17 - Ethical Issues in the Care of Older Persons
Editors: Kane, Robert L.; Ouslander, Joseph G.; Abrass, Itamar B.
Title: Essentials of Clinical Geriatrics, 5th Edition
Copyright 2004 McGraw-Hill
> Table of Contents > Part III - General Management Strategies > Chapter 16 - Nursing Home Care
Chapter 16
Nursing Home Care
The focus of this chapter is the clinical care of nursing home residents. Some of the basic demographic and economic aspects of nursing home care are discussed in Chaps. 2 and 15. The poor quality of care provided in many nursing homes has been recognized for decades (Vladek, 1980). Since the Institute of Medicine issued its critical report in 1986 (Institute of Medicine, 1986) and the mandating of the Resident Assessment Instrument in 1987, the overall quality of care has improved somewhat. A more recent Institute of Medicine report, however, indicates there is still considerable room for further improvements in care quality (Institute of Medicine, 2000).
Despite the logistic, economic, and attitudinal barriers that can foster inadequate medical care in the nursing home, many straightforward principles and strategies can lead to improvements in the quality of medical care provided to nursing home residents. Fundamental to achieving these improvements is a clear perspective on the goals of nursing home care, which are in many respects quite different from the goals of medical care in other settings and patient populations.
THE GOALS OF NURSING HOME CARE
The modern nursing home serves multiple roles. Table 16-1 lists the key goals of nursing home care. While the prevention, identification, and treatment of chronic, subacute, and acute medical conditions are important, most of these goals focus on the functional independence, autonomy, quality of life, comfort, and dignity of the residents. Physicians who care for nursing home residents must keep these goals in perspective at the same time the more traditional goals of medical care are being addressed.
TABLE 16-1 GOALS OF NURSING HOME CARE | |
|---|---|
|
The heterogeneity of the nursing home population must also be recognized in order to focus and individualize the goals of care. This heterogeneity results in a diversity of goals for nursing home care. Nursing home residents can be subgrouped into five basic types (Fig. 16-1). While it is not always possible to isolate these different types of residents geographically, and although residents often overlap or change between the types described, subgrouping nursing home residents in
P.426
this manner will help the physician and interdisciplinary team to focus the care-planning process on the most critical and realistic goals for individual residents.
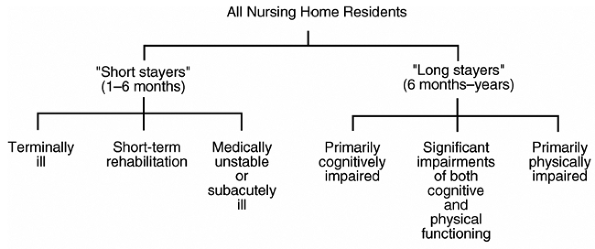 |
FIGURE 16-1 Basic types of nursing home patients. |
The underlying social contract implied by nursing home admission is quite different for each of these groups. In some cases, access to treatment takes precedence over the living environment; in other circumstances, the environment may be the most critical element of care. Those admitted to a nursing home with the intent of active treatment and discharge home may be willing to accept a living situation akin to that of a hospital in the expectation that the benefit they receive from treatment will offset any discomfort or inconvenience. For terminally ill persons under the hospice model, the living environment is made as flexible and supportive as possible. Efforts are directed toward making these patients comfortable and permitting them to enjoy their last days.
There is a trend to separate the cognitively impaired from those who are primarily physically impaired. There is a growing number of special care units (SCUs) for the cognitively impaired where their care can be coordinated to maximize attention to the behavioral aspects of dementia care and to minimize the use of psychoactive drugs and restraints while maintaining a safe environment. Some see SCUs as a way of achieving better results. Others view them as controlled environments in which demented residents can be treated more humanely by staff who have chosen to concentrate on such care. Still others see the primary gain from SCUs as removing otherwise disruptive patients from the environment of those still alert enough to resent the intrusion. There are no strong data, however, that demonstrate major improvements in outcomes of patients treated on these units.
