37 - Anti-Infective Chemotherapeutic Antibiotic Agents
Tierney, Lawrence M., McPhee, Stephen J., Papadakis, Maxine A.
Current Medical Diagnosis & Treatment, 45th Edition
document.getElementById('working').innerHTML = ''; function hide_scrollbar() { var e = document.body; e.style.scrollbarBaseColor = '#fff'; e.style.scrollbarArrowColor = '#fff'; e.style.scrollbarDarkShadowColor = '#fff'; e.style.scrollbarShadowColor = '#fff'; } function show_scrollbar() { var e = document.body; e.style.scrollbarBaseColor = '#ccc'; e.style.scrollbarArrowColor = '#000'; e.style.scrollbarDarkShadowColor = '#000'; e.style.scrollbarShadowColor = '#666'; } function toggle_CA(e) { var src; src = window.parent.getSrc(e); if (src.nextSibling.style.display == 'block') { src.nextSibling.style.display='none'; src.innerHTML='View Answer'; } else { src.nextSibling.style.display='block'; src.innerHTML='Hide Answer'; } } function resolve_link(e,setid,locator,dbid,toan) { e.href = "ovidweb.cgi?S=IDNJHKKKJGEPJK00D;FTS+Link+Set+Ref=" + setid + "|" + locator + "|" + dbid + "|" + toan; return true; }
40
Cancer
Hope S. Rugo MD
See http://www.cmdtlinks.com
This chapter mainly covers the clinical aspects of cancer: prevention, diagnosis, primary treatment, management of complications, and paraneoplastic syndromes. Further information may be obtained by calling the National Cancer Institute (NCI) Cancer Information Service at 1-800-4CANCER or accessing NCI's comprehensive cancer information database “Physician Data Query” (PDQ) via the Internet at http://www.cancer.gov/cancerinformation. PDQ is also available on CD-ROM. The CANCERLIT feature of Medline (PubMed) is a familiar resource for articles about cancer that can be accessed by author or by subject words. A series of oncology practice guidelines compiled by a panel of United States experts and encompassing diagnosis and treatment of a wide variety of cancers as well as pain management is now available free of charge at the National Comprehensive Cancer Network Web site (http://www.nccn.org) and is updated yearly. This site also provides a stepwise guide to diagnosis and to treatment options for patients as well as links to a variety of useful sites, including the American Cancer Society.
Many new Web sites are now available for both clinician and patient use, and are regularly updated with new drug approvals and prevention and treatment guidelines. Information includes statistics, treatment, and clinical trial information. Web sites can be found by searching for the words “cancer” or “oncology.” The American Society of Clinical Oncology has an information Web site for patients and their families (http://www.PeopleLivingWithCancer.org) as well as patient guides on subjects such as follow-up care for breast and colorectal cancers, understanding tumor markers, treatment of nausea and vomiting, and advanced lung cancer. Two Web sites provide updated data as well as review articles on advances in oncology; these sites allow the user to search for specific areas of interest as well: PeerView Press (info@peerviewpress.com) and Medscape Hematology-Oncology (http://www.medscape.com/hematology-oncologyhome).
INCIDENCE & ETIOLOGY
Cancer is the second most common cause of death in the United States. The American Cancer Society estimates that almost 1.4 million new cases of invasive cancer will be diagnosed in the year 2005, with over 570,000 deaths. Slightly less than one out of every two men and slightly more than one out of every three women in the United States will develop some type of invasive cancer during their lifetime. Based on the SEER 2004 database, the lifetime probability of developing cancer is about 46% for men and 38% for women and varies by race, and age. Table 40-1 summarizes current U.S. incidence and mortality figures for the ten leading types of cancer. Women have an approximately 1:7 lifetime chance of developing breast cancer, and men have an approximately 1:6 chance of developing prostate cancer. Cancers of the lung, prostate, and breast and of the colon and rectum account for about 55% of all new cancer diagnoses and for over 50% of cancer deaths in the United States. Lung cancer is the leading cause of cancer death in the United States, accounting for almost one-third of deaths in men and women. Table 40-2 summarizes the lifetime risk of being diagnosed with or dying from the leading causes of cancer as well as from all types of cancer. Rates are age adjusted to the year 2000 standard million population based on the 2000 census data. The incidence of and the mortality from cancer decreased an average of 1% per year from 1992 to 2001 in the United States, with variations by gender and race. This now sustained decline is attributed to changes in lifestyle as well as improved prevention, early detection, and treatment. However, the single most important risk factor for developing cancer is age. About 76% of cancers are diagnosed in persons aged 75 years or older. As the United States population increases in numbers and grows older, it is estimated that the number of cancer cases will double, by the year 2050, from 1.3 million cases per year to 2.6 million cases per year.
Cancer incidence and mortality vary significantly among racial and ethnic groups, with blacks having the highest rates of mortality even in diseases for which the incidence of the specific cancer is lower than that seen in the white population. Stage for stage, 5-year survival rates are lower, even when the fact that cancers are less likely to be diagnosed in localized sites is taken into account. Recent data suggest that this difference is due in part to marked variations in the biology of the cancer itself, with a higher incidence of worse prognosis disease found in blacks compared to
P.1640
whites. In addition, differences in treatment and comorbid conditions play a significant role. Overall, cancer rates are higher for whites and blacks than for Asians/Pacific Islanders. Among the leading cancers, the incidence of prostate cancer among black men is about 1.5 times higher than among white men, and 2.7 times higher than among Asian/Pacific Islanders. In contrast, breast cancer among white women is about 1.2 times higher than among black women, and 1.7 times higher than among Asian/Pacific Islander women. Other racial differences include a higher rate of multiple myeloma in black men and women and a higher rate of liver, intrahepatic bile duct, and stomach cancers in Asian/Pacific Islander men and women. Data from the 2000 census confirm the existence of geographic variability in cancer incidence, although this is lower than previously thought; for example, breast cancer rates in Marin County in California and in Washington state appear to be among the highest in the United States. Interestingly, the increased incidence is similar to that seen in higher socioeconomic groups with higher attained education, delayed childbearing, a lower rate of breast-feeding, and higher relative alcohol intake—and appears to affect mostly the white population. The contribution of environmental factors, exposure to toxins, and other dietary factors is not fully understood but clearly plays a role. Current research is focusing on exposures and risks that occur in adolescence.
Table 40-1. Incidence of and mortality from the ten most common cancers in the United States in males and females (all races), 1997–2001. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The cause of most cancers remains unknown, although workers in the field of molecular biology have begun to unravel the complex pathways leading to cancer cell growth and metastases. Mutations in DNA sequences leading to abnormal or unregulated expression of protooncogenes or deletion of tumor suppressor genes—or both—have been linked to abnormal
P.1641
cellular proliferation. Oncogenes encode for cellular growth factor receptors, growth factors, or elements of the proliferative machinery of the cancer cell. Tumor suppressor genes either code for or control regulatory proteins that normally suppress cellular proliferation; loss of these genes leads to cell growth. Cancer results from these and other mutations, which may be due to environmental exposure, genetic susceptibility, infectious agents, and other factors.
Table 40-2. Lifetime risks for the most common cancers, 1999–2001. | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
Most tumors exhibit chromosomal abnormalities such as deletions, inversions, translocations, or duplications. Although usually nonspecific, certain genetic alterations are strongly associated with specific malignancies and in some cases can be used to assess prognosis. In Burkitt's lymphoma, the c-myc oncogene is activated by translocation of genetic material from chromosome 8 to chromosome 14. Chronic myelogenous leukemia (CML) is defined by a reciprocal translocation of the long arms of chromosomes 9 and 22, resulting in the generation of a fusion protein (BCRABL) with tyrosine kinase activity. In colon cancer, loss of the long arm of chromosome 18 (18q) predicts a poor outcome, whereas mutations in the gene for the type II receptor for transforming growth factor-β1 (TGF-β1) with microsatellite instability predict a favorable outcome. In one study, 5-year survival following adjuvant chemotherapy for stage III colon cancer was 74% in those who retained the 18q allele and 50% in those with loss of the allele. Five-year survival was 74% for patients whose cancers had both microsatellite instability and a mutated gene for the type II receptor for TGF-β1 and 46% if the tumor did not have the mutation. Genetic mutations in chronic lymphocytic leukemia (CLL) have been shown to occur in up to 82% of cases and strongly predict outcomes. For example, patients with deletions of the short arm of chromosome 17 had a survival of only 2.7 years, whereas those with deletions of the long arm of chromosome 13 had a survival of 11 years. Overexpression of the HER-2/neu gene in breast cancer has been associated with more aggressive tumors, a higher stage at diagnosis, and a shorter survival. However, this gene has also been associated with marked chemotherapy responsiveness to specific agents, and has provided a successful target for a targeted biologic agent in the treatment of breast cancer.
The p53 gene appears to trigger programmed cell death (apoptosis) as a way of regulating uncontrolled cellular proliferation in the setting of aberrant growth signals. Mutations in the p53 gene result in loss of the ability of the gene product to bind to DNA, thereby removing its suppressive effect. p53 can also be inactivated by overexpression of an oncogene whose protein product binds to normal p53 and prevents its action. This occurs in many soft tissue sarcomas. The Bcl-2 family of proteins act as “arbiters of cell death” with a balance of both “antideath” and “prodeath” activity. Bcl-2 and Bcl-XL appear to function as “antideath” proteins to prevent programmed cell death of cancer cells; overexpression of these proteins in cancer confers resistance to chemotherapy and radiation therapy. Bcl2 and Bcl-XL are overexpressed at a high level (50–100%) on common cancers, including cancers of the breast, colon, prostate, head and neck, and ovary. Agents that target the receptors to which these proteins bind or their production might work to overcome cancer resistance (see section on novel therapies at the end of this chapter).
Another control against abnormal cellular proliferation also contributes to cellular aging. As a cell divides and ages, there is progressive shortening of the ends of the chromosomes, or telomeres. A striking correlation between cancer and the overexpression of telomerase (an enzyme capable of preventing the shortening of telomeres) suggests that it might be partially responsible for tumor cell immortality. Telomerase activity is present in about 85% of malignant tumors but absent in most normal somatic tissues. The stage and severity of neuroblastoma, breast cancer, and other cancers have been found to correlate with levels of telomerase activity, indicating a prognostic role of enzyme activity. Normal human cells transfected with the telomerase gene in vitro exceed their normal life span and ability to divide, thereby establishing a causal relationship between telomere shortening and cellular senescence. This suggests important possibilities for targeting telomerase activity as part of cancer therapy.
The development of cancer is a complicated multistep process that appears to involve the acquisition of an increasing number of genetic mutations, eventually resulting in invasive disease. Clinical examples of this stepwise progression can be found in many common cancers, including breast, colon, and prostate cancers. A history of the benign finding of atypical ductal hyperplasia on breast biopsy is clearly associated with a twoto fourfold increase in the risk of subsequent invasive cancer. Noninvasive breast cancer (ductal carcinoma in situ) is a preinvasive lesion that can progress into invasive cancer if left untreated. Understanding the cascade of genetic changes associated with the progression of benign cells to invasive cancer is a critical step in developing therapies targeted to a specific cancer. These genetic changes can now be mapped by a process called comparative genomic hybridization; this is an intense area of research. DNA microarray studies can detect activation of thousands of genes in a single experiment. The resulting DNA expression profile can be used not only to understand the development of cancer but also to assess prognosis, predict response to therapy, and direct targeted therapies. Studies have recently associated certain DNA profiles with specific cancer phenotypes, an important first step in this exciting area of research. In non-small cell lung cancer, reduced expression of the adhesion molecule E-cadherin detected by tissue microarray analysis correlated with reduced survival as well as local invasion and regional metastases.
Defining chromosomal aberrations and their association with prognosis will help in designing targeted therapies as well as risk-adapted treatment strategies. Several
P.1642
recent studies suggest that clusters of genes may help both to define specific chemotherapy sensitivities of specific tumors and to more accurately estimate prognosis. Gene expression analysis using array technologies allows the simultaneous examination of the relative abundance of thousands of genes in a cell or tissue and avoids the need to identify each gene individually. Specific gene expression profiles have been associated with survival in breast cancer. In one study, frozen tissues from diagnostic biopsies of breast tumors were analyzed and the results then correlated with response to neoadjuvant chemotherapy administered before surgery. A specific clustering of genes was highly correlated to the complete disappearance of tumor at the time of surgery. There were very few patients in this pilot trial; ongoing studies are examining serial biopsies during chemotherapy in an attempt to further predict response to treatment. Ideally, these data will be used in the future to individualize treatment for specific cancers. Rapid progress is being made in the use of genetic analysis of tumors to more accurately predict prognosis and perhaps response to therapy in breast cancer. The Oncotype Dx assay is a test that evaluates sixteen cancer-related and five reference genes in fixed tumor tissue—as expressed in RNA—to assess the risk of metastatic breast cancer recurrence at 10 years in women with estrogenor progesterone-receptor-positive breast cancers with negative axillary node involvement. A recurrence score is calculated based on the relative expression of the cancer-related genes in a particular tumor. In a large study evaluating tumors from patients enrolled in a clinical trial more than 10 years ago, the recurrence score was found to be a more accurate predictor of risk of recurrence than standard prognostic indicators such as tumor grade or size. Subsequent studies have suggested that the recurrence score may also be able to predict benefit from chemotherapy, with the primary benefit being in women with high scores. A woman with a higher risk of recurrence might receive chemotherapy as well as hormonal therapy, whereas a woman with a low risk would receive hormonal therapy alone. Current studies are trying to further validate this interesting tool, which is now clinically available though quite expensive (http://www.genomichealth.com). The assay can be performed in fixed, paraffin-embedded tissue, which should be readily available in all patients with a cancer diagnosis. It is validated only in axillary-node negative, hormone receptor-positive breast cancer.
A second study evaluated gene expression in 86 patients with newly diagnosed stage I adenocarcinoma of the lung. Clustering of gene expression profiles with 4966 genes revealed three clusters of lung adenocarcinomas with a significant relationship between the specific cluster and tumor stage or differentiation. In addition, high-risk and low-risk groups were identified with very different survival statistics. Understanding differences in the behavior of early-stage cancers using gene expression profiling will in the future permit differential treatment directed toward maximizing outcome, choosing appropriate therapy, and accurately estimating prognosis.
Genetic analysis may help to determine appropriate dosing of effective but toxic chemotherapeutic agents. Specific polymorphisms or variations in the UGT1A1 gene have recently been shown to predict severe neutropenia resulting from the colorectal cancer drug irinotecan. The UGT1A1 gene produces a protein that metabolizes the active metabolite of irinotecan; alterations in this gene are quite common. Genotyping using a simple blood test may be able to identify patients at high risk for life-threatening side effects, allowing individualization of dosing to improve the therapeutic ratio for patients with colorectal cancer. A screening test could become available within the next few years.
Another area of study is the field of proteomics. Genes encode proteins, and proteins may be easier to evaluate than genes. Identifying and analyzing individual proteins are both difficult and time consuming, but describing patterns or panels of proteins is more straightforward. The field of proteomics seeks to associate specific patterns of protein expression with disease states, prognosis, and response to treatment in both tissue and serum. Proteomics has already been used successfully to aid in early detection of cancer; a good example is the use of prostate-specific antigen for the detection of prostate cancer. A division of the NCI is devoted to the study of proteomics and serves as an important source of information for researchers.
Hereditary Factors
Hereditary predisposition to some cancers has been linked to genetic events and is manifested by a family history of a common cancer or cancers occurring frequently—in a younger than expected age group—or any history of a relatively rare cancer. Examples include familial retinoblastoma, familial adenomatous polyposis (FAP), multiple endocrine neoplasia (MEN) syndromes, and the hereditary breast and ovarian cancer syndromes. Although FAP is a rare syndrome, somatic mutations in the affected gene (adenomatous polyposis coli; APC) occur in more than 60% of patients with colonic carcinomas and in an equal proportion of patients with adenomas. Genetic mutations associated with an increased risk of developing breast and ovarian cancers appear to be much more common than previously thought and are strongly related to age at diagnosis of cancer. It is estimated that 5–10% of all breast cancers and more than 40% of breast cancers occurring in women under 30 years of age are due to inheritance of an abnormal gene. The risk of ovarian and other cancers is also significantly increased in carriers of these susceptibility genes.
A tumor suppressor gene termed BRCA1 on chromosome 17 has been shown to be abnormal in some families with early onset and high frequencies of breast cancer and ovarian cancer. More than 100 mutations have been identified in the BRCA1 gene, making identification of high-risk individuals difficult. Two population-based studies found that up to 20% of Jewish
P.1643
women with breast cancer diagnosed at or before the age of 40 years and approximately 10% of all women with breast cancer diagnosed before the age of 35 years harbor mutations in the BRCA1 gene. Inheritance of a mutated BRCA1 gene confers a lifelong risk of approximately 85% for breast cancer and 50% for ovarian cancer. Inheritance of the BRCA1 gene also appears to increase the risk of developing both colon and prostate cancers. Another susceptibility gene, BRCA2, has been associated with an increased risk for male breast cancer as well as malignant melanoma and other cancers. There is clearly an association of phenotype and inheritance of susceptibility genes. Breast cancers in BRCA1 carriers tend to be hormone receptor negative, whereas cancers in BRCA2 carriers are generally hormone receptor positive. For a woman diagnosed with breast cancer between the ages of 30 and 34 years, the likelihood of a BRCA1 mutation is as high as 27% if her tumor is both hormone receptor negative and of high grade.
Risk Factors & Prevention
Carriers of BRCA mutations who have children appear to be at higher risk for developing breast cancer by age 40 years than carriers who are nulliparous—in contrast to the usual risk factors for sporadic breast cancer. Interestingly—and despite the association of BRCA1 with an increased risk of hormone receptor-negative breast tumors—recent data confirm that oophorectomy in women with either mutation before the age of 40 years significantly reduces the risk of breast cancer (up to 75%) and ovarian cancer, presumably by decreasing exposure of breast tissue to estrogen. The use of oral contraceptives for more than 5 years appears to significantly reduce the risk of ovarian cancer as well, perhaps by regulating ovarian cycling. Compared with sporadic ovarian cancers, those associated with the BRCA1 mutation appeared to have a better clinical course, with a median survival of 77 months in women carrying the mutation compared with 29 months in controls. Many other less common genes have been identified that increase the risk of breast and other cancers, although clearly there are many yet to be identified. One study found that women who have an identical twin sister with breast cancer are at least three times more likely than average to develop cancer. If the twin was diagnosed before age 40 years, 25% of the remaining siblings developed cancer over the next 20 years. Increased risk in this setting is probably due to a combination of genes that will be more difficult to discern.
Screening for Genetic Risk Factors
With the discovery and cloning of cancer susceptibility genes such as BRCA1, commercial testing has been developed for “screening” using linked genetic markers. Tests for genes linked to familial cancer have raised concerns about the impact of positive results on patients. One study has evaluated indications for testing of the APC gene. Of the patients tested, 85% were felt to have valid indications for testing. However, only 20% received genetic counseling before the test; only 15% gave informed consent; and in 30% of cases the clinicians misinterpreted the results. It is essential that clinicians recognize the limitations of these tests and that genetic testing be made available in the appropriate setting. Educational programs and publications are available to help educate patients regarding genetic testing. Many cancer centers now have genetic screening and counseling programs. Patients with a strong family history of cancer should be referred to such programs before testing is performed. Early and regular cancer screening is recommended for affected members of the family, and aggressive but relatively effective preventive measures such as prophylactic mastectomy and oophorectomy should also be discussed. Updated guidelines for testing—including indications for testing, counseling about medical management, confidentiality of results, insurance coverage, and protection from discrimination—have recently been published (see reference below) and are available without cost at http://www.asco.org (search under genetic testing).
Other Familial Cancers
Other familial clusterings of cancer have been described that have not yet been associated with inheritance of a particular gene. Evaluation of participants in a study of colonic polyps revealed an increased risk of colorectal cancer in the siblings and parents of patients with adenomatous polyps, particularly when the adenoma was diagnosed before age 60 years or (for a sibling) when a parent had colorectal cancer. This syndrome, referred to as a hereditary nonpolyposis colorectal cancer (HNPCC), has been associated with a germline mutation of DNA mismatch-repair genes. In one European cohort, at least 2% of patients with colorectal cancer had these mutations. Testing for replication errors should be considered in patients under age 50 years with colorectal cancer who have a family history of colorectal or endometrial cancer. Family members of patients with this syndrome may benefit from early screening.
In addition to the germline mutations found in HNPCC, up to 10–15% of sporadic colorectal cancers have somatic mutations in DNA repair genes resulting in microsatellite instability (MSI) or alterations in the size of repetitive nucleotide sequences. These cancers are usually in the right side of the colon and have been associated with both a better prognosis and a striking sensitivity to adjuvant chemotherapy. The HER-2/neu oncogene is a somatic (not inherited or germline) mutation that encodes a tyrosine kinase receptor in the epidermal growth factor receptor (EGFR) family and is overexpressed in about 20% of breast cancers. HER-2/neu overexpression is associated with more aggressive cancers, a worse prognosis, and enhanced tumor sensitivity to anthracycline chemotherapy. An antibody that targets this receptor (trastuzumab) has been shown to improve survival when
P.1644
used with chemotherapy to treat HER-2/neu overexpressing metastatic breast cancer. HER-2/neu overexpression in prostate cancer also appears to correlate with a poorer 5-year prognosis, though this result remains to be validated. Identifying genetic factors that are associated with specific cancer phenotypes may allow effective tailoring of adjuvant chemotherapy, as well as lead to the development of targeted therapeutics to effectively treat the biologic pathways driving tumor growth.
Immune Factors
Autoimmune suppression may contribute to the development of cancer. Tumors are allowed to exist because of tolerance—the ability of the tumor to escape the host immune system. The host immune system cannot recognize the tumor as foreign because of an absence of critical immunostimulatory molecules on the tumor itself, resulting in a state of anergy (deletion of tumor-specific lymphocytes) toward the growing cancer. Novel therapies (such as vaccines) aimed at correcting this immunodeficient state and stimulating the host immune response against tumor cells are now being tested clinically. (See section on novel therapies at the end of this chapter.)
Environmental, Infectious, & Therapeutic Carcinogens
It is difficult to link exposures to specific carcinogens with the development of cancer, since latency is long and the nature of exposure is poorly documented. Environmental carcinogens include chemical carcinogens such as benzene and asbestos, oncogenic viruses such as the human papillomavirus and the Epstein–Barr virus, and physical agents such as ionizing radiation and ultraviolet light.
Certain viral infections may increase the risk of cancer and clearly have a pathogenetic role, such as the association between Epstein–Barr virus infection and endemic Burkitt's lymphoma and non-Hodgkin's lymphoma. Chronic infection with hepatitis B or C viruses increases the risk of hepatocellular carcinoma. Largely owing to the increase in chronic hepatitis, the incidence of hepatocellular carcinoma significantly increased during the 1990s compared with the 1970s. Interestingly, treatment with the antiviral agent interferon-a following resection of hepatitis C-related hepatocellular carcinoma in a randomized trial appeared to significantly reduce the risk of cancer recurrence. Screening for cancer with regular scans in patients with known persistent hepatitis B and C infection is now standard practice as early identification of hepatocellular carcinoma is critical to effective treatment. Infection with human immunodeficiency virus (HIV) has been associated with non-Hodgkin's lymphoma, Hodgkin's disease, Kaposi's sarcoma, and cervical and anal cancers. The finding of human herpesvirus-8 (HHV-8) DNA sequences in both acquired immunodeficiency syndrome (AIDS)-associated and non-AIDS-associated Kaposi's sarcoma (KS) supports a causative role of the herpesviruses in the development of some cancers. It appears that HHV-8 is sexually transmitted among men. Antibodies to HHV-8 correlate with the subsequent development of KS and it is now thought that infection is necessary for KS to develop. The sexually transmitted human papillomavirus (HPV) is a major risk factor for the development of cervical carcinoma and anal cancer; nearly 100% of women with cervical cancer have evidence of this infection. Fifteen HPV subtypes have been identified with an increased risk of cervical cancer; HPV 16 and 18 are the most common and are associated with a more than 200fold increased risk of cancer. HPV is a common infection, and most infected women do not develop cancer. Progression is associated with persistent infection over a decade or more; additional genetic or systemic cofactors are required, although only partially understood. Understanding the infectious cause of cervical cancer has led to the development of a vaccine directed against HPV 16 and 18; large-scale testing of this vaccine is now in progress. Chronic infection with bacteria has also been associated with an increased risk of malignancy. Infection with Helicobacter pylori is thought to increase the risk of cancer of the distal portion of the stomach approximately sixfold, and also increases the risk for gastric lymphoma. Approximately 60% of gastric cancers are associated with H pylori infection. Geographic variations in the incidence of gastric cancer may be influenced by geographic variations in the strain of H pylori; strains that produce a specific protein are more likely to be associated with cancer than those that do not. Screening for and treatment of H pylori may be a cost-effective way to prevent gastric cancer in the United States.
An additional cause of cancer is chemotherapy or radiation therapy for a prior malignancy. More aggressive chemotherapeutic and radiation regimens—and especially those combining the two treatment modalities— have been associated with increased rates of both secondary leukemias and solid tumors. The latency period may be short (2–5 years for leukemia) or very long (10–20 years for solid tumors), but the prognosis is uniformly poor. Chemotherapeutic agents known to cause secondary malignancies include alkylating agents—busulfan, cyclophosphamide, mechlorethamine, etc—and topoisomerase II inhibitors, including epipodophyllotoxins (etoposide), anthracyclines, ie, doxorubicin and epirubicin, and anthracenediones (mitoxantrone). Secondary leukemias can be characterized to some degree by the causative agent. Alkylator-induced leukemias are usually associated with abnormalities involving chromosomes 5 and 7 and generally occur within 5–7 years after exposure. In contrast, topoisomerase II-induced leukemias occur within 2–3 years following exposure and involve aberrations in a specific gene within the long arm of chromosome 11 (11q23). Abnormalities of 11q23 often occur at a specific breakpoint region thought to be involved in DNA transcription. An increase in the rate of secondary acute leukemia has been reported in breast cancer patients treated with dose intensification of cyclophosphamide in combination with doxorubicin (a topo-
P.1645
isomerase II active drug) from 1992 to 1994. The incidence is approximately 0.3% in a multicenter study involving over 2500 women with positive axillary nodes. Increased dosages and frequency of administration of anthracyclines, anthracenediones, and the alkylating agent cyclophosphamide have been reported to increase the risk of leukemia to as high as 3–4%. Prolonged oral exposure to etoposide or alkylator agents can result in a much higher risk of secondary leukemia as well. Platinum-based chemotherapy for ovarian cancer has been reported to increase the risk of leukemia twofold to eightfold, with larger doses and longer treatment courses associated with higher risks. This risk was significantly higher in women who had also received intravenous melphalan.
The risk of certain secondary cancers may be age dependent. Radiation therapy for Hodgkin's disease increases the risk of breast cancer (including bilateral disease) if the radiation occurred in women under the age of 30 years. The relative risk of solid tumors and leukemias has been found to increase significantly with younger age at first chemotherapy treatment for Hodgkin's disease. This risk is especially high when chemotherapy and radiation are combined. Nevertheless, the risk of secondary malignancies in children surviving at least 5 years after diagnosis is relatively low at 3.2% 20 years postdiagnosis, with primary disease recurrence remaining the most common cause of mortality. The Childhood Cancer Survivor Study (CCSS) is a large prospective study of over 14,000 survivors of childhood cancer designed to characterize the late effects of therapy in this increasing population. Although the risk of complications is highest in the first 5 years after diagnosis and treatment, risks of additional sequelae persist for many years.
Estrogen & Progesterone
Retrospective data indicate that the combination of estrogen and progesterone given as long-term hormonal replacement to postmenopausal women may significantly increase the risk of breast cancer over estrogen therapy alone. The best evidence for the risks and benefits of postmenopausal hormone use comes from the Women's Health Initiative (WHI), a large randomized clinical trial of over 16,000 healthy women ages 50–79 years that compared the effects of combined estrogen and progesterone to placebo on a variety of health outcomes. The trial, sponsored by the National Institutes of Health (NIH), was halted early when, in July 2002, investigators reported that the overall risks of estrogen plus progestin—specifically Prempro—outweighed the benefits. The WHI found that use of Prempro increased the risk of breast cancer (by 24%, or an additional eight cases of breast cancer for every 10,000 women treated), heart disease, stroke, and blood clots, although there were fewer cases of hip fractures and colon cancer in the treatment arm. Follow-up is still short, and at this time there is no difference in mortality. However, recent data from this trial indicate that the breast cancers developing in women receiving combined hormonal therapy were significantly larger than those developing in women on placebo and were diagnosed at a more advanced stage. Hormonal therapy increases breast density, increasing the difficulty in diagnosing cancers at an early stage. The WHI study has also shown that almost twice the number of women receiving Prempro had abnormal mammograms at 1 year compared with women receiving placebo medication. The HABITS (hormonal replacement therapy after breast cancer) trial evaluated the safety of hormone replacement therapy (HRT) after a diagnosis of breast cancer. After a median follow-up of only 2.1 years, more than three times the number of women in the HRT group had developed a new breast cancer event compared to the women in the best treatment group. These dramatic differences led to early closing of the trial.
An update of the WHI study showed that in women aged 65 years and over, use of estrogen plus progestin doubled the risk of developing dementia. Additionally, an analysis of the quality of life of a subgroup of WHI participants aged 50–79 years found no change in general health, vitality, mental health, depressive symptoms, or sexual satisfaction associated with use of combined hormonal replacement.
Estrogen alone appears to be less risky, but does not protect against chronic disease. The estrogen alone component of the WHI study randomized over 10,700 postmenopausal women with prior hysterectomy to either conjugated equine estrogen (CEE) or placebo, and has now been published with 6.8 years of follow-up. Women treated with CEE had an increased risk of stroke, a decreased risk of hip fracture, and no difference in the rate of either coronary heart disease or breast cancer. The rate of incident disease events was equivalent in the placebo and CEE arms, indicating no overall benefit. In women aged 65 tears and older, CEE had an adverse effect on cognition, although there was no apparent increase in dementia. An extension study is planned to continue to follow all women enrolled in the WHI study through 2010.
In an observational study of over 40,000 women, those who used estrogen alone for 10–19 years were twice as likely to develop ovarian cancer as women who did not use menopausal hormones. For women who used estrogen for 20 or more years, the risk of ovarian cancer increased to three times that of women who did not use menopausal hormones. Another study suggests that the increased risk appears to be limited to women who used estrogens for 10 or more years. There are insufficient data on which to base a conclusion about whether combined estrogen and progesterone use affects the risk of developing ovarian cancer.
It is clear that other dietary and lifestyle factors play a significant role in the risk of developing specific cancers, although much of the specifics still need to be elucidated (see section on Primary Prevention, below).
American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. Adopted on March 1, 2003. J Clin Oncol 2003;21:1.
Anderson GL et al: Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA 2004;291:1701.
P.1646
Beer DG et al: Gene-expression profiles predict survival of patients with lung adenocarcinoma. Nat Med 2002;8:816.
Bremnes RM et al: High-throughput tissue microarray analysis used to evaluate biology and prognostic significance of the E-cadherin pathway in non-small cell lung cancer. J Clin Oncol 2002;20:2417.
Buys CH: Telomeres, telomerase, and cancer. N Engl J Med 2000;342:1282.
Chlebowski RT et al: Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women's Health Initiative randomized trial. JAMA 2003;289:3243.
