9 - Blood Vessels
Editors: Mills, Stacey E.
Title: Histology for Pathologists, 3rd Edition
Copyright 2007 Lippincott Williams & Wilkins
> Table of Contents > IV - Nervous System > 12 - Pituitary and Sellar Region
function show_scrollbar() {}
12
Pituitary and Sellar Region
M. Beatriz S. Lopes
Peter J. Pernicone
Bernd W. Scheithauer
Eva Horvath
Kalman Kovacs
Embryology
To fully appreciate the anatomy of the pituitary (hypophysis), an understanding of its embryogenesis is essential. The gland consists of an anterior lobe (adenohypophysis), a posterior lobe (neurohypophysis), and an intermediate zone (Figure 12.1). The development of each differs significantly.
The adenohypophysis has its origin in a thickening of oral ectoderm (1,2,3,4). During the third week of gestation, this thickened plate invaginates in a cephalad direction to form the Rathke's pouch, which retains its connection to the stomodeum via a narrow stalk. In the sixth week, the stalk becomes so attenuated that the pouch loses its stomodeal attachment as it comes into contact with the infundibulum. Cellular proliferation in the anterior wall of Rathke's pouch gives rise to the pars distalis, the principal portion of the anterior lobe. In addition, a tonguelike'' extension of the pars distalis, the pars tuberalis, grows upward to partially surround the anterior surface of the infundibulum. The posterior portion of Rathke's pouch gives rise to what in humans is a thin segment of pituitary, the pars intermedia or intermediate lobe. In this zone, microcystic remnants of Rathke's pouch containing colloidlike material are commonly seen (Figure 12.1). Gross cystic dilatation of such remnants is common but infrequently produces clinically significant intermediate lobe or Rathke's cleft cysts.
A remnant of the pharyngohypophysial stalk, demonstrable in fetuses and occasionally encountered in adults, comprises the pharyngeal pituitary (5,6). Located in the midline, beneath the muco-periosteum of the nasopharynx, it extends from the posterior border of the vomer along the sphenoid bone. Although the full spectrum of anterior pituitary hormone-producing cells may be demonstrated in pharyngeal pituitaries, they are rarely the seat of medical or surgical disease.
The neurohypophysis develops from a neuroectodermal bud first noticeable in the floor of the diencephalon at 4 weeks' gestation (1,3). Two weeks later, the outgrowth grows ventrally to abut the posterior portion of Rathke's pouch. This specialized portion of the nervous system comprises magnocellular nuclei, their axons within the median eminence and infundibular stalk, and their terminations in the pars nervosa (posterior lobe). Oxytocin and vasopressin, as well as their carrier proteins, the neurophysins,
P.322
are detectable in supraoptic and paraventricular nuclei at 19 weeks and in the posterior lobe at 23 weeks (7).
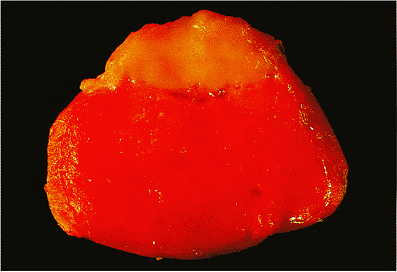 |
Figure 12.1 Normal unfixed adult pituitary gland cut in the horizontal plane. The posterior lobe is located at the top of the field. A few intermediate lobe cysts are present. The deep red color of the anterior lobe is a reflection of its extensive vascularity. |
As early as 7 to 8 weeks' gestation, the portal system begins to develop. Although by 12 weeks both the median eminence and the anterior lobe are vascularized, the circulation of the hypothalamic pituitary portal system is not completed until 18 to 20 weeks (7).
The hypothalamus develops from a swelling in the diencephalon. Although the hypothalamic nuclei as well as the supraopticohypophysial tract are demonstrable at 8 weeks' gestation, unmyelinated axons, growing ventrally from the magnocellular (supraoptic and paraventricular) nuclei, do not reach the posterior lobe until 6 months.
By 12 weeks, a number of cartilaginous plates have fused to form the cartilaginous neurocranium (1). The body of the sphenoid bone and the sella turcica result from fusion of hypophysial cartilaginous plates located on either side of the developing pituitary. The sella is well formed by 7 weeks and matures through a process of enchondral ossification.
Rare developmental malformations of the pituitary gland, including ectopic pituitary gland and pituitary dystopia, have been reported (8,9).
The understanding of pituitary development has recently expanded as a result of the identification of molecular mechanisms that may specify cell determination and differentiation. Recent advances in pituitary development in mammals have suggested that pituitary organogenesis is controlled by a combination of sequential exogenous and endogenous signals (10,11,12). These signals induce the expression of interacting transcriptional regulators in temporal and spatial patterns. Pituitary cell types appear to emerge from a common stem cell under the response of transcription regulators critical for determination and differentiation of specific cell type. Briefly, the transcription factor pituitary homeobox 1 (Ptx1) appears in early development of the pituitary and cooperates with more functionally oriented transcription factors. Pit-1 is a transcription factor that regulates the functional differentiation of the somatotrophs, lactotrophs, and thyrotrophs. A family of basic helix-loop-helix transcription factors, Neuro D1, and a novel T box factor, Tpit, appear to synergistically play a role in the functional differentiation for pituitary pro-opiomelanocortin (POMC) cell lineage and corticotroph cells. The nuclear receptor steroidogenic factor-1, SF-1, is a key factor for differentiation of LH and FSH cells.
On the other hand, the time period of recognition of the various human pituitary hormone producing cells during embryonal development have been well determined by immunohistochemical stains. Corticotrophs are the first cells to differentiate in the human fetal pituitary (at around 5 weeks gestational age). Somatotrophs appear around 8 to 9 weeks, followed by thyrotrophs and gonadotrophs at 12 to 15 weeks. Lactotrophs, although seen in small numbers as early as 12 weeks, are only fully recognizable at 23 weeks (7,13,14).
Gross Anatomy
Bony Sella
The pituitary gland is centrally situated at the base of the brain, where it lies safely nestled in the sella turcica, a saddle-shaped concavity within the sphenoid bone (Figures 12.2,12.3,12.4). It is attached to the hypothalamus by both the pituitary stalk and a tenuous vascular network (Figures 12.5,12.6,12.7). By virtue of its location, the pituitary
P.323
gland has many important anatomic relations (15,16,17). Anterior to the sella, the sphenoid bone forms a midline slope, the tuberculum sella, as well as a transverse indentation, the chiasmal sulcus, so named for the overlying optic chiasm (see Figures 12.3,12.4). The optic canals, which transmit the optic nerves, lie anterolateral to the sulcus, whereas the optic tracts are posterolateral. In view of the pituitary's proximity to the optic apparatus, pituitary lesions that extend superiorly may cause significant visual field deficits (Figures 12.2, 12.5,12.6,12.7,12.8,12.9,12.10,12.11). Specifically, compression of decussating fibers in the chiasm produces bitemporal hemianopsia, whereas compromise of an optic tract leads to homonymous hemianopsia. Further suprasellar extension may cause hypothalamic dysfunction and hydrocephalus.
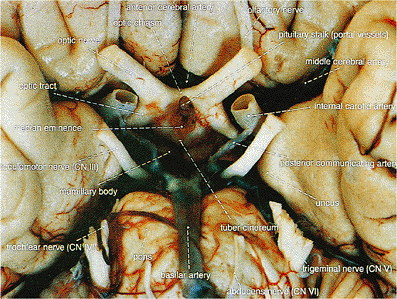 |
Figure 12.2 Ventral surface of normal brain showing the pituitary stalk and surrounding structures. The pituitary gland has been removed. The proximity of the optic chiasm to the pituitary is the basis for the visual field deficits accompanying suprasellar extension of pituitary adenomas. Visible along the posterior aspect of the stalk are tributaries of the portal system. |
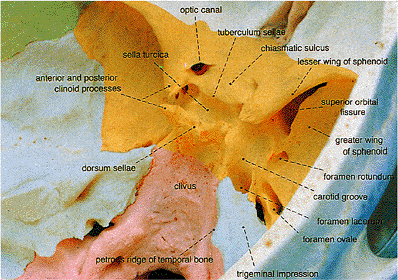 |
Figure 12.3 Oblique view of the normal skull base; the various skull bones are indicated in color. The sella turcica is centrally located with several foramina nearby. The foramen spinosum is not visible in this view. Yellow, sphenoid; pink, occipital; light blue, temporal; green, parietal; white, frontal. |
 |
Figure 12.4 This normal lateral skull radiograph shows the central location of the sella turcica and surrounding bony anatomy. |
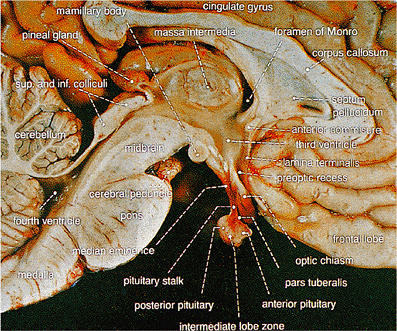 |
Figure 12.5 Midline sagittal section through the brain at the level of the pituitary stalk and pituitary gland, showing the pituitary gland with surrounding structures including hypothalamus, third ventricle, optic chiasm, and sphenoid sinus. |
The floor of the sella forms a portion of the roof of the sphenoid air sinus, a fortuitous relationship that permits ready surgical access (18) (Figures 12.4, 12.6,12.7,12.8,12.9,12.10,12.11,12.12). Indeed, the transsphenoidal approach to the pituitary initially involves mobilization of the nasal septal cartilage followed by resection of a portion of the ethmoid plate. A sublabial incision is then made, and the sphenoid
P.324
speculum is placed in the septal space, permitting direct visualization of the anterior wall of the sphenoid sinus. Upon breaking through the anterior sphenoid wall, the sella may be seen bulging into the roof of the sinus. A septated sphenoid sinus may affect the surgeon's orientation at surgery (Figures 12.8,12.9). The pituitary is then exposed by traversing the bony sellar floor and incising the dural investment around the gland.