Residents who are more cognitively intact may benefit from newer forms of institutional care such as assisted living (described in Chap. 15). These residents
P.427
can maximize their quality of life in individual rooms that afford them privacy and a greater sense of control over their surroundings. Those residents who are, for all intents and purposes, completely out of touch with their environments (e.g., those in permanent vegetative states or advanced dementia) may be well served by simple environments designed to maintain them safely. These individuals are the subject of increasing ethical debate (see Chap. 17).
CLINICAL ASPECTS OF CARE FOR NURSING HOME RESIDENTS
In addition to the different goals for care in the nursing home, several factors make the assessment and treatment of nursing home residents different from those in other settings (Table 16-2). Many of these factors relate to the process of care and are discussed in the following section. (For a more complete discussion of medical care in the nursing home, see the suggested readings and Ouslander et al., 1997.) A fundamental difference in the nursing home is that medical evaluation and treatment must be complemented by an assessment and care-planning process involving staff from multiple disciplines. The integral involvement of nurses' aides in the development and implementation of care plans is crucial to high-quality nursing home care. Data on medical conditions and their treatment are integrated with assessments of the functional, mental, and behavioral status of the resident in order to develop a comprehensive data base and individualized plan of care.
TABLE 16-2 FACTORS THAT MAKE ASSESSMENT AND TREATMENT IN THE NURSING HOME DIFFERENT FROM THAT IN OTHER SETTINGS | |
|---|---|
|
Medical evaluation and clinical decision making for nursing home residents are complicated for several reasons. Unless the physician has cared for the resident
P.428
P.429
before nursing home admission, it may be difficult to obtain a comprehensive medical data base. Residents may be unable to relate their medical histories accurately or to describe their symptoms, and medical records are frequently unavailable or incomplete, especially for residents who have been transferred between nursing homes and acute-care hospitals. When acute changes in status occur, initial assessments are often performed by nursing home staff with limited skills and are transmitted to physicians by telephone. Even when the diagnoses are known or strongly suspected, many diagnostic and therapeutic procedures among nursing home residents are associated with an unacceptably high risk:benefit ratio. For example, a barium enema may cause dehydration or severe fecal impaction; nitrates and other cardiovascular drugs may precipitate syncope or disabling falls in frail ambulatory residents with baseline postural hypotension; and adequate control of blood sugar may be extremely difficult to achieve without a high risk for hypoglycemia among cognitively impaired diabetic residents with marginal or fluctuating nutritional intake who may not recognize or complain of hypoglycemic symptoms.
Further compounding these difficulties is the inability of many nursing home residents to participate effectively in important decisions regarding their medical care. Their previously expressed wishes are often not known, and an appropriate or legal surrogate decision maker has often not been appointed. These issues are discussed further on in this chapter and in Chap. 17.
Table 16-3 lists the most commonly encountered clinical disorders in the nursing home population. They represent a broad spectrum of chronic medical illnesses; neurological, psychiatric, and behavioral disorders; and problems that are especially prevalent in frail older adults (e.g., incontinence, falls, nutritional disorders, chronic pain syndromes). Although the incidence of iatrogenic illnesses has not been systematically studied in nursing homes, it is likely to be as high as or higher than that in acute-care hospitals. The management of many of the conditions listed in Table 16-3 is discussed in some detail in other chapters of this text (for specific conditions, see Table of Contents and Index).
TABLE 16-3 COMMON CLINICAL DISORDERS IN THE NURSING HOME POPULATION | |
|---|---|
|
In addition to the numerous factors already mentioned that render the medical assessment and treatment of these conditions different, the process of care in nursing homes also differs substantially from that in acute care hospitals, clinics, and home care settings.
PROCESS OF CARE IN THE NURSING HOME
The process of care in nursing homes is strongly influenced by numerous state and federal regulations, the highly interdisciplinary nature of nursing home residents' problems, and the training and skills of the staff that delivers most of the hands-on care. Federal rules and regulations contained in the Omnibus Budget Reconciliation Act of 1987 (OBRA 1987) and implemented in 1991 place heavy
P.430
P.431
emphasis on assessment and care planning as a means of achieving the highest practicable level of functioning for each resident and the use of the Resident Assessment Instrument.
