61 - Fibrothorax and Decortication of the Lung
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section XII - Thoracic Trauma > Chapter 73 - Management of Foreign Bodies of the Airway
Chapter 73
Management of Foreign Bodies of the Airway
Julie L. Wei
Lauren D. Holinger
Foreign body aspiration is a serious and potentially fatal occurrence. Through advances in prevention, first aid, and endoscopic technology, a nearly 20% decrease in deaths from foreign body aspiration has occurred within the United States over the last decade. Nevertheless, in 1997, the National Safety Council reported an average of more than eight deaths per day from foreign body aspiration in the United States. Generally, the longer a foreign body has been lodged within the tracheobronchial tree, the greater the morbidity. Thus, an early diagnosis remains a key to successful and uncomplicated management of these accidents. Although this chapter deals exclusively with children, the same principles apply to the adult population.
The first extraction of an airway foreign body was performed by Gustav Killian near the end of the 19th century, as he describes in the following passage:
On March 27, 1897, whilst eating some soup, [J.W.] aspirated a bone. This accident was followed by attacks of violent cough and dyspnoea, which, however, became gradually less On direct laryngeal examination by means of Kirstein's spatula, the patient being seated with his head strongly deflected to the left, I saw in the right principal bronchus a white mass. On the following day I introduced, under cocaine anaesthesia, a straight tube of 9 millimetres diameter and 25 centimetres length through the larynx and the trachea until I came near the foreign body. The curvature of the trachea was thus removed, and the foreign body could be seen distinctly. I had great difficulty in catching hold of the foreign body, using a pair of slender forceps which had specially and quickly been made. The difficulties were great, as at that time I was still without the necessary practice which enables one to look easily, and even more to operate, through long tubes. Eventually I succeeded in catching the bone and in extracting it. The patient was able to return home on the following day (Killian, 1902).
The basic principles of extraction were meticulously developed by Chevalier Jackson during the first half of the 20th century. Jackson's concepts of the various mechanical problems and demonstrations of their solutions remain valid today. At any given institution, airway foreign body problems should be managed by the individuals with the best training and most experience, regardless of their particular subspecialty. As Jackson (1938) stated and Hughes and colleagues (1996) reiterated, the techniques of foreign body extraction should be mastered through practice on lung models and then on anesthetized laboratory animals before they are attempted in human beings.
EPIDEMIOLOGY AND ETIOLOGY
Older infants and toddlers constitute the vast majority of patients with foreign body aspiration. Darrow and Holinger (1995) reviewed multiple case series and found that children younger than 5 years account for approximately 84% of cases and children younger than 3 years account for 73%. The high incidence in this age group reflects the tendency of children to explore the world using their mouths. In addition, these children have not developed a full posterior dentition and may have immature neuromuscular mechanisms for swallowing and airway protection. Moreover, many youngsters are allowed to talk, run, or play with food or other objects in their mouths. For uncertain reasons, boys aspirate foreign bodies more frequently than girls by a ratio of approximately 2:1. In adults, other factors play a role in foreign body aspiration, such as neurologic dysfunction, dental trauma, and aspiration of larger than normal pieces of food, usually associated with alcohol consumption.
Although adults most commonly aspirate bones from fish, birds, or small mammals, children usually aspirate vegetable matter. Darrow and Holinger (1995) found that nuts, particularly peanuts, account for approximately 34% of cases of foreign bodies found in the pediatric airway. Even nut fragments found in crunchy peanut butter have been aspirated. Other commonly aspirated types of vegetable matter include pieces of raw carrot, apple, dried beans, popcorn, and sunflower, watermelon, or pumpkin seeds. Darrow and Holinger (1995) found that the most commonly aspirated inorganic objects in school-aged children include tacks, nails, pencil erasers, pins, plastic beads, and even marbles.
P.996
The spectrum of airway foreign bodies varies from country to country, depending on the diet and customs of the population. For example, Mu and colleagues (1990) reported that in mainland China, nearly 95% of aspirated foreign bodies in children were organic. In contrast, more industrialized countries have a greater incidence of aspiration of plastic foreign bodies, because plastic parts are used frequently by the toy industry. Other reported examples of the cultural influence on these accidents include aspiration of Mardi Gras beads, pieces of crab shell, holiday decorations and gifts, and straight pins by Middle Eastern women and girls, who hold the pins between their lips while securing their head scarves. Fortunately, ingestion of safety pins has become rare since the advent of disposable diapers. Rarely, medical therapy itself may be responsible. Aspiration of pills, a thermometer fragment, and an object within a metered-dose inhaler have been reported.
HISTORY
Three stages of symptoms result from the aspiration of an object into the airway:
Initial event. Violent paroxysms of coughing, choking, and gagging, and possibly airway obstruction, occur immediately after a foreign body is aspirated. An esophageal foreign body large enough to cause posterior tracheal compression may cause similar symptoms. Such a history can be elicited in most cases, but unfortunately many parents tend to downplay the significance of such an event or do not recall the incident until after the foreign body has been extracted. Some parents engage in wishful thinking and minimize the symptoms, hoping that nothing is wrong and that no surgical intervention will be required. Older children often are reluctant to admit to such an episode for fear of being punished.
Asymptomatic interval. During the second stage, the foreign body becomes lodged, reflexes fatigue, and the immediate irritating symptoms subside. This stage is the most treacherous and accounts for a large percentage of delayed diagnoses and overlooked foreign bodies. It is during this second stage that the physician is inclined to minimize the possibility of a foreign body accident, being reassured by the absence of signs and symptoms.