Diller L et al: Breast cancer screening in women previously treated for Hodgkin's disease: a prospective cohort study. J Clin Oncol 2002;20:2085.
Eng C et al: Genetic testing for cancer predisposition. Annu Rev Med 2001;52:371.
Green DR et al: A matter of life and death. Cancer Cell 2002;1:19.
Hankinson SE et al: Towards an integrated model for breast cancer etiology: the lifelong interplay of genes, lifestyle, and hormones. Breast Cancer Res 2004;6:213.
Holmberg L et al: HABITS (hormonal replacement therapy after breast cancer—is it safe?;), a randomised comparison: trial stopped. Lancet 2004;363:453.
Modugno F et al: Ovarian cancer and high-risk women—implications for prevention, screening, and early detection. Gynecol Oncol 2003;91:15.
Rossouw JE et al: Risks and benefits of combined estrogen and progestin in healthy menopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321.
Schiffman MH et al: Epidemiologic studies of a necessary causal risk factor: human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst 2003;95:E2.
Soussi T: The p53 tumor suppressor gene: from molecular biology to clinical investigation. Ann NY Acad Sci 2000;910:121.
van de Vijver MJ et al: A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 2002;347:1999.
Watanabe T et al: Molecular predictors of survival after adjuvant chemotherapy for colon cancer. N Engl J Med 2001;344:1196.
Weir HK et al: Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst 2003;95:1276.
Wulfkuhle JD et al: Proteomic applications for the early detection of cancer. Nat Rev Cancer 2003;3:267.
PREVENTION OF CANCER
PRIMARY PREVENTION
1. Lifestyle Modifications
Population studies suggest that lifestyle—including tobacco use, diet, obesity, and alcohol consumption— accounts for a majority of avoidable cancer deaths in the United States. Other factors, including obesity, parity, and length of lactation, have also been associated with increased cancer risk. Although prostate and breast cancers are the most common malignancies in men and women, respectively, the most common cause of cancer-related death in both sexes is still lung cancer. Since 1973, there has been only a 10% increase in the incidence of lung cancer in men compared with a 124% increase in women, reflecting a marked increase in the number of women who smoke. In 2005, the American Cancer Society estimates that more than 175,000 cancer deaths will be caused by tobacco use, and smoking remains the most preventable cause of death in our society. Because tobacco-related cancers account for at least 30% of all fatal forms of cancer and 87% of lung cancer-related deaths, smoking cessation is an important area for continued education and prevention efforts. Strategies for helping patients stop smoking are described in Chapter 1. Programs directed both at cessation of smoking and at reversing the social acceptability of cigarette smoking have been more successful than programs encouraging cessation alone. In California, Massachusetts, Florida, and Maine, comprehensive tobacco control programs have resulted in a substantial decrease in the prevalence of adult smoking. In California, this program was responsible for halving of the per capita consumption of cigarettes and translated into a significant decline (almost five times greater than the rest of the United States) in the incidence of lung cancer in both men and women in the state from 1988 to 1997. The decline in women is even more striking when compared with the rest of the United States, where the rate of lung cancer in women is still increasing. For an excellent article (with graphics) on this topic, go to http://www.asco.org and search under Tobacco Control and Global Issues, or see Cancer Prevention and Early Detection Facts and Figures 2004, accessible at http://www.cancer.org/downloads/STT/CPED2004PWSecured.pdf.
The molecular targets for carcinogens such as alcohol and tobacco have not yet been identified. However, an evaluation of tumor samples from over 100 patients with squamous cell carcinoma of the head and neck found an association between smokers and genetic mutations in the p53 gene, thought to result in the initiation or progression of this cancer. This supports epidemiologic evidence that abstinence from smoking is important in preventing head and neck cancer. Cigarette smoking has been linked to cancers of the lung, mouth, larynx, esophagus, pancreas, kidney, and bladder. In addition, a study by the American Cancer Society found a 30–40% increase in the risk of death from colorectal cancer in cigarette smokers, with the increased risk occurring after 20 years of smoking and increasing with the number of cigarettes smoked daily. The risk decreased each year after quitting smoking, indicating that change in this major lifestyle factor can still reduce risk of death from cancer. In addition, a recent study showed that patients who stopped smoking following a diagnosis of small cell lung cancer and who were treated with
P.1647
chemotherapy and radiation had significantly longer 2year and 5-year survivals than those who continued smoking. A similar prolongation in survival occurs in patients with head and neck cancer who quit smoking following diagnosis. Although cigarette smoking has not been related to the incidence of breast cancer, early data suggest that mortality from established breast cancer is higher in smokers than in nonsmokers. This supports the hypothesis that ongoing toxicity even in patients already diagnosed with cancer contributes to mortality. However, up to 50% of all lung cancers occur in those who have stopped smoking for at least 1 year, indicating that at least some of the carcinogenic effect of cigarette smoking may be irreversible.
Diet is an important area of intervention for primary cancer prevention. Epidemiologic studies suggest an inverse relationship between fruit and vegetable intake and the risk of common carcinomas, indicating a potential protective role of these dietary components. A casecontrol study in South Asia found a small reduction in the risk of breast cancer associated with a diet rich in vegetables. High intakes of fat and specific fatty acids have been postulated to increase the risk of breast, colon, prostate, and lung cancer, although a recent study in Canada found no association between carbohydrate intake and risk of colorectal cancer in women. Linoleic acids in essential fatty acids are the food source for arachidonic acid—and this metabolic pathway has been postulated to play an important role in the development of cancer. However, the Nurses' Health Study, which followed more than 88,000 women for 14 years with food frequency questionnaires every 4 years beginning in 1980, found no evidence that a lower intake of total fat or specific major types of fat decreased the risk of breast cancer. A recent subset analysis of premenopausal women aged 26–46 years within the Nurses' Health Study found a slightly increased risk of breast cancer with intake of animal but not vegetable fat. A higher intake of animal fat was also associated with a larger body mass index as well as other known risk factors. Data from the Nurses' Health Study and other epidemiologic studies suggest that a high consumption of red meat and excess alcohol consumption (probably also in combination with a diet low in possible preventive vitamins such as folate) may increase the risk of colorectal cancer. A meta-analysis published in 1999 evaluated dietary fat intervention studies (published from 1966 through 1998) on serum estradiol levels and fat consumption. These findings did not rule out the possibility that reducing fat consumption below 20% of calories might reduce breast cancer risk by lowering serum estradiol levels. Another study compared the dietary intake of saturated fat of 1665 men with prostate cancer to the diet of an equal number of men without the disease. A high intake of saturated fat increased the risk of prostate cancer in all four major ethnic groups evaluated. There was no increase in prostate cancer among men with the lowest intake of saturated fats.
Phytoestrogens are plant estrogenic substances including isoflavones, coumestans, and lignans. There has been interest in the role of phytoestrogens in the prevention of breast cancer, due to the lower rates of breast cancer observed in women with a high consumption of phytoestrogens, such as in Asia. A variety of studies have evaluated epidemiologic data regarding intake, but are limited based on problems with dietary recall, or short duration of exposures in prospective designs. Ongoing trials are assessing the role of phytoestrogen supplementation on the reduction of breast density, a surrogate and short-term marker for breast cancer risk. Phytoestrogens clearly have the potential to affect estrogen-driven cell growth in either a positive or negative way. To date, there are no data to suggest that dietary plant phytoestrogens stimulate cancer growth.
Obesity or a high body mass index has been implicated as a risk factor for breast, colorectal, and lung cancers (in nonsmokers) as well as others. Body mass index and elevated blood pressure have been associated with an increased risk of renal cell cancer in men. Dietary factors may further increase risk in already highrisk populations. A high intake of saturated fat in 27,111 smokers participating in the Alpha-Tocopherol, Beta-Carotene (ATBC) Cancer Prevention study significantly increased the risk of developing pancreatic cancer, suggesting that diet may be a modifiable factor in the prevention of pancreatic cancer in this population.
Increased intake of dietary fiber has been thought to reduce the risk of colorectal cancer and adenomas. The Nurses' Health Study investigated the intake of dietary fiber in the same population specified above, and no association was found between the intake of dietary fiber and the risk of colorectal cancer or adenomas. A prospective study of over 10,000 men likewise did not find a significant association between fiber intake and the risk of developing adenomas. Two prospective, randomized trials tested the value of a high-fiber, low-fat diet or a high-fiber cereal supplement versus a standard diet in reducing the risk of recurrent colorectal adenomas in men and women with a recent prior diagnosis of adenoma and demonstrated no difference in the risk of recurrent adenoma based on dietary regimens. Other dietary factors such as folate, methionine, and vitamin D may reduce the risk of colorectal malignancy, but this too will require further investigation.
Various lifestyle and dietary factors have been associated with a reduced risk of breast cancer. Increased duration of lactation, particularly for at least 1 year and with more than one pregnancy, reduced the subsequent risk of breast cancer in one large meta-analysis. In another study, Korean women who breast-fed for less than a year had a 20% lower risk of developing breast cancer, and those who breast-fed for more than 24 months had a 40% reduced risk compared with those who had no history of lactation. The California Teachers Study is a prospective study of over 133,000 active and retired teachers and administrators that is evaluating a variety of factors related to the risk of de-
P.1648
veloping cancer over time. At 2 years of follow-up, the only dietary factor associated with an increased risk of breast cancer was alcohol ingestion, with two or more glasses of wine per day associated with a 50% increased risk (relative risk 1.5) compared with nondrinkers. It may be that women with a higher risk of breast cancer could modify their risk by reducing overall alcohol intake.
The WHI, begun in 1992, examined the effects of three distinct interventions—a low-fat eating pattern, hormone replacement therapy, and calcium and vitamin D supplementation—on the prevention of cancer, cardiovascular disease, and osteoporosis in 64,500 postmenopausal women of all races. An additional 100,000 women have been enrolled in an observational study. Both the estrogen–progesterone and estrogen-alone components of this study have been closed (see Incidence & Etiology, above). Information on the dietary and vitamin intervention component of this trial should be available in the next 1–2 years. Recent data from the WHI study found that postmenopausal women who exercised regularly and not necessarily strenuously had a lower risk of breast cancer than those who did not; those who reported the equivalent of 1.25–2.5 hours of brisk walking per week had an 18% lower risk of breast cancer compared with inactive women. This impact increased with duration and intensity of exercise. Other ongoing intervention trials include the Women's Healthy Eating and Living (WHEL) study, which targets women 1–3 years following a diagnosis of breast cancer to assess the effects of a low-fat, high-fiber diet on recurrence and death from cancer.
Given the general lack of specific information linking diet to the risk of cancer, what should we recommend to patients now? A diet low in saturated fat and rich in whole grains, fruits, and vegetables appears to improve health in a variety of ways—certainly in reducing cardiovascular disease and diabetes and, based on epidemiologic data, reducing the overall risk of developing cancer. Similarly, weight loss appears to be a prudent recommendation. For more specific diets—in particular, reducing the risk of recurrence of a known cancer or precancer—we will have to wait for more data. Regular physical exercise should be incorporated into all general health recommendations.
Another lifestyle factor with important implications for primary prevention is exposure to ultraviolet light. Chronic cumulative exposure to solar ultraviolet radiation is the major risk factor for nonmelanomatous skin cancer. Regular use of sunscreen prevents the development of precancerous solar keratoses and results in regression of existing keratoses, although the effect of sunscreens on the prevention of melanoma is not clear. Protection from sunlight and the regular use of sunscreens should be recommended for the primary prevention of skin cancers.
Alberts DS et al: Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. N Engl J Med 2000;342:1156.
Cho E et al: Premenopausal fat intake and the risk of breast cancer. J Natl Cancer Inst 2003;95:1079.
Gerber B et al: Nutrition and lifestyle factors on the risk of developing breast cancer. Breast Cancer Res Treat 2003;79:265.
Horn-Ross PL et al: Recent diet and breast cancer risk: the California Teachers Study (USA). Cancer Causes Control 2002; 13:407.
Hughes JR: New treatments for smoking cessation. CA Cancer J Clin 2000;50:143.
Kup H et al: Tobacco use, cancer causation and public health impact. J Intern Med 2002;251:455.
Mathers JC: Nutrition and cancer prevention: diet-gene interactions. Proc Nutr Soc 2003;62:605.
McTiernan A et al: Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women's Health Initiative Cohort Study. JAMA 2003;290:1331.
Peeters PH et al: Phytoestrogens and breast cancer risk. Review of the epidemiological evidence. Breast Cancer Res Treat 2003;77: 171.
Riboli E et al: Epidemiologic evidence of the protective effect of fruit and vegetables on cancer risk. Am J Clin Nutr 2003; 78(3 Suppl):559S.
Seow A et al: Food groups and the risk of colorectal carcinoma in an Asian population. Cancer 2002;95:2390.
Westmaas JL et al: Altering risk in patients who smoke. Respir Care Clin North Am 2003;9:259.
2. Chemoprevention
Chemoprevention focuses on the prevention of cancer by administering chemical compounds that interfere with the multistaged carcinogenic process. Better understanding of the biochemical and molecular mechanisms of carcinogenesis has made possible the identification of potential chemopreventive agents. Four risk groups have been identified for intervention: (1) previous cancer patients (to prevent second malignancies), (2) patients with preneoplastic lesions, (3) patients at high risk for malignancy (family history, lifestyle, occupation), and (4) the general population.
Chemicals used in chemoprevention must be nontoxic and well tolerated by otherwise asymptomatic individuals. Because of the long natural history of carcinogenesis, there must also be a method of evaluating the efficacy of chemopreventive agents other than waiting for the development of tumors. Biomarkers, including the premalignant markers such as leukoplakia, colonic polyps, and aberrant crypt formation in the colon, are currently in clinical use. Other less specific surrogate markers for cancer risk such as breast density are also in use as primary end points in prevention studies. Molecular susceptibility markers may become useful; nuclear retinoic acid receptor agonists are under investigation in chemoprevention studies of patients with head and neck cancer.
Retinoids, the natural derivatives and synthetic analogs of vitamin A, are the best-studied chemopreventive agents. Nonsteroidal anti-inflammatory drugs (NSAIDs)—specifically, the selective cyclooxygenase (COX)-2 inhibitors—and hormonal agents such as
P.1649
tamoxifen, raloxifene, and finasteride appear to have an important role in prevention of some cancers. Numerous additional investigations include the role of specific dietary components such as vitamins and of pharmaceutical agents such as the statins. Ongoing research in this area is assessing the impact and appropriate use of selective NSAIDs, vitamins, hormonal agents, and, more recently, statins in cancer prevention.
Isotretinoin & Acyclic Retinoids
Retinoids are modulators of epithelial cell differentiation both in vivo and in vitro that are thought to act on nuclear receptors to regulate both cellular growth and differentiation and cell apoptosis.
Isotretinoin has been shown to suppress leukoplakia, a premalignant lesion of the aerodigestive tract. Effectiveness and tolerability of low doses of isotretinoin have been demonstrated. In a randomized maintenance trial, only patients with a demonstrated response to highdose induction (1.5 mg/kg/d) were placed on low-dose maintenance therapy (0.5 mg/kg/d). The disease progression rate was only 8% compared with a rate of 55% in a separate group taking β-carotene.
High doses of isotretinoin may prevent the development of second primary tumors in patients with early squamous cell carcinoma of the head and neck. An initial phase III study showed a statistically significant reduction in the incidence of new aerodigestive cancers when isotretinoin versus placebo was given for 1 year following definitive local therapy (4% versus 24%). There were no significant differences in disease recurrence or survival at a median follow-up of 55 months, and 30–40% of patients required reduced dosages or discontinued therapy due to toxicity. A second randomized study using lower doses of a different and probably less active retinoid showed no differences in the incidence of second primary tumors. Based on these preliminary results, three large randomized trials were performed to assess the preventive effects of retinoids on second primary tumors.
The first trial (Euroscan) studied 2 years of treatment with retinyl palmitate and acetylcysteine in over 2500 patients with either lung cancer or head and neck cancer. No differences were found in the incidence of second primary tumors. A U.S. intergroup trial studied the use of isotretinoin to prevent second primary tumors following definitive therapy of stage I non-small cell lung cancer. Because of side effects seen with the higher (50to 100-mg) dose, the drug was given at a dosage of 30 mg/d for 3 years. After a median follow-up of 3.5 years, there was no difference in time to second primary tumor, recurrence, or mortality. Subset analysis suggested that never-smokers might benefit from isotretinoin, whereas there was a higher risk of cancer recurrence and mortality in smokers in the isotretinoin arm. The major toxicity at higher doses includes skin dryness, cheilitis, hypertriglyceridemia, and conjunctivitis. These toxicities require dose reduction or temporary discontinuation of the drug. The third double-blind randomized study investigated the effect of low-dose isotretinoin for 3 years in the prevention of second primary tumors in 1200 patients definitively treated for stage I or stage II head and neck cancer, with 4 years of subsequent follow-up. The annual second primary tumor rate was 4.7% in both arms and was highest in current smokers, with the most common tumor being tumor of the lung. Although there was a transient protective effect on local recurrence in patients who received isotretinoin, this effect was lost after treatment was discontinued. A number of trials have confirmed a significantly higher rate of second primary tumor formation in smokers versus former smokers or never-smokers as well as a significant adverse effect on survival—prospectively proving the impact of active smoking on second primary tumor development. An interesting recent report suggests that nicotine may suppress the antigrowth effects of retinoids in lung cancer cells.
Retinoids have been synthesized that may be more potent chemopreventive agents with less side effects. The acyclic retinoid polyprenoic acid inhibits chemically induced hepatocarcinogenesis in rats and spontaneous hepatomas in mice. In patients with hepatocellular carcinoma, the rate of recurrent and second primary tumors is high despite curative therapy with surgical resection and ethanol injection therapy. In one study, 89 patients who were free of disease after either method of treatment were randomized to receive either 600 mg/d of polyprenoic acid or placebo for 12 months. After a median follow-up of 38 months, 27% of patients in the polyprenoic acid group versus 49% of the patients in the placebo group had recurrent or new hepatocellular carcinomas, a result that was statistically significant. The difference was even greater in the groups that had secondary hepatomas. Longer follow-up has also shown a survival advantage. At a median of 62 months of follow-up, 75% of the treatment group versus 45% of the placebo group are alive. Toxicity was quite modest (headache, nausea), with none of the side effects usually described with isotretinoin.
Three strategies that have been proved to prevent liver carcinogenesis are vaccination against hepatitis B, treatment of chronic active hepatitis C with interferon, and deletion of premalignant and latent malignant cells in the remnant livers of patients undergoing complete resection of hepatocellular carcinomas. The retinamide fenretinide (4-HPR) is a potent apoptosis-inducing synthetic vitamin A analog with significant in vitro activity. Fenretinide appears to reduce the activity of telomerase, which is important in lung carcinogenesis. Expression of telomerase reverse transcriptase (TERT), the catalytic subunit of telomerase, was evaluated on bronchial biopsies in 57 heavy smokers before and after 6 months of treatment with fenretinide or placebo. A 25% reduction in expression of TERT was found in the fenretinidetreated patients. Although clinical follow-up is clearly critical, the hope is that this type of surrogate marker will improve our ability to assess the effectiveness of possible chemopreventive agents and perhaps also iden-
P.1650
tify patients at higher risk for cancer development. A large randomized trial evaluated the effect of fenretinide versus placebo for 5 years to prevent contralateral breast cancer in women aged 30–70 years with a history of resected breast cancer and no other adjuvant therapy. Although no overall effect was observed, subset analysis found a reduction in contralateral and ipsilateral breast cancer rates in premenopausal women. Fenretinide is being studied in randomized trials as a chemopreventive agent in patients with superficial bladder cancer and in women at increased risk for ovarian cancer. Newer and more potent retinoids are being developed and tested for use in a variety of cancers.
Aspirin & Other NSAIDs
Aspirin and other NSAIDs inhibit tumor growth in experimental systems. In rats, prostaglandin inhibitors reduce the size and number of colon tumors induced by chemicals or radiation by inhibiting COX activity in the arachidonic acid pathway (COX-1 and COX-2). Regular aspirin administration at low doses (16 or more doses of 325 mg per month for at least 1 year) may reduce the risk of fatal colon cancer by as much as 40–50%. Low-dose aspirin may also protect against cancers of the esophagus, stomach, and rectum.
A study evaluating the use of sulindac versus placebo in patients with FAP showed reduction of both the number and the size of colorectal adenomas. The effect was incomplete, without complete regression of all polyps in any patient. After the sulindac was discontinued, both polyp size and polyp number increased. A large prospective cohort study was subsequently published evaluating aspirin use and the risk for both colorectal cancer and adenoma in 48,000 male health professionals over a 4-year period. The subsequent risk of developing colorectal cancer and adenomas was lower in men reporting regular use of aspirin (250 mg more than twice a week) on the study entry questionnaire even when multiple other variables were taken into account. In the Nurses' Health Study, 90,000 women were evaluated for the risk of colorectal cancer over a 12-year period according to the number of consecutive years of regular aspirin use (two or more 325-mg tablets per week) reported on three consecutive questionnaires. There was a statistically significant decrease in the risk of colorectal cancer after 20 years of consistent aspirin use, with the maximal reduction seen in women who took four to six tablets per week. A slight reduction in risk was seen in women who took aspirin for 10–19 years as well. Known risk factors such as diet did not influence this risk reduction. The Physicians Health Study is the only randomized prospective trial of aspirin (325 mg every other day for 5 years) versus placebo. At the end of the trial, no differences were seen in the frequency of self-reported new colorectal cancers.
The selective COX-2 enzyme inhibitors have been the subject of intense research in the area of prevention and treatment of cancer. COX-2 expression is inducible, unlike the constitutive expression of COX-1, and COX-2 up-regulation occurs in most epithelial tumors, including colorectal cancer and cancers of the lung and breast. This up-regulation is thought to be secondary to other initiating events, such as oncogene activation or mutation of a tumor suppressor gene. COX-2 levels increase throughout oncogenesis, and expression appears to promote angiogenesis (new blood vessel growth) and decrease apoptosis (programmed cell death). One selective COX-2 inhibitor, celecoxib, has been shown to induce regression of polyps in patients with FAP at a dosage of 400 mg twice a day for 6 months. Based on these data, celecoxib was approved by the Food and Drug Administration (FDA) for chemoprevention of polyps in patients with FAP. Up until recently, the primary known side effect of COX-2 inhibitors was thought to be gastrointestinal bleeding. However, in September 2004, a study evaluating rofecoxib found an increased incidence of cardiovascular events, including deaths, in patients taking the medication for 18 months or more. Subsequent data have confirmed an increase in cardiovascular risk for all the COX-2 inhibitors, including celecoxib and valdecoxib. Unfortunately, this apparent class effect of the selective COX-2 inhibitors markedly limits their possible use as chemopreventive agents; multiple national trials focusing on either prevention or treatment of cancer have been either closed or redesigned to eliminate the arms containing celecoxib. The gene for COX-2 is overexpressed in a number of common cancers, and overexpression correlates with worse outcomes including shorter remission durations and survival. Based on in vitro data suggesting antitumor activity of NSAIDs, including antiangiogenic effects, induction of apoptosis, and reduction of proliferation, it still appears that COX-2 inhibition is a reasonable target—but clearly new agents need to be tested that better fit the criteria for safe chemopreventive agents.
β-Carotene & Vitamin E
The carotenoids are plant pigments that protect plant cells from damage and were thought to have an antioxidant role in human tissues. β-carotene is a carotenoid found in high concentrations in human tissues; its importance as an antioxidant is controversial. A role for β-carotene and another antioxidant, vitamin E, in the prevention of either premalignant or malignant disease has not been established.
Several randomized studies have evaluated the effect of β-carotene and vitamin E on the prevention of cancer in high-risk populations. The ATBC Cancer Prevention Study randomized 29,000 Finnish male smokers to receive β-carotene, vitamin E, both agents, or neither agent for an average of 6 years. A minimal (2%) and statistically insignificant reduction in the incidence of lung cancer was seen in the men who received vitamin E. In contrast, there was a statistically significant 18% higher incidence of lung cancer in the group taking β-carotene. Vitamin E supplementation reduced prostate cancer incidence by 34% and colorectal cancer by 16%, though only the reduction in prostate cancer
P.1651
incidence was statistically significant. Men in the control group with higher levels of vitamin E or β-carotene before the study was initiated developed fewer lung cancers, suggesting that other components of foods high in these vitamins may be responsible for the protective effects noted in epidemiologic studies.
The Beta-Carotene and Retinol Efficacy Trial (CARET), a lung cancer chemoprevention study targeting high-risk populations, randomized a total of 18,000 smokers, nonsmokers, and workers with extensive occupational exposure to asbestos to receive either a combination of 30 mg/d of β-carotene (as an antioxidant) and 25,000 international units/d of retinol (vitamin A—as a tumor suppressor) or placebo. With an average of 4 years and 73,000 person-years of follow-up, the combination of β-carotene and vitamin A had no benefit on the incidence of lung cancer. In fact, the active treatment group had a 28% higher incidence of lung cancer than the placebo group, and the mortality from all causes and the rate of death from cardiovascular disease were higher by 17% and 26%, respectively. On the basis of these results, this study was stopped early.
The Physician's Health Study randomized 22,000 U.S. male physicians to receive β-carotene (50 mg on alternate days) or placebo. The physicians were treated for an average of 12 years; 11% were current smokers and 39% were former smokers at the beginning of the study. In this trial, no evidence either of benefit or of increased risk for cancer was found, with a much longer follow-up than either of the two other studies. There were no differences in the overall incidence of malignant neoplasms, cardiovascular disease, or overall mortality in the group as a whole or in the smokers.
One additional randomized study that found a positive effect of β-carotene supplementation evaluated a poorly nourished population group rather than the wellnourished populations described above. Linxian, China, is an area with one of the world's highest rates of esophageal and stomach cancers and a habitually low intake of several nutrients. In nearly 30,000 participants from the general population, the mortality rates from cancer were substantially lower among those who received daily supplementation with a combination of β-carotene, α-tocopherol, and selenium over a 5-year period. A marked reduction in the cancer death rate (13%) was observed in the supplemented group, largely due to a 21% decrease in stomach cancer mortality. Over 85% of cancers arose in the esophagus or stomach, but 31 deaths were caused by lung cancer. The risk of death from lung cancer was reduced by 45% among those receiving supplements, though the numbers were very small (11 versus 20 lung cancer deaths), and only 30% were cigarette smokers. A second study evaluated the effect of supplements, including β-carotene, on prevention of esophageal and gastric cancers in over 3300 people with esophageal dysplasia. Although esophageal cancer mortality and total cancer mortality were not significantly lower in the supplemented group, the incidence of mortality due to stomach cancer was higher. On repeat endoscopy comparing results 2 and 6 years after randomization, dysplasia had resolved in about two-thirds of patients in both arms at 6 years. These findings emphasize the need for placebocontrolled trials in the area of cancer prevention. The NCI is currently collaborating with agencies in China to pursue further chemoprevention studies in this unique population.
In summary, there is no evidence to support the use of β-carotene in the primary prevention of cancer in well-nourished populations. The major criticism of the large studies conducted to date is that increasing one type of vitamin—even one stereoisomer of a vitamin— does not reflect the vitamin content of a diet high in vegetables. In addition, intake of β-carotene is a marker of increased fruit and vegetable consumption. The balanced mixture of antioxidants found in a diet rich in fruit and vegetables may be more important and more effective in reducing cancer risk than β-carotene supplementation. Other micronutrients such as vitamin E may prove more promising.
The Women's Health Study, begun in 1992, is a randomized, double-blind, placebo-controlled trial testing the risks and benefits of vitamin E, β-carotene, and aspirin in the primary prevention of cancer and cardiovascular disease in 40,000 healthy female health professionals in the United States. Results are expected in the next few years.
Calcium & Selenium
Dietary patterns continue to be associated with a risk of colorectal neoplasia. The changes in risk may be contributed to by alterations in bile acids. Calcium appears to bind bile acids in the bowel lumen, inhibiting bileinduced mucosal damage and perhaps carcinogenesis. A modest reduction in the incidence of adenomas in patients taking calcium supplementation has been shown in patients receiving it over a 4-year period. The Selenium and Vitamin E Cancer Prevention Trial (SELECT) is the largest chemoprevention study ever to be undertaken and began in August 2001. This NCIsponsored trial will randomize 32,400 men aged 50–55 years and older to selenium, vitamin E, both, or placebo for 7–12 years in 435 sites in the United States, Canada, and Puerto Rico. This study is based on the results of the ATBC Cancer Prevention Study, in which vitamin E reduced prostate cancer incidence by 32%, and the selenium and skin cancer trial, in which selenium reduced the incidence of prostate cancer by 63%. As of January 2003, there were 18,881 participants enrolled in this trial, and results are not expected until 2012. Further information on the SELECT trial can be found at the following Web sites: http://www.crab.org/select and http://www.cancer.gov/select. Vitamin D induces bile acid breakdown in vitro and may have a role in protection against colon cancer. This effect will need in vivo evaluation.
Tamoxifen
Tamoxifen is a selective estrogen receptor modulator (SERM) with both antiestrogen and proestrogen activity
P.1652
that has an important role in the treatment of both early and advanced breast cancer. Studies of women taking tamoxifen as adjuvant therapy for unilateral breast cancer have shown a 30–40% reduction in the risk of developing a second primary in the opposite breast. The Breast Cancer Prevention Trial (BCPT) is a nationwide trial that randomized 13,400 women at high risk for breast cancer to receive either tamoxifen (20 mg/d) or placebo for 5 years. The trial was stopped at a median follow-up of 4 years due to a striking 50% reduction in the risk of breast cancer in the women taking tamoxifen—89 women taking tamoxifen developed breast cancer, compared with 175 taking placebo. This benefit was restricted solely to the development of estrogen-receptor-positive cancers. In addition to invasive cancer, there was a similar reduction in the risk of noninvasive breast cancer such as ductal or lobular carcinoma in situ. Tamoxifen also decreased the number of bone fractures. Two much smaller European studies that used different parameters to determine risk (and study eligibility) did not show a significant reduction in cancers with the use of tamoxifen. It is likely that tamoxifen is not as effective in preventing breast cancer in very high-risk groups, ie, those with genetic predispositions. Side effects of tamoxifen include an age-dependent small increase in the risk of endometrial cancer (including sarcoma of the uterus), deep vein thrombosis, and pulmonary embolism. These side effects are seen primarily in women over age 50 years.
The use of tamoxifen for primary prevention of cancer is controversial because of its known secondary effects, mainly the increase in endometrial cancer. This risk is small when compared with the incidence of breast cancer in younger women on placebo in the trial. Even if the incidences of endometrial cancer and breast cancer are considered together, there was still a 30% reduction in the risk of cancer in the women receiving tamoxifen. Alternatives to tamoxifen (and raloxifene) are under study; these agents (aromatase inhibitors) are likely to be more effective with a different side effect profile as well (see ongoing trials, below).
Raloxifene
Early results of the Multiple Outcomes of Raloxifene Evaluation (MORE) trial have provided more information regarding prevention of breast cancer. Raloxifene is a novel SERM with estrogenic effects on bone and lipids and estrogen antagonist effects on the breast and uterus. Two different doses of raloxifene or placebo were administered to 7700 postmenopausal women to test the hypothesis that raloxifene would reduce the risk of bone fractures. After 2.5 years, a 70% reduction in the risk of breast cancer was found in the women taking raloxifene compared with the women taking placebo. A suggestion of decreased risk of endometrial cancer was also found. The long-term safety and follow-up of raloxifene in these women are ongoing. The effects of raloxifene in women with breast cancer or in women at high risk for developing breast cancer have not been evaluated (see below). Raloxifene should not be combined with tamoxifen, or used for the treatment of osteoporosis in women on hormonal therapy for breast cancer.
