17. The Liver
Authors: Corwin, Elizabeth J.
Title: Handbook of Pathophysiology, 3rd Edition
Copyright 2008 Lippincott Williams & Wilkins
> Table of Contents > Unit V - Nutrition, Elimination, and reproductive function and dysfunction > Chapter 17 - The Liver
Chapter 17
The Liver
The liver lies in the upper right quadrant of the abdominal cavity and is the largest organ in the body. The functions of the liver are diverse and essential and depend on the liver's unique blood flow system and its specialized cells (Table 17-1). When the liver is damaged, all body systems are affected.
Physiologic Concepts
Structure
The liver is encased in a fibroelastic capsule called Glisson's capsule and is grossly separated into right and left lobes. Glisson's capsule contains blood vessels, lymph vessels, and nerves. The two liver lobes consist of many smaller units called lobules. The lobules contain the liver cells (hepatocytes) that line up together in plates. The hepatocytes are considered to be the functional units of the liver. Liver cells are capable of cell division and readily reproduce when needed to replace damaged tissue.
Hepatic Blood Flow and Pressure
The liver receives its blood supply from two different sources. Most liver blood flow, approximately 1000 mL/min, is venous blood draining from the stomach, the small and large intestines, the pancreas, and the spleen. This blood comes to the liver via the portal vein. Because it is venous blood, it is poorly oxygenated but has a rich supply of nutrients, including
P.575
glucose, which the liver can convert into glycogen and immediately store. The blood may also contain intestinal bacteria, toxins, and ingested drugs. The other source of blood for the liver enters via the hepatic artery at a flow rate of approximately 500 mL/min. This is arterial blood and well saturated with oxygen. After perfusing the liver, both blood sources drain into the liver capillaries, called sinusoids. From the sinusoids, blood drains into a central vein in each lobule and from there into the hepatic vein. The hepatic vein empties into the inferior vena cava.
Table 17-1. Functions of the Liver | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
In healthy individuals, there is virtually no resistance to the flow of blood in the portal vein. As a result, blood pressure in the portal venous system is low, approximately 3 mmHg. Blood flows easily out of the liver into the vena cava as well, where pressure is nearly 0 mmHg.
Metabolic Functions of the Liver
Metabolism refers to the cellular processes that occur when basic food molecules (sugars, amino acids, and fatty acids) are built into cell structures or energy stores and are broken down later to run cell functions. The buildup of cell structures and energy stores is called anabolism; the breakdown is called catabolism. The cells of the liver are key components in the interplay between anabolism and catabolism.
P.576
Glucose Handling by the Liver
After glucose is digested and absorbed into the bloodstream, it is delivered to all cells of the body to be used as an energy source. As discussed in Chapter 16, insulin is required for glucose to gain entry to most cells. If glucose is unnecessary for immediate energy, it can be stored in cells as glycogen. The liver is especially capable of storing large amounts of glucose as glycogen. Because the liver can store glycogen, it acts as a glucose buffer for the blood. When glucose levels rise in the blood, the liver's conversion of glucose to glycogen and the storage of glycogen increase. Glycogen formation, called glycogenesis, occurs in the absorptive phase of digestion, which is the period soon after a meal when glucose levels are high. Glycogenesis is insulin dependent. By increasing the conversion and storage of glucose in times of excess, the liver returns plasma glucose levels toward normal.
In times of fasting or between meals, the breakdown of glucagon to glucose occurs in the liver, again serving to normalize circulating levels of glucose. The breakdown of glycogen is called glycogenolysis. In addition, when glucose levels decrease between meals, the liver initiates gluconeogenesis (the new formation of glucose) to keep blood glucose levels constant. Gluconeogenesis is accomplished in the liver by conversion of amino acids to glucose after deamination (removal of the amino group) and by conversion of glycerol, a product of fatty acid breakdown, to glucose. The breakdown of glycogen and the formation of glucose occur in the postabsorptive phase of digestion, the time between meals when external food sources are not readily available. The postabsorptive stage of digestion is under the control of the pancreatic hormone glucagon and other gastrointestinal hormones, as discussed in Chapter 15.
![]() ediatric Consideration
ediatric Consideration
Infants and children are particularly dependent on fatty acid oxidation during periods of fasting as a result of reduced glycogen storage, immature activity of enzymes involved in glycolysis and gluconeogenesis, and increased basal metabolic needs. Ketone bodies are produced and can serve as alternative fuel for cardiac and skeletal muscles. Excess ketones, however, can lower blood pH.
Amino Acid Handling by the Liver
After digestion, amino acids enter all cells and are converted to proteins to be used by the cells to make either enzymes or structural components such as ribosomes, collagen, or muscle contractile proteins. Although a variety of organs (including the kidney and intestinal mucosa) participate in the storage of extra amino acids as proteins, the liver is the major storage tissue for protein. When amino acids are needed, the breakdown of stored protein occurs, and free amino acids are liberated. A decrease in
P.577
plasma amino acids below a certain level triggers the breakdown of stored proteins.
All cells, including liver cells, have limits on how much protein they can store. When no further amino acids can be stored as protein, the liver deaminates the extra amino acids and either uses the products as energy or changes them into glucose, glycogen, or fatty acids. These substances can be stored in the liver glucose as glycogen and fatty acids as triglycerides (fat). Fatty acids can also be stored in other cells of the body, especially adipose tissue.
During deamination of amino acids, ammonia is released. It is almost entirely converted in the liver to urea, which is then excreted by the kidneys.
Fatty Acid Handling by the Liver
Nearly all digested fats are absorbed into the lymphatic circulation as chylomicrons conglomerates of triglycerides, phospholipids, cholesterol, and lipoprotein. The chylomicrons are delivered by the lymph to the thoracic duct, where they join the systemic circulation. Triglycerides are subsequently changed back into fatty acids and glycerol by enzymes in the walls of all capillaries, especially the capillaries that serve the liver and the adipose tissue. From the capillaries, fatty acids and glycerol can diffuse into most cells.
Once inside the liver and other cells, fatty acids and glycerol again combine to form triglycerides. Triglycerides are stored until needed during the postabsorptive stage. At this time they may be metabolized back to glycerol and free fatty acids. Glycerol and fatty acids can enter the Krebs cycle to produce ATP, so that cells are provided with energy. Elevations in the hormones glucagon, cortisol, growth hormone, and the catecholamines signal cells to break down stored triglycerides into free fatty acids and glycerol.
Instead of directly entering the Krebs cycle, some glycerol and free fatty acids may be used by the liver to produce new glucose. This can result in the production of ketones when triglyceride breakdown is excessive. The brain itself cannot use free fatty acids directly for energy production. Therefore, the liver's conversion of fats to glucose (gluconeogenesis) is essential for supporting the energy needs of the brain when glucose levels are low.
Cholesterol Handling by the Liver
Cholesterol is a lipid substance produced by the liver and used in the digestion of fat. During digestion, cholesterol is packaged with bile salts, phospholipids, and the triglycerides into small suspensions called micelles. Once the triglycerides are suspended as micelles, they can be digested by pancreatic enzymes and absorbed into the bloodstream. The cholesterol from the micelles is recirculated to the liver. The liver metabolizes some of the cholesterol and recycles it to be used again in digestion. The remainder is complexed with phospholipids and released into the bloodstream as
P.578
lipoproteins. As lipoproteins, cholesterol is carried to body cells to be used for the production of cell membranes, intracellular structures, and steroid hormones. High levels of two types of lipoproteins, low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL), suggest that the liver is handling high amounts of cholesterol. These types of lipoproteins may injure cells, including the endothelial cells lining the arteries, by releasing oxygen free radicals and high-energy electrons during their metabolism. High-density lipoprotein (HDL), on the other hand, carries cholesterol away from cells to the liver and protects against arterial disease.
