106 - Surgical Treatment of Non-Small Cell Lung Cancer
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume II > The Esophagus > Section XVIII - Anatomy > Chapter 123 - Anatomy of the Esophagus
Chapter 123
Anatomy of the Esophagus
Jeffrey A. Hagen
Tom R. DeMeester
RADIOGRAPHIC AND ENDOSCOPIC ANATOMY OF THE ESOPHAGUS
The esophagus begins as the continuation of the pharynx in the neck and ends at the junction with the stomach. When the head is in normal anatomic position, the transition from pharynx to esophagus occurs at the lower border of the sixth cervical vertebra. Topographically, this corresponds to the cricoid cartilage anteriorly and the palpable transverse process of the sixth cervical vertebra laterally (Fig. 123-1). Flexion and extension of the neck shifts this point craniad or caudad by the length of one cervical vertebral body. After traversing the thorax and passing through the diaphragm, the esophagus terminates in the stomach at the level of the eleventh thoracic vertebra. The esophagus is firmly attached to the cricoid cartilage at its upper end and to the diaphragm at its lower end, with these points of fixation moving craniad the distance of one cervical vertebral body during the act of swallowing.
Radiographically, the appearance of the resting esophagus is determined by the contiguous structures it passes and the environmental pressure of the cavities it traverses. On a barium esophagogram, the cervical portion of the esophagus is flattened, owing to compression by adjacent structures; the thoracic portion is more rounded, owing to the negative intrathoracic pressure; and the abdominal portion is flattened, owing to the positive intraabdominal pressure.
On the anteroposterior radiograph (Fig. 123-2A), the esophagus lies in the midline with a deviation to the left in the lower portion of the neck and upper portion of the thorax. At the midthoracic level, near the bifurcation of the trachea, the esophagus returns to the midline. In the lower portion of the thorax, the esophagus again deviates to the left to pass through the diaphragmatic hiatus.
On the lateral radiograph (Fig. 123-2B), the esophagus follows the curve of the vertebral column, except in the lower thoracic area, where it curves anteriorly to pass through the diaphragmatic hiatus. This posterior curvature and terminal left anterior deviation are of importance in the performance of rigid esophagoscopy. The patient should be positioned to allow maximum extension of the cervical and thoracic spine so that the rigid scope can be safely manipulated through this terminal arc. As a result of the anterior and leftward deviation of the distal esophagus, this region is the second most common site for traumatic esophageal perforation during rigid endoscopy, the first being the narrow entrance of the esophagus at the level of the cricopharyngeus.
There are three normal areas of anatomic narrowing in the esophagus that appear on the barium esophagogram and at esophagoscopy. The uppermost narrowing is located at the entrance into the esophagus and is caused by the cricopharyngeus muscle. The average luminal diameter is 1.5 cm at the cricopharyngeus, the narrowest point of the esophagus. The second narrowing is the result of an indentation of the anterior and left lateral esophageal wall caused by the crossing of the left main-stem bronchus and the aortic arch. The average luminal diameter at this point is 1.6 cm. The lowermost narrowing of the esophagus is at the hiatus of the diaphragm and is caused by the anatomic lower esophageal sphincter. The luminal diameter at this point varies somewhat depending on the extent of distention of the esophagus by the passage of food, with measurements ranging from 1.6 to 1.9 cm. These areas of constriction are of importance in that swallowed foreign objects tend to hold up at these points, and it is at these sites where mucosal injury occurs when corrosive liquids or pills are swallowed.
Measurements obtained during endoscopic examination (Fig. 123-3) show that the average distance from the incisor teeth to the gastroesophageal junction is 38 to 40 cm in men and 2 cm shorter in women. These distances are proportionately shorter in children, being 18 cm at birth, 22 cm at age 3 years, and 27 cm at age 10. In men, the length of the esophagus from the cricopharyngeus muscle to the gastroesophageal junction ranges from 19 to 25 cm, with a median of 22 cm. In women, the range is 18 to 22 cm, with a median of 21 cm. The distance from the incisor teeth to the cricopharyngeus is 15 cm in men and 1 cm shorter in women. The bifurcation of the trachea and the indentation of the aortic arch ranges between 24 and 26 cm from the incisor teeth. It is helpful to locate an abnormality such as a
P.1886
P.1887
tumor or stricture in relation to the anatomic indentations caused by the aortic arch and left main bronchus, in order to select the appropriate thoracotomy approach to avoid interference from the aortic arch.