Complications. In the third stage, obstruction, erosion, or infection develop and again direct attention to the presence of a foreign body. Signs include fever, cough, and hemoptysis. Complications include formation of bronchial granulation tissue, atelectasis, pneumonia, lung abscess, and, eventually, bronchocutaneous fistula. Such complications occur more rapidly after aspiration of vegetable matter and sharp objects than of plastics and other biologically inert materials.
The current medical practice of treating an asthmatic or croupy child with antibiotics or corticosteroids may obscure signs and symptoms that normally would be expected with a retained foreign object. Clearing of symptoms with these agents cannot always be assumed to be diagnostic of a specific disease process. The fact that a wheeze disappears or a pneumonic process temporarily clears may merely mean that the patient's reaction to a foreign body has been controlled temporarily. The recurrence of asthma after tapering of therapy should heighten a physician's suspicion of an aspirated foreign body.
A positive history must never be ignored. A negative history may be misleading. Choking or coughing episodes accompanied by wheezing are highly suggestive of foreign body aspiration. The literature reveals that diagnosis is delayed more than 24 hours in 50% of cases, as noted by Wiseman (1984), and more than 1 week in 15% of cases, as reported by Reilly and colleagues (1997). Disregarding a child's story because of age or lack of symptoms may cause a delay in diagnosis, which may make removal more difficult and complicated. As Wetmore (1994) stated, once an aspirated foreign body is suspected, the burden of proof is on the bronchoscopist. Furthermore, Mantor and colleagues (1989) suggested that some negative bronchoscopies are necessary in order to prevent the morbidity that occurs from a missed foreign body aspiration.
PHYSICAL EXAMINATION
Laryngeal Foreign Bodies
Large globular foreign bodies that become lodged between the vocal cords usually cause complete obstruction and asphyxiation unless promptly expelled. Flat, thin, and sharp objects, such as eggshell and bone, may become lodged between the vocal cords in the sagittal plane. Dysphonia, croupy cough, stridor, and varying degrees of dyspnea ensue, all of which increase as edema and inflammation progress. Odynophagia may occur also.
Tracheal Foreign Bodies
Jackson and Jackson (1936) described three features of tracheal foreign bodies. The audible slap and the palpatory thud result from the impact of a mobile foreign body against the tracheal wall on deep inspiration or coughing. The asthmatoid wheeze results from partial bronchial obstruction from the foreign body and the inflammatory reaction. Biphasic stridor also may occur if the foreign body is within the extrathoracic trachea.
Bronchial Foreign Bodies
Wiseman (1984) noted that the classic triad of wheezing, coughing, and decreased air entry to the obstructed side was
P.997
present in only 31% of children examined within 24 hours of bronchial foreign body aspiration and only 47% of children examined after 24 hours. Moreover, physical signs may change rapidly with migration of the foreign body and with the development of edema and infection. If the foreign body eventually lodges within one bronchus, the physical examination may stabilize.
RADIOLOGIC EVALUATION
Inspiratory and expiratory posteroanterior and lateral chest radiography is standard when foreign body aspiration is suspected. If the foreign body is radiopaque, a film is taken in the greatest diameter of the object for accurate localization before endoscopy. More than 90% of foreign bodies, however, are radiolucent, as reported by Vane and colleagues (1988). This percentage is likely to increase as more polyethylenes are used to make toys.
Jackson and Jackson (1950) described the pathophysiology behind the radiographic diagnosis of radiolucent bronchial foreign bodies. Initially, the object creates a bypass valve, which still allows ingress and egress of air. At this stage, radiography results are normal. As edema of the surrounding bronchial wall develops, a check valve is created. On inspiration, the bronchus dilates and permits ingress of air. However, on expiration, the bronchus constricts, and contact of the edematous bronchus with the foreign body blocks the egress of air. Thus, air trapping (obstructive emphysema) results. Radiographically, when a check valve is created, the inspiratory film is normal, whereas the expiratory film shows hyperinflation of the affected lung and shift of the mediastinum to the opposite side (Fig. 73-1). If inspiratory and expiratory films are not possible because a child is tachypneic or uncooperative, lateral decubitus chest films or fluoroscopy may also identify air trapping. Eventually, when enough edema develops to block both ingress and egress of air, a stop valve is created. Obstructive atelectasis is seen radiographically. This late complication usually takes days or weeks to develop.
Although reports vary, Black and colleagues (1994) found that inspiratory and expiratory chest radiography was diagnostic in 83% of 440 children with tracheobronchial foreign bodies. In cases of suspected tracheal foreign bodies, posteroanterior and lateral soft tissue neck films (high-kilovoltage airway films) are the radiographic tests of choice. As Esclamado and Richardson (1987) reported, airway films are abnormal in 92% of children with tracheal foreign bodies, whereas chest radiography is abnormal in only 58%. Pneumomediastinum is a rare but highly diagnostic finding. It was reported by Burton and colleagues (1989) in 7% of patients with tracheobronchial foreign bodies. When a radiolucent foreign object's aspiration is suspected and the airway or chest radiography is negative, one may take a radiograph of a duplicate object if available. If the object appears to be radiopaque, then the absence of finding on the radiograph is reassuring.
In rare cases, when a radiolucent foreign object is lodged too far in the lung periphery for endoscopic management, it may be precisely localized by bronchography, computed tomography, or in certain cases, magnetic resonance imaging. Imaizumi and colleagues (1994) noted that because of
P.998
peanuts' high lipid content, peanut fragments appear as high-intensity signals on T1-weighted images. Such information would confirm the diagnosis and would assist in localization if thoracotomy and segmentectomy were to become necessary.
