124 - Lymphatic Drainage of the Esophagus
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume II > The Esophagus > Section XXIII - Benign Esophageal Disease > Chapter 144 - Cardial Incompetence and Associated Gastroesophageal Reflux
Chapter 144
Cardial Incompetence and Associated Gastroesophageal Reflux
Marleta Reynolds
Nelson and associates (1997) reported that up to 50% of all infants up to 3 months of age and 67% of infants 4 to 6 months of age have some degree of recurrent vomiting. When such infants are followed for 1 year, Nelson and colleagues (1998) found that most suffer no complications from the vomiting and that their symptoms disappear by 9 to 12 months of age. Local anatomic defects play a role in recurrent vomiting because infants with diaphragm and esophageal anomalies have a higher incidence of cardial incompetence. Neurologically impaired children are also prone to cardial incompetence.
Although most infants have a normal lower esophageal sphincter (LES) pressure, Moroz and associates (1976) found the LES to be located above the diaphragm for the first 6 months of life. This prevents diaphragmatic crural contraction around the gastroesophageal junction and compression of the lower esophagus. Omari and colleagues (1998) found that most reflux episodes are associated with transient LES relaxation.
A small percentage of infants will develop complications of vomiting, such as malnutrition, aspiration pneumonia, reactive airway disease, or sudden death. The esophageal and respiratory complications develop when normal protective reflexes are disturbed. Poor esophageal clearance of gastric acid will result in esophagitis. Laryngospasm, asthma, or recurrent pneumonia may develop when normal airway protective reflexes are inadequate. Many infants or children with neurologic disorders have associated poor esophageal motility and decreased esophageal acid clearance.
SYMPTOMS
Vomiting is the most common symptom of cardial incompetence and may begin shortly after birth. It usually occurs after feedings and consists of ingested materials. In babies who develop esophagitis, coffee-ground emesis may become apparent. Failure to thrive leading to malnutrition develops as formula changes fail to relieve the vomiting.
Chronic aspiration may lead to nocturnal wheezing and chronic cough. Some infants and children are mistakenly treated for asthma. Balson and colleagues (1998), however, suggest that abnormal reflux can be diagnosed in some children with severe asthma and that these asthmatics should be evaluated and aggressively treated when reflux is found. Pneumonia may develop and require hospitalization and parenteral antibiotic therapy. Leape and associates (1977) confirmed an association of respiratory arrest and gastroesophageal reflux (GER) in 10 infants younger than 6 months. Apnea may or may not be related to cardial incompetence.
Strictures of the distal esophagus may develop after prolonged esophagitis. Although usually found in older children, I have treated several infants with severe strictures from prolonged reflux. Intolerance to feedings results when the stricture persists untreated (Fig. 144-1). Barrett's esophagus is very rare in children. Hassall (1997) reported that in many children with Barrett's esophagus, the following comorbidities exist: neurologic impairment, chronic lung disease, esophageal atresia, and malignancies treated with chemotherapy.
DIAGNOSIS
A careful history is imperative in differentiating cardial incompetence and associated GER from rumination and normal spit-up. A barium esophagogram and upper gastrointestinal series with fluoroscopic recording should be the initial studies of choice to rule out other surgical causes of vomiting. The gastroesophageal scintiscan can accurately diagnose reflux when an esophagogram has been normal. Twenty-four-hour pH monitoring is the most accurate means to test for GER. A new technique mentioned by Lee and Rudolph (2001) of measuring intraluminal electrical
P.2187
impedance is under investigation to help evaluate the relation of nonacidic gastroesophageal reflux to apnea. Esophagoscopy and biopsy of esophageal mucosa confirm the presence of esophagitis and Barrett's esophagus. They are also useful for excluding eosinophilic or infectious esophagitis.
