47 - Chest Wall Reconstruction
Editors: Shields, Thomas W.; LoCicero, Joseph; Ponn, Ronald B.; Rusch, Valerie W.
Title: General Thoracic Surgery, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > Volume I - The Lung, Pleura, Diaphragm, and Chest Wall > Section XI - The Pleura > Chapter 57 - Physiology of Pleural Fluid Production and Benign Pleural Effusion
Chapter 57
Physiology of Pleural Fluid Production and Benign Pleural Effusion
Richard W. Light
The author (2001) has estimated that more than 1 million cases of pleural effusions occur annually in the United States. The possibility of a pleural effusion should be considered whenever a patient with an abnormal chest radiograph result is evaluated. Increased densities on chest radiography are frequently attributed to parenchymal infiltrates when they actually represent pleural fluid. Free pleural fluid is best demonstrated with lateral decubitus chest radiography, ultrasonography, or computed tomographic (CT) scans. If, on lateral decubitus chest radiography or ultrasonography, the distance between the inside of the chest wall and the outside of the lung is greater than 10 mm, a diagnostic thoracentesis is usually indicated. If this distance is less than 10 mm, the pleural effusion is probably not clinically significant and a thoracentesis is not indicated. The presence of loculated pleural fluid is best demonstrated with ultrasonography.
FORMATION AND RESORPTION OF PLEURAL FLUID
Pleural fluid has several possible origins. It can originate in the capillaries in the parietal or visceral pleura. It can come from the interstitial spaces of the lung, or it can come from the peritoneal cavity through small holes in the diaphragm. Wiener-Kronish and co-workers (1984) have reported that the rate of entry of fluid into the pleural space in normal individuals is approximately 0.01 mL/kg per hour.
Capillary Origin
The movement of fluid across the pleural membranes is believed to be governed by Starling's law of transcapillary exchange. When this law is applied to the pleura:
![]()
where QF is the liquid movement; Lp is the filtration coefficient per unit area or the hydraulic water conductivity of the membrane; A is the surface area of the membrane; P and are the hydrostatic and oncotic pressures, respectively, of the capillary (cap) and pleural (pl) space; and d is the solute reflection coefficient for protein, a measure of the membrane's ability to restrict the passage of large molecules. Kinasewitz and colleagues (1984) have estimated that d is approximately 0.80 in humans.
Estimates for the magnitude of the pressures affecting fluid movement in and out of the pleural space are shown in Fig. 57-1. When the parietal pleura is considered, a gradient for fluid filtration is normally present. The hydrostatic pressure in the parietal pleura is approximately 30 cm H2O, whereas the pleural pressure is approximately -5 cm H2O. The net hydrostatic pressure gradient is therefore 30 - (-5)=35 cm H2O and favors the movement of fluid from the capillaries in the parietal pleura to the pleural space. Opposing this hydrostatic pressure gradient is the oncotic pressure gradient. The oncotic pressure in the plasma is approximately 34 cm H2O. Because the oncotic pressure of the small amount of pleural fluid is approximately 5 cm H2O, the net oncotic gradient is 34 - 5=29 cm H2O. Thus, the net gradient is 35 - 29=6 cm H2O, favoring the movement of fluid from the capillaries in the parietal pleura to the pleural space.
Albertine and co-workers (1984) have shown that the blood supply to the visceral pleura in humans is from the bronchial artery rather than the pulmonary artery. The net gradient for fluid movement across the visceral pleura in humans is probably close to zero. The pressure in the visceral pleural capillaries is approximately 6 cm H2O less than that in the parietal pleural capillaries because the former drain into the pulmonary veins. Because this is the only pressure that differs from those affecting fluid movement across the parietal pleura and because the net gradient for the parietal pleura is 6 cm H2O, it follows that the net gradient
P.807
for fluid movement across the visceral pleura is approximately zero. It is also quite likely that the filtration coefficient (Lp) for the visceral pleura is substantially less than that for the parietal pleura because Albertine and co-workers (1982) have shown that the capillaries in the visceral pleura are much farther from the pleural space than are those in the parietal pleura.
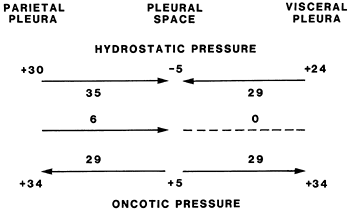 |
Fig. 57-1. Diagram of the various pressures that influence the movement of fluid in and out of the pleural space in humans. From Light RW: Pleural Diseases. 3rd Ed. Baltimore: Williams & Wilkins, 1995, p. 9. With permission. |
Interstitial Origin
Convincing evidence has been presented that the origin of a substantial percentage of pleural fluid is the interstitial spaces of the lung. Broaddus and co-workers (1990) have demonstrated that when sheep, a species with a pleura anatomically similar to that of humans, were volume overloaded by administration of 20% of their body weight as Ringer's lactate, transudative liquid flowed across the visceral pleura of the isolated, in situ lungs. The pleural fluid contained the same protein concentration as did the lung lymph and the interstitial edema liquid in the lung. The volume of pleural fluid constituted approximately 25% of all edema formed in the lung. In other experiments, Allen and colleagues (1989) have shown that with high-pressure pulmonary edema in sheep, pleural fluid accumulates only after pulmonary edema develops. In the clinical situation, Wiener-Kronish and co-workers (1985) have shown that in patients with congestive heart failure, the presence of pleural effusions on ultrasonography correlates more closely with the pulmonary venous pressure than with the systemic venous pressure and that the likelihood of pleural effusions increases as the severity of the pulmonary edema on chest radiography increases.
Exudates found in association with increased permeability pulmonary edema probably also originate from the lung interstitium. When Wiener-Kronish and associates (1988) induced increased permeability edema in sheep by the infusion of oleic acid, pleural fluid accumulated only after pulmonary edema developed. In this report, no detectable injury to the visceral pleura was seen by morphologic studies. They found that approximately 20% of the excess lung liquid that formed after oleic acid-induced lung injury was cleared from the lung through the pleural space. Other researchers have come to similar conclusions. Amouzadeh and colleagues (1991) concluded that the high-protein pleural effusion that developed in rats after the administration of xylazine had its origin in the parenchymal interstitial spaces of the lung. Bernaudin and associates (1986) made similar conclusions about the exudative pleural effusions induced by hypoxia in rats.
Peritoneal Origin
Fluid that is free in the peritoneal cavity can move directly into the pleural space if the diaphragm has holes in it. This mechanism is responsible for the pleural effusions that occur in conjunction with cirrhosis and ascites, pancreatic ascites, Meigs' syndrome, and peritoneal dialysis.
Lymphatic Clearance
Figure 57-1 might lead one to conclude that pleural fluid should continuously accumulate because Starling's equation favors fluid formation through the parietal pleura and no gradient exists for fluid absorption through the visceral pleura. Fluid clearance via the pleural lymphatics is thought to explain the lack of fluid accumulation in the normal individual. Stewart (1963) demonstrated that proteins, cells, and all other particulate matter are removed from the pleural space by lymphatics in the parietal pleura. Wang (1975) demonstrated that, at least in rabbits, the pleural space is in communication with the lymphatic vessels by means of stomas located within the parietal pleura. No such stomas are present in the visceral pleura. Although these stomas have been more difficult to demonstrate in humans, Li (1993) has demonstrated the presence of stomas in the diaphragmatic parietal pleura but not in the thoracic parietal pleura or the visceral pleura. Li (1993) reported that the mean diameter of the stomas was 6.2 m and that there were great numbers of microvilli on the mesothelial cells surrounding their openings.
