Movement Disorders and Ataxia
Authors: Flaherty, Alice W.; Rost, Natalia S.
Title: Massachusetts General Hospital Handbook of Neurology, The, 2nd Edition
Copyright 2007 Lippincott Williams & Wilkins
> Table of Contents > Adult Neurology > Movement Disorders and Ataxia
Movement Disorders and Ataxia
A. See also
Pediatric movement disorders, p. 145.
B. Terminology
Movement disorders tends to include only problems with a presumed basal ganglia cause. Extrapyramidal is a term used mostly by psychiatrists to distinguish from pyramidal, corticospinal sx.
C. Movement disorder consult service jingle
Jerky or stiff?/We're there in a jiff./Trouble with tone?/Call us on the phone.
D. H&P
What tasks are difficult? Nature and frequency of falls. Associated depression, dementia, incontinence. Alcohol, benzodiazepine, or neuroleptic use. Assess facial expression, saccades, voice, handwriting, involuntary movements, speed, amplitude, tone, ability to rise from a chair, posture, postural reflexes, gait base, arm swing, festination, freezing, turning Romberg sign, weakness, ataxia.
E. Gait disorders
Table 18. Common gait disorders. | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
F. Ataxia and dysmetria
Ataxia, dysmetria; inaccurate movement targeting and coordination, from cerebellar or brainstem disorder. Dysmetria (AKA intention tremor) is an oscillation that worsens as the limb approaches the target. In postural muscles, it is called ataxia; in eye movements, nystagmus.
1. Acute: Often with vertigo, nystagmus, N/V. From drugs, post fossa bleed/stroke. Secondary edema may need rapid decompression.
2. Subacute: From drugs, tumor, postinfectious cerebellitis, vasculitis.
3. Chronic progressive: Alcoholism, Wilson's dz, drugs, toxins, CJD, hereditary, hereditary metabolic dz, paraneoplastic syndromes.
4. DDx: Action tremor; other gait disorders (see above).
P.75
G. Hereditary ataxias and movement disorders
leaves out most recessive dzs, genes for dzs that are usually sporadic (e.g., PD), and very, very rare dzs (all are rare).
1. Trinucleotide repeat diseases: Typically adult onset. Dzs caused by CAG repeats sometimes show anticipation; in successive generations, repeat length is longer, age of onset is younger, and severity is greater.
2. Genetic testing: Pts often request testing of at-risk relatives. Especially in dzs where preventive rx is not available, strongly urge, even insist, that they see a professional genetic counselor first to discuss emotional and economic risks (e.g., that a positive test may affect health insurance access).
Table 19. Hereditary disorders causing ataxia, chorea, or weakness.
Disease1 Sx2 Triplet? Transmitted3 Comments Friedreich's A + AR Heart, DM Huntington's M,P + AD Firsttsx may be psych. SCA1 A,W,N,P + AD Usually pure ataxia SCA2 N,P + AD Slow saccades SCA3 (MJD) A,N + AD Dystonia, spasticity SCA6 (SBMA) A + AD Usually pure ataxia SCA7 (OPCA) A,N + AD Retinal degeneration DRPLA A,M,P + AD Pedi myoclonic epilepsy Myotonic dyst. W,P + AD Heart, DM Fragile X P + XL Long face, big testes Wilson's A,M,P AR Liver dz DRD M ADi Sx best in AM DYT-1 M ADi Pure dystonia 1SCA = spinocerebellar ataxia; MJD = Machado-Joseph's disease; SBMA = spinobulbar
muscular atrophy (Kennedy's syndrome); OPCA =olivopontocerebellar atrophy; DRPLA = dentatorubral
- pallidoluysian atrophy; DRD = dopa - responsive dystonia; DYT - 1 = primary
dystonia.2 A = ataxia; M = Mvt disorder; W = weak; P = psychological/cognitive. 3AD = autosomal dominant; ADi = with incomplete penetrance; AR = autosomal recessive;
XL = X - linked
H. Basal ganglia movement disorders
Impair starting, stopping, sequencing.