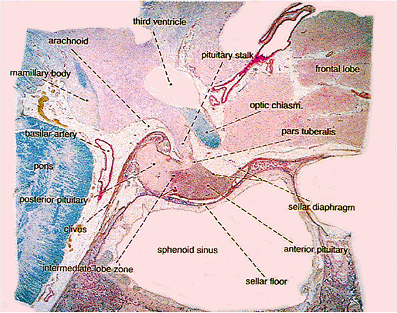 |
Figure 12.6 Sagittal whole-mount section of normal pituitary gland and surrounding structures. The anterior (at right) and posterior (at left) lobes are clearly delineated. The pars tuberalis is the thin tongue-shaped portion of anterior lobe that extends for a short distance up the stalk. This diagram illustrates the proximity of the optic chiasm to the pituitary. Superior extension of a pituitary tumor may compress the optic chiasm with resultant visual field deficits, whereas downward extension may fill the sphenoid sinus (Luxol-Fast Blue PAS). |
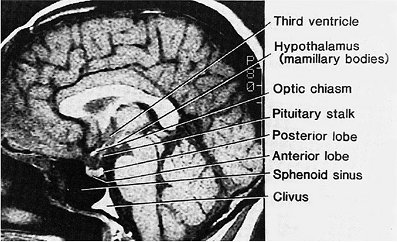 |
Figure 12.7 Magnetic resonance imaging (MRI): sagittal view of the brain at the level of the pituitary stalk and gland. The clarity of the pituitary gland, stalk, hypothalamus, and optic chiasm is remarkable, making MRI an excellent imaging modality for the assessment of pituitary lesions. One advantage of MRI over computed tomography (CT) is the absence of bony artifact with MRI. |
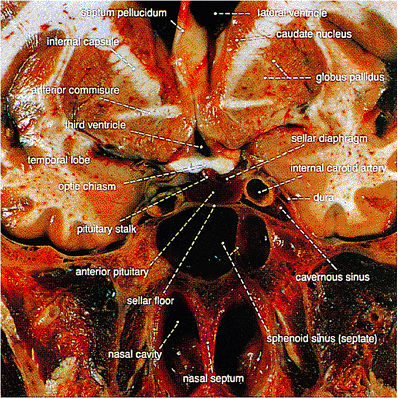 |
Figure 12.8 Coronal section of the head at the level of the pituitary stalk and gland. This photograph clearly illustrates the intimate relationships between the cavernous sinuses, the sphenoid sinus, and the pituitary gland. Invasive adenomas may extend laterally into one or both cavernous sinuses or inferiorly into the sphenoid sinus. Note the proximity of the optic chiasm to the pituitary. |
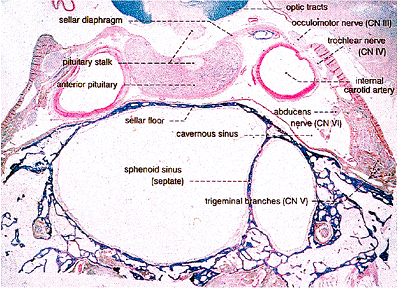 |
Figure 12.9 Coronal whole-mount view of the normal pituitary gland and surrounding structures. Note the location of cranial nerves III, IV, VI, and branches of cranial nerve V within the cavernous sinuses, a relationship explaining the occurrence of cranial nerve palsy in association with invasive pituitary adenomas. This section also illustrates the proximity of the internal carotid arteries to the pituitary gland (Luxol-Fast Blue PAS). |
The sloping anterior sellar wall terminates in posterolateral projections, the anterior clinoid processes (Figures 12.3,12.4). Posterior to the sella, the sphenoid bone continues as the dorsum sellae, anterolateral portions of which form the posterior clinoid processes (see Figures 12.3,12.4). Posterior to the dorsum sellae lies the downward-sloping clivus, notorious as the site of predilection of chordomas (Figures 12.3, 12.4, 12.6,12.7). A number of neurovascular foramina are situated in the sellar region; by name and contents from anterior to posterior, they include the foramen rotundum (maxillary nerves), ovale (mandibular nerves), spinosum (middle meningeal arteries), and lacerum (internal carotid arteries) (Figure 12.3).
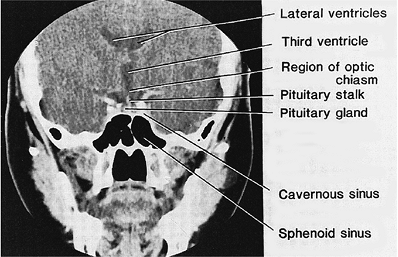 |
Figure 12.10 A computed tomographic (CT) coronal view of the normal skull and brain at the level of the pituitary stalk and gland. The CT scan is a good imaging modality for assessing the pituitary gland; however, radiologists often encounter problems with bony artifact. For this reason, MRI is superior. |
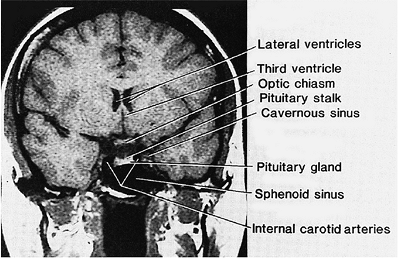 |
Figure 12.11 Coronal MRI of the skull and brain at the level of the pituitary stalk and gland. |
P.325
Meninges
The physical relationship of the meninges to the pituitary and sella is unusual in that the pituitary lacks a leptomeningeal investment. Periosteal dura lines the sella turcica, whereas the dura proper covers the lateral aspects of the cavernous sinuses and forms the sellar diaphragm. The diaphragm is usually thin at the center and thick at its periphery and possesses a variably sized central aperture through which the pituitary stalk passes (15). Leptomeninges do encircle the stalk; however, below the level of the sellar diaphragm, they reflect back upon themselves to form a circumferential channel, the infradiaphragmatic hypophysial cistern. This arrangement explains the higher incidence of development of meningiomas in the suprasellar surface of the diaphragm rather than in the intrasellar compartment.
In some individuals, the leptomeninges exhibit an important anatomic variation. It consists of extension or herniation of the arachnoid through an inordinately large diaphragmatic opening. In one study, the incidence of an intrasellar arachnoidocele was found to exceed 20% (19). In such cases, transsphenoidal surgery may result in persistent cerebrospinal fluid (CSF) rhinorrhea because of inadvertent violation of the subarachnoid space. With prolonged exertion of even normal CSF pressure, enlargement of such arachnoidoceles may produce sellar enlargement and pituitary compression, the gland being reduced to a thin crescent on the posterior sellar floor (Figures 12.13). The so-called empty sella syndrome, shows a distinct predilection for obese, multiparous females (Figure 12.14). Its anatomic manifestations are fully expressed in as many as 5.5% of autopsies (20,21). Compression of the gland
P.326
and traction deformation of the pituitary stalk may cause mild to moderate hypopituitarism and hyperprolactinemia, respectively.
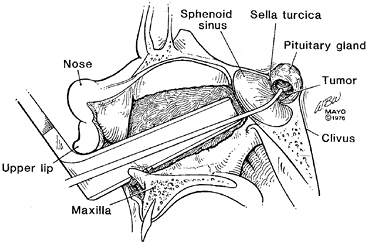 |
Figure 12.12 Transsphenoidal approach to the pituitary gland. After mobilizing the nasal septal cartilage and resecting a portion of ethmoid plate, a sublabial incision is made, and a sphenoid speculum is placed. Next, the floor of the sphenoid sinus and the floor of the sella turcica are traversed. Finally, the dural investment of the pituitary gland is incised, and the gland is exposed. This diagram illustrates a curette in place for removal of a pituitary adenoma. |
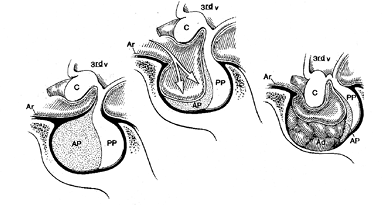 |
Figure 12.13 Illustration of normal as well as variants of the empty sella. A. The normal pituitary-sellar relationships. The leptomeninges cover the stalk and sellar diaphragm but do not extend into the sella. B. In primary empty sella syndrome, an excessively large diaphragmatic orifice permits herniation of leptomeninges into the sella. Prolonged CSF pressure compresses the gland against the sellar floor. C. Secondary empty sella may result from infarction of a pituitary adenoma, infarction of the pituitary gland, and surgical or radioablation of the gland. (Ar, arachnoid; AP, anterior pituitary; PP, posterior pituitary; C, optic chiasm; 3rd v, third ventricle) |
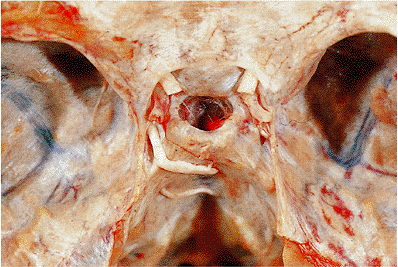 |
Figure 12.14 Superior view of the skull base, demonstrating an incidentally encountered primary empty sella. Normally in this view the upper surface of the pituitary gland would be visible through the diaphragmatic aperture, but here the sella appears empty. Only rarely is primary empty sella syndrome symptomatic. This specimen is from a 57-year-old obese diabetic woman. |
Vasculature
Vascular structures of major surgical significance abound in the sellar region. The paired cavernous sinuses are situated on either side of the sella and, in part, lie lateral and superior to the sphenoid sinuses (Figures 12.8,12.9,12.10,12.11). Each cavernous sinus is partially invested by dura of the middle fossa, as well as by thin bony walls of the sphenoid sinus. Venous drainage to the sinuses comes from a number of sources, including the eye (superior ophthalmic vein), brain (inferior and middle cerebral veins), and sphenoparietal sinus. Communication between right and left cavernous sinuses takes place through intercavernous sinuses bordering the anterior and posterior aspects of the sella (22). The complex thus forms a venous ring around the sella and its contents. Additional intercavernous sinuses are located along the ventral surface of the pituitary. The cavernous sinuses proper contain, in addition to their content of venous sinuses, a number of vital neurovascular structures (23,24). These include the cavernous segments of the internal carotid arteries and segments of cranial nerves III (oculomotor), IV (trochlear), V (trigeminal), and VI (abducens) (Figures 12.8,12.9). Delicate areolar tissue fills the interstices between venous channels, arteries, and nerves. The location of the horizontal portions of the internal carotid arteries within the cavernous sinuses varies, not only from person to person but from left to right. As a result, the carotids may lie immediately adjacent to the sella, in which case they may create a surgical risk (19) (Figures 12.8,12.9). Furthermore, the anterior portions of the carotids may indent the sphenoid bone and thus be separated from the cavity itself by as little as 1 mm of bone (15). Several branches of the internal carotid artery arise within the cavernous sinus, including the meningohypophysial trunk (the largest intracavernous branch), the artery of the inferior cavernous sinus, and small capsular branches (23,24). The meningohypophysial trunk gives rise to several vessels, one of which, the inferior hypophysial artery, supplies the posterior or neural lobe and the pituitary capsule.
Given their location, the cavernous sinuses may be directly involved by pituitary tumors. For example, extension of an invasive adenoma into the cavernous sinuses may produce neuropathies of cranial nerves III through VI (Figure 12.9), including ptosis, facial pain, or diplopia.
The principal arterial supply of the pituitary originates in two branches of the internal carotids: the superior and inferior hypophysial arteries (25,26) (Figure 12.15). A single superior hypophysial artery springs from each carotid shortly after its entry into the cranial cavity and promptly divides into posterior and anterior branches, each of which anastomoses with the corresponding branch from the opposite side to form an arterial ring around the upper pituitary stalk. The anterior branches give rise to trabecular or loral arteries, which descend on the upper surface of the anterior lobe, course toward the pituitary stalk, and terminate in long stalk arteries along the pars tuberalis. In their brief course along the anterior lobe, trabecular arteries each give rise to a small artery of the fibrous core (25). The posterior and anterior branches of the superior hypophysial arteries are also the source of short stalk arteries, which penetrate the superior aspect of the pituitary stalk to run upward or downward within it. In contrast to the superior hypophysial arteries, the inferior branches originate from the meningohypophysial trunks within the cavernous sinuses. They contact the inferolateral portions of the gland and bifurcate into medial and lateral branches that anastomose with their opposite counterparts to form an
P.327
arterial circle about the posterior lobe. Thus, branches of the inferior hypophysial arteries supply primarily the posterior lobe and lower portion of the stalk, contributing only small capsular branches to the periphery of the anterior lobe (27). Although many of the arterial branches in the pituitary stalk and infundibulum form arterioles and capillaries, some give rise to unique vascular complexes termed gomitoli (Figures 12.15,12.16). These balls of thread consist of a central artery surrounded by a glomeruloid tangle of capillaries. The transition from central arteries to the capillaries is via short specialized arterioles endowed with thick smooth muscle sphincters that serve to regulate blood flow. The mixture of periarteriolar capillaries drains into an extensive pampiniform network, the portal system, which envelopes the stalk (Figures 12.2, 12.15).