Broaddus and co-workers (1988) produced artificial hydrothoraces in awake sheep by injecting an autologous protein solution at a volume of 10 mL/kg with a protein level of 1.0 g/dL. They found that the hydrothorax was removed almost completely by the lymphatics in a linear fashion at a rate of 0.28 mL/kg per hour. This linearity suggests that the lymphatics operate at maximum capacity once the pleural liquid exceeds a certain threshold volume. Note that the capacity
P.808
for lymphatic clearance is 28 times the normal rate of pleural fluid formation.
In the aforementioned experiments of Broaddus and colleagues (1988), the fluid that was introduced into the pleural space had an oncotic pressure of approximately 5 cm H2O. From Fig. 57-1 one might speculate that if fluids with oncotic pressures other than 5 cm H2O were introduced, the equilibrium would have been altered such that fluid would enter the pleural space from visceral pleura in animals with high pleural fluid oncotic pressures and would leave the pleural space through the visceral pleura in animals with low pleural fluid oncotic pressures. This does not appear to be the case. Aiba and co-workers (1984) produced artificial pleural effusions in dogs with protein levels ranging from 0.1 to 9.0 g/dL. Even when the induced pleural effusion had an oncotic pressure of 0.1 g/dL, no increase in the concentration of protein occurred with time, indicating that the low oncotic pressure did not induce a rapid efflux of fluid out of the pleural space. When the protein concentration of the induced effusions was greater than 4 g/dL, the concentration of protein in the pleural fluid did decrease with time, indicating a net transfer of protein-free fluid into the pleural space. However, the net amount of fluid entering the pleural space, even with a protein level of 9.0 g/dL, was only 0.22 mL/kg per hour. This degree of fluid flux is similar to the lymphatic clearance of 0.22 mL/kg per hour reported in the same studies. These observations explain why protein levels and hematocrits remain relatively stable in individuals with hemothoraces.
The amount of fluid that can be cleared through these lymphatics is substantial. Stewart (1963) found that the mean lymphatic flow from one pleural space in seven patients was 0.40 mL/kg per hour, whereas Leckie and Tothill (1965) found that the mean lymphatic flow was 0.22 mL/kg per hour in seven patients with congestive heart failure. In both these studies, marked variability was noted from one patient to another. If these results from patients with congestive heart failure can be extrapolated to the normal person, a 60-kg individual should have the capacity to absorb approximately 20 mL/h or 500 mL/day from each pleural space through the lymphatics.
In summary, if the experimental results in sheep can be extrapolated to humans, it appears that a small amount (0.01 mL/kg per hour) of fluid constantly enters the pleural space from the capillaries in the parietal pleura. Almost all of this fluid is removed by the lymphatics in the parietal pleura, which can remove approximately 0.20 mL/kg per hour. Little net fluid movement occurs across the visceral pleura. A pleural effusion develops when the amount of fluid that enters the pleural space exceeds the amount that can be removed via the lymphatics. Accordingly, pleural effusions can develop and are caused by increased pleural fluid formation, decreased lymphatic clearance from the pleural space, or a combination of these two factors. The three primary origins of pleural fluid are the pulmonary interstitial spaces, pleural capillaries, and peritoneal cavity.
DIFFERENTIAL DIAGNOSIS
Pleural effusions can occur as complications of many different diseases and therapeutic procedures (Table 57-1). The initial step in evaluation of the patient is the differentiation between exudative and transudative effusions.
Separation of Exudates from Transudates
When it is found that a patient has a pleural effusion that measures more than 10 mm on decubitus radiography, a diagnostic thoracentesis should usually be performed. The author (2002) recommends that if the patient has obvious congestive heart failure, the thoracentesis should be postponed until the heart failure is treated. However, if such a patient is febrile or has pleuritic chest pain or if the effusions are not of comparable size on both sides, a thoracentesis should be performed without delay. Shinto and I (1990) have shown that the characteristics of pleural fluid associated with heart failure change little with diuresis over several days.
The first question to be answered with a diagnostic thoracentesis is whether the patient has a transudative or an exudative pleural effusion. Broaddus and I (1992) have modified the classic definitions of the transudates and exudates to take into account the newer theories concerning the formation and resorption of pleural fluid. By this new definition, transudative effusions arise from increased hydrostatic pressures or decreased oncotic pressure, whereas exudative effusions result from increased permeability. This differentiation can be made by simultaneous analysis of the protein and lactic acid dehydrogenase (LDH) levels in the pleural fluid and in the serum. Exudative pleural effusions meet at least one of the following criteria, whereas transudative pleural effusions meet none, according to the classic definitions of the author and colleagues (1972): (a) pleural fluid protein to serum protein greater than 0.5, (b) pleural fluid LDH to serum LDH greater than 0.6, and (c) pleural fluid LDH greater than two-thirds the upper limit of normal for serum. If none of these criteria is met, the patient has a transudative pleural effusion and the pleural surfaces and the lung can be ignored while the congestive heart failure, cirrhosis, or nephrosis is treated. However, a transudative pleural effusion can result from pulmonary embolization.
The previously mentioned criteria misidentify a transudative effusion as an exudative effusion in approximately 20% of cases. If a patient appears to have a transudative effusion clinically, but the pleural fluid meets exudative criteria, the difference between the serum and pleural fluid albumin levels should be assessed. Burgess and co-workers (1995) have shown that if this difference exceeds 1.2 g/dL, the patient in all probability has a transudative effusion. Eid and associates (2002), however, have recently demonstrated that patients with congestive heart failure who have an exudative effusion usually have a noncardiac cause for the pleural effusion.
Table 57-1. Differential Diagnoses of Pleural Effusions | |
|---|---|
|
P.809
Differentiating Exudative Pleural Effusions
Once it has been determined that a patient has an exudative pleural effusion, one should attempt to determine which of the diseases listed in Table 57-1 is responsible, remembering that pneumonia, malignancy, and pulmonary embolization account for the great majority of all exudative pleural effusions. The author (2002) recommends that the following tests be obtained on the pleural fluid from a patient with an undiagnosed exudative pleural effusion: glucose level, LDH level, cell count and differential, microbiological studies, and cytology. In selected patients, other tests on the pleural fluid, such as the pH, amylase, adenosine deaminase (ADA) level, interferon- level, polymerase chain reaction (PCR) for tuberculous DNA, and lipid analysis, may be of value.
Appearance of Pleural Fluid
The gross appearance of the pleural fluid should always be described and its odor noted. If the pleural fluid smells putrid, the patient has a bacterial infection, probably anaerobic, of the pleural space. If the pleural fluid smells like urine, the patient probably has a urinothorax caused by obstruction of the ureters. If the pleural fluid is bloody, a pleural fluid hematocrit should be obtained. If the pleural fluid hematocrit is greater than 50% that of the peripheral blood, the patient has a hemothorax, and one should consider inserting a chest tube. If the pleural fluid is turbid, milky, or bloody, the supernatant should be examined after centrifugation. If the supernatant is clear, then the turbidity was caused by cells or debris in the pleural fluid. If the turbidity persists, then the patient probably has a chylothorax or a pseudochylothorax.
