4 - Cellular and Molecular Biology of the Lung
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section I - Anatomy of the Chest Wall and Lungs > Chapter 6 - Lymphatics of the Lungs
function show_scrollbar() {}
Chapter 6
Lymphatics of the Lungs
Thomas W. Shields
The lung has an extensive network of lymphatic vessels that are situated in the loose connective tissue beneath the visceral pleura, in the connective tissue in the interlobular septa, and in the peribronchial vascular sheaths.
In the pulmonary parenchyma, the lymphatic capillaries form extensive plexuses within the connective tissue sheaths that surround the airways and the blood vessels. The origin of these channels is believed to be at the level of the terminal and respiratory bronchioles, and they do not extend into the interalveolar septa according to Okada and colleagues (1979) as well as Leak and Jamuar (1983). The channels begin as blind-end tubes and saccules. As these channels extend proximally toward the hilar area associated with the enlarging airways and blood vessels, they have been designated as juxtaalveolar lymphatics by Lauweryns (1971) and Leak (1980). These networks drain into larger collecting vessels with thicker walls and contain monocuspid, conical valves that direct the flow of lymph toward the hilar area in a centripetal direction. The physiologic mechanisms controlling this lymphatic flow are little understood.
Lymphatic channels that also drain the periphery of the lung lobules run in the lobular septa along with the pulmonary veins. With the occurrence of extraalveolar interstitial edema, some of these may be recognized as Kerley's B lines radiographically, as noted by Steiner (1973).
The extensive subpleural network drains primarily by the channels in the interlobular septa to the hilar area, but direct connections to the mediastinum have been recorded by Rouvi re (1932), Borrie (1952, 1965), and Riquet (1993), as well as he and his associates (1989). The channels in the lobular septa have multiple connections with the channels in the bronchovascular sheaths. These connecting channels are frequently up to 4 cm in length and lie midway between the hilus and the periphery of the lung. When distended, they are recognized as Kerley's A lines.
Collections of lymphatic cells may be seen along the course of the lymphatic channels and within the bronchial structures, but recognizable intrapulmonary lymph nodes are identified only infrequently in contrast to the common presence of bronchopulmonary lymph nodes.
PULMONARY LYMPH NODES
The pulmonary lymph nodes are divided into the intrapulmonary and bronchopulmonary nodes. The latter are subdivided into the lobar and hilar lymph nodes.
Intrapulmonary Lymph Nodes
The intrapulmonary lymph nodes, when present, are located most often just beneath the visceral pleura. Rarely, a peripheral lymph node may present as a solitary peripheral nodule, as reported by Greenberg (1961), Houk and Osborne (1965), and Ehrenstein (1970). In addition to these infrequent, radiographically identified intrapulmonary lymph nodes, Trapnell (1963) reported the identification of other intrapulmonary lymph nodes in the substance of the lung by a combined technique of injection of the subpleural lymphatics and subsequent radiologic evaluation of autopsy lung specimens. Intrapulmonary nodes were observed in 5 of 28 injected specimens, an incidence of 18%. The actual location of these nodes was undocumented. However, Trapnell (1964) was able to identify peripheral lymph nodes radiologically in only 1 of 92 inflated lungs obtained at autopsy, an incidence of just over 1%. Despite this early study, Dail (1995) reported that intraparenchymal lymph nodes could be identified in about 10% of resected lobes when they were sought, and Kradin and associates (1985) had previously recorded that all such nodes were anthracotic and were not encapsulated. In Kradin and associates' (1985) report, the identified lymph nodes were solitary in 65% of the cases and multiple in the remainder; in 22%, two lymph nodes were found, and in 12% there were three or more identified. The multiple nodes may be in the same lobe in 40% of the cases in which they are found, but in 60%, the lymph nodes are located bilaterally. Most are in the size range of 0.5 to 1.0 cm; occasionally, nodes as large as 1.5 cm are identified. Only rarely is a larger one present. All these intraparenchymal lymph nodes are within 1 cm of the pleura, adjacent to it or in an interlobular septum. With rare exception,
P.75
these lymph nodes are found only in adults and are identified more commonly in individuals older than 50 years of age.
With high-resolution computed tomography (HRCT), some of the small lesions identified in patients with multiple metastases to the lung are proved subsequently to be small peripheral lymph nodes. Ohbuchi and associates (1999) reported the video-assisted thoracic surgery (VATS) excision of 10 intrapulmonary lymph nodes suspected as malignant lesions, either primary or secondary, over a 1-year period. The average size of the pulmonary nodes was 5.9 mm, and all were located in the lower lobes: 7 on the left and 3 on the right. Nagahiro and colleagues (2001) resected 13 intrapulmonary lymph nodes in 9 patients over a 2-year period that had been identified on chest radiographs in 3 and on HRCT scan in the other 6. The characteristics of these nodes on HRCT were that the border was sharp, the shape was ovoid, all were located in the lower portion of the lungs in a subpleural location, and the interval density was high and homogeneous. No borders were irregular, although short spicules could be present, and none contained cavities or calcifications. As the aforementioned authors, as well as Ohbuchi (1999) and Yokomise (1998) and their associates, have pointed out, these lesions must be differentiated from small malignant nodules.
Bronchopulmonary Lymph Nodes
Nagaishi (1972) noted that segmental lymph nodes are related to the bifurcation of the segmental bronchi or may lie in the bifurcation of the branches of the associated pulmonary arteries and may extend out to the fifth- or sixth-order segmental bronchi.
Table 6-1. Distribution of Bronchopulmonary Lymph Nodes | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
The lobar bronchopulmonary lymph nodes are found at the angles formed by the origins of the various lobar bronchi and lie in close association with the bronchus or the adjacent pulmonary vessels. The hilar lymph nodes are situated alongside the lower portions of the main bronchi or the respective pulmonary artery and the pulmonary veins lying within the visceral pleural reflections.
The number of bronchopulmonary lymph nodes is variable. These lymph nodes more frequently are present in greater numbers in children than in adults. Borrie (1965) suggests that the maximal development of these nodes is reached by the end of the first decade of life, and then these lymph nodes gradually atrophy and disappear during adulthood. The presence of pulmonary infection or malignancy greatly affects the number of bronchopulmonary lymph nodes that may be identified.
In a study of 200 operative specimens of lungs containing lung cancer, Borrie (1965) identified lymph nodes in 13 locations in the right lung and 15 locations in the left lung that are now considered bronchopulmonary lymph nodes. These sites are listed in Table 6-1 and are shown schematically in Figures 6-1 and 6-2. The incidence of bronchopulmonary lymph nodes present in each location is listed in Table 6-2.
Hilar Lymph Nodes
The hilar lymph nodes are contiguous with the lobar lymph nodes distally as well as with the mediastinal lymph nodes proximally. The hilar lymph nodes lying superior to the right main-stem bronchus classically have been considered to extend up to the inferior border of the azygos vein, but this concept was questioned by Tisi and associates (1983) in their recommendations about the location of the
P.76
various mediastinal lymph node stations. The lymph nodes medial to the right main-stem bronchus may be considered as hilar nodes when located away from the tracheal carina and within the visceral pleural sheath, but as they become subjacent to this structure, they are best termed subcarinal lymph nodes and thus belong to the lymph nodes of the mediastinal compartment.
