37 - Complications of Pulmonary Resection
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section IX - The Chest Wall > Chapter 45 - Anterior Transthoracic Approaches to the Spine
Chapter 45
Anterior Transthoracic Approaches to the Spine
Kamal A. Mansour
Jacob DeLaRosa
In the last half of the 20th century, the anterior transthoracic approaches to the spinal column have become the preferred techniques to manage most problems involving the lower cervical, thoracic, and upper lumbar portions of the spine in children and adults. Hodgson and Stock (1956) and Hodgson and co-workers (1960) in Hong Kong were the first to use anterior spinal fusion in the radical treatment of Pott's disease and Pott's paraplegia (tuberculosis of the spine). The reports of Cauchoix and Binet (1957) suggested the use of median sternotomy to expose the vertebral bodies from C7 to T4. Perot and Munro (1969) described the transthoracic removal of midline thoracic disc protrusions causing spinal cord compression. Dwyer and colleagues (1969) recorded the anterior approach to scoliosis, and Harrington (1981) described the use of methyl methacrylate for vertebral body replacement and anterior stabilization of pathologic fracture-dislocations of the spine due to metastatic disease. Cook (1971) was also among the initial surgeons to bring to the attention of American surgeons the anterior thoracic approach to the spine. In addition to these early reports, a large volume of publications on this subject has been recorded in orthopedic and neurosurgical, as well as general thoracic, literature over the past 30 years. Mack and associates (1993) were the first to report the application and techniques of video-assisted thoracic surgery (VATS) for the spine. The improvement of VATS has increased the application of minimally invasive techniques to anterior transthoracic approaches to the spine.
INDICATIONS
The indications for the use of a transthoracic approach for exposure of the spine are the presence of a destructive process of one or more vertebral bodies or intervertebral discs, fractures of the thoracic or lumbar spine, and major spinal deformities (Table 45-1). The incidence of the various lesions managed by these anterior approaches varies in children and adults. Spinal deformities are much more common in children and adolescents, whereas degenerative disorders, both infectious and malignant, are more common in adults. Spinal deformities are the result of idiopathic disease, neuromuscular disorders, hemivertebra-fracture, pseudoarthrosis, Scheuermann's disease, and tumors (primarily neurofibromatosis), as well as some other uncommon causes. In contrast, in adults, Anderson and associates (1993) found the indications for these approaches to be: (a) the presence of a herniated nucleus pulposus (30%), (b) metastatic disease to the spine (27%), (c) infection (22%), (d) spinal deformities (12%), (e) fracture (6%), and (f) primary tumors involving the spine (3%). In regard to metastatic tumors and primary tumors of the spine or an adjacent structure such as the lung, mesenchymal or neurogenic tumor, McAfee and Zdeblick (1989) and Walsh and co-workers (1997) have noted that metastatic disease was by far the most common cause of destruction of a vertebral body. The common primary tumors are of the lung, kidney, breast, melanoma, multiple myeloma, pancreas, and thyroid. The indications for operation in these patients are severe pain or impending paraplegia. Lesions from the lung (primarily superior sulcus tumors), neurogenic tumors such as neuroblastoma, or ganglioneuroblastomas, as well as the benign neurofibromas, Wilms' tumor, and mesenchymal tumors such as liposarcomas, chondrosarcomas, and chordomas, are among the tumors that may secondarily involve a vertebral body. Primary tumors of the vertebral body are uncommon and include osteosarcoma, plasmacytoma, and chondrosarcoma. Operation may be for cure or at times only for palliation. Rarely, an astrocytoma may require a spinal decompression, as noted by Naunheim and associates (1994). A destructive aneurysmal bone cyst, as recorded by Janik and colleagues (1997), may require vertebrectomy and spinal stabilization. Lastly, traumatic injury with fracture and impending or present neurologic complications has been a major indication for transthoracic exposure of the lower cervical, thoracic, or thoracolumbar spine as recorded in the series of McElvein (1988) and of Naunheim (1994) and their associates.
The major indications for spinal operations are the relief of pain, stabilization of deformities, cosmesis, drainage of
P.704
areas of spinal infection, and progression of neurologic changes indicative of cord compression that may result in paresis or paralysis.