Physician involvement in nursing home care and the nature of medical assessment and treatment offered to nursing home residents are often limited by logistic and economic factors. Few physicians have offices based either inside the nursing home or in close proximity to the facility. Many physicians who do visit nursing homes care for relatively small numbers of residents, often in several different facilities. Many nursing homes, therefore, have numerous physicians who make rounds once or twice per month, who are not generally present to evaluate acute changes in resident status, and who attempt to assess these changes over the telephone. In some areas, practice patterns are shifting to a model of physician nurse practitioner practices caring for large numbers of residents in several nursing homes. Many nursing homes do not have ready availability of laboratory, radiologic, and pharmacy services with the capability of rapid response, further compounding the logistics of evaluating and treating acute changes in medical status. Thus, nursing home residents are often sent to hospital emergency rooms, where they are evaluated by personnel who are generally not familiar with their baseline status and who frequently lack training and interest in the care of frail and dependent elderly patients.
P.432
Restrictive Medicare and Medicaid reimbursement policies may also dictate certain patterns of nursing home care. While physicians are required to visit nursing home residents only every 30 to 60 days, many residents require more frequent assessment and monitoring of treatment especially with the shorter acute-care hospital stays brought about by the prospective payment system. While Medicare reimbursement for physician visits in nursing homes has improved, reimbursement for a routine visit is generally inadequate for the time that is required to provide good medical care in the nursing home, including travel to and from the facility; assessment and treatment planning for residents with multiple problems; communication with members of the interdisciplinary team and the resident's family; and proper documentation in the medical record. Activities often essential to good care in the nursing home, such as attendance at interdisciplinary conferences, family meetings, complex assessments of decision-making capacity, and counseling residents and surrogate decision makers on treatment plans in the event of terminal illness, are generally not reimbursable at all. Medicare intermediaries restrict reimbursement for rehabilitative services for residents not covered under Part A skilled care, thus limiting the treatment options for many residents. Although Medicaid programs vary considerably, many provide minimal coverage for ancillary services that are critical for optimum medical care, and may restrict reimbursement for several types of drugs that may be especially helpful for nursing home residents.
Amid these logistic and economic constraints, expectations for the care of nursing home residents are high. Table 16-4 outlines the various types of assessment generally recommended for the optimal care of nursing home residents. Physicians are responsible for completing an initial assessment within 72 hours of admission and for arranging for monthly visits thereafter for the next 90 days. Licensed nurses assess new residents as soon as they are admitted, on a daily basis, and generally summarize the status of each resident weekly. The nationally mandated Minimum Data Set (MDS) must be completed within 14 days of admission and updated when a major change in status occurs; several sections must be routinely updated on a quarterly basis.
TABLE 16-4 IMPORTANT ASPECTS OF VARIOUS TYPES OF ASSESSMENT IN THE NURSING HOME | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The extent of involvement of other disciplines in the assessment and care-planning process varies depending on the residents' problems, the availability of various professionals, and state regulations. Representatives from nursing, social services, dietary management, activities, and rehabilitation therapy (physical and/or occupational) participate in an interdisciplinary care-planning meeting. Residents are generally discussed at this meeting within 2 weeks of admission and quarterly thereafter. The product of these meetings is an interdisciplinary care plan that separately lists interdisciplinary problems (e.g., restricted mobility, incontinence, wandering, diminished food intake, poor social interaction), goals for the resident related to the problem, approaches to achieving these goals, target dates for achieving the goals, and assignment of responsibilities for working toward the goals among the various disciplines. These care plans are an important force in driving nursing staff behavior and expectations and should be reviewed by the primary physician.
P.433
P.434
P.435
P.436
P.437
P.438
The MDS is intended to assist nursing home staff in identifying important clinical problems and to trigger the use of Resident Assessment Protocols (RAPs), which have been developed for 18 common clinical conditions. The MDS and the RAPs are critical tools for developing individual care plans. The interdisciplinary care-planning process serves as a cornerstone for resident management in many facilities, but is a difficult and time-consuming process that requires leadership and tremendous interdisciplinary (and interpersonal) cooperation.