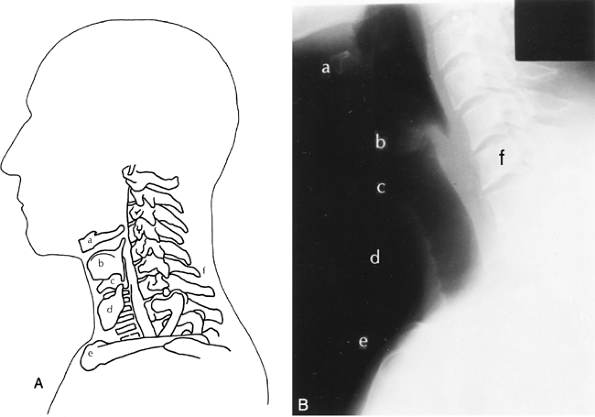 |
Fig. 123-1. A. Topographic relationships of the cervical esophagus: (a) hyoid bone, (b) thyroid cartilage, (c) cricoid cartilage, (d) thyroid gland, (e) sternomanubrial joint, (f) C6. B. Lateral radiographic appearance. |
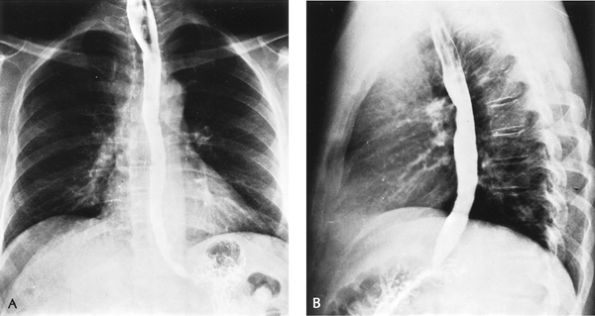 |
Fig. 123-2. Barium esophagogram. A. Anteroposterior view. B. Lateral view. |
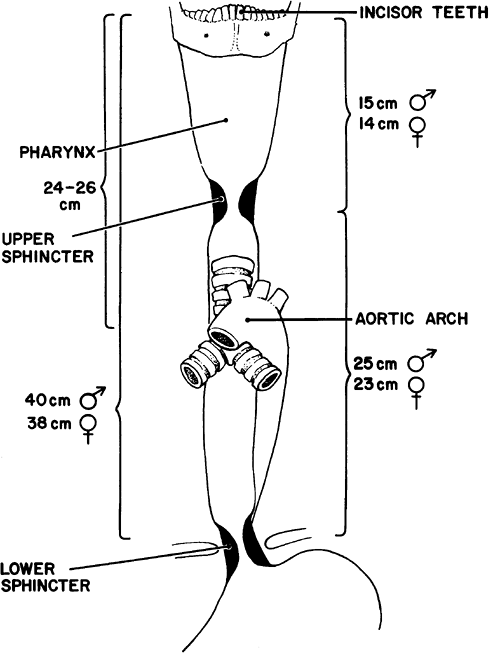 |
Fig. 123-3. Important clinical endoscopic measurements of the esophagus in adults. |
Manometrically, the length of the esophagus between the lower border of the cricopharyngeus and upper border of the lower sphincter varies according to the height of the individual. Figure 123-4 shows a nomogram for esophageal length based on height.
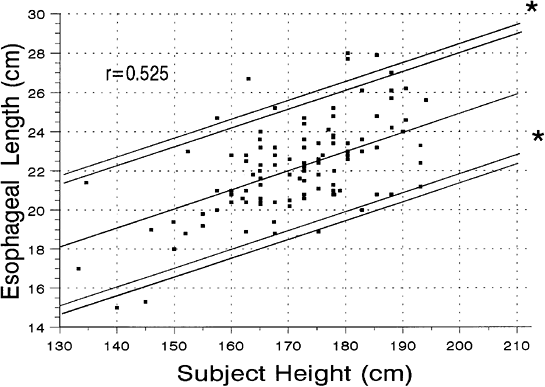 |
Fig. 123-4. Nomogram of subject height versus esophageal length. |
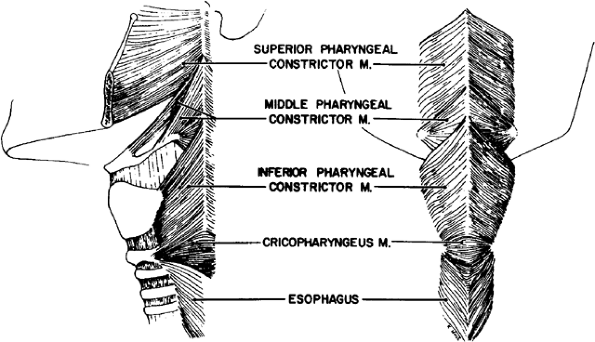 |
Fig. 123-5. External muscles of the pharynx. |
RELATIONSHIP OF THE ESOPHAGUS TO THE HYPOPHARYNX
The esophagus serves as a conduit between the pharynx and the stomach. As such, the esophagus represents an extension of the hypopharynx beginning at the lower border of the larynx at the level of the sixth cervical vertebra. The pharyngeal musculature above consists of three overlapping, broad, flat, fan shaped constrictors (Fig. 123-5). They are the superior constrictor arising mainly from the medial pterygoid plate, the middle constrictor arising from the hyoid bone, and the inferior constrictor arising from the thyroid and cricoid cartilages. These muscles insert with their corresponding muscle from the opposite side into a median posterior raphe.