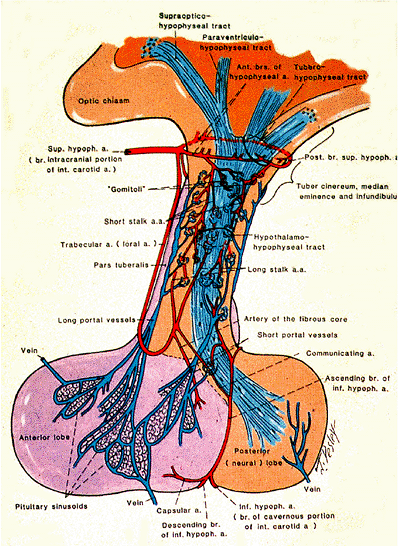 |
Figure 12.15 Diagrammatic representation of the vasculature of the pituitary gland. The superior and inferior hypophysial arteries and branches of the internal carotid arteries comprise the major blood supply of the gland. Small terminal branches of the superior and inferior hypophysial arteries give rise to tangled capillary loops termed gomitoli, which drain into portal vessels. The latter traverse the length of the stalk and terminate as a capillary bed in the anteior lobe. The anterior pituitary thus receives the majority of its blood supply not from arteries but from the portal system. The portal system forms a vital link between the hypothalamus and the pituitary gland. |
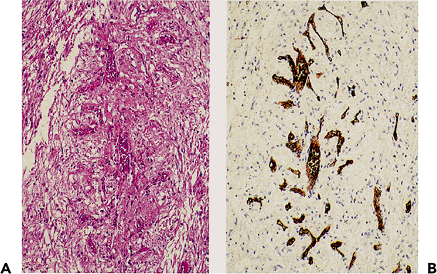 |
Figure 12.16 Gomitoli, tortuous capillary loops surrounding a central arteriole in the upper portion of the pituitary stalk (A) (H&E, original magnification 100). The complex vascularity of the gomitoli is highlighted by staining with Ulex europeus lectin (B) (immunostain, original magnification 100). |
The hypophysial portal system, the critical link between hypothalamus and pituitary, takes its origin from the capillary plexus of the median eminence and stalk, which itself is derived from terminal ramifications of the superior and inferior hypophysial arteries (22). The capillary plexus in the median eminence and superior stalk, the site of uptake of hypophysiotrophic factors, drains into the long portal vessels that course along the surface of the stalk to supply the majority (90%) of the anterior lobe, whereas the smaller capillary plexus in the lower stalk gives rise to the short portal vessels that descend into its central portion, including that bordering the posterior lobe (27,28). Distally, the portal system communicates with a delicate capillary network in the anterior lobe, which carries hypophysiotrophic factors into the pituitary and conveys anterior lobe hormones to the general circulation (Figure 12.17).
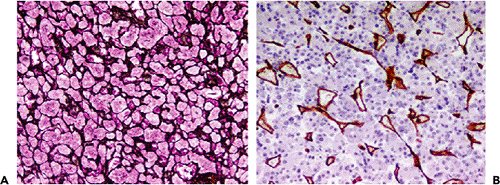 |
Figure 12.17 Adenohypophysis. A. The intricate capillary and connective tissue network outlined in reticulin stain. The reticulin stain is invaluable in the evaluation of pituitary adenomas, which are largely devoid of reticulin, whereas the surrounding normal gland retains it (Wilder reticulin, original magnification 40). B. The capillary endothelium of the anterior lobe capillary network stains strongly for CD31 (immunostain 100). |
Venous outflow of the pituitary is via collecting vessels that drain into the subhypophysial sinus, cavernous sinus, and superior circular sinus (26).
There is considerable variability in the vascular anatomy of the pituitary. Aside from a minor direct arterial supply via capsular branches of the inferior hypophysial arteries, the majority of the anterior lobe's circulation is venous, originating from the portal vessels (25,26). In contrast to that of the anterior lobe, the blood supply of the posterior lobe is direct and arterial, a characteristic that explains the predilection of metastatic carcinomas for the neural lobe.
Physiology and Histology
Hypothalamus
The pituitary is known to be under significant hypothalamic control. In fact, the pituitary and the hypothalamus form a complex neurohormonal circuit, a vital element for maintainance of a normal endocrine status. Weighing approximately 5 g and forming the walls and floor of the inferior third ventricle, the hypothalamus lies above the
P.328
pituitary to which it is connected by the pituitary stalk (Figures 12.512.6,12.7,12.18,12.19). As the name suggests, the hypothalamus lies inferior to the thalamus. Although at first glance it appears poorly demarcated, the hypothalamus is bordered anteriorly by the anterior commissure, lamina terminalis, and optic chiasm; posteriorly and superiorly by the midbrain tegmentum and mamillary bodies; dorsally by the hypothalamic sulcus; and laterally by subthalamic nuclei (29,30). The region consists of several ill-defined but functionally related neuronal nuclei (Figures 12.18,12.19,12.20,12.21). Afferent and efferent connections bring these nuclei into contact with nearby as well as remote portions of the central nervous system, including other diencephalic structures, the cerebrum, brain stem, and spinal cord. Two major and distinct hypothalamohypophysial secretory systems are recognized. One consists of the supraoptic and paraventricular nuclei and their projections to the posterior lobe (supraopticohypophysial and paraventriculohypophysial tracts); the other is composed mainly of nuclei of the tuberal region, the funnel-shaped floor of the third ventricle, and their processes terminating in the median eminence (tuberohypophysial tract) (Figure 12.18).
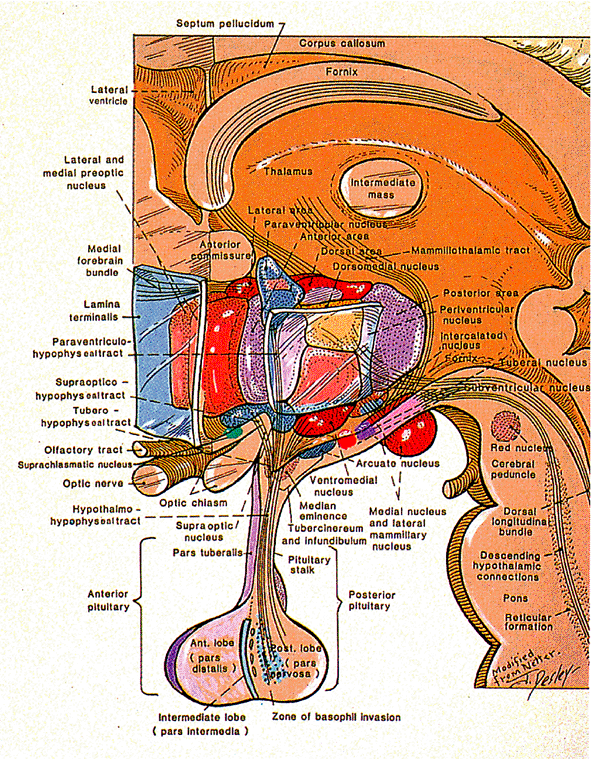 |
Figure 12.18 A diagrammatic representation of the hypothalamic nuclei, showing the supraopticohypophysial and paraventriculohypophysial tracts, as well as the tuberohypophysial tract. The former carry vasopressin and oxytocin along axons to the posterior lobe, whereas the latter carries hypothalamic releasing and inhibiting hormones to the median eminence, where they enter the portal system for transport to the anterior lobe. |
The supraoptic nuclei are located superior to the optic tracts, whereas the wedge-shaped paraventricular nuclei lie ventromedial to the fornix and abut the walls of the third ventricle (Figure 12.19). Due to their predominant composition of large neurons measuring up to 25 m, these are termed magnocellular nuclei (Figure 12.20). Each contains
P.329
vasopressin- and oxytocin-producing neurons, but only one hormone is produced by a given neuron. Their axons form the supraopticohypophysial and paraventriculohypophysial tracts, which carry vasopressin and oxytocin (the two so-called neurohypophysial hormones), as well as their respective carrier proteins, the neurophysins, to the posterior lobe of the pituitary gland. Oxytocin and vasopressin, both nonapeptides, are synthesized as 20-kDa prohormones, which include in their structure the cysteine-rich neurophysin carrier proteins, neurophysin I and neurophysin II, respectively. The precursor molecules are packaged into secretory granules within the Golgi apparatus and transported by axoplasmic flow within unmyelinated axons to nerve terminals in the posterior pituitary lobe, where they are released into the circulation by a calcium-dependent exocytosis (31). Large intra-axonal accumulations of these hormones, named Herring bodies, are often visible by light microscopy as round, granular structures that appear eosinophilic on hematoxylin and eosin (H&E) sections (Figure 12.22). In transit from the hypothalamus to the posterior lobe, prohormones undergo extensive processing and cleavage to form the final products, vasopressin and oxytocin. Although these hormones differ by only two amino acids, oxytocin exhibits virtually no antidiuretic activity, and vasopressin has negligible oxytocic effect. Oxytocin mediates the milk let-down reflex by stimulating contraction of myoepithelial cells surrounding terminal mammary lobules. In addition, it serves a role in parturition, binding, and facilitating contraction in the final stages of parturition. The major physiologic role of vasopressin, also called antidiuretic hormone (ADH), is the formation of hypertonic urine. Acting via cyclic adenosine
P.330
monophosphate, vasopressin increases the water permeability of renal collecting ducts, allowing the hypotonic intraductal fluid to equilibrate with the hypertonic fluid in the medullary interstitium. The results are concentrated urine and conservation of body water. Damage to the neurohypophysis from head trauma, surgery, inflammatory processes, or neoplasms may destroy vasopressin-producing neurons and cause diabetes insipidus.
