28 - Sleeve Lobectomy
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section VII - Pulmonary Resections > Chapter 36 - Anterior Approach to Superior Sulcus Lesions
Chapter 36
Anterior Approach to Superior Sulcus Lesions
Philippe G. Dartevelle
Sacha Mussot
Superior sulcus lesions include a constellation of benign or malignant tumors extending to the superior thoracic inlet. They cause steady, severe, and unrelenting shoulder and arm pain along the distribution of the eighth cervical nerve trunk and first and second thoracic nerve trunks. They also cause Horner's syndrome (i.e., ptosis, miosis, and anhidrosis) and weakness and atrophy of the intrinsic muscles of the hand, a clinical entity known as Pancoast's syndrome (Pancoast, 1924). Bronchial carcinoma represents the most frequent cause of superior sulcus lesions, and we refer to this cause throughout. However, Macchiarini and colleagues (1993) reported that a wide variety of other conditions can result in Pancoast's syndrome (Table 36-1); thus, a histologic diagnosis is required when the syndrome is encountered.
PRESENTATION
Superior sulcus lesions of non small cell histology account for fewer than 5% of all bronchial carcinomas, as reported by Ginsberg and associates (1994). These tumors may arise from either upper lobe and tend to invade the parietal pleura, endothoracic fascia, subclavian vessels, brachial plexus, vertebral bodies, and first ribs. However, their clinical features are influenced by their location. Tumors located anterior to the anterior scalene muscle may invade the platysma and sternocleidomastoid muscles, external and anterior jugular veins, inferior belly of the omohyoid muscle, subclavian and internal jugular veins and their major branches, and the scalene fat pad (Fig. 36-1). They invade the first intercostal nerve and first rib more frequently than the phrenic nerve or superior vena cava, and patients usually complain of pain distributed to the upper anterior chest wall.
Tumors located between the anterior and middle scalene muscles may invade the anterior scalene muscle with the phrenic nerve lying on its anterior aspect; the subclavian artery with its primary branches, except the posterior scapular artery; and the trunks of the brachial plexus and middle scalene muscle (Fig. 36-2). These tumors present with signs and symptoms related to the compression or infiltration of the middle and lower trunks of the brachial plexus (e.g., pain and paresthesia radiating to the shoulder and upper limb).
Tumors lying posterior to the middle scalene muscles are usually located in the costovertebral groove and invade the nerve roots of T1, the posterior aspect of the subclavian and vertebral arteries, paravertebral sympathetic chain, inferior cervical (stellate) ganglion, and prevertebral muscles. Some of these posterior tumors can invade transverse processes (Fig. 36-3) and, indeed, the vertebral bodies (only those abutting the costovertebral angle or extending into the intraspinal foramina without intraspinal extension may yet be resected). Because of the peripheral location of these lesions, pulmonary symptoms, such as cough, hemoptysis, and dyspnea, are uncommon in the initial stages of the disease. Abnormal sensation and pain in the axilla and medial aspect of the upper arm in the distribution of the intercostobrachial (T2) nerve are more frequently observed in the early stage of the disease process. With further tumor growth, patients may present with full-blown Pancoast's syndrome.
PREOPERATIVE STUDIES
Any patient presenting with signs and symptoms that suggest the involvement of the thoracic inlet should undergo a careful and detailed preoperative evaluation to establish the diagnosis of bronchial carcinoma and assess operability. These patients usually present with small apical tumors that are hidden behind the clavicle and the first rib on routine chest radiographs. The diagnosis is established by history and physical examination, biochemical profile, chest radiographs, bronchoscopy and sputum cytology, fine-needle transthoracic or transcutaneous biopsy and aspiration (FNA), and computed tomography (CT) of the chest. A video-assisted thoracoscopy (VATS) occasionally might be indicated to obtain tissue proof when the other investigations are negative and to eliminate the possibility of pleural metastatic disease. If there is evidence of mediastinal
P.546
adenopathy on chest radiographs or CT scanning, histologic proof is mandatory because patients with clinical N2 disease are not suitable for operation.
Table 36-1. Causes of Pancoast's Syndrome | ||
|---|---|---|
|
Neurologic examination, magnetic resonance (MR) imaging, and electromyography delineate the tumor's extension to the brachial plexus, phrenic nerve, and epidural space. Vascular invasion is evaluated by venous angiography, subclavian arteriography, Doppler ultrasonography (cerebrovascular disorders may contraindicate sacrifice of the vertebral artery) MR imaging (Fig. 36-4). MR imaging has to be performed routinely when tumors approach the intervertebral foramina to rule out invasion of the extradural space (Fig. 36-5).
