3 - Alcohol and Stroke
Editors: Norris, John W.; Hachinski, Vladimir
Title: Stroke Prevention, 1st Edition
Copyright 2001 Oxford University Press
> Table of Contents > I - Primary Prevention > 3 - Alcohol and Stroke
function show_scrollbar() {}
3
Alcohol and Stroke
Jean-Marc Orgogozo
Serge Renaud
The mortality rate from coronary heart disease (CHD) and stroke has declined consistently since the 1970s in most industrialized countries.1,2,3 In the former socialist economies of eastern Europe, such as Bulgaria, Hungary, Czechoslovakia, Poland, and Russia, the death rate from both causes increased during same period. This concordance of trends for these two diseases suggests common causes that may be sensitive to the same preventive measures. The most important of these measures include careful control arterial hypertension, avoidance of smoking, and proper diet. The MONICA project of WHO, with more than 40 centers in 20 countries, has produced data on mortality and risk factors for both CHD and stroke4 revealing a significant correlation between cerebrovascular and CHD mortality (Fig. 3.1). These findings raise the questions of which intrinsic factors are common to CHD and stroke and which factors represent environmental influences that can be modified, such as the effects of alcohol.
Dietary habits, with their marked geographical and cultural diversity among ethnic groups, are among the most important influences. Alcohol and wine consumption may have the greatest impact on stroke risk, both positively and negatively. The effects of moderate alcohol consumption on the risk of stroke are still debated, but strong evidence exists for a protective effect on stroke of mild to moderate consumption, particularly of wine. However, the risk of cerebral hemorrhage increased markedly with the consumption of alcoholic beverages.5,6
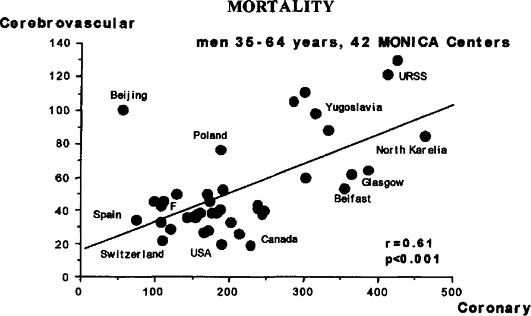 |
FIGURE 3.1. Relationship between cerebrovascular and coronary heart disease mortality in 42 MONICA centres. Adapted from WHO, World Health Statistics, 1989 (1994). |
P.44
Relation Between Alcohol Consumption and Cardiovascular Mortality
Earlier studies of this relationship focused on deaths from ischemic heart disease, where the results favored a protective effect of moderate alcohol consumption.7,8,9,10,11,12,13 A similar protective effect was later found for global mortality.14,15,16,17 But some of the cohort studies found an increase in overall mortality proportional to alcohol consumption18,19 beginning at rather low levels of consumption. These correlations tended to disappear after adjustment for major vascular risk factors (e.g., age, smoking, hypertension, hypercholesterolemia). Hypertension is induced by regular alcohol consumption,20 but if separated from the rest of the analysis, the adverse relationship between alcohol and cardiovascular risk disappears, suggesting that alcohol-induced hypertension is the main determinant.21
Stroke mortality has been less well studied and was often included in global cardiovascular mortality. The first study specifically to address stroke mortality was one of ecologic epidemiology carried out by Saint-Leger and Cochrane in 1979.22 They found a trend toward reduction of stroke mortality and a very significant reduction of cardiac mortality relating to wine consumption in the 18 countries they surveyed. The highly publicized paper by Renaud and de Lorgeril in 199223 on the French Paradox, based an ecologic survey of coronary heart disease mortality (but not specifically stroke) in 17 countries supported the finding that wine drinking exerts a dose-dependant protective effect on risk of stroke and CHD. These results were confirmed in a survey of 21 countries by Criqui
P.45
and Ringel in 1994,24 but the lower cardiovascular mortality associated with alcohol drinking, particularly wine, was partly counter-balanced by a proportional increase in the rate of fatal liver cirrhosis. Moreover, the only country with a lower CHD mortality than France was Japan, where the average wine consumption was extremely low at that time, a sort of Japanese Paradox. Because ecologic epidemiology studies are sensitive to major confounders, they must be interpreted with caution.
The first large prospective study on alcohol drinking and mortality from various causes (Fig. 3.2)15 found that alcohol consumption in the range of lOg per day decreased the risk of cerebrovascular mortality by approximately 20%, much less than for cardiovascular mortality. However, at a consumption of more than 25g of alcohol per day, the risk increased steadily, up to 50% 60%. The pattern of cerebrovascular response to alcohol drinking was very similar that of mortality from all causes, that is, a J-shaped curve, while mortality CHD continued to decrease with increasing amounts of alcohol, up to a certain threshold.25 This upper limit was about 6 glasses a day in a study of 13,000 elderly male British physicians17 and 2 glasses a day for women 6 men in the 490,000 subjects enrolled in the Cancer Prevention Study II.26 Shanghai,
P.46
total mortality was reduced by 19% in 18,244 middle-aged men who consumed 1 to 14 drinks a week,27 while those who consumed up to 28 per week had a 36% reduction in CHD mortality. However, no of stroke mortality was found at any level of alcohol consumption in this study.
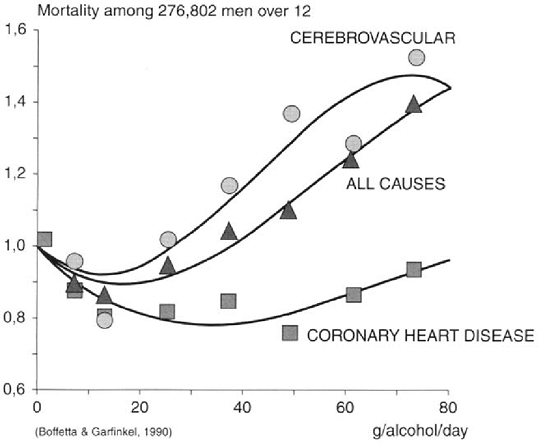 |
FIGURE 3.2. Mortality for cerebrovascular, coronary heart disease, and all causes in relation to the consumption of alcohol. Adapted from Boffetta and Garfinkel (1990). |
In the Copenhagen Heart Study,28 a follow-up for 10 12 years of 13,285 subjected aged 30 to 70 years showed that the incidence of cardiovascular mortality was reduced in proportion to the daily average consumption of wine, up to 3 5 glasses a day (RR = 0.51; 95% CI = 0.32 0.81), while no change in mortality was found in beer drinkers and an increased incidence at more than 2 glasses of spirits a day (RR = 1.34; 95% CI = 1.05 1.71). This study was the first to make a direct comparison of the effects moderate wine consumption to that of beer and spirits. Earlier, Klatsky Armstrong29 had also shown some possible advantage of wine drinking against CHD mortality in the more then 123,000 subjects of the Kaiser Permanente study and later confirmed this finding for patients hospitalized CHD.30 Other studies showed the same protective effects for beer and spirits as for wine,31 so that alcohol itself perhaps explains most of the protective role against CHD.