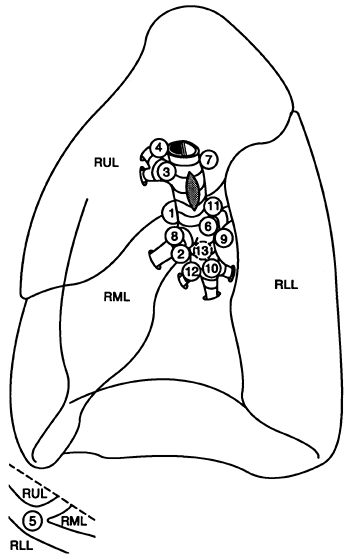 |
Fig. 6-1. Bronchopulmonary lymph nodes of the right lung. Drawing of the medial aspect of the right lung shows the 13 most common locations of lymph nodes identified in 93 specimens by Borrie. The sites are numbered in the order of decreasing frequency in which lymph nodes were identified in each respective site (see Tables 6-1 and 6-2). Inset at bottom shows the lateral view of the junction of the oblique and transverse fissures. At this site, lymph nodes are lateral to the origins of the middle and lower lobe branches of the right pulmonary artery. RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe. Redrawn from Borrie J. Lung Cancer. Surgery and Survival. New York: Appleton-Century-Crofts, 1965. |
On the left side, the anatomic separation between the hilar and the mediastinal lymph nodes proximally is at an imaginary plane connecting the lateral surfaces of the ascending and descending portions of the thoracic aorta. The left hilar nodes are located medial, anterior, posterior, and lateral to the left main-stem bronchus in order of decreasing frequency in number. The hilar nodes located anteriorly are found in relationship to the left main-stem pulmonary artery. Proximally, these latter nodes are contiguous with the subaortic lymph nodes of the mediastinum, including the lymph node located at the site of the ligament arteriosum, the so-called Bartello's node. The nodes on the medial surface of the
P.77
main-stem bronchus, as their position advances upward, become subcarinal in location.
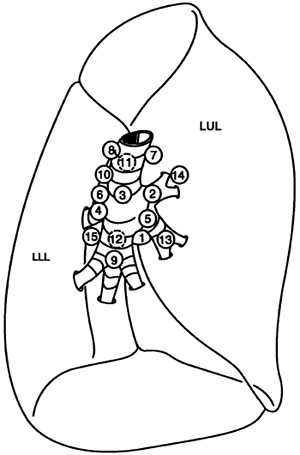 |
Fig. 6-2. Bronchopulmonary lymph nodes of the left lung. Drawing of the medial aspect of the left lung shows the 15 most common locations of bronchopulmonary lymph nodes identified in 101 specimens by Borrie. The sites are numbered in the order of decreasing frequency in which lymph nodes were identified in each respective site (see Tables 6-1 and 6-2). LLL, left lower lobe; LUL, left upper lobe. Redrawn from Borrie J. Lung Cancer. Surgery and Survival. New York: Appleton-Century-Crofts, 1965. |
Table 6-2. Bronchopulmonary Nodes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Lobar Lymph Nodes
The two most common locations in which lobar lymph nodes are found in the right lung are between the upper lobe bronchus and middle lobe bronchus: the area that Borrie (1952) termed the right bronchial sump [the superior interlobar lymph node of Rouvi re (1932)] and the region just below the middle lobe bronchus adjacent to the lower lobe bronchus [the inferior interlobar lymph node of Rouvi re (1932)]. In the left lung, the most common location is at the angle of the left upper lobe bronchus and the lower lobe bronchus. Borrie (1952) designated this area as the left lymphatic sump, and the nodes found here correspond to the left interlobar node of Rouvi re (1932).
Right Lymphatic Sump
The lymph nodes in the lymphatic sump of the right lung lie in relationship to the bronchus intermedius (Fig. 6-3). According to Nohl-Oser (1989), a constant lymph node is found at the upper posterior end of the major fissure in the angle between the right upper lobe bronchus and the bronchus intermedius. A branch of the bronchial artery coursing over the posterior aspect of the right main bronchus leads to it (Fig. 6-4). Another lymph node is found on the interlobar portion of the pulmonary artery where this vessel gives off the posterior ascending segmental branch to the posterior segment of the upper lobe and the superior segmental artery to the superior segment of the lower lobe. Inferiorly, this lymph node is contiguous with a constant node lying above the superior segmental bronchus of the lower lobe. Other lymph nodes of the sump are found at the base of the major fissure lying closely alongside the interlobar portion of the pulmonary artery or in the bifurcations of its branches. Frequently, lymph nodes are identified more anteriorly, lying among the upper lobe branches of the superior pulmonary vein.
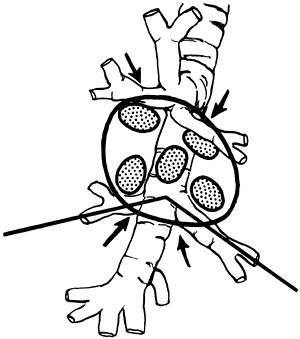 |
Fig. 6-3. The collection of lymph nodes lying within the right lymphatic sump. The line drawn through the axis of the superior segmental bronchus of the lower lobe and the middle lobe bronchus represents the level below which nodes are not involved by malignant disease in the upper lobe. Arrows indicate the tendency of lymphatic drainage. From Nohl-Oser HC. Lymphatics of the lung. In: Shields TW, ed. General Thoracic Surgery. 3rd Ed. Philadelphia: Lea&Febiger, 1989. With permission. |
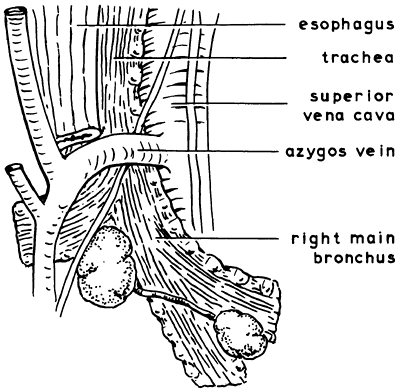 |
Fig. 6-4. The posterior aspect of the right main bronchus, as seen when the lung is pulled forward during dissection. The subcarinal lymph nodes and the node below the right upper lobe bronchus are seen. A constant bronchial artery leading to the latter node is shown. From Nohl-Oser HC. Lymphatics of the lung. In: Shields TW, ed. General Thoracic Surgery. 3rd Ed. Philadelphia: Lea&Febiger, 1989. With permission. |
Other Interlobar Lymph Nodes of the Right Lung
In addition to the sump nodes, the other interlobar lymph nodes can be grouped, according to Borrie (1965), into those of the upper, middle, and lower lobes. The lymph nodes of the right upper lobe are located above the upper lobe bronchus, medial to it, and just behind it. Those lying above the bronchus merge with the hilar nodes of the distal portion of the right main-stem bronchus. The lymph nodes of the middle lobe, in addition to the subjacent node below the middle lobe bronchus [the inferior interlobar node of Rouvi re (1932)] are located lateral to the middle lobe bronchus near its confluence with the lower lobe bronchus, as well as medial to it. The right lower lobe lymph nodes, in addition to the aforementioned superior and inferior sump nodes, are
P.78
found medial to the superior segmental bronchus or between it and the basal bronchi. Lymph nodes are present also in relationship to the basal stem of the lower lobe bronchus and lie on its medial aspect, lateral to it, and between the anterior and medial basal bronchi.
Left Lymphatic Sump
The collection of lymph nodes described by Nohl (1956, 1962) and Nohl-Oser (1972) as composing the left lymphatic sump lies between the upper and lower lobes in the main fissure (Fig. 6-5). A constant node is present in the bifurcation between the upper and lower lobe bronchi in close relationship to the origin of the lingular (inferior division) branch of the upper lobe (Fig. 6-6). A small bronchial arterial branch passing across the membranous portion of the left main bronchus leads to it. Other lymph nodes are found lying on the interlobar portion of the left pulmonary artery in the fissure and in the angles formed by its branches. Another constant node is described, which is found above and posterior to the left interlobar bronchus. This node is contiguous with a node lying in the angle formed by the interlobar bronchus and the takeoff of the bronchus to the superior segment of the lower lobe.