Pleural Fluid White Blood Cell Count and Differential
When pleural fluid is sent for cell count and differential, Conner and co-workers (2003) have shown that the tube with the pleural fluid must contain an anticoagulant; otherwise the cells are likely to clump, which leads to inaccurate cell counts. The absolute pleural fluid white blood cell count is of limited usefulness. Counts greater than 10,000 cells per microliter are most commonly observed with parapneumonic effusions but also are seen with pancreatitis, pulmonary embolism, collagen vascular disease, malignancy, and tuberculosis. The differential cell count on the pleural fluid is of more usefulness than is the absolute cell count. If the pleural fluid contains predominantly polymorphonuclear leukocytes, then it is caused by an acute disease process such as pneumonia, pulmonary embolization, pancreatitis, intraabdominal abscess, or early tuberculosis. If the pleural fluid contains predominantly mononuclear cells, then malignancy, tuberculosis, or a resolving acute process is probably responsible for the effusion. The majority of patients with pleural fluid eosinophilia
P.810
have either blood or air in their pleural space. If neither air nor blood is present in the pleural space, several unusual diagnoses should be considered. Benign asbestos pleural effusions are frequently eosinophilic. Patients with pleural effusions secondary to drug reactions (e.g., nitrofurantoin, bromocriptine, or dantrolene) typically have pleural fluid eosinophilia. The pleural fluid of patients with pleural paragonimiasis is typically eosinophilic with a low glucose, low pH, and a high LDH level. No diagnosis is ever determined for approximately 20% of exudative pleural effusions, and pleural fluid eosinophilia is found in approximately 40% of these effusions. Kalomenidis and the author (2003) have shown that the reported prevalence of eosinophilic pleural effusions among malignant pleural effusion has varied between 2.3% and 11.6%, while less than 2% of tuberculous pleural effusions are eosinophilic. The demonstration that more than 50% of the white blood cells in an exudative pleural effusion are small lymphocytes indicates that the patient probably has malignancy, tuberculosis, or a post-coronary artery bypass surgery pleural effusion.
Pleural Fluid Glucose
The presence of a reduced pleural fluid glucose level (<60 mg/dL) narrows the diagnostic possibilities to seven: parapneumonic effusion-empyema, malignant effusion, tuberculous effusion, rheumatoid effusion, hemothorax, paragonimiasis, or Churg-Strauss syndrome. If a patient with a parapneumonic effusion has a pleural fluid glucose level less than 40 mg/dL, tube thoracostomy should be performed. Most patients with rheumatoid pleural effusions have a pleural fluid glucose level below 30 mg/dL.
Pleural Fluid Amylase
An elevated (i.e., above the upper limit of normal for serum) pleural fluid amylase indicates that the patient has esophageal perforation, pancreatic disease, or malignant disease. The best screening test for a ruptured esophagus is probably the pleural fluid amylase. The origin of the amylase in this instance is the salivary glands. It is important to establish this diagnosis expeditiously, because the mortality rate exceeds 50% if the mediastinum is not explored within 24 hours of the perforation. Approximately 10% of patients with acute pancreatitis have an accompanying pleural effusion. Occasionally chest symptoms dominate the clinical picture and an elevated pleural fluid amylase is the first clue that the primary problem is pancreatic rather than pulmonary. Patients with chronic pancreatic disease may develop a sinus tract between the pancreas and the pleural space, which leads to a chronic illness dominated by a large pleural effusion. Unless the pleural fluid amylase level is measured, one may wrongly ascribe the chronic illness and the large pleural effusion to malignancy. The pleural fluid amylase level is elevated in approximately 10% of malignant pleural effusions. Analysis of the amylase isoenzymes permits differentiation of pancreatic disease from malignant disease. Kramer and associates (1989) have shown that the amylase associated with malignancy is of the salivary subtype.
Pleural Fluid Lactic Acid Dehydrogenase
The pleural fluid LDH level should be measured every time a diagnostic thoracentesis is performed because the level of LDH in the pleural fluid is a good indicator of the degree of inflammation in the pleural space. If the pleural fluid LDH level increases with serial thoracentesis, the degree of inflammation is worsening, and one should be more aggressive in pursuing a diagnosis. Alternatively, a decreasing pleural fluid LDH level indicates that the pleural inflammation is improving.
Pleural Fluid Cytology
Pleural fluid cytology is quite useful in establishing the diagnosis of malignant pleural effusion because the diagnosis can be established in 40% to 90% of patients, depending on the tumor type, the amount of fluid submitted, and the skill of the cytologist. Prakash and Reiman (1985) have shown that the cytology result is usually positive if the primary tumor is an adenocarcinoma, whereas it is usually not positive if the primary tumor is a squamous cell carcinoma, lymphoma, or mesothelioma. Lee and co-workers (1996), among others, have shown that the use of immunohistochemical tests using monoclonal antibodies facilitates the differentiation of adenocarcinoma cells, benign mesothelial cells, and malignant mesothelial cells.
Culture and Bacteriologic Stains
Pleural fluid from patients with undiagnosed exudative pleural effusions should be cultured for bacteria, both aerobically and anaerobically, mycobacteria, and fungi. A Gram's stain of the fluid also should be obtained.
Pleural Fluid pH and Pco2
The pleural fluid pH is most useful in determining whether chest tubes should be inserted in patients with parapneumonic effusions. If the pleural fluid pH is less than 7.00, the patient invariably has a complicated parapneumonic effusion, and tube thoracostomy should be instituted. If the pleural fluid pH is greater than 7.20, the patient probably does not require tube thoracostomy. The pleural fluid pH can be reduced to less than 7.20 with eight other conditions: systemic acidosis, esophageal rupture, rheumatoid pleuritis, tuberculous pleuritis, malignant pleural disease, hemothorax, paragonimiasis, or Churg-Strauss syndrome. When the pleural fluid pH is used as a diagnostic test, it must be measured with the same care as arterial pH. The
P.811
fluid should be collected anaerobically in a heparinized syringe and placed in ice for transfer to the laboratory to avoid spontaneous acid generation by the fluid. The pleural fluid pH must be measured with a blood gas machine. Cheng and co-workers (1998) have shown that pleural fluid pH measured with either a pH meter or pH indicator strips is not sufficiently accurate for clinical decision making.
Pleural Fluid Tests for the Diagnosis of Tuberculous Pleuritis
Three tests namely, the pleural fluid ADA level, the pleural fluid interferon- level, and the PCR for tuberculous DNA have been shown to be useful in the diagnosis of tuberculous pleuritis. In a study reported from Spain by Valdes and co-workers (1998), 253 of 254 patients (99.6%) with tuberculous pleuritis had a pleural fluid ADA level above 47 U/L. Burgess and associates (1996) have shown that the specificity of the pleural fluid ADA level for tuberculosis can be increased if it is combined with a pleural fluid lymphocyte to neutrophil ratio of greater than 0.75. In their series, the specificity of the pleural fluid ADA level increased from 81% to 95% if the diagnosis of tuberculosis was based on an ADA level above 50 U/L and a lymphocyte neutrophil ratio of 0.75 or higher. Lee and associates (2001) have demonstrated that lymphocytic pleural effusions not due to tuberculosis rarely have ADA levels above 40 U/L. Patients with tuberculous pleuritis tend to have a high pleural fluid interferon- level. In a study of 345 patients with exudative pleural effusions, Villena and co-workers (1996) reported that the sensitivity of a pleural fluid interferon- with a cutoff level of 3.7 U/mL was 0.99 whereas the specificity was 0.98. The PCR for tuberculous DNA on pleural fluid also appears to be useful in the diagnosis of tuberculous pleuritis. Querol and associates (1995) reported that the sensitivity and specificity of PCR and ADA were comparable for the diagnosis of tuberculous pleuritis. It is likely that the results with PCR will improve as its technology is refined.
