstrated HIV RNA. These ulcers respond to treatment with systemic corticosteroids (40 mg of prednisone daily, tapering by 10 mg every week over 4 weeks), endoscopic corticosteroid injection, and thalidomide.
Other viruses have been associated with esophageal infection. Human papillomavirus may infect the normal and immunocompromised host. Orlowska and associates (1994) described a series of patients with nodular squamous papillomas of the esophagus associated with human papillomavirus. Ebstein Barr viral esophagitis has been described by Kitchen and co workers (1990). Herpes zoster can sometimes affect the esophagus as part of a more generalized infection. Often, the esophagitis is mild; rarely does it proceed to a necrotizing esophagitis. Acyclovir is effective therapy.
A reasonable approach to the patient with AIDS and odynophagia is initially to inspect the mouth carefully. If evidence of candidal infection in the oral cavity or the pharynx is found, a trial of fluconazole therapy should be instituted. If the patient fails to respond to fluconazole, upper endoscopic examination of the esophagus should be performed. This examination should include cytologic sampling of the affected area, and biopsy samples of tissues from multiple areas within the esophagus. Again, AIDS patients often have two or three infections simultaneously; hence, multiple esophageal infections can coexist. In addition, sometimes an HSV esophagitis can resemble Candida esophagitis, with a large amount of exudate. Cultures of the esophagus are less useful because these organisms may be commensal and noninvasive. Evidence of tissue invasion should be sought in the cytologic analysis and the tissue sampling.
BACTERIAL INFECTIONS
Bacterial infections of the esophagus occur rarely. Mycobacterium tuberculosis has been associated with either primary or secondary tuberculosis. Patients usually present with an ulcerated lesion. Tuberculous esophagitis is typically due to extension from mediastinal disease or swallowed from a laryngeal focus. The recent upsurge in
P.2144
tuberculous (TB) infections in HIV infected individuals has increased the incidence of TB infections, especially Mycobacterium avium intracellulare. Primary TB can manifest with an exophytic process within the esophagus, suggesting a tumor, and it is one of the causes of pseudotumor. It may also cause obstructive esophageal stenosis and fistulization into the tracheobronchial tree. Generally, primary or secondary tuberculosis responds to usual antimycobacterial therapy, including isoniazid, rifampin, and ethambutol.
Polymicrobial infection of the esophagus with multiple gram-positive organisms, including Streptococcus viridans and Staphylococcus aureus, has been described. This usually occurs in patients with underlying hematologic malignancy and severe neutropenia and may result in a dramatic endoscopic picture of multiple dark esophageal pseudomembranes. It may be difficult to determine whether the infection is primary or a result of saprophytic bacterial colonization of the esophagus. Walsh and colleagues (1985) established strict diagnostic criteria for the diagnosis of bacterial esophagitis: bacterial aggregates with invasion into deeper layers without evidence of fungal, viral, or neoplastic disease or previous esophageal surgery.
EOSINOPHILIC ESOPHAGITIS
The esophagus is immunologically unique and does not contain eosinophils. Gastroesophageal reflux or allergic drug reactions may induce modest esophageal mucosal eosinophilia (less than 10 eosinophils per high power field). A unique entity of primary eosinophilic esophagitis is being diagnosed with increasing frequency. Eosinophilic esophagitis is distinct from eosinophilic gastroenteritis. Most patients are men who present with dysphagia, recurrent food impactions, or heartburn that is unresponsive to acid antisecretory therapy. The esophagus on endoscopy has a unique feature of multiple concentric rings (Fig. 140-5), primarily in the proximal esophagus. Histology reveals greater than 20 eosinophils per high-power field. Patients do not demonstrate peripheral eosinophilia. Mishra and associates (2001) suggested that the immunopathogenesis of primary eosinophilic esophagitis is mechanistically linked to asthma in that cytokines such as interleukin 5 and CD4 positive T cells are intimately involved in inducing mucosal damage. Elimination diets in atopic individuals and systemic corticosteroids have been effective treatments. Teitelbaum and colleagues (2002) demonstrated the beneficial therapeutic effects of using orally swallowed nebulized fluticasone propionate in these patients.
 |
Fig. 140-5. Multiple circumferential rings in the midesophagus in a patient with eosinophilic esophagitis. |
UNCOMMON INFECTIONS AND INFLAMMATORY DISORDERS
Protozoal diseases can present with primary esophageal involvement. Patients with AIDS and primary cryptosporidiosis or Pneumocystis carinii of the esophagus have been reported, although these presentations are rare.