Bile Secretion
Bile is made by all hepatocytes and consists of water, bile salts, bilirubin, cholesterol, fatty acids, lecithin, and electrolytes. Except for water, the most abundant substance in bile is bile salt. Bile salts are synthesized in the liver from cholesterol that either has been delivered to the liver from the small intestine or synthesized directly by the liver in the process of fat metabolism. All hepatic cells participate in making bile and each secretes bile into the small bile canaliculi that surround all liver cells. The canaliculi empty into progressively larger ducts that ultimately join into the hepatic duct and common bile duct. These ducts deliver bile either to the gallbladder for storage or into the intestine directly. Bile salts function in the digestion of fat (see Chapter 15) and are normally recycled after use in the small intestine. Without bile, as much as 40% of fats in the diet would not be absorbed across the intestine and so would be lost in the stool. The absorption of fat-soluble vitamins across the small intestine would be similarly affected. For example, without bile, a vitamin K deficit would occur and be apparent in less than a week. Without adequate vitamin K, blood coagulation would be impaired.
The liver also functions in the handling of another component of bile, bilirubin. Bilirubin is formed as an end product of hemoglobin breakdown and must be metabolized by the liver for it to be excreted.
Metabolic Biotransformation
The liver has an important role in transforming biologic substances that may be toxic at high levels or that cannot be excreted from the body without transformation. Substances acted upon in this manner by the liver may include both those ingested by an individual as well as those produced by the body itself. Examples of substances that are transformed by the liver include bilirubin, various hormones, drugs, and toxins. Metabolic biotransformation is also referred to as metabolic detoxification.
Bilirubin Biotransformation
Bilirubin is a product of red blood cell breakdown. When a red blood cell has lived out its 120-day life span, the cell membrane becomes fragile and
P.579
ruptures. Hemoglobin is released and is acted upon by circulating phagocytic cells to form free bilirubin. Free bilirubin binds to plasma albumin and circulates in the bloodstream to the liver.
Free bilirubin is considered unconjugated in that, although it is bound to albumin, the binding is reversible. Once in the liver, bilirubin releases from albumin and, because free bilirubin is lipid soluble, moves easily into the hepatocytes. Once inside the hepatocytes, bilirubin is rapidly bound to another substance, usually glucuronic acid, and is now considered conjugated. Conjugated bilirubin is water soluble, not lipid soluble.
Most conjugated bilirubin is actively transported into the bile canaliculi. From there it is delivered along with the other components of bile to the gallbladder or small intestine. A small amount of conjugated bilirubin does not go to the intestine as a bile component, however, but rather is absorbed back into the bloodstream. Therefore, in the bloodstream, there is always a small amount of conjugated bilirubin present, along with unconjugated bilirubin on its way to the liver.
Once in the intestine, conjugated bilirubin is acted upon by bacteria and changed into urobilinogen. Most urobilinogen enters the bloodstream and is excreted by the kidneys in the urine, some is excreted in the stool, and some is recycled back to the liver in the enterohepatic (intestinal to liver) circulation. Figure 17-1 shows the steps involved in the conjugation and excretion of bilirubin.
The conjugation of bilirubin is essential for its excretion. Without conjugation, bilirubin cannot be excreted by either the kidneys or the intestines. The handling of bilirubin by the liver is a form of metabolic detoxification. Without conjugation, unconjugated bilirubin would build up in the bloodstream to toxic levels.
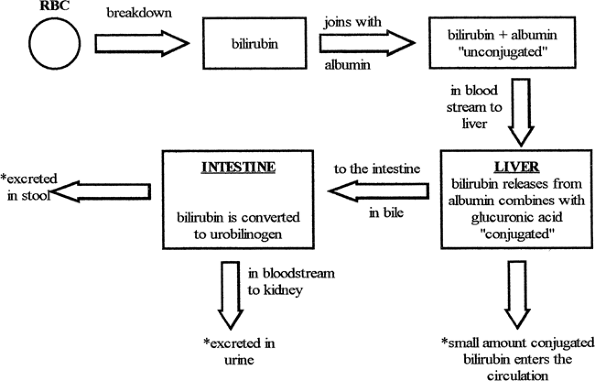 |
Figure 17-1. Conjugation of bilirubin. |
P.580
Hormone Biotransformation
The liver inactivates or modifies many hormones of the body. It acts on steroid hormones, including cortisol, estrogen, testosterone, progesterone, and aldosterone, to make them water soluble rather than lipid soluble, allowing them to be excreted. If this biotransformation does not occur, these hormones tend to concentrate in the body and build up in tissues, especially adipose tissue.
Liver proteases inactivate or deaminate other hormones such as insulin, glucagon, and anti-diuretic hormone (ADH, also called vasopressin). Thyroxine is deiodinated and inactivated. These actions allow the hormones to be excreted from the body.
Ammonia Biotransformation
Ammonia is a by-product of protein breakdown. It is transformed into urea in the liver and excreted in the urine. Without this liver function, ammonia levels build up in the blood and cause neurological dysfunction and possibly coma and death.
Drug and Toxin Metabolism
Drugs and toxins often are modified by the liver to be either inactivated or made water soluble by conjugation with another chemical compound. By these processes, the liver permits the body to excrete these substances. Without good liver function, many drugs and toxins accumulate in the body. Moreover, many of the chemical compounds used by the liver to conjugate lipid-soluble drugs and toxins, such as plasma proteins, are themselves synthesized by the liver. Therefore, they are in inadequate supply in the case of a poorly functioning liver.
Alcohol Handling by the Liver
Alcohol is an example of a drug that is primarily metabolized by the liver. Alcohol metabolism follows two pathways in the liver. The first pathway uses the enzyme alcohol dehydrogenase and results in the end-product of acetaldehyde. Acetaldehyde is then changed to acetate and hydrogen ions. These reactions occur in the cytoplasm and the mitochondria of the hepatocyte.
The second metabolic pathway, called the microsomal ethanol oxidizing system (MEOS) pathway, named after the specific enzymes involved, occurs in the endoplasmic reticulum of the hepatocyte and is primarily used in the liver of individuals who have a long history of alcohol abuse. This pathway results in the production of acetaldehyde and free radicals. The free radicals and the acetaldehyde produced by either metabolic pathway are highly damaging to liver cells.
The MEOS pathway is also damaging to an individual because one of the enzymes required for running this pathway, cytochrome P450, is
P.581
essential in the liver's transformation of many other toxins and drugs and excess fat-soluble vitamins. If this enzyme is preferentially used to detoxify alcohol, it is unavailable for its other roles. Thus, long-term alcohol abusers are susceptible to damage from many different toxins and drugs, and to the toxic effects of some vitamins.
Another coenzyme in alcohol metabolism is nicotinamide adenine dinucleotide (NAD). This coenzyme is also required for many other metabolic processes, including running the Krebs cycle to metabolize nutrients, making ATP, and allowing the liver to perform gluconeogenesis. Without NAD, hypoglycemia and lactic acid accumulation may develop. Hypoglycemia is a significant problem for many long-term alcohol abusers who typically have poor diets. Lactic acid accumulation can contribute to gout because increased lactic acid decreases the renal excretion of uric acid.
Blood Storage in the Liver
The liver is a storage organ for blood. If blood volume decreases, for example, during a hemorrhage, the liver can release blood to the circulation. Likewise, the liver can increase its blood storage if volume is significantly increased or if blood backs up in the peripheral circulation in response to a failing right heart. The amount of blood stored at any one time varies depending on an array of cardiovascular indices, but it may be as much as 400 to 500 mL.
Plasma Protein Synthesis
The liver is responsible for synthesizing plasma proteins, including albumin. The albumin concentration in the plasma is the main source of plasma osmotic pressure, the primary force causing reabsorption of fluid from the interstitial space into the capillary (see Chapter 13). If the liver is incapable of making adequate amounts of plasma proteins, osmotic pressure in the capillary will be low, and plasma filtered out at the start of the capillary will not flow back in by the time the capillary reforms to a venule. Therefore, swelling and edema of the interstitial space will occur.