In an analysis of 30,014 men who volunteered for a health appraisal in Nancy, France, and were followed for 10 15 years,32 a moderate intake of wine (2 5 glasses a day) was associated with 24 30% reduction in all causes of death (RR = 0.70; 95% CI = 0.59 0.52 for 22 32g of alcohol per day; RR = 0.76; 95% CI = 0.66 0.87 for 33 54g/day). Heavy drinkers (more than 126g/day) had increased mortality compared to nondrinkers (RR = 1.37; 95% CI = 1.16 1.61).
Wine contains polyphenolic compounds, particularly flavonoids, gallic acid, and resveratrol, which may prevent ischemic cardiovascular diseases mainly through their antioxidant and antiaggregant properties.33,34,35,36,37 This may explain the apparent superiority of wine drinking for cardiovascular protection in some studies, but healthier life styles in wine drinkers may explain at least part of this difference.38 Binge drinking of beer increases the risk of fatal myocardial infarction.39
In summary, moderate consumption of alcoholic beverages is associated with a 20% 60% reduction in the risk of myocardial infarction and death. This was also observed after myocardial infarction in 5539 participants to the Physicians' Health Study,40 and even recent consumption seems to have a protective effect.41 Both these findings suggest that moderate alcohol consumption plays a role in the secondary prevention of large artery atherosclerotic disease.
Relation Between Drinking Habits and the Risk of Stroke
A number of studies have addressed specifically the relationship between alcohol (or wine) consumption and stroke. Early studies reported no association.42,43 Accumulating evidence, however, suggests a global beneficial effect of moderate
P.47
alcohol consumption against stroke, but the results are less impressive and less consistent than for ischemic heart disease. This might be due to the fact that fewer studies, with less subjects and less events per subjects, have addressed this point, thus yielding lower statistical power. Also, stroke is far less homogenous than myocardial infarction; in addition to the main dichotomy between ischemic and hemorrhagic strokes, ischemic strokes have subtypes that are possibly different in their response to alcohol. Also, stroke tends occur much later life than CHD, at an age at which the risk factors for atherosclerosis are no longer the same as for CHD.
Compared to studies of stroke mortality alone, studies and morbidity are more informative because they help discriminate the different mechanisms of stroke and often allowed a more precise estimate average alcohol consumption. In 198944 Camargo surveyed 62 studies published in English, and several others have been published since then, most to be found in the thorough reviews by Van Gijn et al. 199345 and Camargo in 1996.46 The main studies are summarized below and/or presented in Tables 3.1 and 3.2.
TABLE 3.1. Relative Risks (or odds ratios OR) of Stroke According to Alcohol Consumption in Epidemiology Studies; Case Control Studies, 1994 1999 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 3.2. Relative Risk of Stroke (or Odds Ratios) of Stroke According to Alcoholic Consumption in Epidemiology Studies; Prospective Cohort Studies, 1986 1997 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
P.48
P.49
The first case control studies, published in the 1980's, showed either a moderate increase in the risk of all strokes or no change stroke risk associated with moderate alcohol consumption. For example, Herman et al.47 analyzed the risk according to the level of alcohol intake and found no different between drinkers and nondrinkers at any lever.
Gill et al.48,49 performed two studies based on the same 230 patients hospitalized consecutively for stroke, with 230 controls in the first study and 577 controls in the second, relating recent alcohol consumption and biological markers of chronic alcohol abuse with the occurrence of stroke. In the first comparison the controls were hospitalized in a surgery ward; they were randomized from a cohort of workers in the second. A standardized questionnaire was used to quantify alcohol consumption during the preceding months. After adjustment for high blood pressure, smoking, and anticoagulant treatment, the risk of stroke was halved (expressed as the odds ratio: OR = 0.5) in moderate drinkers (10 90g of alcohol a week) and increased (4-fold in the first study 2-fold second)
P.50
in heavy drinkers (more than 300g of alcohol a week). The ascending part this J-shape curve was parallel to the levels of main seric markers heavy alcohol consumption but not to the mean red cell volume. These results were valid only for men, the number of women being too low in both studies. Unfortunately, only 20% of the cases had a computed tomography scan. A later study50 found opposite differences in relative risk of stroke above 300g alcohol/week if the controls were medical patients (RR = 0.73) or people in the community = 1.93), but none of the correlations was significant. This set of studies is quoted mainly to exemplify the sensitivity of case control studies to the choice controls: the resulting instability of results should be kept in mind for their interpretation.
Another interesting case control study51 was based on 156 men less than 61 years of age admitted consecutively for an acute ischemic stroke, compared with 153 matched controls. Heavy drinking, defined as more than 300g of pure alcohol per week, was associated with a 4.45 higher relative risk of stroke compared to nondrinkers, with a large confidence interval (95% CI = 1.09 18.1). In light drinkers (up to 150 g/week) the risk, as assessed through odds ratio, was reduced by about half but also with a confidence interval that included unity (OR = 0.54; 95% CI = 0.28 1.05). No change in risk was found among moderate drinkers (150 300g/week). Due to the small sample size, these results would not have added much to already existing knowledge, except that on comparing regular drinkers (i.e., at least a drink 4 to 7 days week) to irregular drinkers (i.e., 3 days a week or less), much stronger negative association was found between light drinking and stroke in regular drinkers (OR = 0.12; 95% CI = 0.02 0.65) and a possible protection in moderate regular drinkers (OR = 055; NS), while intermittent drinking yielded no benefit.
Rodgers et al.52 studied 364 cases of acute stroke compared with community-based control subjects. The odds ratio for the risk of stroke lifelong abstainers compared with subjects who had ever drunk regularly, particularly women (but not current heavy drinkers) was 2.36 (95% CI = 1.67 3.37). No relation was found between stroke and current nondrinkers (i.e., ex-drinkers). Hence, regular moderate drinking seems to be the most protective behavior.