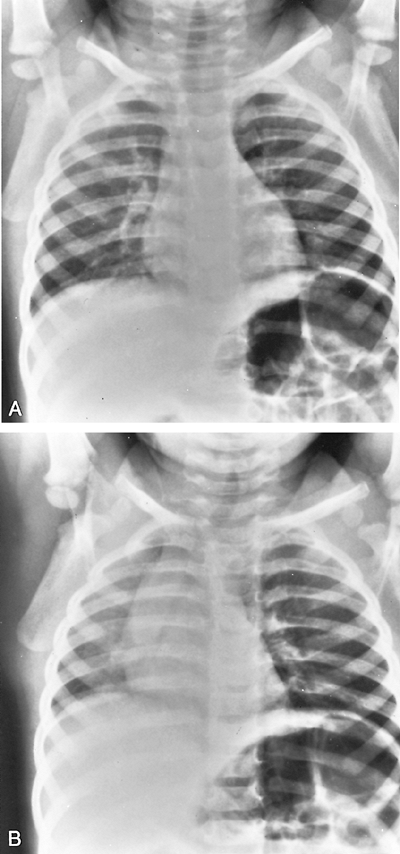 |
Fig. 73-1. A. Anteroposterior radiograph of the chest during inspiration. B. Anteroposterior radiograph of the chest during expiration. Note the trapping of air in the left lung field caused by a peanut in the left main-stem bronchus. |
TREATMENT
A bronchial foreign body usually does not constitute an acute emergency unless there is complete obstruction of one main bronchus, causing inadequate oxygenation. Supraglottic, glottic, and tracheal foreign bodies are more likely to cause acute emergent situations with severe respiratory distress. In general, the treatment of choice is reasonably prompt endoscopic removal under conditions of maximum safety and minimum trauma. Too often, foreign bodies are considered emergencies, leading to hasty, inadequate preoperative planning and poorly prepared, improper attempts at removal. Most patients with foreign bodies who have come to the endoscopic surgeon have already passed the acute phase. When no urgent danger to the patient's life exists, the problem should be approached with complete and thoughtful consideration of the physiologic and mechanical factors involved.
The endoscopic removal can be scheduled once trained personnel are available, instruments have been checked, and techniques have been tested. However, untoward delay of bronchoscopic removal is potentially harmful because the foreign body may become dislodged from the bronchus and impacted in the larynx, causing asphyxiation. Therefore, endoscopy is deferred only until preoperative studies have been obtained and the patient has been prepared for surgery by adequate hydration and emptying of the stomach. Foreign bodies in the larynx or tracheobronchial tree are usually removed on the same day the diagnosis is considered.
Two situations exist, however, in which an airway foreign body does constitute an acute emergency: actual and potential airway obstruction.
Actual or Potential Airway Obstruction
The most serious complication of foreign body aspiration is complete obstruction of the airway. Globular food objects, such as hot dogs, grapes, nuts, and candies, are the most frequent offenders, whereas rubber balloons and other toys are common among nonfood objects. Large or multiple esophageal foreign bodies also can cause airway obstruction, by posterior compression. Stephen Bradwell remarked on the matter in 1633: Of Things that endanger stopping of the breath in swallowing, some are Sharp, and some Blunt. I have heard of a Child in Woodstreet strangled with a Grape.
Although the yearly death toll from foreign body aspiration in the United States remains at approximately 3,000, the incidence of asphyxiation in the pediatric population has demonstrated a progressive decline. Among children between birth and 4 years of age, 650 died of foreign body ingestion in 1968. By 1990, this number had decreased to 261. As Ryan and colleagues (1990) reported, this trend probably is the result of improved public awareness and prevention, the development of rapid-response paramedic teams, and the introduction of and public education about the Heimlich maneuver.
Hot dogs rarely are seen as foreign bodies by the endoscopist. Toddlers who choke on hot dogs usually asphyxiate on the spot unless the incident is recognized and treated at the scene. Hot dogs are the most common cause of food asphyxiation, either by complete obstruction of the oropharynx, hypopharynx, or the glottic larynx. Recognition of complete airway obstruction is critical to the success of first aid efforts. Coughing, gagging, and throat clearing are reflexes that protect the airway and are indications that the obstruction is not complete. First aid delivered to such a patient is unnecessary and potentially dangerous. Probing the hypopharynx with a finger may drive a loose foreign body into the larynx, transforming a partial obstruction into a complete obstruction.
The foreign body also may be forced into the esophagus, where compression of the trachea against the upper sternum may cause an obstruction that cannot be relieved even by tracheotomy. Similarly, back blows with the victim inverted also are ill advised in the incompletely obstructed child. Such treatment may cause a bronchial foreign body to lodge in the glottis from below, precipitating complete obstruction.
Complete airway obstruction may be recognized in the conscious child as sudden respiratory distress with an inability to speak or cough. An older child or adult might use the choking distress signal, which is the gesture of clutching the neck between the thumb and index finger. In the completely obstructed patient, attempts at rescue breathing are unsuccessful, resulting in no chest expansion.