Clotting Factor Synthesis
The liver functions in the production of several clotting factors, including factors I (fibrinogen), II (prothrombin), and VII (proconvertin). Without adequate production of these substances, blood clotting is impaired and bleeding may be extensive. In addition, vitamin K is a fat-soluble vitamin required for the formation of these and other clotting factors. Because bile salts are required for across-the-gut absorption of all fat-soluble vitamins, liver dysfunction resulting in decreased synthesis or supply of bile to the intestine can also lead to bleeding problems.
P.582
Immunologic Function
The many capillaries of the liver are called sinusoids. Blood flow in the sinusoids is a mixture of venous blood from the portal vein and arterial blood from the hepatic artery. The sinusoids are lined with phagocytic macrophage cells called Kupffer's cells. These cells remove bacteria, dead cells, and other foreign substances from the blood, especially the portal blood, flowing into the liver from the intestines.
Storage of Vitamins and Minerals
The liver has the capability to store vitamins B12, D, and A. Iron is stored in the liver as ferritin. The vitamins and iron can be released to the body from the liver when circulating levels decrease.
Tests of Liver Function
Tests of liver function are frequently performed. Some of the most common ones include:
Measurement of total bilirubin, as well as separate levels of conjugated and unconjugated bilirubin. Levels increase in various combinations with liver disease.
Measurement of liver enzymes, including serum glutamic pyruvic transaminase (SGPT), serum glutamic oxaloacetic transaminase (SGOT), and alkaline phosphatase. Levels increase with liver disease.
Measurement of plasma protein concentration. Levels decrease with liver disease.
Measurement of prothrombin time (a test of coagulation). Because coagulation depends on adequate liver production of coagulation factors, prothrombin time increases with liver disease.
Ultrasound, computed tomography (CT) scan, and magnetic resonance imaging (MRI) can indicate structural defects or stones in the bile duct or gallbladder.
Liver biopsy allows tissues to be observed directly for confirmation of infection, fatty infiltration or fibrosis, and cancer.
Pathophysiologic Concepts
Portal Hypertension
Portal hypertension is excessively high pressure in the portal vein. Normal portal venous pressure is approximately 3 mmHg. Pressure greater then 9 to 10 mmHg in the portal vein is considered portal hypertension. Portal hypertension develops when the resistance to blood flow through or out of the liver is high. Excessive blood flow going into the liver can also lead to portal hypertension.
P.583
Effects of Portal Hypertension
With the development of portal hypertension, blood normally going into the liver via the portal vein begins to bypass the liver in search of alternative routes that offer less resistance to flow. This bypass can result in collateral vessels opening from the portal vein to other lower-resistance vessels. When blood bypasses the liver, the hepatocytes cannot maintain their essential functions of biologic transformation, detoxification, and metabolism of foodstuffs. In addition, the opened collateral circulations frequently cannot handle the increased blood flow, and third spacing results (described below).
Causes of Portal Hypertension
Portal hypertension may develop if there is obstruction to flow through or out of the liver. Obstruction to flow through the liver can occur as a result of fibrosis and scarring of the liver, conditions that occur with repeated infections, or long-term liver disease such as cirrhosis. Obstruction to flow through the liver can also result from acute or chronic inflammation because swelling and edema in the interstitial space which occurs as part of the processes of inflammation provide resistance to blood flow. Hepatitis is an infection of the liver that is associated with acute or chronic inflammation. Likewise, a thrombus in the portal vein itself can block blood flow through the liver. If blood flow through the liver is impeded by any cause, portal pressure increases and portal hypertension can develop.
Obstruction to flow out of the liver can occur if there is a thrombus (arterial buildup) or an embolus (blood clot) in the hepatic vein draining the liver. Likewise, anything that blocks flow through the vena cava or into or out of the right side of the heart, including right-heart failure, cardiac myopathy, and pericarditis, can cause blood to back up into the liver, increasing the pressure in the portal venous system.
Third Spacing
Third spacing refers to fluid, primarily water, filtered from the plasma. This fluid accumulates in areas of the body other than inside cells or in the vascular system.
Types of Third Spacing
There are two types of third spacing that occur with liver pathology: ascites and interstitial edema. Ascites is the accumulation of serous (serum-like) fluid in the peritoneal cavity. The peritoneal cavity includes the abdominal cavity and the pelvic region up to the underside of the diaphragm, excluding the kidneys. The peritoneal cavity is lined by a thin membrane called the peritoneum.
Ascites usually occurs as a result of portal hypertension. With high resistance to blood flow through the liver, blood flow is diverted to mesenteric
P.584
(abdominal-peritoneal) vessels. The increased flow causes increased capillary pressure in these vessels of the abdominal cavity, resulting in net filtration of fluid out of the vessels and into the peritoneal cavity. In addition, high pressure in the liver itself causes fluid to ooze across the liver into the peritoneal cavity. This fluid contains a high concentration of albumin. The loss of albumin from the vascular compartment (the blood) in ascites contributes to the depletion of blood proteins seen with advanced liver disease. It also contributes to the decrease in plasma osmotic pressure, leading to the development of interstitial edema.
Interstitial edema occurs throughout the body with advanced liver disease. It occurs as a direct result of the loss of serum albumin in ascites and from impaired protein synthesis. If plasma protein concentration is reduced, the force favoring reabsorption of fluid into all capillaries from the interstitial space is reduced, and edema of the interstitial compartment occurs (see Chapter 13).
Effect of Third Spacing on Blood Pressure
As a result of the accumulation of fluid in the peritoneal cavity and in the interstitial compartment throughout the body, circulating blood volume decreases. A significant decrease in blood volume can result in decreased blood pressure. When blood pressure decreases, the carotid and the aortic baroreceptors are activated (see Chapter 13), leading to various reflex responses aimed at returning pressure toward normal. One of these reflex responses (see Chapters 13 and 18) is an increase in the release of the hormone renin from the juxtaglomerular cells of the kidney.
Reflex Responses to Third Spacing
As described in previous chapters, increased renin ultimately results in an increase in the production of the hormone angiotensin II (AII). AII causes constriction of arterioles throughout the body, increasing total peripheral resistance and blood pressure. Increased AII also causes increased release of the hormone aldosterone from the adrenal cortex. Aldosterone increases the reabsorption of sodium ions across the kidney tubules and back into the blood. Because ADH (vasopressin) from the posterior pituitary is also released with a decrease in blood pressure, water follows the sodium ions back into the blood, expanding blood volume and increasing blood pressure. In fact, levels of ADH and aldosterone can become increasingly elevated with liver disease because a poorly functioning liver is less able to inactivate these and other hormones.
With increased plasma volume, even more fluid moves into the peritoneal cavity and the interstitial space, causing the ascites, swelling, and edema to increase. Eventually, hydrostatic (water) pressure in the peritoneal cavity and the interstitial space increases enough so that further filtration is opposed, and a new equilibrium of fluid pressures inside and outside of the capillaries is reached.
P.585
Portal-Systemic Venous Shunts
When portal hypertension reduces blood flow through the liver, collateral vessels, or shunts, open between the portal vein and the systemic veins that drain the abdominal wall, esophagus, and rectum. The shunts divert blood flow, bypassing the liver. Unfortunately, these thin-walled vessels are poorly equipped to handle such high blood flow and begin to develop into varices (distorted, swollen veins). The varices are subject to rupture and, especially in the esophagus, significant bleeding may occur. Variceal rupture can lead to a fatal hemorrhage if shunt flow is high. Rectal varices can cause painful hemorrhoids. Complicating and worsening any hemorrhage is the fact that production of many coagulation factors is decreased with liver pathology, prolonging bleeding time.
Splenomegaly
Splenomegaly is enlargement of the spleen. With portal hypertension, blood flow is diverted to the spleen via the splenic vein. Some extra blood (as much as a few hundred milliliters in an adult) can be stored in the spleen, leading to its enlargement. Because the blood stored in the spleen is unavailable to the general circulation, anemia (decreased red blood cells), thrombocytopenia (decreased platelets), and leukopenia (decreased white blood cells) can occur.