The initial evaluation also includes all preoperative cardiopulmonary functional tests routinely performed before
P.547
any major lung resection and investigative procedures to identify the presence of any metastatic disease.
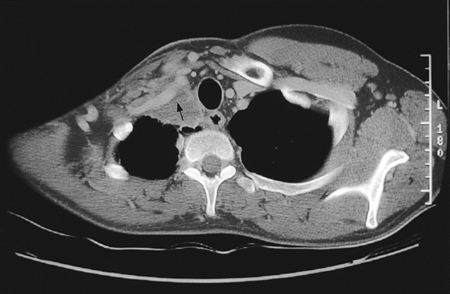 |
Fig. 36-1. Computed tomographic scan showing a right superior sulcus bronchial carcinoma invading the anterior thoracic inlet, including the subclavian vein (arrow). |
 |
Fig. 36-2. Magnetic resonance image showing a left superior sulcus bronchial carcinoma invading the middle thoracic inlet, including the subclavian artery (arrow). |
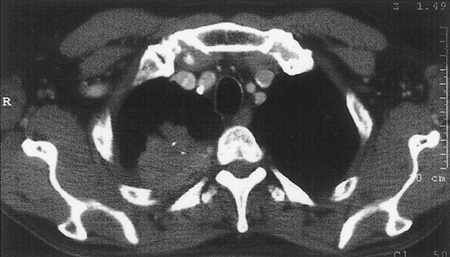 |
Fig. 36-3. Computed tomographic scan showing a right superior sulcus bronchial carcinoma invading the posterior arch and the transverse process of the first rib and abutting the costovertebral angle. |
 |
Fig. 36-4. Angiogram illustrating a massive tumoral invasion of the intrascalenic left subclavian artery (arrow). |
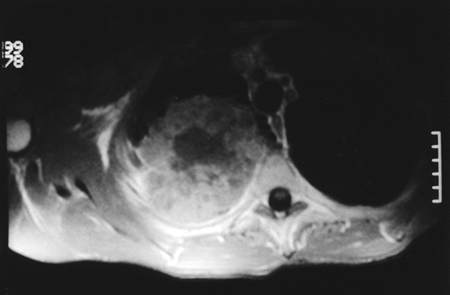 |
Fig. 36-5. Magnetic resonance image that rules out invasion of the intervertebral foramina by the tumor. |
TREATMENT
Despite their small size and general lack of extrathoracic metastasis at presentation, one of the most perplexing characteristics of superior sulcus tumors has been their almost universal and rapid mortality. For many years, it was believed that these tumors were not amenable to surgery until Chardack and MacCallum (1953) successfully performed a lobectomy and chest wall excision followed by radiation therapy. Five years later, Shaw and colleagues (1961) approached superior sulcus tumors with preoperative radiation therapy (30 to 45 Gy in 4 weeks, including the primary tumor, mediastinum, and supraclavicular region) followed by surgical resection. This multimodality approach (radiation therapy and subsequent surgical excision) shortly became the standard treatment, yielding better disease control and survival than other treatments. More recently, Ginsberg and colleagues (1994) provided evidence that en bloc resection of the chest wall and the involved adjacent structures as well as lobectomy must be considered the standard surgical approach for superior sulcus tumors to be combined with external radiation (preoperative, postoperative, or both). The goal of the operation is the complete and en bloc resection of the upper lobe in continuity with the invaded ribs, transverse processes, subclavian vessels, T1 nerve root, upper dorsal sympathetic chain, and prevertebral muscles.
One of us (PGD) and Macchiarini (1998) reviewed surgical approaches for the treatment of superior sulcus lesions. All of them must be known because the ultimate hope for cure depends on whether a complete resection is performed. As a general rule, superior sulcus tumors not invading the thoracic inlet are completely resectable through the classic posterior approach of Shaw and associates (1961) alone. Because the posterior approach does not allow direct and safe visualization, manipulation, and complete oncologic clearance of all anatomic structures that compose the thoracic inlet, superior sulcus lesions extending to the thoracic inlet should be resected by the anterior transcervical approach as described by one of us (PGD) and colleagues (1993). This operative procedure is increasingly accepted as a standard approach for all benign and malignant lesions of the thoracic inlet structures, including nonbronchial cancers (e.g., osteosarcomas of the first rib and tumors of the brachial plexus), and for exposing the anterolateral aspects of the upper thoracic vertebrae.