The best management of the child with complete airway obstruction caused by foreign body aspiration is controversial and evolving. Committee on Accident and Poisoning Prevention of the American Academy of Pediatrics (1990) revised its policy statement on first aid for the choking child to advocate back blows followed by chest thrusts as primary therapy for infants. Because of the risk of rupture of abdominal viscera, abdominal thrusts are not recommended for children younger than 1 year. For all others, abdominal thrusts as described by Heimlich (1975) are recommended. If laryngeal obstruction persists despite these efforts, cardiopulmonary resuscitation should continue until skilled medical personnel and appropriate equipment are available to secure the airway via laryngoscopy and foreign body extraction, cricothyroidotomy, or tracheostomy. These recommendations conform with those of the American Heart Association and the American Red Cross for both children and adults.
 |
Fig. 73-2. When 8-year-old J. B. fell into a huge trailer filled with soybeans, he essentially drowned, aspirating multiple soybeans, four of which are seen on the left. The two soybeans on the right were brought in by his father for comparison. They contained approximately 13% moisture when harvested from the field and are about one-half the size of the moisture-swollen beans that were extracted from the tracheobronchial tree. Despite preoperative cyanosis, the patient recovered without sequelae. From Holinger LD: Foreign bodies of the airway and esophagus. In Holinger LD, Lusk RP, Green CG (eds): Pediatric Laryngology and Bronchoesphagology. Philadelphia: Lippincott Raven, 1997, p. 236. With permission. |
P.999
Dried Beans or Peas
When a main bronchus is obstructed by a dried bean or pea for more than 24 hours, absorbed moisture may cause the capsule to burst (Fig. 73-2). As the bean rapidly swells, the airway becomes increasingly obstructed. If the patient does not asphyxiate, the swelling at least obliterates forceps spaces, making the technical aspects of bronchial foreign body extraction extremely difficult. Most children raised on farms are taught from a young age not to play near large containers of dried beans or peas, to prevent drowning and asphyxiation.
Similarly, a sucralfate tablet can also cause rapid airway obstruction, even in adults. Overdahl and Wewers (1994) hypothesized that obstruction occurs because an aspirated sucralfate tablet not only expands rapidly but also binds to mucosa. The sooner such a patient undergoes bronchoscopy, the greater the probability of a successful endoscopic retrieval.
Disc Battery Ingestion and Esophageal Perforation
The bronchoesophagologist may encounter two other foreign body situations that mandate urgent intervention: disc battery ingestion with esophageal lodging and esophageal perforation. Maves and colleagues (1984) demonstrated that disc batteries cause esophageal mucosal damage after 1 hour, erosion into the muscular layers within 2 to 4 hours, and esophageal perforation within 8 to 12 hours. Thus, a disc battery that is lodged in the esophagus must be removed urgently. Similarly, any patient exhibiting signs and symptoms of esophageal perforation should undergo prompt confirmatory diagnostic studies followed by retrieval of the foreign body and appropriate medical and surgical therapy. Discussion of esophageal foreign bodies is presented in Chapter 137.
Preoperative Preparation
When foreign body aspiration is not an acute emergency, the endoscopist gathers as much information as possible and prepares equipment before the patient enters the operating room. If the parents know what the foreign body might be, they are asked to return home to obtain a duplicate. If this is not possible, they are asked to draw the object as accurately as possible. They are questioned carefully about the object's size, color, and texture. When a duplicate object can be obtained, it is tested to determine which bronchoscope and forceps are best suited for extraction. When the object has multiple contours, a method of disimpaction, disentanglement, or eversion and seizure should be worked out for each possible presentation. As Holinger (1962) pointed out, if two hours are spent in such preparation, the safe endoscopic removal of the foreign body may take only two minutes. But if only two minutes are taken for preparation, the endoscopist may find himself attempting makeshift ineffective procedures for the next frustrating two hours.
Because the patient's family may be distraught, the preoperative discussion with them is an essential part of the preparation for endoscopy. The risks of the procedure, including complete airway obstruction, the need for temporary tracheotomy, possible rupture of the trachea or bronchi, and failed extraction are discussed, but in such a way that the patient or parents do not delay the procedure unnecessarily. A thorough medical history is taken and careful assessment of the patient's general medical condition is carried out. This may include additional laboratory studies and control of medical problems such as dehydration or asthma and cardiac conditions in adults. Patients with sharp and potentially contaminated foreign bodies are also given tetanus prophylaxis.
Instrumentation
Rigid bronchoscopes are the instruments of choice for foreign body extraction, especially within the pediatric airway. The major drawback of flexible instruments is that they lack control of the foreign body and provide inadequate control of the airway. The rigid bronchoscopes are available in a greater range of size, allow the use of a greater variety of forceps, provide better exposure of the foreign body, and permit sheathing of sharp points within the tube during extraction. The flexible bronchoscope may be of some help in a patient who is unable to extend the head and neck or in the occasional adult patient with a foreign body lodged far in the lung periphery.
P.1000
For pediatric airway foreign body extraction, the 3.75-cm by 30.0-cm Doesel-Huzly rigid bronchoscope with rod-lens telescope is most commonly used. In general, the shortest, widest bronchoscope that atraumatically reaches the foreign body is chosen. Two laryngoscopes and two bronchoscopes are lighted and available; should a light fail or a forceps become jammed in the scope, a backup is immediately available.
Passive-action forceps offer a wide range of blades for the various types of mechanical problems. Four types exist: forward-grasping, rotation, ball-bearing (globular object), and hollow-object forceps. At least 60 variations of these four basic types have been designed. Positive-action forceps have the advantage of a narrower shaft and have the capacity to dilate a bronchus. This may be critical when a round object is wedged in a distal bronchus and forceps spaces are not apparent. The blades of the positive-action forceps can be used to dilate the bronchial wall to advance past the equator of the object.
The standard forward-grasping forceps has a powerful grip that pulls the object proximally. It is useful for dense foreign bodies that require a firm grasp to prevent stripping off. For more delicate manipulation, and particularly for friable foreign bodies, a lighter forceps such as a fenestrated peanut forceps or a positive-action forceps with delicate curved blades is best. A magnified view may be obtained with a rod-lens telescope or the optical forceps. Optical forceps have become popular because visualization is so superior to other techniques (Fig. 73-3). Finally, a large alligator forceps is selected in case the foreign body becomes stripped off or dropped in the larynx or hypopharynx.