Table 45-1. Etiology of Spinal Disorders that Indicate Anterior Thoracic Approaches | |
|---|---|
|
Using a multidisciplinary approach with thoracic, orthopedic or neurologic surgeons for the patient with a spinal disorder results in improved quality of care. The advantages of the thoracic surgeon being involved are improved preoperative physiologic assessment, expedient surgical exposure, and expertise in postoperative care. The major advantages of the anterior thoracic approach to the thoracic and lumbar spine are improved visualization and increased ease of access to the area of involvement with the exposure provided.
SPECIAL PREOPERATIVE CONSIDERATIONS
Cardiopulmonary Evaluation
Certain principles will help the general thoracic surgeon to improve the quality of care to the patient. An adequate assessment of the physiologic status of the respiratory system as determined by pulmonary function studies and arterial blood gases help in planning preoperative and postoperative care. An assessment of the cardiovascular system when indicated should decrease unsuspected postoperative complications. When major chronic obstructive pulmonary disease is present, the operation may be canceled or the patient may be given preoperative pulmonary preparation.
Preoperative Embolization
Preoperative embolization may become necessary in some patients with metastatic disease involving a vertebra (e.g., renal cell carcinoma and thyroid carcinoma) because such entities may involve excessive vascularity of the metastatic lesion. Walsh and associates (1997) suggested preoperative embolization to reduce excessive blood loss. This procedure was performed in eight of their patients, but in three patients a major complication occurred: an asymptomatic aortic dissection, transient Brown-Sequard syndrome that improved significantly, and a spinal artery syndrome that resulted in paraplegia that did not improve with time. It would appear that embolization should be resorted to only if absolutely necessary.
Anesthesia
General endotracheal anesthesia with a single lumen tube is sufficient for patients undergoing cervical approaches (C7 T2). A double lumen tube is the preferred method in thoracic and lumbar approaches (T2 L2) and all VATS approaches. A single-lumen tube with a bronchial blocker can be used, but this technique is very anesthesiologist dependent and can prolong operative time if occlusion is lost. When performing an anterior approach followed immediately by a posterior approach, care must be taken to change the double-lumen endotracheal tube to a single-lumen tube before turning the patient to the prone position. Delaying the change of the endotracheal tube until after the change to the prone position places the patient at increased risk secondary to swelling of the trachea and facial edema. Occasionally the airway may be difficult to intubate initially and a tube exchanger may have to be used to switch to a double-lumen from a single-lumen tube.
Spinal Blood Supply
The thoracic surgeon must have specific knowledge of the segmental arteries. Paired segmental arteries at every vertebral level supply intraspinal and extraspinal structures. The anatomy of the segmentals and their relationship to intercostal and anterior spinal arteries is shown in Fig. 45-1. The lower cervical region is supplied by radicular branches of the vertebral, thyrocervical, and costocervical arteries. The thoracic and lumbar arteries arise from the aorta. The segmental arteries should be ligated unilaterally and close to the aorta so that the collateral supply from the intercostal arteries to the spinal cord remains intact, thus preventing ischemia. The collateral supply to the spinal cord is redundant in the cervical and lumbar regions compared with the T4 T9 level, which has poor collateral supply and represents the narrowest area of the spinal cord. This latter area is called the critical vascular zone of the spinal cord, and interference with its vascular supply is likely to result in paraplegia. The artery of Adamkiewicz is the largest feeder to the anterior and posterior spinal artery in the lumbar area. It arises on the left side in 75% to 80% of patients between the bed of T7 and L4, most often at the level of T8 to T10 (Fig. 45-2). Selective angiography of this vessel with avoidance of the artery may be helpful in deciding on the surgical approach and preventing paraplegia. There is controversy as to whether this vessel must be visualized
P.705
by preoperative angiography before operation on the lower thoracic spine, but many, including McElvein (1993), believe it is unnecessary. It is our practice, however, to perform spinal angiography in patients who require bilateral ligation of the segmental vessels and in patients with congenital kyphosis where arteriovenous malformations are common. Evoked potentials are obtained to ensure that injury to the spinal cord does not occur.