Finally, the esophagus can be involved with systemic diseases, such as the primary dermatologic conditions epidermolysis bullosa, pemphigus, pemphigoid, and erythema multiforme. Often, the esophageal and pharyngeal involvement with erythema multiforme and epidermolysis bullosa is severe and is the most serious manifestation of the generalized process. Beh et's disease also rarely involves the esophagus. In patients who have undergone bone marrow transplantation, graft versus host disease (GVHD) can affect the esophagus along with the rest of the gastrointestinal tract. Under these circumstances, the esophagus is ulcerated in a way similar to other diseases that produce ulcerations.
Sarcoidosis rarely is associated with primary esophageal involvement, with an ulcerating or a nodular esophagitis. Esophageal involvement in Crohn's disease, although rare, has been well described. The real incidence of Crohn's disease of the esophagus is not known, but Tishler and Helman (1984) and Geboes and associates (1986) on retrospective analyses noted a 1% to 3% rate of esophageal involvement. Almost all cases of esophageal Crohn's disease demonstrate concomitant ileocolonic disease. The typical findings are of aphthous ulcers, at times coalescing into ulcerative esophagitis or long fibrotic strictures.
In allogenic bone marrow transplantation, graft versus host disease may occur as early as 1 to 2 months after transplantation and present with acute dysphagia and esophageal ulceration. Chronic GVHD (more than 100 days after transplantation) of the esophagus may also occur, causing esophageal fibrosis and stricturing. The diagnosis requires biopsy, and treatment involves immunosuppression with corticosteroids.
REFERENCES
Baehr PH, McDonald GB: Esophageal infections: risk factors, presentation, diagnosis, and treatment. Gastroenterology 106:509, 1994.
P.2145
Barbaro G, et al: Fluconazole versus itraconazole for Candida esophagitis in acquired immunodeficiency syndrome. Gastroenterology 111:1169, 1996.
Brandt LJ, et al: Use of a new cytology balloon for diagnosis of esophageal disease in acquired immunodeficiency syndrome. Gastrointest Endosc 4:559, 1993.
Brodt HR, et al: Changing incidence of AIDS-defining illnesses in the era to antiretroviral combination therapy. AIDS 11:1731, 1997.
Ehrlich KS, et al: Acyclovir resistant Herpes simplex virus infections in patients with the acquired immunodeficiency syndrome. N Engl J Med 320:293, 1989.
Fazio RA, Wickremesinghe PC, Arsura EL: Ketoconazole treatment of Candida esophagitis. A prospective study of 12 cases. Am J Gastroenterol 78:261, 1983.
Frick T, et al: Incidence and treatment of candida esophagitis in patients undergoing renal transplantation. Data from the Minnesota prospective randomized trial of cyclosporine versus antilymphocyte globulin-azathioprine. Am J Surg 155:311, 1988.
Geboes K, et al: Crohn's disease of the esophagus. J Clin Gastroenterol 8:31, 1986.
Genereau T, et al: Herpes simplex esophagitis in patients with AIDS: report of 34 cases. The Cooperative Study Group on Herpetic Esophagitis in HIV Infection. Clin Infect Dis 22:926, 1996.
Glick SN: Barium studies in patients with candida esophagitis. AJR Am J Roentgenol 163:349, 1994.
Hibberd PL, et al: Preemptive ganciclovir therapy to prevent cytomegalovirus disease in cytomegalovirus-positive transplant recipients. A randomized controlled trial. Ann Intern Med 123:18, 1995.
Kitchen VS, et al: Epstein-Barr virus associated oesophageal ulcers in AIDS. Gut 31:1223, 1990.
Kodsi BE, et al: Candida esophagitis. A prospective study of 27 cases. Gastroenterology 71:715, 1976.
Laine L, et al: Fluconazole compared with ketoconazole for the treatment of Candida esophagitis in AIDS. A randomized trial. Ann Intern Med 117:655, 1992.
Larner AJR, Lendrum R: Oesophageal candidiasis after omeprazole therapy. Gut 33:860, 1992.
McDonald GB, et al: Esophageal infections in immunocompromised patients after bone marrow transplantation. Gastroenterology 88:1111, 1985.
Mirra SS, et al: Concomitant herpes-monilial esophagitis: case report with ultrastructural study. Hum Pathol 13:760, 1982.
Mishra A, et al: An etiological role for aeroallergens and eosinophils in experimental esophagitis. J Clin Invest 107:83, 2001.