Contraindications to this approach include extrathoracic metastasis, invasion of the brachial plexus above the T1 nerve root, invasion of the vertebral canal and sheath of the medulla, massive invasion of the scalene muscles and extrathoracic muscles, mediastinal lymph node metastasis, and significant cardiopulmonary disease.
ANTERIOR TRANSCERVICAL TECHNIQUE
One-lung anesthesia and measurements of urine output and body temperature are necessary, as is an arterial line opposite to the primary lesion and at least two venous lines for volume expansion as necessary. The patient is supine, with the neck hyperextended and the head turned away from the involved side. A bolster behind the shoulder elevates the operative field. The skin preparation extends from the mastoid downward to the xiphoid process and from the midaxillary line laterally to the contralateral midclavicular line medially.
An L-shaped cervicotomy incision is made, including a vertical presternocleidomastoid incision carried horizontally below the clavicle up to the deltopectoral groove (Fig. 36-6).
P.548
The incision is then deepened with cautery. The sternal attachment of the sternocleidomastoid muscle is divided. The cleidomastoid muscle, along with the upper digitations of the ipsilateral pectoralis major muscle, is scraped from the clavicle. A myocutaneous flap is then folded back, providing full exposure of the neck and cervicothoracic junction.
 |
Fig. 36-6. Anterior transcervical approach, as described by one of us (PD) and colleagues (1993). |
Once the inferior belly of the omohyoid muscle is divided, the scalene fat pad is dissected and pathologically examined to exclude scalene lymph node metastasis. Inspection of the ipsilateral superior mediastinum after division of the sternothyroid and sternohyoid muscles is then made by the operator's finger along the tracheoesophageal groove. The tumor's extension to the thoracic inlet is then carefully assessed. We recommend resection of the medial half of the clavicle only if the tumor is deemed resectable.
The jugular veins are dissected first, so that branches to the subclavian vein can eventually be divided. On the left side, ligation of the thoracic duct is usually required. Division of the distal part of the internal, external, and anterior jugular veins facilitates visualization of the venous confluence at the origin of the innominate vein; one must not hesitate to suture or ligate the internal jugular vein to increase exposure of the subclavian vein (Fig. 36-7). If the subclavian vein is involved, it can be easily resected after proximal and distal control have been achieved. Direct extension of the tumor to the innominate vein does not preclude resection.
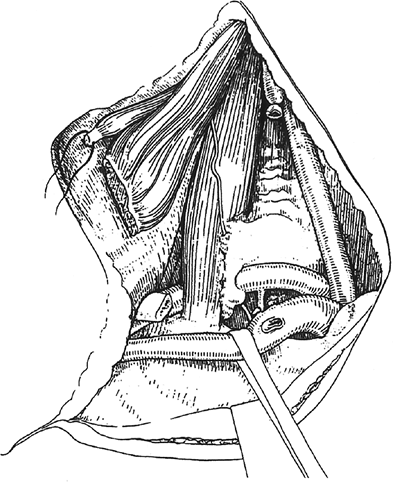 |
Fig. 36-7. Illustrative view after having divided the sternal head of the sternocleidomastoid and the inferior belly of the omohyoid muscles and resected the scalene fat pad and the internal half of the clavicle. Thereafter, the exposure, dissection, and division of the external and internal jugular vein greatly facilitates the exposure of the subclavian vein and permits assessment of tumor resectability. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
Next, the anterior scalene muscle is divided with cautery either at its insertion on the scalene tubercle of the first rib or in a tumor-free margin (Fig. 36-8). If the tumor has invaded the upper part of this muscle, it needs to be divided at its insertions on the anterior tubercles of the transverse processes of C3 C6. Before dealing with the anterior scalene muscle, the status of the phrenic nerve is carefully assessed because its unnecessary division has a deleterious influence on the postoperative course. It should be preserved whenever possible.