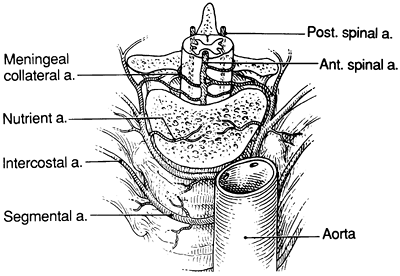 |
Fig. 45-1. Anatomy of segmental arteries in relation to aorta and intercostal arteries. a., artery; Ant., anterior; Post., posterior. |
Patient Positioning
Proper patient positioning is the most commonly overlooked step in thoracic surgery. It is extremely important to position the patient appropriately to simplify the operation but also to protect the patient from significant morbidity involved with lengthy operations. In a cervical thoracic approach (C7 T2) the patient is in a supine position with arms tucked and padded by the side. The head is slightly turned to either the right or left to expose the anterior neck area. In an upper thoracic (T2 T6) and thoracic (T6 T12) and VATS approach, the patient is placed in either a left lateral decubitus position or a right lateral decubitus position. Care is taken when turning the patient that all lines and indwelling catheters are moved with the patient. A standard beanbag can be used to hold the patient in place, but other techniques such as sticky rolls have also been used satisfactorily. An axillary roll should be placed to prevent brachial plexus injury. Care is taken to pad all areas of the patient with direct contact to a hard surface. In lower thoracic and upper lumbar (T12 L3) approach, the patient is placed supine with the thorax in a slight right lateral decubitus position with the hips lying parallel to the operating room table. With this positioning, the retroperitoneal abdomen can be approached if necessary.
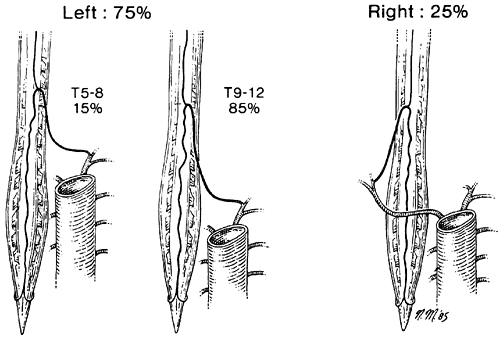 |
Fig. 45-2. Variation in the origin of the artery of Adamkiewicz from the intercostal vessels of the thoracic arch. From Shields TW, Reynolds M. Neurogenic tumors of the thorax. Surg Clin North Am 68:645, 1988. With permission. |
Intraoperative Monitoring
Wilkins and Rengachary (1985) and Jacobson and Tew (1987) suggested that intraoperative monitoring of somatosensory evoked potentials helps guide the surgeon and prevents damage to the cord, and it is common practice in the majority of centers doing this type of operation. When substantial blood loss is anticipated, the use of a cell preservation device prevents excess use of blood products.
SURGICAL APPROACHES
The choice of approach is dictated by the level and length of spinal involvement. When dealing with scoliosis and other deformities, the choice of laterality according to McElvein and colleagues (1988) should favor the side toward which the apex of the curve is pointed. The thoracic incision is placed over the rib that leads to the apex of the curve or the rib corresponding to the level of involvement. The rib may be excised as a free graft or left as a pedicle graft if required. The aorta can be visualized easily and, unless a concomitant aneurysm is present, should not be a major problem. The presence of the liver on the right and a lower spinal lesion at T10 T12 on the right may present some technical problems. Once entrance is obtained and the lung deflated, the mediastinal pleura overlying the appropriate vertebral body is incised and segmental arteries are exposed. The segmental arteries are ligated proximally and distally close to the aorta to prevent injury to the anterior spinal artery, which is supplied by collaterals from the intercostal arteries. A bipolar electrocautery must be used when operating near the neural foramen to avoid infarction of the anterior spinal artery and injury to the spinal cord. Attention should be directed to the lumbar area because of the potential injury to the lumbar veins that may occur with mobilization. If exposure of the lumbar area or from T12 to L3 is required, it is generally necessary to detach the diaphragm. The diaphragm is divided 1 to 2 cm from its costal margin and reattached at the completion of the procedure
P.706
using interrupted sutures of #1 silk. The peritoneum is then pushed anteriorly with care taken to avoid injury to the ureter and other retroperitoneal contents.
Surgical approaches can be described in terms of the lesion at four anatomic levels of the spinal column: (a) C7 to T2; (b) T2 to T6; (c) T6 to T12; and (d) T12 to L3 or L4.
Lesions from C7 to T2 are best approached through a combined upper neck sternal split to the level of the fourth intercostal space; lesions from T2 to T6, through a right thoracotomy incision; lesions from T6 to T12 through a left thoracotomy; and lesions from T12 to L3 L4 through a left thoracoabdominal approach with takedown of the diaphragm.