A complete instrumentation is essential. Failure to remove a foreign body or loss of a patient can never be excused or justified by the lack of proper equipment. Many of the complications and failures of attempted foreign body removal arise because the endoscopist lacks the instruments specifically designed for the problem. This is not a valid excuse, but merely a regrettable explanation of the failure. If a full range of rigid scopes and foreign body forceps is not available, the procedure should not be attempted.
The equipment must be in perfect repair and working order. The forceps are adjusted and lubricated so that they are smooth in operation and the blades close completely when the handles are closed. At least two forceps are selected before surgery because unexpected circumstances arising during the procedure may require an alternative instrument. Potential problems may arise if instruments are wrapped in sterile packages and kept in storage areas outside the endoscopy suite.
Surgical Team
Adequate training and experience are important for the anesthesiologist, nursing personnel, and endoscopist. The importance of cooperation, communication, and a team approach to foreign body extraction cannot be overemphasized. The anesthesiologist, scrub nurse, circulating nurse,
P.1001
and endoscopist all must have experience with the extraction of foreign bodies. If such a team cannot be assembled promptly, consideration should be given to delaying the procedure until they are available. A plan for orderly removal of the object is discussed with each member of the team, and his or her role in that plan is delineated clearly. The procedure is not begun until all members of the team are prepared and positioned appropriately.
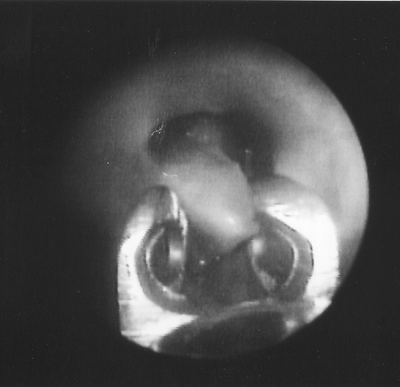 |
Fig. 73-3. Endoscopic view of an optical forceps used to extract a peanut segment from the right main bronchus. |
Anesthesia
General anesthesia is used for endoscopic extraction of foreign bodies. In children, preoperative sedation is generally avoided. Instead, the parents, anesthesiologist, and nursing staff help keep the child calm before induction to avoid dislodgment of the foreign body because of crying. In adults, small amounts of a short-acting anxiolytic in a monitored setting often are of benefit to keep the patient calm. Electrocardiography, pulse, oxygen saturation, and end-tidal carbon dioxide are routinely monitored. A large-bore intravenous catheter is placed.
Spontaneous respiration during the procedure is preferred because it is somewhat safer than apneic techniques in which the patient is completely paralyzed and therefore cannot move any air if the airway is temporarily lost. Positive-pressure ventilation (bagging) is avoided because this tends to drive the foreign body further peripherally. As anesthesia lightens, an occasional cough actually may help propel the foreign body toward the bronchoscope.
For children, a short-acting inhalation anesthetic is delivered through the closed system of a rigid bronchoscope. In adults, agents such as propofol may be the anesthetic of choice. The larynx and trachea are sprayed with topical 4% lidocaine before the bronchoscope is introduced. Once the bronchoscope is in place, lidocaine also can be administered to the bronchi. During the actual attempts at extraction, 100% oxygen is given through the bronchoscope. If spontaneous respiration is not possible due to bronchial hyperactivity, short-acting, nondepolarizing muscle relaxant may be used with ventilation maintained at lower tidal volumes during extraction attempts.
Basic Technique
Prepared by practice with a duplicate of the foreign body and review of the radiographs, the surgeon introduces the bronchoscope. Once the bronchoscope has been advanced into the trachea, ventilation is established and confirmed by the endoscopist. The tracheobronchial tree is inspected completely because multiple foreign bodies are present in up to 9% of cases, as emphasized by Hughes and colleagues (1996). Inspection begins with the normal bronchus. All secretions are aspirated to ensure optimal respiratory function when the involved side is inspected. The location of the foreign body is approached slowly and carefully to avoid overriding or displacement. Care is taken to avoid driving the foreign body further down. Suction is used to remove secretions from around the foreign body, but it is not used in the attempt at extraction.
The endoscopist must resist the impulse to seize the foreign body as soon as it is discovered. Before any attempt at extraction, a careful study is made to determine the size, shape, position, probable location of unseen parts, and relation to surrounding structures. As determined by the appearance of the presenting part, combined with the knowledge obtained from the radiographic studies, the endoscopist may suspect that sharp points are buried deep within the mucosa or outside the wall in the mediastinum. The presentation of the foreign body may be modified with the tip of the scope, a technique that is especially helpful when establishing forceps spaces between the object and the lumen walls. When the most favorable position for grasping has been ascertained, the closed forceps is inserted through the scope.
All manipulation is gentle and delicate. The forceps is advanced until it lightly touches the foreign body, and the endoscope is withdrawn a short distance to permit the forceps blades to be opened. The forceps blades are advanced until the tips pass the equator of the object; then the forceps blades are closed. The tip of the scope is advanced against the foreign body, which is held against the tube mouth. The grasp of the forceps is maintained firmly by the fingers of the right hand while all traction for withdrawal is made by the left hand. The thumb of the left hand firmly clamps the forceps to lock the relationship between the forceps and the scope during extraction so that the three units are extracted as one. The bronchoscope keeps the vocal cords apart until the foreign body has exited the glottis. Just before exiting the glottis, the foreign body is rotated to the sagittal plane, which is the largest diameter of the laryngeal lumen.