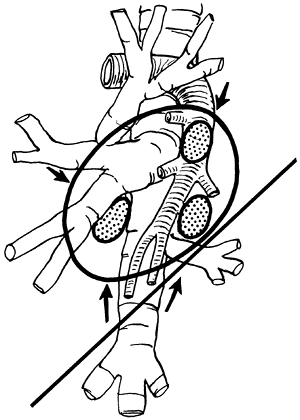 |
Fig. 6-5. The left lymphatic sump (see text), found by opening the main fissure. The straight line, drawn through the superior (apical) segmental bronchus of the left lower lobe, represents the level below which lymphatic drainage from the upper lobe does not occur. Arrows indicate tendency of lymphatic drainage. From Nohl-Oser HC. Lymphatics of the lung. In: Shields TW, ed. General Thoracic Surgery. 3rd Ed. Philadelphia: Lea&Febiger, 1989. With permission. |
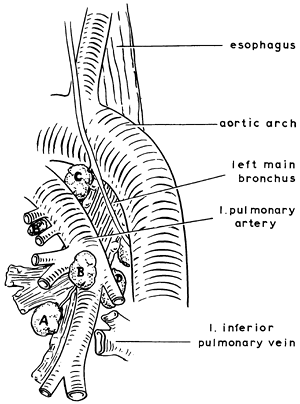 |
Fig. 6-6. The lymph nodes most frequently seen on opening the main fissure of the left lung. A constant node (A) lies in the angle between the upper and lower lobe bronchi, with a bronchial artery leading to it. Other lymph nodes (B and B') are found on the main pulmonary artery and in the angles of the branches. The constant node (C) behind and above the pulmonary artery, before it enters the fissure, is shown. Another node (D) above the inferior pulmonary vein is seen with its connections to the inferior tracheobronchial nodes higher up. From Nohl-Oser HC. Lymphatics of the lung. In: Shields TW, ed. General Thoracic Surgery. 3rd Ed. Philadelphia: Lea&Febiger, 1989. With permission. |
Other Interlobar Lymph Nodes of the Left Lung
In addition to the left lymphatic sump nodes, Borrie (1965) noted that lymph nodes of the left upper lobe are present medial, posterior, and lateral to the upper lobe bronchus. Lymph nodes are present also between the segmental divisions of this bronchus.
The lymph nodes of the left lower lobe are located more commonly in the vicinity of the superior segmental bronchus of the lobe. They are found medial, above, and inferior to it, between it and the basal bronchi. The other lobar nodes of the lower lobe are found medial or lateral to the basilar stem of the lower lobe bronchus.
LYMPHATIC DRAINAGE OF THE LOBES OF THE LUNG TO THE BRONCHOPULMONARY LYMPH NODES
The lymphatic drainage of the lobes of the lungs is primarily to the bronchopulmonary nodes, although direct lymphatic
P.79
drainage to the mediastinal lymph nodes was described by Rouvi re (1932), Borrie (1952), Cordier (1958), and Riquet (1989) and their colleagues, as well as by the latter author in 1993. This direct drainage is discussed subsequently.
The right upper lobe lymphatic drainage, as deduced from the study of Borrie (1956), is commonly to one of the superior interlobar lymph nodes (the sump nodes) on the lateral aspect of the bronchus intermedius, to the nodes above the right upper lobe bronchus and to those medial to it. Subsequent drainage is proximal to the azygos or subcarinal lymph nodes. Distal drainage has not been described as occurring to any lymph nodes below the lower level of the right lymphatic sump.
The middle lobe lymphatics drain to lymph nodes of the superior sump region, although drainage to the inferior sump node also occurs. Okada and associates (1979) also recorded drainage directly to the subcarinal nodes. Later studies by Watanabe (1991) and Asamura (1999) and their colleagues, as well as by Naruke (2000), have confirmed this direct drainage to the subcarinal area and also to the midline pretracheal mediastinal nodal area. Drainage from the right lower lobe is to the inferior interlobar node and to the superior sump nodes, primarily those lying on the medial surface of the bronchus intermedius. Proximal drainage may also occur directly as well to the subcarinal nodes as recorded by Okada and colleagues (1979) and subsequently by the aforementioned authors noted in the discussion of the drainage of the middle lobe.
Drainage of the left upper lobe from all segments may occur to the left sump nodes. Nodes around the upper lobe bronchus and the left main-stem bronchus also receive drainage from this lobe. Direct drainage to subaortic mediastinal nodes may occur from the superior division of the left upper lobe, whereas direct drainage to the mediastinum from the inferior division (lingula), when it occurs, is commonly to the subcarinal mediastinal nodes as recorded by Asamura and associates (1996, 1999). Lymphatic drainage of the lower lobe is to the subjacent peribronchial nodes and to the interlobar sump nodes. From here, drainage is proximal to the hilar or mediastinal lymph node groups, or both.
Lymphatic drainage from the middle and right lower lobes and the left lower lobe also occurs to the nodes in the respective pulmonary ligament. These lymph nodes are considered to be mediastinal lymph nodes. The incidence of nodes identified in Borrie's work (1965) was 12% in the right pulmonary ligament and 47% in the left.
MEDIASTINAL LYMPH NODES
The mediastinal lymph nodes that are important in the lymphatic drainage of the lungs can be divided into four distinct but interconnected groups: the anterior (prevascular) lymph nodes in the anterior mediastinal compartment, the tracheobronchial lymph nodes, the paratracheal lymph nodes, and the posterior lymph nodes in the posterior area of the visceral compartment of the mediastinum.
Anterior Mediastinal Lymph Nodes
The anterior mediastinal lymph nodes are in the prevascular compartment of the mediastinum and override the upper portions of the pericardium and great vessels as these extend upward. On the right side, the nodes lie parallel and anterior to the right phrenic nerve. They extend upward to and along the superior vena cava (these may be located between the vein and the ascending aortic arch) to the area beneath the right innominate vein. On the left, they are in close proximity to the origin of the pulmonary artery and the ligamentum arteriosum. They extend upward near the left phrenic nerve to lymph nodes lying along the inferior border of the left innominate vein in the region where it is joined by the left superior intercostal vein.
Tracheobronchial Lymph Nodes
The tracheobronchial lymph nodes lie in three groups around the bifurcation of the trachea. The right and left superior tracheobronchial nodes are located in the obtuse angles between the trachea and the corresponding main-stem bronchus. These nodes lie outside of the pretracheal fascia. The lymph nodes of the right superior tracheobronchial group are medial to (beneath) the arch of the azygos vein and above the right pulmonary artery. These nodes are contiguous with the right superior hilar nodes distally and the right paratracheal nodes proximally. On the left side, the superior tracheobronchial nodes lie deep within the concavity of the aortic arch. Some are closely related to the left recurrent laryngeal nerve; others are situated slightly more anteriorly and are contiguous with the node at the ligamentum arteriosum and the root of the left pulmonary artery. Their association with these nodes constitutes the link between the nodes in the visceral compartment and those in the anterior mediastinal lymph node group. Last, the paraaortic nodes lying anterior and lateral to the ascending aorta and the arch are also in the anterior compartment.
The inferior tracheobronchial nodes, more comm only referred to as the subcarinal nodes, lie in the angle of the bifurcation of the trachea (Fig. 6-7). Although these nodes, in contrast to the superior tracheobronchial groups, lie within the pretracheal fascial envelope, they lie outside the relatively dense bronchopericardial membrane. These nodes are contiguous with the hilar nodes on the medial aspect of both the right and left main-stem bronchi. Some of the subcarinal lymph nodes lie more posteriorly in relationship to the tracheal bifurcation and are on the anterior surface of the esophagus and are thus connected with the posterior group of lymph nodes. In addition, Brock and Whytehead (1955)
P.80
described a low anterior tracheal group lying in front of the lower end of the trachea, which constitutes a bridge between the right superior tracheobronchial lymph nodes and the subcarinal, inferior tracheobronchial lymph nodes.