The subclavian artery is then dissected (Fig. 36-9). To improve its mobilization, its branches are divided; the vertebral artery is resected only if invaded and if no significant extracranial occlusive disease was detected on preoperative Doppler ultrasound. If the tumor rests against the wall of the subclavian artery, the artery can be freed following a subadventitial plane. If there is invasion of the arterial wall, resection of the artery to obtain tumor-free margins is necessary. After proximal and distal control are obtained, the artery is divided on either side of the tumor (Fig. 36-10). Revascularization is performed at the end of the procedure either with a polytetrafluoroethylene graft (6 or 8 mm) or, more often,
P.549
with an end-to-end anastomosis after freeing the carotid and subclavian arteries (Fig. 36-11). During these maneuvers, the pleural space is usually opened by dividing Sibson's fascia.
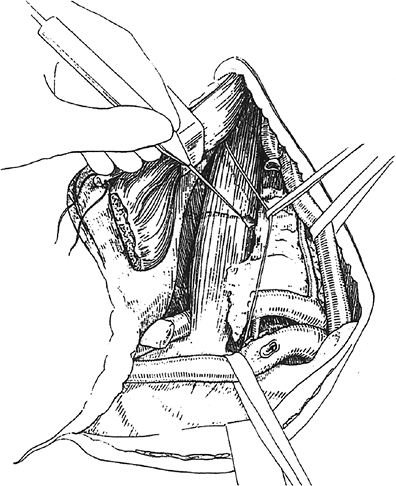 |
Fig. 36-8. The subclavian artery is exposed after division of the insertion of the anterior scalenus muscle on the first rib; the phrenic nerve is protected and preserved. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
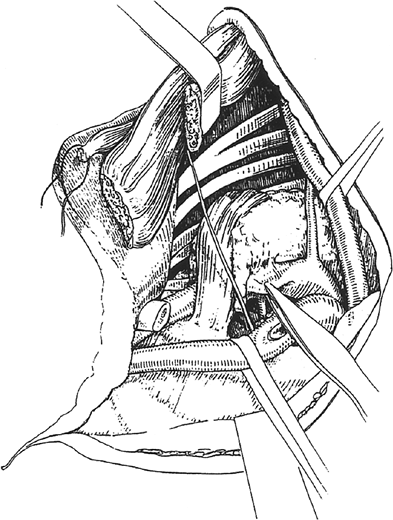 |
Fig. 36-9. The retraction of the anterior scalenus muscles allows the identification of the interscalenic trunks of the brachial plexus; the subclavian artery might be gently freed from the tumor by dividing all collateral branches (the vertebral artery is generally preserved if not invaded). Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105: 1025, 1993. |
The middle scalene muscle is divided above its insertion on the first rib or higher, as indicated by the extension of the tumor. This might require division of its insertions on the posterior tubercles of the transverse processes of vertebrae C2 C7, especially for apical tumors invading the middle compartment of the thoracic inlet. The nerve roots of C8 and T1 are then easily identified and dissected free from outside to inside up to where they join to form the lower trunk of the brachial plexus. Thereafter, the ipsilateral prevertebral muscles are resected, along with the paravertebral sympathetic chain and stellate ganglion, from the anterior surface of the vertebral bodies of C7 and T1 (Fig. 36-12). This permits oncologic clearance of the major lymphatic vessel draining the thoracic inlet, as well as visualization of the intervertebral foramina. The T1 nerve root is usually divided proximally beyond visible tumor, just lateral to the T1 intervertebral foramen. Although the tumor's spread to the brachial plexus may be high, neurolysis is usually achieved without division of the nerve roots above T1 (Fig. 36-13).
P.550
Injury of the lateral and long thoracic nerves should be avoided because it may result in a winged scapula.