After removal of a foreign body from the tracheobronchial tree, the laryngoscope is reinserted and a second pass is made with the bronchoscope. Retained secretions are aspirated, and the entire tracheobronchial tree is rechecked to be certain that no fragments or other objects remain. Granulation tissue is resected as necessary, and bleeding can be controlled with a topical vasoconstrictive agent. For children, oxymetazoline probably has the greatest therapeutic index for the respiratory mucosa, as demonstrated by Riegle and colleagues (1992), but dilute epinephrine (1:10,000 v/v) and iced saline provide adequate control in adults.
Special Techniques
In the rare circumstance that a spherical foreign body cannot be removed, a Fogarty catheter may be lubricated and passed through the bronchoscope, distal to the object. The balloon is then inflated and withdrawn in order to dislodge the object proximally and allow its extraction. Good
P.1002
and Deutsch (1998) suggest that a Fogarty catheter may be especially useful in the case of a hollow spherical object, such as a hair bead. If an object such as a marble cannot be successfully retrieved, a thoracotomy may be necessary. Even if the spherical object is withdrawn to the proximal trachea, the surgical team must be prepared to create a temporary tracheostomy for extraction in case it cannot pass through the glottis. If a thoracotomy is necessary, as with a marble in one main bronchus, the airway may be safely secured by intubation with a double-lumen endotracheal tube using flexible bronchoscopy. This will allow ventilation of the unaffected bronchus while thoracotomy and bronchotomy are carried out.
Special techniques have been developed for the extraction of pointed objects (Fig. 73-4). The endoscopist must resist being pressured into hasty action without thorough preparation. The first priority during the extraction procedure is to localize the point. The point is released and sheathed within the scope. It often is necessary to accomplish this by first moving the object distally to disengage the point, then advancing the scope over the object, rather than pulling the object into the tube.
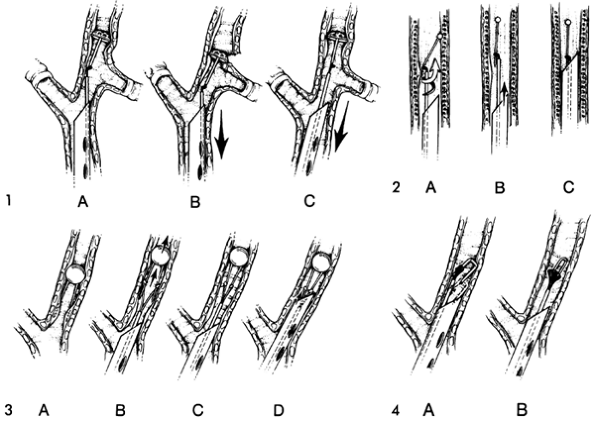 |
Fig. 73-4. Techniques of endoscopic removal. 1. Long-axis traction is particularly important for pointed objects with large heads. The point may be easily located (A), but greater hazard lies in the risk of tearing the bronchial wall with the head of the tack (B). Positioning the patient's head toward the opposite side straightens the axis of airway, permitting relatively safe, slow, and steady withdrawal of the object (C). 2. Inward rotation method is used for pins or needles with imbedded points. Side-grasping forceps capture pin near point (A). Corkscrew motion is used to push the pin distally while rotating it clockwise, freeing the point and aligning the shaft with the long axis of the forceps (B). The scope is advanced over the point to sheathe (C) for extraction. 3. Technique of managing bendable double-pointed objects. Points buried in the mucosal wall (A) are released by moving them distally (B). Points are approximated (C), then sheathed for extraction by advancing the rigid scope (D). 4. Tucker staple forceps (A) is angled to permit sheathing of both points within the beveled tip of the bronchoscope. Jackson broad-staple forceps (B) grasps and protects both points during advancement of the bronchoscope to sheathe them. From Holinger LD: Management of sharp and penetrating foreign bodies of the upper aerodigestive tract. Ann Otol Rhinol Laryngol 99:684, 1990. With permission. |
Long, pointed objects typically lodge with the point facing upward. This occurs even if the object enters point first. The point becomes engaged by the mucosa and the object tumbles, then proceeds with the point trailing. Pins, needles, and similar long, pointed objects fall into two categories: breakable needles and pins and bendable pins. A pin-bending forceps may be useful in extracting these objects.
Special techniques for long, pointed objects include aligning the bronchus to approach the object by its long axis. Biplane fluoroscopy may be of assistance in this situation. Magnets have been used also. Tacks, nails, and large-headed foreign bodies in the tracheobronchial tree are released, sheathed, and removed with an inward rotation method that is used for pins and needles with imbedded points. A side-grasping forceps captures the pin at the point. A corkscrew motion is used to push the pin distally while rotating it clockwise, freeing the point and aligning the
P.1003
shaft with the long axis of the forceps. The scope is then advanced over the point to sheath it for extraction.
Double-pointed objects sometimes can be bent to convert them to a single point for extraction. A broad-tack forceps or wide-staple forceps may be used to protect both points simultaneously during extraction.
When a point cannot be sheathed, the foreign body may be withdrawn with the point trailing. A rotation forceps allows a point to rotate and trail.
For a sharp bone that could not be safely dislodged, Boelcskei and colleagues (1995) described the use of the neodymium:yttrium-aluminum-garnet laser to cut the bone into smaller fragments to facilitate extraction.
Fluoroscopic assistance is used for radiopaque upper lobe foreign bodies, pins in the lung periphery, and sharp or irregular foreign bodies, such as dental bridge work. For accurate localization, simultaneous biplane fluoroscopy is required; it may be available only in a special procedures room within the radiology department. The technique is deceptively simple but extremely hazardous because the fluoroscope does not visualize the tissues that lie between the forceps blades and the foreign body.