1. Hypokinetic disorders: Slow movements; subcortical cognitive problems (q.v. Table 8, p. 43), poor motivation, depression.
a. Causes: Decreased dopamine or lesion of the direct pathway (excitatory) through the internal pallidum.
b. Sx: Rigidity, bradykinesia, rest tremor.
c. Rx: Dopaminergics, anticholinergics
P.76
2. Hyperkinetic disorders: Excessive, rapid movements; also delusions, agitation, impulsivity.
a. Causes: Lesions that raise dopamine or that affect the indirect (inhibitory) pathway through the external pallidum.
b. Sx: Chorea, dyskinesia, tics, athetosis, akathisia.
c. Rx: Typical neuroleptics (D2-blockers).
3. Mixed disorders: Dystonia
I. Akathisia
Motor restlessness. May be excruciating. Often a transient neuroleptic SE or after neuroleptic d/c. Try benztropine 0.5-1 mg bid, propranolol 10-20 mg tid, clonidine 0.1 mg bid, or clonazepam 0.5-1.0 mg bid.
J. Asterixis
Irregular, slow, tremor-like flapping of hands, trunk, from temporary lapses of tone. Treat underlying cause usually metabolic, e.g., liver failure.
K. Choreoathetosis
Chorea is involuntary, rapid movements, often incorporated into voluntary movements. Athetosis is slower, more writhing.
1. Causes of choreoathetosis:
a. Chemicals: Especially neuroleptics.
b. Immune-mediated: Sydenham's, SLE, chorea gravidarum .
c. Hereditary disorders:
1) Huntington's dz: Autosomal dominant CAG sequence repeat, genetic test available. Presents usually in adulthood with chorea or psychiatric sx.
d. Other: Huntington's, Wilson's, Hallervorden-Spatz dz, idiopathic torsion dystonia .
2. Rx of choreoathetosis: Typical neuroleptics (via D2 receptor antagonism), e.g., haloperidol: start 0.5 mg bid, up to 8 mg bid. Atypical neuroleptics work only to the extent of their D2 antagonism, so you usually need higher dose.
L. Dyskinesia
Reserved for chorea caused by dopamine receptor hypersensitivity. See Parkinsonian dyskinesias (p. 77); Tardive dyskinesia (p. 171).
M. Dystonia
Involuntary maintenance of abnormal posture, expression, or limb position. Often task dependent and relieved by sensory tricks (gestes antagonists).
1. DDx: Spasticity, musculoskeletal lesion .
2. Acute dystonia: Reaction to antiemetic or neuroleptic, carbon monoxide, stroke, etc. Rx: diphenhydramine 50 mg IV/IM.
3. Chronic dystonia:
a. Focal: Torticollis, blepharospasm, writer's cramp, spasmodic dysphonia (q.v.), Meige's syndrome (lip smacking and blepharospasm) .
1) Rx: Botulinum toxin injections q 3-4 mo; perhaps clonazepam or anticholinergic.
b. Generalized: See Causes of choreoathetosis, above; pediatric dystonia, p. 146. Genetic tests available. Rx:
1) Always try levodopa/carbidopa to r/o dopa-responsive dystonia.
2) Anticholinergics: E.g., trihexyphenidyl. Start 0.5 mg qhs, may need 20-50 mg tid.
3) Other: Baclofen, clonazepam, pallidal deep brain stimulator.
P.77
N. Myoclonus
Brief, monophasic, irregular jerks in different body parts. Often triggered by sensory stimuli.
1. DDx: Tics, myoclonic epilepsy, periodic limb movements of sleep, tremor, chorea.
2. Causes: Metabolic or hypoxic encephalopathy, seizure, benign essential myoclonus, physiological myoclonus (sleep jerks), drugs (e.g., opiates) .
3. Rx: Clonazepam: start 0.5 mg tid, to 2 mg tid. Valproate ER: start 250 mg qhs, to 500-1,000 mg bid.
O. Neuroleptic-induced movement disorders
see p. 170.
P. Serotonin-induced movement disorders
see p. 164.