The opening of the esophagus is collared by the cricopharyngeus muscle, which arises from both sides of the cricoid cartilage of the larynx and forms a continuous transverse muscle band without an interruption by a median raphe. Anatomically, the fibers of this muscle blend inseparably with those of the inferior pharyngeal constrictor above and the inner circular muscle fibers of the esophagus below. This has led some investigators to conclude that the cricopharyngeus is part of the inferior constrictor; that is, the inferior constrictor has two parts, an upper portion or thyropharyngeus having diagonal fibers, and a lower portion or cricopharyngeus having transverse fibers. Physiologically, however, Keith (1910) showed that these two parts of the same muscle serve totally different functions. The cricopharyngeal portion serves as the upper sphincter of the esophagus and relaxes when the thyropharyngeal portion contracts to force the swallowed bolus from the pharynx into the esophagus.
RELATIONSHIP OF THE CERVICAL ESOPHAGUS TO STRUCTURES AND FASCIAL PLANES OF THE NECK
The cervical portion of the esophagus is approximately 5 cm long and descends between the trachea and the vertebral column from the level of the sixth cervical vertebra to the
P.1888
level of the interspace between the first and second thoracic vertebrae posteriorly, or the suprasternal notch anteriorly. It is separated from the posterior wall of the trachea and from the prevertebral fascia posteriorly by a layer of loose fibrous tissue. The recurrent laryngeal nerves lie in the right and left grooves between the trachea and the esophagus. The left recurrent nerve lies somewhat closer to the esophagus than the right owing to the slight deviation of the esophagus to the left and the more lateral course of the right recurrent nerve around the right subclavian artery. Laterally, the esophagus is bounded on each side by the carotid sheaths and the respective lobes of the thyroid gland.
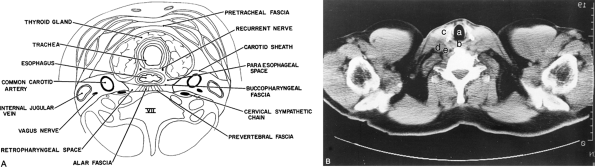 |
Fig. 123-6. A. Cross section of the neck at the level of the thyroid isthmus. B. Computed tomographic appearance viewed from above: (a) trachea, (b) esophagus, (c) left thyroid lobe, (d) internal jugular vein, (e) common carotid artery. |
Anteriorly, the cervical esophagus and trachea are covered by the pretracheal fascia, which splits to envelop the thyroid gland, continuing down to the aortic arch. Posteriorly, the trachea and esophagus are bounded by the prevertebral fascia, and laterally by the fascia forming the carotid sheath (Fig. 123-6). The buccopharyngeal fascia, which lies over the posterior pharyngeal muscles, extends inferiorly, directly on the posterior wall of the esophagus and laterally to the carotid sheaths, separating the esophagus from the prevertebral fascia. These fascial planes form two potential spaces in the neck: a paraesophageal space containing the thyroid gland, larynx, trachea, and part of the pharynx, and a retroesophageal space. The retroesophageal space, between the prevertebral fascia and the buccopharyngeal fascia, is a continuous space from the base of the skull above to the superior mediastinum below. These spaces are important clinically because they allow access for extension of infections in the neck into the mediastinum.