A nested case control study was conducted on a population-based registry by Jamrozik et al.53 in Australia. Of 536 strokes, each was matched for age and sex with up to 5 controls from the same geographic area. The usual drinking habits of the subjects were estimated from reported consumption during preceding week. With univariate analysis, the main finding was a significantly lower incidence of all strokes (OR = 0.43; 05% CI = 0.32 0.58), ischemic strokes, and of primary hemorrhage strokes associated with a consumption of l-20g alcohol per day during the previous week. Average consumptions of 21 40 and 41 60g per day were also associated with an apparent less marked risk reduction (OR = 0.67 and 0.55, respectively, NS), while consumption of more than
P.51
60g per day was associated with a 2.51 increase in risk of all strokes (95% CI = 1.33 4.74), rising to 6.71 (95% CI 1.68 26.8) for first-ever strokes and to 5.88 (95% CI = 1.19 29.1) for cerebral hemorrhage (Table 1).
In Spain, Caicoya et al.54 performed a careful analysis of risk factors in a consecutive series of strokes. Despite its relatively small size (cases = 467, controls = 477), this was the first study on alcohol to analyse separately cortical versus deep strokes and to find a similar pattern of correlation for the two categories. This suggests that an effect on large artery atherosclerosis may not be in the main determinant of the observed protection. This study was also one of the few to find a lower risk of hemorrhagic strokes associated with mild to moderate alcohol consumption (Table 3.1).
The latest, and so far the largest, case control study was conducted in northern Manhattan55 on 667 cases of ischemic stroke in men and women various ethnic groups compared with 1139 matched community controls. The results showed that an average consumption of up to 2 drinks a day, and even 3 to 4 drinks a day of any alcoholic beverage, was associated with significantly lower risk of ischemic stroke after adjustment for cardiac disease, hypertension, diabetes, current smoking, body mass index, and education (Table 3.1). This effect was observed in both sexes, at all ages, and in all ethnic groups. At excessive levels of consumption (7 or more drinks/day) there was an apparent increased risk.
Some earlier and smaller anecdotal series of case control studies6,56,57 suggested an increased risk of hemorrhagic stroke with heavy alcohol consumption (acute or chronic), which might explain at least part of the net increase in stroke risk observed in alcohol abusers some early studies. Studies on case series of binge drinking indicated that this behavior is associated with an increased risk of ischemic stroke, in particular the next morning. 58,59,60,61 This has not been verified in formal epidemiology studies so far.62 In young subjects, the risk is increased by a concomitant consumption of cigarettes.61 Hypercoagulability induced by high blood alcohol content56 or a rebound of hypercoagulability at withdrawal after temporary drinking63 could explain this pattern of stroke occurrence, as well cardiac sudden deaths in the same context.64
More important from the point of view possible causality are the prospective epidemiologic cohort studies, which are less susceptible to biases and yield, in general, more reliable estimates of the correlations than case control studies. They therefore produce more convincing evidence of an association between drinking patterns and stroke, even if this evidence remains observational. A number of such studies reported results for all strokes. Among those controlling confounding factors,65,66,67,68 all found an elevated relative risk in the highest alcohol consumption categories, but the upper limits were open-ended in these studies, and no consistent definition of heavy drinking was established. So it is
P.52
possible that the observed modest increase of risk for all stroke was due entirely to the excessive drinkers, who are at particular risk of cerebral hemorrhage. This was confirmed in most studies that separately analyzed ischemic and hemorrhagic strokes (Tables 3.2 and 3.3).
The Honolulu Heart Program69 followed for 12 years a cohort of 8006 men of Japanese ancestry. Alcohol consumption was recorded at baseline and classified in four categories: none, mild (10 390g/month), moderate (420 1090g/month), and heavy (more than 1 lOOg/month). The diagnosis of ischemic stroke was made clinically, but when there was suspicion of hemorrhage, radiologic examinations were made. Globally, no significant relation was found between alcohol consumption and ischemic strokes, but the relative risk of hemorrhagic stroke was 2.2 in mild drinkers, 2.9 in moderate drinkers, and 4.7 in heavy drinkers, compared
P.53
to nondrinkers. This increase of hemorrhagic risk was larger for subarachnoid hemorrhages (RR = 5.8) than for intracerebral hemorrhages = 3.9). After adjustment, the authors concluded that these results were independent of high blood pressure, suggesting that a direct and causal relation existed between alcohol consumption and the risk of intracranial hemorrhage. Another analysis was performed later70 on the 2946 men who were not lost at the end of 1988 and had reported a stable alcohol intake during the periods 1965 to 1968 and 1971 to 1974. A trend was found for lower rate of occurrence fatal and nonfatal coronary heart disease with increasing alcohol consumption in all age subgroups but, differing from most previously published data, an insignificant but almost linear trend was found for higher risk of stroke events with increasing alcohol consumption in middle aged (51 64-year-old) men and a similar higher risk trend for light (l-14ml alcohol/day) and moderate (15 39ml/day) drinkers in elderly men (65 years and older). This was not found heavy drinkers (40ml/day and more). In all subgroups, the numbers of subjects events were small.
TABLE 3.3. Relative Risk of Stroke (or Odds Ratios) of Stroke According to Alcohol Consumption in Prospective Epidemiology Studies in Asians | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In the Nurses Health Study, Stampfer et al.67 analyzed data on 85,526 nurses aged 34 59, who were followed for four years. Their weekly alcohol consumption was recorded initially through a self-questionnaire of main dietary habits that had been earlier validated in a sample of 170 nurses. Even though only 66 ischemic and 28 hemorrhagic strokes occurred during the follow-up, statistical calculations, with adjustment for vascular risk factors such as smoking, hypertension, age, and diabetes, showed that the risk of ischemic stroke was reduced by f by mild alcohol consumption (between 5 and 14g/day) and halved by moderate consumption (15g or more/day). By contrast, the risk of meningeal hemorrhage was fourfold higher in the moderate drinkers, but overall a lower risk of all strokes was associated with moderate consumption (Table 3.2) since hemorrhagic strokes are much rarer than ischemic strokes in this age group.
This effect may not be present in all countries. Researchers Japan found no reduction of stroke incidence in beer and spirit drinkers at any level consumption.71 In this study, stroke risk increased at any level of consumption in hypertensive patients, mainly due to an excess of cerebral hemorrhage.