Staffing limitations in relation to the amount of time and effort required makes intensive interdisciplinary care planning and teamwork unrealistic in many nursing homes. Although physicians are seldom directly involved in the care-planning meetings in most facilities, they are generally required to review and sign the care plan, and may find the team's perspective very valuable in planning subsequent medical care.
Implementation of the OBRA 1987 regulations primarily affects the activities of the nursing home staff. But some aspects of these regulations have a direct bearing on physicians who are caring for nursing home residents. Several of the RAPs require involvement of the physician in the evaluation and management of common geriatric conditions seen in nursing home residents (e.g., delirium, incontinence). The RAPs do not directly address many common medical conditions (e.g., congestive heart failure, arthritis, infections) that must be identified and managed outside the MDS/RAP paradigm. Perhaps the most direct effect on physicians relates to the specifications around the use of psychoactive medications. OBRA 1987 defines criteria for appropriate use of these medications, and requires the documentation of specific diagnoses as well as the quantitative documentation of the response of target behavioral symptoms to these drugs. Psychoactive medications can no longer be used simply as a means to control symptoms of aggressive or disruptive behavior (i.e., as chemical restraints ), or on a continued as-needed basis. These rules have stimulated a rethinking of psychoactive drug use among nursing home residents, and there is evidence that the prescription of these drugs has changed since OBRA 1987 went into effect (Llorente et al., 1998). The appropriate use of antipsychotics for patients with dementia and psychosis must be distinguished from the use of drugs as chemical restraints. Physician attention is also directed to the use of physical restraints. In keeping with changing attitudes about such care, the use of these restraints is generally discouraged. Restraints can be applied only upon a physician's order and only after documenting that less restrictive measures are not effective. Physical restraints can be safely removed from most residents (Evans et al., 1997). While not all residents can be free of restraints at all times, a restraint-free environment is an appropriate goal in the nursing home setting.
The general pressure for better documentation of care and assessments should provide a welcome improvement in the quality of care for nursing home residents. These rules will inevitably mean that physicians will be asked to make more detailed clinical notes, especially with respect to indicating the underlying reasons for their actions.
P.439
Although these changes may place a modest added burden on the attending physician, they do not demand a great deal of extra effort and should help to provide a better environment in which to practice.
STRATEGIES TO IMPROVE MEDICAL CARE IN NURSING HOMES
Several strategies might improve the process of medical care delivered to nursing home residents. Four strategies are briefly described: (1) the use of improved documentation practices; (2) a systematic approach to screening, health maintenance, and preventive practices for the frail, dependent nursing home population; (3) the use of nurse practitioners or physicians' assistants; and (4) use of practice guidelines and related quality improvement activities.
In addition to these strategies, strong leadership of a medical director who is appropriately trained and dedicated to improving the facilities' quality of medical care is essential in order to develop, implement, and monitor policies and procedures for medical services. The role of the medical director in nursing homes is discussed in detail elsewhere (see the suggested readings). The medical director should set standards for medical care and serve as an example to the medical staff by caring for some of the residents in the facility. The medical director should also be involved in various committees (pharmacy, infection control, quality assurance), and should involve interested medical staff in these committees, as well as in educational efforts through formal in-service presentations, teaching rounds, and appropriate documentation procedures.
The federal government's approach to improving the quality of care in nursing homes is based on the OBRA 1987 rules, and the MDS and RAPs in particular. Computerized MDS data is now used to generate selected quality indicators and to identify outlier facilities that may require targeted evaluation (Zimmerman et al., 1995). While some data suggest that various aspects of nursing home care have improved since the implementation of the OBRA 1987 rules and regulations, many caveats about these early data have been voiced (Ouslander, 1997). Other approaches to improving quality will be necessary to complement the OBRA rules and regulations (Kane, 1998).