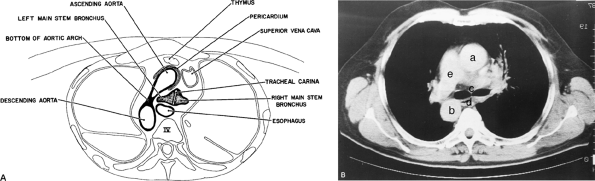 |
Fig. 123-7. A. Cross section of the thorax at the level of the tracheal bifurcation. B. Computed tomographic appearance viewed from above: (a) ascending aorta, (b) descending aorta, (c) tracheal carina, (d) esophagus, (e) pulmonary artery. |
RELATIONSHIP OF THE THORACIC ESOPHAGUS TO MEDIASTINAL STRUCTURES
The thoracic portion of the esophagus is approximately 20 cm long and starts at the thoracic inlet. From the thoracic inlet to the tracheal bifurcation, the thoracic esophagus is
P.1889
intimately related to the posterior wall of the trachea and the prevertebral fascia. Just above the tracheal bifurcation, the esophagus passes to the right of the aorta. This anatomic relationship causes the indentation in the left lateral wall of the esophagus seen on a barium swallow radiograph. Immediately below this notch, the esophagus crosses both the bifurcation of the trachea and the left main stem bronchus, owing to the slight deviation of the terminal portion of the trachea to the right by the aorta (Fig. 123-7). From there down, the esophagus passes over the posterior surface of the subcarinal lymph nodes, and then descends behind the pericardium of the left atrium to reach the diaphragmatic hiatus (Fig. 123-8).
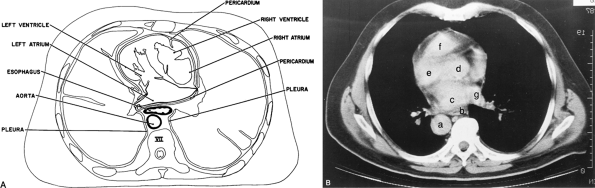 |
Fig. 123-8. A. Cross section of the thorax at mid-left atrial level. B. Computed tomographic appearance viewed from above: (a) aorta, (b) esophagus, (c) left atrium, (d) right atrium, (e) left ventricle, (f) right ventricle, (g) pulmonary vein. |
The right lateral surface of the thoracic esophagus is completely covered by the parietal pleura, except at the level of the fourth thoracic vertebra, where the azygos vein turns anteriorly over the esophagus to join the superior vena cava. The left lateral surface of the upper portion of the thoracic esophagus is covered anteriorly by the left subclavian artery and posteriorly by the parietal pleura. The distal portion of the esophagus, from the aortic arch down, lies to the right of the descending thoracic aorta. At the level of the eighth thoracic vertebra, where the esophagus moves anterior to the aorta to enter the esophageal hiatus, it is covered on the left lateral wall only by the parietal pleura. This location, owing to the lack of support from adjacent structures, is a common site of perforation in Boerhaave's syndrome. From the bifurcation of the trachea downward, both the vagal nerves and the esophageal nerve plexus lie on the muscular wall of the esophagus.
Posteriorly, the thoracic esophagus follows the curvature of the spine and remains in close contact with the vertebral bodies down to the level of the eighth thoracic vertebral body (see Figs. 123-7 and 123-8). At this point, the esophagus moves ventrally away from the spine and passes through the esophageal hiatus of the diaphragm directly in front of the aorta (Fig. 123-9). The inferior vena cava, while not in direct apposition to the esophagus, lies close by, anterior and to the right. Dorsally, the esophagus is crossed by the first five intercostal arteries and the hemiazygos vein. The thoracic duct is also posterior to the esophagus as it passes through the hiatus of the diaphragm on the anterior surface of the vertebral column behind the aorta and under the right crus of the diaphragm. As it courses superiorly, the thoracic duct lies dorsal to the esophagus between the azygos vein on the right and the descending thoracic aorta on the left. From the level of the fifth thoracic vertebra upward, the thoracic duct gradually moves to the left and settles between the esophagus and the left parietal pleura, dorsal to the aortic arch and the intrathoracic portion of the subclavian artery. In the neck, it turns away from the esophagus to join the venous system at the junction of the left subclavian and internal jugular veins.
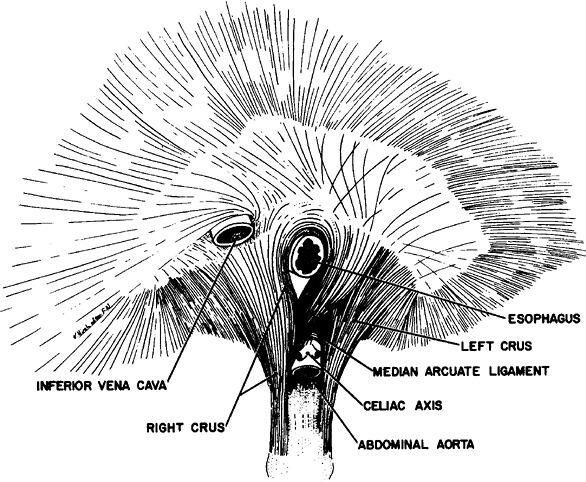 |
Fig. 123-9. The diaphragm and esophageal hiatus seen from below. |
P.1890
RELATIONSHIP OF THE TERMINAL ESOPHAGUS TO THE DIAPHRAGMATIC HIATUS AND STOMACH
The muscular fibers forming the crura of the diaphragm arise as tendinous bands from the anterolateral surface of the first three or four lumbar vertebrae and their intervening fibrocartilages (Fig. 123-9). The right crus is longer and thicker than the left, and the inferior extension of its fibers gives rise to the ligament of Treitz. The upper abdominal aorta lies at the base of the diaphragmatic hiatus just anterior to the vertebral bodies, and directly posterior to the junction of the right and left crura. The celiac and superior mesenteric arteries, as they arise from the upper abdominal aorta, separate the muscle bundles of the right and left crura. Anterior to the aorta and above the celiac artery, the right and left crura join together as the median arcuate ligament. In cadaver dissections described by Lindner and Kemprud (1971), it has been shown that in most situations, the median arcuate ligament is a firm, well-defined ligamentous structure, but in several cadavers it was difficult to identify any definite connective tissue structure where the muscles join.