Other Diagnostic Tests on Pleural Fluid
If the supernatant of the pleural fluid is cloudy, levels of cholesterol and triglycerides in the pleural fluid should be obtained to differentiate chylothorax from pseudochylothorax. With chylothorax, the pleural fluid triglyceride levels are usually elevated above 110 mg/dL. With pseudochylothorax, the pleural fluid cholesterol level is elevated.
Numerous reports have advocated the use of tumor markers in the pleural fluid for diagnosing malignant pleural effusion. However, the use of tumor markers for the diagnosis of pleural malignancy is not recommended because no tumor marker has yet been found that is 100% specific and one does not want to falsely establish the diagnosis of malignant pleural effusions.
Various reports have advocated measuring other enzymes and proteins in the pleural fluid, including antinuclear antibody levels, rheumatoid factor, lysozyme, and alkaline and acid phosphatase. However, none has proven to be useful in the differential diagnosis or management of patients with pleural effusions.
Invasive Tests for Undiagnosed Exudative Pleural Effusions
In the majority of patients, the cause of the pleural effusion is apparent after the initial clinical assessment and a diagnostic thoracentesis. If the diagnosis is not apparent, the following invasive tests might be considered: needle biopsy of the pleura, thoracoscopy, bronchoscopy, and open biopsy of the pleura. It is important to remember that no diagnosis is established for approximately 20% of exudative pleural effusions, and these resolve spontaneously, leaving no residual. Three factors should influence the vigor with which one pursues the diagnosis in patients with undiagnosed exudative effusions.
The symptoms and clinical course of the patient. If the symptoms are minimal or if they are improving, a less aggressive approach is indicated.
The trend of the pleural fluid LDH level. If the pleural fluid LDH tends to increase with serial thoracenteses, a more aggressive approach is indicated because the process is getting worse.
The attitude of the patient. If the patient is desperate to know why he or she has developed a pleural effusion, an aggressive approach should be taken.
Needle Biopsy of the Pleura
With special needles, small specimens of the parietal pleura can be obtained relatively noninvasively. Since the 1930s, the diagnosis of tuberculous pleuritis has been established primarily via needle biopsy of the pleura. However, as outlined previously under the section on Differential Diagnosis, noninvasive tests for establishing the diagnosis of tuberculous pleuritis have been developed, and hence needle biopsy of the pleura is usually not necessary to establish this diagnosis. The other main diagnosis that is established with needle biopsy of the pleura is malignant pleural disease. Prakash and Reiman (1985) have demonstrated that needle biopsy results of the pleura are usually negative in patients who have negative cytology results. If the diagnosis of malignancy is strongly suspected and the cytology result on the fluid is negative, it is preferable to proceed to thoracoscopy rather than needle biopsy of the pleura.
Thoracoscopy
With this procedure, discussed in more detail in Chapter 18, the pleural surfaces can be directly visualized through a scope introduced through a small incision in the chest wall.
P.812
The instrumentation for video-assisted thoracic surgery (VATS) has improved dramatically, and video-thoracoscopy has become the primary means of diagnosing pleural malignancy in patients who have negative cytology results.
Thoracoscopy is excellent at establishing the diagnosis of malignancy. As shown by Loddenkemper (1998), thoracoscopy establishes the diagnosis of malignant pleural disease in 95% of patients with pleural malignancy. When one does a diagnostic thoracoscopy, one should be prepared to perform a procedure to create a pleurodesis, such as pleural abrasion, to prevent recurrence of the pleural effusion. Although the diagnosis of tuberculous pleuritis also can be made with thoracoscopy, other benign etiologies for pleural effusions are rarely established with thoracoscopy. If a thoracoscopy is nondiagnostic, one can say with reasonable certainty, however, that the patient has neither pleural malignancy nor pleural tuberculosis.
Bronchoscopy
Bronchoscopy is sometimes useful in the evaluation of patients with an undiagnosed exudative pleural effusion. Not all patients with an undiagnosed pleural effusion should undergo bronchoscopy. Chang and Perng (1989) demonstrated that bronchoscopy was useful only if the patient had a parenchymal abnormality or hemoptysis. Patients with an undiagnosed pleural effusion should undergo computed tomography (CT) of the chest. Bronchoscopy is performed only if the CT scan demonstrates parenchymal abnormalities or if the patient has hemoptysis. At the time of bronchoscopy, special attention is directed to those portions of the lung in which the parenchymal abnormalities were demonstrated.
Bronchoscopy is probably not indicated for the patient with a pleural effusion and no parenchymal abnormality, no hemoptysis, and less than a massive effusion. Poe and associates (1994) reported that bronchoscopy was diagnostic in only 1 of 48 (2%) such patients. Similarly, bronchoscopy is rarely diagnostic in the patient with a cytologically positive pleural effusion and no parenchymal abnormality. Feinsilver and co-workers (1986) reported that bronchoscopy was diagnostic in 2 of 17 (12%) such patients.
Open Biopsy of the Pleura
Thoracotomy with direct biopsy of the pleura provides the best biopsy specimens. However, it has been replaced by video-thoracoscopy in centers in which this procedure is available. It should be emphasized that open pleural biopsy does not always provide a diagnosis in patients with pleural effusions. Ryan and co-workers (1981) reported that between 1962 and 1972, 51 patients with pleural effusion at the Mayo Clinic had no diagnosis after an open pleural biopsy. In 31 of these patients, there was no recurrence of the pleural effusion and no cause ever became apparent. However, 13 of the patients were eventually proven to have malignant disease.
BENIGN CONDITIONS CAUSING PLEURAL EFFUSION
The remainder of this chapter deals with specific conditions that cause pleural effusion. The reader is referred to the following chapters for a discussion of other diseases of the pleura: Chapter 58 for parapneumonic effusion, Chapter 60 for tuberculous and fungal pleural infections, Chapter 63 for chylothorax, Chapter 65 for mesothelioma, and Chapter 68 for malignant pleural effusions.
Transudative Pleural Effusions
Transudative pleural effusions occur because of increased hydrostatic or decreased oncotic pressures.
Congestive Heart Failure
Congestive heart failure is responsible for more pleural effusions than any other disease process. The pleural effusions that occur with congestive heart failure tend to be bilateral and of approximately the same size on each side. Almost all patients with pleural effusions secondary to congestive heart failure have left ventricular or biventricular failure. Patients with congestive heart failure and pleural effusion should undergo diagnostic thoracentesis if the effusions are not bilateral and comparable in size, if the patients are febrile, or if they have pleuritic chest pain to verify that the fluid is transudative. Otherwise, the effusion can be observed while the heart failure is treated, and it usually resolves.
Rarely, a patient with congestive heart failure has a persistent pleural effusion despite intensive therapy. If such patients are dyspneic and if their dyspnea is relieved by a therapeutic thoracentesis, consideration can be given to attempting a pleurodesis with a sclerosing agent such as a doxycycline.
Hepatic Hydrothorax
Pleural effusions occur in approximately 5% of patients with cirrhosis and ascites. The predominant mechanism responsible for the pleural effusion is the direct movement of peritoneal fluid through small holes in the diaphragm into the pleural space. The effusions are usually right-sided and frequently are large enough to produce severe dyspnea. If medical management of the cirrhosis and ascites does not control the pleural effusion, several options exist.
The ideal treatment is to reverse the liver disease. This is best done with a liver transplant, but not all patients with a hepatic hydrothorax are candidates for transplantation. The next best treatment is probably implantation of a transjugular intrahepatic portal systemic shunt. Gordon and associates (1997) performed this procedure in 24 patients and reported that 14 patients had complete relief of their symptoms
P.813
after shunt placement and did not require further thoracentesis. Five additional patients required fewer thoracenteses, but the remaining five patients developed worsening liver function and died within 45 days.