Ongoing Trials in Breast Cancer
The Study of Tamoxifen and Raloxifene (STAR) is designed to determine whether raloxifene is as effective as tamoxifen at reducing the risk for breast cancer. The trial opened in 1999 and closed to enrollment in 2004 after randomizing 19,000 American and Canadian postmenopausal women who are at least 35 years of age and who are at increased risk of breast cancer to either daily tamoxifen (20 mg/d) or raloxifene (60 mg/d) for 5 years. Initial results are projected to be available in the summer of 2006. Additional information regarding the STAR trial as well as other studies on breast cancer can be found at the NCI clinical trials Web site (http://www.cancer.gov/clinical_trials) or by calling 800-4-CANCER. At the prevention Web site (http://www.breastcancerprevention.org), a link is provided to permit calculation of the risk for an individual patient of developing breast cancer and determining eligibility for the trial.
A new class of hormonal agents is now in early clinical trials for primary prevention. The aromatase inhibitors block the peripheral conversion of androstenedione and testosterone to estradiol in menopausal women and are effective in the treatment of earlyand late-stage breast cancer. There is significant variability in tissue estradiol levels in postmenopausal women, and the aromatase inhibitors block the tissue production of estrogen that is thought to play an important role in the development of postmenopausal breast cancer. Data from a number of adjuvant hormonal therapy trials indicate that the aromatase inhibitors have a potent effect in the prevention of new breast cancers in women with previously diagnosed invasive cancer.
The aromatase inhibitors do not appear to cause either an increased risk of thrombosis or endometrial cancer, making them much more suitable agents for prevention in a healthy population. The primary side effects include accelerated loss of bone mineral density, joint and muscle aches, and an altered lipid profile. These agents are active only in postmenopausal women, as they do not suppress estrogen production from the ovary. Ongoing trials targeting women at high risk of developing breast cancer, postmenopausal women with BRCA mutations, and women with a diagnosis of ductal carcinoma in situ are comparing the different aromatase inhibitors to each other, or to tamoxifen. Further follow-up and results from these trials will be needed to understand the impact of aromatase inhibitors in the area of prevention as well as their long-term side effects.
Isoflavones
Isoflavones are found in a variety of natural substances, including soy. Laboratory studies have shown that isofla-
P.1653
vones such as those found in soy inhibit the growth of breast cancer cell lines; however, epidemiologic studies evaluating consumption of isoflavone-containing foods have shown inconsistent results. The Japan Public Health Center-based Prospective Study on Cancer and Cardiovascular Diseases enrolled almost 22,000 Japanese women between the ages of 40 and 59 years. The risk of breast cancer in women who consumed three or more bowls of miso soup daily containing over 25 mg of genistein was 50% less than the risk in women who consumed less than one bowl (about 7 mg genistein), and this effect was greatest among postmenopausal women. Interestingly, consumption of other foods containing soy—soybeans, tofus, etc—was not associated with a reduction in risk of breast cancer. Further trials, including trials in white women who have a higher baseline risk of breast cancer, are required to confirm this interesting observation.
Finasteride
Finasteride is a 5α-reductase inhibitor used to treat benign prostatic hyperplasia. This agent inhibits the enzyme responsible for converting testosterone to 5α-dihydrotestosterone, suppressing prostate cell and organ growth. In rats, finasteride prevented macroscopic but not microscopic prostate carcinogenesis—supporting the use of this agent in the prevention of conversion of latent prostate carcinoma to life-threatening disease. The Prostate Cancer Prevention Trial (PCPT) randomized 18,000 healthy men aged 55 years or older with normal digital rectal examinations and prostate-specific antigen (PSA) concentrations to finasteride or placebo. The trial was closed a year before its planned completion in response to the documented strength of the reduction in prostate cancer in the treatment arm. There was a 25% reduction in the incidence of prostate cancer in the treatment arm, with absolute rates of 18% versus 24% in the placebo arm. This corresponds to 15 less cancers in 1000 older men. Interestingly—and similar to results seen in prevention trials targeting breast cancer with tamoxifen—more high-grade tumors were seen in the finasteride group (37%) than in the placebo-treated men (22%). Although there was enthusiasm about these data—supporting manipulation of androgen levels as a way of preventing prostate cancer—caution was advised in the use of finasteride across the board. There are no survival data from the PCPT as yet, and it is not clear that the tumors prevented in this trial posed a significant threat to life or health. However, finasteride may be a reasonable preventive option for men with a high risk of prostate cancer until additional data are obtained. Side effects from finasteride, given at a dose of 5 mg by mouth every day, include reduced libido and improved ability to urinate in men with prostatic hyperplasia (the current approved use of this drug).
Other Current Trials
Additional trials are underway investigating the effect of both diet and pharmacologic agents in the prevention of cancer. These include studies of folic acid, dietary fat and fish oils, vitamin supplementation, and others. Dietary agents such as polyprenols in green tea are thought to play a role in chemoprevention and are under investigation. There is great interest in moving the new biologic therapies that target specific pathways important in carcinogenesis into the prevention setting. These include farnesyl transferase inhibitors and agents that block the EGFR.
A recent case-control study of 300,000 residents in Europe found a 20% reduction in cancer risk in those taking cholesterol-lowering statin drugs. Data were adjusted for diabetes mellitus, hospitalizations, comorbidities, use of other medications, and sex hormone levels. When specific cancer rates were analyzed separately, reductions in risk were significant only for prostate cancer and renal carcinoma since the rates of other cancers were too low to show significance. Only people who took statins for more than 4 years had a significant 36% reduction in cancer risk, and an increase in cumulative dose also appeared to have a protective effect. The majority of patients took simvastatin as their cholesterollowering agent. A second prospective study evaluated the incidence of breast cancer in 7528 white women with a mean age of 77 years in the United States, 7.7% of whom reported using lipid-lowering drugs; patients were followed for almost 7 years. A marked reduction in the rate of breast cancers was found in women reporting statin use, with a 72% reduction in risk. Women taking any lipid-lowering drug had a 68% reduction in risk, even when results were adjusted for known breast cancer risk factors. Inhibition of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase reduces endogenous production of mevalonate, resulting eventually in decreased biologic activity of several oncogenes, including ras. These data are preliminary but intriguing; future studies must also control for important risk factors such as smoking and diet. Two prospective prevention trials are planned to start in the near future, investigating the use of statins to prevent progression of in situ cancer of the breast to invasive disease.
Further information about ongoing chemoprevention trials can be obtained from the Chemoprevention Branch of the National Cancer Institute (301-496-8563) and at http://www.cancer.gov/prevention/. An excellent article summarizing ongoing prevention and early detection trials, including eligibility, risks, and contact information, is available at http://www.CAonline.AmCancerSoc.org.
Ford LG et al: Prevention and early detection clinical trials: opportunities for primary care providers and their patients. CA Cancer J Clin 2003;53:82.
Hawk ET et al: Colorectal cancer chemoprevention—an overview of the science. Gastroenterology 2004;126:1423.
Holick CN et al: Dietary carotenoids, serum beta-carotene, and retinol and risk of lung cancer in the alpha-tocopherol, betacarotene cohort study. Am J Epidemiol 2002;156:536.
Klein EA et al: SELECT: the selenium and vitamin E cancer prevention trial. Urol Oncol 2003;21:59.
P.1654
Lamprecht SA et al: Chemoprevention of colon cancer by calcium, vitamin D and folate: molecular mechanisms. Nat Rev Cancer 2003;3:601.
Leach R et al: Chemoprevention of prostate cancer. Focus on key opportunities and clinical trials. Urol Clin North Am 2003;30:227.
Rao CV et al: NSAIDs and chemoprevention. Curr Cancer Drug Targets 2004;4:29.
Rhee JC et al: Advances in chemoprevention of head and neck cancer. Oncologist 2004;9:302.
Serrano D et al: Progress in chemoprevention of breast cancer. Crit Rev Oncol Hematol 2004;49:109.
Thompson IM et al: The influence of finasteride on the development of prostate cancer. N Engl J Med 2003;349:213.
Tsao AS et al: Chemoprevention of cancer. CA Cancer J Clin 2004;54:150.
SECONDARY PREVENTION (Early Detection)
Given the inadequacy of current knowledge concerning the causes of cancer, effective prevention can be achieved for only a minority of malignancies. Other than primary prevention and perhaps chemoprevention, the most effective clinician intervention is early diagnosis. Screening is used for early detection of cancer in otherwise asymptomatic populations. Detection of cancer may be achieved through observation (eg, skin, mouth, external genitalia, cervix), palpation (eg, breast, mouth, thyroid, rectum and anus, prostate, testes, ovaries and uterus, lymph nodes), and laboratory tests and procedures (eg, Papanicolaou smear, sigmoidoscopy or colonoscopy, mammography). Effective screening requires a test that will specifically detect early cancers or premalignancies, be cost effective, and result in improved therapeutic outcomes. For most cancers, stage at presentation is related to curability, with the highest cure rates reported when the tumor is small and there is no evidence of metastasis. However, for some tumors (eg, lung or ovarian cancer), distant metastases tend to occur early, even from a small primary tumor. More sensitive detection methods such as tumor markers are being developed for many forms of cancer. Some tumor markers, such as PSA, are already a regular (though controversial) part of routine cancer screening (see section on tumor markers). Screening is not useful if a method of early detection does not exist (eg, cancer of the pancreas) or if there is no apparent localized stage (eg, leukemia). Current guidelines for cancer screening from the American Cancer Society can be found on line at http://www.CAonline.AmCancerSoc.org in the January/February 2003 issue, and are updated regularly at http://www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp and in Table 1-9. These recommendations include general cancer-related check-ups as well as screening for cancers of the prostate, breast, colorectum, and cervix.
Cancers for which screening or early detection has led to an improvement in outcome include cancers of the breast, cervix, colon, prostate, oral cavity, and skin. Ongoing trials are evaluating the use of newer screening methods for the most common malignancies, including cancers of the breast, lung, and prostate as well as colorectal and ovarian cancers.
It is critical that clinicians involve patients in decisions about whether to order tests for early detection of breast and prostate cancers so that patients will understand the risks and benefits. The rates of routine cancer screening in the United States remain low, with less than 50% having recent screening for colorectal cancer and less than 60% having recent mammography and clinical breast examination. Data from the WHI Observational Study cohort, which represents a large and diverse group of older women, indicate that health insurance is among the most important determinants of cancer screening independent of other factors. Improving insurance coverage of screening and access to health insurance for older adults in the United States may have an important role in improving early detection of cancer through screening. Screening is underutilized in minority groups in the United States, especially in inner city and rural areas. This results in the diagnosis of cancers at more advanced stages. Educational and outreach programs should be directed at these underserved areas.
Screening for Breast Cancer
Techniques for early detection of breast cancer include self-examination, clinical examination, and mammography. The benefits of screening mammography have been reviewed in two large meta-analyses and these results remain controversial based on a number of factors. First, several of the large published studies evaluating the value of mammography have serious flaws. Second, mammography increases the detection of the preinvasive ductal carcinoma in situ (DCIS), which has an extremely low 10-year mortality. Lastly, available data suggest that the most significant reduction in mortality obtained from mammographic screening may be in women over the age of 60 years (24–33% reduction), with smaller benefits in younger women. The Agency for Healthcare Research and Quality (AHRQ) conducted its own review of the meta-analysis and rated the included studies based on the quality of data and the inclusion of younger age groups as well as other factors. They concluded that there is a demonstrated 20% reduction in the number of deaths from breast cancer in women undergoing screening mammography both in the over-50 and under-50 year age groups, though the times required in follow-up to see these benefits may be quite different. The AHRQ—along with the American Cancer Society (ACS) and the NCI—have put forth the following recommendations for mammographic screening: Every 1–2 years for women between the ages of 40 and 49 years, then annually in women 50 years and older. The upper age limit for mammographic screening has not been established.
Both mammography and clinical examination of the breast are associated with a significant number of false-positive results, leading to further testing. Screening mammograms and clinical breast examinations in
P.1655
2400 women over a 10-year period found that 24% and 13%, respectively, of women had at least one false-positive mammogram or false-positive clinical examination. The controversy regarding mammographic screening is thus far from resolved; however, it is the best screening method currently available. Women between the ages of 40 and 49 years should be active participants in decisions regarding screening and should have an understanding of known risks and benefits. Despite the sensitivity of mammography, between 15% and 25% of breast cancers are not visible by this radiographic technique; this is particularly true for young women with dense breasts. All clinically suspicious lesions should be biopsied regardless of a negative mammogram.
Digital mammography is a newer technique that uses computers and special detectors to produce a digital image displayed on high-resolution monitors. The NCI launched the Digital Mammographic Imaging Screening Trial (DMIST) in October 2001 to determine if digital mammography is as good as or better than standard screen (x-ray) mammography with regard to sensitivity, specificity, and predictive values. Overall, 49,500 women in the United States and Canada entered this trial, which is now closed to enrollment, and all women will have both types of radiographic screening at study entry and at 1 year with 2 years of followup. Initial results should be available in late 2005. Further information about the DMIST can be found at http://www.cancer.gov/DMIST or http://www.dmist.org.
Magnetic resonance imaging (MRI) screening of the breast appears to be a useful technique in women at very high risk for developing breast cancer. This highly sensitive test is unfortunately not very specific, leading to unnecessary biopsies. It is currently of value only in very high-risk women when regular screening might not be sensitive enough to detect breast cancer.
The value of clinical breast examination for the early detection of breast cancer remains unclear. A large study in China found no benefit in survival in women trained to perform monthly examinations; however, these data may not apply to the U.S. population for a variety of reasons. At this time, screening guidelines include monthly breast self-examination as well as yearly mammography.
Screening for Lung Cancer
It is clear that current and former smokers are at high risk of developing lung cancer and that early detection of lung cancer may result in detection of lesions when they are still surgically resectable and, therefore, potentially curable. However, data available so far are inconclusive as to whether either chest x-rays or the more sensitive computed tomography (CT) scan can reduce lung cancer mortality. The National Lung Screening Trial (NLST) is a large randomized trial designed to determine whether lung cancer mortality is reduced in long-term or heavy current and former smokers by screening with chest x-ray versus spiral CT. The trial, which opened in September 2002, enrolled 50,000 participants as of February 2004, included men and women in good health between the ages of 55 and 74, and is now closed to enrollment. Spiral CT or chest x-ray is performed once a year for 3 years. Interim results are hoped for in 2006; the study will continue until 2009. Further information regarding the NLST can be found at http://www.cancer.gov/nlst and at http://www.cancer.org.
Screening for Cervical Cancer
Regular screening for cervical cancer (every 3 years in standard risk groups) with Papanicolaou tests has been found to decrease the mortality rate in women who are sexually active or are 18 years of age or older. Testing for HPV DNA in high-risk populations may improve early detection and management of cervical cancer, helping to determine which women with low-grade cytologic abnormalities require colposcopic evaluation. Recent data indicate that screening every 2 years with both Papanicolaou and HPV testing is more cost effective than screening with either test alone. A large German study found that HPV testing was a highly sensitive method for detecting high-grade cervical intraepithelial neoplasia (CIN), suggesting that routine HPV testing might be of value in higher-risk women. Self-collected vaginal swabs for DNA testing may improve screening in areas where cytologic study is not readily available or in populations in which women are hesitant to undergo regular examinations. The ACS has updated its screening guidelines to include HPV DNA testing in high-risk individuals. Routine screening with vaginal Papanicolaou smears in women who have previously undergone a hysterectomy for benign gynecologic disease is not useful because of the very low incidence of squamous cell cancers of the vagina.
Screening for Colorectal Cancer
Annual fecal occult blood testing and screening with sigmoidoscopy every 5 years in people over age 50 years decreases the mortality rate from colorectal cancer. An evaluation of over 46,000 people aged 50–80 years in the Minnesota Colon Cancer Control study over an 18-year follow-up period showed that either annual or biennial screening of two stool samples significantly reduced the incidence of colorectal cancer when an abnormal fecal blood screen was followed by colonoscopy. Removing polyps detected by colonoscopy reduces the risk of colorectal cancer, and, following polypectomy, colonoscopy is superior to double-contrast barium enema for the detection of recurrent polyps. Even adenomatous polyps 5 mm or less in diameter detected in the rectosigmoid by sigmoidoscopy are markers for more advanced proximal neoplasms. These patients should undergo colonoscopy to evaluate the proximal bowel. However, colonoscopic screening can detect advanced colonic neoplasms in asymptomatic adults even in the absence of distal adenomas. Regular fecal occult blood testing and flexible sig-
P.1656
moidoscopy are still recommended for general screening because of the lower cost and facility of sigmoidoscopy compared with colonoscopy. Computed tomographic “virtual” colonoscopy is a new technique used to screen for colorectal neoplasia. A small rectal catheter is used to introduce air into the colon, then CT scanning is performed while the patient is supine and prone. Image processing allows image interpretation of the air-filled colon. This controversial imaging modality is nonetheless appealing to patients and less invasive; skilled interpretation and state of the art equipment are required. Further data will be required to fully validate the sensitivity and specificity of virtual colonoscopy. A novel test to examine stool for DNA alterations that might help to screen for colorectal cancer is in development.
The Prostate, Lung, Colorectal, & Ovarian (PLCO) Cancer Screening Trial
The PLCO Cancer Screening Trial is a large cancer screening study that was opened between 1992 and 2001 and randomized over 154,000 healthy men and women between the ages of 55 and 74 years to routine health care versus prescribed screening. The goal of this study is to determine the effect of cancer screening tests on sitespecific cancer mortality. Screening will occur for a total of 6 years, with 10 years of follow-up. Screening tests include PSA annually for 6 years; digital rectal examination (DRE) annually for 4 years; chest x-ray annually for 4 years in smokers and for 3 years in never-smokers; sigmoidoscopy at entry and then after 3 or 5 years on study (see below); transvaginal ultrasound annually for 4 years; and CA 125 (an ovarian cancer tumor marker; see section on tumor markers) annually for 6 years. Preliminary results are available on the role of sigmoidoscopy repeated at a 3-year interval in 9317 participants. A polyp or growth was detected in 13.9%, with 3.1% having a distal colon advanced adenoma or cancer—in an area that had been carefully evaluated 3 years earlier. These data suggest that higher-risk patients might benefit from more frequent sigmoidoscopic screening, though there are no data on mortality at this time. Additional data on the role of the PSA test in prostate cancer screening is discussed below.
Screening for Other Cancers
Unfortunately, screening for ovarian cancer with serum markers (eg, CA 125), transvaginal ultrasound, or pelvic examinations has not been shown to decrease the mortality rate from this disease. The PLCO trial should help to assess the impact of combined markers and ultrasound on both detection and mortality for this difficult disease. Screening for prostate cancer and hepatocellular cancer is discussed in the section on tumor markers; prostate cancer is evaluated in the PLCO trial (see above).
Bach PB et al: Screening for lung cancer: the guidelines. Chest 2003;123(1 Suppl):83S.
Ball C et al: Update on cervical cancer screening. Current diagnostic and evidence-based management protocols. Postgrad Med 2003;113:59.
Nystrom L et al: Long-term effects of mammography screening: updated overview of the Swedish randomized trials. Lancet 2002;359:909.
Pickhardt PJ et al: Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med 2003;349:2191.
Saslow D et al: American Cancer Society guidelines for the early detection of cervical neoplasia and cancer. CA Cancer J Clin 2003;52:342.
Sawaya GF et al: Current approaches to cervical cancer screening. N Engl J Med 2001;344:1603.
Schoen RE et al: Results of repeat sigmoidoscopy 3 years after a negative examination. JAMA 2003;290:41.
Segnan N et al: Randomized trial of different screening strategies for colorectal cancer: patient response and detection rates. J Natl Cancer Inst 2005;97:347.
Smith RA et al: American Cancer Society guidelines for breast cancer screening: Update 2003. CA Cancer J Clin 2003;54:141.
Smith RA et al: American Cancer Society guidelines for the early detection of cancer, 2003. CA Cancer J Clin 2003;53:27.
Subramanian S et al: Use of colonoscopy for colorectal cancer screening: evidence from the 2000 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev 2005;14:409.
SPECIAL TOPICS IN PREVENTION
Patients with a family history of colorectal cancer are at increased risk to develop this disease and should undergo regular screening, which clearly reduces the incidence and mortality from invasive cancer. Guidelines for patients with a risk of hereditary nonpolyposis colon cancer are referenced below.
Approximately 10% of breast and ovarian cancers are due to inherited genetic mutations, occurring primarily in women with mutations of BRCA1 and BRCA2. Patients with a family history of breast or ovarian cancer are at higher risk to develop these cancers and require frequent monitoring for early detection, though screening is inadequate to detect early ovarian cancer. Women with a family history of premenopausal or bilateral breast cancer—or any family history of ovarian cancer—should be referred for genetic counseling to better assess their risk of carrying one of the known mutations.
Prophylactic oophorectomy after completion of childbearing can significantly decrease the risk of ovarian cancer in women with BRCA1 and BRCA2 mutations; there is still a small risk of peritoneal cystadenocarcinoma. The actual risk reduction in a recent small prospective trial was 96%, similar to results from the Prevention and Observation of Surgical Endpoints (PROSE) study group and significantly higher than women electing intensive surveillance. In addition, bilateral prophylactic oophorectomy reduces the risk of subsequent breast cancer in high-risk women by 50–75%, presumably because of decreased exposure to
P.1657
ovarian estrogens. Oral contraceptive use for 6 years or more decreased the risk of ovarian cancer by as much as 60% in women with a family history of ovarian cancer. Prophylactic mastectomy has been used for decades to reduce the risk of breast cancer in high-risk women and is associated with a substantial reduction in breast cancer risk. In women at both high and moderate risk of breast cancer based on family history, the incidence of breast cancer (and death from breast cancer) is reduced by up to 99%. Decisions about such prophylactic surgery in high-risk women must be made taking full account of many other factors— breast or ovarian cancer will develop in most but not all women with BRCA mutations.
Any patient with a history of dysplasia or premalignant lesions is at high risk for development of invasive cancer and should undergo frequent and thorough screening for subsequent malignancy. Patients at a particularly high individual risk for cancer may require additional screening procedures. Enthusiasm about the ability of spiral CT to image early lung cancers has reawakened interest in screening high-risk individuals with the goal of reducing lung cancer mortality with detection of early, treatable lesions. Randomized trials are ongoing (see above) to investigate whether screening for lung cancer with this expensive test can actually reduce mortality rates. At present, general guidelines are to consider routine chest x-ray screening on an annual basis for heavy current or former smokers (more than 20 pack-years) over the age of 55 years.
Cruz-Correa M et al: Diagnosis and management of hereditary colon cancer. Gastroenterol Clin North Am 2002;31:537.
Deligeoroglou E et al: Oral contraceptives and reproductive system cancer. Ann NY Acad Sci 2003;997:199.
Hampel H et al: Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. J Med Genet 2004;41:81.
Kauff ND et al: Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 2002;346: 1609.
Mulshine JL et al: Lung cancer. 2: screening and early diagnosis of lung cancer. Thorax 2002;57:1071.
Rebbeck TR et al: Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 2002;346: 1616.
STAGING OF CANCER
Standardized staging for tumor burden at the time of diagnosis is important both for determining prognosis and for making decisions about treatment. The American Joint Committee on Cancer (AJCC) has developed a simple classification scheme that can be incorporated into a form for staging and universally applied. This scheme is designed to encompass the life history of a tumor and is referred to as the TNM system. The untreated primary tumor (T) will gradually increase in size, leading to regional lymph node involvement (N) and, finally, distant metastases (M). The tumor is usually not clinically evident until local invasion or even spread to regional draining lymph nodes has occurred.
TNM staging is used clinically to indicate the extension of cancer before definitive therapy begins. The manner in which staging is accomplished—eg, by clinical examination or pathologic examination of a surgical specimen—must be carefully documented. Certain types of tumors, such as lymphomas and Hodgkin's disease, are usually staged by a different classification scheme that reflects the natural history of this type of tumor spread and helps to direct treatment decisions.
The TNM system allows a numerical assessment of the extent of primary tumor (T), the absence or presence and extent of regional lymph node metastases (N), and the absence or presence of distant metastases (M). The AJCC has just published a new version of the TNM staging criteria with major revisions directed toward providing a standardized method for classifying the extent of cancer at diagnosis and estimating the risk of recurrence and death from cancer. Examples of changes in staging included in the new system are staging melanoma based on the thickness and ulceration of the lesion instead of the level of invasion and the stratification of breast cancer stage based on the number of involved axillary nodes. Based on data that indicate prolonged survival in breast cancer patients with a single involved ipsilateral supraclavicular node, this presentation is now staged as stage IIIb rather than stage IV. The new staging system took effect internationally in January 2003 and is a required part of medical records for all cancer patients. Details regarding these revisions may be found at the AJCC Web site: http://www.cancerstaging.net.
Traditional staging does not take into account the biology or aggressiveness of a particular tumor and may not allow differentiation of prognostic risk groups. For this reason, specific pathologic characteristics are added into the prognostic evaluation for certain tumors (eg, estrogen and progesterone receptors, grade and proliferative index for breast cancer; histologic grade for sarcomas and the majority of adenocarcinomas). Overexpression or underproduction of oncogene products (eg, HER-2/neu in breast cancer), infection of cancer cells with specific viral genomes (eg, HPV-18 in cervical cancer), and certain chromosomal translocations or deletions (eg, alteration of the retinoic acid receptor gene in acute promyelocytic leukemia) have important prognostic significance and may direct riskadapted or cancer-specific therapy. As these characteristics become standardized and better understood, they may allow us to identify patients with a poorer prognosis early in the course of disease when the patient might benefit from more aggressive therapy. In addition, characterizing cancers with genetic profiling or proteomics may completely change our concept of cancer staging in the future.
P.1658
Greene FL et al (editors): AJCC Cancer Staging Manual, 6th ed. Springer, 2002.
PRIMARY CANCER TREATMENT
The reader is referred to the National Comprehensive Cancer Network (NCCN) Oncology Practice Guidelines: http://www.cancernet.com. These guidelines are updated yearly.
SURGERY & RADIATION THERAPY
Most cancers present initially as localized tumor nodules and cause local symptoms. Depending on the type of cancer, initial therapy may be directed locally in the form of surgery or radiation therapy. Surgical excision or local radiation (or both) is the treatment of choice for a variety of potentially curable cancers, including most gastrointestinal and genitourinary cancers, central nervous system tumors, and cancers arising from the breast, thyroid, or skin as well as most sarcomas.
Surgery at presentation has both diagnostic and therapeutic effectiveness, since it permits pathologic staging of the extent of local and regional invasion as well as an opportunity for removal of the primary neoplasm. CT and MRI play an increasing role in noninvasive tumor staging. Based on results of a prospective clinical trial, positron emission tomography (PET) appears to be a more sensitive method than traditional imaging with CT scanning for detecting local and distant metastases in patients with non-small cell lung cancer. The effect on survival is unknown. One way to improve the specificity and sensitivity of these scans is to integrate the PET and CT images with computer technology rather than the traditional visual correlation. A recent study evaluated integrated PET-CT in 50 patients with non-small cell lung cancer. Additional information was obtained on 41% of patients compared with visual correlation; this included improved tumor staging, detection of involved nodes, and certainty of metastases. PET has also been shown to improve detection of recurrent disease for the purpose of second-look laparotomy and debulking in colon cancer patients with rising levels of carcinoembryonic antigen (CEA).
A monoclonal antibody against CEA labeled with technetium-99m (arcitumomab, CEA-Scan) is now approved for imaging of cancers with increased levels of CEA and has been found to be more sensitive and specific than CT scans in the detection of both resectable and nonresectable disease. High-resolution MRI scanning with highly lymphotropic superparamagnetic nanoparticles may improve radiographic detection of occult lymph node metastases in patients with prostate cancer. The nanoparticles gain access to lymph nodes by means of interstitial-lymphatic fluid transport. Eighty patients with prostate cancer were evaluated before surgery; MRI with nanoparticles correctly identified all patients with nodal metastases, compared with a detection rate of only 30% using standard imaging. These newer, more sensitive (and much more expensive) scans may allow better assessment of resectability before surgery, sparing patients needless surgery but also providing appropriate surgery when cure with local treatment alone is possible. The best and most cost-effective use of these techniques remain to be determined.
Although standard surgery for breast cancer has included excision of axillary nodes, this can result in chronic lymphedema, pain, and decreased range of motion of the arm. Sentinel axillary nodes can be detected by injection of radioactive colloid or blue dye into the breast around the tumor or the biopsy cavity. “Hot spots” are then identified with a gamma probe and resected. Biopsy of sentinel nodes can predict the presence or absence of axillary node metastases and direct more aggressive surgery with up to 97% accuracy. However, the procedure is technically challenging and the success rate thus varies with the surgeon. This technique is also used for staging of malignant melanoma. Cryosurgical ablation of localized prostate cancers has been used instead of radiotherapy by some investigators and appears to reduce postablation voiding dysfunction. Radiofrequency ablation (frictional heating) and cryosurgical ablation are being tested as primary treatment of small, localized breast cancers.
Surgery may also play an important role in the treatment of selected patients with limited metastatic cancer. Resection of isolated metastases has been used most commonly for breast cancer with single brain lesions or isolated liver or lung lesions. Removal of isolated liver metastases may result in long-term survival, with 20% of patients living more than 5 years. Additional surgery after subsequent limited recurrence may also result in long-term disease-free survival. Surgical resection of both hepatic and pulmonary metastases may improve survival in appropriately selected colon cancer patients.
For certain tumor sites, complete surgical removal of the tumor can be disfiguring, disabling, or unachievable. Under those circumstances, primary local therapy with ionizing radiation may prove to be the treatment of choice. In other instances, surgery and radiation therapy are used in sequence. For stage I and stage II breast cancer, local excision or “lumpectomy” with axillary node sampling combined with radiation results in equivalent 10-year survivals when compared with the more disfiguring mastectomy procedure. Despite these well-established data, breast-conserving therapy is still underused in patients with larger tumors, mainly because of surgeon bias and lack of technical skill. Preoperative or “neoadjuvant” chemotherapy and radiation therapy allow limb-sparing surgery in osteosarcoma and organ preservation in oropharyngeal cancer, among others. Laser surgery is used to
P.1659
minimize surgical resection in esophageal and nonsmall cell lung cancers.
Radiation therapy is usually delivered as brachytherapy or teletherapy. In brachytherapy, the radiation source is placed close to the tumor. This intracavitary approach is used for many gynecologic or oral neoplasms and occasionally for breast cancer. In teletherapy, supervoltage radiotherapy is usually delivered with a linear accelerator, as this instrument permits more precise beam localization and avoids the complication of skin radiation toxicity. Various beam-modifying wedges, rotational techniques, and other specific approaches are used to increase the radiation dosage to the tumor bed while minimizing toxicity to adjacent normal tissues. Changes in dosing schedules have been used to either improve response or minimize long-term toxicity, although few data exist on the effectiveness of these approaches. For example, twice-daily radiation to the breast over 2 weeks is being compared to the standard 6-week daily dosing schedule, and radiation to the whole brain is often given in smaller doses over 4 weeks rather than the standard 2-week schedule to reduce long-term cognitive effects. Examples of new approaches to minimize radiation to surrounding tissues while maximizing radiation to the cancer include three-dimensional-conformal radiation therapy (3D CRT) and intensity modulated radiation therapy (IMRT). Conventional radiation beams are of uniform intensity. In contrast, IMRT's beam intensity is modulated to produce maximum doses where desired and minimal radiation to sensitive surrounding normal tissues. Improved outcomes have been shown for prostate cancer patients receiving IMRT.
