26 - Endocrinology
Tierney, Lawrence M., McPhee, Stephen J., Papadakis, Maxine A.
Current Medical Diagnosis & Treatment, 45th Edition
document.getElementById('working').innerHTML = ''; function hide_scrollbar() { var e = document.body; e.style.scrollbarBaseColor = '#fff'; e.style.scrollbarArrowColor = '#fff'; e.style.scrollbarDarkShadowColor = '#fff'; e.style.scrollbarShadowColor = '#fff'; } function show_scrollbar() { var e = document.body; e.style.scrollbarBaseColor = '#ccc'; e.style.scrollbarArrowColor = '#000'; e.style.scrollbarDarkShadowColor = '#000'; e.style.scrollbarShadowColor = '#666'; } function toggle_CA(e) { var src; src = window.parent.getSrc(e); if (src.nextSibling.style.display == 'block') { src.nextSibling.style.display='none'; src.innerHTML='View Answer'; } else { src.nextSibling.style.display='block'; src.innerHTML='Hide Answer'; } } function resolve_link(e,setid,locator,dbid,toan) { e.href = "ovidweb.cgi?S=IDNJHKKKJGEPJK00D;FTS+Link+Set+Ref=" + setid + "|" + locator + "|" + dbid + "|" + toan; return true; }
30
General Problems in Infectious Diseases
Richard A. Jacobs MD, PhD
See http://www.cmdtlinks.com
Most infections are confined to specific organ systems, and many of the important infectious disease pathogens are discussed in chapters dealing with the relevant anatomic areas. This chapter discusses some important general problems related to infectious diseases.
FEVER OF UNKNOWN ORIGIN
To fulfill the original criteria for fever of unknown origin (FUO), a patient must have had an illness of at least 3 weeks' duration, fever over 38.3 C on several occasions, and remain without a diagnosis after 1 week of study in the hospital. The intervals specified are arbitrary ones intended to exclude patients with protracted but self-limited viral illnesses and to allow time for the usual radiographic, serologic, and cultural studies to be performed. Because of costs of hospitalization and the availability of most screening tests on an outpatient basis, the criterion requiring 1 week of hospitalization has been modified to accept patients in whom a diagnosis has not been made after three outpatient visits or 3 days of hospitalization.
Several additional categories of FUO have been added: (1) Nosocomial FUO refers to the hospitalized patient with fever of 38.3 C or higher on several occasions, due to a process not present or incubating at the time of admission, in whom initial cultures are negative and the diagnosis remains unknown after 3 days of investigation (see Nosocomial Infections, below). (2) Neutropenic FUO includes patients with fever of 38.3 C or higher on several occasions with less than 500 neutrophils per microliter in whom initial cultures are negative and the diagnosis remains uncertain after 3 days (see Chapter 2 and Infections in the Immunocompromised Patient, below). (3) HIV-associated FUO pertains to HIV-positive patients with fever of 38.3 C or higher who have been febrile for 4 weeks or more as an outpatient or 3 days as an inpatient, in whom the diagnosis remains uncertain after 3 days of investigation with at least 2 days for cultures to incubate (see Chapter 31). Although not usually considered separately, FUO in solid organ transplant recipients is a common scenario with a unique differential diagnosis and is discussed below.
For a general discussion of fever, see the section on fever and hyperthermia in Chapter 2.
Etiologic Considerations
A. COMMON CAUSES
Most cases represent unusual manifestations of common diseases and not rare or exotic diseases—eg, tuberculosis, endocarditis, gallbladder disease, and HIV (primary infection or opportunistic infection) are more common causes of FUO than Whipple's disease or familial Mediterranean fever.
B. AGE OF PATIENT
In adults, infections (25–40% of cases) and cancer (25–40% of cases) account for the majority of FUOs. In children, infections are the most common cause of FUO (30–50% of cases) and cancer a rare cause (5–10% of cases). Autoimmune disorders occur with equal frequency in adults and children (10–20% of cases), but the diseases differ. Juvenile rheumatoid arthritis is particularly common in children, whereas systemic lupus erythematosus, Wegener's granulomatosis, and polyarteritis nodosa are more common in adults. Adult Still's disease, giant cell arteritis, and polymyalgia rheumatica occur exclusively in adults. In the elderly (over 65 years of age), multisystem immune-mediated diseases such as temporal arteritis, polymyalgia rheumatica, sarcoidosis, rheumatoid arthritis, and Wegener's granulomatosis account for 25–30% of all FUOs.
C. DURATION OF FEVER
The cause of FUO changes dramatically in patients who have been febrile for 6 months or longer. Infection, cancer, and autoimmune disorders combined account for only 20% of FUOs in these patients. Instead, other entities such as granulomatous diseases (granulomatous hepatitis, Crohn's disease, ulcerative colitis) and factitious fever become important causes. One-fourth of patients who say they have been febrile for 6 months or longer actually have no true fever or underlying disease. Instead, the usual normal circadian variation in temperature (temperature 0.5–1 C higher in the afternoon than in the morning) is interpreted as abnormal. Patients with episodic or recurrent fever (ie, those who meet the criteria for FUO but have feverfree periods of 2 weeks or longer) are similar to those
P.1287
with prolonged fever. Infection, malignancy, and autoimmune disorders account for only 20–25% of such fevers, whereas various miscellaneous diseases (Crohn's disease, familial Mediterranean fever, allergic alveolitis) account for another 25%. Approximately 50% of cases remain undiagnosed but have a benign course with eventual resolution of symptoms.
D. IMMUNOLOGIC STATUS
In the neutropenic patient, fungal infections and occult bacterial infection are important causes of FUO. In the patient taking immunosuppressive medications (particularly organ transplant patients), cytomegalovirus (CMV) infections are a frequent cause of fever, as are fungal infections, nocardiosis, Pneumocystis jiroveci (formerly Pneumocystis carinii) pneumonia, and mycobacterial infections.
E. CLASSIFICATION OF CAUSES OF FUO
Most patients with FUO will fit into one of five categories.
1. Infection
Both systemic and localized infections can cause FUO. Tuberculosis and endocarditis are the most common systemic infections, but mycoses, viral diseases (particularly infection with Epstein-Barr virus and CMV), toxoplasmosis, brucellosis, Q fever, catscratch disease, salmonellosis, malaria, and many other less common infections have been implicated. Primary infection with HIV or opportunistic infections associated with the AIDS—particularly mycobacterial infections—can also present as FUO. The most common form of localized infection causing FUO is an occult abscess. Liver, spleen, kidney, brain, and bone are organs in which abscess may be difficult to find. A collection of pus may form in the peritoneal cavity or in the subdiaphragmatic, subhepatic, paracolic, or other areas. Cholangitis, osteomyelitis, urinary tract infection, dental abscess, or paranasal sinusitis may cause prolonged fever.
2. Neoplasms
Many cancers can present as FUO. The most common are lymphoma (both Hodgkin's and non-Hodgkin's) and leukemia. Other diseases of lymph nodes, such as angioimmunoblastic lymphoma and Castleman's disease, can also cause FUO. Primary and metastatic tumors of the liver are frequently associated with fever, as are renal cell carcinomas. Atrial myxoma is an often forgotten neoplasm that can result in fever. Chronic lymphocytic leukemia and multiple myeloma are rarely associated with fever, and the presence of fever in patients with these diseases should prompt a search for infection.
3. Autoimmune disorders
Still's disease, systemic lupus erythematosus, cryoglobulinemia, and polyarteritis nodosa are the most common autoimmune causes of FUO. Giant cell arteritis and polymyalgia rheumatica are seen almost exclusively in patients over 50 years of age and are nearly always associated with an elevated erythrocyte sedimentation rate (> 40 mm/h).
4. Miscellaneous causes
Many other conditions have been associated with FUO but less commonly than the foregoing types of illness. Examples include thyroiditis, sarcoidosis, Whipple's disease, familial Mediterranean fever, recurrent pulmonary emboli, alcoholic hepatitis, drug fever, and factitious fever.
5. Undiagnosed FUO
Despite extensive evaluation, the diagnosis remains elusive in 10–15% of patients. Of these patients, the fever abates spontaneously in about 75%, and the clinician never knows the cause; in the remainder, more classic manifestations of the underlying disease appear over time.
Approach to Diagnosis of FUO
Because the evaluation of a patient with FUO is costly and time-consuming, it is imperative to first document the presence of fever. This is done by observing the patient while the temperature is being taken to ascertain that fever is not factitious (self-induced). Associated findings that accompany fever include tachycardia, chills, and piloerection. A thorough history— including family, occupational, social (sexual practices, use of injection drugs), dietary (unpasteurized products, raw meat), exposures (animals, chemicals), and travel—may give clues to the diagnosis. Repeated physical examination may reveal subtle, evanescent clinical findings essential to diagnosis.
In addition to routine laboratory studies, blood cultures should always be obtained, preferably when the patient has not taken antibiotics for several days, and should be held by the laboratory for 2 weeks to detect slow-growing organisms. Cultures on special media are requested if Legionella, Bartonella, or nutritionally deficient streptococci are considered possible pathogens. “Screening tests” with immunologic or microbiologic serologies (“febrile agglutinins”) are of low yield and should not be done. Specific serologic tests are helpful if the history or physical examination suggests a specific diagnosis. A single elevated titer rarely allows one to make a diagnosis of infection; instead, one must demonstrate a fourfold rise or fall in titer to confirm a specific infectious cause. Because infection is the most common cause of FUO, other body fluids are usually cultured, ie, urine, sputum, stool, cerebrospinal fluid, and morning gastric aspirates (if one suspects tuberculosis). Direct examination of blood smears may establish a diagnosis of malaria or relapsing fever (Borrelia).
All patients with FUO should have a chest radiograph. Studies such as sinus films, upper gastrointestinal series with small bowel follow-through, barium enema, proctosigmoidoscopy, and evaluation of gallbladder function are reserved for patients who have symptoms, signs, or a history that suggest disease in these body regions. CT scan of the abdomen and pelvis is also frequently performed and is particularly useful for looking at the liver, spleen, and retroperitoneum. When the CT scan is positive, the findings often lead to a specific diagnosis. A negative CT scan
P.1288
is not quite as useful; more invasive procedures such as biopsy or exploratory laparotomy may be needed. The role of MRI in the investigation of FUO has not been evaluated. In general, however, MRI is better than CT for detecting lesions of the nervous system and is useful in diagnosing various vasculitides. Ultrasound is sensitive for detecting lesions of the kidney, pancreas, and biliary tree. Echocardiography should be used if one is considering endocarditis or atrial myxoma. Transesophageal echocardiography is more sensitive than surface echocardiography for detecting valvular lesions, but even a negative transesophageal study does not exclude endocarditis (10% false-negative rate). The usefulness of radionuclide studies in diagnosing FUO is variable. Theoretically, a gallium or positron emission tomography (PET) scan would be more helpful than an indium-labeled white blood cell scan, because gallium and fluorodeoxy-glucose may be useful for detecting infection, inflammation and neoplasm whereas the indium scan is useful only for detecting infection. Indium-labeled immunoglobulin may prove to be useful in detecting infection and neoplasm and can be used in the neutropenic patient. It is not sensitive for lesions of the liver, kidney, and heart because of high background activity. In general, radionuclide scans are plagued by high rates of falsepositive and false-negative results that are not useful when used as screening tests and, if done at all, are limited to those patients whose history or examination suggests local inflammation or infection.
Invasive procedures are often required for diagnosis. Any abnormal finding should be aggressively evaluated: Headache calls for lumbar puncture to rule out meningitis; skin from a rash should be biopsied to look for cutaneous manifestations of collagen vascular disease or infection; and enlarged lymph nodes should be aspirated or biopsied and examined for cytologic features to rule out neoplasm and sent for culture. Bone marrow aspiration with biopsy is a relatively low-yield procedure (except in HIV-positive patients, in whom mycobacterial infection is a common cause of FUO), but the risk is low and the procedure should be done if other less invasive tests have not yielded a diagnosis. Liver biopsy will yield a specific diagnosis in 10–15% of patients with FUO, and should be considered in any patient with abnormal liver function tests even if the liver is normal in size. The role of exploratory laparotomy is debatable since the advent of CT scanning and MRI. Laparotomy or laparoscopy should be considered when the patient continues to deteriorate and the diagnosis is elusive despite extensive evaluation.
Therapeutic Trials
Therapeutic trials are indicated if a diagnosis is strongly suspected—eg, it is reasonable to give antituberculous drugs if tuberculosis is suspected, or tetracycline if brucellosis is suspected. However, if there is no clinical response in several weeks, it is imperative to stop therapy and reevaluate the patient. In the seriously ill or rapidly deteriorating patient, empiric therapy is often given. Antituberculosis medications (particularly in the elderly or foreign-born) and broadspectrum antibiotics are reasonable in this setting.
Empiric administration of corticosteroids should be discouraged; they can suppress fever if given in high enough doses, but they can also exacerbate many infections, and infection remains a leading cause of FUO.
Knockaert DC et al: Fever of unknown origin in adults: 40 years on. J Intern Med 2003;253:263.