The anatomy of the esophageal hiatus is variable. In the most common variant, found in 46% of individuals, the right crus forms both the right and left margins of the hiatus. As the right crus ascends, it divides into superficial and deep muscle layers. The superficial layer, by a gradual anterior curve, forms the muscular rim of the right edge of the esophageal hiatus. The deep layer inclines obliquely to the left over the anterior surface of the abdominal aorta and then ascends to form the left margin of the esophageal hiatus. The left crus ascends vertically against the fibers to the left margin of the hiatus. The most common anatomic variant is a shift to the left of various degrees, depending on the extent to which the margins of the hiatus are formed by muscle fibers from the left crus.
As the esophagus passes through the diaphragmatic hiatus, it is surrounded by the phrenoesophageal membrane, a fibroelastic ligament arising from the subdiaphragmatic fascia as a continuation of the transversalis fascia lining the abdomen (Fig. 123-10). The phrenoesophageal membrane divides at the lower margin of the esophageal hiatus into a stout, elongated ascending leaf that surrounds the terminal segment of the esophagus in tentlike fashion, and into a shorter, thin, descending leaf, which merges as the visceral peritoneal covering of the stomach. The upper leaf of the membrane attaches itself circumferentially around the esophagus, about 1 to 2 cm above the level of the hiatus. Between the upper leaf of the membrane and the esophagogastric junction is a ring of fatty tissue interspersed with fibers from the lower leaf of the membrane. These fibers blend in with the elastic-containing adventitia of the distal 2 cm of the esophagus and the proximal stomach. This makes up the abdominal portion of the esophagogastric junction, which is subjected to the positive pressure environment of the abdomen.
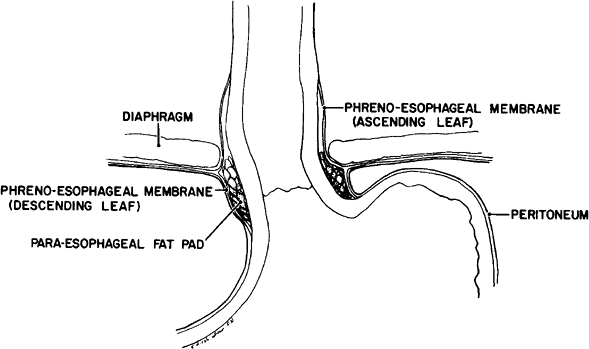 |
Fig. 123-10. Attachments and structure of the phrenoesophageal membrane. |
At the gastroesophageal junction, the outer longitudinal muscle fibers of the esophagus are continuous with the outer longitudinal muscle fibers of the stomach, while the inner circular fibers of the esophagus interlace with and are eventually replaced by the inner oblique gastric fibers that arise in the direction of the gastric fundus (Fig. 123-11). For a distance of 1.5 cm caudad from the insertion of the upper phrenoesophageal membrane, the muscular wall of the stomach gradually becomes thicker because of increased density of the esophageal circular musculature on the lesser curvature side and the gastric oblique musculature on the greater curvature side. The line of maximal muscular thickness has an oblique orientation so that, on the greater curvature side, it is more cephalad than on the lesser curvature side. It is also asymmetric in that the muscle mass on the side of the greater
P.1891
curvature is larger (Fig. 123-11). The function of this asymmetric oblique muscle thickening is difficult to determine, but Liebermann-Meffert and associates (1979) pointed out some relationships of interest. First, the manometrically defined, lower esophageal high pressure zone is located in this area. Second, the length of the high pressure zone is similar to that of this area of thickening. Third, the highest pressure recorded in the high pressure zone is found in the area of the greatest muscle thickening. Based on these observations, it has been proposed that this muscle thickening might, at least in part, coincide with the lower esophageal sphincter. Although some researchers ascribe a role in the antireflux mechanism to this muscular arrangement, other factors contribute to the closing mechanism of the lower esophageal high pressure zone. These factors include the segment of esophagus and stomach as described that is subject to the intraabdominal pressure, the rosettelike configuration of the gastric mucosa at the gastroesophageal junction, the sharp angle between the lower esophagus and the gastric fundus, and the phrenoesophageal membrane and its attachments to the esophageal hiatus at the diaphragm. None of these latter structures, however, can be considered to function as a definite anatomic sphincter.