Novel modalities are occasionally used to enhance penetrance into large tumors or to specifically target the site of radiation. Gamma knife radiosurgery allows focused radiation for limited brain metastases and is associated with fewer long-term complications such as cognitive dysfunction compared with whole brain irradiation. It also extends treatment options for patients with isolated brain recurrences following whole brain radiation. Cyberknife is a newer radiosurgical technique designed to perform tumor ablation in any site in the body. This unique system combines robotics and advanced image guidance to deliver radiosurgery treatment to tumors along the spinal cord or at other critical locations previously considered untreatable with surgery or radiation. It can also be used to treat recurrences in a previously radiated site or to boost standard radiotherapy.
Well-oxygenated tumors are more radiosensitive than hypoxic ones. Hypoxic tumors are often bulky, implying a potential synergistic role of surgical debulking prior to radiotherapy. Radiation therapy is normally delivered in a fractionated fashion over 4–6 weeks, this method appearing to have radiobiologic superiority by permitting time for recovery of normal host tissues (but not the tumor) from sublethal damage during treatment. However, a more accelerated fraction radiation schedule improves local-regional control in patients with head and neck cancer compared with standard fractionated radiation. Efaproxiral (RSR13) binds to hemoglobin and reduces oxygen-binding affinity (allosteric modification), enhancing oxygen unloading from hemoglobin to hypoxic tissue, potentially enhancing the effectiveness of radiation therapy. Clinical trials have demonstrated a possible improvement in response and survival in patients with primary brain tumors when patients are given efaproxiral during whole brain radiation therapy, compared to historic controls. Ongoing randomized trials are testing the efficacy of efaproxiral in patients with primary and metastatic tumors to the brain. The primary toxicity of this agent is hypoxia; patients require close monitoring and supplemental oxygen following therapy.
For most tumor types, there is a sigmoid curve of increasing rate of control of the local tumor with increasing radiation dose. Radiosensitive tumors usually exhibit radiosensitivity over the dose range of 3500–5000 cGy.
Currently, more than 50% of all patients with cancer receive radiation therapy during the course of their illness. Radiation therapy is frequently the sole agent used with curative intent for tumors of the larynx (permitting cure without loss of the voice), oral cavity, pharynx, esophagus, uterine cervix, vagina, prostate, and skin, Hodgkin's disease, and some tumors of the brain and spinal cord. For more extensive cancers, radiation is combined with surgery (eg, cancer of the breast, ovary, uterus, cervix, urinary bladder, rectum, and lung, soft tissue sarcomas, and seminoma of the testis). Following mastectomy for breast cancer, radiation has been shown to reduce the risk of local recurrence from large or high-risk tumors and may increase overall survival by decreasing distant recurrence.
Radiation given in combination with chemotherapy may improve long-term disease control. The combination of chemotherapy and radiation therapy for the treatment of invasive carcinoma of the cervix is significantly superior to radiation therapy alone. There is at least a 10% improvement in 3-year survival and a 30–50% reduction in the risk of death from cervical cancer with combination therapy. Twice-daily radiation given concurrently with combination chemotherapy for the treatment of limited small cell lung cancer results in significantly improved 5-year survival rates compared with any prior treatment results. Twicedaily radiation also appears superior to once-daily treatment for this disease. Radiation combined with chemotherapy for cancer of the rectum or hormone therapy for cancer of the prostate improves survival over treatment with radiation alone, and concurrent radiation and chemotherapy for cancer of the head and neck reduces mortality from that disease compared with either treatment alone. Radiation can also improve disease control when given as an adjuvant to chemotherapy for bulky lymphomas, for non-small cell lung cancer, and for some cancers in children.
Occasionally, chemotherapy is used to sensitize tumor cells to the toxic effects of radiation. Radiation
P.1660
therapy for palliation of pain or dysfunction (eg, bone pain associated with advanced breast or other cancers) may improve the quality of life of patients suffering from incurable malignancies. Radiation therapy to lytic lesions of the bone can reduce the risk of fracture as well.
Various normal tissues (particularly skin, mucosa, myocardium, spinal cord, bone marrow, and lymphoid system) can exhibit early or late toxicity from radiation therapy. Acute toxicity may include generalized fatigue and malaise, anorexia, nausea and vomiting, local skin changes, diarrhea, and mucosal ulceration of the irradiated area. Radiation of large areas, especially the pelvis and proximal long bones, may result in bone marrow suppression. Radiation of the lungs, heart, and gastrointestinal tract must be approached with appropriate shielding to avoid toxicity such as radiation pneumonitis, congestive heart failure, or radiation gastroenteritis. Long-term toxicity from radiation therapy has significant long-term side effects that must be weighed against its possible benefits. Women under age 60 years treated with left-sided adjuvant radiation for breast cancer with 10–15 years of follow-up have a significant increase in risk of death from myocardial infarction. However, more recent radiation techniques use tangential beams that avoid significant radiation to adjacent organs such as the heart or lung. Increased cardiac mortality has also been seen in patients who received radiation at a young age for Hodgkin's disease. Secondary leukemias and solid tumors can be seen after radiation therapy for a wide variety of cancers. This risk is particularly high in patients receiving a combination of both radiation and chemotherapy that includes alkylating agents. Treatment programs now combine less toxic chemotherapy with limited field radiation therapy to limit these fatal side effects in long-term survivors from cancer. Other long-term toxicities include decreased function of the radiation organ (eg, decreased cognitive function after whole brain radiation), myelopathy, osteonecrosis, and hyperpigmentation of the involved skin.
Regional hyperthermia (40–42 C) is an adjunct to ionizing irradiation for some tumor sites. The most useful application of hyperthermia to date has been in superficial or easily implantable tumors as well as in relatively bulky hypovascular tumors with some degree of hypoxia. Electron beam therapy has been used effectively to treat superficial tumors in the skin. Radiolabeled antibodies are currently under investigation as a means of delivering high levels of radiation locally to the tumor bed, thereby avoiding systemic toxicity. Ibritumomab tiuxetan and tositumomab are the first radiolabeled antibodies to be FDA approved for the treatment of cancer—specifically, relapsed low-grade non-Hodgkin's lymphoma (see section on novel therapies at the end of this chapter).
Increasingly, the primary local therapy of cancer is integrated with systemic therapy, an approach that has proved to be superior for apparently localized tumor types with a high propensity for early metastatic spread and for which anticancer drugs are available.
Bosset JF et al: Preoperative chemoradiotherapy versus preoperative radiotherapy in rectal cancer patients: assessment of acute toxicity and treatment compliance. Report of the 22921 randomised trial conducted by the EORTC radiotherapy group. Eur J Cancer 2004;40:219.
Chao C et al: Update on the use of the sentinel node biopsy in patients with melanoma: who and how. Curr Opin Oncol 2002;14:217.
Choti MA et al: Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 2002;235:759.
Harisingham MG et al: Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med 2003;348:2491.
Lardinois D et al: Staging of non-small-cell lung cancer with integrated positron-emission tomography and computed tomography. N Engl J Med 2003;348:2500.
Moroz P et al: Status of hyperthermia in the treatment of advanced liver cancer. J Surg Oncol 2001;77:259.
Recht A et al: Postmastectomy radiotherapy: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol 2001;19:1539.
Steffan RP et al: Allosteric modification of hemoglobin by RSR13 as a therapeutic strategy. Adv Exp Med Biol 2003;530:249.
SYSTEMIC CANCER THERAPY
Use of cytotoxic drugs, hormones, antihormones, and biologic agents has become a highly specialized and increasingly effective means of treating cancer. Therapy should be administered by a medical oncologist. Selection of specific drugs or protocols for various types of cancer has traditionally been based on results of prior clinical trials. Many patients are treated on protocols to search for optimal therapy for refractory or poorly responsive malignancies. Treatment may be inadequate or ineffective because of drug resistance of the tumor cells. This has been attributed to spontaneous genetic mutations in subpopulations of cancer cells prior to exposure to chemotherapy. After chemotherapy has eliminated the sensitive cells, the resistant subpopulation grows to become the predominant cell type (Goldie–Coldman hypothesis). This has been the basis of alternating non-cross-resistant chemotherapy regimens.
Molecular mechanisms of drug resistance are now the subject of intense study. In many instances, specific drug resistance results from an amplification in the number of gene copies for an enzyme inhibited by a specific chemotherapeutic agent. A more general form of “multidrug resistance” (MDR) has been described in association with expression of a gene (MDR1) encoding a 170-kDa transmembrane glycoprotein (P-glycoprotein) on tumor cells. This protein is an energy-dependent transport pump that facilitates drug efflux from tumor cells and promotes resistance to a broad spectrum of unrelated cancer drugs. Although a variety of agents have been shown to at least partially and temporarily reverse acquired MDR in multiple myeloma and lymphoma, the doses of these agents required to overcome drug resistance are associ-
P.1661
ated with serious side effects. MDR modulators will need to be both less toxic and more potent to be clinically useful. Both improved response rates and improved survival with a tolerable toxicity profile using novel therapy such as this will have to be demonstrated to prove the effectiveness of this approach.
Variation in drug metabolism due to gene polymorphisms is emerging as a cause of relative resistance or sensitivity to chemotherapeutic agents. In one study, women with breast cancer who had single-nucleotide polymorphisms in the CYP3A4 and CYP3A5 genes were not able to metabolize cyclophosphamide and had a significantly shorter survival than women without this polymorphism. Polymorphisms in CYP have also been shown to increase sensitivity to some environmental carcinogens. Genetic variations in the DNA repair genes XPD and XRCC1 may predict response to the chemotherapy drugs cisplatin or carboplatin in lung cancer, with certain variations associated with a shortened survival. With an increased understanding of individual susceptibility or resistance factors, pretreatment evaluation of drug metabolism genes might allow individualization of therapy.
Chemotherapy is used primarily to cure a small percentage of malignancies, as adjuvant therapy to decrease the rate of relapse or improve the disease-free interval, and to palliate symptoms and prolong survival in some patients with incurable malignancies. In addition, chemotherapy is playing an increasing role as preoperative or “neoadjuvant” therapy to reduce the size and extent of the primary tumor, thereby allowing complete excision at the time of surgery. Neoadjuvant (preoperative) chemotherapy results in identical survival when compared with standard postsurgical chemotherapy for breast cancer and allows more limited or complete surgical excision of the primary tumor as well as giving important information about chemosensitivity. Randomized studies now suggest that neoadjuvant chemotherapy may improve survival in patients with esophageal cancer and bladder cancer. Combined neoadjuvant chemotherapy and radiation followed by surgery and additional chemotherapy has been shown to prolong survival in patients with non-small cell lung cancer that has metastasized to mediastinal nodes compared with those who received only chemotherapy and radiation. In addition, survival rates at 3 years exceeded those seen in prior studies. There are two additional benefits to the neoadjuvant approach. First, understanding the clinical response to specific chemotherapeutic agents may allow modification of this treatment in an individual patient to improve response. Second, serial biopsies during treatment along with improved imaging may help us to understand the genes responsible for chemotherapy resistance and sensitivity and hopefully allow for individualization of cancer treatment with combinations of chemotherapy and targeted agents in the future.
Chemotherapy was first shown to be curative in the treatment of advanced stages of choriocarcinoma in women. It is also curative in Hodgkin's disease, diffuse large cell and some high-grade lymphomas (including Burkitt's), carcinoma of the testis, some cases of acute leukemia, and embryonal rhabdomyosarcoma. When combined with initial surgery—and in some instances with irradiation—chemotherapy increases the rate of long-term control and cure of breast cancer, cervical cancer, small cell and non-small cell lung cancer, colon cancer, gastric cancer, esophageal cancer, rectal cancer, and osteogenic sarcomas. Combination chemotherapy provides palliation and prolongation of survival in adults with low-grade non-Hodgkin's lymphoma, mycosis fungoides, multiple myeloma and Waldenstr m's macroglobulinemia, acute and chronic leukemias, and breast, ovarian, cervical, and small cell lung carcinoma as well as carcinoid. Patients with incurable tumors who desire aggressive treatment should be referred for experimental therapy in well-designed clinical trials. (See section on novel therapies at the end of this chapter.)
High-dose chemotherapy followed by bone marrow transplantation is curative therapy for various types of leukemia, high-risk or relapsed lymphoma, and testicular cancer and occasionally multiple myeloma. Allogeneic or autologous bone marrow or peripheral blood stem cells with or without ex vivo purging are used depending on the disease. The use of growth factors and blood stem cells has decreased the toxicity and cost of bone marrow transplantation. Autologous transplantation may now be used with relatively low morbidity and mortality on selected patients up to age 70 years. Dose-intense chemotherapy with autologous bone marrow or peripheral blood stem cell rescue has been extensively studied for the treatment of both high-risk and metastatic breast cancer for the past decade and has shown no apparent benefit over standard therapy and significantly more toxicity and risk of mortality. Details of these studies are presented in the section on adjuvant therapy.
Nonmyeloablative allogeneic peripheral blood stem cell transplantation (“mini” transplant) is now being investigated as immunotherapy for some advanced cancers. This highly toxic and intensive therapy has been shown to result in sustained regression of chemotherapy-resistant metastatic renal cell carcinoma in ten out of nineteen treated patients, with three complete remissions. Tumor response was associated with acquisition of the donor immune system, resulting in a “graft-versus-tumor” effect. Further investigation is required to confirm sustained beneficial effects, reduce toxicity, improve efficacy, and better understand in which diseases this type of therapy can be effective. However, nonmyeloablative transplant is now an alternative to the much more toxic full allogeneic transplant for hematologic malignancies when the patient cannot tolerate a full transplant due to age or comorbidity, or as a second transplant following autologous transplantation. Although the initial treatment is less intensive, the late immune effects are still a significant problem, as is disease relapse.
Chemotherapeutic agents can now be given on a variety of schedules to reduce toxicity and enhance anti-
P.1662
tumor effects. “Dose-dense” chemotherapy can be given in two ways, either as standard doses of chemotherapy given more frequently with growth factor support or as smaller doses given on a weekly or more frequent schedule (“metronomic” dosing). Animal studies have suggested that these dosing regimens may reverse some types of chemotherapy resistance. A recent study found that standard doses of chemotherapy for breast cancer given every 2 weeks were superior to the same doses given at the standard 3-week interval. Both disease-free and overall survival were improved in this study. Somewhat surprisingly, toxicity was lower in the “dose-dense” arm, due to the routine use of myeloid growth factors to avoid neutropenia and its associated complications.
Although most anticancer drugs are used systemically, there are selected indications for local or regional administration. Regional administration involves direct infusion of active chemotherapeutic agents into the tumor site (eg, intravesical therapy for bladder cancer, intraperitoneal therapy for ovarian cancer, hepatic artery infusion with or without embolization of the main blood supply of the tumor for cancers metastatic to the liver or as primary therapy for hepatocellular carcinoma). These treatments can result in palliation and prolonged survival.
A summary of the types of cancer responsive to chemotherapy and the current treatments of choice is offered in Table 40-3. In some instances (eg, Hodgkin's disease, breast cancer, ovarian and lung cancers), optimal therapy may require a combination of therapeutic resources, eg, radiation plus chemotherapy rather than either modality alone. Patients with stage I and II Hodgkin's disease are often treated with radiation alone, avoiding the potential toxicity of systemic chemotherapy. A small percentage of these patients may require chemotherapy later for disease recurrence.
Newer Anticancer Drugs
New drugs to treat cancer are under constant development and testing, with the aim of reducing toxicity to normal cells and increasing the toxicity to resistant cancer cells. Several of these newer agents developed over the past decade and now available are described in this section.
We have entered an exciting new era in the understanding and treatment of malignancies. Molecular techniques have allowed insight into the biologic events resulting in cancer, and these same techniques have resulted in identification of just the beginning of a cascade of biologic therapies directed toward specific molecular or cellular factors critical to the pathogenesis of cancer growth and survival. Rather than the traditional cytotoxic therapy, newer treatments are more specific and less globally cytotoxic, but are still associated with the potential for serious side effects. A number of biologic therapies are either approved or under investigation for use in the treatment of cancer. The time from development of a novel agent to clinical use and FDA approval has been markedly shortened; in the first 6 months of 2001, two biologic therapies, imatinib mesylate and alemtuzumab, were rapidly approved for use based on marked efficacy with low toxicity for the treatment of two different hematologic malignancies. In 2003 through the first quarter of 2004, seven new agents were approved by the FDA for the treatment of a variety of cancers, including novel cytotoxics, biologic therapy, and radioimmunoconjugates. Two agents to reduce chemotherapy-associated nausea and vomiting were also released for use. In the beginning of 2005, the first nanoparticle taxane, nab-paclitaxel was approved for the treatment of metastatic breast cancer. In the next decade we will probably see the development of a whole new class of agents and, consequently, a new paradigm for the treatment of cancer.
Newer Cytotoxics
Paclitaxel (Taxol) is a novel agent isolated from the pacific yew tree that has replaced cyclophosphamide as front-line therapy (combined with carboplatin) for the treatment of ovarian cancer. Intraperitoneal instillation may also be helpful for advanced disease. Paclitaxel (and docetaxel; see below) has also been shown to be one of the most effective agents available to treat earlyand late-stage breast cancer; it is also effective in AIDS-associated Kaposi's sarcoma and cancer of the lung among other cancers. The primary toxicities of paclitaxel are hematologic and neurologic. Both are dose dependent; the hematologic toxicity can be ameliorated by the use of myeloid growth factors. Recent data on breast cancer indicate that weekly or every-2week dosing is the most effective way to give paclitaxel. Nab-paclitaxel ABI-007 (abraxane) is a novel taxane that combines paclitaxel with albumin into a nanoparticle 1/100th the size of a red blood cell. This avoids the need for solvents, which result in a risk of serious allergic reactions to standard paclitaxel. A recent randomized, phase III trial compared paclitaxel to abraxane in the treatment of metastatic breast cancer. Treatment with abraxane significantly increased the response rate as well as time to tumor progression, and there were no allergic reactions seen—thereby avoiding the use of routine steroid premedications. The major toxicity of abraxane appears to be neuropathy, which can be ameliorated by giving lower doses on a weekly schedule. This drug was FDA approved for the treatment of metastatic breast cancer in early 2005. A number of novel taxanes (also called epothilones) are in clinical trials at this time.
Docetaxel is a synthetic analog of paclitaxel that has also been shown to be highly effective in the treatment of breast cancer as well as many other advanced malignancies, including non-small cell lung cancer and ovarian cancer. Its toxicities include bone marrow suppression and significant peripheral edema. The edema can be treated and generally prevented with steroids. Changing the schedule of administration appears to change toxicity. When docetaxel is given on a
P.1663
P.1664
P.1665
weekly schedule, it is associated with significantly less hematopoietic toxicity, but also with novel toxicities including lacrimal duct stenosis requiring stenting, and marked damage to the fingernails. A recent randomized trial compared every-3-week dosing of docetaxel to paclitaxel in women with metastatic breast cancer. Time to progression and survival were superior in patients treated with docetaxel. Weekly paclitaxel has been shown to be superior to every-3-week dosing, raising questions about the use of paclitaxel and appropriate dosing schedules.
Table 40-3. Treatment choices for cancers responsive to systemic agents. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vinorelbine, a semisynthetic vinca alkaloid, has been shown to be effective in treating advanced nonsmall cell lung cancer. Response rates of 30% have been observed when vinorelbine is used as a single agent against this poorly responsive tumor. Vinorelbine is also used to treat metastatic breast cancer as well as other tumors. Toxicities include significant bone marrow suppression, neuropathy, and transient ileus.
Capecitabine is an oral 5-fluorouracil (5-FU) prodrug that is approved to treat anthracyclineand taxane-resistant breast cancers as well as metastatic colo-
P.1666
rectal cancer. Response rates range from 25% to 35%. Treatment can be complicated by a painful, red, and sometimes blistering rash on the palms and soles and severe diarrhea that resolves upon withholding therapy and subsequent dose reduction. A variety of other 5FU prodrugs are in clinical trials but are not yet approved for use. One study showed a 3-month improvement in survival using the combination of docetaxel and capecitabine versus docetaxel alone in the treatment of advanced metastatic breast cancer, though there were considerably more side effects in the combination arm. This combination is now FDA approved, although newer dosing schedules with reduced toxicity are being used. It is still not clear that the combination is better than sequential single agent chemotherapy, however; a substantial number of patients treated on the docetaxel alone arm were never able to receive capecitabine due to geographic location outside of the United States and Europe.
Gemcitabine, a pyrimidine analog for intravenous use, has been approved to treat pancreatic cancer and non-small cell lung cancer but is active in other advanced malignancies, including breast cancer, particularly in combination with other chemotherapeutic or biologic agents. Toxicities are quite modest, and are primarily fatigue, myelosuppression, and an occasional rash. A recent trial combining gemcitabine and paclitaxel in the treatment of metastatic breast cancer showed a short survival benefit compared to paclitaxel alone; however, less than 50% of patients received additional chemotherapy after study treatment similar to the capecitabine study outlined above. The primary toxicity was bone marrow suppression.
Topotecan was the first of a class of drugs called camptothecans that inhibits the enzyme topoisomerase I to be FDA approved for use. It is used to treat advanced ovarian cancer and has shown some efficacy in the treatment of several other tumors.
Irinotecan is highly effective in the treatment of metastatic colorectal cancer. Two randomized studies compared the combination of irinotecan, fluorouracil, and leucovorin (IFL) to treatment with fluorouracil and leucovorin alone in patients with untreated metastatic colorectal cancer. The use of irinotecan resulted in a significantly higher response rate, delayed time to progression, and, in one study, improved survival. Toxicity in the irinotecan arm was also significantly higher, and with longer follow-up mortality was concerningly high at 3.5%. With appropriate management, much of the toxicity appears to be reversible and includes severe diarrhea and neutropenia. It is now understood that genetic polymorphisms resulting in delayed metabolism of irinotecan are largely responsible for the severe toxicities that are occasionally seen. Studies are ongoing to better understand and test for these individual differences in drug metabolism. Guidelines are available to improve management and reduce mortality from this regimen, which was due either to inflammation of the bowel, leading to sepsis, or to thrombosis. A newer agent, oxaliplatin, is now an alternative to irinotecan as first-line therapy for colorectal cancer (see below). Antitumor responses have been shown using irinotecan to treat non-small cell lung cancer, small cell lung cancer, ovarian cancer, gliomas, breast cancer, and others.
Results of a phase III randomized trial demonstrated a significant improvement in response rates, time to progression, and median survival using a new regimen to treat metastatic colorectal cancer consisting of the platinum derivative oxaliplatin combined with infusional fluorouracil and leucovorin (FOLFOX4) compared with the IFL regimen. Toxicity was also reduced, with less nausea, vomiting, diarrhea, and myelosuppression but an increase in neuropathy. Oxaliplatin is now approved for use in the United States based on the results of this trial. The primary toxicities of oxaliplatin are infusion reactions and reversible neuropathy. One of the challenges in the treatment of cancer is that few agents cross the blood–brain barrier, making it difficult to treat primary or metastatic cancers in the central nervous system. Temozolamide is an oral alkylating agent with the very unusual property of excellent central nervous system penetration. It is useful in the treatment of primary tumors of the brain, and is also being tested as a treatment for tumors metastatic to the brain. Temozolamide has recently been found to be effective in the treatment of metastatic melanoma as well.
Inhibitors of Thymidylate Synthase
Novel inhibitors of thymidylate synthase are under study for the treatment of advanced colorectal cancer. Treatment of malignant mesothelioma with the multitargeted antifolate agent pemetrexed—in combination with cisplatin—has been shown to significantly improve survival from this highly resistant disease when compared with treatment with cisplatin alone. This is the first chemotherapeutic agent that has been shown to alter survival from malignant mesothelioma, a cancer that is rising in incidence due to occupational exposure to asbestos. Pemetrexed, recently approved by the FDA, must be given with folic acid and vitamin B12 supplementation. Raltitrexed is currently being used in Europe based on early data showing similar efficacy compared with fluorouracil and high-dose leucovorin.
Liposomal encapsulation of active chemotherapeutic agents may improve drug delivery and decrease systemic toxicity. Two liposomally encapsulated drugs, doxorubicin (Doxil) and daunorubicin (Daunosome), are indicated in the treatment of Kaposi's sarcoma and have shown efficacy in treating many other diseases, including breast cancer and lymphoma.
Monoclonal Antibodies
An increasing number of monoclonal antibodies are used in cancer chemotherapy. Rituximab, a chimeric antibody against the B lymphocyte antigen CD20, is effective therapy for relapsed or resistant low-grade
P.1667
lymphomas and has shown limited usefulness in higher-grade lymphomas as well. Almost 50% of patients with low-grade lymphoma respond with shrinkage of lymph nodes to once-weekly dosing for 4 weeks. Responses lasted a median of over 1 year. Rituximab has been shown to be effective in longer courses lasting 8 weeks and as retreatment following relapse. A randomized study compared standard cyclophosphamide, doxorubicin (hydroxydaunomycin; Adriamycin), vincristine (Oncovin), and prednisone (CHOP) chemotherapy with rituximab combined with CHOP as initial therapy for patients aged 60 years or older with diffuse large B cell lymphomas. Response rates, 12-month event-free survival, and overall survival were significantly improved in the combination arm. Rituximab has been effective in treating a wide range of Blymphocyte-mediated disorders including benign autoimmune disease as well as lymphoid malignancies. Toxicities are generally quite mild, though anaphylaxis (resulting in death) and infusion-related side effects have been reported.
The HER-2/neu oncogene (also called c-erbB-2), a gene that encodes a receptor tyrosine kinase, is known to be overexpressed in many human cancers and is associated with tumors with poorer prognoses. In breast cancer, overexpression of HER-2/neu is seen in about 20% of women and is associated with a higher risk of metastatic disease and poorer survival. Trastuzumab (Herceptin) is a recombinant humanized monoclonal antibody directed against the HER-2/neu gene product that is indicated for the treatment of HER-2/neu-expressing metastatic breast cancer. When trastuzumab was used as a single agent to treat anthracycline-resistant breast cancer, the response rate was about 15%, with a median duration of response of over 8 months. However, when trastuzumab was added to first-line chemotherapy for metastatic breast cancer and compared with chemotherapy alone, patients receiving the combination therapy had a response rate of almost 50% with significant improvement in both duration of remission and survival. The most promising combination appears to be trastuzumab and paclitaxel (Taxol) or docetaxel (Taxotere) either with or without platinum salts (carboplatin or cisplatin); combinations with other agents, including vinorelbine and gemcitabine, also appear to be effective. The combination of trastuzumab and doxorubicin (Adriamycin) resulted in an increase in subclinical and clinical cardiac toxicity; combinations with anthracyclines should be avoided. Other toxicities of trastuzumab appear to be primarily infusion related. Ongoing randomized trials are evaluating trastuzumab therapy in combination with neoadjuvant or adjuvant therapy for node-positive breast cancer; preliminary results should be available in early 2006. In addition, trastuzumab is being tested for use in other HER-2/neu-expressing tumors such as prostate and ovarian cancers.
Alemtuzumab is a humanized monoclonal antibody that is approved to treat relapsed or resistant CLL. It targets the CD52 antigen, which is prevalent on the abnormal B lymphocytes found in this common leukemia. In clinical trials of patients with CLL refractory to fludarabine and with prior exposure to alkylating agents, response rates of 33% were seen with a median duration of response of 7 months. Early studies in untreated patients suggest a response rate of up to 87% with a high rate of complete responses. Alemtuzumab is given by subcutaneous injection, and side effects include infusion-related events, infections, and bone marrow suppression.
Cetuximab is a chimeric human/mouse recombinant monoclonal antibody, recently FDA approved to treat metastatic colorectal cancer, that overexpresses the EGFR. EGFR is a gene that is also overexpressed in many human cancers and has been associated with a poorer prognosis and resistance to therapy. Similar to the HER-2/neu oncogene, EGFR encodes a receptor tyrosine kinase that is closely related to HER-2. In patients with cancers that are resistant to irinotecan with or without oxaliplatin, the addition of cetuximab has been shown to result in about a 25% response rate, suggesting reversal of resistance. Response rates to its use as a single agent are about 11–15%. The major toxicities are infusion reactions and a significant and often painful acneiform rash. Cetuximab is indicated in the treatment of EGFR-expressing metastatic colorectal cancer in patients who are refractory to irinotecan-based chemotherapy.
Bevacizumab is the first antiangiogenic agent to be approved for clinical use in the treatment of cancer. Bevacizumab is a monoclonal antibody that binds to vascular endothelial growth factor (VEGF), the ligand for the VEGF receptors—thereby inhibiting activation of this receptor on the surface of endothelial cells as well as resulting endothelial cell proliferation and new blood vessel formation. As first-line therapy for metastatic colorectal cancer, the combination of bevacizumab with IFL was found to result in improved response rates as well as a 25% improvement in survival compared to the chemotherapy regimen alone. Bevacizumab is indicated for use in combination with fluorouracil-based chemotherapy in the first-line treatment of metastatic colorectal cancer. Preliminary data indicate activity of bevacizumab against a variety of other malignancies, including renal cell cancer and breast cancer. As a single agent, bevacizumab resulted in tumor shrinkage in renal cell cancer, and about a 10–15% response rate in resistant breast cancer. Ongoing large randomized trials are assessing the effectiveness of bevacizumab combined with chemotherapy in a variety of tumor types. The primary toxicities of bevacizumab include hypertension and proteinuria. Delays in wound healing, fatal hemorrhage, and bowel perforation have been reported in patients with lung and colorectal cancers.
Antibodies Linked to Cytotoxic Agents or Radiation
Radiolabeled and toxin-linked antibodies have been used to treat lymphomas with very encouraging results and appear more effective than antibody therapy alone.
P.1668
Ibritumomab tiuxetan is an yttrium-90-labeled antibody to CD20 that is FDA approved for the treatment of low-grade non-Hodgkin's lymphoma refractory to rituximab or transformed B cell non-Hodgkin's lymphoma. This is the first targeted radioimmunotherapy to be FDA approved for clinical use. This unique drug consists of an antibody to CD20 bound to tiuxetan, a high-affinity chelator for yttrium-90 and indium-111. A recently published randomized controlled trial compared ibritumomab tiuxetan with rituximab in patients with relapsed or refractory low-grade non-Hodgkin's lymphoma or transformed non-Hodgkin's lymphoma. The overall response rate was 80% for the radiolabeled antibody versus 56% for rituximab alone, with a corresponding prolongation in duration of response and time to disease progression. Durable responses were significantly longer in the ibritumomab tiuxetan group. The primary toxicity is reversible but significant myelosuppression. This agent must not be used in patients with impaired marrow function or extensive involvement of marrow with lymphoma. Treatment is given in two steps. On day 1, a dose of rituximab is given followed by indium-111-labeled ibritumomab tiuxetan to determine biodistribution of antibody. One week later, a second dose of rituximab is followed by yttrium-90-labeled antibody. Yttrium-90 is a pure b emitter with a half-life of 64 hours and a short path length of 5 mm, making it relatively safe to use in clinical practice.