If liver transplantation or transjugular intrahepatic portal systemic shunt is not feasible, then the best treatment is probably video-thoracoscopy with closure of the diaphragmatic defects and talc insufflation. Milanez de Campos and co-workers (2000) performed this procedure on 18 patients. They found diaphragmatic defects that could be closed in 5 of the 18 patients. The procedure was effective in 10 of the 18 patients (56%). Patients with hepatothorax are seriously ill as reflected by the morality rate of 30% in the 3 months following surgery as reported by Milanez de Campos and associates (2000). Pleurodesis also can be attempted with an agent such as doxycycline after tube thoracostomy, but Runyon and co-workers (1986) believe that this procedure is contraindicated in patients with hepatothorax because of the danger of hypovolemia and even death.
An alternative treatment is the insertion of a peritoneojugular shunt. As demonstrated by Park and co-workers (1997), these shunts can sometimes control the effusion. However, they frequently do not because fluid preferentially moves to the pleural space, where the hydrostatic pressure is less than it is in the central veins.
One possibility that must be kept in mind when managing a patient with a hepatic hydrothorax is a spontaneous bacterial empyema. Spontaneous bacterial empyema is the infection of a preexisting hepatic hydrothorax in which a parapneumonic infection has been excluded. In a prospective study at a university-based referral hospital, Xiol and associates (1996) reported that 16 of 120 patients (13%) admitted with a diagnosis of hepatic hydrothorax had a spontaneous bacterial empyema. The criteria for the diagnosis of a spontaneous empyema are a positive pleural fluid culture result and a pleural fluid neutrophil count greater than 250 cells/mL with the exclusion of a pneumonic process. Culture-negative spontaneous bacterial empyema is diagnosed in patients with a negative pleural fluid culture result, but with a compatible clinical course and a neutrophil count greater than 500 cells per milliliter. Xiol and co-workers reported that 10 of 24 episodes (43%) were not associated with bacterial peritonitis. Treatment of spontaneous empyema does not require tube thoracostomy.
Nephrotic Syndrome
Pleural effusions occur in approximately 20% of patients with the nephrotic syndrome. The effusions are thought to be caused by the decreased plasma oncotic pressure in conjunction with increased hydrostatic pressure due to salt retention. The possibility of pulmonary emboli should always be considered in patients with this syndrome, and a spiral lung scan, pulmonary arteriography, or both should be obtained to exclude this diagnosis. Optimally, treatment of the nephrotic syndrome results in an increased level of protein in the serum and resolution of the pleural effusion.
Peritoneal Dialysis
Large pleural effusions occasionally complicate peritoneal dialysis. Nomoto and co-workers (1989) reported that 1.6% of 3,196 patients receiving continuous ambulatory peritoneal dialysis developed a pleural effusion. The mechanism appears to be a diaphragmatic defect that is similar to the mechanism for the hydrothorax seen with cirrhosis and ascites. Frequently, one wants to continue the dialysis in these patients. Such cases can be managed by chemical pleurodesis induced by a tetracycline derivative combined with a short period of small-volume intermittent peritoneal dialysis as recommended by Chow and associates (1988), or by thoracoscopy with closure of the pleuroperitoneal communication coupled with a procedure to produce a pleurodesis as described by Di Bisceglie and colleagues (1996).
Exudative Pleural Effusions
Pleural Effusions that Are Caused by Pulmonary Embolization
The diagnosis most commonly overlooked in the differential diagnosis of a patient with an undiagnosed pleural effusion is pulmonary embolization. The symptoms of patients with pleural effusions accompanying pulmonary embolization are no different from those in patients with emboli but without pleural effusion. Dyspnea is reported by more than 80% of the patients and is usually greater than one would expect from a similar-sized effusion with a different etiology.
The pleural effusion associated with pulmonary embolization usually occupies less than one third of the hemithorax. Coche and associates (1998) reported that 13 of 26 patients (50%) with pulmonary emboli had pleural effusions, which were bilateral in 6 (46%). Romero Candeira and associates (2002) analyzed the pleural fluid findings in 60 patients with pulmonary embolism and reported that all were exudates and that the fluid could contain predominantly neutrophils or lymphocytes. The pleural fluid red blood cell count exceeded 10,000 per microliter in 67%, and 18% contained more than 10% eosinophils.
Any patient with an undiagnosed pleural effusion should undergo perfusion lung scanning or contrast-enhanced spiral CT. In addition to demonstrating the presence or absence of a pulmonary embolus, spiral CT can also demonstrate parenchymal or mediastinal abnormalities. The treatment of the patient with a pleural effusion secondary to pulmonary embolism is the same as for any patient with pulmonary emboli. If the pleural effusion increases in size with treatment, the patient probably has recurrent emboli or
P.814
another complication such as a hemothorax or a pleural infection.
Pleural Effusions Secondary to Diseases of the Gastrointestinal Tract
Esophageal Perforation
The possibility of esophageal rupture should be considered in acutely ill patients with pleural effusion, because the mortality rate from this condition approaches 100% if it is not appropriately diagnosed and treated within 48 hours. Esophageal rupture can occur spontaneously in patients who have vomited or iatrogenically after endoscopy or insertion of a Blakemore tube. Patients with esophageal rupture are acutely ill with chest pain and dyspnea caused by the mediastinal and pleural infection. The best screening test for esophageal rupture is the measurement of the level of amylase in the pleural fluid. With esophageal rupture, the pleural fluid amylase level is elevated because of the high amylase level in the saliva that enters the pleural space. The diagnosis is confirmed with the demonstration of esophageal disruption via contrast studies. The treatment of esophageal rupture is discussed in Chapter 138.
Acute Pancreatitis
A high prevalence of pleural effusions occurs in patients with acute pancreatitis. In a study of 133 patients with acute pancreatitis who underwent contrast-enhanced CT scans, Lankisch and co-workers (1994) found that the prevalence of pleural effusions with acute pancreatitis is approximately 50%. Fifty-one of the effusions were bilateral, 10 were unilateral left-sided, and 5 were unilateral right-sided. At times, with acute pancreatitis, respiratory symptoms consisting of pleuritic chest pain and dyspnea may dominate the clinical picture. The prevalence of pancreatic pseudocyst is much higher in patients with pleural effusion than in those without pleural effusion. If the pleural effusion does not resolve within 2 weeks of starting appropriate therapy for the pancreatitis, the possibility of a pancreatic abscess or a pancreatic pseudocyst should be considered.
Chronic Pancreatic Disease
Patients with chronic pancreatic disease on occasion develop a sinus tract from their pancreas through the diaphragm into the mediastinum and then into the pleural space. The clinical picture of patients with chronic pancreatic disease and pleural effusion is usually dominated by chest symptoms such as dyspnea, cough, and chest pain. Rockey and Cello (1990) found that most patients do not have abdominal symptoms, because the pancreaticopleural fistula decompresses the pseudocyst. The pleural effusion is usually massive and recurs rapidly after thoracentesis. The effusion is most commonly left-sided but may be right-sided or bilateral.
The diagnosis is suggested by a high pleural fluid amylase level and is confirmed by abdominal CT scan or ultrasonography. Endoscopic retrograde cholangiopancreatography usually documents the fistulous tract or other pathology in the pancreas.