Mourad O et al: A comprehensive evidence-based approach to fever of unknown origin. Arch Intern Med 2003;163:545.
Tal S et al: Fever of unknown origin in the elderly. J Intern Med 2002;242:295.
Vanderschueren S et al: From prolonged febrile illness to fever of unknown origin. Arch Intern Med 2003;163:1033.
INFECTIONS IN THE IMMUNOCOMPROMISED PATIENT
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Clinical symptoms may be blunted because of immunosuppression.
Fever may be absent.
General Considerations
Immunocompromised patients have one or more defects in their natural defense mechanisms that put them at an increased risk for developing infections. Not only is the risk of infection greater in these individuals, but once established it is often severe, rapidly progressive, and life-threatening. In addition, microorganisms that are not usually pathogens in the immunocompetent patient may cause serious disease in the immunocompromised patient. Individuals are most commonly so impaired because of dysfunction of their immune system (granulocytopenia, T and B cell deficiency, hypogammaglobulinemia), but the presence of coexisting illness can also predispose to infection.
Granulocytopenia is common following bone marrow transplantation—as a result of myelosuppressive chemotherapy—and in acute leukemias. The risk of infection begins to increase when the absolute granulocyte count falls below 1000/mcL, with a dramatic increase in frequency and severity when the granulocyte count falls below 100/mcL. The granulocytopenic patient is particularly susceptible to infections with gram-negative enteric organisms, Pseudomonas, grampositive cocci (particularly Staphylococcus aureus, Staphylococcus epidermidis, and viridans streptococci), Candida, Aspergillus, and other fungi that have recently emerged as pathogens such as Trichosporon, Sce-
P.1289
dosporium, Fusarium, and Pseudallescheria. The methods used for detection of deficiencies in the immune system can be found in Chapter 19.
Defects in humoral immunity are often congenital, although hypogammaglobulinemia can occur in multiple myeloma and chronic lymphocytic leukemia. Patients with ineffective humoral immunity lack opsonizing antibodies and are at particular risk for infection with encapsulated organisms such as Haemophilus influenzae and Streptococcus pneumoniae.
Patients with cellular immune deficiency encompass a large and heterogeneous group, including patients with HIV infection (see Chapter 31), those with lymphoreticular malignancies such as Hodgkin's disease, and patients receiving immunosuppressive medications such as corticosteroids, cyclosporine, tacrolimus, and other cytotoxic drugs. This latter group—the immunosuppressed as a result of medications—includes transplant patients, many solid tumor patients receiving therapy, and patients receiving prolonged high-dose corticosteroid treatment (for asthma, temporal arteritis, systemic lupus, etc). Patients with cellular immune dysfunction are susceptible to infections by a large number of organisms, particularly ones that replicate intracellularly. Examples include bacteria such as Listeria, Legionella, Salmonella, and Mycobacterium; viruses such as herpes simplex, varicella, and CMV; fungi such as Cryptococcus, Coccidioides, Histoplasma, and Pneumocystis; and protozoa such as Toxoplasma.
Patients functionally or anatomically asplenic are unable to clear organisms from the bloodstream and are at an increased risk for overwhelming bacteremia with encapsulated bacteria (primarily S pneumoniae but also H influenzae and Neisseria meningitidis), S aureus, gram-negative organisms (Escherichia coli, Klebsiella pneumoniae, Salmonella sp, Capnocytophaga sp), Plasmodium, and Babesia.
Finally, a large group of patients who are not specifically immunodeficient are at increased risk for infection because of debilitating injury (eg, burns or severe trauma), invasive procedures (eg, hyperalimentation lines, Foley catheters, dialysis catheters), central nervous system dysfunction (which predisposes to aspiration pneumonia and decubitus ulcers), obstructing lesions (eg, pneumonia due to an obstructed bronchus, pyelonephritis due to nephrolithiasis, cholangitis secondary to cholelithiasis), and use of broad-spectrum antibiotics.
Despite these generalizations, any pathogen can cause infection in any immunosuppressed patient at any time. Thus, a systematic evaluation to identify a specific organism is required.
Organisms not usually pathogens in the immunocompetent person may cause serious life-threatening infection in the compromised patient (eg, S epidermidis, Corynebacterium jeikeium, Propionibacterium acnes, Bacillus species). Therefore, culture results must be interpreted with caution, and isolates should not be disregarded as mere contaminants. A contaminating organism in an immunocompetent individual may be a pathogen in an immunocompromised one.
Approach to Diagnosis
Not all fevers are due to infection. Transplant rejection, organ ischemia and necrosis, thrombophlebitis, and lymphoma (posttransplant lymphoproliferative disease) may all present as fever and must be considered in the differential diagnosis.
Because infections in the immunocompromised patient can be rapidly progressive and life-threatening, diagnostic procedures must be done promptly, and empiric therapy is usually instituted before a specific pathogenic organism has been isolated:
(1) Routine evaluation includes complete blood count with differential, chest x-ray, and blood cultures; urine and sputum cultures should be obtained if indicated clinically or radiographically. Any focal complaints (localized pain, headache, rash) should prompt imaging and cultures appropriate to the site.
(2) Patients who remain febrile without an obvious source should be evaluated for viral infection (CMV blood cultures or antigen test), abscesses (which usually occur near previous operative sites), candidiasis involving the liver or spleen, or aspergillosis. Serologic evaluation may be helpful if toxoplasmosis, aspergillosis (detected by galactomannan level in serum), or an endemic fungal infection (coccidioidomycosis, histoplasmosis) is a possible cause.
(3) Special diagnostic procedures should also be considered. The cause of pulmonary infiltrates can be easily determined with simple techniques in some situations—eg, induced sputum yields a diagnosis of Pneumocystis pneumonia in 50–80% of AIDS patients with this infection. In other situations, more invasive procedures may be required (bronchoalveolar lavage, transbronchial biopsy, or even open lung biopsy). Other investigations such as skin, liver, or bone marrow biopsy may be helpful in establishing a diagnosis.
(4) In patients who have undergone solid organ transplants, immediate postoperative infections often involve the transplanted organ. Following lung transplantation, pneumonia and mediastinitis are particularly common; following liver transplantation, intraabdominal abscess, cholangitis, and peritonitis may be seen; after renal transplantation, urinary tract infections, perinephric abscesses, and infected lymphoceles can occur. In contrast to solid organ transplant recipients, the source of fever cannot be found in 60–70% of bone marrow transplant patients.
(5) The time of occurrence of infection, particularly following solid organ transplantation, can be helpful in determining the infectious origin. Most infections that occur in the first 2–4 weeks posttransplant are related to the operative procedure and to hospitalization itself (wound infection, intravenous catheter infection, urinary tract infection from a Foley catheter) or are related to the transplanted organ (see paragraph [4], above). Infections that occur between
P.1290
the first and sixth months are often related to immunosuppression. During this period, reactivation of viruses occurs, and herpes simplex, varicella-zoster, and CMV infections are quite common. Opportunistic infections with fungi (eg, Candida, Aspergillus, Cryptococcus, Pneumocystis), Listeria monocytogenes, Nocardia, and Toxoplasma are also common. After 6 months, when immunosuppression has been reduced to maintenance levels, infections that are found in any population occur.
Prevention of Infection
There is great interest in preventing infection with prophylactic antimicrobial regimens but no uniformity of opinion about optimal drugs or dosage regimens.
Trimethoprim-sulfamethoxazole (TMP-SMZ), one double-strength tablet three times a week, one doublestrength tablet twice daily on weekends, or one singlestrength tablet daily for 3–6 months, is frequently used to prevent Pneumocystis infections in transplant patients. It may also decrease the incidence of bacterial pneumonia, urinary tract infections, Nocardia infections, and toxoplasmosis. In patients allergic to TMPSMZ, aerosolized pentamidine is used in a dosage of 300 mg once a month, as is dapsone, 50 mg daily or 100 mg three times weekly. (G6PD levels should be determined before therapy with the latter is instituted.) Acyclovir prevents herpes simplex infections in bone marrow and solid organ transplant recipients and is given to seropositive patients who are not receiving acyclovir or ganciclovir for CMV prophylaxis. The usual dose is 200 mg orally three times daily for 4 weeks (bone marrow transplants) to 12 weeks (other solid organ transplants).
Prevention of CMV is more difficult, and no uniformly accepted approach has been adopted. Prevention strategies often depend on the serologic status of the donor and recipient and the organ transplanted, which determines the level of immunosuppression after transplant. In solid organ transplants (liver, kidney, heart, lung), the greatest risk of developing CMV disease is in seronegative patients who receive organs from seropositive donors. These high-risk patients usually receive ganciclovir, 2.5–5 mg/kg intravenously twice daily, during hospitalization (usually about 10 days) and then are placed on a regimen of oral ganciclovir, 1 g three times daily, or the better absorbed valganciclovir, 900 mg twice daily, for 3 months. Other solid organ transplant recipients (seropositive recipients) are at lower risk for developing CMV disease and usually receive intravenous ganciclovir while in the hospital followed by either highdose oral acyclovir at a dosage of 800 mg four times daily or oral ganciclovir for 3 months. Ganciclovir, valganciclovir, and acyclovir prevent herpesvirus reactivation. Because immunosuppression is increased during periods of rejection, patients treated for rejection usually receive intravenous ganciclovir during rejection therapy.
Recipients of bone marrow transplants are more severely immunosuppressed than recipients of solid organ transplants, are at greater risk for developing serious CMV infection, and thus usually receive more aggressive prophylaxis. Two approaches have been used: universal prophylaxis or preemptive therapy. In the former, all high-risk patients (seropositive patients who receive allogeneic transplants) receive 5 mg/kg of intravenous ganciclovir every 12 hours for a week, followed by oral ganciclovir, 1 g three times daily or the better absorbed valganciclovir 900 mg twice daily to day 100. This method is costly and associated with significant toxicity and is therefore being used less frequently. Alternatively, patients can be monitored without specific therapy and have blood sampled weekly for the presence of CMV. If CMV is detected by an antigenemia assay, preemptive therapy with ganciclovir is given (5 mg/kg intravenously twice daily for 7–14 days, followed by oral valganciclovir 900 mg twice daily for a minimum of 3 weeks or until day 100, whichever is longer). This approach is effective but does miss a small number of patients in whom CMV disease subsequently develops. Other preventive strategies include use of CMV-negative or leukocyte-depleted blood products for CMV-seronegative recipients.
Routine decontamination of the gastrointestinal tract to prevent bacteremia in the neutropenic patient is not recommended. Prophylactic administration of antibiotics in the afebrile, asymptomatic neutropenic patient is controversial, although many centers have adopted this strategy. Rates of bacteremia are decreased, but overall mortality is not affected and emergence of resistant organisms is a common problem. Use of intravenous immunoglobulin is reserved for the small number of patients with severe hypogammaglobulinemia following bone marrow transplantation and should not be routinely administered to all transplant patients.
Prophylaxis with antifungal agents to prevent invasive mold (primarily Aspergillus) and yeast (primarily Candida) infections is routinely used, but the optimal agent, dose, and duration have not been standardized. Moderate-dose (0.5 mg/kg/d) and low-dose (0.1–0.25 mg/kg/d) amphotericin B, liposomal preparations of amphotericin B, aerosolized amphotericin B, and itraconazole (capsules and solution) have all been used with varying success in the neutropenic patient. Because voriconazole appears to be more effective than amphotericin for documented Aspergillus infections, one approach to prophylaxis is to use oral fluconazole (400 mg/d) for patients at low risk for developing fungal infections (those who receive autologous bone marrow transplants) and oral voriconazole (200 mg twice daily) for those at high risk (allogeneic transplants) at least until engraftment (usually 30 days). In solid organ transplant recipients, the risk of invasive fungal infection varies considerably (1–2% in liver, pancreas, and kidney transplants and 6–8% in heart and lung transplants). Whether universal prophylaxis or observation with preemptive therapy is the best ap
P.1291
proach has not been determined. Although fluconazole is effective in preventing yeast infections, emergence of resistant strains of Candida krusei, other Candida species, and molds (Fusarium, Aspergillus, Mucor) has raised concerns about its routine use as a prophylactic agent.
Hand washing is the simplest and most effective means of decreasing nosocomial infections in all patients, especially the compromised patient. Invasive devices such as central and peripheral lines and Foley catheters are a potential source of infection.
Approach to Treatment
Reduction or discontinuation of immunosuppressive medication may jeopardize the viability of the transplanted organ, but in life-threatening infections it is necessary as an adjunct to effective antimicrobial therapy. Hematopoietic growth factors (granulocyte and granulocyte-macrophage colony-stimulating factors) stimulate proliferation of bone marrow stem cells, resulting in an increase in peripheral leukocytes. These agents shorten the period of neutropenia and have been associated with fewer infections. Use of growth factors in patients with prolonged neutropenia (> 7 days) is an effective means of reversing immunosuppression.
Antimicrobial drug therapy is rationally based on culture results (see Chapter 37). Therapy should be specific for isolated pathogens, and bactericidal agents should be used. Combinations of antimicrobials are often required to provide synergy, to prevent resistance, or to serve as broad-spectrum coverage of multiple pathogens (since infections in these patients are often polymicrobial).