Exposure of C7 to T2
Lesions from C7 to T2 are best approached by a neck incision paralleling the sternocleidomastoid muscle combined with an upper sternotomy to T4. This allows optimal exposure at this level of the spinal column with optimum operating risk conditions (Fig. 45-3). The combined neck/ sternal approach is executed as follows: The skin incision is made along the anterior border of the sternocleidomastoid muscle with an upper sternotomy to T4. The head of the sternocleidomastoid muscle is divided and the carotid sheath is retracted laterally. The innominate artery is encircled and retracted inferiorly. The pharynx, thyroid, and esophagus are retracted medially with gentle pressure applied. With this approach, Walsh and colleagues (1997) suggested that a left-sided neck incision be used unless contraindicated by the laterality of the disease process because there is less likelihood of injury to the contralateral recurrent laryngeal nerve by retraction of the trachea and esophagus to obtain the appropriate exposure. Furthermore, these researchers noted that good exposure might be obtained from C4 to T3 by this approach. In patients with kyphotic deformity the left innominate vein crosses the field and can be under tension, Fang and Ong (1964) recommend dividing the vein when confronted with this situation.
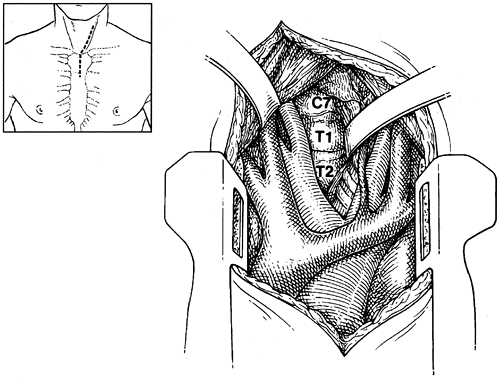 |
Fig. 45-3. Surgical exposure of C7 to T2 through combined oblique neck and upper sternotomy incision. |
Alternative approaches at this level to T1 T2 include a high transthoracic approach with freeing of the scapula from the posterior muscular and tendinous attachments to allow forward retraction, a posterolateral thoracotomy incision with removal of the second rib, or a transaxillary thoracotomy or a transsternoclavicular approach as described by Sundaresan and associates (1984).
Exposure of T2 to T6
Lesions from T2 to T6 are best approached through a right posterolateral thoracotomy going above the rib of involvement corresponding to the appropriate level of spinal pathology. For example, a disc at the level of T4 would be approached through a right fourth intercostal space incision. Exposure is obtained by deflation of the lung with medial retraction. A left-sided approach may be used if the disease process is primarily left sided, if there is involvement of the left lung or other structure, or if a previous right-sided operation has been performed. Division of the appropriate segmental arteries close to the vertebral bodies in the manner previously described ensures preservation of the anterior spinal artery. At completion, closure is preceded by placement of two standard chest tubes.
P.707
Exposure of T6 to T12
Lesions from T6 to T12 are best approached through a left posterolateral thoracotomy incision at the appropriate rib site of entrance corresponding to the level of spinal pathology. If a rib graft is needed it is obtained at the time of entry. On entering the thoracic cavity, the lung is deflated and appropriate segmental arteries are divided. If mobilization of the aorta is required this can be easily done. Intercostal arteries should only be divided if necessary because of the potential resultant morbidity. If the thoracic pathology involves a substantial number of spinal segments below T6, a spinal angiogram should be performed to visualize the artery of Adamkiewicz. Once the procedure is completed closure is executed in a routine manner.
Exposure of T12 to L3 L4
Lesions of the lower thoracic and lumbar spine extending to L3 L4 are best approached through a left thoracoabdominal incision with takedown of the diaphragm (Fig. 45-4). The patient is positioned in a 45-degree oblique chest position with the hips and abdomen rotated posteriorly. An incision is made generally through the bed of the removed tenth rib, harvesting the rib to be used as a free graft. The diaphragm is divided 1 to 2 cm from the periphery in a circumferential fashion starting with the crus posteriorly and advancing anteriorly to avoid entering the peritoneum. Lateral fibers of external and internal oblique as well as transversus abdominis muscles are divided. The peritoneum and retroperitoneal structures are mobilized medially and retracted with particular attention directed to the location of the ureter. Once exposure is obtained, segmental arteries can be divided and excellent exposure provided.