Patients with chronic pancreatic pleural effusions should be given a trial of conservative therapy for 2 to 3 weeks. Rockey and Cello (1990) recommended that this therapy consist of nasogastric suction, no oral intake, suppression of pancreatic secretion with atropine, and repeated therapeutic thoracenteses. Pederzoli and associates (1986) reported that the administration of a continuous infusion of somatostatin may decrease the secretions through the fistula and facilitate closure. If conservative treatment fails, which Parekh and Segal (1992) reported is much more common when the patient has severe pancreatitis, a laparotomy should be performed. The anatomy of the pancreatic ductal system should be assessed preoperatively with endoscopic retrograde cholangiopancreatography or at the time of operation with an operative pancreatogram. If a sinus tract is found, it should be ligated or excised. The pancreas should be partially resected, drained with a Roux-en-Y loop, or both. Faling and colleagues (1984) suggested an alternate approach whereby the pancreatic pseudocyst was drained by percutaneous catheter drainage. Decortication of the pleura may be necessary for some patients.
Intraabdominal Abscess
Pleural effusions frequently accompany intraabdominal abscesses, including subphrenic (80%), pancreatic (40%), intrasplenic (35%), and intrahepatic abscesses (20%). The pleural fluid is a sterile exudate with predominantly neutrophils. The possibility of an intraabdominal abscess should be considered seriously in a patient with a persistent neutrophilic pleural effusion and no parenchymal infiltrates. The diagnosis is best established by abdominal CT scan, and treatment consists of antibiotics plus drainage.
Pleural Effusions after Surgical Procedures
After Coronary Artery Bypass Surgery
A high prevalence of small pleural effusions occurs after coronary artery bypass surgery. Vargas and associates (1994) reported that the incidence of pleural effusion after coronary artery bypass surgery approached 90%. The incidence is comparable whether saphenous vein graphs or internal mammary artery grafts are used. The pathogenesis of the effusions is unknown, but Vargas and co-workers (1994) have speculated that they are related to trauma during surgery.
The effusions are predominantly small and on the left side. The natural history of these effusions in one of gradual
P.815
resolution over weeks to months. In studies of patients undergoing coronary artery bypass graft (CABG) surgery, the author and colleagues (1999, 2002) reported that the prevalence of pleural effusion at 28 days postsurgery was 63%. The majority of the effusions (73.4%) were unilateral on the left or larger on the left. Only 7.2% of the effusions were unilateral on the right or larger on the right. The effusions were large, occupying more than 25% of the hemithorax in 37 patients (10.6%).
Sadikot and associates (2000) have divided the large effusions (those occupying >25% of the hemithorax) into early and late effusions, both of which are exudates. The primary symptom for both the early and the late post-CABG effusion is dyspnea. The presence of fever or chest pain suggests an alternate diagnosis. The early effusions reach their maximal size within 30 days of surgery and are bloody (mean hematocrit >5), have a high LDH, are usually eosinophilic, often with peripheral eosinophilia, and respond to one or two therapeutic thoracenteses. In contrast, the effusions that reach their maximal size after 30 days are not bloody or eosinophilic, have more than 50% small lymphocytes, and have a relatively low pleural fluid LDH. Most patients with these late post-CABG pleural effusions can also be managed with one to three thoracenteses. In patients who present with large pleural effusions, the differential diagnosis in addition to the post-CABG pleural effusion includes chylothorax, pleural infection, the postcardiac injury syndrome, pulmonary embolism, and congestive heart failure.
Post-Cardiac Injury Syndrome
The post-cardiac injury syndrome, also called the postpericardiectomy or post-myocardial infarction (Dressler's) syndrome, is characterized by pericarditis, pleuritis, or pneumonitis, or a combination of these, that occurs after injury to the myocardium or pericardium. Mott and associates (2001) have defined noncomplicated post-cardiac injury syndrome as the presence of a temperature of greater than 100.5 F, patient irritability, pericardial friction rub, and a small pericardial effusion with or without pleural effusion. A complicated post-cardiac injury syndrome has the same criteria as a noncomplicated post-cardiac injury syndrome plus the need for hospital readmission with or without the need for pericardiocentesis or thoracentesis. The author (2001) has demonstrated that the two cardinal symptoms of this syndrome are chest pain and fever. The syndrome typically develops approximately 3 weeks after the injury but can occur anytime between 3 days and 1 year. The pleural fluid is an exudate that is frequently serosanguineous or bloody. Mott and co-workers (2001) reported that the incidence of the noncomplicated syndrome after cardiac surgery in children was 11.2%, whereas the incidence of the complicated syndrome was 3.4%. The treatment of choice is the use of antiinflammatory agents such as aspirin or indomethacin. Patients with this syndrome after coronary artery bypass procedures should be treated with corticosteroids because the pericarditis may cause graft occlusion.
After Fontan Procedure
With this procedure, the right ventricle is bypassed by an anastomosis between the superior vena cava, the right atrium, or the inferior vena cava and the pulmonary artery. This surgery is usually performed for tricuspid atresia or univentricular heart. As reported by Laks and co-workers (1984), a transudative pleural effusion occurs postoperatively in nearly every patient and is a significant problem postoperatively in many patients. Spicer and associates (1996) have demonstrated that effusions are more likely to occur in patients who have significant aortopulmonary collateral vessels preoperatively. They recommend embolization of these vessels at preoperative angiography. The treatment of choice for this condition is probably the insertion of a pleuroperitoneal shunt, as suggested by Sade and Wiles (1990). An alternative treatment is creation of a late fenestration as suggested by Rychik and co-workers (1997).
After Abdominal Surgery
The author and George (1976) reported that the incidence of pleural effusion in the 2 to 3 days after abdominal surgery is approximately 50%. The incidence of postoperative pleural effusion is greater in patients undergoing upper abdominal surgery, in patients with postoperative atelectasis, and in those patients with free abdominal fluid at surgery. The pleural effusion in the postoperative period is probably caused either by diaphragmatic irritation or the transdiaphragmatic movement of intraabdominal fluid. If a patient develops a significant amount of fluid postoperatively, a diagnostic thoracentesis should be performed to rule out pleural infection as a cause of the effusion. The possibility of pulmonary embolization also should be considered. If the effusion develops more than 72 hours postoperatively, it is probably not related to the surgical procedure itself, and alternate explanations must be found such as pulmonary embolus, intraabdominal abscess, or hypervolemia.
After Endoscopic Variceal Sclerotherapy
Endoscopic variceal sclerotherapy is one of the principal forms of therapy for patients who have bled from ruptured esophageal varices, although it is being replaced by endoscopic variceal ligation in many centers. Edling and Bacon (1991) have reported that small pleural effusions complicate this procedure approximately 50% of the time. The pleural effusion is thought to result from the extravasation of the sclerosant into the esophageal mucosa, which results in an intense inflammatory reaction in the mediastinum and
P.816
pleura. The effusions can be right-sided, left-sided, or bilateral, and the fluid is exudative. If the effusion persists for more than 24 to 48 hours and is accompanied by fever or if the effusion occupies more than 25% of the hemithorax, a thoracentesis should be done to rule out an infection or an esophagopleural fistula. The latter diagnosis is suggested by a high pleural fluid amylase level.