![]() Documentation Practices
Documentation Practices
Nursing home residents often have multiple coexisting medical problems and long previous medical histories. Residents often cannot relate their medical histories, and their previous medical records are frequently unavailable or incomplete. There is also a danger in perpetuating old diagnoses that are inaccurate. This is especially true for psychiatric diagnoses, but may also occur for other
P.440
medical diagnoses such as congestive heart failure and stroke. Thus, it is difficult and sometimes impossible to obtain a comprehensive medical data base. The effort should, however, be invested and not wasted. Critical aspects of the medical data base should be recorded on one page or face sheet of the medical record. Figure 16-2 shows an example of a format for a face sheet. Additional standardized documentation should contain social information, such as individuals to contact at critical times and information about the resident's treatment status in the event of acute illness. These data are essential to the care of the resident and should be readily available in one place in the record, so that when emergencies arise, when medical consultants see the resident, or when members of the interdisciplinary team need an overall perspective, they are easy to locate. The face sheet should be copied and sent to the hospital or other health care facilities to which the resident might be transferred. Time and effort is required in order to keep the face sheet updated. For facilities with access to computers and/or word processing, incorporating the face sheet into a database should be relatively easy and facilitate its rapid completion and periodic updating.
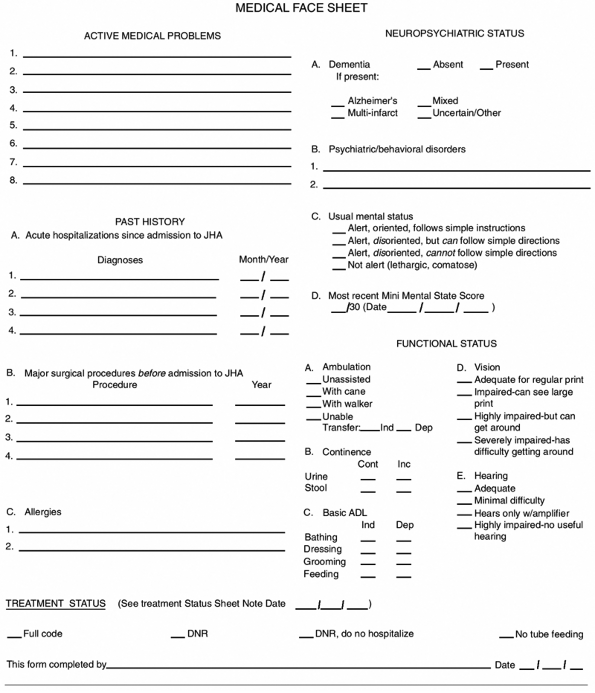 |
FIGURE 16-2 Example of a face sheet for a nursing home record. |
Medical documentation in progress notes for routine visits and assessments of acute changes is frequently scanty and/or illegible. Statements such as stable or no change are too frequently the only documentation for routine visits. While time constraints may preclude extensive notes, certain standard information should be documented. The SOAP (subjective, objective, assessment, plan) format for charting routine notes is especially appropriate for nursing home residents (Table 16-5). Simple forms, flow sheets, or databases with word-processing capabilities can be used to enable physicians to efficiently produce legible, concise, yet comprehensive progress notes. Another tool for documenting change in residents over time is the benchmark approach using flow sheets (see Chap 4).
TABLE 16-5 SOAP FORMAT FOR MEDICAL PROGRESS NOTES ON NURSING HOME RESIDENTS | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Another area in which medical documentation is often inadequate relates to the residents' decision-making capacity and treatment preferences. These issues are discussed briefly at the end of this chapter as well as in Chap. 17. In addition to placing critical information in a standardized format in readily accessible locations, it is essential that physicians thoroughly and legibly document all discussions they have had with the resident, family, or legal guardians; they must also document any durable power of attorney for health care about these issues. Failure to do so may result not only in poor communication and inappropriate treatment, but also in substantial legal liability. Notes about these issues should not be removed from the medical record and are probably best kept on a separate page behind the face sheet.