Momin F, Chandrasekaar PH: Antimicrobial prophylaxis in bone marrow transplantation. Ann Intern Med 123:205, 1995.
Mukherjee S: Torulopsis glabrata esophagitis. Am J Gastroenterol 95: 1106, 2000.
Orlowska J, et al: Squamous cell papillomas of the esophagus: report of 20 cases and literature review. Am J Gastroenterol 89:434, 1994.
Ramanathan J, et al. Herpes simplex esophagitis in the immunocompetent host: an overview. Am J Gastroenterol. 95:2171, 2000.
Rattner HM, Cooper DJ, Zaman MB: Severe bleeding from herpes esophagitis. Am J Gastroenterol 80:523, 1985.
Teitelbaum JE, et al: Eosinophilic esophagitis in children: Immunopathological analysis and response to fluticasone propionate. Gastroenterology 122:1216, 2002.
Tishler JMA, Helman CA: Crohn's disease of the esophagus. J Can Assoc Radiol 35:28, 1984.
Villanueva A, et al: A randomized double-blind study of caspofungin versus amphotericin for the treatment of Candidal esophagitis. Clin Infect Dis 33:1529, 2001.
Vinson P, Sutherland CG: Esophagobronchial fistula resulting from actinomycosis: report of a case. Radiology 6:63, 1926.
Walsh TJ, Belitsos NJ, Hamilton SR: Bacterial esophagitis in immunocompromised patients. Arch Intern Med 146:1345, 1985.
Wilcox CM, Straub RF, Schwartz DA: Cytomegalovirus esophagitis in AIDS; a prospective study of clinical response to ganciclovir therapy, relapse rate, and long-term outcome. Am J Med 98:169, 1995.
Wilcox CM, Straub RF, Schwartz DA: Prospective evaluation of biopsy number for the diagnosis of viral esophagitis in patients with HIV infection and esophageal ulcer. Gastrointest Endosc 44:587, 1996.
Winston DJ, et al: Infectious complications of human bone marrow transplantation. Medicine (Baltimore) 58:1, 1979.
Reading References
Baehr PH, McDonald GB: Esophageal infections: risk factors, presentation, diagnosis, and treatment. Gastroenterology 106:509, 1994.
Baden L, Maguire JH: Gastrointestinal infections in the immunocompromised host. Infect Dis Clin North Am 15:639, 2001.
Bini EJU, Micale PL, Weinshel EH: Natural history of HIV-associated esophageal disease in the era of protease inhibitor therapy. Dig Dis Sci 45:1301, 2000.
Blanshard C, et al: Treatment of AIDS-associated gastrointestinal cytomegalovirus infection with foscarnet and ganciclovir: a randomized comparison. J Infect Dis 172:622, 1995.
Furuta GT: Eosinophilic esophagitis: an emerging clinicopathologic entity. Curr Allergy Asthma Rep 2:67, 2002.
Goodman JL, et al: A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med 326:845, 1992.
Goodrich JM, et al: Early treatment with ganciclovir to prevent cytomegalovirus diseases after allogeneic bone marrow transplantation. N Engl J Med 325:601, 1991.
Kim J, Minamoto GY, Grieco MH: Nocardial infection as a complication of AIDS: report of six cases and review. Rev Infect Dis 13:624, 1991.
Laine L, Bonacini M: Esophageal disease in human immunodeficiency virus infection. Arch Intern Med 154:1577, 1994.
Monkemuller KE, Wilcox CM: Diagnosis and treatment of esophagitis in AIDS. Compr Ther 26:163, 2000.
Poles MA, et al: Actinomyces infection of a cytomegalovirus esophageal ulcer in two patients with acquired immunodeficiency syndrome. Am J Gastroenterol 89:1569, 1994.
Rothenberg, ME, et al: Pathogenesis and clinical features of eosinophilic esophagitis. J Allergy Clin Immunol 108:891, 2001.
Sullivan KM, et al: Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol 28:250, 1991.
Sutton FM, Graham DY, Goodgame RW: Infectious esophagitis. Gastrointest Endosc Clin N Am 4:713, 1994.
van Hogezand RA, et al: Proximal Crohn's disease: review of the clinicopathologic features and therapy. Inflamm Bowel Dis 7:328, 2001.
Villanueva JL, et al: Leishmania esophagitis in an AIDS patient: an unusual form of visceral leishmaniasis. Am J Gastroenterol 89:273, 1994.
EAN: 2147483647
Pages: 203