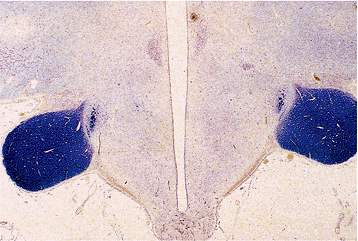 |
Figure 12.19 Coronal whole-mount section through the hypothalamus and third ventricle. The paraventricular nuclei are visible as darkly staining areas beneath the ependyma of the third ventricle (upper field), whereas the supraoptic nuclei lie above the heavily myelinated optic tracts. The arcuate nucleus lies inferior to the base of the third ventricle (cresyl violet). |
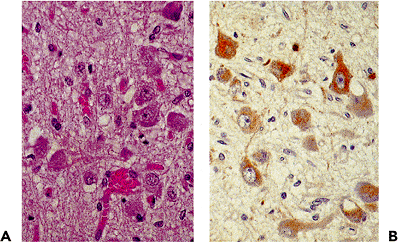 |
Figure 12.20 Paraventricular nucleus of the hypothalamus.A. Its high degree of vascularity is a characteristic of magnocellular nuclei (H&E, original magnification 100). B. The nerve cell bodies stain positively for vasopressin (immunostain, original magnification 100). |
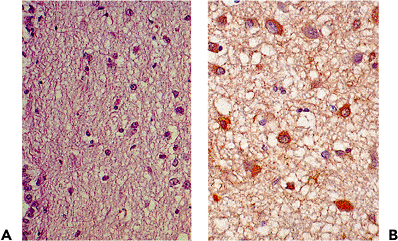 |
Figure 12.21 Periventricular nucleus. A. Lying beneath the ependyma of the third ventricle (bottom left), this ill-defined nucleus is composed of small nerve cell bodies (H&E, original magnification 63). B. Its constituent neurons stain for CRH, a tropic hormone that exerts its effect on corticotrophs in the anterior lobe (immunostain, original magnification 100). |
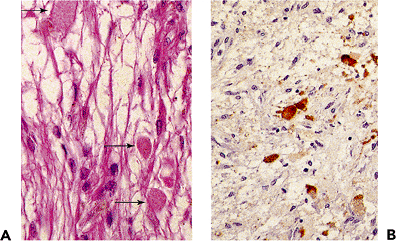 |
Figure 12.22 Pituitary stalk. Axonal swellings termed Herring bodies characterize its axons. A. They are distinguished by their ovoid shape and granular character on H&E [upper left and lower right; arrows]. Herring bodies represent intra-axonal accumulations of oxytocin- and vasopressin-containing granules en route to the posterior lobe (H&E, original magnification 100). B. Herring bodies staining for vasopressin (immunostain, original magnification 100). |
The second component of the hypothalamohypophysial system is the tuberoinfundibular tract. Its fibers originate in a number of hypothalamic nuclei lying within the walls of the inferior third ventricle and tuberal region (29) (Figures 12.18,12.19, 12.21). Products of these nuclei, targeted for the anterior pituitary, consist of releasing and inhibiting hormones. Unlike the magnocellular neurons of the supraoptic and paraventricular nuclei, these are small neurons and for this reason are termed parvicellular neurons (Figure 12.21). Their processes project to the median eminence, a highly vascular zone, located in the posterior proximal portion of the pituitary stalk. Here, the hypothalamic hormones are released into the first portion of the portal system for transport to the anterior lobe. Ultrastructurally, the median eminence consists of closely packed nerve terminals containing membrane-bound neurosecretory granules. Because the terminals lie in close proximity to the fenestrated capillaries that form the origin of the portal system, the overall anatomic arrangement permits ready entry of hypothalamic releasing and inhibiting hormones and perhaps other modulators into the portal system and consequently the anterior lobe. The hypothalamic hormones include five peptide hormones: corticotropin-releasing hormone (CRH), growth hormone-releasing hormone (GHRH), somatostatin, gonadotropin-releasing hormone (GnRH or LHRH), and thyrotropin-releasing hormone (TRH). The sites of synthesis of the various hypothalamic hormones, their characteristics, and target cells are summarized in Tables 12.1 and 12.2. In addition to these hormones, several bioactive substances produced in the hypothalamus participate in the regulation of anterior pituitary hormone secretion. The most significant one is dopamine, which has a tonic inhibitory control of pituitary lactotrophs (32).
Table 12.1 Pituitary Hormones and Hypothalamic Stimulatory and Inhibitory Hormones | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||
Adenohypophysis
The pituitary is a tan to brown, bean-shaped structure varying in weight from 500 to 700 mg (Figure 12.1). An average-sized gland of 600 mg measures about 13 10 6 mm. Generally, the weight of the female pituitary is greater than that of the male (33). Among females, the gland is smaller in nulliparas than in multiparas. In pregnancy the gland enlarges significantly (up to 30%) primarily as a result of lactotroph cell hyperplasia (33,34). The anterior lobe comprises 80% of the pituitary and includes the pars distalis, intermedia, and tuberalis. The body and stalk of the gland are surrounded by a delicate capsule derived from the meninges (35). Staining characteristics roughly divide the pars distalis into a central mucoid wedge and two lateral wings, zones best visualized in coronal and horizontal sections.
By light microscopy, the cells of the anterior lobe show variation, not only in size and shape but also in their histochemical staining characteristics (Figure 12.23,12.24). They are arranged in nests, cords, and small acini bounded by an interlacing capillary network that is best seen on reticulin stain (see Figure 12.17). This architectural pattern, altered in hyperplasia and conspicuously absent in adenomas, is of considerable diagnostic significance. The pars intermedia, poorly developed in humans, consists in large part of epithelium-lined spaces containing periodic acid-Schiff (PAS)-positive colloid; the constituent cells are ciliated, goblet, and endocrine; the last show variable immunoreactivity
P.331
for pituitary hormones (36) (Figure 12.25). Incidental Rathke's cleft remnants, the vast majority of which are microscopic in size, are present in 30% of pituitaries; the majority of them are located in the intermediate lobe (37).
Table 12.2 Major Hypothalamic Hormones: Their Composition and Localization | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In H&E-stained sections, three principal cell types are identified in the normal anterior lobe: acidophils (40%), basophils (10%), and chromophobes (50%) (Figures 12.23,12.24). The designations reflect their staining affinities for acidic and basic dyes, with the chromophobic cells lacking affinity for either. These reactivities form the basis of an outdated classification of pituitary adenomas that offers little in specifying their hormone content or endocrine function. On the other hand, advances in immunohistochemistry permit morphologic and functional correlation (Figure 12.26). Numerous cells in the central or mucoid wedge are basophilic and stain strongly via the PAS method. Such cells produce adrenocorticotropin (ACTH) and glycoprotein hormones (LH, FSH, TSH). In contrast, most cells in the lateral wings are acidophilic and are engaged either in growth hormone (GH) or, less frequently, in prolactin (PRL) production. The essential morphologic features of the five principal cell types and the biochemical characteristics of the six hormones of the anterior pituitary are summarized in Table 12.3. Their ultrastructural features are presented in Table 12.4.
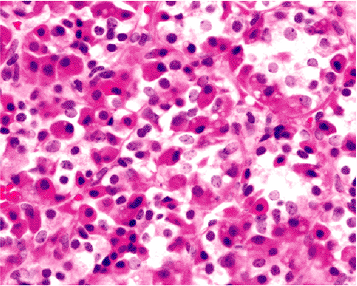 |
Figure 12.23 Anterior lobe. An H&E-stained section shows chromophobic, acidophilic, and basophilic cells. Acidophils are most numerous in the lateral wings, whereas basophils are found in greatest number in the central or mucoid wedge. The different cell types are arranged in acinar formations that can be highlighted by reticulin stain (see Figure 12.17) (original magnification 200). |
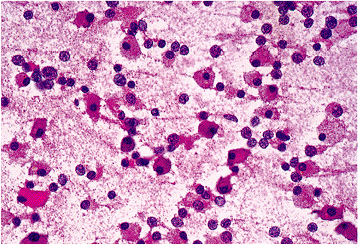 |
Figure 12.24 H&E-stained cytologic smear of the normal anterior lobe, demonstrating acidophils, chromophobes, and basophils. Delicate nuclei, inconspicuous nucleoli, and variable cytoplasmic staining characterize normal cells and permit their distinction from adenoma cells (original magnification 100). |
P.332
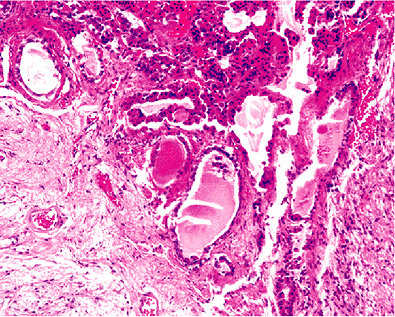 |
Figure 12.25 Intermediate lobe remnant. Such cysts are lined by a single layer of cuboidal to columnar epithelium that may be nonciliated, ciliated, mucin-producing, or granulated. The cyst contains an eosinophilic colloid (H&E, original magnification 100). |
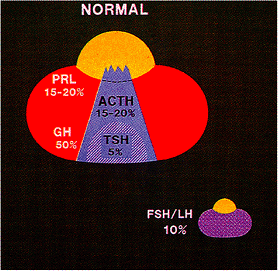 |
Figure 12.26 Preferential localization and relative frequency of functional anterior lobe cell types in the normal pituitary gland. Note that gonadotrophs (LH/FSH cells), represented in the small gland (lower right), are distributed diffusely and show no preferential localization. |
Table 12.3 The Normal Anterior Pituitary: Morphologic and Functional Features of Secretory Cells | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
P.333
Table 12.4 The Normal Pituitary: Ultrastructural Features | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
P.334
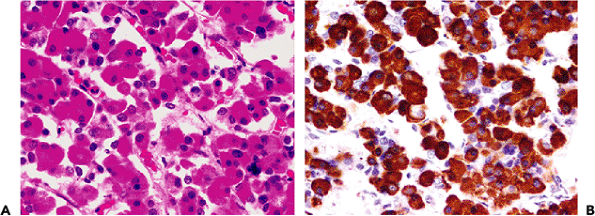 |
Figure 12.27 Somatotrophs. A. By H&E stain, somatotrophs are medium-sized cells with abundant, eosinophilic and granular cytoplasm GH. Somatotrophs comprise 50% of anterior lobe cells (original magnification 200). B. The strong staining reaction is a reflection of the numerous secretory granules present at the ultrastructural level (see Figure 12.28) (immunostain, original magnification 200). |
Somatotroph cells.
Somatotrophs, or GH cells, occur in greatest density in the lateral wings and comprise approximately 50% of all adenohypophysial cells. A minority of somatotroph cells are scattered throughout the median portion of the gland. They are medium-sized, ovoid cells with round, centrally located nuclei, relatively prominent nucleoli, and with abundant acidophilic granules (Figure 12.27). Immunohistochemical stains for GH shows strong and diffuse cytoplasm staining, consistent with the numerous secretory granules present at the ultrastructural level (Figures 12.27,12.28). Somatotroph cells are rather stable during life, and their number, morphology, and immunoreactivity are unchanged by age.
The product of GH cells has extensive effects by direct action of GH and actions through mediators of hepatic origin called somatomedins (insulin-like growth factor-I, or IGF-1) (32). Growth hormone functions as the major promotor of growth but also in several other metabolic pathways, including glucose, insulin, and fatty acid. The pulsatile secretion of GH from the anterior lobe is under the control of the two hypothalamic regulatory hormones: growth hormone releasing hormone (GHRH) and somatostatin (growth hormone-release inhibiting hormone). The GHRH controls GH synthesis by regulating transcription of GH mRNA via control of cAMP levels. Somatostatin appears to determine the timing and amplitude of GH pulses but has no effect on GH synthesis. Hypersecretion of GH in children causes gigantism, whereas its overproduction in adults leads to acromegaly.
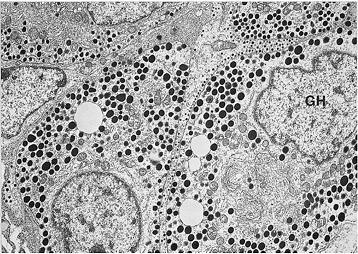 |
Figure 12.28 Densely granulated somatotrophs (GH cells) showing prominent Golgi and numerous 200- to 500-nm secretory granules (original magnification 11,700). |
Lactotroph cells.
Lactotrophs, or PRL cells, comprise approximately 20% of anterior pituitary cells and are concentrated in the posterior portions of the lateral wings. Histologically, they appear either acidophilic (densely granulated) or chromophobic (sparsely granulated). Chromophobic cells are more numerous, are located predominantly in the posterior lateral wings, possess elongate processes, and, despite an abundance of endoplasmic reticulum and well-developed Golgi complexes, contain relatively few cytoplasmic granules (Figures 12.29,12.30, and Table 12.4). Densely granulated lactotrophs are thought to represent a storage phase, whereas sparsely granulated cells are engaged in active secretion. A characteristic pattern of PRL staining of lactotrophs by immunohistochemistry, the so-called Golgi pattern, is the presence of paranuclear staining corresponding to PRL in the Golgi apparatus (Figure 12.29).
With the exception of pregnancy and lactation, there is no significant difference in PRL cell number between males and females. The doubling in volume of the pituitary during pregnancy is due to striking hyperplasia as well as hypertrophy of chromophobic lactotrophs, termed pregnancy cells. They persist until shortly after delivery or the termination of lactation (33,34). Prolactin cell hyperplasia also may accompany estrogen administration and hypothyroidism (32). The existence of mammosomatotrophs, cells engaged in PRL and GH production and possessing unique ultrastructural features, attests to the existence of a histogenetic relationship between PRL and GH cells (38).