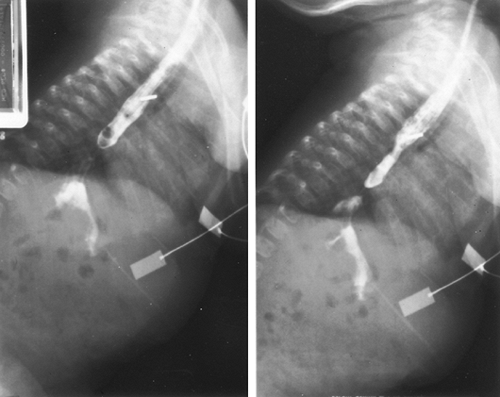 |
Fig. 144-1. Barium esophagogram demonstrates a distal esophageal stricture in a neonate with severe gastroesophageal reflux. |
TREATMENT
Medical Therapy
Conservative therapy can control symptoms in most children with cardial incompetence and GER. Dietary manipulations include increasing the frequency and decreasing the volume of feedings and thickening feedings with rice cereal. A 2-week trial of hypoallergenic formula should be attempted. Some authors recommend the prone upright position. Risk of sudden infant death syndrome (SIDS) precludes prone positioning during sleeping. The risk of SIDS must be weighed against the risk of complications of reflux. Orenstein (1992) advocates acid-reducing agents, such as H2 blockers, as the first line of therapy in infants and children. Proton pump inhibitors block hydrogen ion production and are used as the second line of therapy. Cisapride (Propulsid) is a prokinetic agent and is no longer available for use because of its association with life-threatening arrhythmias.
Surgical Intervention
Approximately 15% of patients with cardial incompetence require surgical intervention to correct persistent gastroesophageal
P.2188
reflux. The incidence of neurologic disorders is high in this subset of patients. Fonkalsrud and colleagues (1985) reported that 32% of the infants and children in their series who required surgical intervention had coexisting neurologic problems. For many patients who do not respond to medical therapy, a period of nasogastric drip feedings or total parenteral nutrition may be required to improve their nutritional status and make them adequate surgical candidates.
 |
Fig. 144-2. A. The operation may be performed through an upper midline or left subcostal incision. B. A large catheter is placed in the esophagus, and short gastric vessels are ligated and divided. C. The diaphragmatic crura are closed with Ti-Cron pledgeted sutures. D. The fundus of the stomach is passed behind the esophagus and sutured to the esophageal wall. E. The 360-degree wrap forms the fundoplication. From Raffensperger JG: Gastroesophageal reflux. In Raffensperger J.G. (ed): Swenson's Pediatric Surgery. Norwalk CT: Appleton and Lange, 1990, p. 811. With permission. |
Respiratory complications of GER, including recurrent pneumonias, life-threatening reactive airway disease, and sudden-death events, are the most common indications for surgical treatment. Other less common indications include esophageal strictures, Barrett's esophagus, and prevention of postoperative injury following laryngeal reconstruction.
Operations
The Nissen fundoplication and Thal fundoplication are used most frequently to treat cardial incompetence and GER in children. Both secure the esophageal hiatus below the diaphragm, create a new angle of His, and provide an artificial valvelike mechanism to recreate a normal lower esophageal sphincter. The Thal fundoplication is favored over the Nissen in children with esophageal dysmotility.
 |
Fig. 144-3. A. Exposure of the hiatus is through an upper midline or left subcostal incision. The short gastric vessels are not divided. A suture closes the hiatus, and a continuous permanent suture is begun to the left of the esophagus. B. The suture is continued up the esophagus, securing the stomach to the esophagus. C. The suture continues across and down the right side to achieve a 210-degree wrap around the anterior wall of the esophagus. From Raffensperger JG: Gastroesophageal reflux. In Raffensperger J.G. (ed): Swenson's Pediatric Surgery. Norwalk CT: Appleton and Lange, 1990, p. 811. With permission. |
In performing a Nissen fundoplication, I place a mercury bougie into the distal esophagus from the mouth to prevent the wrap from becoming too tight. I approach the hiatus through a left subcostal or midline incision and isolate the distal esophagus. The diaphragmatic crus is sutured with interrupted pledgeted suture, and the fundus of the stomach is passed around the gastroesophageal junction after division of several short gastric vessels. The 360-degree wrap is created with permanent suture, sewing the stomach to itself and the underlying esophagus and diaphragm superiorly (Fig. 144-2).