Empiric therapy is often instituted at the earliest sign of infection in the immunosuppressed patient because prompt therapy favorably affects outcome. The antibiotic or combination of antibiotics used depends on the type of immunocompromise and the site of infection. For example, in the febrile neutropenic patient, the primary concern is bacterial and fungal infections. Often in this patient population an algorithmic approach to therapy is used, with initial treatment directed at gram-positive and gram-negative organisms. If the patient does not respond, broader-spectrum antibiotics and antifungal drugs are added. Although a number of different agents can be used, choices should be based on local microbiologic trends. One example would be to initiate therapy with a fluoroquinolone active against gram-positive organisms (such as levofloxacin, gatifloxacin, or moxifloxacin) when the absolute neutrophil count falls below 500/mcL. If fever develops, cultures are obtained and vancomycin, 10–15 mg/ kg every 12 hours, is given (to cover methicillin-resistant S aureus, S epidermidis, and enterococcus). If after 48–72 hours fever continues, antifungal coverage can be increased by changing to voriconazole, 200 mg twice daily (if the patient was on fluconazole prophylaxis), and broader-spectrum antibiotics can be added sequentially. For example, to better cover Acinetobacter, Citrobacter, and Pseudomonas, the fluoroquinolone may be switched to cefipime, 2 g every 8 hours intravenously; with continued fever, imipenem, 500 mg every 6 hours (or meropenem, 1 g every 8 hours), with or without tobramycin, 1.8 mg/kg every 8 hours, may be used in place of cefipime. If fevers persist, TMP-SMZ at 10 mg/kg/d (of trimethoprim) in three divided doses can be added to cover Stenotrophomonas. Regardless of whether the patient becomes afebrile, therapy is continued until resolution of neutropenia. Failure to continue antibiotics through the period of neutropenia is associated with a high incidence of relapse that can be associated with septic shock. Patients with fever and neutropenia who are at low risk for developing complications (neutropenia expected to persist for less than 10 days, no comorbid complications requiring hospitalization, and cancer adequately treated) can be treated with oral antibiotic regimens (ciprofloxacin, 750 mg every 12 hours, plus amoxicillin-clavulanic acid, 500 mg every 8 hours). In the organ transplant patient with interstitial infiltrates, the main concern is infection with Pneumocystis or Legionella species, so that empiric treatment with a macrolide and TMP-SMZ would be reasonable. If the patient does not respond to empiric treatment, a decision must be made to add more antimicrobial agents or perform invasive procedures (see above) to make a specific diagnosis. By making a specific diagnosis, therapy can be specific and polypharmacy with multiple potentially toxic agents avoided.
Leather HL et al: Infections following hematopoietic stem cell transplantation. Infect Dis Clin North Am 2001;15:483.
Rubin RH: The direct and indirect effects of infection in liver transplantation: pathogenesis, impact, and clinical management. Curr Clin Top Infect Dis 2002;22:125.
Simon DM et al: Infectious complications of solid organ transplantation. Infect Dis Clin North Am 2001;15:521.
Viscoli C et al: Treatment of febrile neutropenia: what is new?; Curr Opin Infect Dis 2002;15:377.
NOSOCOMIAL INFECTIONS
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Nosocomial infections are defined as those not present or incubating at the time of hospital admission and developing 48–72 hours after admission.
Hand washing is the easiest and most effective means of preventing nosocomial infections and should be done routinely even when gloves are worn.
P.1292
In the United States, approximately 5% of patients who enter the hospital free of infection acquire a nosocomial infection resulting in prolongation of the hospital stay, increase in cost of care, significant morbidity, and a 5% mortality rate. Although most such fevers are due to infections, about 25% of patients will have fever of noninfectious origin. Causes include drug fever, nonspecific postoperative fevers (atelectasis, tissue damage or necrosis), hematoma, pancreatitis, pulmonary embolus, myocardial infarction, and ischemic bowel disease. The most common infections are urinary tract infections, usually associated with Foley catheters or urologic procedures; bloodstream infections, most commonly from indwelling catheters but also from secondary sites such as surgical wounds, abscesses, pneumonia, the genitourinary tract, and the gastrointestinal tract; pneumonia in intubated patients or those with altered levels of consciousness; surgical wound infections; and Clostridium difficile colitis.
Some general principles are helpful in preventing, diagnosing, and treating nosocomial infections:
(1) Many infections are a direct result of the use of invasive devices for monitoring or therapy such as intravenous catheters, Foley catheters, shunts, surgical drains, catheters placed by interventional radiology for drainage, nasogastric tubes, and orotracheal or nasotracheal tubes for ventilatory support. Early removal reduces the possibility of infection.
(2) Patients in whom nosocomial infections develop are often critically ill, have been hospitalized for extended periods, and have received several courses of broad-spectrum antibiotic therapy. As a result, nosocomial infections are often caused by organisms that are multidrug-resistant and are different from those encountered in community-acquired infections. Examples are S aureus and S epidermidis (a frequent cause of prosthetic device infection) that may be resistant to nafcillin and cephalosporins and require vancomycin for therapy; Enterococcus faecium resistant to ampicillin and vancomycin; gram-negative infections caused by Pseudomonas, Citrobacter, Enterobacter, Acinetobacter, and Stenotrophomonas, which may be sensitive only to fluoroquinolones, carbapenems, aminoglycosides, or TMP-SMZ. When choosing antibiotics to treat the seriously ill patient with a nosocomial infection, the previous antimicrobial the patient has received as well as the “local ecology” must be considered. It is often necessary to institute therapy with vancomycin and a carbapenem or aminoglycoside until a specific agent is isolated and sensitivities are known, at which time the least toxic and most cost-effective drug can be used.
One promising approach to preventing the development of multidrug-resistant organisms is antibiotic cycling. By changing the class of antibiotic primarily used every 6–12 months (eg, a cephalosporin, then fluoroquinolones, then carbapenems), selection pressure is decreased and less resistance emerges.
Because widespread use of antimicrobial drugs contributes to the selection of drug-resistant organisms that cause nosocomial infections, every effort should be made to limit the use of antibiotics to treat documented infections. All too often, unreliable or uninterpretable specimens are obtained for culture that result in unnecessary use of antibiotics. The best example of this principle is the diagnosis of line-related or bloodstream infection in the febrile patient. Blood cultures from unidentified sites, a single blood culture from any site, or a blood culture through an existing line will often be positive for S epidermidis and will result in therapy with vancomycin. The likelihood that such a culture represents a true bacteremia is 10–20%. Unless two separate venipuncture cultures are obtained— not through catheters—interpretation of results is impossible and unnecessary therapy is given. Every such “pseudobacteremia” increases laboratory costs, antibiotic use, and length of stay and increases costs of hospitalization by about $4500. To avoid unnecessary use of antibiotics, thoughtful consideration of culture results is mandatory. A positive wound culture without signs of inflammation or infection, a positive sputum culture without pulmonary infiltrates on chest x-ray, or a positive urine culture in a catheterized patient without symptoms or signs of pyelonephritis are all likely to represent colonization, not infection.
Prevention is of paramount importance in controlling nosocomial infections. The concept of universal precautions emphasizes that all patients are treated as though they have a potential blood-borne transmissible disease, and thus all body secretions are handled with care to prevent spread of disease. Almost all hospitals have implemented body substance isolation, which requires use of gloves whenever a health care worker anticipates contact with blood or other body secretions. The use of gloves is intended to prevent contamination of the hands of health care workers with infected secretions and subsequent spread of infection to other patients by direct contact. Hand washing is the easiest and most effective means of preventing nosocomial infections and should be done routinely even when gloves are worn. Application of a rapid drying, alcohol-based antiseptic is easy to do, takes less time than traditional hand washing with soap and water, is more effective at reducing hand colonization, promotes compliance with hand decontamination, and is rapidly becoming the method of choice for hand disinfection. Peripheral intravenous lines should be replaced every 3 days and arterial lines every 4 days. Lines in the central venous circulation (including those placed peripherally) can be left in indefinitely and are changed or removed when they are clinically suspected of being infected, when they are nonfunctional, or when they are no longer needed. Silver alloy-impregnated Foley catheters reduce the incidence of catheterassociated bacteriuria, and antibiotic-impregnated (minocycline plus rifampin or chlorhexidine plus silver sulfadiazine) venous catheters reduce line infections and bacteremia. Whether the increased cost of these devices justifies their routine use should be determined by individual institutions based on local infection rates. Selective decontamination of the digestive tract
P.1293
with nonabsorbable antibiotics to prevent nosocomial pneumonia is widely used in Europe, but the therapeutic efficacy of this expensive intervention is controversial. Attentive nursing care (positioning to prevent decubitus ulcers, wound care, elevating the head during tube feedings to prevent aspiration) is critical in preventing nosocomial infections. In addition, monitoring of high-risk areas by hospital epidemiologists detects increases in infection rates early and is a key factor in prevention of these types of infections.
Several highly effective vaccines have been approved by the US Food and Drug Administration (FDA) that add to our armamentarium for prevention of certain nosocomial infections. Hepatitis A, hepatitis B, and the varicella vaccine should be considered in the appropriate setting. (See section below on Immunization Against Infectious Diseases.)
Kollef MH: Prevention of hospital-associated pneumonia and ventilator-associated pneumonia. Crit Care Med 2004;32: 1396.
Lorente C et al: Prevention of infection in the intensive care unit: current advances and opportunities for the future. Curr Opin Crit Care 2002;8:461.
Vincent JL: Nosocomial infections in adult intensive-care units. Lancet 2003;361:2068.
INFECTIONS OF THE CENTRAL NERVOUS SYSTEM
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Central nervous system infection is a medical emergency.
Symptoms and signs common to all types of central nervous system infection include headache, fever, sensorial disturbances, neck and back stiffness, positive Kernig and Brudzinski signs, and cerebrospinal fluid abnormalities.
General Considerations
Infections of the central nervous system can be caused by almost any infectious agent, including bacteria, mycobacteria, fungi, spirochetes, protozoa, helminths, and viruses. Although it is rare for all of the symptoms and signs to be present in any one individual, the presence of even one should suggest the possibility of a central nervous system infection.
Evaluation of a patient with suspected meningitis includes a history, physical examination, blood count, blood culture, lumbar puncture followed by careful study and culture of the cerebrospinal fluid, and a chest film. The fluid must be examined for cell count, glucose, and protein, and a smear stained for bacteria (and acid-fast organisms when appropriate) and cultured for pyogenic organisms and for mycobacteria and fungi when indicated. Latex agglutination tests can detect antigens of encapsulated organisms (S pneumoniae, H influenzae, N meningitidis, and Cryptococcus neoformans) but are rarely used except for detection of Cryptococcus or in partially treated patients. Polymerase chain reaction (PCR) testing of cerebrospinal fluid has been used to detect bacteria (S pneumoniae, H influenzae, N meningitidis, Mycobacterium tuberculosis, Borrelia burgdorferi, and Tropheryma whippelii) and viruses (herpes simplex, varicella-zoster, CMV, Epstein-Barr virus, and enteroviruses) in patients with meningitis. The greatest experience is with PCR for herpes simplex and varicella-zoster, and the tests are very sensitive (> 95%) and specific. Tests to detect the other organisms may not be any more sensitive than culture, but the real value is the rapidity with which results are available, ie, hours compared with days or weeks. At present, with the exception of PCR for herpes simplex, these tests are performed only in reference laboratories. Although it is difficult to prove with existing clinical data that early antibiotic therapy improves outcome in bacterial meningitis, prompt therapy is still recommended.
Since performing a lumbar puncture in the presence of a space-occupying lesion (brain abscess, subdural hematoma, subdural abscess) may result in brainstem herniation, a CT scan is performed prior to lumbar puncture if a space-occupying lesion is suspected on the basis of papilledema, coma, seizures, or focal neurologic findings. If delays are encountered in obtaining a CT scan and bacterial meningitis is suspected, blood cultures should be drawn and antibiotics and corticosteroids administered even before cerebrospinal fluid is obtained for culture to avoid delay in treatment (Table 30-1). Antibiotics given within 4 hours before obtaining cerebrospinal fluid probably do not affect culture results.
Etiologic Classification
Central nervous system infections can be divided into several categories that usually can be readily distinguished from each other by cerebrospinal fluid examination as the first step toward etiologic diagnosis (Table 30-2).
A. PURULENT MENINGITIS
Patients with bacterial meningitis usually seek medical attention within hours or 1–2 days after onset of symptoms. The organisms responsible depend primarily on the age of the patient as summarized in Table 30-1. The diagnosis is usually based on the Gramstained smear (positive in 60–80%) or culture (positive in over 90%).
B. CHRONIC MENINGITIS
The presentation of chronic meningitis is less acute than purulent meningitis. Patients with chronic meningitis usually have a history of symptoms lasting weeks to months. The most common pathogens are Mycobacterium tuberculosis, atypical mycobacteria, fungi (Cryptococcus, Coccidioides, Histoplasma), and
P.1294
spirochetes (Treponema pallidum and B burgdorferi, the cause of Lyme disease). The diagnosis is made by culture or in some cases by serologic tests (cryptococcosis, coccidioidomycosis, syphilis, Lyme disease).