Jaundice
Jaundice is the yellowish discoloration of the skin and sclera of the eyes seen as a result of excess bilirubin in the blood (greater than 1.2 mg/dL). Bilirubin is a product of red blood cell breakdown. Jaundice is also referred to as icterus. There are three main types of jaundice: hemolytic jaundice, intrahepatic jaundice, and extrahepatic obstructive jaundice.
Hemolytic Jaundice
Caused by excessive red blood cell lysis (breakdown), hemolytic jaundice is a prehepatic cause of jaundice because it occurs as a result of factors not necessarily related to the liver. Hemolytic jaundice can occur anytime red blood cell destruction is excessive and the liver cannot conjugate (and so the body cannot excrete) all the released bilirubin. It is seen with transfusion reactions and with red cell lysis associated with faulty hemoglobin (e.g., sickle cell anemia and thalassemia). Autoimmune destruction of red cells can also lead to hemolytic jaundice.
In hemolytic jaundice, much of the bilirubin is still conjugated. Therefore, urine and stool color are normal. Unconjugated bilirubin levels (called free bilirubin or indirect hyperbilirubinemia) are elevated, because the liver's ability to conjugate bilirubin cannot keep up with the magnitude of the red cell destruction.
P.586
Intrahepatic Jaundice
Decreased hepatic uptake, conjugation, or excretion of bilirubin due to dysfunction of the hepatocytes or obstruction of the bile canaliculi are triggers of intrahepatic jaundice. Liver dysfunction can occur if the hepatocytes are infected by a virus, for instance, in hepatitis, or if the cells of the liver are damaged by cancer or cirrhosis. Some congenital disorders also affect the liver's ability to handle bilirubin. Certain drugs, including steroid hormones, some antibiotics, and the anesthetic halothane, can impair liver cell function. When the liver cannot conjugate bilirubin, unconjugated levels increase, leading to jaundice.
Intrahepatic jaundice caused by obstruction of the small bile canaliculi can occur with an intrahepatic tumor or stone, or it may result from widespread inflammation. Although the hepatocytes do conjugate bilirubin, obstruction in the canaliculi reduces the passage of the conjugated bilirubin into the bile duct. This obstruction results in an increase in the amount of conjugated bilirubin that enters the bloodstream. Depending on the degree of obstruction, stools may be pale or nearly normal in color. The urine is dark and frothy because large amounts of bilirubin are excreted by way of this route.
Extrahepatic Obstructive Jaundice
Blockage of bile flow through the bile duct also leads to obstructive jaundice. Extrahepatic obstruction can occur if the bile duct is blocked by gallstones or by a tumor. Again, as described above for intrahepatic jaundice due to obstruction, the liver continues to conjugate bilirubin, but the bilirubin cannot reach the small intestine. The result is reduced or absent stool excretion of urobilinogen, causing clay-colored stools. The conjugated bilirubin enters the bloodstream and much is excreted by the kidneys, giving the urine a dark, frothy appearance. If the obstruction is unrelieved, the bile canaliculi in the liver eventually become congested and rupture, spilling the bile into the lymph and the bloodstream.
Cirrhosis
Diffuse liver scarring and fibrosis characterize cirrhosis. Hard fibrous nodules replace normal liver tissue, and constrictive, fibrous bands encircle the hepatocytes. Normal liver architecture and function are disrupted.
Cirrhosis occurs in the liver in response to repeated incidents of cellular injury and the resultant inflammatory reactions. Causes of cirrhosis include infections such as hepatitis; bile duct obstruction, leading to bile buildup in the canaliculi and the subsequent rupture of the canaliculi; and toxin-induced injury to the hepatocytes. Alcohol is the toxin most often implicated in causing injury and inflammation in the liver
Angiotensin II (AII) appears to play a role in the development of cirrhosis. Although normally involved in hepatic tissue repair, under some
P.587
circumstances, AII stimulates hepatic inflammation and collagen synthesis. Individuals suffering from ascites frequently demonstrate elevated levels of AII, which may contribute to worsening of liver function.
Hepatitis
Hepatitis is the inflammation of the liver. It can be caused by an infection or by toxins, including alcohol, and is seen with hepatic cancer. Signs and symptoms for each type of hepatitis are similar. Modes of transmission and eventual outcomes may be different.
Conditions of Disease or Injury
Physiologic Jaundice
A significant example of hemolytic jaundice is jaundice seen in the newborn, called physiologic jaundice. This condition is especially prevalent in premature infants. It occurs as a result of increased breakdown of fetal hemoglobin in the first few days after birth combined with the immaturity of the liver at birth (especially in premature infants). Levels of unconjugated bilirubin build up in the blood, and because unconjugated bilirubin cannot be excreted in the urine, jaundice develops. Physiological jaundice is more common in breast-fed infants, and indeed, jaundice caused by breast-feeding may be a normal occurrence in the healthy infant. Levels of bilirubin and degree of jaundice usually are more pronounced and more prolonged in premature infants.
Clinical Manifestations
Unconjugated bilirubin levels will be elevated in the newborn, usually peaking 2 to 4 days after birth, and subsiding on their own within 1 to 2 weeks after birth. Levels may remain elevated longer in premature infants.
Jaundice accompanies the elevated bilirubin.
Diagnostic Tools
Peak total bilirubin levels (conjugated and unconjugated) may reach 12 to 15 mg/dL, compared with normal levels of less than 6 mg/dL in a full-term infant. Levels of unconjugated bilirubin greater than 15 mg/dL are of concern.
Complications
Because unconjugated bilirubin may precipitate out in the brain, brain damage from very high levels of unconjugated bilirubin, called kernicterus, may rarely occur (described below).
P.588
Treatment
For most infants with mildly elevated bilirubin, treatment will include phototherapy. Phototherapy involves exposing an infant to fluorescent light in the visible spectrum (between 420- and 470-nm wavelengths) for extended periods (usually 1 to 3 days). This wavelength of light causes unconjugated bilirubin to be converted to a more water-soluble form, which, like conjugated bilirubin, can be excreted in the urine and feces.
Breast-feeding jaundice need not be treated.
Hemolytic Disease of the Newborn
Hemolytic disease of the newborn is a more serious type of jaundice that appears at birth. This disease may result from either ABO or Rh incompatibility between the infant and the mother. ABO incompatibility is more common; Rh factor incompatibility is more serious. In Rh incompatibility, a mother who does not possess the Rh antigen on her red blood cells (i.e., she is Rh negative) makes antibodies against that antigen after being exposed to it on the red blood cells of her fetus. An Rh-negative woman could be exposed to the Rh antigen if the father of her child was Rh positive and her fetus carried that trait. With significant maternal antibody produced against fetal red blood cells, excessive lysis of the fetal cells can occur. Lysis of red blood cells leads to the release of bilirubin as well as agglutination (clumping) of the cells. This can occur before or during birth, overloading the already reduced capacity of the infant's liver to conjugate bilirubin. Typically, a woman develops antibodies against fetal Rh antigens only after several pregnancies or miscarriages in which she was repeatedly exposed to the antigen.
Clinical Manifestations
Hemolytic disease of the newborn may be mild or severe, depending on the degree of maternal antibodies and the extent of infant red blood cell lysis. If the disease is mild, the skin is moderately pale and the infant's liver may be slightly enlarged.
With severe disease, obvious jaundice, hepatomegaly, and splenomegaly are present. In addition, the classic symptoms of anemia, including increased heart rate and respiratory rates, are present.
Diagnostic Tools
With pronounced disease, blood analysis demonstrates severe anemia and high levels of unconjugated bilirubin.
An indirect Coombs' test that measures circulating maternal antibodies to the Rh antigen will be positive, demonstrating the mother has been exposed to the antigen.
A direct Coombs' test measuring maternal antibodies actually bound to fetal or newborn red blood cells confirms hemolytic disease.