Q. Idiopathic Parkinson's dz (IPD)
Must distinguish IPD from atypical parkinsonism, below.
1. H&P: Bradykinesia, rigidity, tremor are cardinal. Falls, stooping, festination, response to carbidopa/levodopa, depression, cognitive changes, hallucinations, orthostasis, autonomic dysfunction.
2. Tests: Levodopa/carbidopa challenge is nearly diagnostic for IPD. MRI only rules out rare causes. Fluorodopa PET is rarely done.
3. Cause: Dopamine idiopathic Parkinson's dz (IPD). Must distinguish IPD from atypical parkinsonism, below.
4. Rx of early/moderate dz: Start all meds slowly, with meals, to avoid N/V. See also Dopaminergic Drugs, p. 169.
a. Medication-induced nausea: Take meds with meals. Extra carbidopa 25 mg, or ondansetron 1 mg, before dose. AVOID metoclopramide, prochlorperazine, etc. Med nausea passes in months.
b. Precursor: Levodopa/carbidopa 25/100 mg tid, or much higher.
1) Levodopa does not worsen dz progression but is commonly perceived to.
2) Minimize dose fluctuations to decrease receptor hypersensitization and dyskinesias.
c. COMT inhibitors: E.g., entacapone; prolong DA half-life.
d. Dopamine agonists: E.g., pramipexole. More sedation and hallucinations but longer half-life and less link to dyskinesias than levodopa.
e. MAO-B inhibitors: E.g., selegiline, rasagiline. Safer than the MAO-A inhibitors used as antidepressants.
f. Antioxidants: Initial studies show sx slowed by coenzyme Q10 at doses >1,200 mg divided daily. No evidence for vitamin E.
5. Rx of complications:
a. Constipation: Bowel stimulant, e.g., senna, milk of magnesia.
b. On-off dose fluctuations: Use smaller, more frequent levodopa doses, partial replacement with an inhibitor or agonist.
c. Meal-related changes: Take levodopa on an empty stomach, and avoiding its CR form, to enhance absorption.
d. Dyskinesias: Amantadine 100 mg tid, or clozapine.
e. Off-phase dystonia: Artane 2 mg tid.
f. Hallucinations or nightmares: Quetiapine 25 mg qhs, but it may worsen severe rigidity. Clozapine 12.5-25 mg qhs is safe and underused.
g. Orthostatic BP: Consider high-salt diet, head of bed up 10 degrees (place bricks under bed), fludrocortisone 0.1 mg qd, or midodrine 10 mg tid.
h. Subthalamic nucleus deep brain stimulator (DBS): Actually, the current DBS inhibits or jams STN function to decrease PD sx. Pts can turn on/of and sometimes adjust the current DBS. For questions, call 1-800-328-0810.
1) Indication: Medical rx failed. Strong levodopa effect is best prognostic sign DBS does not help PD-plus. Alzheimer's type cortical dementia is a contraindication, but PD-related executive dysfunction (see p. 150) is not.
2) If pt is too rigid: Have them check if DBS is on; increase voltage using their access device, increase PD meds.
3) If pt is dyskinetic/dystonic: Decrease or turn off DBS; decrease PD meds.
4) MRIs with DBS: Voltage must be turned to zero by a trained provider not just turned off by the pt. Can only do head scans on some scanner brands and can never do body scans.
5) EKGs with DBS: If there is interference, have pt shut off DBS with their access device.
6) Surgery with DBS: Usually safe, use bipolar cautery with pad far from head.