Prolactin secretion is unique among the anterior pituitary hormones in that it is under tonic hypothalamic
P.335
inhibition by dopamine (hypothalamic PRL-inhibitory factor, or PIF) produced by tuberoinfundibular dopamine neurons. Several prolactin-releasing factors participate in PRL secretion, including TRH and vasoactive intestinal peptide (VIP). A fragment of GnRH also has been shown to inhibit PRL release. Prolactin synthesis is also regulated by effects of estrogen on PRL gene expression. Disruption of the hypothalamus or the hypothalamic hypophysial stalk may impede dopamine delivery to the anterior lobe, causing hyperprolactinemia, a phenomenon termed stalk effect. Common situtations are any space-occupying sellar or parasellar mass (e.g., pituitary macroadenoma, Rathke's cleft cyst, craniopharyngioma, or glioma) that compresses the pituitary stalk. The most striking example of stalk effect is the hyperprolactinemia that follows surgical transection of the stalk, a practice now obsolete but once used in the past for the treatment of metastatic breast cancer (39).
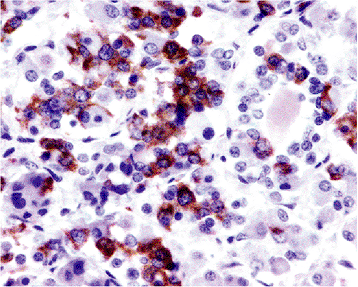 |
Figure 12.29 Lactotrophs. Lactotrophs comprise 15% to 20% of anterior lobe cells. The majority are sparsely granulated, angular cells with processes that may wrap around adjacent cells. Many lactotrophs in this field show paranuclear staining, a pattern corresponding to PRL in the Golgi apparatus (PRL immunostain, original magnification 100). |
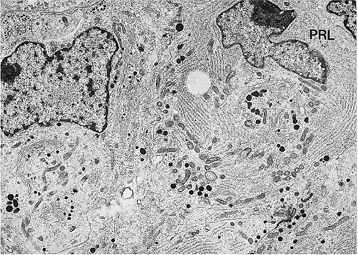 |
Figure 12.30 Sparsely granulated PRL cell. Note the abundant cisternae of rough endoplasmic reticulum and the prominent Golgi complex containing pleomorphic developing granules. Mature PRL granules range in size from 200 to 350 nm (original magnification 8,700). |
Prolactin acts through specific prolactin receptors in multiple tissues, including breast, liver, ovary, testis, and prostate. The main site of PRL action is in the breast, where it stimulates the formation of casein, lactalbumin, lipids, and carbohydrates, all essential components of breast milk. During pregnancy, high levels of estrogen, progesterone, placental lactogen, and PRL induce acinar development and promote milk formation. As previously noted, milk secretion is under the control of oxytocin, a potent stimulator of myoepithelial cell contraction in breast tissue.
Corticotroph cells.
Corticotrophs, or ACTH cells, comprise 15% to 20% of adenohypophysial cells and are most numerous in the mid- and posterior portions of the mucoid wedge (Figure 12.26). Histologically, corticotroph cells are polygonal, medium- to large-sized, and basophilic (Figure 12.31). A paranuclear vacuole that corresponds to one or several lysosomal structures at the ultrastructural level is
P.336
typically seen in the cytoplasm (Figure 12.32) (36,40). Corticotroph cells are strong PAS positive due to a carbohydrate moiety contained in proopiomelanocortin (POMC), the precursor molecule of ACTH. In immunostained preparations, corticotrophs may be shown to contain not only ACTH (Figure 12.31) but also other POMC derivatives, including -lipotropin ( -LPH), melanocyte-stimulating hormone (MSH), endorphin, and enkephalin. Perinuclear bundles of cytokeratin filaments are also a characteristic feature of ACTH cells (Table 12.4). Under conditions of glucocorticoid excess, either exogenous or endogenous, corticotrophs accumulate cytokeratin as a manifestation of Crooke's hyaline change (Figures 12.33,12.34).
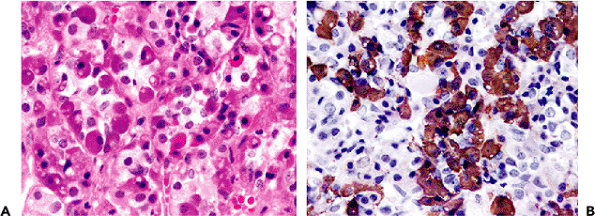 |
Figure 12.31 Corticotrophs (ACTH cells). A. Corticotrophs comprise about 15% to 20% of anterior lobe cells and are mainly located in the mucoid wedge. By H&E stain, corticotrophs are basophilic cells with ovoid to polyhedral shape and central nucleus. Many have a small vacuole near the nucleus, representing a massive lysosome (original magnification 200). B. Note the clustering of cells, a characteristic feature of corticotrophs (ACTH immunostain, original magnification 200). |
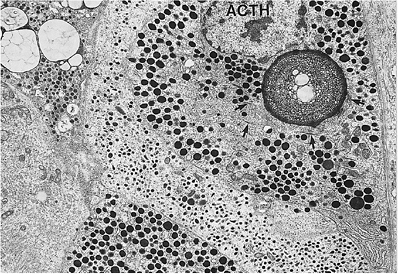 |
Figure 12.32 Corticotroph (ACTH cell). The cell contains the typical large lysosome and spherical to slightly pleomorphic and variably electron-dense secretory granules measuring 150 to 450 nm. Bundles of intermediate filaments (arrows) are a regular feature of corticotrophs. The adjacent cells with small granules are likely TSH cells (original magnification 8,250). |
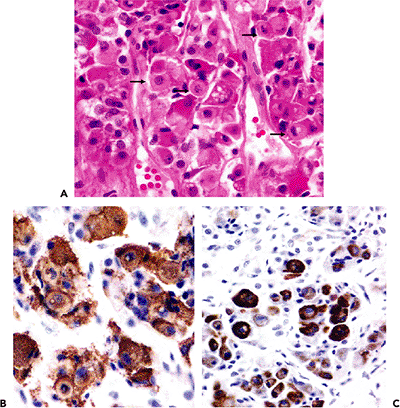 |
Figure 12.33 Crooke's hyaline change. A. Crooke's cells (arrows) are characterized by a conspicuous eosinophilic perinuclear ring consisting of cytokeratin (H&E, original magnification 100). B. ACTH stains show central displacement of the nucleus and organelles by filament accumulation (ACTH immunostain, original magnification 100). C. Staining for cytokeratin show strong reactivity of the Crooke's cells (CC immunostain, original magnification 100). |
Adrenocorticotropin (ACTH), the principal product of corticotrophs, stimulates the adrenal cortex to secrete glucocorticoids, mineralocorticoids, and androgens (32). It plays a critical role in both the transport of amino acids and glucose into muscle, as well as the stimulation of insulin release from the pancreas. Pituitary ACTH secretion is
P.337
regulated by hypothalamic corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP). Adrenocorticotropin is part of a larger precursor molecule, proopiomelanocortin (POMC), which is enzymatically cleaved in the anterior pituitary into -LPH and ACTH. In the intermediate lobe, ACTH is cleaved into melanocyte-stimulating hormone (MSH) and other ACTH-like peptides. Excess secretion of ACTH, such as occurs in Cushing's disease, leads to stereotypic abnormalities such as truncal obesity, hypertension, diabetes mellitus, amenorrhea, hirsutism, muscle atrophy, striae, impaired wound healing, and mental status changes. Hyperpigmentation also may occur in this setting and is due to the effects of MSH.
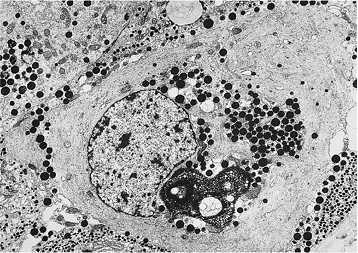 |
Figure 12.34 Crooke's cell. This electron micrograph of the pituitary adjacent to a corticotroph cell adenoma displays massive accumulation of cytokeratin filament. Secretory granules are displaced to the perinuclear zone or to the periphery of the cytoplasm. Note the large lysosome in the lower portion of the field (original magnification 6,720). |
Thyrotroph cells.
Thyrotrophs, or TSH cells, are located primarily in the anterior part of the mucoid wedge and comprise only 5% of adenohypophysial cells (41). They are medium sized and angular or elongate (Figures 12.35,12.36). Like corticotrophs, normal TSH cells are basophilic and are PAS positive (see Table 12.4 for ultrastructural features).
Thyroid-stimulating hormone (TSH, a glycoprotein hormone) binds to thyroid cells, inducing RNA and protein synthesis and thereby the production of thyroglobulin and thyroid hormones. Like the other two glycoprotein hormones of the pituitary [luteinizing hormone (LH) and follicle-stimulating hormone (FSH)], TSH consists of two noncovalently bound subunits, alpha ( ) and beta ( ). The -subunit is common to all three glycoprotein hormones; the -subunit is specific for each hormone and confers biological specificity. Secretion of TSH is regulated by both hypothalamic hormones and circulating thyroid hormones. Thyrotropin-releasing hormone (TRH) stimulates TSH release, while somatostatin and dopamine can inhibit TSH secretion. In the setting of primary hypothyroidism, thyrotrophs undergo hypertrophy and hyperplasia. When excessive, the response may produce sufficient hypertrophy of the pituitary gland to mimic adenoma. Pituitary adenomas that elaborate TSH are rare; most occur in the setting of hypothyroidism (36), although a minority result in hyperthyroidism.
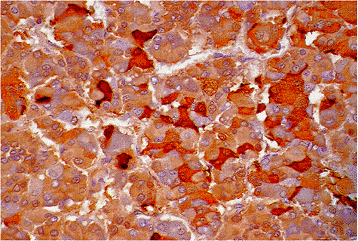 |
Figure 12.35 Thyrotroph (TSH cell). Thyrotrophs are medium-sized angulated cells with some demonstrating elongate processes. They comprise only about 5% of anterior lobe secretory cells and show strong TSH immunoreactivity (TSH immunostain, original magnification 100). |
Gonadotroph cells.
Gonadotrophs, or FSH and LH cells, comprise 10% of the adenohypophysis, show a strong affinity for both basic and PAS stains, and generally are evenly distributed throughout the anterior lobe. Immunohistochemical and ultrastructural studies have shown that FSH and LH may be produced in isolation or by the same cell (42) (Figures 12.37,12.38) (see Table 12.4 for ultrastructural features). In the daily practice of surgical pathology, monoclonal antibodies against the specific -subunits of LH and FSH are universally applied. In addition, antibodies
P.338
against the -subunit of the glycoprotein pituitary hormones (LH, FSH, and TSH) is useful for determination of abnormal production and/or secretion of this subunit hormone.