In the first Copenhagen Heart Study,72 an analysis was made of first stroke occurrence during 12 years of follow-up 12,971 subjects aged 35 and over in whom life-style risk factors had been recorded initially. A tendency was found for daily moderate to heavy . alcohol intake be associated with lower risk of stroke (OR = 0.86, NS), which was significant 0.79, 95% CI: 0.65 0.97) only in the subgroup of cigarette smokers, a group at much higher risk of stroke. With longer follow-up73 a reduction of stroke incidence was associated only with moderate wine consumption and not with beer or spirit consumption. In 13,329 subjects of both sexes aged 45 to 84 years followed for 16 years, 833 first-ever strokes occurred that were related to various known risk factors and to average
P.54
alcohol consumption. The reduction of stroke incidence was 33% to 41%, depending on the adjustments, in weekly wine drinkers and slightly less daily wine drinkers (Table 3.2). Further studies in Europe have confirmed this lower risk of stroke in moderate drinkers but these studies did not discriminate between wine and other drinkers.74,75
The results of both case control and prospective epidemiologic studies can be summarized as follows: the risk of hemorrhagic stroke increases at least linearly, and possibly exponentially, as a function of alcohol consumption, independently of high blood pressure (which itself can be induced by chronic alcoholism). The relation between alcohol consumption and ischemic stroke is more complex: mild to moderate consumption is associated with a definite risk reduction in most studies, but heavy consumption is either associated with no change or with an increased risk (quadratic effect). This differs from myocardial infarction studies, in which the risk reduction is proportional to the daily amount ingested, including at levels qualifying as unsafe drinking and alcoholism.29
A likely explanation for the J- (or U-) shaped curve relationship between alcohol consumption and all strokes is that mild to moderate consumption decreases the risk of ischemic stroke without increasing the risk of cerebral hemorrhage, while at higher levels of consumption alcohol induced hemorrhages outnumber the ischemic strokes prevented. In other words, the risk/benefit balance is positive for light to moderate levels of consumption and becomes negative at a point above which the total number of strokes increases. What is not precisely known is the optimal level of consumption, at which net risk reduction is maximum ( healthy drinking ). It is estimated to be between 1 and 4 glasses a day, and the point above which risk increases (the limit of safe drinking ) is estimated to be between 3 and 6 standard glasses a day. Because some alcohol-induced pathologies, such as liver cirrhosis76 and digestive tract cancer, can be increased above a consumption of 3 standard glasses a day,77 it is important to carefully weigh recommendations about what exactly are healthy and safe drinking. It may appear to vary in different countries because the definitions of standard units also differ (Table 3.4).
In the cohort of elderly British male doctors,12 mortality from all causes and from ischemic heart disease were minimal at daily consumption of 2 and 3 standard glasses a day, respectively. An increase of alcohol deaths was observed above 4 glasses a day and an increase of deaths from all causes well above 6 day. This cohort comprised over 12,000 long-term survivors out of about 40,000 men recruited in their early 50's, and initially enrolled to assess the hazards of cigarette smoking. The age range was 60 to 90 years; in men of this age group the main cause of mortality is cardiovascular, and censoring age groups below 60 largely eliminates most types of alcohol related mortality.
In young male military recruits in Sweden,78 a linear increase was found death rates from all causes (mostly accidents, violence, and suicide) with increasing alcohol consumption. In the Cancer Prevention Study II,26 in which subjects
P.55
were enrolled from age 30 and above, a 30% increase of breast cancer was found during the 9 years of follow-up in women having at least one drink daily (RR = 1.3, 95% CI 1.1 1.6). However, mild alcohol consumption was globally associated with a substantial reduction in deaths due to all cardiovascular diseases and with a small reduction in overall mortality middle-aged men and women. Mortality from all causes increased in heavy drinkers, particularly those below 60 years of age without cardiovascular risk factors. In the middleaged men of the Nancy study,32 an increased risk of mortality (+37%) appeared only above an average consumption of 128g per day (10 French glasses), with a majority wine drinkers (70%). More direct evidence in favor of came from a study in Denmark79 which wine drinkers tended to have less cancers of the upper digestive tract, while even a moderate intake of beer or spirits increased this risk considerably.
TABLE 3.4. Correspondance Between Standard Units (Drinks or Glasses) and Amount of Pure Alcohol in Various Countries | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
By and large, almost all studies reporting potential benefits of moderate alcohol consumption on health and mortality indicate that these benefits are restricted to older subjects and that they increase with increasing age, at least in established market economies.80 This should be viewed in conjunction with the recent observation that in people above 65 years of age, regular consumption 3 to 4 glasses of wine a day is also associated with marked reduction in the incidence of dementia and Alzheimer's disease.81,82
Mechanisms of the Effects Alcohol and Wine on Stroke
For a biological explanation of the effects alcohol on atherosclerosis and on the hemostatic system that is relevant to the pathophysiology of various types of ischemic and hemorrhagic stroke, the following observations have been made:83
P.56
A significant relationship exists between alcohol consumption and seric levels of HDL2 cholesterol, the main protective type against atherosclerosis, and also HDL3;1,84,85,86,87,88 in addition, ethanol decreases the level of LDL cholesterol ( bad cholesterol) when it is high.89,9091 This has been questioned in other studies.92,93
Ethanol stimulates liver microsomial oxidases, hence increasing synthesis of apolipoproteins Al and A2, which contribute to the HDL levels.94,95
Ethanol has an antiplatelet effect, as evidenced by in vitro studies96,97,98,99,100,101 and by a significant prolongation of bleeding time in volunteers.102 The antiplatelet effect of alcohol is correlated with its protective against CHD.23 However, this effect is only short lasting, and a rebound of platelet activation occurs one or two hours after an acute ingestion of alcohol103 and after withdrawal in chronic alcoholics.63 This rebound effect could be due to an increase in lipidic perodixides.104 In vitro, ethanol enhances the antiaggregating effect of both aspirin and prostacyclin in a dose-dependent manner.105,106,107 In vivo, it potentiates the prolongation of bleeding time induced by aspirin.108 In human studies, a relation was found between reported alcohol consumption and an increased fibronolytic activity in plasma,109,110,111,112 with plasma t-PA production113,114 a major factor of fibrinolytic in vivo, and also with urokinase-like plasminogen activator.115
Possible explanations for the difference between the effect of wine and of other alcoholic beverages in relation to cerebrovascular mortality seem imply platelets. While an intake of alcohol is associated, within minutes, with a decrease in platelet aggregability, 97 it is followed hours later by a rebound effect, that is by an increased response of platelets to aggregation,63 especially after an episode of drunkenness,103 which can also be responsible for cardiac sudden death and ischemic stroke. It has been shown that the increased platelet aggregability following alcohol withdrawal is not observed after wine drinking, especially red wine.116 This protection could be due to the antioxidant effects of the tannins (polyphenols) contained in wine.