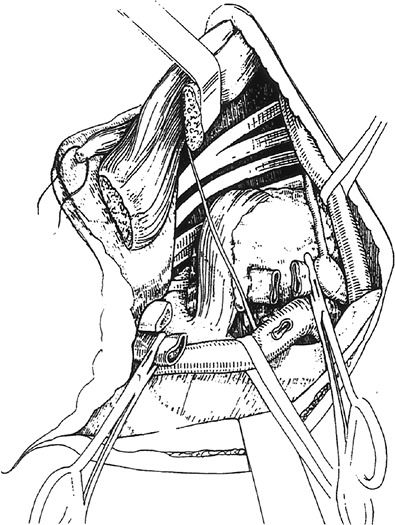 |
Fig. 36-10. If involved by the tumor, the subclavian artery might be divided after its proximal and distal control. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
 |
Fig. 36-11. Postoperative angiogram after resection through the anterior transcervical approach of a superior sulcus tumor invading the intrascalenic subclavian artery and vein, and origin of the right common artery (per Fig. 36-1). Revascularization was accomplished by an end-to-end anastomosis between the postscalenic right subclavian and the brachiocephalic artery and end-to-side anastomosis between the right common carotid and postscalenic arteries. |
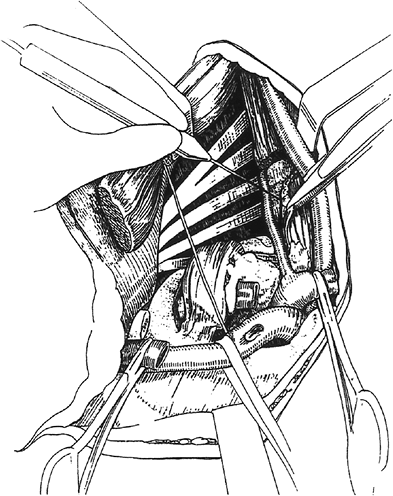 |
Fig. 36-12. The prevertebral muscles are extensively detached from the vertebral bodies, and both the stellate ganglion and dorsal sympathetic chain are isolated and finally released, using raspatories, from all surrounding attachments. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
Before the upper lobectomy, the chest wall resection is completed (Fig. 36-14). The anterolateral arch of the first rib is divided at the costochondral junction. The second rib is divided at the level of its middle arch, and the third rib is scraped on the superior border toward the costovertebral angle. The specimen is then progressively freed. The divided ribs are disarticulated from the transverse processes of the first two or three thoracic vertebrae. It is through this cavity that an upper lobectomy can be performed to complete the operation, although it is technically demanding. In effect, unlike the original description by one of us (PGD) and colleagues (1993), it has become evident that an additional posterior thoracotomy is usually not required. The upper lobectomy and chest wall resection of the first four ribs can be performed through the transcervical approach only, without resorting to a posterolateral thoracotomy. The cervical incision is closed in two layers after the sternal insertion of the sternocleidomastoid muscle is sutured, and conventional postlobectomy drainage of the ipsilateral chest cavity is carried out.
There is increasing concern about the functional and aesthetic benefit of preserving the clavicle. We believe that the indications for preserving and reconstructing the clavicle are limited to the combined resection of the serratus anterior muscle and the long thoracic nerve because this causes the scapula to rotate and to be drawn forward. This entity (scapula alata), combined with the resection of the internal half of the clavicle, pushes the shoulder anteriorly and medially and leads to severe cosmetic and functional discomfort. If this circumstance is anticipated, we recommend an oblique section of the manubrium that fully preserves the sternoclavicular articulation, its intraarticular disc, and the costoclavicular ligaments rather than the simple sternoclavicular disarticulation. Clavicular osteosynthesis can then be accomplished by placing metallic wires across the lateral clavicular edges and across the divided manubrium.
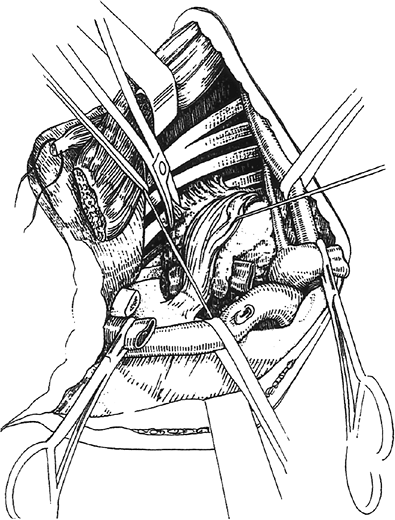 |
Fig. 36-13. Tumor's involvement of the brachial plexus requires an outside-inside neurolysis if the upper trunks are involved, or a resection of T1 if the lower trunk or nerve roots are involved. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
One of us (PGD, 1997) developed a technique for resecting posteriorly located superior sulcus tumors extending into the intervertebral foramina without intraspinal extension (Fig. 36-15). The underlying principle is that one can perform a radical procedure by resecting the intervertebral foramina and dividing the nerve roots inside the spinal canal by a combined anterior transcervical and posterior midline approach. The first step of the operation includes the transcervical approach, during which resectability is assessed and all tumor-bearing areas are freed in tumor-free margins, as described. On completion, the patient is placed in a ventral
P.551
position, and a median vertical incision is extended from spinal processes C7 T4. After a unilateral laminectomy on three levels, the nerve roots are divided inside the spinal canal at their emergence from the external sheath covering the spinal cord. After division of the ipsilateral hemivertebral bodies, the specimen is resected en bloc with the lung, ribs, and vessels through the posterior incision (Fig. 36-16). On the side of the tumor, spinal fixation is performed from the pedicle above to the pedicle below the resected hemivertebrae; on the contralateral side, a screw is placed in each pedicle (Fig. 36-17). However, the presence of an anterior spinal artery penetrating the spinal canal through an invaded
P.552
intervertebral foramen contraindicates surgery. Tumors involving transverse processes should be resected with the anterior approach. The maneuver is similar to what is used with the posterior approach but from the front to the back, with a finger placed behind the transverse process of T1 and T2 to give the correct direction of the chisel (Fig. 36-18).