P.589
Complications
If unconjugated bilirubin levels reach 25 to 30 mg/dL, infants may develop kernicterus. Kernicterus is a complex of neurologic symptoms related to high levels of unconjugated bilirubin crossing the neonatal blood-brain barrier and gaining access to the infant's central nervous system. Neurologic symptoms include behavioral changes and lethargy. If the condition persists or worsens, tremors, hearing loss, seizures, and death can occur. Survivors, if severely affected, may be mentally retarded, deaf, or prone to seizures.
With high levels of maternal antibodies, the fetus may die in utero of a condition called hydrops fetalis, which is characterized by gross edema of the entire fetus.
Treatment
For mild cases, phototherapy may successfully treat the disease.
In cases of moderate or severe hyperbilirubinemia, infants are treated with exchange blood transfusions. Exchange blood transfusions involve transfusing the infant with Rh-positive blood containing no Rh antibody. Transfusions are continued until twice the baby's blood volume has been replaced and the bilirubin levels are decreased. This treatment also resolves the anemia. Some Rh-positive fetuses at risk of dying in utero may be treated before birth with transfusions of red blood cells.
The most important aspect of treatment of hemolytic disease of the newborn is prevention of the disease by identification of mothers at risk of developing Rh antibodies. At-risk mothers are Rh-negative women who are carrying a child by an Rh-positive father. It is now possible to administer a concentrated form of Rh-positive antibody, called Rh immune globulin, or RhoGAM, to women at risk. RhoGAM binds any Rh-positive antigen that gains entrance to the mother's bloodstream, thereby taking the antigen out of circulation before the mother develops her own permanent antibodies against it. Administration of RhoGAM produces a temporary, passive immunity to the Rh antigen in the mother. RhoGAM is typically given to women at 7 months' gestation if Rh incompatibility is suspected. Within 72 hours of delivery of an Rh-positive infant to an Rh-negative mother, RhoGAM is again administered to the mother to protect future pregnancies. RhoGAM cannot remove antibodies to the Rh antigens if the mother has already produced them in previously untreated pregnancies (including miscarriages and abortions), but it might reduce the extent of new antibody production.
Alcoholic Cirrhosis
Also called La nnec's cirrhosis, alcoholic cirrhosis occurs after years of alcohol abuse. The end-products of alcohol digestion, especially the
P.590
end-products produced in the liver of a chronic alcohol abuser, include oxygen free radicals, which are toxic to hepatocytes. Poor nutrition, commonly seen in patients with an alcohol abuse problem, also contributes to liver damage, perhaps by over-stimulating the liver to undergo gluconeogenesis and protein metabolism. Alcoholic cirrhosis has three stages: fatty liver disease, alcoholic hepatitis, and cirrhosis.
Fatty liver disease is the first, relatively benign stage of alcoholic cirrhosis. It is a reversible condition characterized by triglyceride accumulation in the hepatocytes and is believed to occur in up to 90% of individuals who abuse alcohol chronically. Alcohol may cause triglycerides to accumulate in the liver by acting as fuel for energy production such that cells use alcohol, and fatty acids are no longer needed. Alcohol end-products, especially acetaldehyde, also interfere with the oxidative phosphorylation of fatty acids by the hepatocyte mitochondria, causing trapping of fatty acids inside the hepatocytes. In this first stage of cirrhosis, fatty infiltration of the liver is reversible if alcohol ingestion stops.
Alcoholic hepatitis is the second stage of alcoholic cirrhosis and is estimated to develop in approximately 20 to 40% of individuals abusing alcohol for an extended period of time. Hepatitis is the inflammation of liver cells. Inflammation and subsequent necrosis of some cells usually occurs after a serious increase in alcohol intake in long-term alcohol abusers. Damage to the hepatocytes probably occurs as a result of the cellular toxicity of the end-products of alcohol metabolism, especially acetaldehyde and hydrogen ion. With alcoholic hepatitis, neutrophil infiltration of the liver and the secretion of the cytokine tumor necrosis factor alpha (TNF- ) drive the inflammation. Liver cells are stimulated to undergo apoptosis (programmed cell death) that can lead to scarring and fibrosis. This stage also may be reversible if alcohol intake stops.
Cirrhosis itself is the final, irreversible stage of alcoholic cirrhosis. In this stage, dead liver cells are replaced by scar tissue. Fibrous bands develop from the chronic activation of inflammatory responses and encircle and entwine between the remaining hepatocytes. The chronic inflammation results in substantial interstitial swelling and edema, which can collapse small blood vessels and cause increased resistance to blood flow through the liver, resulting in portal hypertension and ascites. Esophageal, rectal, and abdominal varices are common, and hepatocellular jaundice is apparent. Resistance to flow through the liver progressively increases and liver function further deteriorates.
Clinical Manifestations
Early stages of cirrhosis may cause no specific symptoms, but hepatomegaly may be present.
With continued progression, vague abdominal discomfort, anorexia, and nausea may occur. Fatigue is common. Edema, ascites, and jaundice begin.
With advanced cirrhosis, manifestations of liver failure may appear.
P.591
Diagnostic Tools
Liver function tests are altered with all stages of alcoholic cirrhosis except fatty liver.
Elevated bilirubin levels are present.
Prolonged prothrombin time resulting from decreased coagulation factors.
Liver biopsy can confirm cirrhosis.
Complicatons
Liver failure, leading to transplantation or death, may develop.
Treatment
A diet with adequate nutrition is recommended to reduce the metabolic load on the liver.
Cessation of alcohol ingestion is essential.
Rest is recommended.
Management of complications of liver failure if required.
Corticosteroid administration appears to be beneficial in reducing inflammation for some patients.
Inhibition of TNF- as a means to slow apoptosis is receiving widespread attention as a therapy.
Viral Hepatitis
The viruses that cause hepatitis lead to hepatocyte injury primarily by stimulating host inflammatory and immune reactions that secondarily damage the hepatocytes; however, in some circumstances the viruses may directly injure the cells as well. The inflammatory reactions involve mast-cell degranulation and histamine release, cytokine production, complement activation, lysis of infected and neighboring cells, and edema and swelling of the interstitium. A later-occurring immune response supports the inflammatory responses. Further stimulation of complement and cell lysis and direct antibody attack against the viral antigens cause destruction of infected cells. The liver becomes edematous, collapsing capillaries and decreasing blood flow, leading to tissue hypoxia. Scarring and fibrosis of the liver can result.
Several viruses have been identified that are known to infect hepatocytes, the most common of which are hepatitis A, B, C, D, and E (Table 17-2). Other hepatitis viruses also have been identified, with new strains likely to become recognized in the future.
Hepatitis A
Hepatitis A (HAV) was formerly called infectious hepatitis. It is primarily passed by oral-fecal contamination resulting from poor hygiene or
P.592
contaminated food. Individuals living in close quarters where hygiene may be inadequate, such as day care centers, mental institutions, prisons, and homeless shelters, are at risk of developing the disease. The virus may occasionally be passed in the blood. In some countries, HAV infection is endemic.
Table 17-2. Currently Identified Hepatitis Viruses | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The time between exposure and onset of symptoms (incubation period) for HAV is between 4 and 6 weeks. Individuals who have the disease may be contagious for as long as 2 weeks before symptoms appear. Antibodies against the hepatitis A virus are present with the onset of symptoms. The disease usually runs its course within approximately 4 months after exposure. No carrier (chronic) state exists, in which an individual remains contagious for an extended period after the acute illness, nor does a fulminating condition occur after the acute illness. Acute HAV infection in patients who have chronic hepatitis C (HCV) may worsen the progression of that disease.