P.78
6. DDx:
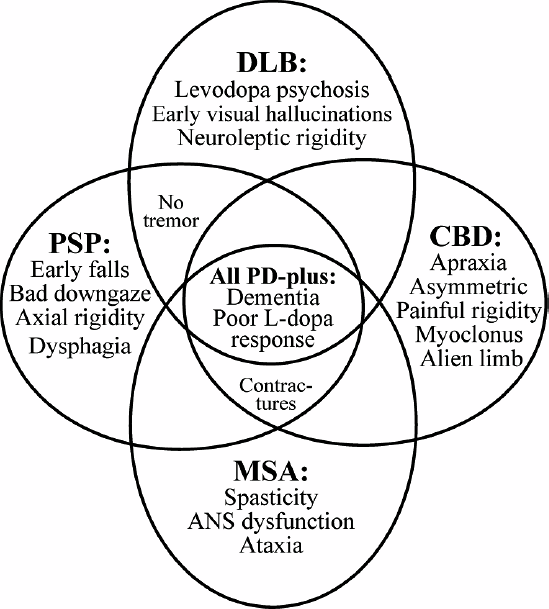
Figure 9. Symptom overlap in syndromes of atypical parkinsonism. Abbreviations are defined in the following text.
P.79
a. Atypical parkinsonism, AKA Parkinson's plus syndromes : All share poor levodopa response, early dementia.
1) Major subtypes: In clinical practice, the symptom complexes overlap. See Figure 9. Progressive supranuclear palsy (PSP), diffuse Lewy body dz (DLB), corticobasoganglionic degeneration (CBD), and multiple systems atrophy (MSA).
2) MSA subtypes: MSA itself includes Shy-Drager syndrome (more ANS dysfunction), striatonigral degeneration (more spasticity), and olivopontocerebellar atrophy (more ataxia).
3) Rx: Symptomatic. High-dose levodopa may help for awhile.
b. Drug-induced parkinsonism: All neuroleptics except clozapine and this includes most antiemetics except ondansetron cause reversible parkinsonism and may unmask latent true IPD.
c. Chemicals: Rotenone, manganese, carbon monoxide, and others can cause irreversible parkinsonism.
d. Other: NPH, essential tremor, depression, arthritis, focal basal ganglia lesions, spasticity, postencephalitic, CJD .
R. Tone
1. Rigidity: Lead-pipe resistance to passive movement, from basal ganglia lesion. Rigid pts are strong, if given enough time to reach full power.
2. Spasticity: Clasp-knife stiffness, weakness, and spasms. From corticospinal tract lesions.
S. Tics
Quick, repetitive, coordinated movements or vocalizations, driven by urge, partly repressible.
1. DDx: Tourette's syndrome, Sydenham's chorea, Wilson's dz, Lesch-Nyhan's syndrome, myoclonus .
2. Rx: (generally not well tolerated)
a. Clonidine (central -agonist): Start 0.05 mg qd, to 2 mg bid.
b. Pimozide (or other D2-blocker): Start 0.5 mg qhs, to 8-16 mg qd.
T. Tremor
Oscillation from alternating contraction of antagonist muscles.
1. Tests: TSH; consider copper studies.
2. DDx: Focal seizure, segmental myoclonus, chorea.
3. Rest (parkinsonian) tremor: 3-5 Hz, decreases during movement, often asymmetric, pill-rolling.
4. Action tremors: Worse with movement.
a. Physiologic tremor: 8-13 Hz, low amplitude. Normal. Worse with adrenergic stimulation (anxiety, caffeine, hyperthyroidism, sedative withdrawal, etc.).
b. Essential (benign) tremor: 4-8 Hz. Genetic. Rx includes:
1) Propranolol: Start 10-20 mg tid, to 60-200 mg qd.
2) Primidone: Start 50 mg qd, to 125 tid.
3) Surgery: Thalamic deep brain stimulator.
c. Cerebellar tremor: Strictly, dysmetria. Oscillations worsen as limb approaches target.
d. Rubral tremor: Midbrain tremor would be a better term. Violent beating or flapping.
e. Hemiballism from a subthalamic nucleus lesion. Looks rubral. Often from small stroke.
f. Anxiety/depression and tremor: Mirtazapine (Remeron) is one of the few antidepressants that does not worsen tremor.
g. Bipolar or mood lability: Change lithium, valproate, or lamotrigine to carbamazepine, gabapentin, or Topamax or, in severe cases, clozapine (can suppress tremor and raise mood).
h. Epilepsy and tremor: Valproate, carbamazepine, gabapentin.
P.80
EAN: 2147483647
Pages: 109