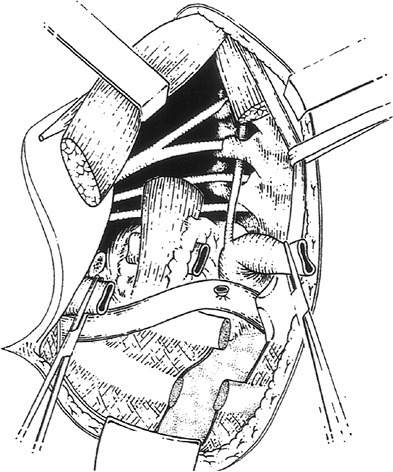 |
Fig. 36-14. Once structures above the thoracic inlet are freed from the tumor, the first two ribs might be separated anteriorly at its chondrocostal junction and resected posteriorly in tumor-free margins. The third rib is scraped on its superior border toward the costovertebral angle and retracted inferiorly. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
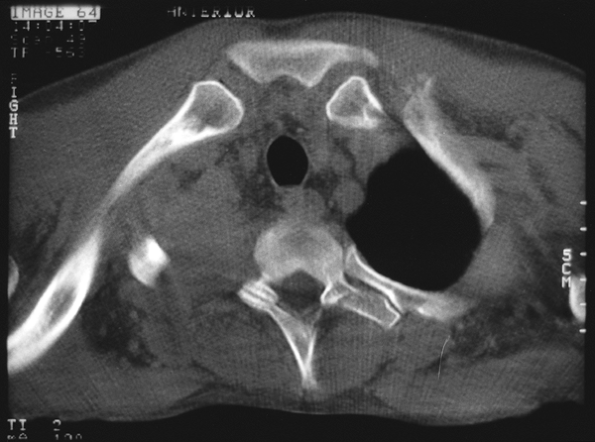 |
Fig. 36-15. Computed tomographic scan of a right superior sulcus bronchial carcinoma extending into the intervertebral foramina without intraspinal extension. |
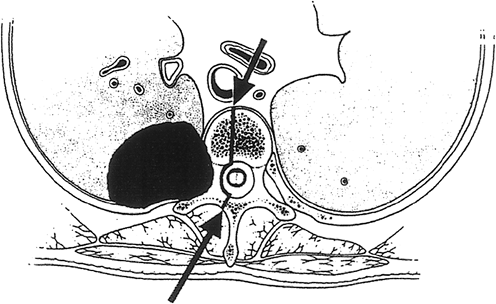 |
Fig. 36-16. Right-sided apical tumor involving the costotransverse space and intervertebral foramen and part of the ipsilateral vertebral body; this tumor is first approached anteriorly as described in the text, and then the operation is completed through a hemivertebrectomy performed through the posterior midline approach. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
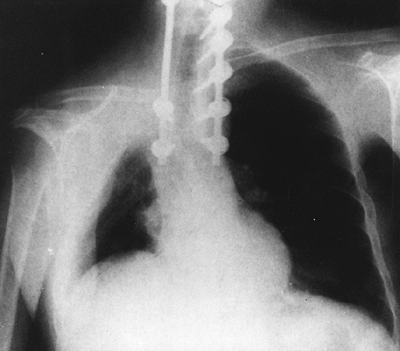 |
Fig. 36-17. Chest radiograph showing bilateral spinal fixation with metal rods interposed. From Dartevelle P: Extended operations for lung cancer. Ann Thorac Surg 63:12, 1997. With permission. |
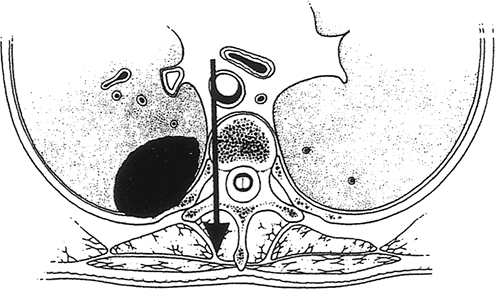 |
Fig. 36-18. Right-sided apical tumor involving the posterior arch of the rib only and resected from the anterior cervical approach by a vertical en bloc resection of part of the lateral vertebral body, the costotransverse space and transverse process. Adapted from Dartevelle P, et al: Anterior transcervical-thoracical approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993. |
SURGICAL MORBIDITY AND MORTALITY
Surgical complications are many. These consist of the following:
Spinal fluid leakage. The risks of air embolism into the subarachnoid space, ventricles, and central canal of the brain and spinal cord justify reoperation, for which a cerebral ventricular-venous shunt may be required.