Table 30-1. Initial antimicrobial therapy for purulent meningitis of unknown cause. | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
C. ASEPTIC MENINGITIS
Aseptic meningitis—a much more benign and selflimited syndrome than purulent meningitis—is caused principally by viruses, especially mumps virus and the enterovirus group (including coxsackieviruses and echoviruses). Infectious mononucleosis may be accompanied by aseptic meningitis. Leptospiral infection is also usually placed in the aseptic group because of the lymphocytic cellular response and its relatively benign course. This type of meningitis also occurs during secondary syphilis and disseminated Lyme disease.
D. ENCEPHALITIS
Encephalitis (due to herpesviruses, arboviruses, rabies virus, flaviviruses [West Nile encephalitis, Japanese encephalitis], and many others) produces disturbances of the sensorium, seizures, and many other manifestations. Patients are more ill than those with aseptic meningitis. Cerebrospinal fluid may be entirely normal or may show some lymphocytes and in some instances (eg, herpes simplex) red cells as well.
Table 30-2. Typical cerebrospinal fluid findings in various central nervous system diseases. | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
P.1295
E. PARTIALLY TREATED BACTERIAL MENINGITIS
Previous effective antibiotic therapy given for 12–24 hours will decrease the rate of positive Gram stain results by 20% and culture by 30–40% but will have little effect on cell count, protein, or glucose. Occasionally, previous antibiotic therapy will change a predominantly polymorphonuclear response to a lymphocytic pleocytosis, and some of the cerebrospinal fluid findings may be similar to those seen in aseptic meningitis.
F. NEIGHBORHOOD REACTION
As noted in Table 30-2, this term denotes a purulent infectious process in close proximity to the central nervous system that spills some of the products of the inflammatory process—white blood cells or protein— into the cerebrospinal fluid. Such an infection might be a brain abscess, osteomyelitis of the vertebrae, epidural abscess, subdural empyema, or bacterial sinusitis or mastoiditis.
G. NONINFECTIOUS MENINGEAL IRRITATION
Carcinomatous meningitis, sarcoidosis, systemic lupus erythematosus, chemical meningitis, and certain drugs— nonsteroidal anti-inflammatory drugs, muromonab-CD3 (OKT3), TMP-SMZ, and others—can also produce symptoms and signs of meningeal irritation with associated cerebrospinal fluid pleocytosis, increased protein, and low or normal glucose. Meningismus with normal cerebrospinal fluid findings occurs in the presence of other infections such as pneumonia and shigellosis.
H. BRAIN ABSCESS
Brain abscess presents as a space-occupying lesion; symptoms may include vomiting, fever, change of mental status, or focal neurologic manifestations. When brain abscess is suspected, a CT scan should be performed. If positive, lumbar puncture should not be performed since results rarely provide clinically useful information and herniation can occur. The bacteriology of brain abscess is usually polymicrobial and includes S aureus, gram-negative bacilli, streptococci, and anaerobes (including anaerobic streptococci and Prevotella species).
I. AMEBIC MENINGOENCEPHALITIS
These infections are caused by free-living amebas and present as two distinct syndromes. The diagnosis is confirmed by culture or identification of the organism in cerebrospinal fluid or on biopsy specimens. No effective therapy is available.
Primary amebic meningoencephalitis is caused by Naegleria fowleri and is an acute fulminant disease characterized by signs of meningeal irritation that rapidly progresses to encephalitis and death. Rare cases have been reported with intravenous and intraventricular administration of amphotericin B.
Granulomatous amebic encephalitis is caused by Acanthamoeba species. It is an indolent disease characterized by headache, nausea, vomiting, cranial neuropathies, seizures, and hemiparesis.
Treatment
Increased intracranial pressure due to brain edema often requires therapeutic attention. Hyperventilation, mannitol (25–50 g as a bolus intravenous infusion), and even drainage of cerebrospinal fluid by repeated lumbar punctures or by placement of ventricular catheters have been used to control cerebral edema and increased intracranial pressure. Dexamethasone (4 mg every 4–6 hours) may also decrease cerebral edema. In purulent meningitis, the identity of the causative microorganism may remain unknown or doubtful for a few days and initial antibiotic treatment as set forth in Table 30-1 should be directed against the microorganisms most common for each age group.
The duration of therapy for bacterial meningitis varies depending on the etiologic agent: H influenzae, 7 days; N meningitidis, 3–7 days; S pneumoniae, 10–14 days; L monocytogenes, 14–21 days; and gram-negative bacilli, 21 days.
Dexamethasone therapy is recommended for adults with pneumococcal meningitis. Ten milligrams of dexamethasone administered 15–20 minutes before or simultaneously with the first dose of antibiotics and continued every 6 hours for 4 days decreases morbidity and mortality. The number of patients with meningitis due to N meningitidis and other bacterial pathogens studied does not support similar conclusions. However, because adverse effects of dexamethasone for short periods are few and because potential benefits are great, many would advocate dexamethasone even if N meningitidis is the causative agent.
Therapy of brain abscess consists of drainage (excision or aspiration) in addition to 3–4 weeks of systemic antibiotics directed against organisms isolated. A regimen often used includes metronidazole, 500 mg intravenously or orally every 8 hours, plus ceftizoxime, 2 g intravenously every 8 hours, or ceftriaxone, 2 g every 12 hours. In cases where abscesses are less than 2 cm in size, where there are multiple abscesses that cannot be drained, or if an abscess is located in an area where significant neurologic sequelae would result from drainage, antibiotics for 6–8 weeks without drainage can be used.
Therapy of other types of meningitis is discussed elsewhere in this book (fungal meningitis, Chapter 36; syphilis and Lyme borreliosis, Chapter 34; tuberculous meningitis, Chapter 33; herpes encephalitis, Chapter 32).
Bernardini GL: Diagnosis and management of brain abscess and subdural empyema. Curr Neurol Neurosci Rep 2004;4:448.
De Gans J et al: Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002;347:1549.
Sinner SW et al: Antimicrobial agents in the treatment of bacterial meningitis. Infect Dis Clin North Am 2004;18:581.
P.1296
ANIMAL & HUMAN BITE WOUNDS
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Cat and human bites are more likely to become infected than dog bites.
Bites to the hand are of special concern because of the possibility of closed-space infection.
Antibiotic prophylaxis indicated for noninfected bites of the hand and hospitalization required for infected hand bites.
All infected wounds need to be cultured to direct therapy.
General Considerations
About 900 dog bite injuries require emergency department attention each day, most often in urban areas. Dog bites occur most commonly in the summer months. Biting animals are usually known by their victims, and most biting incidents are provoked (ie, bites occur while playing with the animal or after surprising the animal or waking it abruptly from sleep). Failure to elicit a history of provocation is important, because an unprovoked attack raises the possibility of rabies. Human bites are usually inflicted by children while playing or fighting; in adults, bites are associated with alcohol use and closedfist injuries that occur during fights.
The animal inflicting the bite, the location of the bite, and the type of injury inflicted are all important determinants of whether they become infected. Cat bites are more likely to become infected than human bites—between 30% and 50% of all cat bites become infected. Infections following human bites are variable: Those inflicted by children rarely become infected because they are superficial, and bites by adults become infected in 15–30% of cases, with a particularly high rate of infection in closed-fist injuries. Dog bites, for unclear reasons, become infected only 5% of the time. Bites of the head, face, and neck are less likely to become infected than bites on the extremities. Puncture wounds become infected more frequently than lacerations, probably because the latter are easier to irrigate and debride.
The bacteriology of bite infections is polymicrobial. Following dog and cat bites, over 50% of infections are caused by aerobes and anaerobes and 36% are due to aerobes alone. Pure anaerobic infections are rare. Pasteurella species are the single most common isolate (75% of cat bites and 50% of dog bites). Other common aerobic isolates include streptococci, staphylococci, Moraxella, and Neisseria; the most common anaerobes are Fusobacterium, Bacteroides, Porphyromonas, and Prevotella. The median number of isolates following human bites is four (three aerobes and one anaerobe). Like dog and cat bites, most human bites are a mixture of aerobes and anaerobes (54%) or are due to aerobes alone (44%). Streptococcus, Staphylococcus, and Eikenella corrodens (found in 30% of patients) are the most common aerobes. Prevotella and Fusobacterium are the most common anaerobes. Although the organisms noted are the most common, innumerable others have been isolated—including Capnocytophagia (dog and cats), Pseudomonas, and Haemophilus—emphasizing the point that all infected bites should be cultured to define the microbiology.
There have been no documented cases of HIV transmission by human bites.
Treatment
A. LOCAL CARE
Vigorous cleansing and irrigation of the wound as well as debridement of necrotic material are the most important factors in decreasing the incidence of infections. Xrays should be obtained to look for fractures and the presence of foreign bodies. Careful examination to assess the extent of the injury (tendon laceration, joint space penetration) is critical to appropriate care.
B. SUTURING
If wounds require closure for cosmetic or mechanical reasons, suturing can be done. However, one should never suture an infected wound, and wounds of the hand should generally not be sutured since a closedspace infection of the hand can result in loss of function.
C. PROPHYLACTIC ANTIBIOTICS
Prophylaxis is indicated in high-risk bites, eg, cat bites in any location (dicloxacillin, 0.5 g orally four times a day for 3–5 days) and hand bites by any animal or by humans (penicillin V, 0.5 g orally four times a day for 3–5 days). Although dicloxacillin and penicillin have been specifically studied, there is concern about their use because of their narrow spectrum of activity. Based on the microbiology of bite wounds, other agents less adequately studied but that have broader spectrums of activity may be better as prophylactic agents. Examples include cefuroxime, amoxicillin-clavulanic acid and, in the penicillin-allergic patient, clindamycin plus a fluoroquinolone. Immunocompromised patients and especially individuals without functional spleens are at risk for developing overwhelming bacteremia and sepsis following animal bites and should also receive prophylaxis, even for low-risk bites.
D. ANTIBIOTICS
For wounds that are infected, antibiotics are clearly indicated. How they are given (orally or intravenously) and the need for hospitalization are individualized clinical decisions. In general, Pasteurella multocida is best treated with penicillin or a tetracycline. Other active agents include secondand third-generation cephalosporins, fluoroquinolones, or azithromycin and clarithromycin. Response to therapy is slow, and ther
P.1297
apy should be continued for at least 2–3 weeks. Human bites frequently require intravenous therapy with a βlactam plus a βlactamase inhibitor combination (Unasyn, Timentin, Zosyn), a second-generation cephalosporin with anaerobic activity (cefoxitin, cefotetan, cefmetazole), or, in the penicillin-allergic patient, clindamycin plus a fluoroquinolone. Because the bacteriology of these infections is so variable, infected wounds should always be cultured.
E. TETANUS AND RABIES
All patients must be evaluated for the need for tetanus (see Chapter 33) and rabies (see Chapter 32) prophylaxis.
Brook I: Microbiology and management of human and animal bite wound infections. Prim Care 2003;30:25.
Medeiros I et al: Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev 2001;(2):CD001738.
Talan DA et al: Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis 2003;37:1481.
SEXUALLY TRANSMITTED DISEASES
Some infectious diseases are transmitted most commonly—or most efficiently—by sexual contact. Most of the infectious agents that cause sexually transmitted diseases are fairly easily inactivated when exposed to a harsh environment. They are thus particularly suited to transmission by contact with mucous membranes. They may be bacteria, spirochetes, chlamydiae, viruses, or protozoa. In most infections caused by these agents, early lesions occur on genitalia or other sexually exposed mucous membranes; however, wide dissemination may occur, and involvement of nongenital tissues and organs may mimic many noninfectious disorders. All sexually transmitted diseases have subclinical or latent phases that play an important role in long-term persistence of the infection or in its transmission from infected (but largely asymptomatic) persons to other contacts. Laboratory examinations are of particular importance in the diagnosis of such asymptomatic patients. Simultaneous infection by several different agents is common, and any person with a sexually transmitted disease should be tested for syphilis; a repeat study should be done in 3 months if negative, since seroconversion is delayed after primary infection.
For each patient, there are one or more sexual contacts who require diagnosis and treatment. As a rule, sexual partners should be treated simultaneously to avoid prompt reinfection. The most common sexually transmitted diseases are gonorrhea,* syphilis,* condyloma acuminatum, chlamydial genital infections*, herpesvirus genital infections, trichomonas vaginitis, chancroid,* granuloma inguinale,* scabies, louse infestation, and bacterial vaginosis (among lesbians). However, shigellosis,* hepatitis A, B, and C,* amebiasis, giardiasis*, cryptosporidiosis*, salmonellosis,* and campylobacteriosis may also be transmitted by sexual (oral-anal) contact, especially in homosexual males. Homosexual contact is a typical method of transmission of HIV, although bidirectional heterosexual transmission is occurring more commonly (see Chapter 31).