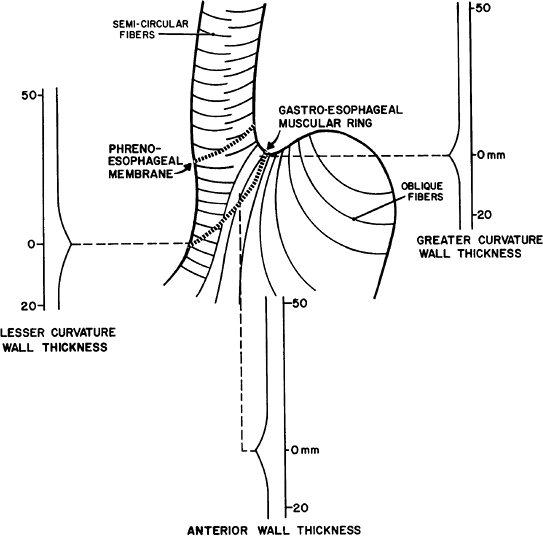 |
Fig. 123-11. The inner muscular fiber arrangement, and muscular thickness at the cardia. Adapted from Lieberman-Meffert D, et al: Muscular equivalent of the lower esophageal sphincter. Gastroenterology 76:31, 1979. With permission. |
MUSCULATURE OF THE ESOPHAGUS
The upper 2 to 6 cm of the esophagus contains only striated muscle fibers. From there on, smooth muscle fibers gradually become more abundant, such that at a distance of 4 to 8 cm from the superior end, or at the junction of the upper and lower two thirds, smooth muscle normally constitutes 50% of the esophageal muscle mass. From this point downward, smooth muscle gradually replaces the striated muscle completely. Because most of the clinically significant esophageal motility disorders involve only the smooth muscle, their effects on esophageal function are maximal in the lower two thirds of the esophagus. In addition, when a surgical esophageal myotomy is indicated, the incision usually needs only to extend this distance.
The musculature of the esophagus can be divided into an outer longitudinal and an inner circular layer. The longitudinal muscle fibers originate from a cricoesophageal tendon arising from the dorsal upper edge of the anteriorly located cricoid cartilage. The two bundles of muscles diverge and meet in the midline on the posterior wall of the esophagus about 3 cm below the cricoid (see Fig. 123-5). From this point on, a layer of longitudinal muscle fibers covers the entire circumference of the esophagus. This configuration of the longitudinal muscle fibers around the most proximal part of the esophagus leaves a V shaped area in the posterior wall covered only with circular muscle fibers. In the upper one third of the esophagus, the longitudinal muscle layer is thicker on the lateral surface than on the ventral or dorsal surfaces. In the lower two thirds, the longitudinal layer becomes more uniform, and its overall thickness decreases distally. The course of the longitudinal muscle fibers is that of an elongated spiral, turning to the left around one quarter of the esophageal circumference (90 degrees) as they descend.
The circular muscle layer of the esophagus is thicker than the outer longitudinal layer. These fibers run horizontally only in the isolated and retracted esophagus. In situ, their course is elliptical, spiraling with an orientation that varies according to the level of the esophagus. In the cervical portion, the highest point of the ellipse is dorsal. In the upper thoracic portion, the highest point is right lateral, while behind the heart the highest point is ventral. In the abdomen, the fibers are nearly horizontal. The arrangement of both the longitudinal and circular muscle fibers makes the peristalsis of the esophagus assume a wormlike drive as opposed to segmental and sequential squeezing. As a consequence, severe motor abnormalities of the esophagus assume a spiraling corkscrew-like pattern on the barium swallow radiograph.