Horner's syndrome and nerve deficits. Although division of the T1 nerve root does not induce significant muscular palsy in the nerve's distribution, resection of the lower trunk of the brachial plexus may result in atrophic paralysis of the forearm and small muscles of the hand, with paralysis of the cervical sympathetic system (Klumpke-D j rine syndrome). This should be discussed with the patient preoperatively. Relief of the preoperative pain and cure are worth the nerve sacrifice, however, and adaptation is usually reasonable.
Hemothorax. Hemothorax may result from extensive pleural adhesion, chest wall resection, or blood spillage from veins around the intervertebral foramina.
Chylothorax. This complication should be prevented intraoperatively by detailed and extensive ligation of the cervical and intrathoracic lymphatic vessels. Whenever it occurs, continued chest tube drainage, lung expansion, or reoperation may be necessary (see Chapter 63).
Prolonged ventilatory support. Because of chest wall dyskinesia and phrenic nerve resection or even temporary paresis from the dissection patients having a combined transcervical and midline approach are more likely than others to develop postoperative atelectasis and perfusion-ventilation mismatch. Thus, they are unable to breathe spontaneously in the early postoperative course.
The postoperative course is usually characterized by atelectasis because of the extended chest wall resection, with or without phrenic nerve sacrifice. Treatment involves measures to achieve complete lung expansion by ensuring the following: adequate ventilation, using mechanical support if necessary; satisfactory chest tube function; prevention of retained secretions by mobilization; coughing; chest physiotherapy; nasotracheal, orotracheal, or bronchoscopic suctioning or a temporary tracheostomy; adequate analgesia; and increase of the transpulmonary pressure with incentive spirometry or continuous positive airway pressure mask
Fluid overload should be avoided and diuretics used judiciously to avoid adult respiratory distress syndrome. Chest tubes remain in place until all air leaks have stopped and there is complete lung expansion and almost no fluid drainage. Incomplete lung expansion with persistent intrapleural air space should be ignored because ultimately it will be filled with serous fluid.
Resection of the subclavian vein should be accompanied by elevation of the ipsilateral forearm to facilitate venous drainage and generation of a collateral venous pathway within 1 to 2 months. One should closely follow the radial pulse to control the patency of the revascularized subclavian artery; after a preoperative loading dose of intravenous heparin, anticoagulant treatment should be switched to oral doses for a 6-month postoperative period only.
RESULTS AND PROGNOSIS
The overall 5-year survival rates after combined radiosurgical (posterior approach) treatment of superior sulcus tumors due to bronchial carcinoma range from 18% to 56% (Table 36-2). The best prognosis is found in patients without nodal involvement who have had a complete resection, as noted by Arcasoy and Jett (1997) and Ginsberg and colleagues (1994). Macchiarini and one of us (PGD) (1998) reported a complete resection rate of 100% with no postoperative mortality or major complications. The 5-year survival rate and median survival time were approximately 35% and 18 months, respectively. The local recurrence rate was less than 1.8% using our approach. Fadel and co-workers (2002) reported 17 en bloc resections of NSCLCs invading the thoracic inlet and intervertebral foramina with a 5-year survival rate and median survival time of 20% and 27 months, respectively. Among the adverse prognostic factors, the nodal status is the only predictor of disease-free survival (Table 36-3).