Conclusion
Although cerebrovascular diseases present similarities with CHD, the effect of alcohol and wine drinking does not appear to be identical on both conditions. One possible reason is that stroke tends to occur later in life than CHD, at a time when high cholesterol no longer increases vascular risk, which may reduce the preventive effects of alcohol and wine on stroke due to large artery atherosclerosis. But the main difference is probably due to the opposite effects of alcohol on ischemic and hemorrhagic stroke. The risk reduction of stroke associated with mild to moderate consumption, particularly of wine, appears similar
P.57
to that found for myocardial infarction. On the contrary, the risk of intracranial hemorrhage increases linearly, and possibly exponentially, in proportion to average alcohol consumption. This observation is consistent with the antithrombotic effects of alcohol, which may be beneficial at low doses but are definitely harmful at high doses. The apparent risk reduction of ischemic stroke observed in most prospective epidemiologic studies of healthy subjects (Table 3.2) is larger than that demonstrated with any antiplatelet drug in trials of secondary prevention,117 and no antiplatelet has ever worked in primary prevention. The very impressive relative stroke risk of 0.2 (an 80% reduction!) observed in moderate drinkers versus nondrinkers in the SPAFI-III trials for patients with atrial fibrillation receiving aspirin for primary prevention2 corresponds to a larger risk reduction than that achieved with anticoagulants in interventional studies.
A notable exception to these favorable observations concerns Asians, in whom all studies have failed to show a reduced incidence of stroke mortality in moderate drinkers in Japan65 and China27 in overall strokes Honolulu,69,70 Japan,71 and Taiwan.118 Instead, most of these studies reported an increased risk of stroke at high levels of consumption (Table 3.3), confirming earlier findings from Japan.119-120 This may be due to the higher proportion of hemorrhagic strokes in Asians,27,121 to their know higher prevalence of relative deficiency the liver aldehyde dehydrogenase,122,123 a key enzyme for the degradation of alcohol, or to both. In addition, the consumption of grape wine in Japan and China was almost nil at the time of these studies.27,71 So recommendations in favor drinking alcohol or wine for health purposes in these populations may be particularly ill-advised.
Can it be concluded that moderate drinking is a valuable preventive measure against ischemic stroke, at least in Caucasians? The weight of evidence is certainly in favor of a true protective effect, but its real magnitude cannot be measured precisely or even estimated because of the observational, not experimental, nature of the available clinical evidence. Therefore, the influence confounders (biases) cannot be ruled out. In addition, the relation between alcohol and cardio vascular diseases is complex, and the following important issues remain to be investigated before any inference as to the prevention of ischemic stroke can be made:
The ratio between potential benefits and risks in younger subjects, especially women, at low risk of cardiovascular disease and even lower risk of ischemic stroke, but who may be at risk of intracranial hemorrhage, liver cirrhosis, and cancer and who may develop drinking problems.
The effects on subtypes of arterial vascular disease, e.g., large artery atherosclerosis124 versus lacunar infarctions due to arteriolosclerosis.54
Confirmation of the apparently more positive effects of wine drinking, particularly red wine, compared to other alcoholic beverages,73 which has been challenged.
The role of confounding socioeconomic,125 health behaviour,126 cultural, and dietary factors38 on this apparent protection.
P.58
For instance, a study in Denmark found that wine drinking was associated with healthier dietary habits,127 while, on the contrary, wine drinking was correlated with a high saturated fat diet in a study Spain.128 New analytical epidemiclogic studies of prospective cohorts, including women and younger age groups, and assessment of potential confounders in more detail are necessary to resolve these questions. Randomized trials of primary or secondary prevention by moderate alcohol or wine consumption, the ultimate proof, may prove difficult, but not impossible, to accomplish. However, the weight of the epidemiologic and experimental data, which identified credible mechanisms by which alcohol and some constituents of red wine can be protective against ischemic cardiovascular disease, are strongly suggestive of a potential protection against the common types of ischemic stroke. The time has not yet come to recommend moderate and regular alcohol consumption for the primary or secondary prevention of stroke, but sufficient evidence exists to advise responsible moderate drinkers in the middle-aged and elderly groups not to change their habits.81
References
1. Gaziano JM, During JE, Breslow JL, et al. Moderate alcohol intake, increased levels of high density lipoprotein and its subfractions, and decreased risk of myocardial infarction. New EnglJ Med 1993;329:1829 1834.
2. Hart RG, Pearce LA, McBride R, et al., on behalf of the Stroke Prevention in Atrial Fibrillation (SPAF) Investigators. Factors associated with ischemic stroke during aspirin therapy in atrial fibrillation: Analysis of 2012 participants the SPAF I-III clinical trials. Stroke 1999;30:1223 1229.
3. Thom TJ, Epstein FH. Heart disease, cancer and stroke mortality trends their interrelations. An international perspective. Circulation 1994;90:574 582.
4. World Health Organization. World Health Statistics Annual. Geneva: World Health Organization, 1994.
5. Weisberg LA. Alcoholic intracerebral hemorrhage. Stroke 1988;19:1565 1569.
6. Montforte R, Estruch Graus F. High ethanol consumption as risk factor of intracerebral hemorrhage in young and middle-aged people. Stroke 1990;21:1529 1532.
7. Stason WB, Neff RK, Miettinen OS, et al. Alcohol consumption nonfatal myocardial infarction. Am J Epidemiol 1976; 104:603 608.
8. Hennekens CH, Rosner B, Cole DS. Daily alcohol consumption and fatal coronary heart disease. Am J Epidemiol 1978;107:196 200.
9. Dyer AR, Stamler J, Paul O. Alcohol consumption and 17-year mortality in the Chicago Western Electric Company Study. Prev Med 1980;9:78 90.
10. Gordon T, Kannel WB. Drinking habits and cardiovascular disease: The Framingham Study. Am Heart J 1983;105:667 673.
11. Colditz GA, Branch LG, Lipnick RJ, et al. Moderate alcohol and decreased cardiovascular mortality in an elderly cohort. Am Heart J 1985; 109:886 889.
P.59
12. Friedman LA, Kimball AW. Coronary heart disease mortality and alcohol consumption in Framingham. Am J Epidemiol 1987;124:481 489.
13. Moore RD, Pearson TA. Moderate alcohol consumption and coronary artery disease: A review. Medicine 1986;65:242 267.
14. Poikolainen K. Alcohol and mortality: A review. Clin Epidemiol 1995;48:455 465.
15. Boffetta P, Garfinkel L. Alcohol drinking and mortality among men enrolled in an American Cancer Society prospective study. Epidemiology 1990; 1:342 348.
16. Klatsky AL, Armstrong MA, Friedman GD. Alcohol and mortality. Ann Intern Med 1992; 17:646 654.
17. Doll R, Peto Hall E, et al. Mortality in relation to consumption of alcohol: 13 years' observations on male British doctors. BMJ 1994;309:911 918.
18. Blackwelder WC, Yano K, Roads GG. Alcohol and mortality: The Honolulu Heart Study. Am J Med 1980;68:164 169.
19. Kozarevic DJ, Vojvodic N, Dawber T. Frequency of alcohol consumption and morbidity and mortality: The Yugoslavia Cardiovascular Disease Study. Lancet 1980; 1:613 616.