The risk of developing a sexually transmitted disease following a sexual assault has not been established. Victims of assault have a high baseline rate of infection (Neisseria gonorrhoeae, 6%, Chlamydia trachomatis, 10%, Trichomonas vaginalis, 15%, and bacterial vaginosis, 34%), and the risk of acquiring infection as a result of the assault is significant but is often lower than the preexisting rate (N gonorrhoeae, 6–12%; C trachomatis, 4–17%; T vaginalis, 12%; syphilis, 0.5–3%; and bacterial vaginosis, 19%). Victims should be evaluated within 24 hours after the assault, and cultures for N gonorrhoeae and C trachomatis should be obtained. (If culture is not available, nonculture tests, such as nucleic acid amplification tests, are acceptable. If the test is positive, it must be confirmed with a second test using a different target sequence.) Vaginal secretions are cultured and examined for Trichomonas. If a discharge is present, if there is itching, or if secretions are malodorous, a wet mount should be examined for Candida and bacterial vaginosis. In addition, a blood sample should be obtained for immediate serologic testing for syphilis, hepatitis B, and HIV. Follow-up examination for sexually transmitted disease should be repeated within 1–2 weeks, since concentrations of infecting organisms may not have been sufficient to produce a positive culture at the time of initial examination. If prophylactic treatment was given (see below), tests should be repeated only if the victim has symptoms. If prophylaxis was not administered, the individual should be seen in 1 week so that any positive tests can be treated. Followup serologic testing for syphilis and HIV infection should be performed in 6, 12, and 24 weeks if the initial tests are negative. The usefulness of presumptive therapy is controversial, some feeling that all patients should receive it and others that it should be limited to those in whom follow-up cannot be ensured or to patients who request it. If therapy is given, a reasonable regimen would be hepatitis B vaccination (without hepatitis B immune globulin, the first dose given at the initial evaluation and follow-up doses at 1–2 months and 4–6 months) and one dose of ceftriaxone, 125 mg intramuscularly, plus metronidazole, 2 g orally as a single dose, plus doxycycline, 100 mg orally twice daily for 7 days, or azithromycin, 1 g orally as a single dose. In premenopausal women, azithromycin should be used instead of doxycycline until the pregnancy status is determined; if the pregnancy test is positive, metronidazole should be given only after the first trimester.
P.1298
Although seroconversion to HIV has been reported following sexual assault when this was the only known risk, this risk is believed to be low. The likelihood of HIV transmission from anal or vaginal receptive intercourse when the source is known to be HIV positive is 1–3 per 1000. Because prophylactic antiretroviral therapy has not been studied in this setting, firm recommendations cannot be made and the decision to institute therapy should be individualized. If therapy is given, it should be prompt, and certainly no later than 72 hours.
Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep 2002;51(RR-6):1.
INFECTIONS IN DRUG USERS
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Common infections that occur with greater frequency in drug users include the following: skin infections; hepatitis A, B, C, D; aspiration pneumonia; tuberculosis; pulmonary septic emboli; sexually transmitted diseases; AIDS; infective endocarditis; osteomyelitis; and septic arthritis.
Rare infections in the United States include tetanus, malaria, and melioidosis.
General Considerations
The use of parenterally administered recreational drugs has increased enormously in recent years. There are now an estimated 300,000 or more injection drug users in the United States.
Common Infections That Occur with Greater Frequency in Drug Users
(1) Skin infections are associated with poor hygiene and use of nonsterile technique when injecting drugs. S aureus (including methicillin-resistant strains) and oral flora (streptococci, Eikenella, Fusobacterium, Peptostreptococcus) are the most common organisms, with enteric gram-negatives less common and seen in those who inject into the groin. Cellulitis and subcutaneous abscesses occur most commonly, particularly in association with subcutaneous (“skin-popping”) or intramuscular injections and the use of cocaine and heroin mixtures (probably due to ischemia). Myositis, clostridial myonecrosis, and necrotizing fasciitis occur infrequently but are life-threatening. Wound botulism in association with black tar heroin occurs sporadically but often in clusters.
(2) Hepatitis is very common among habitual drug users and is transmissible both by the parenteral (hepatitis B, C, and D) and by the fecal-oral route (hepatitis A). Multiple episodes of hepatitis with different agents can occur.
(3) Aspiration pneumonia and its complications (lung abscess, empyema, brain abscess) result from altered consciousness associated with drug use. Mixed aerobic and anaerobic mouth flora are usually involved.
(4) Tuberculosis also occurs in drug users, and infection with HIV has fostered the spread of tuberculosis in this population. Morbidity and mortality rates are increased in HIV-infected individuals with tuberculosis. Classic radiographic findings are often absent; tuberculosis is suspected in any patient with infiltrates who does not respond to antibiotics.
(5) Pulmonary septic emboli may originate from venous thrombi or right-sided endocarditis.
(6) Sexually transmitted diseases are not directly related to drug use, but the practice of exchanging sex for drugs has resulted in an increased frequency of sexually transmitted diseases. Syphilis, gonorrhea, and chancroid are the most common.
(7) AIDS has a high incidence among injection drug users and their sexual contacts and among the offspring of infected women (see Chapter 31).
(8) Infective endocarditis. The organisms that cause infective endocarditis in those who use drugs intravenously are most commonly S aureus, Candida (especially Candida parapsilosis), Enterococcus faecalis, other streptococci, and gram-negative bacteria (especially Pseudomonas and Serratia marcescens). A number of complications of endocarditis can occur, including splenic abscesses, central nervous system infections (meningitis, brain abscess, subdural empyema, epidural abscess), and endophthalmitis. Involvement of the right side of the heart is common, and infection of more than one valve is not infrequent. Right-sided involvement, especially in the absence of murmurs, is often suggested by the presence of septic pulmonary emboli. The diagnosis must be established by blood culture. Therapy, including empiric treatment, is discussed in Chapter 33.
(9) Other vascular infections include septic thrombophlebitis and mycotic aneurysms. Mycotic aneurysms resulting from direct trauma to a vessel with secondary infection most commonly occur in femoral arteries and less commonly in arteries of the neck. Aneurysms resulting from hematogenous spread of organisms frequently involve intracerebral vessels and thus are seen in association with endocarditis.
(10) Osteomyelitis and septic arthritis. Osteomyelitis involving vertebral bodies, sternoclavicular joints, the pubic symphysis, the sacroiliac joints, and other sites usually results from hematogenous distribution of injected organisms or septic venous thrombi. Pain and fever precede radiographic changes, sometimes by several weeks. While staphylococci—often methicillin-resistant—are common organisms, Serratia, Pseudomonas, Candida (usually not Candida albicans), and other pathogens rarely encountered in spontaneous bone or joint disease are found in injection drug users.
P.1299
Infections Rare in United States
A. TETANUS
In the 1950s and 1960s, tetanus was commonly seen in drug users, especially in unimmunized women who injected drugs subcutaneously (“skin-popping”). Increased tetanus immunization among drug users has resulted in a decline in this disease, although cases are still reported.
B. MALARIA
Needle transmission occurs from injection drug users who acquired the infection in malaria-endemic areas outside the United States.
C. MELIOIDOSIS
This chronic pulmonary infection caused by Burkholderia pseudomallei occurs occasionally in debilitated drug users, but most cases are reported in Asia and Australia.
Treatment
A common and difficult clinical problem is management of the parenteral drug user who presents with fever. In general, after obtaining appropriate cultures (blood, urine, and sputum if the chest x-ray is abnormal), empiric therapy is begun. If the chest xray is suggestive of a community-acquired pneumonia (consolidation), therapy for outpatient pneumonia is begun with a secondor third-generation cephalosporin (many clinicians would add azithromycin or doxycycline to this regimen). If the chest x-ray is suggestive of septic emboli (nodular infiltrates), therapy for presumed endocarditis is initiated, usually with a combination of nafcillin (or vancomycin if there is a high prevalence of methicillin-resistant S aureus or if enterococcus is a consideration) and gentamicin. If the chest x-ray is normal and no focal site of infection can be found, endocarditis is presumed. While awaiting the results of blood cultures, empiric treatment with nafcillin (or vancomycin) and gentamicin is started. If blood cultures are positive for organisms that frequently cause endocarditis in drug users (see above), endocarditis is presumed to be present and treated accordingly. If blood cultures are positive for an organism that is an unusual cause of endocarditis, evaluation for an occult source of infection should go forward. In this setting, a transesophageal echocardiogram may be quite helpful since it is 90% sensitive in detecting vegetations and a negative study is strong evidence against endocarditis. If blood cultures are negative and the patient responds to antibiotics, therapy should be continued for 7–14 days (oral therapy can be given once an initial response has occurred). In every patient, careful examination for an occult source of infection (genitourinary, dental, sinus, gallbladder, etc) should be done.
Infections in injection drug users (entire issue). Infect Dis Clin North Am 2002;16:3.
Murphy EL et al: Risk factors for skin and soft-tissue abscesses among injection drug users: a case-control study. Clin Infect Dis 2001;33:35.
ACUTE INFECTIOUS DIARRHEA
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Arbitrarily divided into acute and chronic and mild, moderate, and severe.
Diarrhea is acute if lasts < 2 weeks and chronic if lasts > 2 weeks.
Disease is mild if there are three or fewer stools per day, moderate if there are four or more stools in association with local symptoms (abdominal cramps, nausea, tenesmus), and severe if there are four or more stools per day with systemic symptoms (fevers, chills, dehydration).
General Considerations
Acute diarrhea can be caused by a number of different factors, including emotional stress, food intolerance, inorganic agents (eg, sodium nitrite), organic substances (eg, mushrooms, shellfish), drugs, and infectious agents (including viruses, bacteria, and protozoa). From a diagnostic and therapeutic standpoint, it is helpful to classify infectious diarrhea into syndromes that produce inflammatory or bloody diarrhea and those that are noninflammatory, nonbloody, or watery. In general, the term “inflammatory diarrhea” suggests colonic involvement by invasive bacteria or parasites or by toxin production. Patients present with frequent bloody, smallvolume stools, often associated with fever, abdominal cramps, tenesmus, and fecal urgency. Common causes of this syndrome include Shigella, Salmonella, Campylobacter, Yersinia, invasive strains of E coli, E coli O157:H7, Entamoeba histolytica, and C difficile. Tests for fecal leukocytes or the neutrophil marker lactoferrin are frequently positive, and definitive etiologic diagnosis requires stool culture. Noninflammatory diarrhea is generally milder and is caused by viruses or toxins that affect the small intestine and interfere with salt and water balance, resulting in large-volume watery diarrhea, often with nausea, vomiting, and cramps. Common causes of this syndrome include viruses (eg, rotavirus, Norwalk virus, enteric adenoviruses, astrovirus, coronavirus), vibriones (Vibrio cholerae, Vibrio parahaemolyticus), enterotoxin-producing E coli, Giardia lamblia, cryptosporidia, and agents that can cause food-borne gastroenteritis.
The term “food poisoning” denotes diseases caused by toxins present in consumed foods. When the incubation period is short (1–6 hours after consumption), the toxin is usually preformed. Vomiting is usually a
P.1300
major complaint, and fever is usually absent. Examples include intoxication from S aureus or Bacillus cereus, and toxin can be detected in the food. When the incubation period is longer—between 8 hours and 16 hours—the organism is present in the food and produces toxin after being ingested. Vomiting is less prominent, abdominal cramping is frequent, and fever is often absent. The best example of this disease is that due to Clostridium perfringens. Toxin can be detected in food or stool specimens.
The inflammatory and noninflammatory diarrheas discussed above can also be transmitted by food and water and usually have incubation periods between 12 and 72 hours. Cyclospora, cryptosporidia, and Isospora are protozoans capable of causing disease in both immunocompetent and immunocompromised patients. Characteristics of disease include profuse watery diarrhea that is prolonged but usually self-limited (1–2 weeks) in the immunocompetent patient but can be chronic in the compromised host. Epidemiologic features may be helpful in determining etiology. Recent hospitalization or antibiotic use suggests C difficile; recent foreign travel suggests Salmonella, Shigella, Campylobacter, E coli, or V cholerae; undercooked hamburger suggests E coli, especially O157:H7; and fried rice consumption is associated with B cereus toxin. Prominent features of some of these causes of diarrhea are listed in Table 30-3.
Treatment
Treatment usually consists of replacement of fluids and electrolytes and, very rarely, management of hypovolemic shock and respiratory compromise. In mild diarrhea, increasing ingestion of juices and clear soups is adequate. In more severe cases of dehydration (postural lightheadedness, decreased urination), oral glucosebased rehydration solutions can be used (Ceralyte, Pedialyte). In general, most cases of acute gastroenteritis are self-limited and do not require therapy other than supportive measures. When symptoms persist beyond 3–4 days, initial presentation is accompanied by fever or bloody diarrhea, or if the patient is immunocompromised, cultures of stool are usually obtained. Symptoms have often resolved by the time cultures are completed. In this case, even if a pathogen is isolated, therapy is not needed (except for Shigella, since the infecting dose is so small that therapy to eradicate organisms from the stool is indicated for epidemiologic reasons). If symptoms persist and a pathogen is isolated, it is reasonable to institute specific treatment even though therapy has not been conclusively shown to alter the natural history of disease for most pathogens. Exceptions include infection with Shigella where antibiotic therapy has been shown to shorten the duration of symptoms by 2–3 days, infections with E coli O157:H7 (antibiotic therapy does not ameliorate symptoms and may increase the risk of developing hemolytic-uremic syndrome), and Campylobacter infections (early therapy, within 4 days of onset of symptoms, shortens the course of disease).