![]() Screening, Health Maintenance, and Preventive Practices
Screening, Health Maintenance, and Preventive Practices
A second approach to improving medical care in nursing homes is the development and implementation of selected screening, health maintenance, and preventive practices. Table 16-6 lists examples of such practices. With few exceptions, the efficacy
P.441
of these practices has not been well studied in the nursing home setting. In addition, not all the practices listed in Table 16-6 are relevant for every nursing home resident. For example, some of the annual screening examinations are inappropriate for short-stayers or for many long-staying residents with end-stage dementia (see Fig. 16-1). Thus, the practices outlined in Table 16-6 must be tailored to the specific nursing home population, as well as for the individual resident, and must be creatively incorporated into routine care procedures as much as possible in order to be time-efficient, cost-effective, and reimbursable by Medicare.
TABLE 16-6 SCREENING, HEALTH MAINTENANCE, AND PREVENTIVE PRACTICES IN THE NURSING HOME | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
![]() Nurse Practitioners and Physician Assistants
Nurse Practitioners and Physician Assistants
A third strategy that may help to improve medical care in nursing homes is the use of nurse practitioners and physician assistants. This approach appears to be cost-effective in both managed care and fee-for-service settings (Burl et al., 1998; Ackerman and Kemle, 1998), and these health professionals may be especially helpful in carrying out specific functions in the nursing home setting. Physician assistants and nurse practitioners can bill for services under fee-for-service Medicare; moreover, several states will reimburse their services, and individual facilities and/or physician groups can hire them on a salaried basis. Evercare is a managed care program for long-stay nursing home residents that uses a nurse practitioner-based model of care and is available in several states. Nurse practitioners may have an especially helpful perspective in interacting with nursing staff about the nonmedical aspects of care for nursing home residents. Nurse practitioners and physician's assistants can be very helpful in implementing some of the screening, monitoring, and preventive practices outlined in Table 16-6, and in communicating with interdisciplinary staff, families, and residents at times when the physician is not in the facility. One of the most appropriate roles for nurse practitioners and physicians' assistants is in the initial assessment of acute or subacute changes in resident status. They can perform a focused history and physical examination, and can order appropriate diagnostic studies. Several algorithms have been developed for this purpose, one of which is shown in Fig. 16-3. This strategy enables the onsite assessment of acute change, the detection and treatment of new problems early in their course, more appropriate utilization of acute care hospital emergency rooms, and the rapid identification of residents who need to be hospitalized.
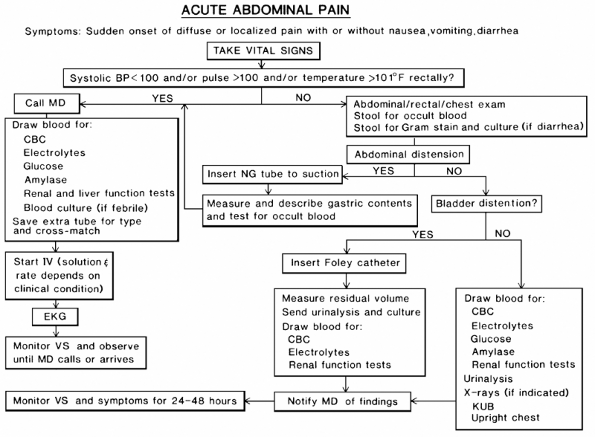 |
FIGURE 16-3 Example of an algorithm protocol for the management of acute abdominal pain in the nursing home by a nurse practitioner or physician's assistant. CBC = complete blood cell count; EKG = electrocardiogram; IV = intravenous; KUB = kidneys, ureters, bladder; MD = medical doctor; NG = nasogastric; VS = vital signs. |
![]() Clinical Practice Guidelines and Quality Improvement Activities
Clinical Practice Guidelines and Quality Improvement Activities
Several clinical practice guidelines relevant to nursing home care have been developed by the American Medical Directors Association (AMDA). In addition,
P.442
P.443
P.444
the 18 RAPs contain basic approaches to common conditions among nursing home residents. While these guidelines are largely based on expert opinion rather than on controlled clinical trials, they are helpful as a basis for standards of practice that will improve care. Implementation and maintenance of practice guidelines can be difficult in nursing homes, as it is in other practice settings (Schnelle et al., 1997).