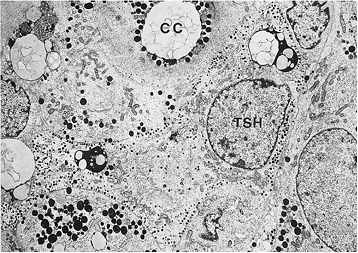 |
Figure 12.36 Thyrotroph (TSH cell). This micrograph of the normal anterior pituitary shows the characteristic elongate thyrotrophs, the large lysosomes frequently observed in cells of this type, and small (150-nm) peripherally located secretory granules. Part of a Crooke's cell (CC) is also shown (original magnification 5,300). |
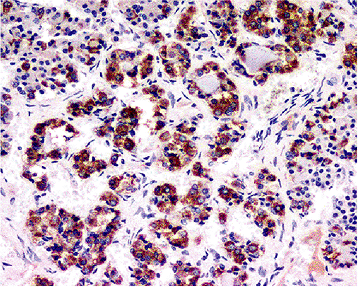 |
Figure 12.37 Gonadotroph (FSH/LH cell). Gonadotroph cells manufacture both LH and FSH. The paucity of strongly staining cells in this field reflects the fact that only 10% of anterior lobe secretory cells are gonadotrophs (FSH immunostain, original magnification 100). |
Both LH and FSH play distinct but essential roles in the reproductive physiology of males and females. Secretion of these hormones from the gonadotroph cells is regulated by integration of the GnRH (LHRH) signal and feedback effects of gonadal steroids and the peptides inhibin, follistatin and activin (43). GnRH (LHRH) interacts with a membrane receptor to regulate both LH and FSH release and synthesis, and it is necessary for gonadotroph cells' function; gonadal steroids and peptides are ineffective alone in stimulating release. In the female, LH is required for ovulation and follicular luteinization. In males, it stimulates interstitial Leydig cells to produce testosterone. Follicle-stimulating hormone promotes follicular development in the female, whereas in the male it induces Sertoli cells to produce an androgen-binding protein.
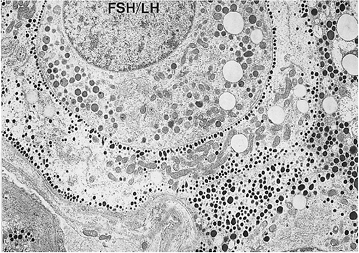 |
Figure 12.38 Gonadotroph (FSH/LH cell). The dull, low-contrast appearance of the cell is typical of gonadotrophs. Their spherical and slightly irregular secretory granules are characteristic; they have variable electron density and measure 250 to 400 nm. The cell process surrounding the gonadotroph likely belongs to a thyrotroph (original magnification 8,250). |
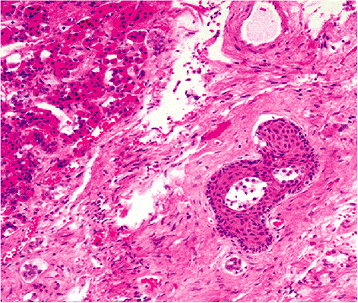 |
Figure 12.39 Anterior pituitary, pars tuberalis. Squamous metaplasia of secretory cells is a common feature of this portion of the gland. |
Par Tuberalis.
The pars tuberalis, an upward extension of the anterior lobe along the pituitary stalk, is composed of normal acini of pituitary cells scattered among surface portal vessels. These cells often show immunoreactivity for ACTH, FSH, LH, and -subunit. Although in functional terms they may or may not differ from similar cells in the pars distalis, these cells do show a distinct tendency to undergo squamous metaplasia (Figure 12.39) (44).
Follicles are not an uncommon feature of the normal anterior pituitary. Their functional constituent cells, termed follicular cells, appear to be derived in large part from various secretory cells (Figure 12.40). Ultrastructurally, they are
P.339
often poorly granulated or agranular and linked by apical junctional complexes. Within follicular lumina, one often finds cellular debris (Figure 12.41). The stimulus for follicle formation is therefore thought to be damage or rupture of anterior lobe secretory cells (45).
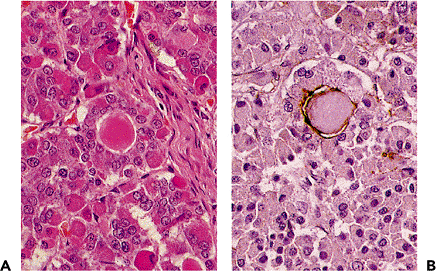 |
Figure 12.40 Anterior pituitary, follicle formation. A. Follicles, some containing a small quantity of colloid-like material, are commonly found in the anterior lobe (H&E, original magnification 100). B. Follicles show prominent apical staining for epithelial membrane antigen (EMA) (EMA immunostain, original magnification 100). |
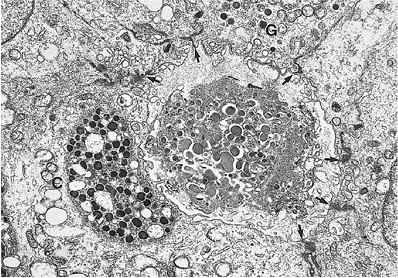 |
Figure 12.41 Electron micrograph of a pituitary follicle. This young follicle contains cell debris within its lumen. The gonadotroph (G), but not the corticotroph (C), is part of this follicle. Follicles are composed of granulated adenohypophysial cells that, through the formation of junctional complexes (arrows), surround damaged adenohypophysial cells (original magnification 12,600). |
Folliculostellate cells.
The folliculostellate cell is the sixth cellular element of the adenophypophysis, a specialized sustentacular-like cell that appears to have multiple functions related to phagocytosis and secretion of growth factors (46,48). They comprise less than 5% of the anterior lobe cells, are scattered about the anterior lobe, and contribute to the formation of anterior lobe follicles and cysts of the intermediate lobe. They are readily identified by their reactivity for S-100 protein (Figure 12.42), and can also be identified by glial fibrillary acidic protein (GFAP) and vimentin. They participate in regulating the activity of anterior pituitary endocrine cells through the production of cytokines (such as interleukin-6, and leukemia inhibitory factor) and growth factors (including basic fibroblast growth factor and vascular endothelial growth factor) (48). Additionally, ultrastructural and immunohistochemical studies on human adenomatous and nonneoplastic pituitary folliculostellate cells suggest that they may represent an adult stem cell progenitor population (47,48).
Variation in Normal Morphology of the Adenohypophysis
A number of normal histologic variations in the pituitary gland may mimic clinically significant lesions. Examples include squamous cell nests in the pars tuberalis, basophil invasion of the posterior lobe, granular cell clusters and tumorlets of the stalk and neurohypophysis, and salivary gland rests.
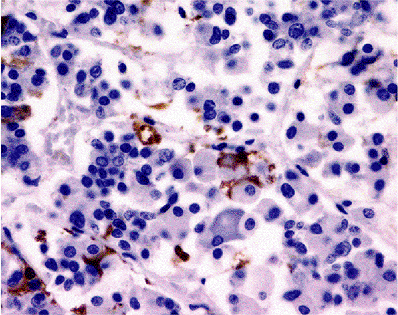 |
Figure 12.42 Anterior lobe folliculostellate cells. Folliculostellate cells comprise less than 5% of anterior lobe cells and are scattered throughout the pituitary, including the intermediate lobe zone. Folliculostellate cells staining for S-100 protein, GFAP, and vimentin (S-100 immunostain, original magnification 100). |
Squamous cell nests show a definite predilection for the pars tuberalis; they have been found in up to 24% of autopsy cases, occur more commonly in elderly patients, and show no sex predilection (49). They arise through a process of metaplastic transformation from adenohypophysial cells, as evidenced by simultaneous expression of keratin and pituitary hormones, most often FSH, LH, or ACTH (44) (Figure 12.39). Because squamous metaplasia also may accompany foci of ischemic infarction in the anterior lobe, it appears to be an inherent property of pituitary secretory cells.
Basophil invasion, a finding more common in males and the elderly, may at first glance mimic an adenoma. It consists of corticotrophic basophils extending from the pars intermedia into the neurohypophysis (Figures 12.43,12.44). Similar to ordinary corticotrophs, these basophilic cells are immunoreactive for ACTH, -LPH, endorphins, and other POMC derivatives; however, they contain few cytokeratin filaments and are less susceptible to Crooke's hyalinization in response to hypercortisolism (36).
Salivary gland rests appear as tubular glands upon the surface or in the substance of the neurohypophysis, often just posterior to the pars intermedia (Figure 12.45). They are composed of a single layer of cuboidal to columnar epithelium with basally oriented nuclei and finely granular, strongly PAS-positive cytoplasm. Salivary gland rests are often oncocytic. Their ultrastructural features include well-developed rough endoplasmic reticulum, secretory droplets, microvilli, and desmosomes, all of which support the contention that they are indeed salivary glands (50).
P.340
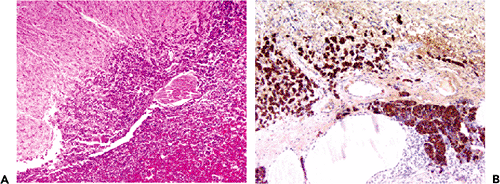 |
Figure 12.43 Basophil invasion. A. This subpopulation of corticotroph cells appears to infiltrate the substance of the posterior lobe (H&E, original magnification 4). B. The invading cells are strongly immunoreactive for ACTH and other POMC derivate hormones (ACTH immunostain, original magnification 40).] |
Age-Related Changes of the Adenohypophysis
The cytology of the anterior pituitary varies with age. For instance, the late fetal or term pituitary gland shows PRL cell hyperplasia, a reflection of high maternal estrogen levels. Also, when compared with the adult pituitary, the prepubertal gland shows gonadotrophic cells to be poorly developed. In adults the pituitary undergoes several changes with increasing age (51,52).
With few exceptions, the main one being pregnancy, the gland weight remains stable throughout life, decreasing only slightly in the elderly due to anterior lobe atrophy. Pregnancy results in a doubling of the size of the pituitary due to gradual increase in large chromophobic PRL cells ( pregnancy cells ) (53,54) (Figure 12.46). The increase in PRL-producing cells during pregnancy appears to result not only from proliferation of PRL cells but also from recruitment of GH cells to PRL production (55). This increase in PRL-producing cells, in large part a hyperplasia, gradually disappears within months after delivery or abortion. The process is often incomplete; hence, the pituitaries of multiparas are larger than those of women who were never pregnant. Pregnancy also results in a significant decrease of gonadotropin immunoreactivity, a reflection of the production of gonadotropic hormones by the placenta.
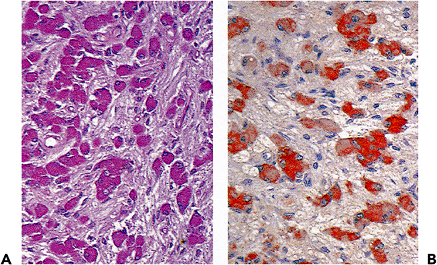 |
Figure 12.44 Basophil invasion. A. PAS staining (original magnification 63). B. ACTH immunostain (original magnification 63). |
The effects of age on the cellular contents of several pituitary hormones has been studied. Specifically, GH and PRL cells have been shown to undergo no significant decrease in number, granularity, distribution, or immunoreactivity with increasing age (56,57). Both ACTH and TSH cells also appear to be unaffected by age, but no data are available regarding the effects of senescence on FSH and LH cells. Small foci of lymphocytes, usually in the intermediate lobe, are present in about 40% of adult pituitaries but are conspicuously absent in newborns and very young children (51).
Fibrosis is the most frequent age-related change in elderly patients. It is generally perivascular in distribution (Figure 12.47)
P.341
but is on occasion patchy, suggesting a remote microinfarct. Interstitial and intracellular deposits of amyloid have been demonstrated in the majority of autopsy-derived anterior pituitaries (58). Immunohistochemically, these reacted for antiamyloid lambda ( ) light chain and amyloid P component. The mean volume percentage of such deposits is approximately 0.5% of the anterior lobe. The occurrence of amyloid and its degree of deposition was related not only to patient age but also to the prevalence of chronic obstructive pulmonary disease and to non insulin-dependent diabetes mellitus.