A second radiolabeled antibody, tositumomab, is linked to 131I, which requires dosimetry and shielding, making clinical use more cumbersome. Tositumomab was recently approved by the FDA for the treatment of low-grade non-Hodgkin's lymphoma refractory to rituxan and chemotherapy and is given in two steps— the dosimetric and therapeutic steps. Each step includes an infusion of tositumomab followed by radiolabeled tositumomab. Toxicity is similar to that of ibritumomab tiuxetan. Many other antibody combinations are either under development or in preliminary clinical trials.
Another agent approved for the treatment of cutaneous T cell lymphomas (CTCL) such as mycosis fungoides resistant to standard therapy is denileukin diftitox (ONTAK), a recombinant DNA-derived cytotoxic protein composed of amino acid sequences for diphtheria toxin fragments followed by the sequences for interleukin-2 (IL-2). This fusion protein was designed to direct the cytocidal action of diphtheria toxin to cells that express the IL-2 receptor (CD25), such as the tumor cells in CTCL. Thirty percent of patients with advanced CTCL responded to denileukin diftitox in a phase III randomized trial. Toxicity is significant, including acute hypersensitivity reactions—requiring administration of this agent in a close-observation setting—and delayed pulmonary and peripheral edema.
Gemtuzumab ozogamicin is an antibody to CD33 linked to a potent antitumor antibiotic, calicheamicin, that is approved for the treatment of patients over the age of 60 years with relapsed or refractory acute myelogenous leukemia (AML). This is the first example of antibody-targeted chemotherapy used clinically. In clinical trials, gemtuzumab ozogamicin resulted in a 31% remission rate in elderly patients with AML in first relapse who could not tolerate standard chemotherapy. Side effects are primarily infusion-related events and bone marrow suppression.
Agents with Novel Mechanisms of Action
Thalidomide, approved for treatment of lepromatous leprosy, has been found to induce significant responses in advanced and relapsed multiple myeloma. It is now being tested in many clinical trials, and the combination of thalidomide with dexamethasone results in enhanced responses. Toxicities that limit the usefulness of thalidomide include rashes, somnolence, and constipation. Revlimid is the lead compound of a new class of more potent and less toxic immunomodulatory drugs or ImiDs, which are believed to affect multiple pathways within the cell and inhibit tumor necrosis factor-a (TNF-a). Multiple ongoing studies are evaluating the effect of revlimid in a variety of malignancies. Preliminary data indicate effectiveness in multiple myeloma and myelodysplastic syndromes.
Bortezomib (Velcade) is the first of a new class of agents, termed proteasome inhibitors, to be approved for the treatment of cancer. Bortezomib is a reversible inhibitor of the chymotrypsin-like activity of the 26S proteasome that degrades ubiquitinated proteins. The ubiquitin-proteasome pathway plays an essential role in regulating the intracellular concentration of specific proteins, thereby maintaining homeostasis within cells. Inhibition of the 26S proteasome prevents targeted breakdown of proteins, which affects multiple signaling cascades within the cell. The disruption in these normal homeostatic mechanisms can lead to cell death. In an open-label study of bortezomib in patients with multiple myeloma who had failed at least two prior therapies, the overall response rate was 28%, with 18% obtaining a clinical remission. The median duration of response was long at about 1 year. Bortezomib is approved for the treatment of multiple myeloma that progresses despite at least two prior therapies. Significant responses have also been seen in patients with relapsed and refractory low-grade lymphomas. It is given intravenously twice weekly for 2 weeks followed by a 10-day rest, then repeated every 3 weeks. The major side effects are peripheral neuropathy, cytopenias, and hypersensitivity reactions.
Tretinoin is the first agent designed to target a specific fusion protein caused by a chromosome translocation. This oral agent induces differentiation and decreased proliferation without cytolysis of acute promyelocytic leukemia cells. Use of tretinoin combined with chemotherapy has been shown to improve disease-free and overall survival from this form of leukemia. Arsenic trioxide has been shown to induce remission in 70% of patients with relapsed or refractory acute promyelocytic leukemia (APL). It is indicated both for induction of remission and for consolidation in this high-risk group of patients.
P.1669
Retinoids modulate the growth and differentiation of a variety of epithelial cells. Bexarotene, a retinoid that selectively activates the retinoid X receptor (RXR), is now FDA approved to treat cutaneous T cell lymphomas such as mycosis fungoides. Targretin is also in clinical trials for use in a variety of advanced solid tumors, but toxicity limits its usefulness.
A purine analog, cladribine (2-chlorodeoxyadenosine; 2-CdA), is used as the primary agent to treat hairy cell leukemia. A 1-week course of therapy results in high and durable remission rates with modest and short-lived toxicity. Repeated courses for disease recurrence are also effective. Pentostatin (2-deoxycoformycin, an adenosine deaminase inhibitor) is also used to treat hairy cell leukemia.
Fludarabine phosphate, another purine analog, has shown improved response rates and progressionfree survival compared with oral chlorambucil or combination chemotherapy for CLL. Fludarabine is now indicated as first-line therapy for most patients with CLL. Side effects include an increased risk of opportunistic infections as well as very rare problems such as hemolytic anemia and severe bone marrow suppression. Fludarabine is also effective therapy for lowgrade lymphomas and Waldenstr m's macroglobulinemia. Cladribine and pentostatin are also used to treat CLL and the above disorders.
Recombinant Growth Factors
Several recombinant growth factors have been shown to be effective in the treatment of malignancy. Recombinant interferon- a has marked antitumor effects in hairy cell leukemia and chronic myelogenous leukemia and moderate effects in lymphomas, in the epidemic (AIDS-associated) form of Kaposi's sarcoma, in multiple myeloma, and as adjuvant therapy for malignant melanoma. Interferon-a has some utility also in metastatic melanoma, renal cell carcinoma, and carcinoid syndrome. Unfortunately, chronic use of interferon-a is associated with fatigue, cytopenias, and fluid retention.
High-dose interferon for about 1 year in patients with malignant melanoma and lymph node metastases has been shown to improve disease-free and overall survival. Combinations of interferon-α-2b and interleukin-2 given with standard chemotherapy for metastatic melanoma prolongs time to progression and survival (by a median of 2.7 months) but is associated with a significant increase in toxicity. Interleukin-2 treatment is effective in a subset of patients with advanced renal cell carcinoma. Recent data indicate improved survival in patients with AL type amyloidosis treated with a combination of dexamethasone and interferon-a compared with standard treatment with oral melphalan and prednisone. The addition of interferon-a to systemic chemotherapy for multiple myeloma appears to enhance the degree of cytoreduction achieved as compared with chemotherapy alone; however, toxicity is additive. Use of interferon-a for myeloma following chemotherapy or autologous bone marrow transplant has prolonged remission duration, though overall survival is not altered.
Prior to the availability of imatinib, patients with CML were treated with interferon-a given with low doses of the chemotherapeutic agent cytarabine. About 30% of patients achieved a cytogenic response to this combination, which was associated with a significantly longer survival than that of patients treated with standard oral chemotherapy. CML is unusual in that almost all cases are associated with a specific reciprocal chromosomal translocation resulting in activation of a tyrosine kinase that is critical to the pathogenesis of the disease.
Oral Small Molecule Tyrosine Kinase Inhibitors
A novel and exciting oral agent, imatinib mesylate (Gleevec), specifically blocks the active tyrosine kinase in CML and is now approved for clinical use in both early-stage and late-stage CML. The response in patients with chronic phase CML was striking, with a 94% hematologic and an 83% cytogenetic response rate. These responses appear to be durable; progression-free survival at 12 months was significantly longer with imatinib mesylate than with the combination of interferon and cytarabine at 97% versus 80% in a phase III trial. Lower but significant response rates are seen in more advanced disease. The effect of imatinib mesylate on long-term disease control will require further follow-up of treated patients, although relapses and resistance clearly occur. Imatinib mesylate also inhibits two other tyrosine kinases, receptors encoded by c-kit and platelet-derived growth factor (PDGF). Expression of the c-kit receptor is found in high frequency in a relatively uncommon tumor of the gastrointestinal tract, gastrointestinal stromal tumor (GIST). GISTs are highly resistant to chemotherapy, and there is no effective therapy for advanced disease. Imatinib mesylate has demonstrated significant activity in GISTs, with a 60% overall response rate. This drug is also being tested in conditions such as myelofibrosis, chronic myelomonocytic leukemia, prostate cancer, and glioblastoma that express PDGF.
Gefitinib (Iressa) is another small molecule tyrosine kinase inhibitor that has recently been approved to treat advanced lung cancer that progresses despite at least two prior chemotherapy regimens. Gefitinib blocks the intracellular component of the epidermal growth factor receptor (EGFR), which is overexpressed on a number of tumors and correlates with poorer prognosis. Response rates in a phase III trial were low at just over 10% overall, but no other treatments are available to this population of patients, and up to 43% of treated individuals experienced symptom relief. For patients who had failed up to two prior treatments, the response rate rose to about 19%. A similar agent, erlotinib (Tarceva), was FDA approved for the treatment of metastatic lung cancer in 2004 based on a study show-
P.1670
ing a 2 month improvement in survival in patients treated with erlotinib versus those treated with placebo. In separate trials, neither gefitinib nor erlotinib combined with first-line chemotherapy for advanced lung cancer offered any advantage over first-line chemotherapy alone. Toxicity from both agents is modest and consists primarily of skin rash and diarrhea. Specific mutations in tumor EGFR are associated with responsiveness to gefitinib and erlotinib. An unusual and resistant form of lung cancer, bronchoalveolar carcinoma (BAC), has demonstrated striking responsiveness to gefitinib and erlotinib therapy and is known to express high levels of EGFR. A number of other oral tyrosine kinase inhibitors that block multiple receptors or angiogenesis are in clinical trials.
Hormonal Therapy
Hormonal therapy plays a critical role in the management of specific cancers. Hormonal therapy or ablation is important in the treatment and palliation of breast and prostatic carcinoma, whereas added progestins are useful in the suppression of endometrial carcinoma. Women with metastatic breast cancer who show objective improvement with hormonal therapy have tumors that contain nuclear estrogen and progesterone receptors. The SERM tamoxifen has been shown to be effective in prolonging survival in both early-stage and late-stage breast cancer. Tamoxifen has both antiestrogen and proestrogen effects, resulting in side effects that include an increase in the risk of endometrial cancer and thrombosis. Newer SERMs without estrogenlike effects are being developed.
Aromatase inhibitors (eg, anastrozole, letrozole) and inactivators (exemestane) block the peripheral conversion of adrenal androgens into estrogens and have been shown to be at least as effective as or more effective than tamoxifen as first-line therapy for metastatic hormone receptor-expressing breast cancer. Aromatase inhibitors are effective only in postmenopausal women and have now been shown to be very effective in the adjuvant setting as well. The Arimidex and Tamoxifen Alone or in Combination (ATAC) trial is a large randomized trial that compared 5 years of tamoxifen to either anastrozole or to the combination as adjuvant therapy in postmenopausal women with hormone receptor-positive early-stage breast cancer. The combination arm was no better than tamoxifen; this arm was closed at the first evaluation of the trial. At 5 years of follow-up, there was a significant decrease in both distant and local recurrence as well as new breast cancers in the opposite breast in the women treated with anastrozole, compared to treatment with tamoxifen. There was no difference in survival, probably due to the slow growth of hormone responsive cancers and variable poststudy therapy in patients depending on the treatment arm of the study. Preliminary data from a second trial, BIG I-98, that compared letrozole to tamoxifen was presented in early 2005 and indicated a similar improvement in disease-free survival favoring the letrozole treated patients. Further data from this trial, and from a subset of patients who were switched from one agent to the other 2 years into therapy, should be available in the next 2 years.
Three additional studies have reinforced the importance and efficacy of aromatase inhibitors in the treatment of early-stage breast cancer. Two trials randomized postmenopausal women who had received tamoxifen for 2–3 years to exemestane or continued tamoxifen (the EIS trial) or to anastrozole or continued tamoxifen (the ABSCG/ARNO trials). Women who switched to the aromatase inhibitor had significantly fewer relapses and new breast cancers than women who continued tamoxifen.
Hormone receptor-positive breast cancer is a relatively slow growing disease, with 50% of all relapses occurring after 5 years. For that reason, extending hormone therapy has long been of interest to researchers. However, the toxicity of continued tamoxifen has precluded its use after 5 years in the adjuvant setting. The MA.17 trial randomized women to letrozole or placebo following 5 years of tamoxifen. This trial was closed early due to results showing an unexpectedly large benefit from letrozole at 3 years. Women treated with letrozole had a significant reduction in the risk of recurrence as well as in the incidence of new cancers. Survival was improved in women with node-positive breast cancer who were randomized to letrozole.
Toxicities in all five trials were modest. The primary toxicities of the aromatase inhibitors are accelerated bone mineral density loss, altered lipid profiles, and temporary but bothersome joint aches and stiffness. Longer-term follow-up, survival, and toxicity data—in particular the impact of these new agents on non-cancer-related morbidity and mortality—should be available over the next few years. Women treated with aromatase inhibitors should have their bone mineral density monitored, with early institution of antiresorptive therapy.
Given the weight of this evidence, for postmenopausal women with early-stage breast cancer, aromatase inhibitors appear to be an important part of treatment. Whether treatment should be given at diagnosis, at 2–3 years into tamoxifen, or after 5 years of tamoxifen is not known. Ongoing trials are comparing different strategies and should help answer these questions in the future. New trials are exploring the use of ovarian suppression and aromatase inhibition or inactivation in the treatment of early-stage breast cancer in premenopausal women.
A new pure antiestrogen (estrogen receptor down regulator), fulvestrant, has now been FDA approved as second-line therapy for metastatic hormone receptorpositive breast cancer. This agent is unique in its class, does not have the estrogen-like effects of tamoxifen, and is given by intramuscular injection once a month. Hormonal approaches are also available to treat prostate cancer, though androgen receptors remain difficult to measure. These include the use of estrogen therapy, gonadotropin-releasing hormone agonists (eg, leupro-
P.1671
lide, triptorelin, goserelin), and antiandrogens (eg, bicalutamide, flutamide). The use of leuprolide plus flutamide (total androgen blockade) can be considered as an alternative to orchiectomy but also causes erectile dysfunction. High-dose ketoconazole has been used to rapidly suppress adrenal production of steroids in crises such as cord compression. Use of this agent requires hydrocortisone supplementation.
Bisphosphonates
Bisphosphonates inhibit osteoclast activation and may also have antitumor and antiangiogenic effects. In addition to reducing bone pain, pamidronate reduces by approximately 50% the frequency of new skeletal events in breast cancer and prostatic cancer metastatic to bone and in multiple myeloma and delays the time to new bone events. Pamidronate must be given intravenously on a monthly basis, and is associated with bone and muscle pain as well as fever on the day following the first infusion. A new and significantly more potent intravenous bisphosphonate, zoledronic acid, was FDA approved in early 2002 for the treatment of metastatic bone lesions. Its advantage compared with pamidronate is a shorter infusion time (15 minutes compared with 2 hours or more) and improved efficacy in some situations. Faster-than-indicated infusion rates of this bisphosphonate can result in reversible renal insufficiency. Zoledronic acid or pamidronate is indicated for the treatment of patients with known bone metastases due to any type of malignancy. Onceyearly infusions of zoledronic acid have been shown to improve bone mineral density in osteopenic postmenopausal women. Ongoing trials are evaluating the ability of zoledronic acid to prevent bone loss associated with hormonal therapy and chemotherapy in breast and prostate cancers. Guidelines for the use of bisphosphonates in the treatment of cancer were recently published.
Clodronate is an oral bisphosphonate that has been shown to reduce the number of new bone metastases in women with breast cancer. A study of women with a primary diagnosis of breast cancer and microscopic evidence of tumor cells in bone marrow randomized to receive either clodronate, 1600 mg/d for 2 years, or placebo—in addition to standard adjuvant therapy—showed a significant reduction of both osseous metastases initially and a reduction in mortality out to 10 years of follow-up. Results of a larger study of women with operable breast cancer but no other specific high-risk features showed a reduction in the incidence of bone metastases during the study period only but no difference in visceral metastases. Surprisingly, this study also showed a survival advantage at 10 years in women treated with clodronate. These observations suggest that bisphosphonates may be a useful treatment in a subset of women with primary breast cancer to prevent recurrence. Clodronate is a less potent bisphosphonate than zoledronic acid and is currently available only in Europe. A clinical trial in the United States comparing the effect of clodronate in women with node-positive breast cancer has recently been completed. As a follow-on trial, a national study opening later in 2005 will evaluate the effects of adjuvant zoledronic acid, clodronate, or ibandronate, a new and potent oral bisphosphonate, for 3 years in 6000 women with early stage breast cancer.
Growth Factors
Hematologic or other toxicity may limit the therapeutic effectiveness of treatment. It is possible to avoid the need for dose reductions or delay in therapy by using granulocyte colony-stimulating factor (G-CSF; filgrastim) or granulocyte-macrophage colony-stimulating factor (GMCSF; sargramostim) to stimulate white blood cell recovery. A long-acting pegylated G-CSF (pegfilgrastim) is now FDA approved to reduce the incidence of neutropenic fever associated with chemotherapy. This agent can be given as a single 6 mg dose subcutaneously on day 2 of each 3-week chemotherapy cycle and in randomized trials was equivalent to 11 doses of filgrastim. Pegfilgrastim is now being used to reduce neutropenia in chemotherapy regimens given every 2 weeks as well; preliminary data indicate that this is a safe and effective approach. Interleukin-11 (oprelvekin) can be used to reduce the need for delay or dose reductions due to thrombocytopenia; however, the usefulness of this cytokine is limited because of its ineffectiveness in severe thrombocytopenia and its toxicity, which includes significant edema. Guidelines are available to direct usage of these expensive but critical growth factors. Erythropoietic growth factors are a very important part of supportive care during cancer chemotherapy; these agents are covered under the section on supportive care.
Table 40-4 sets forth the dosage schedules and toxicities of the most commonly used cancer chemotherapeutic agents. The dosage schedules given are for single-agent therapy; combination therapy is used for most cancers. Newer experimental therapies are discussed briefly at the end of this chapter.
Baum M et al: The ATAC (Arimidex, Tamoxifen Alone or in Combination) Trialists' Group. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer 2003;98:1802.
Coiffier B et al: CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 2002;346:280.
Coombes RC et al: A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 2004;350:1081.
Eton O et al: Sequential biochemotherapy versus chemotherapy for metastatic melanoma: results from a phase III randomized trial. J Clin Oncol 2002;20:2045.
Folprecht G et al: The role of new agents in the treatment of colorectal cancer. Oncology 2004;66:1.
P.1672
P.1673
P.1674
P.1675
P.1676
P.1677
P.1678
Goss PE et al: A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 2003;349:1793.
Grossman HB et al: Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med 2003;349:859.
Hilner BE et al: American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 2003;21:4042.
Hussein MA: New treatment strategies for multiple myeloma. Semin Hematol 2004;41:2.
Johnston SR: Fulvestrant. Curr Opin Investig Drugs 2002;3:305.
P.1679
Kris MG et al: Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 2003;290:2149.
Neville-Webbe HL et al: The anti-tumour activity of bisphosphonates. Cancer Treat Rev 2002;28:305.
O'Brien SG et al: Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2003;348:994.
Rosen LS et al: Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer 2003;98:1735.
Shigematsu H et al: Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst 2005;97:339.
Slamon DJ et al: Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 2001;344:783.
Takahashi Y et al: Nonmyeloablative transplantation: an allogeneic-based immunotherapy for renal cell carcinoma. Clin Cancer Res 2004;10(18 Pt 2):6353S.
Table 40-4. Single-agent dosage and toxicity of anticancer drugs.1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
ADJUVANT CHEMOTHERAPY FOR MICROMETASTASES
One of the most important roles of cancer chemotherapy is as adjuvant therapy to eradicate or suppress minimal residual disease after local treatment with surgery or irradiation. Failure of local therapy to eradicate tumor is due principally to occult micrometastases of tumor stem cells outside the primary field. These distant micrometastases are more likely to be present in patients with positive lymph nodes at the time of surgery (eg, breast and prostate cancer), in patients with tumors known to have a propensity for early hematogenous spread (eg, osteogenic sarcoma, Wilms' tumor), and in patients with certain pathologic or molecular risk factors (eg, high proliferative index, vascular invasion, oncogene amplification). Given specific risk factors, the risk of recurrent or metastatic disease can be extremely high (> 80%). Only systemic therapy can adequately eradicate micrometastases. Chemotherapeutic regimens that have been shown to be effective in inducing regression of advanced cancers may be curative when combined with surgery and/or radiation for high-risk “early” cancer.
More data are now available to support the use of adjuvant therapy in many common neoplasms. Prolongation of survival with combination chemotherapy has been shown for women with breast cancer and negative or positive axillary lymph nodes (stages I, II, and III) following surgical resection; several regimens are used. Anthracycline-based regimens (eg, doxorubicin, epirubicin) have been found to be superior to cyclophosphamide, methotrexate, and fluorouracil (CMF), particularly in nodepositive patients. The addition of taxanes to anthracycline combinations appears to further reduce the risk of recurrence and improve survival. Patients with node-negative breast cancer are treated with chemotherapy depending on a variety of risk factors in the primary tumor. The SERM tamoxifen (blocks the estrogen receptor) and the aromatase inhibitors anastrozole, letrozole, and exemestane (block estrogen production) are used routinely either with or without antecedent chemotherapy if receptors for estrogen or progesterone are present (see preceding section on hormonal therapy). The main challenge in treating women with node-negative (stage I) hormone receptor-positive breast cancer is to identify prognostic factors that distinguish patients at higher risk who are more likely to benefit from adjuvant therapy. A recent study evaluated the use of a 21 gene expression assay (Oncotype Dx Breast Cancer Assay) to predict a patient's individual risk of recurrent breast cancer 10 years after initial diagnosis. All of the women in the study had received 5 years of adjuvant tamoxifen; the test is performed on the original tumor block. A “recurrence score” from 0 to 100 is reported, and defines the level of risk of distant disease recurrence as low, intermediate, or high. This score could help in determining the appropriate treatment for these relatively good risk cancers. The assay has been validated in two studies, and specifically in women with cancers that are hormone receptor positive and in women who have received adjuvant tamoxifen. One additional trial suggested that the primary benefit of adjuvant chemotherapy with CMF was in the high-risk groups with rapidly proliferating disease, whereas the primary benefit of hormonal therapy was in the low-risk group with slow growing cells. Although the test is now approved for use, it is very expensive and is not routinely covered by most insurers. Amplification of the HER-2/neu oncogene in breast cancer clearly correlates with a poorer prognosis, and these patients appear to have a marked benefit from adjuvant chemotherapy containing anthracyclines and taxanes. The antibody trastuzumab, which blocks activation of this receptor and improves survival in metastatic breast cancer, is being tested in combination with chemotherapy as treatment for early-stage breast cancer that overexpresses HER-2/neu. Current research is focusing on the identification of additional and more specific risk factors early in diagnosis that can aid in prognosis and treatment decisions. A study using cytokeratin staining of bone marrow aspirates in women with newly diagnosed breast cancer found a 36% incidence of occult marrow metastases that correlated with a fourfold increased risk of death from breast cancer. A second study found that the presence of these cells 3 years after diagnosis was an even stronger prognostic factor for risk of recurrence and death from this disease. These results must be confirmed before they can be used in clinical practice to direct therapy. The goal is to identify patients with high-risk features at the time of diagnosis with localized disease and provide riskdirected (and effective) therapy.
Adjuvant chemotherapy with fluorouracil plus leucovorin is indicated in Dukes B and C (node-positive) colon cancer and has been shown to reduce the risk of cancer recurrence. Many other cancers may be cured with adjuvant chemotherapy, including cancers of the ovary and testes, malignant melanoma, and choriocarcinoma. Still other malignancies are cured when radiation
P.1680
and chemotherapy are used concurrently as described in the section on radiation therapy.
Other tumors that have been shown to respond to adjuvant therapy include gastric, esophageal, colorectal, and bladder cancers, prostate cancer, osteogenic sarcoma, ovarian cancer, and malignant melanoma— and, recently, non-small cell cancer of the lung. Adjuvant therapy remains investigational for a number of common tumors, including pancreatic cancer. Chemotherapy is often given with curative intent after surgical remission in testicular cancer, non-Hodgkin's lymphoma, and Hodgkin's lymphoma.
Although adjuvant therapy has been shown to reduce the rate of recurrence for some cancers, there is still a high failure rate (up to 60–80% in some highrisk breast cancers despite adjuvant therapy). In most cases, tumor recurrence signifies incurability. The evidence for a dose-response effect of adjuvant chemotherapy for most cancers remains unclear. Although high-dose chemotherapy with either bone marrow or peripheral blood stem cell rescue is curative for some otherwise incurable patients with testicular cancer and lymphomas, efficacy data are lacking for other solid tumors. Research in the past focused on very high doses of chemotherapy for high-risk and metastatic breast cancer; this translated into thousands of transplants and several large randomized clinical trials. Phase II data suggested clinical benefit to this toxic and expensive procedure, but the studies were biased by inappropriate historical controls, rigorous selection criteria, and short follow-up. To date, all randomized studies have failed to show any benefit to high-dose chemotherapy with stem cell rescue compared with intermediate or standard-dose chemotherapy. Two studies performed in South Africa appeared encouraging; however, an on-site review revealed significant scientific misconduct that invalidated all results. At present, high-dose chemotherapy for breast cancer should be performed only in the setting of a properly designed clinical trial; it is experimental therapy. Bone marrow transplantation for other malignancies is covered in more detail in Chapter 13.
Citron ML et al: Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol 2003;21:1431.
Hobday TJ et al: Adjuvant therapy of colon cancer: a review. Clin Colorectal Cancer 2002;1:230.
Janni W et al: The persistence of isolated tumor cells in bone marrow from patients with breast carcinoma predicts an increased risk for recurrence. Cancer 2005;103:884.
Mariotto A et al: Trends in use of adjuvant multi-agent chemotherapy and tamoxifen for breast cancer in the United States: 1975–1999. J Natl Cancer Inst 2002;94:1626.
Scagliotti GV et al: Randomized study of adjuvant chemotherapy for completely resected stage I, II or IIIA non-small-cell lung cancer. J Natl Cancer Inst 2003;95:1453.
Sun W et al: Adjuvant therapy of colon cancer. Semin Oncol 2005;32:95.
Tallman MS et al: Conventional adjuvant chemotherapy with or without high-dose chemotherapy and autologous bone marrow transplantation in high-risk breast cancer. N Engl J Med 2003;349:17.
Trimbos JB et al: International Collaborative Ovarian Neoplasm trial 1 and Adjuvant ChemoTherapy In Ovarian Neoplasm trial: two parallel randomized phase III trials of adjuvant chemotherapy in patients with early-stage ovarian carcinoma. J Natl Cancer Inst 2003;95:105.
TOXICITY & DOSE MODIFICATION OF CHEMOTHERAPEUTIC AGENTS
A number of cancer chemotherapeutic agents have cytotoxic effects on rapidly proliferating normal cells in bone marrow, mucosa, and skin. Still other drugs such as the vinca alkaloids and taxanes produce neuropathy, and hormones often have psychological as well as physical effects. Acute and chronic toxicities of various drugs used to treat cancer are summarized in Table 40-4. Appropriate dose modification may minimize these side effects, so that therapy can be continued with relative safety. Dose modifications are usually considered in settings where treatment is given with palliative intent. Dose intensity and schedule should be maintained if at all possible in the adjuvant setting, when treatment is directed toward preventing recurrence or metastases of the cancer.
Bone Marrow Toxicity
Depression of bone marrow is usually the most serious limiting toxicity of cancer chemotherapy. Autologous bone marrow or peripheral blood stem cell transplantation or rescue can reduce the myelosuppressive toxicity of high-dose chemotherapy; however, cost and toxicity limit its general use. Growth factors that stimulate myeloid proliferation (eg, G-CSF; filgrastim, the longer acting pegfilgrastim, and GM-CSF; sargramostim) or erythroid proliferation (epoetin alfa [erythropoietin]) and the longer acting darbopoetin alfa are now used to ameliorate bone marrow toxicity. G-CSF and GM-CSF have been shown to shorten the period of neutropenia following both standard and high-dose chemotherapy as well as to allow dosing of chemotherapy at more frequent intervals. The risk of febrile neutropenia and mucosal toxicity is reduced as well. Myeloid growth factors are also used to stimulate circulation of stem cells in the peripheral blood either at steady state or during white blood cell recovery following myelosuppressive chemotherapy. These cells are then harvested using an apheresis machine and frozen for later use. When stimulated peripheral blood stem cells are used instead of or in conjunction with bone marrow for autologous transplantation following high-dose chemotherapy and radiotherapy, recovery of both neutrophils and platelets may be hastened by as much as 7–10 days as opposed to the use of bone marrow alone. Recombinant growth factors are expensive and must be used judiciously. Published standard practice guidelines are referenced at the end of this section.
P.1681
Epoetin alfa (erythropoietin) and the newer darbopoetin alfa have been shown to improve anemia associated with malignancy or cancer chemotherapy. Patients must have adequate iron stores to respond to this agent, and even patients with marrow infiltration with tumor may benefit. Higher doses are necessary for patients with cancer than for patients with renal failure (40,000 units a week compared with about 10,000 units a week epoetin alfa). It is useful to check the level of erythropoietin before instituting therapy in patients with hematopoietic malignancies; this is not necessary in patients with solid tumors with either chemotherapyor cancer-related anemia. Very high levels (3 500 ng/mL) predict a poor response. Epoetin alfa may be given as a subcutaneous injection once a week. This dosage schedule is as effective as the traditional three times a week dosing and is much more convenient. For anemia related to cancer chemotherapy or marrow infiltration, a dose of 40,000 units a week is used. Novel erythropoiesis-stimulating protein (NESP; darbopoetin alfa) is now approved to treat anemia associated with renal failure and cancer chemotherapy. Its main advantage over epoetin alfa is its longer half-life, which allows dosing every 2–3 weeks, usually on the same schedule as chemotherapy administration. Current dosing is 200 units every other week, or 300 units every 3 weeks. Clinical trials comparing the two agents suggest similar results in terms of red cell production and need for transfusions. Data from a variety of trials have shown that anemia during treatment for advanced cancer is associated with a poorer outcome. In addition, correction of anemia is associated with improvement across all aspects of quality of life. This has led to trials evaluating the effect of prophylactic epoetin alfa during treatment for early-stage cancers. Clearly, this approach results in improved quality of life in the short term; however, no long-term differences have been demonstrated. The cost as well as potential side effects such as cerebrovascular events associated with high hemoglobin levels have discouraged the routine use of erythroid growth factors as prophylaxis for anemia. However, erythropoietic growth factors should be instituted when the hemoglobin falls to 11 g/dL if continued chemotherapy is planned, or at higher levels in older patients with comorbidities.
Thrombocytopenia remains a problem with high doses of or prolonged exposure to chemotherapeutic agents and may limit therapy. Oprelvekin (recombinant interleukin-11) may be used in treating and preventing chemotherapy-induced thrombocytopenia. It is less effective in treating very severe thrombocytopenia, and its use can be associated with significant fluid retention, arrhythmias, and congestive heart failure.
Commonly used short-acting drugs that affect the bone marrow include the alkylating agents (eg, cyclophosphamide, melphalan, chlorambucil), procarbazine, mercaptopurine, methotrexate, irinotecan, vinorelbine, dactinomycin, anthracyclines, taxanes, and others. The standard dosage schedules for tumor response often induce bone marrow suppression. Continuing some drugs in the face of falling blood counts may result in serious infectious complications or bleeding. Simple guidelines for treatment and follow-up can usually prevent this complication.