Uncomplicated gastroenteritis due to Salmonella does not require therapy because the disease is usually selflimited and therapy may prolong carriage and perhaps increase relapses. Because bacteremia with complications can occur in high-risk patients, some experts have recommended therapy for Salmonella in patients over the age of 50, in organ transplant recipients, in those with HIV, in patients taking corticosteroids, in those with lymphoproliferative diseases, and in those with vascular grafts. Ciprofloxacin, 500 mg every 12 hours for 5 days, is effective in shortening the course of illness compared with placebo in patients presenting with diarrhea, whether a pathogen is isolated or not. However, because of concerns about selecting for resistant organisms (especially Campylobacter, where increasing resistance to fluoroquinolones has been documented and erythromycin is the drug of choice) coupled with the fact that most infectious diarrhea is self-limited, routine use of antibiotics for all patients with diarrhea is not recommended. Antibiotics should be considered in patients with evidence of invasive disease (white cells in stool, dysentery), with symptoms 3–4 days or more in duration, with multiple stools (eight to ten or more per day), and in those with impaired immune responses. Antimotility drugs may relieve cramping and decrease diarrhea in mild cases. Their use should be limited to patients without fever and without dysentery (bloody stools), and they should be used in low doses because of the risk of producing toxic megacolon.
Therapeutic recommendations for specific agents can be found elsewhere in this book.
Diagnosis and management of foodborne illnesses: a primer for physicians and other health care professionals. MMWR Recomm Rep 2004;53(RR-4):1.
Guerrant RL et al: Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 2001;32:331.
Ilnyckyj A: Clinical evaluation and management of acute infectious diarrhea in adults. Gastroenterol Clin North Am 2001;30: 599.
Musher DM et al: Contagious acute gastrointestinal infections N Engl J Med 2004;351:2417.
Thielman NM et al: Clinical Practice. Acute infectious diarrhea. N Engl J Med 2004;350:38.
TRAVELER'S DIARRHEA
![]() ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Usually a benign, self-limited disease occurring about 1 week into travel.
Prophylaxis not recommended unless there is a comorbid disease (inflammatory bowel syndrome, HIV, immunosuppressive medication).
Single-dose therapy of a fluoroquinolone usually effective if symptoms develop.
P.1301
General Considerations
Whenever a person travels from one country to another—particularly if the change involves a marked difference in climate, social conditions, or sanitation standards and facilities—diarrhea is likely to develop within 2–10 days. Bacteria cause 80% of cases of traveler's diarrhea, with enterotoxigenic E coli, Shigella species, and Campylobacter jejuni being the most common pathogens. Less common are Aeromonas, Salmonella, noncholera vibriones, E histolytica, and G lamblia. Contributory causes include unusual food and drink, change in living habits, occasional viral infections (adenoviruses or rotaviruses), and change in bowel flora. Chronic watery diarrhea may be due to amebiasis or giardiasis or, rarely, tropical sprue.
Clinical Findings
A. SYMPTOMS AND SIGNS
There may be up to ten or even more loose stools per day, often accompanied by abdominal cramps and nausea, occasionally by vomiting, and rarely by fever. The stools do not usually contain mucus or blood, and aside from weakness and dehydration, there are no systemic manifestations of infection. The illness usually subsides spontaneously within 1–5 days, although 10% remain symptomatic for 1 week or longer, and symptoms persist for longer than 1 month in 2%.
B. LABORATORY TESTS
In patients with fever and bloody diarrhea, stool culture may be indicated, but in most cases, cultures are reserved for those who do not respond to antibiotics.
Treatment
For most individuals, the affliction is short-lived, and symptomatic therapy with opioids or loperamide is all that is required provided the patient is not systemically ill (fever ≥ 39 C) and does not have dysentery (bloody stools), in which case antimotility agents should be avoided. Packages of oral rehydration salts to treat dehydration are available over the counter in the United States (Infalyte, Pedialyte, others) and in many foreign countries.
Prevention
Avoidance of fresh foods and water sources that are likely to be contaminated is recommended for travelers to developing countries, where infectious diarrheal illnesses are endemic. Prophylaxis is recommended for those with significant underlying disease (inflammatory bowel disease, AIDS, diabetes, heart disease in the elderly, conditions requiring immunosuppressive medications) and for those whose full activity status during the trip is so essential that even short periods of diarrhea would be unacceptable. Prophylaxis is started upon entry into the destination country and is continued for 1 or 2 days after leaving. For stays of more than 3 weeks, prophylaxis is not recommended because of the cost and increased toxicity. For prophylaxis, bismuth subsalicylate is effective but turns the tongue and the stools black and can interfere with doxycycline absorption, which may be needed for malaria prophylaxis; it is rarely used. Numerous antimicrobial regimens for once-daily prophylaxis are effective, such as norfloxacin, 400 mg, ciprofloxacin, 500 mg, ofloxacin, 300 mg, or TMP-SMZ, 160/800 mg. Because not all travelers will have diarrhea and because most episodes are brief and self-limited, an alternative approach currently recommended is to provide the traveler with a supply of antimicrobials to be taken if significant diarrhea occurs during the trip. Loperamide (4 mg loading dose, then 2 mg after each loose stool to a maximum of 16 mg/d) with a single dose of ciprofloxacin (750 mg), levofloxacin (500 mg), ofloxacin (300 mg), or azithromycin (1000 mg) cures most cases of traveler's diarrhea. In pregnant women and in areas with a high prevalence of fluoroquinolone-resistant Campylobacter (such as Thailand), azithromycin is the drug of choice. If diarrhea is severe, associated with fever or bloody stools, or persists despite single-dose ciprofloxacin treatment, then 3–5 days of ciprofloxacin, 500 mg twice daily; levofloxacin, 500 mg once daily; norfloxacin, 400 mg twice daily; ofloxacin, 300 mg twice daily; or azithromycin, 500 mg once daily (for pregnant women) can be given. TMP-SMZ, 160/800 mg twice daily, can be used as an alternative, but resistance is common in many areas. Rifaximin, a nonabsorbable, rifampin-like drug, is also approved for therapy of traveler's diarrhea at a dose of 200 mg three times per day or 400 mg twice a day for 3 days. Because luminal concentrations are high, but tissue level are quite low, it should not be used in situations where there is a high likelihood of invasive disease (eg, fever, systemic toxicity, or bloody stools)
Guerrant RL et al: Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 2001;32:331.
Ramzan N: Traveler's diarrhea. Gastroenterol Clin North Am 2001;30:665.
Rendi-Wagner P et al: Drug prophylaxis for travelers' diarrhea. Clin Infect Dis 2002;34:628.
Thielman NM et al: Clinical Practice. Acute infectious diarrhea. N Engl J Med 2004;350:38.
ACTIVE IMMUNIZATION AGAINST INFECTIOUS DISEASES
RECOMMENDED IMMUNIZATION OF INFANTS, CHILDREN, & ADOLESCENTS
The recommended schedules and dosages of vaccination change often, so the manufacturer's package inserts should always be consulted.
Table 30-3. Acute bacterial diarrheas and “food poisoning.” | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
P.1302
P.1303
P.1304
The schedule for active immunizations in children is presented in Table 30-4 (see also http://www.cdc.gov/nip). All adolescents should see a health care provider to ensure vaccination of those who have not received varicella or hepatitis B vaccine, to make certain that a second dose of measles-mumps-rubella (MMR) has been given as well as a booster for tetanus and diphtheria (Td), and to provide immunizations (influenza and pneumococcal vaccines) that may be indicated for certain high-risk individuals.
RECOMMENDED IMMUNIZATION OF ADULTS
Several vaccines are recommended for adults depending on the individual's previous vaccination status and the risks of exposure to certain diseases. Recommendations are summarized in Table 30-5 (see also http://www.cdc.gov/nip).
Tetanus-Diphtheria Toxoid
All should receive a primary series of immunizations against tetanus and diphtheria once (Table 30-4). Adults who have not previously been immunized should receive two doses of Td 1–2 months apart, followed by a booster dose 6–12 months later. Adults partially immunized in childhood with DTP need only a total of three doses of tetanus and diphtheria toxoid. The historical recommendation has been to give booster doses of Td every 10 years throughout life. An alternative approach emphasizes ensuring that all adults receive primary immunization and recommending a single midlife (age 50 years) booster dose of Td to those who have received the full pediatric immunization, including the booster in the teenage years. If booster doses are given too frequently, an Arthus reaction with severe local pain and swelling can occur. An acellular pertussis vaccine, which is highly immunogenic but associated with far fewer adverse effects than the whole cell vaccine, is now included with tetanus-diphtheria toxoid for use in childhood immunization (DTaP). The acellular vaccine appears to date to be well tolerated in adolescents and adults. Even though adolescents and adults with waning immunity may be reservoirs for Bordetella pertussis—making immunization attractive—routine immunization of this population with the acellular vaccine is not recommended pending further study.
For tetanus prophylaxis in wound management see Chapter 33.
Measles
Adults born before 1957 are considered immune to measles. Adults born in 1957 or later who lack documentation of immunization after age 1 or who do not have a physician-documented history or laboratory evidence of previous infection should receive at least one dose of vaccine. Persons born between 1963 and 1967— a period when inactivated measles vaccine was the only product available—should also receive one dose of live attenuated vaccine. Persons vaccinated before their first birthday should also receive a single dose of vaccine. Because most adults do not have detailed information about childhood immunization or illnesses, a practical approach is to administer a single dose of MMR to all healthy adults born after 1956. Because outbreaks of measles have occurred in young adults who have received a single dose of measles vaccine, revaccination is recommended, particularly before going to college, entering a health care profession, or embarking on foreign travel to areas where measles is endemic. Even though birth before 1957 implies immunity, unvaccinated health care workers (especially women of childbearing age) who do not have a history of measles or laboratory evidence of immunity should be vaccinated. Entrants to colleges and universities and employees of health care institutions who have not previously been vaccinated should receive two doses of vaccine at least 1 month apart. Revaccination of an immune person is not associated with adverse effects—if the vaccination status is unknown and an indication for vaccination exists, it can be safely done. Vaccination of susceptible adults within 72 hours after exposure to an active case of measles is protective.
Fever will develop in about 5–15% of unimmunized individuals, and a mild rash will develop in about 5% 5–12 days after vaccination. Fever and rash are self-limiting, lasting only 2–3 days. Local swelling and induration are particularly common in individuals previously vaccinated with inactivated vaccine. Pregnant women and immunosuppressed persons should not be vaccinated (with the exception of asymptomatic HIV-infected individuals whose CD4 count is > 200/mcL). It is believed that MMR vaccine can be safely given to patients with a history of egg allergy even when severe. A single 0.5 mL dose can be given without prior skin testing or desensitization as long as postvaccination observation for 90 minutes is possible.
Rubella
The purpose of rubella vaccination is to prevent transmission to the fetus. Immunization is recommended for all adults but particularly for women of childbearing age not previously immunized. Although persons born before 1957 are considered immune, this is not an acceptable criterion of immunity for women who could become pregnant. Thus, women of childbearing age, regardless of birth year, should have rubella immunity checked and should be vaccinated if they lack evidence of antibody. They should be counseled not to become pregnant within 4 weeks of immunization. Women who are already pregnant and lack immunity should be vaccinated in the postpartum period. In addition, both male and female hospital workers who may be exposed to patients with rubella or who might have contact with pregnant patients should be immunized. A single immunization is given. MMR trivalent vaccine is recommended, but if immunity to one or more of the components can be demonstrated, monovalent or bivalent vaccines can be used.
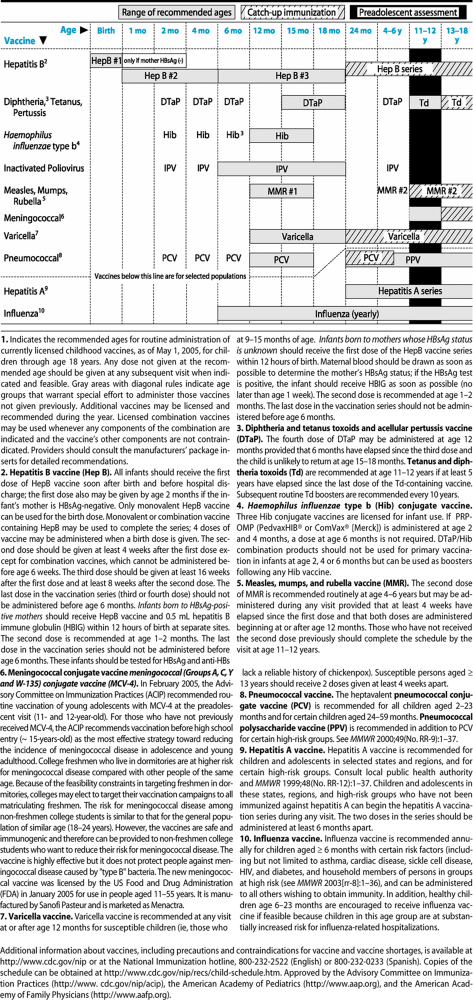 |
Table 30-4. Recommended childhood immunization schedule—United States, 2005.1 |
P.1305
P.1306
Adverse effects are usually mild. Up to 40% of unvaccinated adults (usually women) experience joint pain, often worse than that associated with natural infection. Symptoms begin 1–3 weeks after vaccination and are self-limited, lasting 3–10 days. Frank arthritis is rare. Although vaccination of pregnant women is not recommended, with the currently available RA27/ 3 vaccine strain the congenital rubella syndrome does not occur in the offspring of those inadvertently vaccinated during pregnancy or within 3 months before conception. Persons who are immunosuppressed by virtue of disease or medication should not receive vaccine. HIV infection is an exception—it should be given to asymptomatic individuals who do not have evidence of severe immunosuppression (CD4 count > 200/mcL; severe immunosuppression, CD4 count < 200/mcL) and may be considered in symptomatic patients. Since the vaccine contains trace amounts of neomycin, a history of anaphylaxis to this agent is a contraindication.