ARTERIAL BLOOD SUPPLY OF THE ESOPHAGUS
The cervical portion of the esophagus receives its main blood supply from the inferior thyroid artery with smaller accessory branches from the common carotid, subclavian, and superficial cervical arteries. The thoracic portion receives its blood supply from the bronchial arteries, with 75% of individuals having one right-sided and one or two left-sided branches. Typically, two esophageal branches arise directly from the distal thoracic aorta. The upper branch is usually the shorter of the two, originating at the level of the sixth or seventh thoracic vertebra. The lower branch is longer and originates at the level of the eighth or ninth thoracic vertebra. The abdominal portion of the esophagus receives its blood supply mainly from esophageal branches of the left gastric and inferior phrenic arteries (Fig. 123-12). On entering the wall of the esophagus, the arteries assume a T shaped division to form longitudinal anastomoses, giving rise to an intramural vascular network in the muscular and submucosal layers. As a consequence of this abundant collateral network, the esophagus can be mobilized from the stomach to the level of the aortic arch without fear of devascularization and ischemic necrosis. However, caution should be exercised in extensively mobilizing the esophagus in patients who have had a previous thyroidectomy and ligation of the inferior thyroid arteries proximal to the origin of the esophageal branches.
VENOUS DRAINAGE OF THE ESOPHAGUS
Blood from the capillaries of the esophagus flows into a submucosal venous plexus and then into a periesophageal venous plexus from which the esophageal veins originate. In the cervical region, the esophageal veins empty into the inferior thyroid vein; in the thoracic region, into the bronchial, azygos, or hemiazygos veins; and in the abdominal
P.1892
region, into the coronary vein (Fig. 123-13). The submucosal venous networks of the esophagus and stomach are in continuity with each other, and in patients with portal venous obstruction, this communication functions as an important collateral pathway for portal blood to enter the superior vena cava via the azygos system.
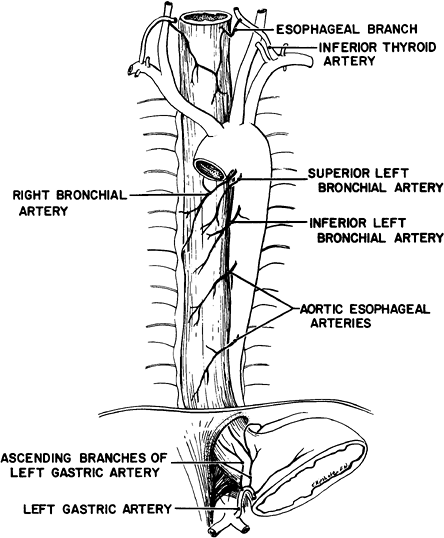 |
Fig. 123-12. Arterial blood supply of the esophagus. |
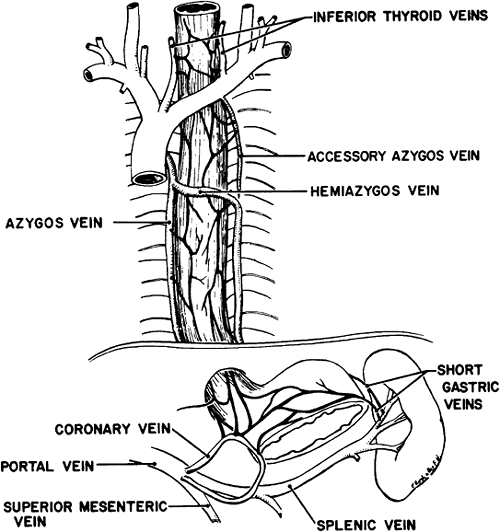 |
Fig. 123-13. Venous drainage of the esophagus. |
NERVE SUPPLY OF THE ESOPHAGUS
The constrictor muscles of the pharynx receive branches from the pharyngeal plexus, which is on the posterolateral surface of the middle constrictor muscle. This plexus is formed by pharyngeal branches of the vagus nerves, with a small contribution from the ninth and eleventh cranial nerves (Fig. 123-14). The complete parasympathetic innervation of the esophagus is provided by the vagus nerves.
The cricopharyngeal sphincter and the cervical portion of the esophagus receive their vagal innervation from branches of both recurrent laryngeal nerves. The right recurrent nerve arises at the lower margin of the subclavian artery, the left at the lower margin of the aortic arch. They both swing dorsally around these vessels and ascend in the groove between the esophagus and trachea, giving branches to each. Damage to these nerves not only interferes with the function of the vocal cords, but also interferes with the function of the cricopharyngeal sphincter and the motility of the cervical esophagus, causing a predisposition to pulmonary aspiration on swallowing.