Table 40-5. A common scheme for dose modification of cancer chemotherapeutic agents.1 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
In patients with normal blood counts as well as normal liver and kidney function, drugs should be started in full dosages. Indeed, the effectiveness of many chemotherapeutic agents, particularly in the adjuvant setting, is dependent on maintaining dose and schedule for efficacy. Bone marrow toxicity is cumulative over time, and this must be anticipated during follow-up. Cumulative toxicity from long-term chemotherapy can require cessation of therapy or reduction in dose. Patients with bone marrow involvement may tolerate chemotherapy poorly initially, with improved counts on future cycles as the tumor burden is reduced.
Drug dosage may be modified as a function of the peripheral white blood cell count or platelet count (or both). These modifications assume that the blood counts are checked shortly before the next course of chemotherapy is to be administered. Dosage modifications should be avoided in the adjuvant setting when treatment is given with curative intent, and are used primarily for repeated courses of oral alkylator or antimetabolite therapy used to treat chronic, incurable disease. A scheme for dosage modification is presented in Table 40-5. Alternatively, the interval between drug courses can be lengthened, thereby permitting more complete hematologic recovery and repetition of full-dose chemotherapy. Both dosage modification and delay of chemotherapy limit the efficacy of treatment.
Dale D: Current management of chemotherapy-induced neutropenia: the role of colony stimulating factors. Semin Oncol 2003;30:3.
Lyman GH: Balancing the benefits and costs of colony-stimulating factors: a current perspective. Semin Oncol 2003;30:10.
Schwartzberg L et al: A multicenter retrospective cohort study of practice patterns and clinical outcomes of the use of darbepoetin alfa and epoetin alfa for chemotherapy-induced anemia. Clin Ther 2003;25:2781.
P.1682
Chemotherapy-Induced Nausea & Vomiting
A number of cytotoxic anticancer drugs induce nausea and vomiting. In general, these symptoms are thought to originate in the central nervous system rather than peripherally. Parenteral administration of agents such as doxorubicin, etoposide, or cyclophosphamide is usually associated with mild to moderate nausea and vomiting, whereas nitrosoureas, dacarbazine, and particularly cisplatin cause more severe symptoms. Combination chemotherapy can also cause severe symptoms. Antiemetics clearly reduce and often eliminate nausea and vomiting associated with these drugs and are especially useful in conjunction with cisplatin.
5-Hydroxytryptamine-3 receptor antagonists (ondansetron, granisetron, dolasetron) have now replaced other drugs as the primary agents for the prevention and treatment of emesis from chemotherapy. These drugs are serotonin receptor-blocking agents with few side effects. They are also effective against radiation-induced and postanesthetic emesis and can be useful in the treatment of delayed and refractory nausea and vomiting following chemotherapy. Ondansetron is administered by the parenteral route as a single dose of 32 mg prior to chemotherapy and may be repeated every 24 hours, or it may be given orally at a dose of 8 mg every 8 hours. Lower parenteral doses may be just as effective. Granisetron is given as a single dose of 10 mcg/kg intravenously 30 minutes before chemotherapy, or orally at a dose of 1–2 mg/d. The dose of dolasetron is 1.8 mg/kg intravenously or 100–200 mg orally before chemotherapy. The serotonin receptor-blocking agents are more effective when given in conjunction with dexamethasone. Palonosetron is a new selective serotonin receptor antagonist with strong binding to the receptor, a long halflife, and little interaction with other medications. It is an effective antiemetic for both acute and delayed nausea and vomiting caused by cancer chemotherapy. It is given as a one-time dose of 0.25 mg intravenously 30 minutes before the start of chemotherapy, and can be repeated as often as once a week. Dexamethasone has antiemetic effects when administered at a dosage of 6–10 mg either as a single dose prior to—or both prior to and every 6 hours following—the administration of chemotherapy for two to four total doses.
Substance P appears to have a causative role in chemotherapy-induced nausea. Its biologic actions are mediated through the neurokinin-1 receptor. A novel oral agent, aprepitant, is a selective high-affinity neurokinin-1 receptor antagonist that is effective in preventing chemotherapy-induced nausea. Two randomized trials comparing granisetron and dexamethasone with or without this agent showed a significant reduction in acute emesis following chemotherapy with cisplatin with the three-drug combination. In addition, aprepitant was effective in preventing delayed emesis from cisplatin. Aprepitant is approved for the treatment of acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy. It is given for 3 days beginning on the day chemotherapy starts.
Other active agents often used in combination as premedication for less emetogenic chemotherapy or as treatment for delayed nausea and vomiting include prochlorperazine, metoclopramide, thiethylperazine, and lorazepam. The phenothiazines (prochlorperazine, thiethylperazine) and metoclopramide can induce extrapyramidal side effects; their incidence is increased with prolonged use. Prochlorperazine is given at a dose of 10 mg orally or intravenously every 6–8 hours. The total dose given over 24 hours should not exceed 40 mg. A 25-mg suppository may be used for patients who are too nauseated to swallow pills without inducing further emesis. Metoclopramide is given at a dose of 10–20 mg orally or intravenously before and then every 6 hours after chemotherapy, usually in combination with dexamethasone. Lorazepam has both antiemetic and sedative effects and is administered at a dose of 0.5–1 mg every 4–6 hours by the sublingual or oral route, making it particularly useful in the outpatient setting. Older patients may experience intolerable psychological side effects.
Combinations of antiemetics are usually more effective than maximal doses of any one agent to block severe emesis. A typical antiemetic regimen might include ondansetron combined with sublingual lorazepam or prochlorperazine and dexamethasone with aprepitant for severely emetogenic regimens. For less emetogenic regimens, the serotonin antagonists can be reserved for failure to control nausea with less expensive regimens.
Dronabinol (D9-tetrahydrocannabinol) is effective in some patients at a dose of 5 mg/m2 prior to and then every 2–4 hours following chemotherapy for a total of four to six doses a day. Dronabinol may cause undesirable side effects such as dysphoria, and it is available only for oral administration.
A patient receiving antiemetics (eg, lorazepam, prochlorperazine, metoclopramide) along with chemotherapy on an outpatient basis must be escorted to and from the clinic, since the antiemetics often induce marked sedation and transient impairment of balance and reflexes. Antiemetics are more effective when given prophylactically. Therefore, regular dosing of an agent such as lorazepam or prochlorperazine is recommended after chemotherapy until the emetogenic effects have dissipated. This is dependent on the patient as well as on the type of chemotherapy administered. One problem with all combinations of antiemetic agents is the development of tachyphylaxis over 4–5 days with continuing highly emetogenic chemotherapy. This limits the effectiveness of any regimen. Acute mucosal injury to the upper gastrointestinal tract may complicate nausea associated with chemotherapy or delayed nausea and vomiting. Agents that reduce acid secretion (eg, omeprazole, ranitidine) can be useful adjunctive therapy to the antinausea regimen.
Bartlett N et al: Control of nausea and vomiting after chemotherapy: what is the evidence? Intern Med J 2002;32:401.
P.1683
Gralla RJ: New agents, new treatment, and antiemetic therapy. Semin Oncol 2002;29:119.
Hesketh PJ: New treatment options for chemotherapy-induced nausea and vomiting. Support Care Cancer 2004;12:550.
Schnell FM: Chemotherapy-induced nausea and vomiting: the importance of acute antiemetic control. Oncologist 2003; 8:187.
Gastrointestinal & Skin Toxicity
Chemotherapeutic agents generally act on rapidly proliferating cells, resulting in damage to the normal cells lining the gastrointestinal tract and mouth. This can result in mouth and throat sores, chronic nausea, and diarrhea. Erythema is an early sign of mucosal toxicity. Ulcerations in the mouth due to chemotherapy must be carefully evaluated for the presence of herpes simplex virus. Herpes ulcerations are common in immunosuppressed cancer patients and may be treated with acyclovir or other antiviral agents. Throat or esophageal pain may be due to either chemotherapy or infection from fungal or viral pathogens. These infections are more common in patients receiving steroids with their chemotherapy regimens. Chemotherapy should be delayed or withheld to allow healing or treatment of infection.
Adequate mouth care with antimicrobial mouthwashes and attention to dental hygiene are essential and may prevent severe toxicity. Common mouthwashes include the microbicidal oral rinse chlorhexidine and a mixture of salt and bicarbonate of soda in warm water, which aids in debridement of dead mucosa. A prophylactic antifungal mouthwash such as nystatin oral suspension may also be used. Certain chemotherapeutic agents can also cause toxicity to the skin, particularly the palms and soles and the skin in the axilla and groin. Common findings are erythema and hyperpigmentation, which may be painful or pruritic. Blistering is uncommon but can occur if chemotherapy is continued after the early signs of skin irritation occur. Toxicities to the gastrointestinal tract and skin may be more serious and harder to treat than bone marrow suppression. Patients receiving drugs that cause these side effects should be monitored closely.
Radiation therapy may cause xerostomia, which can lead to difficulty in swallowing, discomfort, and gum disease. Pilocarpine hydrochloride, 5–10 mg orally three times a day, can relieve symptoms of dry mouth but must be used regularly. Amifostine, a thiol-containing compound that reduces cisplatin-induced nephrotoxicity, has also been shown to reduce acute and chronic xerostomia in patients with head and neck cancers receiving radiation therapy. The dose of amifostine is 200 mg/m2 intravenously daily 15–30 minutes before irradiation. Side effects include nausea and vomiting.
Radiation therapy to areas that include the gastrointestinal tract can cause diarrhea that resolves gradually with cessation of therapy and healing of normal cells. Topical butyrate appears to improve symptoms of acute radiation proctitis following radiation therapy for malignant pelvic disease. The sodium butyrate is given per rectum. Skin toxicity in the form of erythema and occasionally blistering and exfoliation of the area receiving radiation can also occur. Severe skin toxicity requires holding the radiation doses; the affected area is treated with local application of emollients.
Miscellaneous Drug-Specific Toxicities
The toxicities of individual drugs have been summarized in Table 40-4. Several of these warrant additional mention, since they occur with commonly administered agents, and special preventive measures are often indicated.
A. HEMORRHAGIC CYSTITIS INDUCED BY CYCLOPHOSPHAMIDE OR IFOSFAMIDE
Metabolic products of cyclophosphamide that retain cytotoxic activity are excreted into the urine. Some patients appear to metabolize more of the drug to these active excretory products. If their urine is concentrated, the toxic metabolite may cause severe bladder damage. Patients receiving cyclophosphamide must be advised to maintain a high fluid intake. Early symptoms of bladder toxicity include dysuria and frequency despite the absence of bacteriuria. If microscopic hematuria develops, it is advisable to stop the drug temporarily or switch to a different alkylating agent, increase fluid intake, and administer a urinary analgesic such as phenazopyridine. With severe cystitis, large segments of bladder mucosa may be shed and the patient may have prolonged gross hematuria. Such patients should be observed for signs of urinary obstruction and may require cystoscopy for removal of obstructing blood clots. The risk of developing hemorrhagic cystitis is dose related and more common in patients who take the drug orally over a prolonged period of time. The cyclophosphamide analog ifosfamide or very high doses of cyclophosphamide can cause severe hemorrhagic cystitis when either is used alone. However, when they are used in conjunction with the neutralizing agent mesna, bladder toxicity can usually be prevented. Mesna is given with the chemotherapeutic agent and in a series of doses over the following 24 hours. Continuous bladder irrigation with 0.9% saline has been used with high-dose cyclophosphamide to prevent hemorrhagic cystitis. This appears to be less effective than mesna and may result in complications from Foley catheter trauma to the urethra, so it is used infrequently in high-risk situations—often in combination with mesna.
B. NEUROPATHY INDUCED BY VINCRISTINE AND OTHER AGENTS
Neuropathy is a toxic side effect that is peculiar to the vinca alkaloid drugs, especially vincristine and vinorelbine. A primarily sensory peripheral neuropathy is also commonly caused by two of the newer anticancer therapeutic agents, paclitaxel and docetaxel, as well as cis-
P.1684
platin, carboplatin, and topotecan. The peripheral neuropathy associated with vincristine can be sensory, motor, autonomic, or a combination of these effects. In its mildest form, it consists of paresthesias of the fingers and toes. Occasional patients develop acute jaw or throat pain after vincristine therapy. This may be a form of trigeminal or glossopharyngeal neuralgia. With continued vincristine therapy, the paresthesias may extend to the proximal interphalangeal joints, hyporeflexia can appear in the lower extremities, and weakness may develop in the quadriceps muscle group. At this point, it is wise to discontinue vincristine therapy until the neuropathy has subsided. A useful means of judging whether peripheral motor neuropathy is severe enough to warrant stopping treatment is to have the patient attempt to do deep knee bends or rise from a chair without using the arm muscles. In general, the neuropathy associated with paclitaxel and vinorelbine is mild, well-tolerated, and both dose sensitive and schedule sensitive. More frequent dosing of smaller amounts of chemotherapy can reduce this side effect; the neuropathy significantly improves when the chemotherapy is stopped.
Constipation is the most common symptom of autonomic neuropathy associated with vincristine therapy. Patients receiving vincristine or vinorelbine should be started on stool softeners and mild cathartics when therapy is begun; otherwise, severe impaction may result as a consequence of an atonic bowel. More serious autonomic involvement can lead to acute intestinal ileus with signs indistinguishable from those of an acute abdomen.
Bladder neuropathies are uncommon but may be severe. Paralytic ileus and bladder atony are absolute contraindications to continued vincristine therapy. The majority of symptoms from vincristine are mild and resolve slowly although often not completely after therapy has been discontinued. Peripheral neuropathy associated with paclitaxel, docetaxel, vinorelbine, cisplatin, carboplatin, and topotecan worsens over time and can be painful and debilitating.
C. METHOTREXATE TOXICITY AND LEUCOVORIN RESCUE
In addition to standard uses of methotrexate for cancer chemotherapy, this drug is also used in very high doses that could lead to fatal bone marrow toxicity if given without an antidote. High-dose methotrexate therapy with leucovorin rescue is routinely used to treat osteogenic sarcoma, acute lymphocytic leukemia, and some cases of non-Hodgkin's lymphoma as well as primary lymphoma of the central nervous system.
The bone marrow and mucosal toxicity of methotrexate can be prevented by early administration of leucovorin (folinic acid). Serum levels of methotrexate are usually monitored and doses of leucovorin adjusted accordingly. Rescue is required for methotrexate doses over 80 mg/m2 and is usually begun within 4 hours after completing treatment. Up to 100 mg/m2 of leucovorin is given initially every 6 hours, with further doses adjusted for the serum methotrexate level. Rescue is usually continued orally for 3 days or longer until the serum methotrexate level is below 0.05 mcmol/L. Asparaginase can be given as rescue for methotrexate in the treatment of lymphoblastic leukemia. If an overdose of methotrexate is administered accidentally, leucovorin therapy should be initiated as soon as possible, preferably within 1 hour. Intravenous infusion should be employed for larger overdosages to ensure adequate drug delivery. It is generally advisable to give leucovorin repeatedly in this situation. A new agent, carboxypeptidase G2, may be useful for the treatment of patients with methotrexate toxicity, and rapidly reduces high serum methotrexate levels. It is expected to obtain FDA approval in 2005.
Vigorous hydration and bicarbonate loading also appear to be important in preventing crystallization of high-dose methotrexate in the renal tubular epithelium. Serum creatinine is determined before beginning therapy and daily thereafter, since methotrexate excretion is slowed by renal insufficiency and toxicity will be enhanced. In high doses, methotrexate can itself cause renal injury. Methotrexate doses are reduced in renal insufficiency. Concomitant use of certain drugs will slow methotrexate excretion, and they are avoided during therapy. These drugs include aspirin, NSAIDs, penicillins, sulfonamides, and probenecid.
D. BUSULFAN TOXICITY
The alkylating agent busulfan, occasionally used for the treatment of myeloproliferative diseases, has curious delayed toxicities, including increased skin pigmentation, a wasting syndrome similar to that seen in adrenal insufficiency, and progressive pulmonary fibrosis. Patients who develop either of the latter two problems should be switched to a different drug (eg, melphalan) when further therapy is needed. The pigmentary changes are innocuous and will usually regress slowly after treatment is discontinued. Long-term treatment with busulfan also results in an increased risk of secondary leukemias.
E. BLEOMYCIN TOXICITY
Bleomycin is used to treat squamous cell carcinoma, Hodgkin's disease, non-Hodgkin's lymphoma, and testicular cancer. It can produce edema of the interphalangeal joints and hardening of the palmar and plantar skin. More serious toxicities include an anaphylactic or serum sickness-like reaction and a potentially fatal pulmonary fibrotic reaction (seen especially in elderly patients receiving a total dose of over 300 units). If a nonproductive cough, dyspnea, and pulmonary infiltrates develop, the drug is discontinued, and high-dose corticosteroids are instituted as well as empirical antibiotics pending cultures. Fever alone or with chills is an occasional complication of bleomycin and is not an absolute contraindication to continued treatment. The fever may be avoided by administra-
P.1685
tion of hydrocortisone just prior to the injection. Fever alone is not predictive of pulmonary toxicity. About 1% of patients (especially those with lymphoma) may have a severe or even fatal hypotensive reaction after the initial dose of bleomycin. To identify and treat such patients, it is wise to administer a test dose of 5 units of bleomycin first and to have adequate monitoring and emergency facilities available. Patients exhibiting a hypotensive reaction should not receive further bleomycin therapy.
F. ANTHRACYCLINE-INDUCED CARDIOMYOPATHY
The anthracycline antibiotics doxorubicin, daunomycin, and idarubicin and the similar drug mitoxantrone have both acute and delayed cardiac toxicity. The problem is greater with doxorubicin because it has a major role and is used in repeated doses in the treatment of sarcomas, breast cancer, lymphomas, acute leukemia, and certain other solid tumors. Studies of left ventricular function and endomyocardial biopsies indicate that changes in cardiac dynamics occur in most patients by the time they have received 300 mg/ m2 of doxorubicin. The multiple-gated (“MUGA”) radionuclide cardiac scan is the most reproducible noninvasive test for assessing toxicity. Patients should not receive a total dose in excess of 450 mg/m2, and 1–10% of patients who receive this dose develop cardiomyopathy. Doxorubicin should not be used in patients with intrinsic cardiac disease. Prior chest or mediastinal radiotherapy increases the risk of doxorubicin heart disease at lower total doses. The appearance of a high resting pulse may herald the appearance of cardiac toxicity. Unfortunately, the toxicity may be irreversible at dosage levels above 550 mg/m2. At lower doses (eg, 350 mg/m2), the symptoms and signs of cardiac failure generally respond well to medical therapy and cessation of doxorubicin.
Laboratory studies suggest that cardiac toxicity may be due to a mechanism involving the formation of intracellular free radicals in cardiac muscle. Pretreatment with dexrazoxane, an iron chelator that decreases free radical formation, appears to protect the myocardium from anthracycline-induced injury but may also reduce the anticancer efficacy of the anthracycline. Dexrazoxane is useful for the prevention of cardiomyopathy in women with metastatic breast cancer receiving cumulative doxorubicin doses > 300 mg/m2. Liposomally encapsulated doxorubicin and daunorubicin have been FDA approved and appear to have minimal cardiac toxicity. Their main use to date has been to treat Kaposi's sarcoma, but they are also effective in the treatment of other anthracycline-sensitive cancers. The anthracycline analog idarubicin has shown efficacy against acute nonlymphocytic leukemia and breast cancer when used in combination with other agents. Idarubicin appears to have a similar potential for causing cardiotoxicity when compared with other anthracyclines, though a maximum lifetime dosage recommendation has not been made. Epirubicin, an anthracycline with lower cardiac toxicity than doxorubicin (but similar gastrointestinal toxicity), is approved for the treatment of breast cancer. A dose of up to 900 mg/m2 can be tolerated without significant cardiac toxicity. There are no data comparing the effects of doxorubicin with epirubicin, which has been studied primarily in Europe and Canada.
G. CISPLATIN NEPHROTOXICITY AND NEUROTOXICITY
Cisplatin is effective in the treatment of testicular, bladder, and ovarian cancer as well as in several other types of tumor. Nausea and vomiting are common, but nephrotoxicity and neurotoxicity are more serious. Vigorous hydration with or without mannitol diuresis may substantially reduce nephrotoxicity. Renal function must be carefully monitored during cisplatin therapy, as should serum magnesium, which may fall during therapy with this agent. Ototoxicity is a potentially serious neurotoxicity that can result in deafness. Other manifestations include peripheral neuropathy of mixed sensorimotor type that may be associated with painful paresthesias. The neurotoxicity of this drug is delayed and is more common after a total dose of 300 mg/m2. The second-generation platinum analog carboplatin has been shown to be as effective as cisplatin in ovarian cancer. Carboplatin is less nephrotoxic and causes less severe nausea or vomiting, but it does induce significant myelosuppression along with neurotoxicity. Amifostine, an organic thiophosphate initially developed as a radioprotective agent, is effective in preventing renal toxicity from cisplatin. It is approved to reduce cumulative renal toxicity associated with repeat administration of cisplatin in advanced ovarian cancer. In addition, amifostine may reduce chemotherapy-induced hematologic toxicity and neurotoxicity. Glutathione also appears to be a promising agent in preventing cisplatin neurotoxicity. Glutathione has been given at a dose of 1.5 g/m2 intravenously before cisplatin administration, then at a dose of 600 mg by intramuscular injection on days 2–5. These supportive measures do not appear to reduce the therapeutic effectiveness of platinum agents.
H. INTERFERON-α TOXICITIES
Although interferon-a is generally tolerated in the standard doses listed in Table 40-4, it has significant toxicity with the higher doses required to treat CML and malignant melanoma and is more toxic in elderly patients. Even standard doses may be intolerable to some patients. Fever and chills are initial side effects but are infrequent after continued treatment. These symptoms may be ameliorated or prevented by premedication with acetaminophen and bedtime dosing. However, anorexia, fatigue, and weight loss can be cumulative and with time may become severe. These symptoms may be dose or treatment limiting. Thirty percent or more of patients are intolerant of interferon therapy even at low doses. In some patients, central
P.1686
nervous system symptoms develop, usually manifested as confusion or somnolence. Interferon causes a reduction in blood counts, but this is usually not clinically important and is part of the desired effect in the treatment of CML. Interferon-induced side effects are sometimes confused with the symptoms of progressive cancer but usually clear within 1–2 weeks following cessation of interferon therapy.
Brizel DM et al: Phase III randomized trial of amifostine as a radioprotector in head and neck cancer. J Clin Oncol 2000; 18:3339.
Chu E et al (editors): Physicians' Cancer Chemotherapy Drug Manual 2005. Jones & Bartlett, 2005.
Kremer LC et al: Frequency and risk factors of subclinical cardiotoxicity after anthracycline therapy in children: a systematic review. Ann Oncol 2002;13:819.
EVALUATION OF TUMOR RESPONSE
Inasmuch as cancer chemotherapy can induce clinical improvement, serious toxicity, or both, it is important to critically assess the beneficial effects of treatment in patients with advanced cancer to determine that the net effect is favorable. The most valuable signs to follow during therapy include the following.
TUMOR SIZE
Shrinkage in tumor size can be demonstrated by physical examination, chest film or other x-ray, sonography, or a procedure such as radionuclide bone scanning (breast, lung, prostate cancer). CT scanning is important for the evaluation of tumor size and location and the extent of distant spread for a wide variety of tumors and sites. MRI is now the best noninvasive means of evaluating posterior fossa brain tumors, spinal cord tumors, spinal cord compression, and pelvic disease, but CT scanning remains useful and may provide additional information. Sonography is also helpful in the evaluation of pelvic neoplasms. Gallium scanning can be useful to detect residual disease in lymphomas, but some tumors are not gallium avid, which limits the usefulness of this test. PET scanning is an emerging radiographic detection method that depends on metabolic activity for visualization. It appears to be very useful in detection of residual disease in lymphomas and in assessing the extent of disease in several solid tumors. PET combined with CT scans may allow a more accurate determination of response to therapy, differentiating between metabolically active residual tumor and scar. It may also help in evaluating resectable versus nonresectable or early metastatic disease.
A partial response (PR) is defined as a 50% or greater reduction in the original tumor mass. A complete response (CR) refers to the complete disappearance of detectable tumor. Progression is an increase of more than 25% in the size of the tumor or the appearance of any new lesions. Criteria for measuring responses of solid tumors have been established by the World Health Organization to avoid conflicts and inconsistency in measurements that influence reporting of tumor responses and to lead to more uniform reporting of outcomes of clinical trials. The RECIST criteria are based on measuring the largest single diameter of any tumor mass and include a minimum diameter for measurable lesions. These criteria are now incorporated into cancer treatment protocols.
The effectiveness of any agent or combination of agents in the treatment of cancer is determined by the response rates (combination of CR, PR, and, for some aggressive neoplasms, stable disease), response duration, and survival. Treatment efficacy for metastatic or incurable disease is often measured by event-free survival (EFS) or time to progression (TTP). The usefulness of treatment given to prevent recurrence of potentially curable neoplasms is measured by relapse-free survival (RFS) or disease-free survival (DFS) as well as overall survival (OS). The goal of effective palliative therapy for advanced incurable malignancy is to increase survival and improve quality of life. Newer agents and new delivery methods have expanded the treatment options and increased their tolerability for some common cancers. Generally, response to therapy is associated with palliation, but it often happens that just stabilization of disease will have the same effect. Tumor response in this setting must be measured against toxicity, and treatment decisions should be made after available options have been discussed with the patient and family. Because patients tend to have unrealistic expectations of the benefits of palliative chemotherapy, clinician–patient communication is critical.
TUMOR MARKERS
A decrease in the quantity of a tumor product or marker substance reflects a reduced amount of tumor in the body. Examples of such markers include paraproteins (abnormal immunoglobulins) in multiple myeloma and macroglobulinemia, human chorionic gonadotropin (hCG) in choriocarcinoma and testicular cancer, prostatic acid phosphatase and PSA in prostatic cancer, urinary steroids in adrenal carcinoma and paraneoplastic Cushing's syndrome, and 5-hydroxyindoleacetic acid (5-HIAA) in carcinoid syndrome.
Tumor-secreted fetal antigens are also used to follow the course and response to treatment of cancers. These include α1-fetoprotein (AFP) in hepatocellular carcinoma, testicular cancer, teratoembryonal carcinoma, and in occasional cases of gastric carcinoma; ovarian tumor antigen (CA 125) in ovarian cancer; and CEA in carcinomas of the colon, lung, breast, and pancreas. CA 15-3 and CA 27.29 may become important in detecting early recurrence of breast cancer but
P.1687
are mainly used to follow response to therapy in metastatic disease. The CA 19-9 radioimmunoassay is used to monitor response to therapy of pancreatic cancer. Monoclonal antibodies are now used for measurement of a number of tumor markers and offer the potential of delineating a number of additional markers for diagnostic purposes.
Tumor markers may play an important role in the early detection of some common tumors when combined with good physical examinations. PSA, an immunogenic glycoprotein produced solely by the prostate, is currently the only tumor marker with widespread (and controversial) use in cancer screening. PSA was initially used to indicate tumor bulk and disease progression, but it is now commonly used as a screening tool when paired with the digital rectal examination. The American Cancer Society National Prostate Cancer Detection Project is a multicenter study evaluating the use of PSA, DRE, and transrectal ultrasound (TRUS) in a large cohort of healthy men. In this and other studies, the combination of a monoclonal PSA greater than 4 ng/mL and an abnormal DRE was felt to produce a highly sensitive and specific method for detecting prostate cancer. A large Canadian study showed a significant reduction in death from prostate cancer in men undergoing regular screening. This study randomized more than 46,000 men aged 45–80 years to screening, with PSA (using 3 ng/mL as the upper limit of normal) and DRE followed by TRUS for abnormal test results or for a 10% increase in PSA over 12 months. There was an almost threefold advantage of screening and early treatment to reduce mortality.
Annual screening for prostate cancer with DRE and PSA beginning at age 50 years should be offered to men with a life expectancy of at least 10 years. Data obtained from the PLCO Screening Trial suggest that the initial PSA level can be used as a guide to direct frequency of testing. Thirty thousand men aged 55–74 years qualified for inclusion in the trial, and over 90% had normal PSA levels of < 4 ng/mL at baseline. A PSA < 1 ng/mL was associated with only a 1.4% chance of rise over 5 years, and a high percentage of those with a level of 1–2 ng/mL were normal over a period of 2 years. In contrast, 83% of those with an initial screening level of 3–4 ng/mL became abnormal over 5 years. The recommendations are to screen men with an initial level of < 1 ng/mL every 5 years, 1–1.9 ng/mL every 2 years, and ≥ 2 ng/mL yearly. It is estimated that this schedule could reduce PSA testing by 55%, with only a 2.6% risk of missing a positive test. As always, patients need to be involved in the decision to obtain screening PSA testing and should understand the advantages and possible consequences of testing or not testing. A major concern is that PSA testing will detect tumors that would not have resulted in mortality—small, slow-growing tumors in older men.
An abnormal PSA or DRE requires further evaluation by TRUS and possible biopsy. The role of PSA screening must be carefully evaluated for each patient and the risks of screening (unnecessary biopsies and surgeries) discussed in detail. The PSA may be elevated in benign prostatic hypertrophy and in prostatitis. Levels in benign disease are usually between 4 and 10 ng/mL; a level greater than 10 ng/mL increases the likelihood of finding cancer. In addition, 25–45% of patients with localized prostate cancer may have a normal PSA value. The increase in screening for prostate cancer over the past few years has markedly increased the reported incidence of this disease, though prostate cancer-specific mortality has been essentially stable. (See Table 40-1.) The PSA is also used to define early relapse following local treatment with surgery or radiotherapy. One recent study indicated that pelvic radiotherapy and adjuvant androgen deprivation initiated at the time when elevation of the PSA is detected significantly improve survival and decrease the death rate due to prostate cancer. This effect was most prominent in patients with more aggressive, highgrade disease.
Tumor markers may be useful to screen populations at high risk for a specific cancer. A recent study has shown that elevated and altered profiles of AFP can serve as predictive markers for the development of hepatocellular carcinoma in patients with cirrhosis. Most tumor markers are not specific or sensitive enough to be useful as screening tools owing to their frequent elevation in benign disease and their absence in some cases of malignancy. Although screening for ovarian cancer with CA 125 is still being investigated, a rapid fall in levels to normal (versus a slow fall or plateau) following surgery or chemotherapy has favorable prognostic significance.
In general, tumor markers are used to follow response to therapy of a specific cancer. In diseases where early treatment of recurrence can influence survival (eg, testicular cancer and now prostate cancer), tumor markers may be used to screen for recurrent disease before it becomes radiographically or clinically evident.
Andriole GL et al: Prostate cancer screening in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial: findings from the initial screening round of a randomized trial. J Natl Cancer Inst 2005;97:433.
Bast RC et al: 2000 update of recommendations for the use of tumor markers in breast and colorectal cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol 2001;19:1865.
Doyle C et al: Does palliative care palliate?; Evaluation of expectations, outcomes and costs in women receiving chemotherapy for advanced ovarian cancer. J Clin Oncol 2001;19: 1266.
Duffy MJ: Evidence for the clinical use of tumour markers. Ann Clin Biochem 2004;41:370.
Lieberman R: Evidence-based medical perspectives: the evolving role of PSA for early detection, monitoring of treatment response, and as a surrogate end point of efficacy for interventions in men with different clinical risk states for the prevention and progression of prostate cancer. Am J Ther 2004; 11:501.