Stripping Off
As a foreign body is brought out through the larynx, the lateral pressure of the vocal folds may strip it from the forceps grasp. Because complete airway obstruction ensues, a prompt, efficient response is required. The airway is reestablished immediately by removing the object or by pushing it down into the bronchus in which it had been lodged, allowing ventilation of the good lung. The faulty technique is corrected, and the object is relocated and extracted.
A foreign body lost in the trachea usually is carried into the normal bronchus. This occurs because the previously obstructed lung or lobe moves little air and is edematous or narrowed by granulation tissue. This creates an immediate and critical emergency because the patient's only functional lung is completely obstructed. The object must be removed immediately or relocated into the other bronchus. If the foreign body cannot be visualized readily, it may be found next to the scope, below the vocal folds, or in the mouth, hypopharynx, or nasopharynx.
Stripping off may result from factors related to the forceps or the foreign body itself. Forceps factors include faulty application of the forceps, use of the wrong forceps for the problem, mechanically imperfect forceps, and poorly adjusted or poorly constructed forceps. Three foreign body factors can lead to stripping off: poor orientation of the foreign body (solution: rotate 90 degrees at the vocal folds); insecure grasp of the foreign body (solution: sheath the foreign body with the end of the bronchoscope and lock the forceps against the bronchoscope with the left thumb); and a foreign body too large for the laryngeal lumen (solution: fragment the foreign body or remove it through a tracheotomy).
Postoperative Treatment
After endoscopic foreign body extraction, the patient is usually admitted to the hospital for overnight observation. Antibiotics are prescribed only if there was a preoperative diagnosis of pneumonia. In cases of pneumonia or purulent bronchitis, chest physical therapy is indicated. On the day after the procedure, if the patient is afebrile and the lungs are clear to auscultation, the patient is discharged home. However, if the patient remains febrile or has persistent pulmonary signs or symptoms, chest radiography is performed and appropriate therapeutic measures are taken.
COMPLICATIONS
Immediate complications of endoscopic extraction or attempted extraction include pneumomediastinum, laryngeal impaction and complete obstruction, and failure to recover the object, which necessitates thoracotomy. In the recovery room, laryngeal edema or bronchospasm may compromise the airway. Late complications include pneumonia, atelectasis, and granuloma or stricture formation, with their resulting problems.
Traumatic laryngitis and laryngeal edema are treated with elevation of the head of the bed, humidity, racemic epinephrine, and high-dose corticosteroids (1 mg/kg of dexamethasone, up to 20 mg, intravenously as a bolus). When laryngeal edema is anticipated, corticosteroid therapy should be initiated in the operating room. Laryngeal edema is proportional to the time the bronchoscope is in the larynx, the trauma of the procedure, and the size of the bronchoscope in relation to the size of the larynx. To prevent laryngeal edema, smaller bronchoscopes that pass easily through the larynx are preferred, although there may be a slight leak if positive pressure is required.
Repetition of any endoscopic procedure after an unsuccessful attempt at removal is avoided until laryngeal symptoms resolve. Three to 7 days usually is adequate. It is wise to use this waiting period in patients who have had previous attempts at endoscopic extraction elsewhere. The presence of severe respiratory obstruction is an obvious exception to these guidelines.
If the initial attempt at endoscopic extraction is unsuccessful because of abundant, bleeding granulation tissue and purulent bronchitis, the patient should be treated for approximately 3 days with intravenous and nebulized dexamethasone and intravenous antibiotics. Such treatment has resulted in dramatic resolution of the granulation tissue before endoscopic extraction has been reattempted.
The foreign body aspirated by children that is most likely to result in failed endoscopic extraction is the flowering
P.1004
head of grasses. Jackson (1952) noted that by means of its long, stiff bristles, the grasshead propels itself through tissues with each breath, until it emerges days to months later via a bronchocutaneous fistula. At bronchoscopy, usually only granulation tissue and purulent secretions are seen. Thus, thoracotomy and segmentectomy are almost always indicated.
Complications of Nonendoscopic Means of Foreign Body Extraction
Postural drainage (chest physical therapy) and bronchodilators were suggested by Burrington and Cotton (1972) as an alternative to bronchoscopic removal of airway foreign bodies. This ill-advised and poorly conceived technique has led to at least four cases of respiratory arrest, one of which also involved transient cortical blindness. This throwback to the 19th century does no more than serve as a makeshift alternative for those who are unskilled in modern bronchoscopic techniques. Although Campbell and associates (1982) retracted this recommendation for the treatment of foreign bodies in the main bronchi, they continue to advocate its use for peripheral foreign bodies. In a subsequent series of 28 such cases, only 18 were treated successfully with this therapy. Endoscopic extractions salvaged 8 of the 10 failures.
PREVENTION
Potentially all cases of foreign body aspiration are preventable. In 1923, Jackson initiated the first public awareness campaign, directed chiefly at parents, teachers, and nurses. Continued public education is of paramount importance. A reasonable goal would be to instruct every caregiver about foreign body aspiration prevention strategies and first aid techniques at their first visit with a pediatrician. An informative pamphlet entitled Choking Prevention and First Aid for Infants and Children: Guidelines for Parents is available from the American Academy of Pediatrics (1990).
Continued vigilance by the Consumers Products Safety Commission is also necessary. In 1979, the Consumers Products Safety Commission issued federal regulations to ban certain toys from children under 3 years of age. Hazardous toys are identified by their ability to pass through a small parts cylinder. However, as Reilly (1990) noted, many spherical objects that have caused childhood asphyxiation actually pass this test. Therefore, tighter standards in toy testing are indicated.
Foods could also be made safer. In 1984, Harris and colleagues suggested that the U.S. government adopt labeling regulations for dangerous food products, as is done in Sweden. For example, package labels should instruct parents not to feed nuts or crunchy peanut butter to children under 4 years of age. Additionally, labels should instruct parents not to feed hot dogs or grapes to toddlers unless these foods are cut into small quarter sections.