Hepatitis B
Hepatitis B (HBV) is sometimes called serum hepatitis. It is a serious disease throughout the world, with over 300 million people suffering from chronic infection. In some countries, notably Southeast Asia, China, and Africa, HBV is endemic, with more than one-half of the population infected at some point in their lives and more than 8% of the population being chronic carriers of the virus. In countries with high rates of HBV, transmission usually occurs either by way of mother to infant before or during birth or from one child to another in early childhood. Worldwide
P.593
public health campaigns to immunize infants and children are having dramatic effects on childhood infection rates in endemic countries. In countries with low levels of infection, including the United States, transmission is usually through sexual exposure or blood exposure in young adults. During the last few decades, public health campaigns to immunize teens and school-aged children have reduced the incidence in this population as well. Others still at high risk of developing HBV are unvaccinated injection drug users, health care workers, and non-monogamous sexually active heterosexuals and homosexuals. Transmission during tattooing and body piercing in unvaccinated individuals also may occur if hygienic practices are not followed.
HBV has a long incubation period, between 1 and 7 months with average onset of 1 to 2 months. The acute stage of an active infection may last up to 2 months. Approximately 5 to 10% of adults with HBV develop chronic hepatitis and continue to experience hepatic inflammation for longer than 6 months. Chronic hepatitis may be slowly progressive or may be fulminant, leading to hepatic necrosis, cirrhosis, liver failure, and death. An individual infected with HBV might also develop a persistent carrier state, causing him or her to be contagious without demonstrating symptoms. Especially likely to become chronic carriers are those infected during infancy and those who are immunosuppressed.
The HBV virus is a double-stranded DNA virus called a Dane particle. It has a number of well-described surface and viral core antigens that can be identified in the laboratory from a blood sample. In a primary infection, the viral antigen that is usually measurable first in a blood sample is a surface antigen on the viral coat labeled HBsAg. The presence of antibodies against the HBV core antigen (anti-HBc antibodies) follows; early in an infection, these antibodies are mainly of the IgM type. The presence of virus in the blood (viremia) is well-established by the time antibodies are produced, making this acute phase of infection a time of high transmissibility. Identification of the core antigen (HBcAg) or the hepatitis DNA itself in the serum is diagnostic of active infection with HBV. Blood donations are routinely screened for the presence of HBV antigens.
In response to the different viral antigens, different antibodies develop in individuals in a predictable sequence, beginning from the acute stage of illness until the beginning of recovery. Some forms of antibody to HBV last the lifetime of an individual who has experienced infection. If one continues to harbor HBV, however, there will be continual expression of viral antigens, including a second core antigen, HBeAg; the continued presence of viral antigens suggests the person is suffering from chronic hepatitis. With new, highly sensitive assay techniques, individuals with persistent infection still may have measurable anti-viral antibodies; therefore anyone demonstrating viral surface or core antigens, regardless of antibody status, should be presumed to have ongoing viremia. Although in adults most primary infections resolve, approximately 5% of infections will develop into persistent infections; this percentage is much higher in infants and children.
P.594
Hepatitis C
Hepatitis C (HCV) was identified in 1989. This RNA virus is passed in the same manner as HBV and primarily entered the U.S. population through blood transfusions before screening was available. In addition, soldiers and other personnel who have served in Southeast Asia have an increased incidence of infection compared with those who have not. Many individuals infected earlier in life are only now finding out they have the disease. Others who have confirmed infection have no knowledge of infection and no outstanding medical or social history indicative of high risk. Although the virus is present in semen and vaginal secretions, it is uncommon for long-term sexual partners of HCV carriers to become infected with the virus, although individuals who have multiple sexual partners or who engage in high-risk behaviors such as unprotected anal sex are more likely to become infected.
The incubation period for HCV ranges from 15 to 150 days, with an average of about 50 days. Because symptoms tend to be milder than for HBV, individuals may not recognize they have a serious infection and thus may not seek health care or be diagnosed. Unlike hepatitis B, hepatitis C seldom leads to fulminating hepatitis. Unfortunately, there is a high rate of chronic infection that may go undiagnosed for years. In addition, co-infection of individuals with both HCV and the human immunodeficiency virus (HIV) is common and is a major cause of morbidity and mortality in the 21st century. Globally, at least 30% of HIV-positive individuals are co-infected with HCV. Both antibody to HCV and the virus itself are measurable in blood, allowing for effective screening of donated blood. Although offering a quicker turn-around than viral tests, antibody tests may falsely read negative when run early in the course of disease, since the individual may not feel or appear ill, and because there is a relatively long time lapse between when an individual who has the disease is contagious and when he or she begins to express antibodies. The presence of antibodies to HCV does not imply the lack of a chronic state. There is no vaccine available at this time against HCV.
Hepatitis D
Hepatitis D (HDV) is called the delta hepatitis agent and is actually a defective virus that cannot on its own infect the hepatocyte to cause hepatitis. Instead, it co-infects with HBV, leading to a worsening of the HBV infection. Infection with HDV might also develop later in an individual who has mild chronic HBV. The delta agent increases the risk of developing fulminating hepatitis, liver failure, and death. The HDV virus is passed similarly to HBV virus. HDV antigen and antibodies can be tested in blood donations. Prevention is based on avoidance of HBV.
Hepatitis E
Hepatitis E (HEV) was identified in 1990. It is an RNA virus primarily transmitted by ingestion of contaminated water and has symptoms similar to HAV infection. Most reported cases are in developing countries. It neither
P.595
results in a carrier state nor causes chronic hepatitis. However, fulminating disease leading to liver failure and death have occurred, with women who become infected during pregnancy at highest risk.
Clinical Manifestations
Clinical manifestations of viral hepatitis can range from asymptomatic to profound illness, hepatic failure, and death. There are three stages of illness for all types of hepatitis: the prodromal stage, the icterus (jaundice) stage, and the convalescent (recovery) period.
The prodromal stage, called the preicterus period, begins after the viral incubation period ends and the person begins to have signs of illness. This stage is preicterus because jaundice (icterus) has not yet developed. An individual is highly infectious at this time. Antibodies to the virus are not usually present. This stage lasts 1 to 2 weeks. It is characterized by:
General malaise
Fatigue
Symptoms of upper respiratory tract infection
Myalgia (muscle pain)
An aversion to most foods
The icterus or jaundice stage is the second stage of viral hepatitis, and it may last 2 to 3 weeks or much longer. It is characterized in most people, as its name suggests, by the development of jaundice. Other manifestations include:
Worsening of all symptoms present during the prodromal stage
Hepatic tenderness and enlargement
Splenomegaly
Possible itchiness (pruritus) of the skin
The recovery stage is the third stage of viral hepatitis and usually happens within 4 months for HBV and HCV and within 2 to 3 months for HAV. During this period:
Symptoms subside, including jaundice.
Appetite returns.
Diagnostic Tools
Liver enzymes are abnormal, beginning in the prodromal stage.
Antibodies to the virus are elevated, starting in the icterus stage. Some antibody levels subside during the recovery stage; others remain elevated for years.
Viral antigen is detectable in blood of individuals newly infected and those chronically infected.
Complications
A complication of hepatitis is the development of chronic hepatitis that occurs when individuals continue to report symptoms and viral antigens
P.596
persist for more than 6 months. Symptoms of chronic active or fulminating hepatitis may include those of liver failure, with death occurring anywhere from 1 week to several years later. Chronic hepatitis is most common following infection with HCV and HBV.Individuals who are immunocompromised have poorer outcomes.
Individuals infected with both HBV and HCV are at increased risk of developing cirrhosis, hepatocellular carcinoma, and death. Frequent screening of chronically infected patients for signs of advancing liver disease is warranted.
Treatment
Treatment for viral hepatitis includes supportive measures such as rest as needed.
Patients who have hepatitis should avoid consumption of alcohol. Alcohol worsens the degree and accelerates the progression of HBV and especially HCV. Alcohol use in patients who have HCV increases the risk of hepatocellular carcinoma and decreases the response to treatment.
Individuals with hepatitis should be educated concerning modes of transmission to sexual partners and family members.