P.1688
Smith RA et al: American Cancer Society guidelines for the early detection of cancer, 2003. CA Cancer J Clin 2003;53:27.
GENERAL WELL-BEING, PERFORMANCE STATUS, & SUPPORTIVE CARE
The functional status of the cancer patient at diagnosis (or at the start of treatment) is a major prognostic factor and determinant of outcome with or without tumor-directed therapy. It is therefore important to assess functional status as well as tumor burden and symptoms before deciding on possible anticancer therapy. Functional status or performance status evaluates the patient's ability to perform activities of daily living and is clearly related to tumor burden, tumor site, and the patient's underlying physical condition.
Two scales are commonly used to measure performance status. The Eastern Cooperative Oncology Group (ECOG) scale is a five-point system that is simple and easy to apply to clinical practice. The ECOG scoring system ranges from 0 to 4 as follows: 0, entirely asymptomatic; 1, symptomatic but fully ambulatory; 2, symptomatic and in bed less than 50% of the day; 3, symptomatic and in bed more than 50% of the day but not bedridden; and 4, bedridden. The Karnofsky scale ranges from 100% (asymptomatic and fully functional) through 0% (dead) in steps of 10%. For example, a Karnofsky performance status of 40% implies a patient who is disabled and requires special care and assistance. This patient would be unable to work but would be able to live at home with special assistance. These two systems are often the basis for clinical decisions despite their obvious lack of precision. They are also useful in assessing the impact of therapy and disease progression.
The measures assessing functional status described above do not adequately assess quality of life, a major goal of cancer chemotherapy. Performance status is only one component of quality of life, which is a combination of subjective and objective factors. Factors included in the assessment of general well-being include improved appetite and weight gain and decreased pain as well as improved performance status. In general, cancer patients perceive that they receive inadequate analgesia and have impairment of function because of pain. The adequate use of pain medications is hampered by their sedating side effects (see Chapter 5). New guidelines for the management of pain and longacting opioids delivered by a transdermal system may help (eg, fentanyl patch, changed every 3 days). In addition, a short-acting oral transmucosal fentanyl preparation is available that may allow easier titration of analgesia. Tramadol is a centrally acting synthetic opioid analgesic that is available alone or in combination with acetaminophen for management of acute pain.
Sedating effects can sometimes be avoided by adding nonsteroidal anti-inflammatory agents or antidepressants to opioid therapy. Gabapentin can be a useful adjunct to management of pain characterized by nerve compression-like symptoms and can also treat insomnia if given at bedtime. In general, depression is underdiagnosed and undertreated by clinicians; treatment of depression in patients with advanced cancer has been shown to improve functional status. Occasionally, opioids may be given epidurally to relieve severe pain. As with the use of antiemetics, pain medications work better when given prophylactically on a regular schedule rather than as needed for chronic or severe pain. It is only by completely evaluating all of the factors described above that the physician is able to judge whether the net effect of chemotherapy is worthwhile palliation. See Chapter 5 for further discussions of pain management and care at the end of life.
In addition to opioids, agents that inhibit bone resorption may decrease bone pain and protect against skeletal complications (thereby improving quality of life) in patients with cancer metastatic to bone. Either the bisphosphonate pamidronate or the more potent zoledronic acid is well tolerated; the indications for zoledronic acid are broader and include both lytic and blastic bone lesions in any type of cancer. Pamidronate is given at a dosage of 90 mg intravenously over 2 hours once a month; zoledronic acid is given at a dosage of 4 mg intravenously over 15 minutes once a month. In addition to spot radiation, two radioactive agents are available for the palliation of bone pain. Strontium-89 and samarium-153 lexidronam are both given intravenously and have been shown to be effective in reducing bone pain from osteoblastic lesions. The major toxicity is hematopoietic suppression, which may limit the ability to provide other palliative therapy. The use of agents such as pamidronate or zoledronic acid, growth factors such as epoetin alfa (erythropoietin) or darbopoetin, and appetite stimulants such as megestrol acetate (given in dosages ranging from 40 mg orally four times a day up to 800 mg once a day) or dronabinol can improve the quality of life for cancer patients. Mucositis can be a problem that is particularly severe in patients with hematologic malignancies receiving inpatient high dose chemotherapy. Palifermin is a human keratinocyte growth factor (KGF) with improved protein stability produced by recombinant DNA technology in Escherichia coli that was recently FDA approved for mucositis prevention in patients with hematologic malignancies. Palifermin binds to the KGF receptor to stimulate proliferation, differentiation, and migration of epithelial cells. In randomized, placebo-controlled clinical trials, palifermin reduced the duration and incidence of severe mucositis as well as the use of narcotics. The safety of palifermin in patients with nonhematologic malignancies has not yet been established.
As early detection of cancer increases and cancer therapy improves, a growing area of concern is the long-term care of cancer survivors. Careful attention must be paid to psychosocial as well as physical problems resulting from therapy. Chemotherapy often leads to early menopause, depression, sexual difficul-
P.1689
ties, and osteoporosis, among other problems. Longterm cognitive problems are related to intensity and type of therapy. Clinician awareness and referral to the appropriate resources are critical for maintaining quality of life in patients who are “survivors.” Patient advocacy groups can play a very important role in patient education and support. Local groups can be located through cancer resource centers or at the local branch of the American Cancer Society.
Chang HM: Pain and its management in patients with cancer. Cancer Invest 2004;22:799.
Hilner BE et al: American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 2003;21:4042.
Kattlove H et al: Ongoing care of patients after primary treatment for their cancer. CA Cancer J Clin 2003;54:172.
Lewington VJ: Bone-seeking radionuclides for therapy. Nucl Med 2005;46(Suppl 1):38S.
Pfeilschifter J et al: Osteoporosis due to cancer treatment: pathogenesis and management. J Clin Oncol 2000;18: 1570.
Ronson A et al: Psychosocial rehabilitation of cancer patients after curative therapy. Support Care Cancer 2002;10:281.
Stasi R et al: Cancer-related fatigue: evolving concepts in evaluation and treatment. Cancer 2003;98:1786.
CANCER COMPLICATIONS: DIAGNOSIS & MANAGEMENT
ONCOLOGIC EMERGENCIES
Cancer is a chronic disease, but acute emergencies may occur as a consequence of local involvement (spinal cord compression, superior vena cava syndrome, malignant effusions, etc) or generalized systemic effects (hypercalcemia, opportunistic infections, hypercoagulability, hyperuricemia, etc). These complications may be the presenting manifestation of cancer. Two relatively common complications covered elsewhere will not be discussed here: superior vena cava syndrome (Chapter 12) and hypercoagulability (Chapter 13).
Brigden ML: Hematologic and oncologic emergencies. Doing the most good in the least time. Postgrad Med 2001;109:143.
Krimsky WS et al: Oncologic emergencies for the internist. Cleve Clin J Med 2002;69:213.
Merrill P: Oncologic emergencies. Lippincotts Prim Care Pract 2000;4:400.
1. Spinal Cord Compression
Spinal cord compression by tumor mass is manifested by back pain, progressive weakness, and sensory loss (usually in the lower extremities). Less commonly, spinal cord disease may present as chest or abdominal pain or as signs of nerve root compression due to the epidural location of the tumor. Bowel and bladder dysfunction are late findings. Spinal cord compression may occur as a complication of metastatic solid tumor, lymphoma, or myeloma. Back pain at the level of the spinal cord lesion occurs in over 80% of cases and may be aggravated by lying down, weight-bearing, sneezing, or coughing. Because back pain may precede the development of neurologic symptoms or signs, it is important to investigate this complaint thoroughly in any patient with cancer.
If neurologic deficits are present at diagnosis, they are usually irreversible, though treatment immediately after symptoms develop may result in partial recovery. Neurologic impairment can progress rapidly. Treatment of early lesions may completely avoid significant compromise. Although patients who present with paralysis may not recover function, they should still be treated for pain relief and to limit the extent of progression. In addition, patients may respond to systemic therapy depending on the specific tumor type.
The diagnosis of spinal cord compression is made by MRI scan with contrast. With this noninvasive and sensitive test, it is possible to obtain detailed views of the area in question as well as sagittal images of the entire spinal cord and vertebral canal. With the increasing availability of MRI scanning to evaluate bony lesions of the spine, true spinal cord compression has become increasingly uncommon as radiation is used earlier in the course of disease for local control. A detailed examination is important for detection and treatment of multiple lesions. Bone radiographs and bone scans are useful for detecting vertebral metastases, but they do not aid in assessing spinal cord compromise.
Emergency Treatment
Classic treatment of spinal cord compression from tumor metastases has included corticosteroids and radiation therapy to the area of compression as well as two adjacent vertebrae above and below the lesion, with surgery reserved for progression following radiation. However, a recent randomized controlled trial in patients with spinal cord compression involving no more that two vertebral levels demonstrated a marked improvement in outcome in patients treated with surgery followed by radiation versus those treated with radiation alone—so dramatic that the trial was closed early. Patients receiving combined therapy were more likely to walk and regain mobility—and actually walked for more total time, with a trend toward longer survival compared with those who received radiation without surgery. Based on this observation, surgery followed by radiation has become the standard of care for patients presenting with limited spinal cord compression from metastatic cancer.
High doses of glucocorticoids (usually dexamethasone, 10–100 mg intravenously) are administered as
P.1690
soon as the diagnosis is suspected or confirmed. A lower dose (eg, 4–6 mg every 6 hours intravenously or orally) is continued throughout the course of radiation therapy and tapered at or near the end of treatment. Chemotherapy is useful in treating lymphomas and multiple myeloma in conjunction with or following completion of radiation therapy.
2. Leptomeningeal Disease
Leptomeningeal disease, or carcinomatous meningitis, is an uncommon complication occurring in about 3–8% of all cancer patients, though it is being diagnosed more frequently with improved imaging studies and increased longevity in patients with advanced cancer. The most common tumors involving the meninges are cancers of the breast and lung and malignant melanoma. Patients present with varied symptoms, including sequential cranial nerve abnormalities, stroke, and hydrocephalus. The diagnosis is made by finding malignant cells on cerebrospinal fluid cytologic examination or by enhancement of the meninges on gadolinium-enhanced MRI scans. The prognosis is poor, with median survival ranging from 3 to 6 months despite treatment.
Emergency Treatment
Treatment is by radiation to symptomatic areas (usually whole brain and spinal cord) or with intrathecal chemotherapeutic agents, most commonly methotrexate and cytarabine. For this purpose, an intraventricular reservoir system is recommended. Aggressive therapy (particularly the combination of intrathecal therapy and radiation) can be complicated by necrotizing leukoencephalopathy. Patients with chemotherapy-sensitive cancers and an excellent performance status have the best chance of benefiting from therapy. Temozolomide, a newer agent approved for treatment of primary brain tumors, is being tested as a treatment for recurrent metastatic disease to the brain as well as leptomeningeal disease with some preliminary success. Temozolomide is given orally for 5 days each month; its primary side effects are nausea and cytopenias.
Bayley A et al: A prospective study of factors predicting clinically occult spinal cord compression in patients with metastatic prostate carcinoma. Cancer 2001;92:303.
Kesari S et al: Leptomeningeal metastases. Neurol Clin 2003;21: 25.
Quinn JA et al: Neurologic emergencies in the cancer patient. Semin Oncol 2000;27:311.
Schiff D: Spinal cord compression. Neurol Clin 2003;21:67.
3. Hypercalcemia
Hypercalcemia occurs in 10–20% of patients with cancer. Common causes include breast, lung, kidney, and head and neck carcinomas as well as multiple myeloma and lymphoma. Although the majority of cancers associated with hypercalcemia metastasize to the bones, approximately 20% of cases are not associated with bony lesions. The identification of a novel protein called parathyroid hormone-related protein (PTHrP) has revised some previously held views about the pathogenesis of hypercalcemia. Radioimmunoassays have identified this peptide in the serum of approximately two-thirds of cancer patients with hypercalcemia. High levels have been found in patients with hypercalcemia that was previously thought to be due solely to local osteolysis. PTHrP may become a useful tumor marker in normocalcemic patients. In addition, antibodies to PTHrP may be useful as treatment.
The symptoms and signs of hypercalcemia include nausea, vomiting, constipation, polyuria, muscular weakness and hyporeflexia, confusion, psychosis, tremor, and lethargy. Some patients may be asymptomatic. Electrocardiography often shows a shortening of the QT interval. The presence of hypercalcemia does not invariably indicate a dismal prognosis, especially in breast or prostate cancer and multiple myeloma or lymphoma. In the absence of signs or symptoms of hypercalcemia, a laboratory finding of elevated serum calcium should be rechecked to exclude the possibility of laboratory error. The most common cause of hypercalcemia is hyperparathyroidism; caution should be exercised when evaluating a mildly elevated calcium in a patient with a history of localized cancer.
Emergency Treatment
A. HYDRATION
Emergency treatment consists of aggressive intravenous hydration with 3–4 L/d of 0.9% saline followed by diuresis with 10–40 mg of intravenous furosemide. It is essential that the patient be well hydrated before beginning diuretic therapy and that hydration be maintained after diuresis is initiated. Although hydration alone is effective at slowly reducing the calcium level, it is rarely sufficient treatment and can lead to problems with fluid overload.
B. DRUG THERAPY
There are several options for the emergent treatment of hypercalcemia used in conjunction with aggressive hydration.
1. Bisphosphonates— Bisphosphonates are potent inhibitors of osteoclast bone resorption and are currently the most important and least toxic agents for the treatment of cancer-related hypercalcemia. Zoledronic acid is the most potent bisphosphonate available and has replaced pamidronate disodium as the treatment of choice for malignant hypercalcemia. A single 15minute intravenous infusion of 4 mg with adequate hydration produces complete normalization of serum calcium in less than 3 days in 80–100% of patients— with a more rapid onset and duration of effect than pamidronate. Zoledronic acid administration can be repeated as necessary to control hypercalcemia. The most commonly reported side effects have been transient fever, myalgias, and an infusion site reaction.
P.1691
Zoledronic acid has also been found to reduce the incidence of new skeletal lesions and decrease pain from bone disease in cancers with metastatic lesions to bone.
2. Gallium nitrate— Gallium nitrate exerts a hypocalcemic effect by inhibiting calcium resorption from bone. For treatment of hypercalcemia, gallium nitrate is given at a dose of 200 mg/m2/d by continuous intravenous infusion for 5 days. Gallium nitrate is superior to calcitonin both in reducing calcium levels acutely and in keeping the levels low after treatment is completed. Renal function must be carefully monitored. It may take 3–4 days to see the maximum hypocalcemic effect from gallium nitrate; the effect lasts for about 5 days so other treatment must be instituted.
3. Calcitonin— Synthetic calcitonin-salmon works immediately to inhibit bone resorption, however, the effect is short-lived. The usual dose of 4 international units/kg intramuscularly, subcutaneously, or intranasally every 12 hours may be increased to 8 international units/kg every 12 hours after 1–2 days. Calcitonin-salmon alone is not effective at lowering serum calcium levels but can be added to zoledronic acid if necessary for resistant hypercalcemia. Repeated treatment with calcitonin is usually not as effective, and tachyphylaxis usually occurs after 1–3 days of treatment.
4. Other drugs— Prednisone has not been shown to be effective as a single agent to treat hypercalcemia, though it can be used in diseases that are responsive to steroids such as multiple myeloma or lymphoma. Refractory hypercalcemia may be treated with intravenous plicamycin, 25 mcg/kg/d for 3 or 4 days. Although often effective, its effect may be short-lived, and its use is often associated with hepatic, renal, and bone marrow toxicity.
C. CHEMOTHERAPY
Patients with breast cancer may develop hypercalcemia as a “flare” associated with bone pain after initiation of estrogen or antiestrogen therapy. These patients often achieve excellent tumor response with continued therapy. Tumors may respond to chemotherapy or radiation therapy, leading to resolution of hypercalcemia. If chronic hypercalcemia persists and is refractory to chemotherapy, pamidronate and aggressive oral hydration may be tried but are unfortunately rarely effective for long. When the more potent bisphosphonates become available in oral formulations, the management of chronic hypercalcemia may improve.
Body JJ: Hypercalcemia of malignancy. Semin Nephrol 2004;24: 48.
Conte P et al: Bisphosphonates in the treatment of skeletal metastases. Semin Oncol 2004;31:59.
Leyland-Jones B: Treatment of cancer-related hypercalcemia: the role of gallium nitrate. Semin Oncol 2003;30:13.
Major P: The use of zoledronic acid, a novel, highly potent bisphosphonate, for the treatment of hypercalcemia of malignancy. Oncologist 2002;7:481.
4. Hyperuricemia & Acute Urate Nephropathy
Hyperuricemia can occur both as a complication of rapidly proliferating malignancies or with treatmentassociated tumor lysis of hematologic malignancies such as leukemia, lymphoma, and multiple myeloma. Neoplasms with a high nucleic acid turnover such as acute leukemia and lymphoma may present with elevated serum uric acid and associated renal insufficiency. This problem may be compounded by use of thiazide diuretics, which decreases urate excretion. If a patient presents with hyperuricemia, care must be taken to reduce the uric acid before institution of cancer therapy. Patients at risk for tumor lysis syndrome should be followed with twice-daily measurements of uric acid, phosphate, calcium, and creatinine for the first 2–3 days following initiation of chemotherapy. Rapid elevation of serum uric acid can result in acute urate nephropathy caused by uric acid crystallization in the distal tubules, collecting ducts, and renal parenchyma. A serum urate concentration above 15 mg/dL is associated with a high risk of uric acid nephropathy. Gouty arthritis is usually a problem only in patients with a history of gout.
Prophylactic therapy consists of decreasing the production and increasing the renal excretion of uric acid. Allopurinol is a competitive inhibitor of xanthine oxidase and prevents conversion of highly soluble hypoxanthine and xanthine to the relatively insoluble uric acid. Twelve to 24 hours before beginning chemotherapy, a dose of 600 mg is given, followed by 300 mg/d during the period of high risk. Higher doses (up to 900–1200 mg/d) are used when severe hyperuricemia is anticipated following chemotherapy. Patients receiving the purine antagonists mercaptopurine or azathioprine should be given only 25–35% of the calculated dose of chemotherapy if they are also receiving allopurinol, since the latter drug will potentiate both the therapeutic effects and the toxicity of these agents. Renal excretion of uric acid is enhanced by maintaining a high urinary flow and by alkalinizing the urine to prevent uric acid crystallization, which occurs at acid pH. The urine can be alkalinized with 6–8 g of oral sodium bicarbonate per day or by adding two or three ampules of sodium bicarbonate to 1 L of D5W by infusion. Alkaline diuresis to maintain a urine pH near 7.0 is required only for prophylaxis in patients expected to have a rapid tumor response with marked hyperuricemia.
A new option for the treatment of tumor-related hyperuricemia now exists. Rasburicase is a recombinant urate oxidase enzyme that converts uric acid to allantoin, which is more easily excreted in the urine due to enhanced solubility. A randomized trial in pediatric patients demonstrated that rasburicase was more effective than allopurinol in controlling uric
P.1692
acid. Rasburicase is given at a dose of 0.2 mg/kg by intravenous injection once a day.
Emergency Treatment
Emergency therapy for established severe hyperuricemia consists of (1) hydration with 2–4 L of fluid per day; (2) alkalinization of the urine with 6–8 g of sodium bicarbonate per day; (3) allopurinol, 900–1200 mg/d; and (4) in severe cases, emergency hemodialysis. When severe hyperuricemia is present, adequate therapy may be impossible because of associated renal insufficiency and inadequate urinary output. Intravenous allopurinol and rasburicase are available for use in patients unable to tolerate the oral form of this drug. Even if renal failure occurs and dialysis is required, renal function may return to normal after the acute tumor lysis has resolved.
Cairo MS: Prevention and treatment of hyperuricemia in hematological malignancies. Clin Lymphoma 2002;3(Suppl 1):S26.
Davidson MB et al: Pathophysiology, clinical consequences, and treatment of tumor lysis syndrome. Am J Med 2004;116:546.
Goldman SC: Rasburicase: potential role in managing tumor lysis in patients with hematological malignancies. Expert Rev Anticancer Ther 2003;3:429.
5. Malignant Carcinoid Syndrome
Although tumors of argentaffin cells are uncommon, they are important because they secrete a variety of vasoactive materials. These include serotonin, histamine, catecholamines, prostaglandins, and vasoactive peptides. Carcinoid syndrome is usually associated with carcinoid tumors of the small bowel metastatic to the liver and, less commonly, with primary carcinoid tumors in other sites such as the lung or stomach. These tumors tend to metastasize early but have a relatively indolent course, making control of the syndrome important. Related syndromes occur in patients with pancreatic tumors secreting vasoactive peptides, which can cause severe watery diarrhea (pancreatic cholera).
The manifestations of carcinoid syndrome include facial flushing, edema of the head and neck (especially with bronchial carcinoid), abdominal cramps and diarrhea, bronchospasm, cardiac lesions (tricuspid or pulmonary stenosis or regurgitation), telangiectasias, and increased urinary 5-HIAA. The most common symptoms are flushing and diarrhea. The diagnosis is made by finding elevated levels of 5-HIAA in a 24-hour urine collection. Patients with symptomatic carcinoid usually excrete more than 25 mg of 5-HIAA per day in the urine. Ideally, all drugs and serotonin-rich foods such as bananas should be withheld for several days before beginning the urine collection.
Emergency Treatment
Emergency therapy for patients with symptomatic bronchial carcinoid includes prednisone, 15–30 mg/d. The associated abdominal cramping and diarrhea of intestinal carcinoids can often be managed by hydration and diphenoxylate with atropine. For severe diarrhea, the H1-histamine receptor antagonist cyproheptadine (4 mg orally three times daily) or an antiserotonin agent such as methysergide maleate (2 mg orally three times daily until 16 mg has been given) may be effective. Other useful agents include cimetidine and the phenothiazines.
The synthetic peptide somatostatin agonist, octreotide acetate, is the most effective agent for reducing symptoms due to the carcinoid syndrome in association with achieving a reduction in levels of urinary 5-HIAA. The dosage of octreotide in carcinoid syndrome is 100–600 mcg/d in two to four divided doses by subcutaneous injection. Octreotide is also effective in the treatment of symptoms related to vasoactive intestinal peptide-secreting pancreatic tumors (VIPomas), markedly reducing the watery diarrhea syndrome associated with this neoplasm. The dose of octreotide used to treat patients with VIPomas is 200–300 mcg/d in two to four divided doses.
Surgery is important in the treatment of localized carcinoid. Chemotherapy is moderately effective for patients with progressive advanced-stage disease. Active agents include fluorouracil, streptozocin, dacarbazine, cisplatin, doxorubicin, and interferon-α.
Boushey RP: Carcinoid tumors. Curr Treat Options Oncol 2002; 3:319.
Fink G et al: Pulmonary carcinoid: presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest 2001;119:1647.
Kulke MH: Neuroendocrine tumours: clinical presentation and management of localized disease. Cancer Treat Rev 2003;29: 363.
OTHER COMPLICATIONS
MALIGNANT EFFUSIONS
The development of effusions in the pleural, pericardial, and peritoneal spaces may be the presenting sign of some tumors or may cause diagnostic and therapeutic problems in patients with advanced neoplasms. Although the cause of an effusion can be elusive in a newly diagnosed asymptomatic patient, it is rarely difficult in the patient with advanced cancer. Approximately 50% of undiagnosed effusions in patients not known to have cancer will be malignant. The differential diagnosis includes congestive heart failure, pulmonary embolism, trauma, and infections such as tuberculosis. Direct involvement of the serous surface of the involved space with tumor appears to be the most frequent initiating factor, though many other mechanisms such as obstruction of lymphatic drainage that control the flow of fluid in the pleural space may play a role.
P.1693
Most patients with pleural or pericardial effusions are symptomatic at presentation with chest pain, shortness of breath, or cough. The diagnosis is made by tapping the involved space. Pericardial effusions are aspirated under fluoroscopic guidance or direct vision through a subxiphoid incision. The fluid should be heparinized and sent for cell count and differential, protein content, lactate dehydrogenase level, and cytologic study. The gross appearance of the fluid is often helpful as well. Bloody effusions are usually due to cancer but occasionally are due to pulmonary embolism, tuberculosis, or trauma. Chylous effusions may be associated with thoracic duct obstruction or may result from enlarged mediastinal lymph nodes in lymphoma. If the cytologic smear is negative on two occasions but the suspicion of tumor is still high, closed pleural biopsy may be helpful.
The management of effusions should be appropriate to the severity of involvement. Treatment of the underlying neoplasm would be ideal but is often not effective in controlling local effusions. Treatment may result in palliation and improve short-term survival when there is substantial pulmonary or cardiac compromise. Diuretics are used as initial treatment for small to moderate-sized peritoneal effusions and as an adjunct to drainage of large effusions to minimize the possibility of reexpansion pulmonary edema that can occur after thoracentesis. Small or loculated effusions may require ultrasonographic localization, but drainage of a large pleural or peritoneal effusion can be accomplished rapidly using an intravenous catheter and phlebotomy tubing connected to a vacuum bottle. Thoracentesis alone controls fewer than 10% of effusions but may be useful in conjunction with systemic chemotherapy for sensitive tumors (eg, lymphoma, small cell lung cancer, breast cancer). Pleural effusions may occasionally be managed by closed water-seal drainage with a chest tube for 3–4 days; this procedure is usually performed in conjunction with chemosclerosis (see below). The aim of pleural drainage is to allow the pleural surfaces to come into close contact and become adherent.
Recurrent symptomatic effusions can often be controlled by drainage followed by chemosclerosis. In this procedure, a chemotherapeutic or nonchemotherapeutic agent is instilled with or without lidocaine into the involved space. The intended effect is local inflammation and sclerosis to encourage adherence of the serosal surfaces. Several drugs used in the past for this purpose have been abandoned because of severe pain or systemic toxicity, including myelosuppression. The agent in primary use at present is talc; other agents include bleomycin and the anthracenedione compound mitoxantrone.
Five randomized trials have evaluated the efficacy and safety of talc poudrage compared with a control procedure. For the 89 evaluable patients, there was an 89% success rate, with a range of 75–100%. For these reasons as well as cost considerations, talc is now the sclerosing agent of choice for malignant pleural effusions, and is the only FDA-approved substance for this purpose. The primary side effects are fever and pain, with rare acute pneumonitis.
Bleomycin is also effective at controlling pleural effusions. The major side effects of bleomycin are pain, fever, and hypersensitivity reactions. Mitoxantrone has been reported to be effective in controlling malignant pleural effusions, causing minimal fever and local pain. However, one trial evaluated the effectiveness of mitoxantrone versus chest tube alone and found no differences in response or in duration of response. The instillation of sclerosing agents may best be reserved for patients who fail pleural tube drainage alone.
Sclerosis is generally less useful for the management of malignant ascites, but success has been reported using bleomycin, mitoxantrone, doxorubicin, thiotepa, and other agents.
Before instilling the sclerosing agent, it is important that the space be drained as thoroughly as possible. For pleural effusions, a small-bore chest tube or pigtail catheter is usually placed and fluid is removed by negative suction until the drainage is under 100 mL/d and the lung has expanded. Sclerotherapy is ineffective if there is a large residual effusion. Talc is insufflated into the pleural space via a thoracoscope or instilled in a 5 g slurry in sodium chloride via a chest tube. Talc instillation through a chest tube or via a thoracoscope can be done quickly, has minimal complications, and appears highly effective. To use chemotherapeutic agents, the patient is premedicated with an opioid, and 60 units of bleomycin or 30 mg of mitoxantrone in 50–100 mL of 0.9% saline is instilled directly into the chest tube. Regardless of whether talc or chemotherapy is instilled, the chest tube is then clamped, and the patient is placed in different positions every 15 minutes for 4 hours to distribute the agent equally within the pleural space. At the end of this period, the clamp is removed and the chest tube is allowed to drain with suction. After 24 hours, the chest tube is removed from suction, and when the drainage is minimal, the tube is removed. The whole process takes 3–5 days. Occasionally, repeated doses of the sclerosing agent may be required to stop persistent reaccumulation of the effusion.
In some situations, the daily drainage of the effusion is continuously greater than 100 mL/d, making sclerosis procedures impossible. One option for these patients is the placement of an indwelling pleural drainage catheter with a valve that allows intermittent home drainage of the effusion. This catheter is also being tested in the management of malignant ascites. Use of this catheter is reserved for patients with a limited life expectancy, as the risk of infection and blockage reduces long-term effectiveness. Pleuroperitoneal shunting may have limited value in selected patients with high performance status who can participate actively in pumping the shunt for 5–10 minutes four times a day while in a supine position. For the first 24 hours after shunt placement, the catheter must be
P.1694
pumped frequently to drain the accumulated fluid; this is usually done in the hospital. Pleurectomy has a high complication rate but offers excellent control of effusion in carefully selected patients. For malignant pericardial effusion, a pericardial window or stripping also offers good control with a lower complication rate and may also be performed for constrictive pericarditis following radiation therapy to the chest.
Lee YC et al: Management of malignant pleural effusions. Respirology 2004;9:148.
Link KH et al: Intraperitoneal chemotherapy with mitoxantrone in malignant ascites. Surg Oncol Clin North Am 2003; 12:865.
Marchi E et al: Management of malignancy-associated pleural effusion: current and future treatment strategies. Am J Respir Med 2003;2:261.
Ohm C et al: Use of an indwelling pleural catheter compared with thorascopic talc pleurodesis in the management of malignant pleural effusions. Am Surg 2003;69:198.
Speigler PA et al: Rapid pleurodesis for malignant pleural effusions. Chest 2003;123:1895.
Weatherhead M et al: Chemotherapeutic management of malignant pleural effusion. Expert Opin Pharmacother 2004;5: 1233.
INFECTIOUS COMPLICATIONS
The reader is referred also to the section on infections in the immunocompromised patient in Chapter 30.
Many patients with cancer have increased susceptibility to both bacterial and opportunistic infections. This may result from impaired host defense mechanisms (eg, Hodgkin's or non-Hodgkin's lymphoma, CLL, multiple myeloma, acute leukemia or preleukemia) or from the myelosuppressive and immunosuppressive effects of cancer chemotherapy. Impaired host defense mechanisms include defects in neutrophil function, abnormalities in antibody production, depressed cell-mediated immune function, impairment of mechanical barriers by indwelling intravenous catheters, and impairment of mucosal integrity. At least half of the infections seen in neutropenic patients are believed to be endogenous.
The bacterial organisms accounting for the majority of infections in cancer patients include Enterobacteriaceae (Klebsiella, Enterobacter, Serratia, E coli), Pseudomonas, Staphylococcus, and Streptococcus. Other important pathogens include Corynebacterium, Clostridium difficile, Mycobacterium, and Legionella. Patients with prolonged neutropenia or those who have undergone bone marrow transplantation are at risk for infections with fungi such as Candida, Aspergillus, and Pneumocystis and with viruses such as herpes zoster, cytomegalovirus, respiratory syncytial virus, and influenza virus. Infections with resistant bacteria, such as vancomycin-resistant Enterococcus, are being seen with increasing frequency. The incidence of bacteremia rises dramatically when the white count is less than 1000/mcL or when there are fewer than 200 granulocytes per microliter. In patients with neutropenia, hematologic malignancies, or following bone marrow transplantation, infection must be treated emergently and empirically. Although fever may be due to multiple causes, including mucositis, drugs, and the malignancy itself, infection must be the first consideration and may be present even in the absence of fever, especially in patients who are receiving glucocorticoids. Negative cultures in febrile neutropenic patients do not rule out infection, and treatment should be instituted immediately without waiting for culture results to become available. If an indwelling line is present, blood cultures should be drawn from the periphery as well as through the line itself.