20. Witteman JCM, Willett WC, Stampfer MJ, et al. The relation of moderate alcohol consumption and increased risk of hypertension in women. Am J Cardiol 1990; 65:633 637.
21. Taylor JR, Coomes T, Anderson D, et al. Alcohol, hypertension and stroke. Alcohol Clin Exp Res 1984;3:283 286.
22. Saint-Leger AS, Cochrane AL, Moore W. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. Lancet 1979; 1:1017 1020.
23. Renaud S, De Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992;339:1523 1526.
24. Criqui MH, Ringel BL. Does diet or alcohol explain the French paradox? Lancet 1994;344:1719 1723.
25. Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 1991;338:464 468.
26. Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med 1997;337:1705 1714.
27. Yuan JM, Ross RK, Gao YT, et al. Follow up study of moderate alcohol intake and mortality among middle aged men in Shangai, China. BMJ 1997;314:18 23.
28. Gronbaeck M, Deis A, Sorensen TLA, et al. Mortality associated with moderate intakes of wine, beer or spirits, BMJ 1995;310:1165 1169.
29. Klatsky AL, Amstrong MA, Friedman GD. Relations of alcoholic beverage use to subsequent coronary artery disease hospitalization. Am J Cardiol 1986;58:710 714.
30. Klatsky AL. Red wine, white wine, liquor, beer and risk for coronary artery disease hospitalization. Am J Cardiol 1997;80:416 419.
31. Rimm EB, Klatsky A, Grobbee D, et al. Review of moderate alcohol consumption and reduced risk of coronary heart disease: Is the effect due to beer, wine or spirits. BMJ 1996;312:731 736.
32. Renaud SC, Gueguen R, Schenker J, et al. Alcohol and mortality in middle-aged men from eastern France. Epidemiology 1998;9(2):184 188.
33. Hertog MG, Feskens EJ, Hollman PC, et al. Dietary antioxidant flavonoids and risk of coronary heart disease. Lancet 1993;342:1007 1011.
34. Frankel EN, Kanner J, German JB, et al. Inhibition of oxidation human low-density lipoprotein by phenolic substances in red wine. Lancet 1993;341:454 457.
P.60
35. Frankel EN, Waterhouse AL, Kinsella JE. Inhibition of human LDL oxidation by resveratrol. Lancet 1993;341:1103 1104.
36. Pace-Asciak CR, Hahn S, Diamandis P, et al. The red wine phenolics trans-resveratrol and quercetin block human platelet aggregation eicosanoid synthesis: Implication for protection against coronary heart disease. Clin Chim Acta 1995;235: 207 219.
37. Teissedre PL, Frankel EN, Waterhouse AL, et al. Inhibition of in vitro human LDL oxidation by phenolic antioxidants from grapes and wines. Sci Food Chem 1996; 70:55 61.
38. Rimm EB. Alcohol consumption and coronary heart disease: Good habits may be more important than just good wine. Am J Epidemiol 1996;143:1094 1098.
39. Kauhanen J, Caplan GA, Goldberg DE, et al. Beer binging and mortality: Results from the Kuopio ischemic heart disease risk factor study, a prospective population based study. BMJ 1997;315:846 851.
40. Muntwyler J, Hennekens CH, Buring JE, et al. Mortality and light to moderate alcohol consumption after myocardial infarction. Lancet 1998;352:1882 1885.
41. Jackson R, Scragg Beaglehole R. Does recent alcohol consumption reduce the risk of acute myocardial infarction and coronary death in regular drinkers? Am J Epidemiol 1992;819 824.
42. Klatsky AL, Friedman GD, Siegelaub AB. Alcohol and mortality: A ten-year Kaiser Permanente experience. Ann Intern Med 1981;95:139 145.
43. Paganini-Hill A, Ross RK, Henderson BE. Postmenopausal oestrogen treatment and stroke: A prospective study. BMJ 1988;297:519 522.
44. Camargo CA. Moderate alcohol consumption and stroke: The epidemiologic evidence. Stroke 1989;20:1611 1626.
45. Van Gijn J, Stampfer MJ, Wolfe C, et al. The association between alcohol and stroke. In: Verschuren PM, ed. Health Issues Related to Alcohol Consumption. Ilsi Press, 1993:43 79.
46. Camargo CA. Case-control and cohort studies of moderate alcohol consumption and stroke. Clin Chim 1996;246:107 119.
47. Herman B, Shmitz PIM, Leyten ACM. Multivariate logistic analysis of risk factors for stroke in Tilburg, The Netherlands. Am J Epidemiol 1983; 18:514 525.
48. Gill JS, Zezulka V, Shipley MI, et al. Stroke and alcohol consumption. N Engl J Med 1986;315:1041 1046.
49. Gill JS, Shipley MJ, Gill SK, et al. A community case-control study of alcohol consumption in stroke. Int J Epidemiol 1988;3:542 547.
50. Ben-Shlomo Y, Markovwe H, Shipley M, et al. Stroke risk from alcohol consumption using different control groups. Stroke 1991;1093 1098.
51. Palomaki H, Kaste M. Regular light-to-moderate intake of alcohol and the risk of ischemic stroke: Is there a benefit? Stroke 1993;24:1828 1832.
52. Rodgers H, Aitken PD, French JM, et al. Alcohol and stroke: A case-control study of drinking habits past and present. Stroke 1993;24:1473 1477.
53. Jamrozik K, Phil D, Broadhurst J, et al. The role of lifestyle factors in the etiology of stroke: A population-based case-control study in Perth, Western Australia. Stroke 1994;25:51 59.
54. Caicoya M, Rodriguez T, Corrales C, et al. Alcohol and stroke: A community casecontrol study in Asturias, Spain. J Clin Epidemiol 1999;52:677 684.
55. Sacco RL, Elkind M, Boden-Albala B, et al. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA 1999;281:53 60.
P.61
56. Hillbom M, Kaste M. Alcohol intoxication: A risk factor for primary subarachnoid hemorrhage. Neurology 1982;32:706 711.
57. Calandre L, Amal C, Fernandez Ortega J. Risk factors for spontaneous hematomas: Case-control study. Stroke 1986;17:1126 1128.
58. Hillbom M, Kaste M. Ethanol intoxication: A risk factor for ischemic brain infarction. Stroke 1983; 14:694 698.
59. Lindegard B, Hillbom M. Associations between brain infarction, diabetes and alcoholism: Observations from the Gothenburg population cohort study. Acta Neurol Scand 1987;75:195 200.
60. Hillbom M, Kaste M. Alcohol abuse and brain infarction. Ann Med 1990; 22:347 352.
61. Hillbom M, Haapaniemi H, Juvela S, et al. Recent alcohol consumption, cigarette smoking, and cerebral infarction in young adults. Stroke 1995;26:40 45.