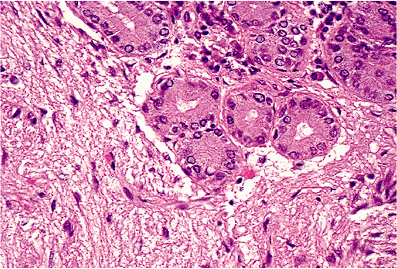 |
Figure 12.45 Salivary gland rest in the posterior lobe. The glands are composed of a single layer of cuboidal to columnar epithelium with basally oriented nuclei and granular PAS-positive cytoplasm. Salivary gland rests are encountered both on the surface of or within the posterior lobe, where it abuts the intermediate lobe zone (H&E, original magnification 63). |
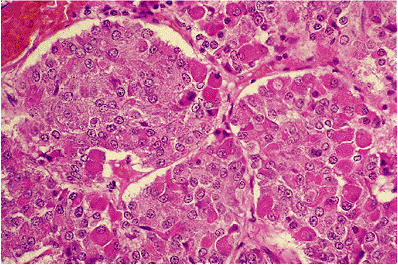 |
Figure 12.46 The pituitary in pregnancy features abundant pale chromophobic PRL cells (pregnancy cells) (H&E, original magnification 100). |
Neurohypophysis
As a functional unit, the neurohypophysis consists of the infundibulum, pituitary stalk, and posterior lobe. The posterior lobe, a ventral extension of the central nervous system, is the site of release of the hypothalamic hormones oxytocin and vasopressin. Its cellular elements consist of unmyelinated axons originating from the supraoptic and paraventricular nuclei and, to a lesser extent, from cholinergic neurons of the hypothalamus, an extensive vascular network, and specialized glial cells termed pituicytes (Figure 12.48).
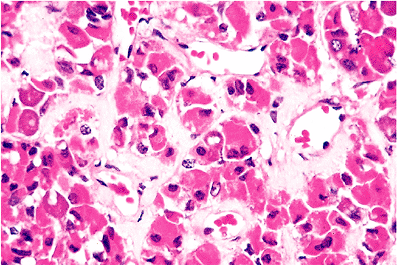 |
Figure 12.47 Perivascular fibrosis is a common feature of the aging pituitary (H&E, original magnification 100). |
Pituicytes, the most numerous cells of the neurohypophysis, are morphologically elongated, uni- or bipolar cells that display the prolongation of the cytoplasm into one or more processes. Pituicytes are strongly positive for glial fibrillary acidic protein (GFAP) (Figure 12.48), as well as S-100 protein and vimentin. Similar to glial cells of other areas of the central nervous system, pituicytes expand processes to adjacent connective tissue or to a blood vessel wall. Pituicytes appear to exist in five principal forms: major, dark, ependymal, oncocytic, and granular (59). Their morphologic diversity, ranging from astrocytic to ependymal, is thought to be a reflection of their physiologic role, which as yet is unclear (60).
Histologically, the axons of the posterior lobe are readily identified using silver stains and/or immunostains for
P.342
neuronal markers. Focal axonal dilatations, known as Herring bodies, represent intra-axonal accumulations of posterior lobe hormones (Figure 12.22). At the ultrastructural level, the unmyelinated axons appear as delicate fibers, measuring 0.05 to 1.0 m in diameter, which contain longitudinal arrays of microtubules and neurofilaments. Two types of neurosecretory axon, A and B, have been described based on the morphology of their neurosecretory granules. Type A fibers, far more numerous than type B, contain 100- to 300-nm oxytocin and vasopressin granules, whereas type B fibers, likely aminergic in nature, contain granules ranging from 50 to 100 nm (61). Neurosecretory fibers are closely associated with pituicytes, their axons often being ensheathed by them (Figure 12.49).
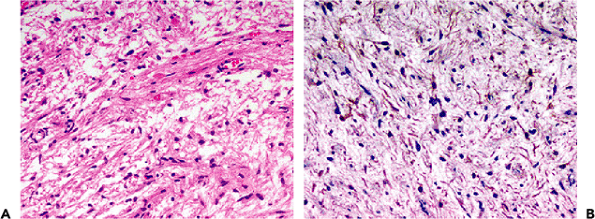 |
Figure 12.48 Posterior lobe. A. Pituicytes have elongated nuclei dispersed within the neuropil of the neurohypophysis (H&E, original magnification 100). B. These cells stain positively for glial fibrillary acid protein (GFAP) (GFAP immunostain, original magnification 100). |
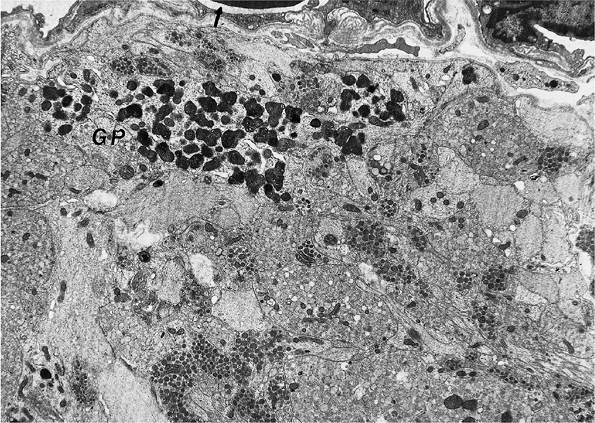 |
Figure 12.49 Pituitary, posterior lobe. This electron micrograph shows axonal processes containing neurosecretory granules of varying electron density. A granular pituicyte (GP) containing numerous prominent lysosomes lies in close proximity to the intravascular space (arrow). The intravascular space is bounded by fenestrated endothelial cells as seen here. Outside the endothelium lies the perivascular space, a region containing a variety of cell types (not shown here), including pericytes, histiocytes, fibroblasts, and mast cells (original magnification 6,200). |
The most important function of the neurohypophysis is the transfer of hormonal substances from neurosecretory granules to the intravascular space. The complex anatomy of the neuronal, vascular, and perivascular compartments forms the basis for this elaborate process. Beginning at the neuronal side, neurohormonal factors appear to be released into minute channels that traverse the outermost, or abluminal, basement membrane of vessels to communicate with the perivascular space. They then traverse the inner, or luminal, basement membrane and endothelium in order to gain access to the vascular space (62) (Figure 12.49).
Variation in Normal Morphology of the Neurohypophysis
Granular cell nests or tumorlets, most located in the stalk or posterior lobe, are found in about 6% of autopsy pituitaries and are more common among the elderly (63). Varying from scattered cells to compact tumorlike nodules, they are composed of plump cells with granular acidophilic and strongly PAS-positive cytoplasm and relatively small nuclei (Figure 12.50). Only rarely do granular cells form clinically significant tumors (64). The origin of granular cell tumorlets and tumors of the neurohypophysis is uncertain. In rare cases, GFAP immunoreactivity has been shown, providing some evidence of the hypothesis that these granular cell nests may originate from pituicytes (65).
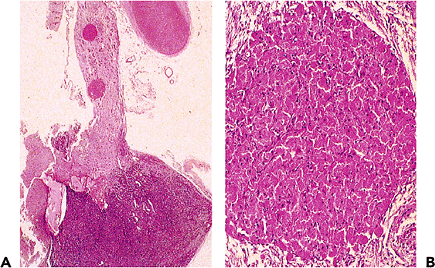 |
Figure 12.50 Pituitary stalk, granular cell tumorlets. A. Low-power view of the stalk shows two tumorlets. The optic chiasm is at the upper portion of the field; the anterior lobe is at the lower portion of the field (H&E, original magnification 20). B. High-power view of a granular cell tumorlet. Such nodules are composed of pituicytes, modified glial cells, with abundant lysosome-rich eosinophilic cytoplasm. Tumorlets, as well as individual granular cells, are of no clinical significance (H&E, original magnification 100). |
P.343
Differential Diagnosis
The principal consideration in differential diagnosis of pituitary lesions is the distinction of normal pituitary tissue from adenoma. The most conspicuous architectural feature of the adenohypophysis is the arrangement of its cells in acini that, depending on orientation of section, vary from round to oval or somewhat elongate. The acini are surrounded by a delicate reticulin- or PAS-positive capillary network (Figure 12.17). In contrast, pituitary adenomas lack this uniform acinar architecture, showing only scant reticulin that is limited to scattered vessels (Figure 12.51). Although most normal pituitary acini are heterogeneous in their cellular content, thus permitting the distinction of normal from adenomatous tissue on H&E sections alone, some parts of the pituitary contain largely a single cell type and appear fairly monomorphous. For instance, eosinophilic GH cells are present in large numbers in the lateral wings. On the other hand, occasional adenomas composed of mixed cell populations (often ones associated with acromegaly) superficially resemble normal adenohypophysis. As a result, the distinction of normal from adenomatous tissue may be more easily achieved by PAS and reticulin staining than by immunohistochemistry alone. Small biopsies of the intermediate lobe may include the so-called basophilic infiltration normally seen in the posterior pituitary (Figures 12.43,12.44). Since these basophilic cells are arranged diffusely or in clusters, and lack the typical acinar formation seen in the anterior pituitary, they may be mistaken for ACTH-microadenomas.
A limited biopsy of the pituitary may occasionally include intermediate zone cysts, which are normal derivatives of Rathke's cleft. Correlation with radiologic and operative data usually obviates confusion with Rathke's cleft cyst. Clinically significant cysts are readily evident on neuroimaging and are identified as sizable cysts by the experienced surgeon.
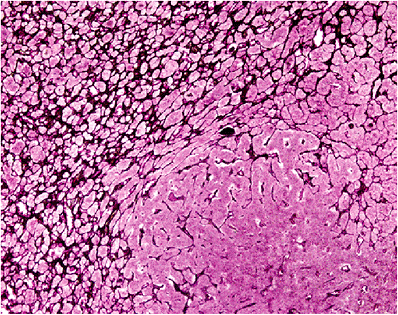 |
Figure 12.51 Disruption of the reticulin network in a pituitary adenoma. Compare the acinar pattern of the normal adenophypophysis (upper left) with the adenoma (bottom right) (wilder reticulin, original magnification 100). |
As previously noted above, adenohypophysial cells may undergo squamous metaplasia, particularly in the pars tuberalis. This location is only occasionally sampled in surgical specimens. Scant in extent, intimately associated with adenohypophysial cells, and cytologically benign, they are unlikely to be confused with either cysts (epidermoid or dermoid cysts) or with neoplasms (craniopharyngiomas). In very small numbers, cytologic benign lymphocytes are seen in the intermediate zone of the normal pituitary in 10% of autopsied subjects (66). Unassociated with endocrine disease, such cells are readily distinguished from the far more widespread and dense infiltrates of lymphocytic hypophysitis or abscess.
A limited biopsy of the neurohypophysis can readily be mistaken for glioma in that the vast majority of its nucleated cells are specialized astrocytes (pituicytes). Unlike pilocytic astrocytomas, the tumor most closely mimicked by posterior pituitary tissue, the neurohypophysis contains large numbers of axons terminating on vessels. Of these axons, some possess PAS-positive swellings (Herring bodies). Secondary involvement of the pituitary by more ordinary diffuse astrocytomas is exceedingly rare.
References
1. Moore KL. The Developing Human: Clinically Oriented Embryology. Philadelphia: WB Saunders; 1988:170 205.
2. Conklin JL. The development of the human fetal adenohypophysis. Anat Rec 1968;160:79 91.
3. Sabshin JK. The pituitary gland anatomy and embryology. In: Goodrich I, Lee KJ, eds. The Pituitary: Clinical Aspects of Normal and Abnormal Function. Amsterdam: Elsevier Science; 1987:19 27.