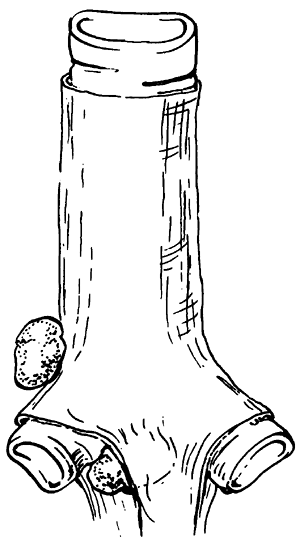 |
Fig. 6-7. The location of the inferior tracheobronchial nodes within the pretracheal fascial envelope and the superior tracheobronchial nodes outside this fascial layer. Redrawn from Sarrazin R, Voog R. La Mediastinoscopie. Paris: Masson, 1968. |
Paratracheal Lymph Nodes
The paratracheal lymph nodes are situated on the right and left sides of the trachea above the respective superior tracheobronchial nodes and extend upward along the trachea. The right paratracheal lymph nodes lie anterolaterally to the trachea and to the right of the innominate artery. Inferiorly, these nodes are overlapped by the superior vena cava. More superiorly, these nodes lie behind and above the innominate artery to the right of the midline of the trachea and extend to the inlet of the chest. Inferiorly, the left paratracheal nodes lie above the tracheobronchial angle to the left of the midline of the trachea behind the aortic arch. More superiorly, they are situated above the arch but behind the great vessels and extend to the inlet of the chest. The left paratracheal lymph nodes are generally smaller in size and number compared with the right paratracheal lymph nodes.
Posterior Mediastinal Lymph Nodes
The posterior mediastinal lymph nodes may be separated into two groups: the paraesophageal nodes and those located in either pulmonary ligament. These posterior nodes are identified less commonly in the superior portion than in the inferior portion of the mediastinum. A paraesophageal node occasionally is found retrotracheally at the level of the arch of the azygos vein. The paraesophageal nodes as a group are more numerous in the inferior portion of the mediastinum and are found more frequently on the left than on the right side. The inferiorly located nodes have connections with the paraaortic nodes beneath the diaphragm. In the pulmonary ligament on either side, usually two or more small lymph nodes may be present. A relatively constant node, and usually the largest, lies in close proximity to the inferior border of the inferior pulmonary vein and is often termed the sentinel node of the pulmonary ligament.
Mediastinal Lymph Node Maps
Naruke and associates (1978) suggested the use of an anatomic map with the aforementioned conventional lymph node stations numbered so that the various lymph node stations involved by tumor could be uniformly recorded in patients with lung cancer (Fig. 6-8). This mapping scheme is
P.81
used by most Japanese surgeons and has been used with minor modifications by the Sloan-Kettering Memorial group and others in North America. The American Joint Committee for Cancer Staging and End Results Reporting (AJC) published a similar map in its 1983 fascicle. The lymph node stations are defined in Table 6-3. The American Thoracic Society (ATS) in a report by Tisi and colleagues (1983), however, noted what they believed to be deficiencies in the commonly accepted specific anatomic definition of each nodal station when determined by mediastinoscopy, mediastinotomy, and computed tomography (CT) examinations of the chest. Although some of the points were minor, a major area of conflict was the recommendation that the hilar stations, the right and left stations 10 of the Naruke and AJC maps, be deleted because of the ambiguity of the radiologic definition of these areas. It was suggested that these areas be redesignated as peribronchial on the left and tracheobronchial on the right and be assigned to the mediastinal compartments, both stations being outside of the pleural reflection. It should be noted that recently Asamura and co-workers (2000) have presented data that support the concept that the station 10 nodes rightly belong in the hilar compartment rather than being included in the mediastinal compartment. The ATS suggested the anatomic stations as listed in Table 6-4 and located as represented in Fig. 6-9. The ATS map has been adopted by many investigators in North America. The validity of one schema over the other is moot. In reviewing data presented in the literature, however, cognizance of the differences in the method of recording the data must be borne in mind for their proper interpretation.
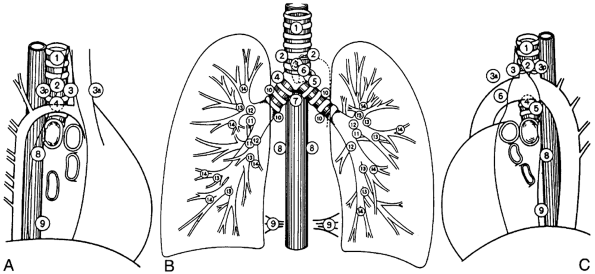 |
Fig. 6-8. Modified lymph node map of Naruke and the American Joint Committee (see Table 6-3 for definitions). A. Right lateral view. B. Frontal view. C. Left lateral view. From Naruke T, et al: Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J Thorac Cardiovasc Surg 76:832, 1978. With permission. |
Table 6-3. American Joint Committee for Cancer Staging and End Results Reporting Classification of Regional Lymph Nodes | ||||
|---|---|---|---|---|
|
In an attempt to resolve the confusion created by the two aforementioned classifications and maps of the lymph node stations, a committee representing both the American Committee on Cancer and the Union International Contre le Cancer decided to adopt a modified version of both the AJC
P.82
and ATS classifications and lymph node maps. The adapted classification and map were published by Mountain and Dresler (1997) (Table 6-5). Graphic representations of the Mountain and Dresler (1997) map that is now in use by most American investigators are shown in Fig. 6-10. Note that in this schema, station 3 lymph nodes (anterior midline paratracheal nodes superior to the tracheal bifurcation and extending upward to the inferior border of station 1) are believed by Naruke (2000) and associates (1999), as well as Asamura (1999) and Watanabe (1991) and their colleagues, among others, to be an important individual mediastinal nodal station and have been placed in the broad category of station 4 nodes. However, station 3 nodes remain in the classification used by most Japanese surgeons. As an aside, station 3a consists of lymph nodes in the anterior mediastinal compartment located on the anterior surface of the superior vena cava at the level of the anterior wall of the ascending aorta; station 3p nodes are the central retrotracheal lymph nodes located behind the trachea extending from the caudal border of station 1 inferior to the apex of the tracheal bifurcation. The recommended schema essentially resolves the problems between the two previous schemata by using anatomic landmarks that identify all lymph node stations within the mediastinal pleural reflection as N2 nodes and anatomic landmarks that identify all lymph node stations distal to the pleural reflections and within the visceral pleural envelope as N1 nodes. However, Asamura and associates (2000) believe that the pleural reflection is an inappropriate boundary to separate N1 from N2 lymph nodes because some lymph nodes around the main bronchus could be considered as N2 lymph nodes. These authors have shown that such nodes should still be considered as N1 nodes in station 10 and that the relationship of the node to the main bronchus is the important feature. This conclusion is agreed to by Riquet and colleagues (2001), although these authors still believe that the number of lymphatic chains involved is more important than the location of the lymph nodes. This, and the problem of station 3 lymph nodes, remains to be resolved.
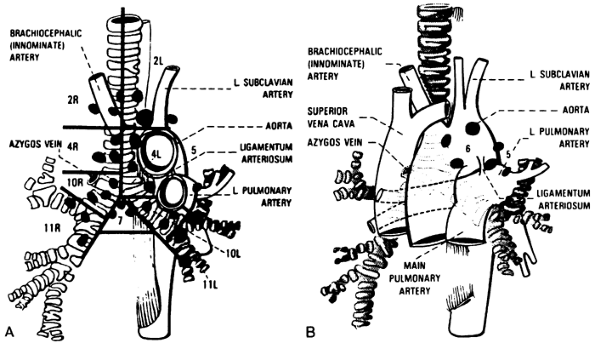 |
Fig. 6-9. A. American Thoracic Society map of regional pulmonary nodes (see Table 6-4 for definitions). B. American Thoracic Society map of regional nodes in stations 5 and 6. From Tisi GM, et al: Clinical staging of primary lung cancer. Am Rev Respir Dis 127:659, 1983. With permission. |
Table 6-4. Proposed Definitions of Regional Nodal Stations for Prethoracotomy Staging | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
To compound these aforementioned issues further, there is now a German lymph node map according to the Deutsche Gesellschaft fur Thorax (1988), and the new first English edition of the Japanese Lung Cancer Society classification (2000) has been printed that contains their nodal map published in 1987. Resolution of the many problems remains to be seen. Parenthetically, it is important to realize that not only is there still a question as to which nodal map is most appropriate, but also the anatomical interpretation of any given map will vary among two or more surgeons, as pointed out by Watanabe and colleagues (2002) at the Royal Brompton Hospital in London, as well as among two or more institutions. This problem will be difficult to solve even if a single map becomes standard throughout the surgical community. What is seen lies in the eyes of the beholder despite the optimistic view expressed by Naruke (2002) in the discussion of the aforementioned report.