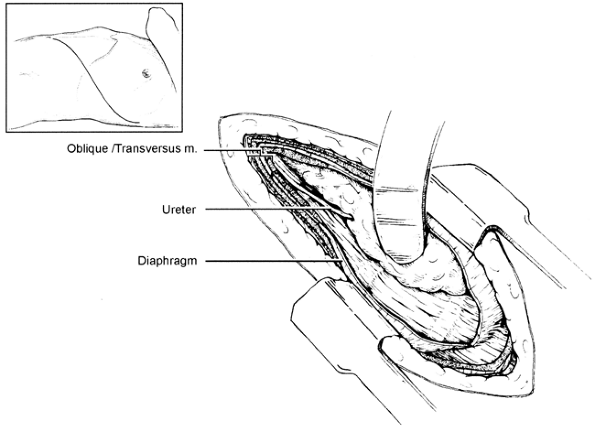 |
Fig. 45-4. Surgical exposure of T12 to L3 through a combined left thoracoabdominal exposure with diaphragmatic take-down. |
Video-Assisted Thoracic Surgery
The application of minimally invasive techniques to surgery of the spine is becoming more widespread, and indications for these techniques are expanding. Initially VATS gave limited access that allowed simple treatments, but with the advent of new equipment and a steady learning curve, complex procedures can be accomplished (Table 45-2). Current procedures that are being performed using VATS encompass the upper thoracic (T2 T6), thoracic (T6 T12), and the lower thoracic vertebrae (T12 L3). Trocars are placed along the fifth or sixth intercostal space in a standard fashion. Standard instruments available to minimally invasive thoracic surgeons accomplish the anterior exposure. Although the procedure is still in its early stages, McAfee and colleagues (1995) reported minimal complications in a series of 78 anterior VATS transthoracic procedures.
THE VERTEBRAL PROCEDURE
Management of the Diseased Vertebra
The treatment of the vertebra and intervertebral disc generally is performed by the neurosurgeon or orthopedic surgeon and depends on the disease process present. In Pott's disease or other infectious processes, a paraspinal abscess is evacuated and precise curettage of the diseased vertebra is executed. In patients with malignant involvement, Walsh and associates (1997) remove the vertebral body and perform
P.708
a discectomy above and below the involved vertebra. The tumor is removed down to the posterior longitudinal ligament, which is incised and retracted to expose and decompress the dural sac. The nerve roots must be visualized as well as the bony end plates of the vertebrae above and below the resected discs. These structures must be free of gross tumor. In patients with a complex kyphoscoliotic deformity, extensive exposure is necessary to manage both upper and lower ends of the spinal curvature as noted by Janik and associates (1997).
Table 45-2. Indications for Video-Assisted Thoracoscopic Surgery Anterior Transthoracic Approach | |
|---|---|
|
Reconstruction and Fixation
Reconstruction may be achieved using bone grafts; autogenous bone is preferred. Most of these are not vascularized, but McElvein and colleagues (1988) suggest the use of a vascularized rib segment. A methylmethacrylate strut may be fashioned and used instead of a bone graft. Walsh and associates (1997) have presented their technique with this material.
Fixation, when indicated, is performed anteriorly by using locking plate and screw constructs whenever possible. When this cannot be done, posterior constructs are placed via a separate posterior incision, either during the same operative procedure or several days later. The former is preferred over the latter approach whenever possible. In patients with scoliosis, special instrumentation (e.g., Dwyer internal fixation apparatus, Harrington rods) is required, as is also the case with fracture-dislocations of C7 T1.
Mortality and Morbidity
The mortality rate after anterior exposure of the spine varies from zero to as high as 8.2% (Table 45-3). These rates depend primarily on the disease process present, patient selection, and the age group undergoing surgery. Cancer patients appear to have the highest incidence of postoperative mortality, although Naunheim and colleagues (1994), by multivariate analysis of their data, showed that the only significant independent predictor of a postoperative fatality was the presence of osteomyelitis, and this was associated with a mortality rate of 25%. Faciszewski and his group (1995) reported only 4 deaths out of the total of 1,223 patients (0.33%). Complete paraplegia was reported in 2 patients (0.16%). Both patients had undergone anterior corpectomy with strut grafting and a strut graft dislodged posteriorly before the posterior procedure could be performed.