Clinical practice guidelines can be useful tools in an overall quality improvement program. Nursing homes are required to have an ongoing quality assurance committee. The most effective approaches are probably those ones based on principles of total quality management (TQM) or continuous quality improvement (CQI) (Schnelle et al., 1993). These approaches use front-line staff to monitor objective outcomes (such as the frequency of falls, severity of incontinence, adverse drug reactions, and skin problems) and to identify work processes that can
P.445
P.446
P.447
P.448
P.449
P.450
P.451
be modified to continuously improve these outcomes. Effective CQI activities will require the further development of software such as that which is used for incontinence care (Schnelle et al., 1995). Nursing home administrators, directors of nursing, and medical directors must create an environment that provides incentives for ongoing CQI activities in order to maintain these programs over time.
SUBACUTE CARE AND THE NURSING HOME ACUTE-CARE HOSPITAL INTERFACE
The need for high levels of skilled postacute care will continue to place increased demands on nursing homes. Medicare risk health maintenance organizations (HMOs) commonly admit patients with acute but relatively stable conditions (e.g., deep vein thrombosis, cellulitis) directly to nursing homes without an acute hospital stay. As a result, nursing homes are providing more and more high-level skilled care. The term subacute care has many connotations; for the purposes of this chapter, it refers to skilled care reimbursed by Medicare Part A (or by a capitated system) in a free-standing nursing home. Subacute care is also discussed in Chap. 15, and more detail is provided in the suggested readings.
Caring for subacutely ill patients in a free-standing nursing home intensifies many of the challenges already alluded to in this chapter (see Table 16-2). This level of care requires greater involvement of physicians, nurse practitioners, and physician assistants; nursing staff trained for more acute patients; ready availability of ancillary services such as lab, x-ray, physical, and respiratory therapy; and more intensive discharge planning. Moreover, Medicare reimbursement for Part A services is being bundled, so that nursing homes will be at financial risk for services that are ordered by medical staff, including drugs, laboratory tests, x-rays, and therapies. This reimbursement structure requires unprecedented cooperation between physicians and nursing home administrators in order to make this form of subacute care economically viable.
As a result of the increasing acuity and frailty of the nursing home resident population, transfer back and forth between the nursing home and one or more acute care hospitals is common. The major reasons for transfer include infection and the need for parenteral antimicrobials and hydration as well as acute cardiovascular conditions and hip fractures. Transfer to an acute care hospital is often a disruptive process for a chronically or subacutely ill nursing home resident. In addition to the effects of the acute illness, nursing home residents are subject to acute mental status changes and a myriad of potential iatrogenic problems (see Chap. 5). Probably the most prevalent of these iatrogenic problems are related to immobility, including deconditioning, difficulty regaining ambulation and/or transfer capabilities, and the development of pressure sores.
Because of the risks of acute care hospitalization, the decision to transfer a resident to the emergency room or hospitalize a resident must carefully balance a
P.452
number of factors. A variety of medical, administrative, logistic, economic, and ethical issues can influence decisions to hospitalize nursing home residents. Decisions regarding hospitalization often boil down to the capabilities of the physician and the nursing home staff to provide services in the nursing home, the preferences of the resident and the family, and the logistic and administrative arrangements for acute hospital care. If, for example, the nursing home staff has been trained and has the personnel to institute intravenous therapy without detracting from the care of the other residents, or if it has arranged for an outside agency to oversee intravenous therapy and there is a nurse practitioner or physician's assistant to perform follow-up assessments, the resident with an acute infection who is otherwise medically stable may best be managed in the nursing home.
ETHICAL ISSUES IN NURSING HOME CARE
Ethical issues arise as much or more in the day-to-day care of nursing home residents as in the care of patients in any other setting. Table 16-7 outlines several common ethical dilemmas that occur in the nursing home. Although most attention has been directed toward those marginally able to express their preferences, important daily ethical dilemmas also face those who are capable of decision making. These more subtle problems are easily overlooked. Physicians, nurse practitioners, and physicians' assistants providing primary care must serve as strong advocates for the autonomy and quality of life for nursing homes residents.