Mumps
Mumps vaccine is recommended for all adults thought to be susceptible. Persons born before 1957 are considered to be naturally immune. Those born in 1957 or later are believed to be susceptible unless they can document infection, prove vaccination, or have laboratory evidence of immunity. Vaccination in those already immune is not associated with an increased incidence of adverse effects.
Mumps vaccine is generally safe. It should not be given to those who are immunosuppressed (except HIV-infected individuals) or who have a history of anaphylaxis to neomycin.
Influenza
Influenza vaccination is recommended yearly. Those at greatest risk for severe complications of influenza should have priority in vaccination programs: (1) Adults and children with chronic cardiopulmonary disease, including asthmatics. (2) Residents, health care workers, and employees of chronic care facilities. (3) Healthy adults 50 years of age or older. (4) Adults and children who have required either regular medical follow-up or hospitalization in the last year for chronic metabolic disorders (including diabetes) or renal disease, those with hemoglobinopathies, and those receiving immunosuppressive drugs. (5) Children and teenagers (age 6 months to 18 years) who are on long-term aspirin therapy and would be at increased risk for developing Reye's syn
P.1307
P.1308
P.1309
P.1310
drome following influenza. (6) Women who will become pregnant during the influenza season. (7) Persons who are likely to transmit influenza to persons of high risk as defined above, such as in-home or out-of-home caregivers or household and close contacts of persons at high risk.
Table 30-5. Recommended adult immunization schedule—United States, 2004–2005. |
Certain high-risk groups of patients (the elderly, persons with AIDS, transplant patients) may have a poor antibody response to vaccine, but there is no reason not to vaccinate them. Concern that vaccination of HIVpositive patients may result in a brief (2to 4-week) period of increased HIV viremia and viral replication has been raised. The clinical significance is probably minimal, as progression of disease after vaccination has not been observed. Thus, the potential benefit of vaccination of HIV-positive individuals outweighs any theoretic risks. To prevent disease in high-risk patients, vaccination is advised for household members and health care providers who have contact with these high-risk patients. Vaccination is recommended also for otherwise healthy adults who provide essential community services and for any individual who wishes to decrease the risk of becoming ill with influenza.
Because of the shortage of vaccine in the 2004–2005 season, the Centers for Disease Control and Prevention (CDC) recommended vaccination be restricted to the highest risk groups that included children 6–23 months of age, adults age 65 or older, persons 2–65 with underlying chronic medical conditions, women who will become pregnant during the influenza season, residents of nursing homes and longterm care facilities, children aged 6 months to 18 years on chronic aspirin therapy, health-care workers with direct patient care and caregivers and household contacts of children less than 6 months of age. Individual providers, institutions, and governmental agencies were forced to modify the indications based on supply.
Local reactions (erythema and tenderness) at the site of injection are common, but fevers, chills, and malaise (which last in any case only 2–3 days) are rare. Like measles, mumps, and yellow fever vaccines, influenza vaccine is prepared using embryonated chicken eggs, and persons with a history of anaphylaxis to eggs should not be vaccinated. The risk of Guillain-Barr syndrome is not increased following vaccination. Influenza vaccination may be associated with multiple false-positive serologic tests to HIV, HTLV-1, and hepatitis C, but it is self-limited, lasting 2–5 months.
A trivalent live attenuated influenza vaccine administered as a single-dose intranasal spray is as effective as inactivated vaccine in preventing disease. It is approved for use in otherwise healthy individuals between the ages of 5 and 49 years (the group studied in clinical trials). Because the risk of transmission of the live attenuated vaccine virus to immunocompromised individuals is unknown, it should NOT be used in household members of immunosuppressed individuals, health care workers, or others with close contact with immunosuppressed persons. It is not recommended for those with reactive airway disease; chronic underlying metabolic, pulmonary, or cardiovascular diseases; children or adolescents on long-term aspirin therapy (because of the risk of Reye's syndrome); those with a history of Guillain-Barr syndrome; pregnant women; or those with a history of egg allergy. Two neuraminidase inhibitors (zanamivir and oseltamivir) are used for therapy of influenza A and B, and oseltamivir for prophylaxis. The dose is 75 mg/d, and the duration of treatment depends on the clinical setting. Amantadine and rimantadine are also effective but only against influenza A.
Pneumococcal Pneumonia
Pneumococcal vaccine contains purified polysaccharide from 23 of the most common strains of S pneumoniae, which cause 90% of bacteremic episodes in the United States. Antibody response following vaccination depends on the patient's immune status and the presence of concomitant disease. Healthy adults have an excellent antibody response, as do patients who are postsplenectomy and those with sickle cell disease. Elderly individuals and those with chronic diseases (diabetes mellitus, alcoholic cirrhosis, chronic obstructive pulmonary disease, chronic renal insufficiency, lupus erythematosus, rheumatoid arthritis) have less vigorous response than young healthy adults. Patients with Hodgkin's disease respond to vaccination if it is given before splenectomy, radiation, or chemotherapy, whereas patients with leukemia, lymphoma, and HIV infection respond sluggishly.
Although the efficacy of pneumococcal vaccine has been questioned, most authorities believe that vaccination is about 60–70% effective in preventing bacteremic disease in immunocompetent persons, but less effective at preventing pneumonia. Fifty percent efficacy is observed in patients with underlying diseases (not severely immunocompromised), and less in immunocompromised patients (10%), largely because of inability to mount an antibody response in this population. It is presently recommended for patients at increased risk for developing severe pneumococcal disease, especially asplenic patients and those with sickle cell disease. It is also indicated for adults at increased risk for developing pneumococcal disease, including those with chronic illnesses (eg, cardiopulmonary disease, alcoholism, cirrhosis, chronic renal failure, nephrotic syndrome, cerebrospinal fluid leaks), those who are immunocompromised (eg, patients with Hodgkin's disease, lymphoma, chronic lymphocytic leukemia, multiple myeloma, congenital immunodeficiency, asymptomatic or symptomatic HIV infection, organ or bone marrow transplant recipients), those receiving immunosuppressive therapy (eg, long-term systemic corticosteroids, alkylating agents, and antimetabolites) and Alaskan Natives. Because of the increased risk of developing pneumococcal meningitis following cochlear implants, patients receiving these implants should be given age-appropriate vaccination. Although not currently recommended for smokers and black adults,
P.1311
some feel that these groups should be routinely immunized because of an increased risk of developing invasive disease. In addition, it is recommended for all individuals over 65 years of age. Whether 65 is the appropriate age to vaccinate healthy adults is unclear. Antibody response declines with age, and some have suggested routine immunization at age 50 similar to the recommendation for tetanus (see above). A single dose of vaccine usually confers lifelong immunity. One-time revaccination 5 years after initial vaccination is recommended for those at highest risk (see list above). In addition, a single revaccination is recommended for those 65 or more years of age who received the vaccine 5 years or more previously and were under age 65 at the time of primary vaccination. Elderly individuals with unknown vaccination status should be immunized once. Revaccination should also be considered for high-risk individuals previously immunized with the older 14-valent vaccine. Since immunocompetent patients respond best to the vaccine, it should be given 2 weeks before splenectomy or before starting chemotherapy if that can be anticipated.
A protein-conjugated heptavalent pneumococcal vaccine used in children under 2 years of age is very effective at preventing meningitis and pneumonia but only modestly effective at preventing otitis media. Limited information about use of this vaccine in adults suggests that those with poor antibody response to the 23-valent vaccine (such as renal transplant recipients) also have poor antibody response to the protein-conjugated vaccine despite its higher immunogenicity.
Mild reactions (erythema and tenderness) to pneumococcal vaccine occur in up to 50% of recipients, but systemic reactions are uncommon. Similarly, revaccination at least 5 years after initial vaccination is associated with mild self-limited local but not systemic reactions.
Hepatitis B
Recombinant hepatitis B vaccine is given intramuscularly in the deltoid (gluteal injection often results in deposition of vaccine in fat rather than muscle, with fewer serologic conversions) on three separate occasions: the first two doses 1 month apart and the last dose 5 months after the second one. It is recommended for all individuals at increased risk for developing hepatitis B. These include injection drug users, men who have sex with men, individuals who have had more than one sex partner in the last 6 months, and persons with sexually transmitted diseases or who attend sexually transmitted disease clinics. Family (household and sexual contacts of hepatitis B carriers) or occupational factors (frequent exposure to blood and blood products, hemodialysis patients and staff, residents, medical students, laboratory technicians, morticians) also serve as indications. Others who should be considered for vaccination are those who work at or inhabit institutions for the developmentally disabled, travelers spending more than 6 months in high-risk areas, and inmates of correctional institutions. For immunosuppressed patients, those being maintained on hemodialysis, and chronic alcoholics, seroresponse to standard doses of vaccine is low, and for that reason preparations delivering a higher vaccine dose (40 mcg/mL) are administered. In addition to higher vaccine doses, these patients may require more frequent immunizations, and some authorities recommend annual screening to determine whether booster doses are needed. Although most often used for preexposure prophylaxis, the vaccine is also given as postexposure prophylaxis along with hepatitis B immunoglobulin following needlestick injury or mucous membrane exposure to blood from an individual who is HBsAg-positive. It is also given along with hepatitis B immunoglobulin to infants of mothers who are HBsAg-positive (Table 30-4). Immunity wanes with time, but periodic serologic monitoring is not recommended, and routine administration of booster doses is not necessary. Adverse reactions are minor and limited to local soreness.
Following vaccination, 90–95% of healthy young individuals develop protective antibodies. A number of factors decrease serologic response, including increasing age over 30, renal failure, HIV infection, diabetes, chronic liver disease, obesity, and smoking. Postvaccination serologic testing is not routinely performed. It is reserved for those whose clinical management would be influenced by their immune status (eg, health care workers, infants born to HBsAg-positive mothers, dialysis patients), and those who may have an impaired response. Those who do not respond should receive a second three-dose vaccine series with serologic testing 1–2 months after completion. Those who do not respond are unlikely to respond to further vaccination even with a different recombinant vaccine and should be considered susceptible; if exposed, they should receive hepatitis B immune globulin.
Varicella
A live attenuated varicella virus vaccine is currently recommended as part of routine childhood immunization (Table 30-4). Although only 10% of adults remain susceptible, varicella in adolescents and adults is a more serious disease. Only about 2% of all cases of varicella occur in adults, but almost 50% of all deaths are in adults. Thus, susceptible adolescents and adults should be immunized, with special emphasis on certain highrisk groups, ie, health care workers; household contacts of immunosuppressed individuals; persons who live or work in environments where transmission can occur, eg, teachers in day care centers or elementary schools, residents and workers in institutional settings such as military and correctional institutions, college students; nonpregnant women of childbearing age; and international travelers. The role of the present vaccine in postexposure prophylaxis has not been widely studied, but it has been suggested that it is 90% effective in preventing varicella in an outbreak, particularly when given within 3–5 days after exposure. The Advisory Commit
P.1312
tee on Immunization Practices (ACIP) recommends vaccination in susceptible persons following exposure. The vaccine is very immunogenic. Seroconversion occurs in 95% of children after a single dose. In adolescents (older than 12 years of age) and adults, seroconversion is seen in 78% after one dose and 99% after two doses. For this reason, two doses given 4–8 weeks apart are recommended in persons 12 years of age and older. The duration of immunity is not known but is probably 10 years. Although the vaccine is very effective in preventing disease, breakthrough infections do occur—but are much milder than in unvaccinated individuals (usually less than 50 lesions, with milder systemic symptoms). Although the vaccine is very safe, adverse reactions can occur as late as 4–6 weeks after vaccination. Tenderness and erythema at the injection site are seen in 25%, fever in 10–15%, and a localized maculopapular or vesicular rash in 5%; a smaller percentage develop a diffuse rash, usually with five or fewer vesicular lesions. Spread of virus from vaccinees to susceptible individuals is possible, but the risk of such transmission even to immunocompromised patients is small and disease, when it develops, is mild and treatable with acyclovir. Nonetheless, the vaccine, being a live attenuated virus, should not be given to immunocompromised individuals, including HIV-positive children and adults, or pregnant women. It is contraindicated in persons allergic to neomycin. For theoretic reasons, it is recommended that following vaccination salicylates should be avoided for 6 weeks (to prevent Reye's syndrome). Several unresolved issues remain, including the need for booster doses, whether universal childhood vaccination will shift the incidence of disease to adolescence or adulthood with the possibility of more severe disease, and whether vaccination might prevent development of herpes zoster.