Table 45-3. Mortality and Morbidity Rates after Anterior Spinal Operations | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
Postoperative morbidity rates vary from 7.8% to as high as 29.5% (see Table 45-3). The major complications are respiratory: pulmonary dysfunction, retained secretions, atelectasis, pulmonary edema, adult respiratory distress syndrome, effusion, and pneumothorax from air leaks. Cardiac complications comprise the second largest number and consist of dysrhythmias, myocardial infarction, and congestive failure. Urinary tract infection, cerebrovascular accident, gastrointestinal complications, wound infection, and dehiscence are recorded in a varying number of patients.
REFERENCES
Anderson TM, Mansour KA, Miller JI Jr: Thoracic approaches to anterior spinal operations: anterior thoracic approaches. Ann Thorac Surg 55: 1447, 1993.
Cauchoix J, Binet J: Anterior surgical approaches to the spine. Ann R Coll Surg Engl 27:237 1957.
Cook WA: Transthoracic vertebral surgery. Ann Thorac Surg 12:54, 1971.
Dwyer AF, Newton NC, Sherwood AA: An anterior approach to scoliosis. A preliminary report. Clin Orthop 62:192, 1969.
Faciszewski T, et al: The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1,223 procedures. Spine 20:1592, 1995.
Fang HSY, Ong GB: Anterior spinal fusion: the operative approaches. Clin Orthop 35:16, 1964.
Harrington KD: The use of methylmethacrylate for vertebral-body replacement and anterior stabilization of pathological fracture-dislocations of the spine due to metastatic malignant disease. J Bone Joint Surg Am 63:36, 1981.
Hodgson AR, Stock FE: Anterior spinal fusion: a preliminary communication on radical treatment of Pott's disease and Pott's paraplegia. Br J Surg 44:266, 1956.
Hodgson AR, et al: Anterior spinal fusion: the operative approach and pathologic findings in 412 patients with Pott's disease of the spine. Br J Surg 48:172, 1960.
Jacobson GP, Tew JM: Intraoperative evoked potential monitoring. J Clin Neurophysiol 4:145, 1987.
Janik JS, et al: Anterior exposure of spinal deformities and tumors: a 20-year experience. J Pediatr Surg 32:852, 1997.
Mack MJ, et al: Application of thoracoscopy for diseases of the spine. Ann Thorac Surg 56:736, 1993.
McAfee PC, Zdeblick TA: Tumors of the thoracic and lumbar spine: surgical treatment via the anterior approach. J Spinal Disord 2:145, 1989.
McAfee PC, et al: The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery: a prospective multicenter study compromising the first 100 consecutive cases. Spine 20:1624, 1995.
P.709
McElvein RB: In Discussion of Anderson TM, Mansour KA, Miller JI Jr: Thoracic approaches to anterior spinal operations: anterior thoracic approaches. Ann Thorac Surg 55:1447, 1993.
McElvein RB, et al: Transthoracic exposure for anterior spinal surgery. Ann Thorac Surg 45:278, 1988.
Naunheim KS, et al: Anterior exposure of the thoracic spine. Ann Thorac Surg 57:1436, 1994.
Perot PL Jr, Munro DD: Transthoracic removal of midline thoracic disc protrusions causing spinal cord compression. Neurosurgery 31:452, 1969.
Sundaresan N, et al: An anterior surgical approach to the upper thoracic vertebrae. J Neurosurg 61:686, 1984.
Walsh GL, et al: Anterior approaches to the thoracic spine in patients with cancer: indications and results. Ann Thorac Surg 64:1611, 1997.
Wilkins RH, Rengachary SS: Neurosurgery. New York: McGraw-Hill, 1985.
Reading References
Bridwell K, Deward R: Spinal Surgery. Philadelphia: JB Lippincott, 1996.
Hoppenfeld S, de Boer P: Surgical Exposure in Orthopedics. Philadelphia: JB Lippincott, 1991.
Watkins R: Surgical Approach to the Spine. New York: Springer-Verlag, 1983.
EAN: 2147483647
Pages: 203
- Challenging the Unpredictable: Changeable Order Management Systems
- ERP System Acquisition: A Process Model and Results From an Austrian Survey
- Context Management of ERP Processes in Virtual Communities
- Healthcare Information: From Administrative to Practice Databases
- Development of Interactive Web Sites to Enhance Police/Community Relations