After Liver Transplantation
Almost all patients who undergo orthotopic liver transplantation develop a pleural effusion postoperatively. Spizarny and associates (1993) prospectively evaluated 42 liver transplant recipients and reported that 40 of 42 patients (95%) developed a right-sided pleural effusion within 72 hours of transplantation. The effusions are bilateral in about one third of patients, but are almost always larger on the right. The effusions may be large. Bilik and co-workers (1992) reported that 23 of 48 children (48%) receiving transplants developed effusions large enough to cause respiratory compromise and that tube thoracostomy was necessary in 15 patients (31%). The pathogenesis of the pleural effusion after liver transplantation is not definitely known, but it has been suggested that the effusion is caused by injury or irritation of the right hemidiaphragm caused by the extensive right upper quadrant dissection and retraction. Uetsuji and associates (1994) have shown that the pleural effusions can be largely prevented if a fibrin sealant is sprayed on the undersurface of the diaphragm around the insertion of the liver ligaments. The natural history of these effusions is that they increase in size over the first 3 postoperative days and then gradually resolve over a period ranging from several weeks to several months. If the effusion increases in size after the first 3 days, subdiaphragmatic pathology such as a hematoma, abscess, or biloma should be suspected.
After Lung Transplantation
With lung transplantation, the lymphatics that normally drain the lung are severed. Accordingly, fluid that normally leaves the lung via these lymphatics exits via the pleural space. Nevertheless, pleural effusions are usually not evident in the few days after lung transplantation because chest tubes are in place. Judson and associates (1996) reported that the mean daily pleural fluid drainage via chest tube decreased from 400 mL on the first postoperative day to 200 mL on the fourth postoperative day. The pleural fluid drainage reached almost 1,000 mL in a patient who developed the postreimplantation response.
As might be expected, patients who develop pleural complications after lung transplantation are likely to develop pleural effusions. Judson and Sahn (1996) reported that pleural effusions occurred with 14 of 19 (74%) episodes of acute rejection, 7 of 8 (88%) instances of chronic rejection, 6 of 11 (55%) episodes of infection, and 3 of 4 (75%) instances of lymphoproliferative disease.
Pleural Effusions Caused by Miscellaneous Diseases
Acquired Immunodeficiency Syndrome
Pleural effusions are relatively uncommon in patients with acquired immunodeficiency syndrome (AIDS). Afessa (2000) reviewed 1,225 consecutive hospital admissions of patients with AIDS in Jacksonville, Florida, and reported that the incidence of pleural effusion was 14.6%. In the series of Afessa (2000), the five leading causes of pleural effusions were pneumonia and empyema (33%), renal failure (9%), hypoalbuminemia (8%), tuberculosis (6%) and pancreatitis (4%). Other common causes of pleural effusions in patients with AIDS include Kaposi's sarcoma, tuberculosis, cryptococcosis, lymphoma, and, rarely, Pneumocystis carinii infection.
Rheumatoid Pleuritis
Approximately 5% of patients with rheumatoid arthritis have a pleural effusion sometime during their life. Most effusions occur in older men with subcutaneous nodules. The pleural fluid with rheumatoid pleuritis is distinctive, characterized by a glucose level less than 30 mg/dL, a high LDH level (700 IU/L), and a low pH (<7.20). The pleural effusion usually resolves spontaneously within 3 months. No controlled study has documented the efficacy of any treatment.
Lupus Erythematosus
Approximately 40% of patients with systemic lupus erythematosus or drug-induced systemic lupus erythematosus develop a pleural effusion during the course of their disease. The pleuritis may be the first manifestation of the underlying disease. Most patients with lupus pleuritis have pleuritic chest pain and are febrile. The diagnosis is made primarily via the clinical picture and serologic test results. Khare and co-workers (1994) have shown that an elevated pleural fluid antinuclear antibody titer is not diagnostic of lupus pleuritis. Patients with lupus pleuritis should be treated with prednisone, 80 mg every other day, with rapid tapering once the symptoms are controlled.
Asbestos Exposure
Pleural effusions develop in approximately 3% of individuals who have had moderate to heavy asbestos exposure. The resulting exudative pleural effusion usually develops 5 to 20 years after the initial exposure. Patients with pleural effusion are usually asymptomatic. The diagnosis of benign
P.817
asbestos effusion is one of exclusion and requires the following: asbestos exposure, exclusion of other causes (e.g., infection, pulmonary embolism, malignancy), and a follow-up of at least 2 years to verify that it is benign.
Drug Reactions
Administration of nitrofurantoin, dantrolene, methysergide, and bromocriptine at times is associated with a syndrome characterized by fever, dyspnea, chest pain, and peripheral blood and pleural eosinophilia, which develop weeks to months after initiation of therapy. Discontinuation of the offending medication results in resolution of the syndrome.
Uremia
Uremia may be complicated by a fibrinous pleuritis and pleural effusion. Approximately 3% of uremics have an exudative pleural effusion, and no close relationship exists between the degree of uremia and the occurrence of a pleural effusion. After dialysis is initiated, the effusion gradually disappears within 4 to 6 weeks in the majority of patients.
REFERENCES
Afessa B: Pleural effusion and pneumothorax in hospitalized patients with HIV Infection: the pulmonary complications, ICU support, and prognostic factors of hospitalized patients with HIV (PIP) study. Chest 117:1031, 2000.
Aiba M, Inatomi K, Homma H: Lymphatic system or hydro-oncotic forces. Which is more significant in drainage of pleural fluid? Jpn J Med 23:27, 1984.
Albertine KH, et al: Structure, blood supply, and lymphatic vessels of the sheep's visceral pleura. Am J Anat 165:277, 1982.
Albertine KH, Wiener-Kronish JP, Staub NC: The structure of the parietal pleura and its relationship to pleural liquid dynamics in sheep. Anat Rec 208:401, 1984.
Allen S, Gabel J, Drake R: Left atrial hypertension causes pleural effusion formation in unanesthetized sheep. Am J Physiol 257(2 part 2):H690, 1989.
Amouzadeh HR, et al: Xylazine-induced pulmonary edema in rats. Toxicol Appl Pharmacol 108:417, 1991.
Bernaudin JF, et al: Protein transfer in hyperoxic induced pleural effusion in the rat. Exp Lung Res 210:23, 1986.
Bilik R, Yellen M, Superina RA: Surgical complications in children after liver transplantation. J Pediatr Surg 27:1371, 1992.
Broaddus VC, et al: Removal of pleural liquid and protein by lymphatics in awake sheep. J Appl Physiol 64:384, 1988.
Broaddus VC, Light RW: What is the origin of pleural transudates and exudates? [Editorial]. Chest 102:658, 1992.
Broaddus VC, Wiener-Kronish JP, Staub ND: Clearance of lung edema into the pleural space of volume-loaded anesthetized sheep. J Appl Physiol 68:2623, 1990.
Burgess LJ, Maritz FJ, Taljaard JJ: Comparative analysis of the biochemical parameters used to distinguish between pleural transudates and exudates. Chest 107:1604, 1995.
Burgess LJ, et al: Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest 109:414, 1996.
Chang SC, Perng RP: The role of fiberoptic bronchoscopy in evaluating the causes of pleural effusions. Arch Intern Med 149:855, 1989.
Cheng DS, et al: Comparison of pleural fluid pH values obtained using blood gas machine, pH meter and pH indicator strip. Chest 114:1368, 1998.
Chow CC, et al: Massive hydrothorax in continuous ambulatory peritoneal dialysis: diagnosis, management and review of the literature. NZ Med J 27:475, 1988.
Coche EE, et al: Acute pulmonary embolism: ancillary findings at spiral CT. Radiology 207:753, 1998.
Conner BD, et al: Variations in pleural fluid white blood cell count and differentials with different sample containers and different methods. Chest 123:1181, 2003.
Di Bisceglie M, et al: Videothoracoscopic obliteration of pleuroperitoneal fistula in continuous peritoneal dialysis. Ann Thorac Surg 62:1509, 1996.
Edling JE, Bacon BR: Pleuropulmonary complications of endoscopic variceal sclerotherapy. Chest 99:1252, 1991.