Number and Size of Lymph Nodes in the Various Mediastinal Locations
The first major report of the number of lymph nodes in the mediastinum was published by Beck and Beattie (1958). In cleared specimens of the mediastinum from five autopsies, they reported an average of three nodes in the anterior mediastinum and an average of 50 in the tracheobronchial area of the mediastinum. Of the latter, an average of 16 nodes were located in the peribronchial region, 11 in the subcarinal, and 23 in the paratracheal regions. These data were essentially nonspecific anatomically, as were the data recorded by Genereux and Howie (1984). These authors, however, were among the first investigators, including Baron (1982), Osborne (1982), Ekholm (1980), and Moak (1982) and their colleagues, to record the size of normal mediastinal lymph
P.83
P.84
nodes as identified by CT scanning. Eighty-nine to 95% of normal lymph nodes identified in these studies were smaller than 11 mm. Genereux and Howie's data (1984) were essentially similar to those of the other early investigators.
Table 6-5. Lymph Node Map Definitions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
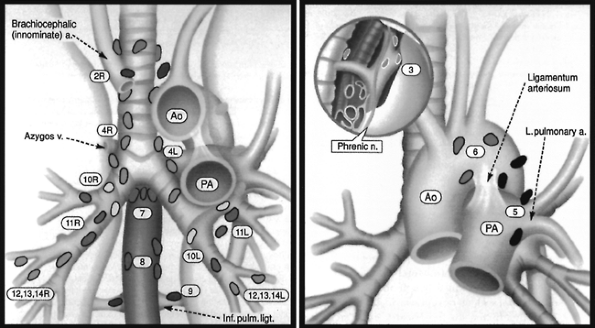 |
Fig. 6-10. Regional lymph node stations: (1) Superior mediastinal nodes are stations 1, 2, 3, and 4; (2) aortic nodes are stations 5 and 6; and (3) inferior mediastinal nodes are stations 7, 8, and 9. Intrapleural nodes are stations 10, 11, 12, 13, and 14. (See Table 6-4 for definitions.) Ao, aorta; PA, pulmonary artery. Adapted from Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 111:1718, 1997. |
Table 6-6. Normal Lymph Nodes in the Mediastinum as Identified on Computed Tomography Examination in 56 Patients | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
Glazer and associates (1985) not only reported the size of normal nodes but also correlated the number of lymph nodes usually identified by CT and their size in each of the superior mediastinal stations and the subcarinal region as described by the ATS map (see Fig. 6-9A and B). The data were generated by a retrospective review of 56 CT scans of patients without primary inflammatory pulmonary disease or primary lung neoplasm. The largest normal mediastinal nodes were found in the subcarinal and right tracheobronchial regions, and as a rule, the nodes were larger on the right side than on the left side. The maximum number of nodes and the size above which a node was considered enlarged are listed in Table 6-6 for each of the mediastinal stations. From these data, it was suggested that 10 mm be considered the upper limit for the short axis of normal mediastinal lymph nodes. An anatomic study by Kiyono and associates (1988) in which the mediastinal lymph nodes were dissected in 40 cadavers produced similar results (Table 6-7). These authors suggested the normal size for the diameter of the short axis of the lymph nodes in stations 2, 5, 6, 8, 9, and 10L to be 8 mm; for stations 4 and 10R to be 10 mm; and for station 7 to be 12 mm.
Table 6-7. Number of Mediastinal Lymph Nodes from Dissection of the Mediastinum of 40 Cadavers | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 6-8. Number of Nodes Identified in the Inferior Compartment of the Mediastinum a by Transesophageal Ultrasound (TEUS) versus Computed Tomography (CT) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Relative to the number of lymph nodes, it may be noted that CT examination may fail to identify all the nodes present, particularly in the subaortic and subcarinal regions, and does not demonstrate nodes present in either of the pulmonary ligaments or those in the inferior paraesophageal area. The use of esophageal endoscopic ultrasound examination, which is particularly sensitive for the detection of mediastinal nodes in these latter areas, was reported by Kondo and colleagues (1990). These investigators, although the patients studied had carcinoma of the lung, were able to identify lymph nodes in these latter areas, but the data are incomplete as to the actual number of normal nodes identified in the various regions (Table 6-8). Again, however, most lymph nodes considered normal were less than 10 mm (97%) in their short axis.
LYMPHATIC DRAINAGE OF THE LUNGS TO THE MEDIASTINAL LYMPH NODES
The lymphatic drainage of the lungs to the mediastinal lymph nodes has been studied extensively. Various techniques of injection of dyes into the lymphatic channels of lungs from autopsy specimens of stillborn infants and adults without pulmonary disease have been used in the studies of Rouvi re (1932), Cordier and associates (1958), Riquet and colleagues (1989)
P.85
, Caplan (1990), and Riquet (1993). Borrie (1952, 1965) and Nohl (1962) studied the drainage patterns by dissection of the operative specimens from lungs of cancer patients, as have many investigators subsequently, including Naruke (1978), Martini (1983), Libshitz (1986), Watanabe (1990, 1991), Ishida (1990), and Asamura (1999) and their associates, as well as additional publications by Naruke in 1993 and 2000. In addition to these studies, Nohl-Oser (1972) and Greschuchna and Maassen (1973) published their findings from the evaluation of the superior mediastinum by mediastinoscopy in patients with lung cancer. Also, in living patients without known pulmonary disease, the lymphatic drainage of the lungs was studied by the technique of lymphoscintigraphy using antimony sulfide colloid or rhenium colloid labeled with technetium 99m (99mTc) injected into the various bronchopulmonary segments through the fiberoptic bronchoscope by Hata and associates (1981).
Although the terminology for the lung segments and the mediastinal lymph nodes, as well as their locations, varied considerably in these multiple studies, relatively consistent drainage patterns for each lung and its respective lobes and segments can be identified.
The patterns of normal lymphatic drainage from the lungs to the mediastinal lymph nodes are relatively consistent despite minor variations suggested by different workers, which may be the result of the methods of investigation used and the selection of the subjects studied. The dynamic study by lymphoscintigraphy in normal healthy subjects as reported by Hata and associates (1981) and summarized in 1990 appears to be a highly satisfactory schema to recommend. The patterns of drainage from the right and left lung segments are seen in Fig. 6-11. A summary of the findings is quoted from Hata and colleagues (1990).
Right Lung
The lymphatic drainage from the apical and posterior segments of the right upper lobe flows through the hilar nodes into the right superior tracheobronchial nodes and further into the paratracheal nodes and up into the neck in the right scalene nodes through ipsilateral upper paratracheal nodes. About one half of the lymph from the anterior segment of the upper lobe flows through the same route. The other one half flows into the subcarinal nodes or into the right anterior mediastinal nodes. Lymph that passes through the subcarinal nodes may flow further into the right scalene nodes through the pretracheal and ipsilateral paratracheal nodes, and a small amount of lymph is observed to flow into the left paratracheal nodes. Lymph that goes to the right anterior mediastinal nodes flows along the left brachiocephalic vein into the left anterior mediastinal nodes and into the left scalene nodes.