Table 36-2. Results of Patients Treated Surgically for Superior Sulcus Tumors | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 36-3. Factors Influencing Survival and Disease-free Survival in Completely Resected Patients Whose Superior Sulcus Tumors Invaded the Thoracic Inlet and Were Surgically Resected through the Anterior Approach | ||
|---|---|---|
|
P.553
REFERENCES
Anderson TM, Moy PM, Holmes EC: Factors affecting survival in superior sulcus tumors. J Clin Oncol 4:1598, 1986.
Arcasoy SM, Jett JR: Superior pulmonary sulcus tumors and Pancoast's syndrome. N Engl J Med 337:1370, 1997.
Chardack WM, MacCallum JD: Pancoast syndrome due to bronchogenic carcinoma: successful surgical removal and postoperative irradiation: a case report. J Thorac Surg 54:831, 1953.
Dartevelle P: Extended operations for lung cancer. Ann Thorac Surg 63: 12, 1997.
Dartevelle P, Macchiarini P: Optimal management of tumors in the superior sulcus. In Franco KL, Putman J Jr (eds): Advanced Therapy in Thoracic Surgery. Hamilton, ON: BC Decker, 1998.
Dartevelle P, et al: Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 105:1025, 1993.
Devine JW, et al: Carcinoma of the superior pulmonary sulcus treated with surgery and/or radiation therapy. Cancer 57:941, 1986.
Fadel E, et al: En bloc resection of non small cell lung cancer invading the thoracic inlet and intervertebral foramina. J Thorac Cardiovasc Surg 123:676, 2002.
Ginsberg RJ, et al: Influence of surgical resection and brachytherapy in the management of superior sulcus tumor. Ann Thorac Surg 57:1440, 1994.
Komaki R, et al: Superior sulcus tumors: treatment selection and results for 85 patients without metastasis (M0) at presentation. Int J Radiat Oncol Biol Phys 19:31, 1990.
Macchiarini P, Dartevelle P: Extended resections for lung cancer. In Roth JA, Hong WK, Cox JD (eds): Lung Cancer. 2nd Ed. Cambridge, UK: Blackwell Scientific Publications, 1998.
Macchiarini P, et al: Technique for resecting primary or metastatic non-bronchial carcinomas of the thoracic outlet. Ann Thorac Surg 55:6, 1993.
Maggi G, et al: Combined radiosurgical treatment of Pancoast tumor. Ann Thorac Surg 57:198, 1994.
McKneally M: Discussion of Shahian DM, Neptune WB, Ellis FH Jr: Pancoast tumors: improved survival with preoperative and postoperative radiotherapy. Ann Thorac Surg 43:32, 1987.
Miller JI, Mansour KA, Hatcher CR Jr: Carcinoma of the superior pulmonary sulcus. Ann Thorac Surg 28:44, 1979.
Okubo K, et al: Treatment of Pancoast tumors. Combined irradiation and radical resection. Thorac Cardiovasc Surg 43:84, 1995.
Pancoast HK: Importance of careful roentgen-ray investigations of apical chest tumors. JAMA 83:1407, 1924.
Paulson DL: Technical considerations in stage T3 disease: the superior sulcus lesion. In Delarue NC, Eschapasse H (eds): International Trends in Thoracic Surgery. Vol. 1. Philadelphia: WB Saunders, 1985, p. 121.
Sartori F, et al: Carcinoma of the superior pulmonary sulcus. Results of irradiation and radical resection. J Thorac Cardiovasc Surg 104:679, 1992.
Shahian DM, Neptune WB, Ellis FH Jr: Pancoast tumors: improved survival with preoperative and postoperative radiotherapy. Ann Thorac Surg 43:32, 1987.
Shaw RR, Paulson DL, Kee JLJ: Treatment of the superior sulcus tumor by irradiation followed by resection. Ann Surg 154:29, 1961.
Wright CD, et al: Superior sulcus lung tumors. Results of combined treatment (irradiation and radical resection). J Thorac Cardiovasc Surg 94: 69, 1987.
EAN: 2147483647
Pages: 203
- The Four Keys to Lean Six Sigma
- Beyond the Basics: The Five Laws of Lean Six Sigma
- Making Improvements That Last: An Illustrated Guide to DMAIC and the Lean Six Sigma Toolkit
- The Experience of Making Improvements: What Its Like to Work on Lean Six Sigma Projects
- Six Things Managers Must Do: How to Support Lean Six Sigma