Drug therapy for individuals with infection usually is reserved for those with chronic infection. Injections of interferon alpha (IFN- ), a potent cytokine, have been used to treat both HBV and HBC. Injections are typically given 3 times a week for at least 3 months. The efficacy of IFN- for either disease is variable. Even in individuals who do show improvement in liver enzymes with treatment, relief may be temporary, with sustained disappearance of HBV occurring in approximately 30% of patients, while long-term disappearance of HCV occurs less often. Interferon is generally contraindicated for individuals with very advanced liver disease. It also is associated with significant side effects, including myalgia, fever, thrombocytopenia, and depression, all of which lead many to be disqualified for this treatment and others to discontinue treatment early.
Nucleotide analogues that selectively target the viral enzyme reverse transcriptase have become important medications for the treatment of chronic hepatitis. These drugs were originally developed for use in patients with HIV, and are especially appealing for the large number of patients suffering both HIV and viral hepatitis. The response rate to drugs of this category is high. Nucleotide analogues, e.g., lamivudine and ribavirin, are usually well tolerated, often making them the first-choice therapy for patients. Other drugs of this type have been developed as well. One limitation is the potential development of resistance to the medication.
Combination therapies of modified interferons plus nucleotide analogues are the most successful treatments at this time. The modified interferons, called pegylated interferons or peginterferons, have a longer half life than IFN- and require less frequent dosing.
P.597
Combination therapy is expensive and side effects are distressing and common as with the traditional interferons.Relatives of individuals diagnosed with hepatitis are offered a purified gamma globulin specific against HAV or HBV, which may offer passive immunity against infection. This is a temporary immunity. A vaccine against HAV is available. This vaccine is made from inactivated hepatitis virus. Studies have shown that it is 96% effective after one dose.
A vaccine against HBV is also available. Given the highly contagious nature of the virus and its potentially deadly effects, it is strongly recommended that all individuals, but especially those in high-risk categories, including all health care workers or others exposed to blood products, be vaccinated. It is also recommended that other individuals at high risk for becoming infected by the virus, including homosexuals and heterosexuals sexually active with more than one partner and injection drug users, be vaccinated as well. There do not appear to be any significant side effects following immunization against HBV.
Since infants infected with HBV are at very high risk of developing chronic infection, it is essential that infants be vaccinated against HBV. While this is imperative for those born in countries with endemic rates of infection, infants world-wide benefit from vaccination soon after birth. There do not appear to be any serious adverse effects of infant vaccination, and in many countries a series of three HBV vaccinations is begun soon after birth. This practice has resulted in a large decrease in the transmission of virus from mother to child and a corresponding decrease in chronic HBV infection and worldwide liver cancer in children.
Vaccines against HBV are produced by way of recombinant DNA administered intramuscularly three times at predetermined intervals. The first and second doses are given 1 month apart, and the third dose is given 2 to 6 months after the second. Vaccination is 85% effective in producing immunity. Individuals who do not show immunity after three doses, as evidenced by negative HBV antibody titers, are revaccinated. After a third or fourth vaccination, most individuals respond.
![]() ediatric Consideration
ediatric Consideration
Especially at risk of developing HAV are toddlers and children who have poor toilet hygiene and children who are cared for by individuals (in day care centers or at home) who do not follow rigorous hand-washing practices after diaper changing.
Especially at risk of developing HBV are infants born to mothers who have HBV. The virus responsible for HBV may pass from mother to fetus through the placenta if the mother becomes infected in the third trimester of pregnancy or suffers from chronic HBV infection. Exposure of an infant to infected blood before or during birth may also result in the infant developing the disease. There is a 90% risk of chronic hepatitis developing in infants infected with HBV before or during birth, making it a serious neonatal infection. Therefore, all infants, regardless of the known HBV status of the mother, are recommended to receive vaccination against HBV within 7 days of birth. Those born to mothers known to be infected are also recommended to receive the HBV immunoglobulin (gamma globulin).
P.598
Liver Failure
Liver failure is the ultimate outcome of any severe, unrelenting liver disease. Liver failure may follow years of low-grade HCV infection or may occur suddenly with the onset of fulminating HBV. Acute liver failure also may follow from an overdose of certain medications, including acetaminophen, taken either during a suicide attempt or inadvertently at high doses by individuals using the drug for pain relief. Liver failure is a complex syndrome characterized by the impairment of many different organs and body functions. Two conditions associated with liver failure are hepatic encephalopathy and hepatorenal syndrome.
Hepatic Encephalopathy
Hepatic encephalopathy is a complex of central nervous system disorders seen in individuals suffering from liver failure. It is characterized by memory lapses and personality changes. A flapping tremor can develop. Other jerking movements and poor balance may also be present. An individual suffering from hepatic encephalopathy may ultimately lapse into a coma and die.
Hepatic encephalopathy likely results from the accumulation of toxins in the blood, which occurs when the liver fails to transform or detoxify them adequately. A failing liver is not only unable to detoxify the blood because of poor hepatocyte function, but it receives less blood to detoxify than usual because much of the portal flow is diverted by high resistance and portal hypertension. As toxins and metabolic byproducts accumulate, osmotic pressure increases, leading to brain swelling and cerebral edema.
One of the main toxins that accumulates and is implicated in causing many of the symptoms of hepatic encephalopathy is ammonia. Ammonia is a by-product of protein metabolism and intestinal bacterial action. An important function of the liver is to transform ammonia to urea. Unlike ammonia, urea is easily excreted by the kidneys. When the ammonia is not transformed into urea, blood levels increase and ammonia is delivered to the brain. Other substances such as hormones, drugs, and gastrointestinal toxins also accumulate in the blood with advanced liver disease and undoubtedly contribute to hepatic encephalopathy.
![]() ediatric Consideration
ediatric Consideration
Liver failure in children is an uncommon occurrence but is devastating when it does happen. Most cases result from acute autoimmune hepatitis, drug toxicity, or an unknown etiology. Wilson's disease, a genetic disorder resulting in the retention of copper in various organs of the body including the liver, is also a known cause of pediatric liver failure.
P.599
Hepatorenal Syndrome
Hepatorenal syndrome refers to the occurrence of renal failure seen in association with advanced liver disease. The kidneys of individuals who have advanced liver disease frequently cease producing urine and fail to function, although the kidneys appear to be physically capable of functioning. Oliguria (decreased production of urine) usually occurs suddenly and is most commonly seen in individuals suffering from alcoholic cirrhosis or fulminating hepatitis. With hepatorenal syndrome, blood volume expands, hydrogen ion accumulates, and electrolyte balance is disturbed.
Suspected causes of functional renal failure associated with liver disease include significant variceal hemorrhage, leading to vascular collapse and shock. Shock of any type leads to a decrease in renal blood flow, which can irreversibly damage the kidney (see Chapter 18). Decreased blood flow to the kidneys might also occur as a result of the peripheral vasoconstriction that occurs in response to ascites and the interstitial accumulation of fluid. Finally, the accumulation of toxins specifically damaging to the kidneys increases because the failing liver is unlikely to be performing biotransformation or detoxification adequately.
Clinical Manifestations
Clinical manifestations of liver failure may be initially subtle but may become extreme as liver failure progresses. Manifestations include:
Jaundice from impaired ability to conjugate bilirubin.
Abdominal pain or tenderness from inflamed liver.
Nausea and anorexia with a profound distaste for certain foods.
Fatigue and weight loss from deficiencies in the performance of many of the liver functions of metabolism.
Splenomegaly.
Ascites.
Peripheral edema caused by a decrease in the forces favoring reabsorption of fluid into the capillary from the interstitial space, which results from a decrease in plasma protein production and a loss of albumin in ascites.
Varices of the esophagus, rectum, and abdominal wall resulting from portal hypertension.
Bleeding tendencies caused by thrombocytopenia (decreased levels of platelets) resulting from blood accumulation in the spleen and prolonged prothrombin time caused by impaired production of several coagulation factors.
Petechiae (small hemorrhagic spots on the skin) caused by thrombocytopenia.