62. Gorelick PB, Redin MB, Langenberg P, et al. Is acute alcohol ingestion a risk factor for ischemic stroke? Results of a controlled study in middle-aged and elderly stroke patients at three urban centers. Stroke 1987; 18:359 364.
63. Fink R, Hutton RA. Changes in the blood platelets of alcoholics during alcohol withdrawal. J Clin Pathol 1983;36:337 340.
64. Peterson B. Analysis of the role alcohol in mortality, particularly sudden unwitnessed death, in middle-aged men in Malmo, Sweden. Alcohol 1988;23:259 263.
65. Kono S, Ikeda M, Tokudome et al. Alcohol and mortality: A cohort study of male Japanese physicians. Int J Epidemiol 1986;15:527 532.
66. Boysen G, Nyboe J, Appleyard M, et al. Stroke incidence and risk factors for stroke in Copenhagen, Denmark. Stroke 1988;19:1345 1353.
67. Stampfer MJ, Colditz GA, Willet WC, et al. A prospective study of moderate alcohol consumption and the risk of coronary disease stroke in women. N Engl J Med 1988;319:267 273.
68. Klatsky AL, Armstrong MA, Friedman GD. Risk of cardiovascular mortality in alcohol drinkers, ex-drinkers and non-drinkers. Am J Cardiol 1990;166:1237 1242.
69. Donahue RP, Abbott RD, Reed DM, et al. Alcohol and hemorrhage stroke: The Honolulu Heart Program. JAMA 1986;255:2311 2314.
70. Goldberg RJ, Burchfield CM, Reed DM, et al. A prospective study of the health effects of alcohol consumption in middle-aged and elderly men: The Honolulu Program. Circulation 1994;89:651 659.
71. Kiyohara Y, Kato I, Iwamoto H, et al. The impact of alcohol and hypertension on stroke incidence in a general Japanese population: The Hisayama Study. Stroke 1995;26:368 372.
72. Lindenstrom E, Boysen G, Nyboe J. Risk factors for stroke in Copenhagen, Denmark. Neuroepidemiology 1993;12:37 42.
73. Truelsen T, Gronbaek M, Schnohr P, et al. For the Copenhagen City Heart Study. Intake of beer, wine and spirits risk of stroke. Stroke 1998;29:2467 2472.
74. Hansagi H, Romelsjo A, Gerhardsson de Verdier M, et al. Alcohol consumption and stroke mortality: 20-year follow-up of 15,077 men and women. Stroke 1995;26(10): 1768 1773.
75. Wannamethee SG, Shaper AG. Patterns of alcohol intake and risk of stroke in middle-aged British men. Stroke 1996;27:1033 1039.
76. Norton R, Batey Dwyer T, et al. Alcohol consumption and the risk of alcohol related cirrhosis in women. BMJ 1987;295:80 82.
77. Popham RE, Schmidt W. The biomedical definition of safe alcohol consumption: A crucial issue for the researcher of the drinker. Br J Addict 1978;73:233 235.
P.62
78. Andreasson S, Allebeck P, Rosmelsjo A. Alcohol and mortality among young men: Longitudinal study of Swedish conscripts. BMJ 1998;226:1021 1025.
79. Gronbaek M, Becker U, Johansen D, et al. Population based cohort study of the association between alcohol intake and cancer of the upper digestive tract. BMJ 1998; 317:844 847.
80. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global burden of disease study. Lancet 1997;349:1436 1442.
81. Orgogozo JM, Dartigues FJ, Lafon S, et al. Wine consumption and dementia in the elderly: A prospective community study in the Brodeaux area. Rev Neurol 1997: 153(3): 185 192.
82. Lemeshow S, Letenneur L, Dartigues JF, et al. Illustration of analysis taking into account complex survey considerations: The association between wine consumption and dementia in the PAQUID study. Am J Epidemiol 1998; 148:298 306.
83. Hillbom M, Numminen H. Alcohol and stroke: Pathophysiologic mechanisms. Neuroepidemiology 1998;17:281 287.
84. Fraser GE, Anderson JT, Foster N, et al. The effect of alcohol on serum high density lipoprotein (HDL). Atherosclerosis 1983;46:275 286.
85. Thornton J, Symes C, Heaton K. Moderate alcohol intake reduces bile cholesterol saturation and raises HDL cholesterol. Lancet 1983; 1:819 821.
86. Taskinen RM, Nikkila EA, Valimaki M, et al. Alcohol-induced changes in serum lipoproteins and their metabolism. Am Heart J 1987; 13:458 464.
87. Contaldo F, D'Arrigo E, Carandente V, et al. Short-term effects of moderate alcohol consumption on lipid metabolism and energy balance in normal men. Metabolism 1989;38:166 171.
88. Suh I, Shaten BJ, Cutler JA, et al. Alcohol use and mortality from coronary heart disease: The role of high-density lipoprotein cholesterol: Multiple Risk Factor Intervention Trial Research Group. Ann Intern Med 1992; 16:881 887.
89. Castelli WP, Doyle JT, Gorden T, et al. Alcohol and blood lipids: The Cooperative Lipoprotein Phenotyping Study. Lancet 1977;2:153 155.
90. Masarei JRL, Puddey IB, Rouse IL, et al. Effects of alcohol consumption on serum lipoprotein: Lipid and apolipoprotein concentrations. Results from an intervention study in healthy subjects. Atherosclerosis 1986;60:79 87.
91. Suzukawa M, Ishikawa T, Yoshida H, et al. Effects of alcohol consumption on antioxidant content and susceptibility of low-density-lipoprotein to oxidative modification. JAm Coll Nutr 1994;13:237 242.
92. Camargo CA Jr, Hennekens CH, Gaziano JM, et al. Prospective study of moderate alcohol consumption and mortality in US male physicians. Arch Intern Med 1997; 157:79 85.
93. Enas AE. Alcohol and cardiovascular mortality in US physicians: Is there a modifier effect by low-density lipoprotein? Arch Intern Med 1997;157:1769 1770.
94. Camargo CA, Williams PT, Vranizan KM, et al. The effect of moderate alcohol intake on serum apolipoproteins Al and All: A controlled study. JAMA 1985;253:2854 2857.
95. Branchi A, Rovellini Tornella C, et al. Association of alcohol consumption with HDL subpopulations defined by apolipoprotein A-I and apolipoproteins I and apolipoproteins A-II content. Eur J Clin Nutr 1997;51:362 365.
96. Davis JW, Philips PE. The effect of ethanol on human platelet aggregation in vitro. Atherosclerosis 1970; 11:473 477.