The upper thoracic esophagus receives its vagal innervation from branches of the left recurrent laryngeal nerve and by direct branches from both vagus nerves as they descend through the superior mediastinum. The lower thoracic esophagus is innervated by the esophageal plexus located directly on both the anterior and posterior esophageal walls. This plexus is formed by fibers from both vagus nerves after they pass behind the hilum of the lung and turn medially to reach the esophagus. The esophageal plexus also receives fibers from the thoracic sympathetic chain. The left vagus nerve splits before the esophageal plexus to form two branches: the first branch runs through the ventral esophageal plexus and
P.1893
constitutes the main element of the anterior or left abdominal vagal trunk; the second branch runs around the left esophageal wall, to join the dorsal esophageal plexus, and contributes to the formation of the posterior or right abdominal vagal trunk. As a result of the intertwining of fibers from both the left and right vagus nerves in the esophageal plexus, both the left or anterior and right or posterior abdominal vagal trunks contain fibers of the original left and right vagus nerves. The average distance above the diaphragm at which the left or anterior vagal trunk becomes a single nerve is 5.13 cm, and the right or posterior vagal trunk is 3.7 cm.
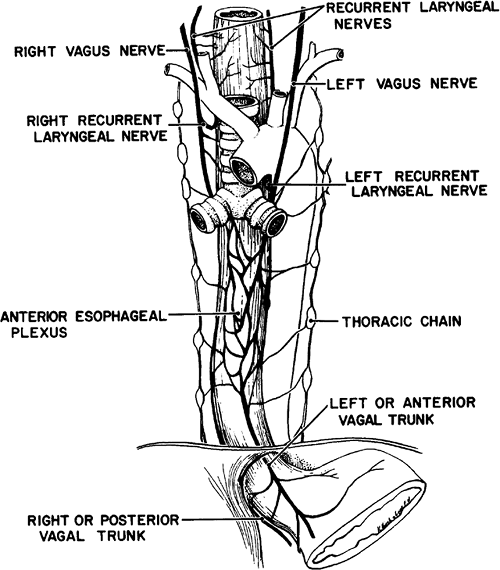 |
Fig. 123-14. Innervation of the esophagus. |
The preganglionic sympathetic fibers supplying the esophagus take origin from the fourth to the sixth spinal cord segments and terminate in the cervical and thoracic sympathetic ganglia. The pharyngeal plexus receives sympathetic fibers that arrive directly from the superior cervical ganglion via vagus nerves. The postganglionic fibers reach the esophagus via nerve branches that veer off from the cervical and thoracic sympathetic chain: some reach the esophageal wall directly, while others join the vagus trunks. Thus, the vagus nerves caudal to their entrance into the neck always contain a number of postganglionic sympathetic fibers. The distal esophageal segments also receive direct sympathetic fibers from the celiac ganglion. These fibers reach the esophagus via the periarterial plexus around the left gastric and phrenic arteries.
Afferent visceral sensory pain fibers from the esophagus end without synapse in the first four segments of the thoracic spinal cord by using a combination of sympathetic and vagal pathways. These pathways are also occupied by afferent visceral sensory fibers from the heart, which explains the frequent overlap in symptomatology between the esophagus and the heart.
LYMPHATIC DRAINAGE OF THE ESOPHAGUS
The detailed lymphatic anatomy of the esophagus and its lymphatic drainage is discussed in Chapter 124.
REFERENCES
Keith A: A demonstration on diverticula of the alimentary tract of congenital or of obscure origin. BMJ 1:376, 1910.
Liebermann-Meffert D, et al. Muscular equivalent of the lower esophageal sphincter. Gastroenterology 76:31, 1979.
Lindner HH, Kemprud E: A clinicoanatomical study of the arcuate ligament of the diaphragm. Arch Surg 103:600, 1971.
Reading References
Abel W: The arrangement of the longitudinal and circular musculature at the upper end of the oesophagus. J Anat Physiol 47:381, 1913.
Arey LB, Tremaine MJ: The muscle content of the lower esophagus of man. Anat Rec 56:315, 1933.
Bowden REM, El-Ramli HA: The anatomy of the oesophageal hiatus. Br J Surg 54:983, 1967.
Butler H: The veins of the oesophagus. Thorax 6:276, 1951.
Demel R: The blood supply of the esophagus: a study of surgery of the esophagus (Die Gefassversorgung der Speiserohre. Ein Beitrag zur Oesophaguschirurgie). Arch Klin Chir 128:453, 1924.
Eliska O: Phreno-oesophageal membrane and its role in the development of hiatal hernia. Acta Anat (Basel) 86:137, 1973.
Shapiro AL, Robillard GL: Gastroesophageal vagal and sympathetic innervation: in relation to an anatomic approach to combined gastric vagal sympathectomy. J Int Coll Surg 13:318, 1950a.
Shapiro AL, Robillard GL: The esophageal arteries: their configurational anatomy and variations in relation to surgery. Ann Surg 131:171, 1950b.
Swigart LL, et al: The esophageal arteries: an anatomic study of 150 specimens. Surg Gynecol Obstet 90:234, 1950.
EAN: 2147483647
Pages: 203