The routes of lymphatic drainage from the bronchi of the middle lobe and the superior segment of the right lower lobe are similar. Most of the lymph from these segmental bronchi flows into the subcarinal or right superior tracheobronchial nodes and then to the right upper paratracheal nodes. Some of the lymph from the bronchi of the middle lobe also flows into the subcarinal, anterior paratracheal, and left paratracheal nodes, or into the right anterior mediastinal nodes, as mentioned for lymphatic drainage from the anterior segment of the right upper lobe.
A dominant flow of the lymphatic drainage occurs from the basal segments of the right lower lobe into the subcarinal nodes through the bronchopulmonary nodes. The lymph then flows into the ipsilateral lower and upper paratracheal nodes and further into the right scalene nodes.
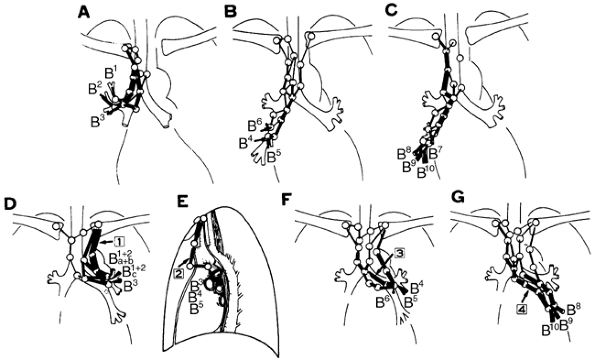 |
Fig. 6-11. Standard patterns of lymphatic drainage of the lungs. A. From segments of the right upper lobe. B. From segments of the middle lobe and superior segment of the right lower lobe. C. From basal segments of the right lower lobe. D. Route 1 from the left lung. E. Route 2 from the left lung. F. Route 3 from the left lung. G. Route 4 from the left lung. See text for explanation. From Hata E, et al: Rationale for extended lymphadenectomy for lung cancer. Theor Surg 5: 191, 1990. With permission. |
P.86
Left Lung
Four major routes are described by Hata and associates (1990) for the lymphatic drainage from the segmental bronchi of the left lung. The first passes through the subaortic nodes. This route divides into two pathways. One runs along the left vagus nerve to the left scalene nodes, and the other runs along the left recurrent laryngeal nerve to the highest left mediastinal nodes. The second route runs through the paraaortic nodes upward along the left phrenic nerve through the anterior mediastinal nodes to the left scalene nodes. The third route runs along the left main bronchus to the left superior tracheobronchial nodes and the paratracheal nodes. From the left tracheobronchial nodes, this route divides into two branches. One extends to the right side of the mediastinum through the right upper pretracheal node, and the other runs upward along the left side of the trachea to the highest left mediastinal nodes. The fourth route runs under the left main bronchus to the subcarinal nodes. After passing the subcarinal nodes, this route extends to the right superior tracheobronchial nodes or through the lower pretracheal node to the right upper paratracheal nodes. Some branches extend upward along the left side of the trachea to the highest left mediastinal nodes.
As a consequence, the lymphatic drainage from the left lung is variable; however, the major routes of lymphatic drainage from each segment are as follows. The most important route of lymphatic drainage from the apicoposterior segmental bronchus of the upper lobe is the first route. Although the second route is the most common for lymphatic drainage from the anterior and lingular segments of the upper lobe, the other routes are used as well for lymphatic drainage from these segments. Lymph from the superior segmental bronchus of the lower lobe drains commonly along the first, third, and fourth routes. The most important route of drainage from the basal segmental bronchi of the lower lobe is the fourth route.
Lymphatic Chains in the Mediastinum
Of special interest is the report by Riquet (1993) of the postmortem injection studies of the subpleural lymphatics of a total of 343 pulmonary segments of the right lung and 344 segments of the left lung. As a result of his investigation, Riquet identified eight drainage lymphatic chains in the superior mediastinum: two major and two minor on the right side and two major and two minor on the left side. In the inferior mediastinum, one major group of nodes was identified as well as two minor chains (the right and left pulmonary ligament chains) and a very infrequently identified group of juxtaesophageal lymph nodes.
The first of the major chains on the right side of the superior mediastinum is the right pretracheal or paratracheal chain (RPT) from the anterior aspect of the tracheal carina to the right supraclavicular fossa. Three groups of nodes were identified, those of station 3, R4, and L4. The second major chain is the tracheoesophageal chain (TE) situated behind the trachea. The minor chains are the right phrenic chain (RP) and the chain of the arch of the azygos vein (AZM); this latter chain empties directly into the thoracic duct, and only infrequently are lymph nodes identified along this chain. In the left superior mediastinum, the preaortic carotid chain (AO) most often begins as a large node situated at the level of the ligamentum arteriosus (station 5) and passes from below upward behind the phrenic nerve anteriorly and in front of the vagus nerve posteriorly to its apex in the neck. The second major chain, the left superior bronchial and left recurrent chain (LSB), corresponds to the tracheoesophageal chain on the right. Two minor chains are the left phrenic chain (LP) and chain of the aortic arch (Azao).
In the inferior mediastinum, a major group of intertracheobronchial lymph nodes (ITB) is arranged in three clusters: one midline subcarinal group (station 7) flanked bilaterally by right and left clusters of nodes located below the respective bronchus. On either side, the chains of the pulmonary ligaments (PL) derive most of their drainage from the ipsilateral basilar segments; subsequent drainage is primarily to the intertracheobronchial nodes, but in 40% of the specimens, some of the flow is either directly to the thoracic duct or indirectly to the duct through an intraabdominal lymph node (20%). The percentages of crossover from an ipsilateral lung to a contralateral mediastinal chain are shown in Table 6-9. The final chain, the juxtaesophageal (JE), drains very little of the lungs. Direct flow from the lungs initially to the mediastinum rather than by a bronchopulmonary route was observed in just over 28% of the injections from each lung. This phenomenon is discussed subsequently in this chapter under Significance of the Lymphatic Drainage Patterns.
Riquet and associates (2002) have continued their investigations of the lymphatic drainage from the various lymph node groups and organs in the thorax. In a portion of this report, they have described the direct tributaries between various nodal groups of the lung and the thoracic duct. These tributaries may be discussed briefly because these lymphatic connections may well be one of the routes of egress of cancer cells directly into the bloodstream. Lymphatic vessels from the lung connected directly with the thoracic duct in 115 of 390 adult cadavers of a total of 530 subjects in whom dye injections were attempted. These connections originated from mediastinal lymph node groups in all (112 specimens) but those specimens (3) in which the connections occurred from the right (inferior) pulmonary ligament. The sites of the direct connections between the tributaries and the thoracic duct were (a) in the mediastinum in 73 specimens, (b) at the level of the arch of the thoracic duct in 40 specimens, and (c) at the origin of the duct in 2 specimens. From the right paratracheal nodes (station 4R), the tributaries traveled along the arch of the azygos vein on the right of the trachea and esophagus. On the left from station 4L, the lymphatic tributaries drained directly into the thoracic duct within the superior mediastinum in 34 specimens and to the arch of the duct in 28. From station 5, again the tributaries drained either directly
P.87
into the duct traveling along the arch of the aorta (4 specimens) or into the arch of the duct by the anterior mediastinal lymph node chain in 11. From station 7, a tributary in 18 specimens joined the duct either on the right or the left of the esophagus. This new information (Table 6-10) is supplemental to the normally described drainage patterns of the various lobes of the lungs.