Ashcraft and colleagues (1984) advocate the Thal fundoplication. The 270-degree wrap is created with a running suture, and, at the apex, the diaphragm is incorporated (Fig. 144-3).
Laparoscopic techniques can be applied to both fundoplication procedures. Rothenberg (1998) reported his initial experience with laparoscopic Nissen fundoplication in over 200 children. Ostlie and associates (2002) and Tashjian and colleagues (2002) more recently reported their laparoscopic experience with Nissen fundoplication. Results using these techniques are similar to the open technique, and complication rates are comparable. Length of hospital stay may be shorter using the minimally invasive techniques. Wales and colleagues (2002) reported their experience using an
P.2189
image-guided gastrojejunal tube as an alternative to fundoplication and gastrostomy in neurologically impaired children with reflux.
Complications of all procedures are not uncommon. Dysphagia and gas bloat are common early postoperative complications of fundoplication. Both improve over time. Pearl and associates (1990) reported that gagging and retching occur most often in children with neurologic disorders. Paraesophageal hernias, suture-line dehiscence, bowel obstructions, and recurrent reflux may occur. Recurrent gastroesophageal reflux develops in 3% to 40% of children treated with a Nissen fundoplication after 4 to 9 years.
REFERENCES
Ashcraft K, et al: The Thal fundoplication for gastroesophageal reflux. J Pediatr Surg 19:480, 1984.
Balson BM, Kravitz EKS, McGeady PJ: Diagnosis and treatment of gastroesophageal reflux in children and adolescents with severe asthma. Ann Allergy Asthma Immunol 81:159, 1998.
Fonkalsrud EW, Ament ME, Berquist W: Surgical management of the gastroesophageal reflux syndrome in childhood. Surgery 97:42, 1985.
Hassall E: Co-morbidities in childhood Barrett's esophagus. J Pediatr Gastroenterol Nutr 25:255, 1997.
Leape LL, et al: Respiratory arrest in infants secondary to gastroesophageal reflux. Pediatrics 60:924, 1977.
Lee P, Rudolph C: Gastroesophageal reflux in infants and children. Adv Pediatr 48:301, 2001.
Moroz SP, et al: Lower esophageal sphincter function in children with and without gastroesophageal reflux. Gastroenterology 71:236, 1976.
Nelson SP, et al: Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med 151:569, 1997.
Nelson SP, et al: One-year follow-up of symptoms of gastroesophageal reflux during infancy. Pediatric Practice Research Group. Pediatrics 102: E67, 1998.
Omari TI, et al: Mechanisms of gastroesophageal reflux in healthy premature infants. J Pediatr 133:650, 1998.
Orenstein SR: Controversies in pediatric gastroesophageal reflux. J Pediatr Gastroenterol Nutr 14:338, 1992.
Ostlie DJ, Miller KA, Holcomb GW 3rd: Effective Nissen fundoplication length and bougie diameter size in young children undergoing laparoscopic Nissen fundoplication. J Pediatr Surg 37:1664, 2002.
Pearl RH, et al: Complications of gastroesophageal antireflux surgery in neurologically impaired versus neurologically normal children. J Pediatr Surg 25:1169, 1990.
Rothenberg SS: Experience with 220 consecutive laparoscopic Nissen fundoplications in infants and children. J Pediatr Surg 37:274, 1998.
Tashjian DB, et al: Laparoscopic Nissen fundoplication for reactive airway disease. J Pediatr Surg 37:1021, 2002.
Wales PW, et al: Fundoplication and gastrostomy versus image-guided gastrojejunal tube for enteral feeding in neurologically impaired children with gastroesophageal reflux. J Pediatr Surg 37:407, 2002.
EAN: 2147483647
Pages: 203