Amenorrhea in women, caused by alterations in steroid hormone production and metabolism.
Gynecomastia (breast enlargement) in males caused by estrogen buildup as the liver fails to perform its biotransformation functions. Testosterone levels usually decrease in men, accompanied by impotence and loss of libido (sex drive).
P.600
Diagnostic Tools
Altered liver function tests.
Blood analysis demonstrates anemia owing to various small and large bleeds, sequestration of red blood cells in the spleen, and impaired production of red blood cells.
Bleeding and clotting studies are abnormal.
Hypoglycemia may occur because gluconeogenesis is impaired.
Complications
Hepatic encephalopathy.
Hepatorenal syndrome.
Variceal bleeding.
Coma and death may result.
Treatment
Although there is no cure for liver failure short of liver transplant, individual symptoms and clinical manifestations can be treated. Treatments are specific for various manifestations. Ascites is treated as follows:
Dietary restriction of salt and a potassium-sparing diuretic increase water excretion.
Potassium supplementation may be necessary to reverse the effects of high aldosterone.
Measures to remove ascitic fluid to relieve discomfort may be performed and include placing a shunt between the peritoneal cavity and the vena cava or paracentesis (aspiration drainage of fluid out of the peritoneal cavity with a large-bore needle). Both measures increase the risk of infection, and paracentesis can cause hypotension. Neither treatment is a cure for the ascites, which returns as long as liver disease continues.
Portal hypertension is treated as follows:
A connection or shunt between the portal vein and another systemic vein can be made to relieve the diversion of blood to the esophagus and other collateral vessels. This maneuver does not restore liver function, but it may reduce collateral flow and the complication of variceal bleeding. It may also reduce ascites. One example of such a connection is a transjugular intrahepatic portosystemic shunt. Careful selection and monitoring of patients for this procedure is essential.
P.601
Variceal bleeding is treated as follows:
A vasoconstrictor drug may be given to decrease flow. Balloon tamponade the insertion of a balloon catheter into the esophagus to exert pressure on the bleeding varicele may be performed. Surgical treatment to tie off the collateral vessels sprouting from the portal vein may be attempted. Vitamin K supplementation can help control bleeding.
Hepatic encephalopathy treatments are as follows:
Ventilation and sedation to protect the airway and to reduce psychomotor agitation, and bolus injections of mannitol to reduce cerebral edema are administered. Blood glucose is closely monitored because hypoglycemia may occur with liver failure.
Most dietary advice is concerned with restriction of dietary protein and inclusion of high-carbohydrate sources.
Prevention of infections and rapid treatment is important.
Liver dialysis (artificial extracorporeal liver support) is increasingly being used.
Liver transplants are becoming more common for the treatment of advanced liver disease. There is variable success for this procedure, depending on the cause of liver failure and the individual patient. The increase in transplants over the past 20 years has reduced chronic liver disease mortality in the U.S.
Liver Cancer
Primary liver cancer is uncommon in the United States but much more common world-wide. When it does occur, it is usually seen in individuals who have a history of HBV or HCV infection or who have chronic liver disease, for example, cirrhosis. Others known to be at high risk for developing liver cancer include those exposed to high levels of known carcinogens, including aflatoxins found on moldy corn or peanuts. Primary liver cancers may be of the hepatocytes themselves (hepatocellular carcinoma) or of the bile ducts (cholangiocarcinoma).
Secondary liver cancer is the result of a metastasis of cancer from areas of the body (e.g., the intestine or the pancreas) that drain into the liver through the portal vein or from other cancers. Both primary and secondary liver cancers themselves frequently metastasize outside the liver, especially to the heart and lungs, because hepatic drainage encounters these organs first. All types of liver cancer have poor prognoses, often related to intrahepatic recurrence of the cancer. Less than 5% of individuals with liver cancer survive longer than 5 years.
Clinical Manifestations
Dull abdominal pain.
A feeling of abdominal fullness.
Nausea and vomiting.
Jaundice.
Anorexia (decreased appetite) and aversion to certain foods.
If the tumor obstructs the bile duct, portal hypertension and ascites may develop. Jaundice worsens, and colicky pain may develop.
Hepatomegaly.
P.602
Diagnostic Tools
Elevated liver enzymes.
Elevated levels of a protein normally not present in adult serum, alpha-fetoprotein.
Treatment
Surgery for some tumors is possible, although outcomes tend to be poor related to intrahepatic metastases that lead to recurrence. Recent evidence suggests that downregulation of the immune response related genes (HLA genes) that encode MHC class II antigens may occur in patients and contribute to cancer recurrence, suggesting a possible target for future therapy.
Chemotherapy.
Selected Bibliography
Alonso, E.M. (2005). Acute liver failure in children: The role of defects in fatty acid oxidation. Hepatology 41, 696 699.
Bataller, R., Sancho-Bru, P., Gines, P., & Brenner, D.A. (2005). Liver fibrogenesis: A new role for the renin-angiotensin system. Antioxidants and Redox Signalling 7, 1346 1355.
Blei, A.T. (2005). The pathophysiology of brain edema in acute liver failure. Neurochemistry International 47, 71 77.
Boyer, T.D., & Haskal, Z.J. (2005). American Association for the Study of Liver Diseases practice guidelines: The role of transjugular intrahepatic portosystemic shunt creation in the management of portal hypertension. Journal of Vascular and Interventional Radiology 16, 615 629.
Ganem, D., & Prince, A.M. (2004). Hepatitis B virus infection Natural history and clinical consequences. New England Journal of Medicine 350, 1118 1129.
Guyton, A.C., & Hall, J. (2006). Textbook of medical physiology (11th ed.). Philadelphia: W.B. Saunders.
Jones, R., Dunning, J., & Nelson, M. (2005). HIV and hepatitis C co-infection. International Journal of Clinical Practice 59, 1082 1087.
LaVecchia, C. (2005). Coffee, liver enzymes, cirrhosis and liver cancer. Journal of Hepatology 42, 444 446.
Marchesini, G., Marzocchi, R., Agostini, F., & Bugianesi, E. (2005). Nonalcoholic fatty liver disease and the metabolic syndrome. Current Opinion in Lipidology 16, 421 427.
Matoba, K., Iizuka, N., Gondo, T., Ishihara, T., Yamada-Okabe, H., & Tamesa, T. (2005). Tumor HLA-DR expression linked to early intrahepatic recurrence of hepatocellular carcinoma. International Journal of Cancer 115, 231 240.
Murray, K.F., & Carithers, Jr., R.L. (2005). AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology 41, 1407 1432.
Neff, G.W., Sherman, K.E., Eghtesad, B., & Fung, J. (2004). Review article: Current status of liver transplantation in HIV-infected patients. Alimentary Pharmacology & Therapeutics 20, 993 1000.
Poland, G.A., & Jacobson, R.M. (2004). Prevention of hepatitis B with the hepatitis B vaccine. New England Journal of Medicine 351, 2832 2838.
P.603
Porth, C.M. (2005). Pathophysiology: Concepts of altered health states (7th ed.). Philadelphia: Lippincott Williams & Wilkins.
Riordan, S.M., & Williams, R. (1997). Treatment of hepatic encephalopathy. New England Journal of Medicine 337, 473 478.
Sougioultzis, S., Dalakas, E., Hayes, P.C., & Plevris, J.N. (2005). Alcoholic hepatitis: From pathogenesis to treatment. Current Medical Research and Opinion 21, 1337 1346.
Teutsch, H.F. (2005). The modular microarchitecture of human liver. Hepatology 42, 317 325.
Vento, S., Garofano, T., Rensini, C., et al. (1998). Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic Hepatitis C. New England Journal of Medicine 338, 286 290.
Vitaglione, P., Morisco, F., Caporaso, N., & Fogliano, V. (2004). Dietary antioxidant compounds and liver health. Critical Reviews in Food Science and Nutrition 44, 575 586.
EAN: 2147483647
Pages: 26