Table 6-9. Percentage of Drainage from the Segments of the Right and Left Lungs to the Mediastinal Chains | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Significance of the Lymphatic Drainage Patterns
The routes described by Hata and associates (1990) mainly agree with the patterns described by Rouvi re (1932) and Nohl (1956). In addition, other significant features of the lymphatic drainage from the various lobes of the lungs to the mediastinal lymph nodes, as well as reemphasis of some of the aforementioned observations, must be pointed out. The drainage from the right lung is essentially unilateral, and crossover to lymph nodes in the contralateral mediastinum is infrequent. Hata and colleagues (1981) noted drainage from the right upper lobe into the left paratracheal nodes and sequentially from the right prevascular nodes into the left prevascular (anterior) nodes. Similar pathways were observed infrequently from the middle lobe and superior segment of the lower lobe. Drainage from the basilar segments of the right lower lobe rarely progressed to the left side of the mediastinum, although Riquet and colleagues (1989) recorded the presence of one direct drainage channel from the right basal segments to the left pulmonary ligament. In patients with known carcinoma of the lung studied by prethoracotomy mediastinoscopy, contralateral drainage from the right lung to the mediastinum was likewise observed with minimal frequency. Nohl-Oser (1972) and Greschuchna and Maassen (1973) reported that the incidence of contralateral metastases from tumors of the right upper lobe with metastatic mediastinal node disease were 5% and 9%, respectively. From tumors of the right lower lobe with associated metastatic mediastinal node disease, the incidences of contralateral disease were 7% and 5%, respectively. When the total number of tumors of the right lung (less than one half with metastatic mediastinal node
P.88
involvement) is used as the denominator in the series reported by Nohl-Oser (1972), the incidences of crossover from the right upper and right lower lobes are reduced to 2% and 3%, respectively.
Table 6-10. Lymphatic Vessels from the Lungs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In contrast, contralateral mediastinal drainage from the left lung is relatively common, occurring most frequently through the subcarinal nodes, as initially pointed out by Rouvi re (1932) and reconfirmed by all of the subsequent studies. Occasionally, crossover occurs by means of the lower pretracheal node in drainage from the left lower lobe. Again, Riquet and associates (1989) identified a direct channel from the left to a right paratracheal node. These workers also described direct channels from the left lower lobe to the opposite side of the lower portion of the inferior mediastinum. In the mediastinoscopy data of Nohl-Oser (1972) and Greschuchna and Maassen (1973), contralateral involvement from tumors of the left upper lobe to the right side of the mediastinum in patients with mediastinal node involvement was 22% and 21%, respectively. From the left lower lobe, the figures were 40% and 33%, respectively. Again, to put these data into perspective, 28% of the patients in Nohl-Oser's (1972) study had metastatic mediastinal nodal involvement from tumors of the left lung, so that the 22% and 40% incidences represent actual 6% and 11% incidences of crossover from the left upper and lower lobes to the right side of the mediastinum. These percentages are in agreement with the findings of Hata and associates (1990), who found 7% and 11% incidences, respectively, in patients who had undergone bilateral mediastinal node dissection for left lung tumors.
Drainage from the lower lobes on either side to the ipsilateral superior mediastinal lymph nodes is common.
Drainage to the inferior mediastinum, to the subcarinal lymph nodes, from the right upper lobe does occur. This finding was first observed by Rouvi re (1932), and although discounted by Nohl (1962) and Nohl-Oser (1972), it has been amply reconfirmed by the studies of Borrie (1965) and Hata (1981, 1990), Riquet (1989), Watanabe (1990), and Asamura (1999) and their associates. Watanabe and colleagues (1990) reported a 13% incidence of subcarinal lymph node involvement in 45 patients with right upper lobe tumors. Libshitz and coinvestigators reported a similar 14% incidence of such involvement.
Drainage of the superior division of the left upper lobe to the subcarinal area is unusual but, as noted by Hata (1981) and Asamura (1999) and their colleagues, commonly occurs from the inferior (lingular) division of that lobe.
Direct lymphatic channels from either lung drain to the mediastinal lymph nodes, bypassing the bronchopulmonary nodes in a significant number of lungs. This phenomenon was observed previously and has been described as skip metastases in lung cancer patients by Martini and Flehinger (1987) and Libshitz (1986) and Ishida (1990) and their associates, among others, including Riquet (1993) and Asamura and associates (1996). Skip metastases from the right upper lobe were seen in the superior tracheobronchial nodes most frequently; a few occurred in the paratracheal node group and infrequently to the subcarinal lymph nodes. Right lower lobe tumors exhibited skip metastases to the subcarinal nodes and to the pulmonary ligament nodes. On the left side, upper lobe lesions tended to show skip metastasis to the aortic window and subcarinal areas; the lower lobe lesion showed a similar pattern as seen on the right; that is, the subcarinal and pulmonary ligament nodes. Riquet (1993) and colleagues (1989) used injection studies of the subpleural lymphatics of adult lungs obtained at autopsy to identify direct lymphatic channels running from the subpleural plexus of the lobar segments to the various mediastinal lymph nodes without passing through the bronchopulmonary nodes. Most of these channels were superficial, but a few penetrated the lung substance. On occasion, these direct but separate channels coexisted with other channels draining into the bronchopulmonary lymph nodes. These direct channels were observed in 28.5% of the segments injected in the right lung and 28.8% of the segments in the left lung in Riquet's 1993 report. In all other specimens, the dye followed the classic patterns and filled the respective bronchopulmonary lymph nodes. A summary of the study by Riquet and colleagues (1989) is found in Table 6-11. Drainage to the ipsilateral pulmonary ligament nodes from the right and left lower lobes and subsequently to the inferior paraesophageal lymph nodes was pointed out by Borrie (1952) and others of the aforementioned investigators.
Drainage from the superior mediastinum continues to progress cephalad to the scalene lymph nodes in the neck, more often involving the right than the left scalene area.
Finally, lymphatic drainage from the lower regions of the mediastinum may progress caudad to the paraaortic lymph nodes below the diaphragm. Riquet (1993) and associates (1988, 1990) described a direct channel from the basal segments of both lungs to juxtaceliac nodes. This drainage pathway also had been noted previously by Meyer (1958).
All of the aforementioned points must be remembered in the overall consideration of the lymphatic drainage from the lungs. The clinical relevance of the lymphatic drainage and the various lymph node groups are discussed in the respective
P.89
chapters relating to infections and tumors of the lungs.
Table 6-11. Direct Pathways to Mediastinal Lymph Nodes from the Lungs | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||
REFERENCES
Asamura H, et al: Lymph node involvement, recurrence, and prognosis in resected small, peripheral, non small cell lung carcinomas: are these carcinomas candidates for video-assisted lobectomy? J Thorac Cardiovasc Surg 11: 1123, 1996.
Asamura H, et al: Lobe-specific extent of systematic lymph node dissection for non small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg 117:1102, 1999.
Asamura H, et al: Where is the boundary between N1 and N2 stations in lung cancer? Ann Thorac Surg 70: 1839, 2000.
Baron RL, et al: Computed tomography in the preoperative evaluation of bronchogenic carcinoma. Radiology 145:727, 1982.
Beck E, Beattie EJ: The lymph nodes in the mediastinum. J Int Coll Surg 29:247, 1958.
Borrie J: Primary carcinoma of the bronchus: prognosis following surgical resection (Hunterian Lecture). Ann R Coll Surg Engl 10:165, 1952.
Borrie J: Lung Cancer: Surgery and Survival. New York: Appleton-Century-Crofts, 1965.
Brock R, Whytehead LL: Radical pneumonectomy for bronchial carcinoma. Br J Surg 43:8, 1955.
Caplan I: Anatomical review of the lymph nodes of the human mediastinum. Surg Radiol Anat 12: 9, 1990.
Cordier G, et al: Les lymphatiques des bronches et des segments pulmonaires. Bronches 8:8, 1958.
Dail DH: Uncommon tumors. In Dail DH, Hammer SP, Colby TV (eds): Pulmonary Pathology Tumors. New York: Springer-Verlag, 1995.
Deutsche Gesellschaft fur Thorax, Herz und Gefasschirurgie/Pneumologie 1988.
Ehrenstein FL: Pulmonary lymph node presenting as an enlarging coin lesion. Am Rev Respir Dis 101: 595, 1970.
Ekholm S, et al: Computed tomography in preoperative staging of bronchogenic carcinoma. J Comput Assist Tomogr 4:763, 1980.
Genereux GP, Howie JL: Normal mediastinal lymph node size and number: CT and anatomic study. AJR Am J Roentgenol 142:1095, 1984.