Eid AA et al: Exudative effusions in congestive heart failure. Chest 122:1518, 2002.
Faling LJ, et al: Treatment of chronic pancreatic pleural effusion by percutaneous catheter drainage of abdominal pseudocyst. Am J Med 76:329, 1984.
Feinsilver SH, Barrows AA, Braman SS: Fiberoptic bronchoscopy and pleural effusion of unknown origin. Chest 90:514, 1986.
Gordon FD, et al: The successful treatment of symptomatic, refractory hepatic hydrothorax with transjugular intrahepatic portosystemic shunt. Hepatology 25:1366, 1997.
Judson MA, Sahn SA: The pleural space and organ transplantation. Am J Respir Crit Care Med 153:1153, 1996.
Judson MA, Handy JR, Sahn SA: Pleural effusions following lung transplantation. Time course, characteristics, and clinical implications. Chest 109:1190, 1996.
Kalomenidis I, Light RW: Eosinophilic pleural effusions. Curr Opin 9:254, 2003.
Khare V, et al: Antinuclear antibodies in pleural fluid. Chest 106:866, 1994.
Kinasewitz GT, et al: Role of pulmonary lymphatics and interstitium in visceral pleural fluid exchange. J Appl Physiol 56:355, 1984.
Kramer MR, Cepero RJ, Pitchenik AE: High amylase in neoplasm-related pleural effusion. Ann Intern Med 110:567, 1989.
Laks H, et al: Experience with the Fontan procedure. J Thorac Cardiovasc Surg 88:939, 1984.
Lankisch PG, Groge M, Becher R: Pleural effusions: a new negative prognostic parameter for acute pancreatitis. Am J Gastroenterol 89:1849, 1994.
Leckie WJH, Tothill P: Albumin turnover in pleural effusions. Clin Sci 29:339, 1965.
Lee JS, et al: Immunohistochemical panel for distinguishing between carcinoma and reactive mesothelial cells in serious effusions. Acta Cytol 40:631, 1996.
Lee YCG, et al: Adenosine deaminase levels in nontuberculous lymphocytic pleural effusions. Chest 120:356, 2001.
Li J: Ultrastructural study on the pleural stomata in human. Func Dev Morphol 3:277 280, 1993.
Light RW: Pleural Diseases. 4th Ed. Philadelphia: Lippincott Williams & Wilkins, 1995.
Light RW: Pleural effusions following cardiac injury and coronary artery bypass graft surgery. Semin Respir Crit Care Med 22:657, 2001.
Light RW: Pleural effusion. N Engl J Med 346:1971, 2002.
Light RW, George RB: Incidence and significance of pleural effusion after abdominal surgery. Chest 69:621, 1976.
Light RW, et al: Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med 77:507, 1972.
Light RW, et al: Prevalence and clinical course of pleural effusions at 30 days after coronary artery and cardiac surgery. Am J Respir Crit Care Med 166(12 part 1):1567, 2002.
Loddenkemper R: Thoracoscopy state of the art. Eur Respir J 11:213, 1998.
Milanez de Campos JR, et al: Thoracoscopy and talc poudrage in the management of hepatic hydrothorax. Chest 118:13, 2000.
Mott AR, et al: The effect of short-term prophylactic methylprednisolone on the incidence and severity of postpericardiotomy syndrome in children undergoing cardiac surgery with cardiopulmonary bypass. J Am Coll Cardiol 37:1700, 2001.
Nomoto Y, et al: Acute hydrothorax in continuous ambulatory peritoneal dialysis a collaborative study of 161 centers. Am J Nephrol 9:363, 1989.
Parekh D, Segal I: Pancreatic ascites and effusion. Risk factors for failure of conservative therapy and the role of octreotide. Arch Surg 127:707, 1992.
Park SZ, et al: Treatment of refractory, nonmalignant hydrothorax with a pleurovenous shunt. Ann Thorac Surg 63:1777, 1997.
P.818
Pederzoli P, et al: Conservative treatment of external pancreatic fistulas with parenteral nutrition alone or in combination with continuous intravenous infusion of somatostatin, glucagon or calcitonin. Surg Gynecol Obstet 163:428, 1986.
Poe RH, et al: Use of fiberoptic bronchoscopy in the diagnosis of bronchogenic carcinoma. A study in patients with idiopathic pleural effusions. Chest 105:1663, 1994.
Prakash URS, Reiman HM: Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion: analysis of 414 cases. Mayo Clin Proc 60:158, 1985.
Querol JM, et al: Rapid diagnosis of pleural tuberculosis by polymerase chain reaction. Am J Respir Crit Care Med 152:1977, 1995.
Rockey DC, Cello JP: Pancreaticopleural fistula. Report of 7 cases and review of the literature. Medicine 69:332, 1990.
Romero Candeira S, et al: Biochemical and cytologic characteristics of pleural effusions secondary to pulmonary embolism. Chest 121:465. 2002.
Runyon BA, Greenblatt M, Ming RHC: Hepatic hydrothorax is a relative contraindication to chest tube insertion. Am J Gastroenterol 81:566, 1986.
Ryan CJ, et al: The outcome of patients with pleural effusion of indeterminate cause at thoracotomy. Mayo Clin Proc 56:145, 1981.
Rychik J, Rome JJ, Jacobs ML: Late surgical fenestration for complications after the Fontan operation. Circulation 96:33, 1997.
Sade RM, Wiles HB: Pleuroperitoneal shunt for persistent pleural drainage after Fontan procedure. J Thorac Cardiovasc Surg 100:621, 1990.
Sadikot RT, et al: Pleural fluid characteristics of patients with symptomatic pleural effusion after coronary artery bypass graft surgery. Arch Intern Med 160:2665, 2000.
Shinto RA, Light RW: The effects of diuresis upon the characteristics of pleural fluid in patients with congestive heart failure. Am J Med 88:230, 1990.
Spicer RL, et al: Aortopulmonary collateral vessels and prolonged pleural effusions after modified Fontan procedures. Am Heart J 131:1164, 1996.
Spizarny DL, Gross BH, McLoud T: Enlarging pleural effusion after liver transplantation. J Thorac Imaging 8:85, 1993.
Stewart PB: The rate of formation and lymphatic removal of fluid in pleural effusions. J Clin Invest 42:258, 1963.
Uetsuji S, et al: Prevention of pleural effusion after hepatectomy using fibrin sealant. Int Surg 79:135, 1994.
Valdes L, et al: Tuberculous pleurisy: a study of 254 cases. Arch Intern Med 158:2017, 1998.
Vargas FS, et al: Relationship between pleural effusion and pericardial involvement after myocardial revascularization. Chest 105:1748, 1994.
Villena V, et al: Interferongamma in 388 immunocompromised and immunocompetent patients for diagnosing pleural tuberculosis. Eur Respir J 9: 2635, 1996.
Wang NS: The preformed stomas connecting the pleural cavity and the lymphatics in the parietal pleura. Am Rev Respir Dis 111:12, 1975.
Wiener-Kronish JP, et al: Protein egress and entry rates in pleural fluid and plasma in sheep. J Appl Physiol 56:459, 1984.
Wiener-Kronish JP, et al: Relationship of pleural effusions to pulmonary hemodynamics in patients with congestive heart failure. Am Rev Respir Dis 132:1253, 1985.
Wiener-Kronish JP, et al: Relationship of pleural effusions to increased permeability pulmonary edema in anesthetized sheep. J Clin Invest 82:1422, 1988.
Xiol X, et al. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology 23:719, 1996.
EAN: 2147483647
Pages: 203