97. Haut MJ, Cowan DH. The effect of ethanol on hemostatic properties of human blood platelets. Am J Med 1974;56:22 33.
P.63
98. Fenn CG, Littleton JM. Inhibition of platelet aggregation by ethanol in vitro shows specificity for aggregating agent used and is influenced by platelet lipid composition. Thromb Haemost 1982;48:49 53.
99. Rand ML, Packham MA, Kinlouigh-Rathbone RL, et al. Effects of ethanol on pathways of platelet aggregation in vitro. Thromb Haemost 1988;59:383 387.
100. Rubin R. Ethanol interferes with collagen-induced platelet activation by inhibition of arachidonic acid mobilization? Arch Biochem Biophys 1989;270:99 113.
101. Benistant C, Rubin R. Ethanol inhibits thrombin-induced secretion by human platelets at a site distinct from phospholipase C or protein kinase C. Biochem J 1990; 269 289.
102. Elmer O, Goransson G, and Zoucas E. Impairment of primary hemostasis and platelet function after alcohol ingestion in man. Hemostasis 1984; 14:223 228.
103. Hillbom M, Kangasaho Kaste et al. Acute ethanol ingestion increases platelet reactivity: Is there a relationship to stroke? Stroke 1985;16:19 23.
104. Cederbaum Al. Introduction: Role of lipid peroxidation and oxidative stress in alcohol toxicity. Free Rod Biol Med 1989;7:537 539.
105. Landolfi R, Steiner M. Ethanol raises prostacyclin in vivo and in vitro. Blood 1984;64:679 682.
106. Mehta P, Mehta J, Lawson D, et al. Ethanol stimulates prostacyclin biosynthesis by human neutrophils and potentiates anti-platelet aggregatory effects of prostacyclin. Thromb Res 1987;48:653 661.
107. Jakubovski JA, Vaillancourt R, Deykin D. Interaction of ethanol, prostacyclin, and aspirin in determining human platelet reactivity vitro. Arteriosclerosis 1988;8: 436 441.
108. Deykin D, Janson P, McMahon I. Ethanol potentiation of aspirin-induced prolongation of the bleeding time. N Engl J Med 1982;306:852 854.
109. Meade TW, Chakrabarti R, Haines AP, et al. Characteristics affecting fibrinolytic activity and plasma fibrinogen concentrations. BMJ 1979;1:153 156.
110. Pikaar NA, Wedel M, van der Beek EJ, et al. Effects of moderate alcohol consumption on platelet aggregation, fibrinolysis and blood lipids. Metabolism 1987;6:538 543.
111. Smokovitis A, Kokolis N, Ploumis T. Enhancement of plasminogen activator activity in the gastric wall after chronic ethanol consumption. Alcohol 1991;8:17 20.
112. Hendriks HFJ, Veenstra J, Velthuis-te Wierick EJM, et al. Effect of moderate dose of alcohol with evening meal on fibronolytics factors. BMJ 1994;308:1003 1006.
113. Laug WE. Ethyl alcohol enhances plasminogen activator secretion by endothelial cells. JAMA 1983;250:772 776.
114. Ridker PM, Vanghan DE, Stampfer MJ, et al. Association of moderate alcohol consumption and plasma concentration of endogenous tissue-type plasminogen activator. JAMA 1994;272:929 933.
115. Sumi H, Hamada Tsushima et al. Urokinase-like plasminogen activator increased in plasma after alcohol drinking. Alchol 1988;23:33 43.
116. Ruf JC, Berger JL, Renaud S. Platelet rebound effect of alcohol withdrawal and wine drinking in rats: Relation to tanins and lipid peroxidation. Arterioscler Thromb Vase Biol 1995; 1:140 144.
117. Antiplatelet Trialist's Collaboration. Collaborative overview of randomized trials of antiplatelet therapy. I: Prevention of death, myocardial infarction and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994;308:81 106.
118. Lee TK, Huang ZS, Ng SK, et al. Impact of alcohol consumption and cigarette smoking on stroke among the elderly in Taiwan. Stroke 1995;26:790 794.
P.64
119. Okada H, Horibe Ohno Y, Hayakawa N, and Aoki N. A prospective study of cerebrovascular disease in Japanese rural communities: Akabane and Asahi, part I: Evaluation of risk factors in the occurrence cerebral hemorrhage and thrombosis. Stroke 1976;7:599 607.
120. Tanaka H, Ueda Y, Hayashi M, Date C, Baba T, Yamashita Shoji Tanaka Y, Owada K, and Detels R. Risk factors for cerebral hemorrhage and infarction in a Japanese rural community. Stroke 1982; 13:62 73.
121. Ueda K. Hasuo Y, Kiyohara et al. Intracerebral hemorrhage in a Japanese community, Hisayama: Incidence, changing pattern during long-term follow-up, and related factors. Stroke 1982;13:62 73.
122. Ohmori T, Koyama Chen CC, et al. The role of aldehyde dehydrogenase isozyme variance in alcohol sensitivity, drinking habits formation and the development of alcoholism in Japan, Taiwan and the Philippines. Prog Neuropsychopharmacol Biol Psychiatr 1986; 10:229 235.
123. Chen CCC, Hwu HG, Yeh EK, et al. Aldehyde dehydrogenase deficiency, flush patterns and prevalence of alcoholism: An interethnic comparison. Acta Med Okayama 1991;45:409 416.
124. Bogousslavsky J, Van Melle G, Despland PA, et al. Alcohol consumption and carotid atherosclerosis in the Lausanne Stroke Registry. Stroke 1990;21:715 720.
125. Wannamethee SG and Shaper AG. Socioeconomic status within social class and mortality: A prospective study in middle-aged British men. Int J Epidemiol 1997:26: 532 541.
126. Pekkanen J, Tuomilheto Uutela A, et al. Social class, health behaviour and mortality among men and women in eastern Finland. BMJ 1995;311:589 593.
127. Tjonneland A, Gronbaek M, Stripp C, et al. Wine intake and diet in a random sample of 48763 Danish men and women. Am J Nutr 1999;69:49 54.
128. Artalejo FR, Guallar-Castillon P, Gautierrez F, et al. Socio-economic level, sedentary lifestyle, and wine consumption as possible explanations for geographic distribution of cerebrovascular disease in Spain. Stroke 1997;28:922 928.
EAN: 2147483647
Pages: 23
- Using SQL Data Definition Language (DDL) to Create Data Tables and Other Database Objects
- Using SQL Data Manipulation Language (DML) to Insert and Manipulate Data Within SQL Tables
- Working with Queries, Expressions, and Aggregate Functions
- Working with Comparison Predicates and Grouped Queries
- Repairing and Maintaining MS-SQL Server Database Files