Glazer GM, et al: Normal mediastinal lymph nodes: number and size according to American Thoracic Society mapping. AJR Am J Roentgenol 144:261, 1985.
Greenberg HB: Benign subpleural lymph node appearing as a pulmonary coin lesion. Radiology 77:97, 1961.
Greschuchna D, Maassen W: Die lymphogenen Absiedlungswege des Bronchialkarzinoms. Stuttgart: Georg Thieme, 1973.
Hata E, Troidl H, Hasegawa T: In vivo Untersuchungen der Lymphdrainage des Bronchialsystems beim Menchen mit des Lympho-Szintigraphie: Eine neue diagnostische Technik. In Hamelmann H, Troidl H (eds): Behandlung des Bronchialkarzinoms. Stuttgart: Georg Thieme, 1981.
Hata E, et al: Rationale for extended lymphadenectomy for lung cancer. Theor Surg 5:19, 1990.
Houk ZN, Osborne DP: Subvisceral pleural lymph node presenting as an expanding intrapulmonary nodule. Am Rev Respir Dis 91: 596, 1965.
Ishida T, et al: Strategy for lymphadenectomy in lung cancer three centimeters or less in diameter. Ann Thorac Surg 50:708, 1990.
The Japan Lung Cancer Society. Classification of lung cancer, the first English edition. Tokyo: Kanehara&Co Ltd, 2000.
Kiyono K, et al: The number and size of normal mediastinal lymph nodes: a postmortem study. AJR Am J Roentgenol 150:771, 1988.
Kondo D, et al: Endoscopic ultrasound examination for mediastinal lymph node metastases of lung cancer. Chest 98:586, 1990.
Kradin RI, Spirn PW, Mark EJ: Intrapulmonary lymph nodes. Clinical, radiologic and pathologic features. Chest 87:662, 1985.
Lauweryns JM: The blood and lymphatic microcirculation of the lung. In Sommers SC (ed): Pathology Annual. New York: Appleton-Century-Crofts, 1971, p. 365.
Leak LV: Lymphatic removal of fluids and particles in the mammalian lung. Environ Health Perspect 35:55, 1980.
Leak LV, Jamuar MP: Ultrastructure of pulmonary lymphatic vessels. Am Rev Respir Dis 128:S59, 1983.
Libshitz HI, McKenna RJ, Mountain CF: Patterns of mediastinal metastases in bronchogenic carcinoma. Chest 90:229, 1986.
Martini N, Flehinger BJ: The role of surgery in N2 lung cancer. Surg Clin North Am 67:1037, 1987.
Martini N, et al: Results of resection in non oat cell carcinoma of the lung with mediastinal lymph node metastases. Ann Surg 198:386, 1983.
Manual for Staging Cancer. Chicago: American Joint Committee for Cancer Staging and End-results Reporting, 1983.
Meyer KK: Direct lymphatic connections from the lower lobes of the lung to the abdomen. J Thorac Surg 35:726, 1958.
Moak GD, et al: Computed tomography vs. standard radiology in the evaluation of mediastinal adenopathy. Chest 82:69, 1982.
Mountain CF, Dresler CM: Regional lymph node classification for lung cancer staging. Chest 111:1718, 1997.
Nagahiro I, et al: Intrapulmonary lymph nodes enlarged after lobectomy for lung cancer. Ann Thorac Surg 72:2115, 2001.
Nagaishi C: Functional Anatomy and Histology of the Lung. Baltimore: University Park Press, 1972.
Naruke T: Significance of lymph node metastases in lung cancer. Semin Thorac Cardiovasc Surg 5:210, 1993.
Naruke T: Mediastinal lymph node dissection: lymph node involvement, incidence and sentinel lymph node for systematic nodal dissection. InShields TW, LoCicero J III, Ponn RB (eds): General Thoracic Surgery. 5th ed. Philadelphia: Lippincott Williams&Wilkins, 2000, p. 1354.
Naruke T: Discussion of Watanabe S, Ladas G, Goldstraw P: Inter-observer variability in systematic nodal dissection: comparison of European and Japanese nodal designation. Ann Thorac Surg 72:245, 2002.
Naruke T, Suemasu K, Ishikawa S: Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J Thorac Cardiovasc Surg 76:832, 1978.
Naruke T, et al: Lymph node sampling in lung cancer: how should it be done? Eur J Cardiothorac Surg 16(Suppl 1):S17, 1999.
Nohl HC: An investigation into the lymphatic and vascular spread of carcinoma of the bronchus. Thorax 11:172, 1956.
Nohl HC: The Spread of Carcinoma of the Bronchus. London: Lloyd-Luke Ltd, 1962.
Nohl-Oser HC: An investigation of the anatomy of the lymphatic drainage of the lungs as shown by the lymphatic spread of bronchial carcinoma. Ann R Coll Surg Engl 51:157, 1972.
Nohl-Oser HC: Lymphatics of the lung. In Shields TW (ed): General Thoracic Surgery. 3rd ed. Philadelphia: Lea&Febiger, 1989.
Ohbuchi T, et al: Clinical features of intrapulmonary lymph node and the role of VATS biopsy. J Jpn Assoc Chest Surg 13:122, 1999.
Okada Y, Ito M, Nagaishi C: Anatomical study of the pulmonary lymphatics. Lymphology 12:118, 1979.
Osborne DR, et al: Comparison of plain radiography, conventional tomography and computed tomography in detecting intrathoracic lymph node metastases from lung carcinoma. Radiology 142:157, 1982.
Riquet M: Anatomic basis of lymphatic spread from carcinoma of the lung to the mediastinum: surgical and prognostic implications. Surg Radiol Anat 15:271, 1993.
Riquet M, Hidden G, Debesse B: Abdominal nodal connexions of the lymphatics of the lung. Surg Radiol Anat 10:251, 1988.
Riquet M, Hidden G, Debesse B: Direct lymphatic drainage of lung segments to the mediastinal nodes. An anatomic study of 260 adults. J Thorac Cardiovasc Surg 97:623, 1989.
Riquet M, Le Pimpec-Barthes F, Lang-Lazdunski L: Boundary between N1 and N2 stations in lung cancer: back to the future of anatomy [Letter to the editor]. Ann Thorac Surg 72:1439, 2001.
Riquet M, et al: Direct metastasis to abdominal lymph nodes in bronchogenic carcinoma [Letter to the editor]. J Thorac Cardiovasc Surg 100:153, 1990.
Riquet M, et al: Thoracic duct tributaries from intrathoracic organs. Ann Thorac Surg 73:892, 2002.
Rouvi re H. Anatomie des Lymphatics de le Homme. Paris: Masson et Cie, 1932.
Steiner RE. The radiology of the pulmonary circulation. In Shanks CS, Kerley P (eds): A Textbook of X-Ray Diagnosis. London: HK Lewis, 1973, p. 121.
Tisi GM, et al: Clinical staging of primary lung cancer. Am Rev Respir Dis 127:659, 1983.
Trapnell DH: The peripheral lymphatics of the lung. Br J Radiol 36:660, 1963.
Trapnell DH: Recognition and incidence of intrapulmonary lymph nodes. Thorax 19:44, 1964.
P.90
Watanabe S, Ladas G, Goldstraw P: Inter-observer variability in systematic nodal dissection: comparison of European and Japanese nodal designation. Ann Thorac Surg 73:245, 2002.
Watanabe Y, et al: Mediastinal spread of metastatic lymph nodes in bronchogenic carcinoma. Mediastinal nodal metastases in lung cancer. Chest 97:1059, 1990.
Watanabe Y, et al: Mediastinal nodal involvement and the prognosis of non small cell lung cancer. Chest 100:422, 1991.
Yokomise H, et al: Importance of intrapulmonary lymph nodes in the differential diagnosis of small pulmonary nodular shadows. Chest 113:703, 1998.
EAN: 2147483647
Pages: 203