Prevention
Details of prevention in immunocompromised hosts are outlined in Chapter 30.
Prophylaxis of infections in high-risk or neutropenic patients can prevent the complications of sepsis. Two randomized clinical trials tested oral versus intravenous antibiotic therapy for hospitalized low-risk febrile patients with neutropenia during cancer chemotherapy. Oral ciprofloxacin plus amoxicillin and potassium clavulanate appeared as effective as intravenous ceftazidime or ceftriaxone and amikacin, indicating that for low-risk patients, outpatient therapy is feasible and safe.
In patients who are severely immunocompromised, some bacterial infections may be prevented with intravenous immune globulin. This is important in patients with chronic lymphocytic leukemia, multiple myeloma, and following bone marrow transplantation if associated immunoglobulin deficiencies are observed.
The availability of recombinant bone marrow growth factors has helped to reduce the morbidity and mortality of infections in immunocompromised hosts. G-CSF (filgrastim and pegfilgrastim) and GM-CSF (sargramostim) have been shown to be effective at reducing the duration of neutropenia and the frequency and severity of infection after myelosuppressive chemotherapy or autologous bone marrow transplantation for nonmyeloid malignancies. These growth factors improve bone marrow tolerance of escalating doses of chemotherapy, allowing higher doses to be given at shorter intervals. The availability of the longacting pegfilgrastim (filgrastim with polyethylene glycol) now allows a single dose of myeloid growth factor for each 3-week chemotherapy dose. G-CSF and GMCSF have been used to stimulate bone marrow stem cell production in both the circulating blood and in bone marrow cell populations collected for autologous transplantation. Administration of growth factors may improve survival after the failure of autologous or allogeneic bone marrow grafts.
Treatment
Infection management has been aimed at treatment of gram-negative bacterial sepsis, the most rapidly lethal
P.1695
infection. Current concepts have been broadened to include prophylaxis and prevention of the most common infections, including those caused by gram-negative, gram-positive, and fungal pathogens. Until recently, empirical therapy of fever consisted of twoor three-drug combinations, including an aminoglycoside and an antipseudomonal penicillin, with resolution of fever and bacteremia in about 70% of patients. Current results using initial monotherapy with a third-generation cephalosporin such as ceftazidime or cefepime or a combination β-lactam appear to yield similar results. Vancomycin or antifungal therapy with fluconazole, intraconazole, or voriconazole may be added on the basis of clinical suspicion, culture results, or prolonged fever in the absence of positive cultures. Multiple alternatives to the more toxic antifungal amphotericin B now exist. These include caspofungin and liposomal encapsulated formulations of amphotericin B. A recent study found that the newer antifungal agent, voriconazole, was as effective as and less toxic than amphotericin B in the empiric treatment of neutropenic patients with persistent fever. For persistent fevers or clinical deterioration, gram-negative rod coverage should be changed to an agent with a broader spectrum (eg, ciprofloxacin or imipenem). If stenotrophomonas is suspected, trimethoprim-sulfamethoxazole should be added.
Garcia-Carbonero R et al: Antibiotics and growth factors in the management of fever and neutropenia in cancer patients. Curr Opin Hematol 2002;9:215.
Garcia-Carbonero R et al: Granulocyte colony-stimulating factor in the treatment of high-risk febrile neutropenia: a multicenter randomized trial. J Natl Cancer Inst 2001;93:31.
Walsh TJ et al: Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med 2002; 346:225.
Wong-Beringer A et al: Systemic antifungal therapy: new options, new challenges. Pharmacotherapy 2003;23:1441.
THE PARANEOPLASTIC SYNDROMES (Table 40-6)
The clinical manifestations of cancer are usually nonspecific—eg, anorexia, malaise, weight loss, fever—or are due to local effects of tumor growth, either in the primary site or at a distant site. The term “paraneoplasia” has been coined to denote the remote effects of malignancy that cannot be attributed either to direct invasion or metastatic lesions. These syndromes may be the first sign of a malignancy and may affect up to 15% of patients with cancer.
The paraneoplastic syndromes are of considerable clinical importance for the following reasons:
They may accompany relatively limited neoplastic growth and provide an early clue to the presence of certain types of cancer.
The course of the paraneoplastic syndrome usually parallels the course of the tumor. Therefore, effective treatment should be accompanied by resolution of the syndrome, and, conversely, recurrence of the cancer may be heralded by the return of systemic symptoms.
The metabolic or toxic effects of the syndrome may constitute a more urgent hazard to life than the underlying cancer (eg, hypercalcemia, hyponatremia).
The paraneoplastic syndromes are usually caused by the secretion of proteins not normally associated with a cancer's normal tissue equivalent. Clinical findings may resemble those of primary endocrine, metabolic, hematologic, or neuromuscular disorders. The mechanisms for such remote effects can be classified into three groups: (1) effects initiated by a tumor product (eg, carcinoid syndrome), (2) effects due to the destruction of normal tissues by tumor products (eg, hypercalcemia due to local secretion of cytokines), and (3) effects due to unknown mechanisms such as unidentified tumor products or circulating immune complexes stimulated by the tumor (eg, osteoarthropathy due to bronchogenic carcinoma and some neurologic syndromes). Even such nonspecific symptoms as fever and weight loss are truly paraneoplastic and are due to the production of specific factors (eg, tumor necrosis factor) by tumor cells or by normal cells in response to the tumor.
Paraneoplastic syndromes associated with ectopic hormone production are the best-characterized entities. Tumor cells secrete a hormone or prohormone that may be of a higher or lower molecular weight than hormones secreted by the more differentiated normal endocrine cell (eg, parathyroid hormone-related peptide in hypercalcemia, ACTH in Cushing's syndrome, antidiuretic hormone in the syndrome of inappropriate antidiuretic hormone [SIADH] secretion). This ectopic hormone production by cancer cells is believed to result from activation of genes in malignant cells that are normally suppressed in most somatic cells. A single syndrome such as hypercalcemia may be due to more than one of a variety of causes. Effective antitumor treatment usually results in return of the serum calcium to normal, though additional therapy may be required (see Hypercalcemia, above). In some cases, a rapid response to cytotoxic chemotherapy may briefly increase the severity of the paraneoplastic syndrome in association with tumor lysis (eg, hyponatremia with SIADH). Several neurologic paraneoplastic syndromes have been found to be caused by the production of antineuronal antibodies that circulate in the serum and spinal fluid. It is thought that the underlying tumor expresses a similar antigen, resulting in production of a cross-reactive antibody. Treatment of the underlying tumor usually results in only modest improvement of the neurologic deficit. Examples of antineuronal antibodies include the anti-Hu antibody causing sensory neuropathy or en-
P.1696
P.1697
P.1698
cephalitis, associated with small cell cancer of the lung; the anti-Yo antibody causing cerebellar degeneration, associated most often with breast or gynecologic malignancies; the stiff man syndrome, associated with breast cancer; and anti-Purkinje cell antibodies causing cerebellar ataxia, associated with Hodgkin's disease as well as gynecologic, breast, and lung cancers.
Table 40-6. Paraneoplastic syndromes associated with common cancers.1 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Other well-described paraneoplastic syndromes include those involving the skin with or without other organ involvement (eg, dermatomyositis, Sweet's syndrome), hematologic syndromes (eg, polycythemia, thrombocytosis), and those involving the kidneys, the gastrointestinal tract, and the joints.
The most common cancer associated with paraneoplastic syndromes is small cell cancer of the lung. This is thought to be due to its neuroectodermal origin.
Bataller L et al: Paraneoplastic neurologic syndromes. Neurol Clin 2003;21:221.
Briemberg HR et al: Neuromuscular complications of cancer. Neurol Clin 2003;21:141.
Mareska M et al: Lambert-Eaton myasthenic syndrome. Semin Neurol 2004;24:149.
Marmur R et al: Cancer-associated neuromuscular syndromes. Recognizing the rheumatic-neoplastic connection. Postgrad Med 2002;111:95.
Mazzone PJ et al: Endocrine paraneoplastic syndromes in lung cancer. Curr Opin Pulmon Med 2003;9:313.
Posner JB: Immunology of paraneoplastic syndromes: overview. Ann NY Acad Sci 2003;998:178.
Sutton I et al: The immunopathogenesis of paraneoplastic neurological syndromes. Clin Sci 2002;102:475.
NOVEL THERAPIES FOR CANCER TREATMENT
The use of cytotoxic drugs against cancer is limited by a number of factors, including toxicity, tumor resistance, and lack of targeted cell death. New strategies are based on increasing and improved knowledge of the molecular events responsible for disordered cellular growth and include antibodies to block receptors, small molecules that inhibit receptor tyrosine kinase-mediated cell signaling, agents directed at suppressing growth of blood vessels that feed cancer growth, vaccines to stimulate immune recognition of cancer cells, cell cycle inhibitors, and gene therapy to turn off signaling pathways or provide a missing tumor suppressor.
One way to block cellular growth is to block growth factor receptors. These receptors cross the cell membrane; the extracellular portion is the ligand-binding site, and the intracellular portion is the receptor tyrosine kinase. Activation of the receptor with ligand phosphorylates the tyrosine kinase and results in cell signaling through a complex series of events. The growth factor receptors and various methods to block their activation are presented in Figure 40-1. EGFR is expressed on most epithelial cells, and activation of the receptor has been shown to promote tumor cell growth, proliferation, and survival. Preclinical models have shown that blockade of this receptor results in tumor growth delay or regression and can potentiate radiation and chemotherapy effects. Trastuzumab (Herceptin) is a monoclonal antibody directed against the HER-2/neu receptor, one of the EGF family of receptors, and was the first growth factor receptor inhibitor approved for clinical use.
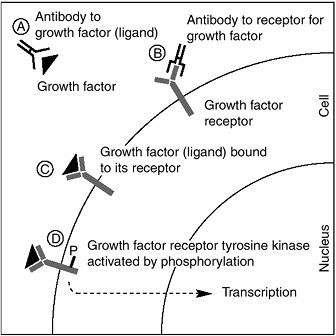 |
Figure 40-1. Signaling through growth factor receptors can be blocked by antibodies to either the growth factor (ligand) (A) (eg, antibody to vascular endothelial growth factor; bevacizumab) or to the extracellular portion of the receptor for the growth factor (tyrosine kinase receptor) (B) (eg, trastuzumab, cetuximab). The binding of growth factors to their receptors (C) leads to phosphorylation of the intracellular portion of the receptor or the receptor tyrosine kinase (D). Phosphorylation activates the receptor and results in many downstream signals in the cell that activate gene transcription, and consequently proliferation. Blockade of receptor phosphorylation—eg, by erlotinib (Tarceva) or gefitinib (Iressa) (oral small molecule tyrosine kinase inhibitors)—interrupts the pathway, with the hoped-for result of blocking tumor growth. |
Agents that block the EGFR are directed against the HER-1 receptor. Two agents targeting the EGFR are in clinical trials with encouraging results. Cetuximab (IMC-C225) is a monoclonal antibody that binds to the extracellular domain of the EGFR, resulting in inhibition of the receptor tyrosine kinase and is now approved for the treatment of advanced colorectal cancer that is resistant to irinotecan and oxaliplatin. In addition to reversing chemotherapy resistance, cetuximab appears to potentiate the effect of radiation therapy in head and neck cancer. This is now being studied in the setting of an ongoing phase III clinical trial.
P.1699
Erlotinib and gefitinib are oral small molecule tyrosine kinase inhibitors that blocks the EGFR by directly blocking phosphorylation of the intracellular receptor tyrosine kinase. One recent study evaluated the effect of erlotinib in patients with bronchoalveolar carcinoma (BAC), a form of non-small cell lung cancer. Twenty-seven percent of patients responded to this novel agent, which was quite striking given that this form of cancer does not usually respond to treatment. Ongoing trials are evaluating the effect of these agents in combination with standard chemotherapy or hormonal therapy. Gefitinib and erlotinib have also been shown to inhibit the HER-2/neu receptor tyrosine kinase in preclinical models; trials are now evaluating the effects of these agents in advanced breast cancers in combination with trastuzumab. The primary toxicity of gefitinib and erlotinib is a potentially severe follicular rash. Lapatanib (GW572016) is an oral dual kinase inhibitor that blocks both HER-1 and HER-2. Early phase clinical trials suggest significant activity against multiply pretreated HER-2-positive metastatic breast cancers. Multiple trials are ongoing in this and other malignancies. Other small molecule tyrosine kinase inhibitors that block multiple receptors within the EGF family are also in clinical trials. These oral agents block receptor combinations of EGF, HER-1, and HER-4.
Angiogenesis (the growth of new blood vessels) is thought to be an essential component of the ability of tumors to invade locally and to metastasize from the primary tumor site. Tumor angiogenesis is regulated by angiogenic stimulators such as VEGF (the ligand for the VEGF receptor) and the newly described inhibitors of angiogenesis: angiostatin and endostatin. There is now intense interest in using inhibitors of angiogenesis to suppress tumor growth and metastases. This type of therapy might avoid the development of chemotherapy resistance and have less toxicity than standard cytotoxic therapy.
A recombinant humanized antibody to VEGF (anti-VEGF, rhuMAb VEGF, bevacizumab) is the first antiangiogenic agent to be FDA approved for the treatment of cancer. Bevacizumab is now available for the first-line treatment of metastatic colorectal cancer, where its use in combination with standard chemotherapy demonstrated improvement in survival as well as response rates. Although a dose-finding phase II trial in advanced refractory breast cancer with bevacizumab found an overall response rate of 11–20%, a phase III randomized trial using anti-VEGF in combination with chemotherapy versus chemotherapy alone in the treatment of advanced and chemotherapy-resistant breast cancer failed to show an improvement in time to disease progression. A second phase III study evaluating the combination of bevacizumab in combination with paclitaxel as first-line therapy for metastatic breast cancer has closed to accrual; results are expected by 2006. Treatment with bevacizumab in patients with renal cell cancer resulted in significant slowing of cancer cell growth, with a 2.5-fold prolongation in time to progression from 2 to 5 months. Tumor regression was rare, with three partial responses. The antibody was well tolerated in this trial, and a confirmatory multiinstitution trial is ongoing. Combinations of bevacizumab with the EGF inhibitor erlotinib are being tested in a variety of cancers; effectiveness has been demonstrated in resistant non-small cell lung cancer, among others.
Endostatin and angiostatin are potent inhibitors of angiogenesis that may be promising. A preclinical study showed that transfer of cells engineered to produce angiostatin into mice inhibited the growth of both the primary tumor and lung metastases from fibrosarcoma. Trials using endostatin to treat patients with advanced malignancy began in late 1999. Two phase I dose-escalation trials using recombinant human endostatin (rHE) or angiostatin (rHA) in patients with advanced solid tumors showed few tumor responses, although both agents were associated with minimal side effects at the doses used. Tumor blood flow decreased with both agents. Phase II trials are ongoing to assess the antitumor effects of endostatin and angiostatin.
Another novel way to suppress angiogenesis is with small molecules that inhibit receptor tyrosine kinases and block VEGF-mediated receptor signaling. Several agents are in clinical trials treating various advanced metastatic cancers, usually in combination with chemotherapy. One agent, SU5416, was found to have unfavorable pharmacokinetics after extensive clinical trials had been conducted; development of this agent has been halted. It is now clear that standard pharmacokinetic studies must be done for novel agents before undertaking large randomized clinical trials. One newer agent, SU011248, has been shown to have striking antitumor effects in GIST that has progressed on imatinib, as well as in non-small cell lung and treatment-resistant renal cell cancers. Ongoing trials are evaluating the effects of this and other agents in a variety of cancers alone and in combination with chemotherapy.
Thalidomide has been shown to have antiangiogenic properties as well as other antitumor effects. Striking responses have been seen in advanced and resistant multiple myeloma. Clinical trials using thalidomide in combination with chemotherapy in multiple myeloma, prostate cancer, and other malignancies are ongoing. A newer, more potent and less toxic immunomodulatory agent, revlimid, has shown efficacy in several malignancies; trials are ongoing. Lenalidomide is a novel 4-aminoglutarimide analog of thalidomide that is more potent but does not have the neurotoxic and teratogenic effects of thalidomide. A recent study treated 43 patients with lenalidomide with transfusion-dependent myelodysplasia with significant hematologic and cytogenetic response. One interesting therapy targets matrix metalloproteases that are thought to be important in the ability of cancer cells to metastasize. Unfortunately, phase III results in small cell lung cancer have been disappointing, indicating at least that the current products are not active enough for clinical use.
Immunotherapy is an exciting area of investigation of the treatment of cancer. The most extensively
P.1700
treated disease with immunotherapeutic modalities is malignant melanoma—for a variety of reasons, including easily identified immunogenic antigens, easy access to tumor cells, and the ability to grow these cells in vitro. Active specific immunotherapy with melanoma vaccines has been evaluated in phase II trials for advanced melanoma as well as in the adjuvant setting with encouraging results. A phase III trial testing the allogeneic melanoma cell lysate vaccine Melacine in 689 patients with intermediate-thickness and clinically node-negative melanoma showed no evidence of improvement in disease-free survival at a median followup of 5.6 years among patients receiving the vaccine. Criticisms of the trial include the lack of sentinel node biopsy and lack of ability to detect small differences in recurrence. However, when patients expressing two or more specific HLA class I antigens were evaluated separately, a highly significant benefit was seen in patients receiving adjuvant treatment with Melacine. This suggests that specific HLA types can determine the immune response and disease impact of vaccine strategies. Further studies are ongoing. Identification of a suitable target is critical for the development of any vaccine. Interesting agents in clinical trials include a vaccine directed against HPV to prevent cervical cancer and individualized vaccines directed toward the unique set of B cell tumor antigens that comprises each participating patient's low-grade lymphoma. This type of vaccine has been demonstrated to induce an immune response as well as either stable disease or actual tumor shrinkage in preliminary trials. Other interesting vaccines include monoclonal antibodies directed toward tumor products such as CA 125 for ovarian cancer, CEA for colon cancer, and HER-2/neu for breast cancer.
The field of cancer vaccines is growing rapidly. One type of tumor vaccine in many clinical trials capitalizes on dendritic cells, which are antigen-presenting cells that enhance the response of the immune system to foreign antigens. Dendritic cells may be loaded with a particular abnormal protein to stimulate the immune response to a specific cancer. Early clinical trials in melanoma, multiple myeloma, and other cancers are in progress. One interesting strategy is to target the dendritic cells to a known growth factor present on the tumor cell. A clinical trial using dendritic cells loaded with HER-2/neu for the treatment of metastatic breast cancer is evaluating the ability of this type of vaccine to stimulate a specific immune response in women with advanced breast cancer. Preliminary results indicate stability of disease, with an immune response generated in all treated patients. In one study, patients with latestage colorectal cancer were treated with a growth factor, FLT-3 ligand, to expand the number of circulating dendritic cells in vivo. The cells were then harvested, loaded with CEA antigen, and reinfused as a cellular vaccine. Early results in all four patients include tumor response or disease stabilization. A larger trial is planned. This type of therapy might also be useful early in the disease course of an aggressive tumor. Dendritic cell vaccines can be used in conjunction with autologous stem cell transplantation; cells are removed at the time of stem cell harvesting, undergo in vitro stimulation, and are then returned to the patient after completion of chemotherapy and radiation therapy to eradicate bulk tumor.
Several problems with vaccine therapy exist, including the difficulty of generating an immune response in an immunosuppressed cancer patient and the fact that an immune response does not necessarily correlate with tumor response. To enhance the immune response to vaccines, growth factors such as GM-CSF are given with the treatment. A GM-CSF gene-modified vaccine is now in clinical trials that produces GM-CSF locally to enhance the immune response. Early results show some evidence of tumor response in non-small cell lung cancer.
The arachidonic acid metabolic pathway is thought to be important in the pathogenesis of cancer. COX-2 is overexpressed in many solid tumors, including tumors of the lung, colon, and breast. Higher levels are thought to increase angiogenesis and decrease apoptosis. However, due to the concern regarding an increase in cardiovascular events in patients on COX-2 inhibitors, trials utilizing celecoxib in treatment or prevention of cancer have largely been halted—it will remain to be seen which studies, if any, are allowed to continue. The goal of gene therapy for cancer is to inhibit the constitutive signals that drive tumor growth. Expanding knowledge about signal transduction has provided multiple possible attack points within this complicated multistep process involving a variety of somatic gene alterations. Although at present it is impossible to deliver therapeutic genes to every cancer cell, bystander effects or the cytotoxic effects produced by engineered cells on nonengineered cells may allow broad effects from a limited number of transduced cells. A variety of approaches are being investigated. These include enhancing the ability of the host immune system to respond to a specific tumor, sensitizing tumor cells to relatively nontoxic drugs or prodrugs, and selective replacement of altered or missing tumor suppressor genes or inactivation of oncogenes. Selective targeting of cells would allow either cell death or return of normal growth patterns without toxicity to nonneoplastic cells. Oblimersen sodium is an antisense oligonucleotide that inhibits the production of Bcl-2. Bcl-2 confers resistance to apoptosis, is overexpressed, and is a negative prognostic indicator in a number of malignancies. Oblimersen sodium binds to Bcl-2 messenger RNA, causing fragmentation of the protein message. Ongoing studies are evaluating the role of oblimersen sodium in combination with chemotherapy in CLL, hormone refractory prostate cancer (HRPC), metastatic malignant melanoma, and other cancers. Encouraging results have been seen in both CLL and HRPC.
One area of research in active clinical trial is replacement of the missing function of the mutated tumor suppressor gene, p53, or inhibition of the function of a dominant oncogene such as ras. One approach is to cre-
P.1701
ate a vaccine directed against cells with mutant p53 to generate a cytotoxic T cell response to tumor cells expressing the p53 protein. A vaccine made from a disabled adenovirus (the vector or carrier) and the p53 gene and injected into the arterial circulation is delivered to tumors that have metastasized to the liver with subsequent expression of the p53 gene.
Another unique approach to tumor killing is the use of an adenovirus engineered to selectively kill tumor cells that are lacking p53 but leave normal cells alone. This agent, ONYX-015, is also in clinical trials both with and without chemotherapy. It appears to be more effective when injected directly into tumors. Results from this and other agents are limited by a variety of problems, including difficulty in delivering the agent, identifying tumors that lack p53, and production of the novel agent. The Bcl-2 protein, overexpressed in many common solid tumors, is thought to be responsible for blocking apoptosis or natural cell death and appears to confer tumor cell resistance to chemotherapy and radiation therapy. Gene therapy is also being investigated in autologous stem cell transplantation for a variety of malignancies. In this setting, antitumor genes are added to cells that have been removed for transplantation following myeloablative chemotherapy. Trials are ongoing to study this form of therapy in chronic myelogenous leukemia. Multiple other trials, including the introduction of new genes that encode inhibitors of oncogene products or enhance tumor cell immunogenicity, are in progress.
Motexafin gadolinium is the first of an investigational class of drugs called texaphyrins, which are rationally designed small molecules that target reactive oxygen species (ROS) and selectively accumulate inside cancer cells to disrupt cellular metabolism and increase sensitivity to oxidative stress caused by radiation and chemotherapy and to induce apoptosis (programmed cell death). This novel agent is a paramagnetic compound so that its presence is visible with MRI. Motexafin is being investigated as a potential therapeutic agent in combination with radiation therapy and/or chemotherapy, monoclonal antibody therapy, and as a single agent for various types of cancers with promising early results. Tesmilifene (BMS-217380-01) is an intracellular histamine antagonist that is being developed as a chemopotentiator for the treatment of malignant solid tumors. Results of one phase III trial in breast cancer have shown an improvement in response and survival in patients treated with the combination of tesmilifene and doxorubicin, compared with those treated with doxorubicin alone. In animal models, tesmilifene has been shown to augment the activity of numerous cycotoxic drugs including doxorubicin, cyclophosphamide, 5-fluorouracil, cisplatin, and mitoxantrone. A number of trials are ongoing in breast cancer, head and neck cancer, and prostate cancer. TLK286 is a novel small molecule that is activated by glutathione S-transferase P1-1 (GST P1-1), an enzyme that is overexpressed in many human cancers and that correlates with resistance to chemotherapy. When activated, TLK286 initiates apoptosis, or programmed cell death. TLK286 has shown activity in advanced ovarian, non-small cell lung, and colorectal cancers, and a phase III trial is ongoing in ovarian cancer. Advexin supplies p53 protein in very high concentrations in cancer tissue, selectively killing cancer cells. This interesting agent has shown activity in head and neck cancer, among other tumors. Two phase III trials are ongoing. A number of other small molecules are in clinical trials to treat cancer. T67 is a novel small molecule agent that binds irreversibly to β-tubulin, an anticancer drug target. T67 has shown clinical activity against hepatocellular carcinoma; early phase clinical trials are investigating its activity compared with doxorubicin. A similar agent, T607, is being tested in esophageal cancer. Tipifarnib (R115777) is a small molecule that blocks activation or farnesylation of the ras protein by suppressing the activity of farnesyl protein transferase. This agent has shown activity in primary brain tumors and in breast cancer. A multicenter trial comparing tipifarnib with hormonal therapy for metastatic breast cancer with hormonal therapy alone is ongoing, along with earlier studies in glioma.
Other areas of investigation include discovery of novel agents that induce apoptosis, stimulate differentiation, prevent tumor invasion or metastases, and specifically target hormone pathways that stimulate tumor growth. In addition, new antiproliferative agents with improved toxicity profiles and less cross-resistance to known agents are being evaluated or are already in use. These include novel taxanes that cross the blood–brain barrier, with encouraging results in phase II trials. Ongoing research is focusing on the identification of new growth factor receptors associated with malignant behavior that can be targeted to suppress cancer growth, such as the HER-2/neu receptor targeted by the antibody trastuzumab. The current proliferation of clinical trials targeting various pathways of tumor growth as well as ongoing research to identify antigenic targets should lead to a new paradigm for cancer therapy in the coming decades.
Bitton RJ: Cancer vaccines: a critical review on clinical impact. Curr Opin Mol Ther 2004;6:17.
Blay JY et al: Targeted cancer therapies. Bull Cancer 2005;92: E13.
Cao Y: Antiangiogenic cancer therapy. Semin Cancer Biol 2004; 14:139.
Ferrari M: Cancer nanotechnology: opportunities and challenges. Nat Rev Cancer 2005;5:161.
Gianni L: The future of targeted therapy: combining novel agents. Oncology 2002;63:47.
Knox SJ et al: Clinical radioimmunotherapy. Semin Radiat Oncol 2000;10:73.
Mazieres J et al: Perspectives on farnesyl transferase inhibitors in cancer therapy. Cancer Lett 2004;206:159.
Reyno L et al: Phase III study of N,N-diethyl-2-[4-(phenylmethyl) phenoxy]ethanamine (BMS-217380-01) combined with doxorubicin versus doxorubicin alone in metastatic/recurrent breast cancer: National Cancer Institute of Canada Clinical Trials Group Study MA.19. J Clin Oncol 2004;22: 269.
P.1702
Scappaticci FA: Mechanisms and future directions for angiogenesis-based cancer therapies. J Clin Oncol 2002;20:3906.
Sondak VK et al: Adjuvant immunotherapy of resected, intermediate-thickness, node-negative melanoma with an allogeneic tumor vaccine: overall results of a randomized trial of the Southwest Oncology Group. J Clin Oncol 2002;20:2058.
Sosman JA et al: Adjuvant immunotherapy of resected, intermediate-thickness, node-negative melanoma with an allogeneic tumor vaccine: impact of HLA class I antigen expression on outcome. J Clin Oncol 2002;20:2067.
Witzig TE et al: Randomized controlled trial of yttrium-90-labeled ibritumomab tiuxetan radioimmunotherapy versus rituximab immunotherapy for patients with relapsed or refractory lowgrade follicular, or transformed B-cell non-Hodgkin's lymphoma. J Clin Oncol 2002;20:2453.
ALTERNATIVE & COMPLEMENTARY THERAPIES FOR CANCER TREATMENT
New areas of cancer therapy are rapidly expanding, and the next decade could bring important changes in the treatment of common malignancies. Many alternatives to traditional cancer therapy exist (one wellknown example is shark cartilage, which is widely available and purported to have completely unproven antiangiogenic properties), but there is little evidence to support their efficacy or assess their potential toxicity, and at present there is no federal regulation of these products. Agents that are commonly used include green tea, echinacea, essiac tea, flaxseed, mistletoe, and coenzyme Q as well as others.
It is critical that herbs be tested with the same rigorous standards as chemotherapeutic agents in scientifically based clinical trials. Most herbal preparations are available over the counter, and no information exists regarding the interaction of these herbs with other medications. Many interactions have been described between St. John's wort and critical medications such as antiretrovirals, cyclosporine, chemotherapeutic agents, and hormonal agents, among others, that resulted in decreased drug levels due to enhanced metabolism.
A dietary supplement containing a combination of eight Chinese herbs with potent estrogenic activity, PC-SPES, has been tested in prostate cancer. All patients with hormone-sensitive and about 60% of patients with hormone-refractory prostate cancer responded with a decline in PSA; some patients also had improvement in bone scans. Toxicity was modest, including allergic reactions and thromboembolic events in about 4% of patients. Unfortunately, laboratory analysis of PC-SPES by the California Department of Health Services found significant contamination of this product with undeclared prescription drugs such as warfarin and alprazolam as well as hormonal agents. Based on these data, the manufacturer of PC-SPES and SPES voluntarily recalled the products nationwide. Investigations will need to be repeated if a noncontaminated product is produced, as the finding of hormonal agents in the herbal preparation suggests that the responses seen in published studies could have been due to contaminants instead of the herbs themselves.
Ongoing research is evaluating the effects of herbal combinations on side effects of adjuvant chemotherapy for breast cancer. The NCI is actively supporting research in the field of alternative therapies for cancer through the National Center for Complementary and Alternative Medicine (NCCAM). Additional information on alternative treatment modalities can be found in Chapter 42.
There are now many Web sites devoted to providing information on alternative cancer therapies. NCCAM lists new research and research trials as well as an introduction to alternative medicine. There is also an extensive bibliography. This Web site may be reached at http://www.nccam.nih.gov. Additional resources can be found at the Cancer Guide Material on Alternative Medicine Web site http://www.cancerguide.org/alternative.html. The Center for Alternative Medicine Research in Cancer at the University of Texas-Houston Health Science Center (UT-CAM) maintains an excellent Web site with data pertaining to a wide variety of alternative medications and therapies. The site can be reached at http://www.nccam.nih.gov.
Deng G et al: Complementary therapies for cancer-related symptoms. J Support Oncol 2004;2:419.
Ernst E: The current position of complementary/alternative medicine in cancer. Eur J Cancer 2003;39:2273.
Richardson MA et al: Complementary and alternative medicine: opportunities and challenges for cancer management and research. Semin Oncol 2002;29:531.
Tagliaferri M et al: Complementary and alternative medicine in early-stage breast cancer. Semin Oncol 2001;28:121.
Vickers AJ et al: Unconventional therapies for cancer and cancerrelated symptoms. Lancet 2001;2:226.
Wilkinson S: Critical review of complementary therapies for prostate cancer. J Clin Oncol 2003;21:2199.
EAN: 2147483647
Pages: 71