TABLE 16-7 COMMON ETHICAL ISSUES IN THE NURSING HOME* | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Nursing homes do care for an extraordinarily high concentration of individuals who are unable or are questionably capable of participating in decisions concerning their current and future health care. Among these same individuals severe functional disabilities and terminal illnesses are prevalent. Thus, questions regarding individual autonomy, decision-making capacity, surrogate decision makers, and the intensity of treatment that should be given at the end of life arise on a daily basis. These questions are both troublesome and complex but must be dealt with in a straightforward and systematic manner in order to provide optimal medical care to nursing home residents within the context of ethical principles and state and federal laws. Nursing homes should be encouraged to develop their own ethics committees or to participate in a local existing committee in another facility. Ethics committees can be helpful in educating staff; developing, implementing, and monitoring policies and procedures; and in providing consultation in difficult cases. Some practical methods of approaching ethical issues are discussed in Chap. 17.
References
Ackerman RJ, Kemle KA: The effect of a physician assistant on the hospitalization of nursing home residents. J Am Geriatr Soc 46:610 614, 1998.
P.453
P.454
Burl JB, Bonner A, Rao M, Khan AM: Geriatric nurse practitioners in long-term care: demonstration of effectiveness in managed care. J Am Geriatr Soc 46:506 510, 1998.
Evans LK, Strumpf NE, Allen-Taylor SL, et al: A clinical trial to reduce restraints in nursing homes. J Am Geriatr Soc 45:675 681, 1997.
Institute of Medicine: Improving the Quality of Care in Nursing Homes. Washington, DC, National Academy Press, 1986.
Institute of Medicine: Improving the Quality of Nursing Home Care. Washington, DC, National Academy Press, 2000.
Kane RL: Assuring quality in nursing home care. J Am Geriatr Soc 46:232 237, 1998.
Kramer AJ, Steiner JF, Schlenker RE, et al: Outcomes and costs after hip fracture and stroke: a comparison of rehabilitation settings. JAMA 277(5):396 404, 1997.
Llorente MD, Olsen EJ, Leyva O, et al: Use of antipsychotic drugs in nursing homes: current compliance with OBRA regulations. J Am Geriatr Soc 46:198 201, 1998.
Ouslander JG: The Resident Assessment Instrument (RAI): promise and pitfalls. J Am Geriatr Soc 45:975 976, 1997.
Schnelle J, Ouslander JG, Cruise PA, et al.: Policy with technology: a barrier to improving nursing home care. The Gerontologist 37(4):527 532, 1997.
Schnelle JF, McNees P, Crook V, et al: The use of a computer-based model to implement an incontinence management program. Gerontologist 36:656 665, 1995.
Schnelle JF, Ouslander JG, Osterweil D, Blumenthal S: Total quality management: administrative and clinical applications in nursing homes. J Am Geriatr Soc 41:1259 1266, 1993.
Vladek B: Unloving Care: The Nursing Home Tragedy. New York, Basic Books, 1980.
Zimmerman DR, Karon SL, et al: Development and testing of nursing home quality indicators. Health Care Fin Rev 16(4):107 127, 1995.
Suggested Readings
Nursing Home Care (General)
Harvell J: Subacute care: its role and the assurance of quality. Annu Rev Gerontol Geriatr 16:37 59, 1996.
Levenson SA (ed.): Medical Direction in Long-term Care: A Guidebook for the Future, 2d ed. Durham, NC, Carolina Academic Press, 1993.
Levenson SA: Subacute and Transitional Care Handbook. St. Louis, Beverly Cracom, 1996.
Ouslander J, Osterweil D: Physician evaluation and management of nursing home residents. Ann Intern Med 121:584 592, 1994.
Ouslander J, Osterweil D, Morley J: Medical Care in the Nursing Home, 2d ed. New York, McGraw-Hill, 1996.
Smith RL, Osterweil D: The medical director in hospital-based transitional care units. Med Dir Long-term Care 11:373 389, 1995.
EAN: 2147483647
Pages: 23