Despite such measures, it is unlikely that all cases of foreign body aspiration can be prevented. Therefore, prevention of unnecessary complications should be considered. As stated initially, a key to preventing complications is an early diagnosis. Schimpl and colleagues (1991) found that the complication rate of pediatric foreign body aspiration is increased 17 times when bronchoscopy is delayed more than 12 hours.
For adults, identification of patients, particularly older patients who have primary or secondary deglutition disorders, will help. These patients and their caregivers should be instructed in prevention of aspiration. Prevention of aspiration of large boluses of food by healthy adults may be impossible. Therefore, posters of the Heimlich maneuver should be displayed conspicuously in restaurants and bars. Instruction in the technique in classrooms may also help save lives.
REFERENCES
American Academy of Pediatrics: Choking Prevention and First Aid for Infants and Children: Guidelines for Parents. Elk Grove Village, IL: American Academy of Pediatrics, 1990.
Black RE, Johnson DG, Matlak ME: Bronchoscopic removal of foreign bodies in children. J Pediatr Surg 29:682, 1994.
Boelcskei PL, Wagner M, Lessnau KL: Laser-assisted removal of a foreign body in the bronchial system of an infant. Lasers Surg Med 17:375, 1995.
Bradwell S: Helps for Sudden Accidents Endangering Life. London: Thomas Purfoot, 1633.
Burrington JD, Cotton EK: Removal of foreign bodies from the tracheobronchial tree. J Pediatr Surg 7:119, 1972.
Burton EM, et al: Pneumomediastinum caused by foreign body aspiration in children. Pediatr Radiol 20:45, 1989.
Campbell DM, Cotton EK, Lilly JR: A dual approach to tracheobronchial foreign bodies in children. Surgery 91:178, 1982.
Darrow DH, Holinger LD: Foreign bodies of the larynx, trachea, and bronchi. In Bluestone CD, Stool S, Kenna MA (eds): Pediatric Otolaryngology. 3rd Ed. Philadelphia: WB Saunders, 1995.
Esclamado RN, Richardson MA: Laryngotracheal foreign bodies in children. Am J Dis Child 141:259, 1987.
Good GA, Deutsch ES: Method for removing endobronchial beads. Ann Otol Rhinol Laryngol 107:291, 1998.
Harris CS, et al: Childhood asphyxiation by food. A national analysis and overview. JAMA 251:2231, 1984.
Heimlich HJ: A life-saving maneuver to prevent food-choking. JAMA 234:398, 1975.
Holinger PH: Foreign bodies in the air and food passages. Trans Am Acad Ophthalmol Otolaryngol 66:193, 1962.
Hughes CA, Baroody FM, Marsh BR: Pediatric tracheobronchial foreign bodies: historical review from the Johns Hopkins Hospital. Ann Otol Rhinol Laryngol 105:555, 1996.
Imaizumi H, et al: Definitive diagnosis and location of peanuts in the airways using magnetic resonance imaging techniques. Ann Emerg Med 23:1379, 1994.
Jackson C: The Life of Chevalier Jackson. New York: Macmillan, 1938.
Jackson CL: Grasses as foreign bodies in the bronchus and lungs. Laryngoscope 62:897, 1952.
Jackson C, Jackson CL: Diseases of the Air and Food Passages of Foreign Body Origin. Philadelphia: WB Saunders, 1936.
Jackson C, Jackson CL: Bronchoesophagology. Philadelphia: WB Saunders, 1950.
P.1005
Killian G: Direct endoscopy of the upper air-passages and oesophagus: its diagnosis and therapeutic value in the search for and removal of foreign bodies. J Laryngol Rhinol Otol 17:461, 1902.
Mantor PC, Tuggle DW, Tunell WP: An appropriate negative bronchoscopy rate in suspected foreign body aspiration. Am J Surg 158:622, 1989.
Maves MD, Carithers JS, Birck HG: Esophageal burns secondary to disc battery ingestion. Ann Otol Rhinol Laryngol 93:364, 1984.
Mu LC, Sun DQ, He P: Radiological diagnosis of aspirated foreign bodies in children: review of 343 cases. J Laryngol Otol 104:778, 1990.
National Safety Council: Accident Facts. Chicago: National Safety Council, 1997.
Overdahl MC, Wewers MD: Acute occlusion of a mainstem bronchus by a rapidly expanding foreign body. Chest 105:1600, 1994.
Reilly JS: Prevention of aspiration in infants and young children: federal regulations. Ann Otol Rhinol Laryngol 99:273, 1990.
Reilly JS, et al: Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope 107:17, 1997.
Riegle EV, et al: Comparison of vasoconstrictors for functional endoscopic sinus surgery in children. Laryngoscope 102:820, 1992.
Ryan CA, et al: Childhood deaths from toy balloons. Am J Dis Child 144:1221, 1990.
Schimpl G, et al: Foreign body aspiration in children. The advantages of emergency endoscopy and foreign body removal [in German]. Anaesthesist 40:479, 1991.
Vane DW, et al: Bronchoscopy for aspirated foreign bodies in children. Experience in 131 cases. Arch Surg 123:885, 1988.
Wetmore RF: Foreign bodies of the aerodigestive tract. In Gates GA (ed): Current Therapy in Otolaryngology Head and Neck Surgery. 5th Ed. St. Louis: Mosby Year Book, 1994.
Wiseman NE: The diagnosis of foreign body aspiration in childhood. J Pediatr Surg 19:531, 1984.
EAN: 2147483647
Pages: 203