4. Falin LI. The development of human hypophysis and differentiation of cells of its anterior lobe during embryonic life. Acta Anat (Basel) 1961;44:188 205.
5. Boyd JD. Observations on the human pharyngeal hypophysis. J Endocrinol 1956;14:66 77.
6. McGrath P. Aspects of the human pharyngeal hypophysis in normal and anencephalic fetuses and neonates and their possible significance in the mechanism of its control. J Anat 1978;127:65 81.
7. Asa SL, Kovacs K. Functional morphology of the human fetal pituitary. Pathol Annu 1984;19:275 315.
8. Colohan AR, Grady MS, Bonnin JM, Thorner MO, Kovacs K, Jane JA. Ectopic pituitary gland simulating a suprasellar tumor. Neurosurgery 1987;20:43 48.
9. Lennox B, Russell DS. Dystopia of the neurohypophysis: two cases. J Pathol Bacteriol 1951;63:485 490.
10. Scully KM, Rosenfeld MG. Pituitary development: regulatory codes in mammalian organogenesis. Science 2002;295:2231 2235.
11. Osamura RY, Egashira N. Recent developments in molecular embryogenesis and molecular biology of the pituitary. In: Lloyd RV, ed. Endocrine Pathology: Differential Diagnosis and Molecular Advances. Totowa, NJ: Humana Press, Inc; 2004:75 86.
12. Asa SL, Ezzat S. Molecular basis of pituitary development and cytogenesis. In: Kontogeorgos G, Kovacs K, eds. Molecular Pathology of the Pituitary. Frontiers of Hormone Research. Vol 32. Basel, Switzerland: Karger; 2004:1 19.
13. Dubois PM, Begeot M, Dubois MP, Herbert DC. Immunocytological localization of LH, FSH, TSH and their subunits in the pituitary of normal and anencephalic human fetuses. Cell Tissue Res 1978;191:249 265.
P.344
14. Begeot M, Dubois MP, Dubois, PM. Growth hormone and ACTH in the pituitary of normal and anencephalic human fetuses: immunocytochemical evidence for hypothalamic influences during development. Neuroendocrinology 1977;24:208 220.
15. Renn WH, Rhoton AL Jr. Microsurgical anatomy of the sellar region. J Neurosurg 1975;43:288 298.
16. Lang J. Anatomy of the midline. Acta Neurochir Suppl (Wien) 1985;35:6 22.
17. Osteology. In: Williams PL, Warwick R, eds. Gray's anatomy. 36th ed. Philadelphia: WB Saunders; 1980:230 418.
18. Kern EB, Laws ER Jr. The rationale and techniques of selective transsphenoidal microsurgery for the removal of pituitary tumors. In: Laws ER Jr, Randall RV, Kern EB, Abboud CF, eds. Management of Pituitary Adenomas and Related Lesions with Emphasis on Transsphenoidal Microsurgery. New York: Appleton-Century-Crofts; 1982:219 233.
19. Bergland RM, Ray BS, Torack RM. Anatomical variations in the pituitary gland and adjacent structures in 225 human autopsy cases. J Neurosurg 1968;28:93 99.
20. Berke JP, Buxton LF, Kokmen E. The empty sella. Neurology 1975;25:1137 1143.
21. Kaufman B, Chamberlain WB Jr. The ubiquitous empty sella turcica. Acta Radiol 1972;13:413 425.
22. Kaplan HA, Browder J, Krieger AJ. Intercavernous connections of the cavernous sinuses. The superior and inferior circular sinuses. J Neurosurg 1976;45:166 168.
23. McGrath P. The cavernous sinus: an anatomical survey. Aust N Z J Surg 1977;47:601 613.
24. Harris FS, Rhoton AL. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg 1976;45:169 180.
25. Stanfield JP. The blood supply of the human pituitary gland. J Anat 1960;94:257 273.
26. Xuereb GP, Prichard MM, Daniel PM. The arterial supply and venous drainage of the human hypophysis cerebri. Q J Exp Physiol Cogn Med Sci 1954;39:199 217.
27. Gorczyca W, Hardy J. Arterial supply of the human anterior pituitary gland. Neurosurgery 1987;20:369 378.
28. Xuereb GP, Prichard MM, Daniel PM. The hypophyseal portal system of vessels in man. Q J Exp Physiol 1954;39:219 230.
29. Scheithauer BW. The hypothalamus and neurohypophysis. In: Kovacs K, Asa SL (eds). Functional Endocrine Pathology. Boston: Blackwell; 1991:170 224.
30. Pansky B, Allen DJ. Review of Neuroscience. New York: Macmillan; 1980.
31. Brownstein MJ, Russell JT, Gainer H. Synthesis, transport, and release of posterior pituitary hormones. Science 1980;207:373 378.
32. Thorner MO, Vance ML, Laws ER Jr, Horvath E, Kovacs K. The anterior pituitary. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR, eds. Williams Textbook of Endocrinology. 9th ed. Philadelphia: WB Saunders; 1998:249 340.
33. Scheithauer BW, Sano T, Kovacs KT, Young WF Jr, Ryan N, Randall RV. The pituitary gland in pregnancy: a clinicopathologic and immunohistochemical study of 69 cases. Mayo Clin Proc 1990;65:461 474.
34. Goluboff LG, Ezrin C. Effect of pregnancy on the somatotroph and the prolactin cell of the human adenohypophysis. J Clin Endocrinol Metab 1969;29:1533 1538.
35. Ciric I. On the origin and nature of the pituitary gland capsule. J Neurosurg 1977;46:596 600.
36. Kovacs K, Horvath E. Tumors of the Pituitary Gland. Washington, DC: Armed Forces Institute of Pathology; 1986.
37. McGrath P. Cysts of sellar and pharyngeal hypophyses. Pathology 1971;3:123 131.
38. Mulchahey JJ, Jaffe RB. Detection of a potential progenitor cell in the human fetal pituitary that secretes both growth hormone and prolactin. J Clin Endocrinol Metab 1988;66:24 32.
39. Turkington RW, Underwood LE, Van Wyk JJ. Elevated serum prolactin levels after pituitary-stalk section in man. N Engl J Med 1971;285:707 710.
40. Horvath E, Ilse G, Kovacs K. Enigmatic bodies in human corticotroph cells. Acta Anat (Basel) 1977;98:427 433.
41. Phifer RF, Spicer SS. Immunohistochemical and histologic demonstration of thyrotropic cells of the human adenohypophysis. J Clin Endocrinol Metab 1973;36:1210 1221.
42. Phifer RF, Midgley AR, Spicer SS. Immunohistologic and histologic evidence that FSH and LH are present in the same cell type in the human pars tuberalis. J Clin Endocrinol Metab 1973;36:125 141.
43. Muttukrishna S, Tannetta D, Groome N, Sargent I. Activin and follistatin in female reproduction. Mol Cell Endocrinol 2004;225:45 56.
44. Asa SL, Kovacs K, Bilbao JM. The pars tuberalis of the human pituitary. A histologic, immunohistochemical, ultrastructural and immunoelectron microscopic analysis. Virchows Arch A Pathol Anat Histopathol 1983;399:49 59.
45. Horvath E, Kovacs K, Penz G, Ezrin C. Origin, possible function and fate of follicular cells in the anterior lobe of the human pituitary. Am J Pathol 1974;77:199 212.
46. Marin F, Stefaneanu L, Kovacs K. Folliculo-stellate cells of the pituitary. Endocr Pathol 1991;2:180 192.
47. Horvath E, Kovacs K. Folliculo-stellate cells of the human pituitary: a type of adult stem cell? Ultrastruct Pathol 2002;26:219 28.
48. Inoue K, Mogi C, Ogawa S, Tomida M, Miyai S. Are folliculo-stellate cells in the anterior pituitary gland supportive cells or organ-specific stem cells? Arch Physiol Biochem 2002;110:50 53.
49. Luse SA, Kernohan JW. Squamous-cell nests of the pituitary gland. Cancer 1955;8:623 628.
50. Schochet SS Jr, McCormick WF, Halmi NS. Salivary gland rests in the human pituitary. Light and electron microscopical study. Arch Pathol 1974;98:193 200.
51. Shanklin WM. Age changes in the histology of the human pituitary. Acta Anat (Basel) 1953;19:290 304.
52. Sano T, Kovacs KT, Scheithauer BW, Young WF Jr. Aging and the human pituitary gland. Mayo Clin Proc 1993; 68:971 977.
53. Scheithauer BW, Sano T, Kovacs KT, Young WF Jr, Ryan N, Randall RV. The pituitary gland in pregnancy: a clinicopathologic and immunohistochemical study of 69 cases. Mayo Clin Proc 1990;65:461 474.
54. Stefaneanu L, Kovacs K, Lloyd RV, et al. Pituitary lactotrophs and somatotrophs in pregnancy: a correlative in situ hybridization and immunocytochemical study. Virchows Arch B Cell Pathol Incl Mol Pathol 1992;62:291 296.
55. Frawley LS, Boockfor FR. Mammosomatotropes: presence and functions in normal and neoplastic pituitary tissue. Endocr Rev 1991;12:337 355.
56. Calderon L, Ryan N, Kovacs K. Human pituitary growth hormone cells in old age. Gerontology 1978;24:441 447.
57. Kovacs K, Ryan N, Horvath E, Penz G, Ezrin C. Prolactin cells of the human pituitary gland in old age. J Gerontol 1977;32:534 540.
58. R cken C, Saeger W, Fleege JC, Linke RP. Interstitial amyloid deposits in the pituitary gland. Morphometry, immunohistology, and correlation to diseases. Arch Pathol Lab Med 1995;119:1055 1060.
59. Takei Y, Seyama S, Pearl GS, Tindall GT. Ultrastructural study of the human neurohypophysis. II. Cellular elements of neural parenchyma, the pituicytes. Cell Tissue Res 1980;205:273 287.
60. Hatton GI. Pituicytes, glia, and control of terminal secretion. J Exp Biol 1988;139:67 79.
61. Seyama S, Pearl GS, Takei Y. Ultrastructural study of the human neurohypophysis. I. Neurosecretory axons and their dilatations in the pars nervosa. Cell Tissue Res 1980;205:253 271.
62. Seyama S, Pearl GS, Takei Y. Ultrastructural study of the human neurohypophysis. III. Vascular and perivascular structures. Cell Tissue Res 1980;206:291 302.
63. Luse SA, Kernohan JW. Granular-cell tumors of the stalk and posterior lobe of the pituitary gland. Cancer 1955;8:616 622.
64. Lopes MBS, Scheithauer BW, Saeger W. Granular cell tumour. In: DeLellis RA, Lloyd RV, Heitz PU, Eng C, eds. World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of Endocrine Organs. Lyon: IARC Press; 2004:44 45.
65. Nishioka H. Immunohistochemical study of granular cell tumors and granular pituicytes of the neurohypophysis. Endocr Pathol 1993;4:140 145.
66. Shanklin WM. Lymphocytes and lymphoid tissue in the human pituitary. Anat Rec 1951;111:177 191.
- ERP System Acquisition: A Process Model and Results From an Austrian Survey
- Distributed Data Warehouse for Geo-spatial Services
- Intrinsic and Contextual Data Quality: The Effect of Media and Personal Involvement
- Healthcare Information: From Administrative to Practice Databases
- Development of Interactive Web Sites to Enhance Police/Community Relations