Hepatitis A
Two inactivated hepatitis A vaccines (Havrix, VAQTA) are approved for use in the United States. They are indicated for individuals 2 years of age or older who are at an increased risk for developing hepatitis A. Potential vaccinees include travelers (including military personnel) to areas where hepatitis is endemic (Africa, Asia, Central and South America, Mexico, parts of the Caribbean); certain populations that experience outbreaks (such as indigenous Alaskans, certain American Indian reservations, various religious communities and states where the risk of hepatitis A is high among children); employees of day care centers, caretakers for developmentally impaired institutionalized individuals, and laboratory workers who handle live hepatitis A virus or work closely with nonhuman primates; men who have sex with men; illicit drug users; persons who receive clotting factor concentrates; and those with chronic liver disease. The role of hepatitis A vaccine in controlling outbreaks in day care centers, hospitals, and institutions for the disabled has not been investigated, and immune globulin is used in those settings. A single intramuscular injection of vaccine in adults elicits antibodies in 55–60% of individuals at 2 weeks and 95% by 1 month, although rates of seroconversion may be lower in immunocompromised individuals. The different formulations come in different strengths, and dosage depends on the age of the vaccinee and the preparation used (see package insert). In general, two doses are required, the second 6–18 months after the first. The duration of immunity may be lifelong, and at present repeat vaccination is not recommended. Adverse effects are minimal and consist mainly of pain at the injection site. If vaccine is not available, temporary passive immunity may be induced by the intramuscular injection of immune globulin, 0.02 mL/kg every 2–3 months or 0.1 mL/kg every 6 months. Protection with immune globulin is recommended for persons traveling to areas where sanitation is poor and the risk of exposure to hepatitis A high because of contaminated food and water supplies and contact with infected persons. Preparation of immunoglobulin from plasma involves steps that inactivate HIV, thus making it incapable of transmitting HIV infection.
Combined Hepatitis A & B Vaccine
A combined hepatitis A and B vaccine is approved for use in individuals 18 years of age and older. The components are identical to individual vaccines. It is highly immunogenic and should be used in individuals who have an indication for both hepatitis A and B vaccination, as noted above. The product is safe, and adverse effects are similar to those of the individual components. It is administered in three doses at 0, 1 and 6 months.
Smallpox
Smallpox vaccination, discontinued in the United States in the early 1970s, has been reinstituted because of concerns about bioterrorism. The vaccine is a live vaccinia virus derived through serial passage of cowpox and does not contain the actual smallpox virus. Vaccine is administered with a bifurcated needle, making 15 puncture wounds in a small area of the skin (5 mm) just deep enough to cause bleeding. Because the inoculation site is contagious, it should be covered with gauze or a semipermeable dressing such as OpSite. If vaccination is successful, the site goes through a characteristic evolution: In 3–4 days the site becomes red, itchy, and indurated; a vesicle umbilicates and evolves into a well-formed pustule by day 6–11; the pustule scabs over between week 2 and week 3; and by the end of the third week the scab falls off, leaving a scar. At the end of the first week, fever for several days, tenderness at the vaccination site, and localized axillary adenopathy occur in 10–20% of first-time vaccinees, but these reactions are less common in those who have been previously vaccinated within the last 10 years. Successful vaccination is indicated by the presence of a
P.1313
pustular lesion at day 7 in a nonimmune individual and by the presence of a pustule or area of induration in a previously vaccinated person. Failure to see these reactions is an indication for revaccination.
In general, adverse effects are more common in children under 5 years of age and in first-time vaccinees. Other than the local reactions, the most common adverse effect (estimated at 1:2000) is autoinoculation to another site, most commonly the face, eyelid, mouth, and genitalia. These lesions usually are selflimited and heal without specific therapy. Generalized vaccinia occurs in 1:5000 vaccinees and is characterized by widespread lesions appearing 6–9 days after vaccination, the result of hematogenous spread. The lesions usually heal without therapy in immunocompetent individuals but can be life-threatening in the immunosuppressed. Eczema vaccinatum occurs in patients with active or healed eczema and can progress to involve all areas of the skin involved with the skin disorder. Although uncommon (1:25,000), this is a potentially fatal complication. Progressive vaccinia or vaccinia necrosum is seen in immunocompromised individuals. The vaccination site fails to heal and the virus spreads to surrounding areas with progressive necrosis and gangrene, a serious complication with a high mortality. Postvaccination encephalitis occurs 1–2 weeks after vaccination, is usually seen in those under 1 year of age, occurs in 1:300,000 vaccinations, and is associated with death in 25% and severe disability in another 25%. Following mass vaccination of military personnel, two additional adverse events have been described—local and generalized folliculitis and myopericarditis. Folliculitis occurred 8–10 days following vaccination, was concentrated in hair-bearing areas (face, extremities, back), resolved spontaneously in 3–5 days, and was not associated with scarring. Myopericarditis was seen in first-time vaccine recipients, occurred 7–19 days after vaccination, and was selflimited. In brief follow-up, permanent sequelae have not been described.
Vaccinia immune globulin is available from the CDC but is in limited supply. It is recommended for severe adverse reactions such as eczema vaccinatum, progressive vaccinia, severe generalized vaccinia, and inadvertent inoculation of the eye or eyelid without vaccinia keratitis. It is not recommended for postvaccination encephalitis. Cidofovir, a nucleotide analog used to treat CMV infections, has activity against variola virus and has been effective in animal models for the therapy of vaccinia infections. It should be considered for those with serious adverse effects.
Routine vaccination—in the absence of a case of smallpox—is not recommended for those under 18 years of age. It is also not recommended for those with a history of or active eczema or household associates of such individuals. Those with other skin diseases (atopic dermatitis, impetigo) may also be at risk for complications and should not be vaccinated until skin lesions have healed. Pregnancy, altered immune states as described above, and allergy to vaccine components (neomycin, streptomycin, polymyxin, chlortetracycline) are contraindications to smallpox vaccination. Household contacts of individuals with altered immunity should also not be vaccinated.
RECOMMENDED IMMUNIZATIONS FOR TRAVELERS
Individuals traveling to other countries frequently require immunizations in addition to those listed above and may benefit from chemoprophylaxis against various diseases. These are listed in Health Information for International Travel, published by the CDC. An updated version is published yearly and is available from the Superintendent of Documents, United States Government Printing Office, Washington, DC 20402, or on the Internet: http://www.cdc.gov/nip/home.html.
Various vaccines can be given simultaneously at different sites. Some, such as cholera, plague, and typhoid vaccine, cause significant discomfort and are best given at different times. In general, live attenuated vaccines (measles, mumps, rubella, yellow fever, and oral typhoid vaccine) should not be given to immunosuppressed individuals or household members of immunosuppressed people or to pregnant women. Immunoglobulin should not be given for 3 months before or at least 2 weeks after live virus vaccines, because it may attenuate the antibody response.
Chemoprophylaxis of malaria is discussed in Chapter 35.
Cholera
Because cholera among travelers is rare and the vaccine marginally effective, the World Health Organization (WHO) does not require immunization for persons traveling to endemic areas. Although no country officially requires it, some local authorities may require documentation of vaccination.
Cholera vaccine contains a suspension of killed vibriones of prevalent antigenic types. Two injections are given intramuscularly 2–6 weeks apart, followed by booster injections every 6 months during periods of possible exposure. Protection depends largely on booster doses. A more effective inactivated oral vaccine is not available in the United States. A live attenuated oral vaccine is being investigated. The WHO certificate is valid for 6 months only.
Hepatitis B
Persons traveling to and spending more than 6 months in endemic areas of hepatitis B virus infection who will have close contact with the local population should be considered for vaccination. Short-term travelers to areas of moderate or high endemic infection (Southeast Asia, China, most of the Middle East, Haiti, the Dominican Republic, and most of Africa) who will be in contact with potentially infected body secretions of residents should be vaccinated. Vaccina
P.1314
tion should begin at least 6 months before travel to allow for completion of the series.
Hepatitis A
As indicated above, susceptible individuals traveling to areas of high or intermediate endemicity for hepatitis A (eg, anywhere except Canada, western Europe, Japan, Australia, and New Zealand) should be vaccinated. The vaccine is given at least 4 weeks prior to travel, as protective antibodies develop in 95% of vaccinees by that time. If given 2 weeks before travel, up to 45% will not have protective antibodies, and if the person is traveling to a high-risk area, intramuscular immune globulin (0.02 mL/kg) should be administered at a separate site.
Meningococcal Meningitis
If travel is contemplated to an area where meningococcal meningitis is epidemic (Nepal, sub-Saharan Africa, the “meningitis belt” from Senegal in the west to Ethiopia in the east, northern India) or highly endemic, polysaccharide vaccines from types A, C, W135, and Y may be indicated. (Saudi Arabia requires immunization for pilgrims to Mecca.) Although the need for revaccination has not been determined, antibody levels decline over 2–3 years, and revaccination is reasonable in 3–5 years if risk continues.
Plague
Plague vaccine is a suspension of killed plague bacilli given intramuscularly. Three injections are given—the second, 4 weeks after the first; the third, 5 months after the second. The risk of acquiring plague is so low that vaccination is reserved for travelers who will have exposure to rodents or rabbits in rural areas where plague is endemic (parts of South America, Southeast Asia, the southwestern states of the United States). For continuing exposures, booster doses at intervals of 1–2 years are recommended.
Poliomyelitis
Adult travelers to tropical or developing countries who have not previously been immunized against poliomyelitis should receive a primary series of three doses of inactivated enhanced-potency poliovaccine (IPV), as follows: two doses of 0.5 mL subcutaneously 4–8 weeks apart and then a third dose 6–12 months after the second dose. If more than 8 weeks will elapse before travel, three doses of IPV can be given 4 weeks apart. If 4–8 weeks will elapse before travel, two doses are given 4 weeks apart, and if less than 4 weeks will elapse, a single dose is given. Vaccination can be completed upon return if continued or future exposure to polio is anticipated. Travelers who have previously been fully immunized with OPV or IPV should receive a one-time booster dose with IPV. Data do not indicate the need for more than one adult booster. Live attenuated poliovaccine is no longer recommended because of the risk of vaccine-associated disease.
Rabies
For travelers to areas where rabies is common in domestic animals (eg, India, Asia, Mexico), preexposure prophylaxis with human diploid cell vaccine (HDCV), rabies vaccine adsorbed (RVA), or purified chick embryo cell culture (PCEC) vaccine should be considered. It usually consists of two intramuscular (deltoid area) injections of 1 mL given 1 week apart with a booster dose 2–3 weeks later. Alternatively, two intradermal injections of 0.1 mL of HDCV are given 1 week apart, with a booster dose given 2–3 weeks later. Chloroquine can blunt the immunologic response to rabies vaccine. If malaria prophylaxis with chloroquine is required, vaccination should be given intramuscularly (not intradermally) to ensure adequate antibody response. Until further studies are done, interaction between mefloquine and rabies vaccine, while not established, makes intramuscular administration prudent if mefloquine is to be given.
Typhoid
Typhoid vaccination is recommended for travelers to developing countries (especially Latin America, Africa, and Asia) who will have prolonged exposure to contaminated food and water. Three preparations of approximately equal efficacy (50–75% effective) are available: (1) a heat-phenol-inactivated vaccine for parenteral use, (2) an oral live-attenuated Ty21a vaccine supplied as enteric-coated capsules, and (3) a Vi capsular polysaccharide (Vi CPS) vaccine for parenteral use. The phenol-inactivated preparation that has been historically used is associated with more side effects and is not recommended unless the other preparations are not available. The Ty21a vaccine is given as one capsule every other day for four doses. The capsules must be refrigerated and taken with cool liquids (37 C or less) at least 1 hour before meals. All four doses must be taken for maximum protection. Adverse effects are minimal and consist primarily of gastrointestinal upset. The Vi CPS vaccine is given as a single intramuscular injection. Adverse effects consist mainly of local irritation at the site of injection, but fever and headache occur. If continued or repeated exposures are anticipated, boosters are recommended. A dose of the heat-inactivated vaccine is recommended every 3 years, the Vi CPS every 2 years. The optimal booster dose of the Ty21a is not known, but the manufacturer recommends repeating the fourdose series every 5 years. The live attenuated vaccine should not be used in immunosuppressed patients, including those with HIV infection.
Yellow Fever
The live attenuated yellow fever virus vaccine is administered once subcutaneously. Although the risk of
P.1315
yellow fever is low for most travelers, a number of countries require vaccination for all visitors and others require it for travelers to or from endemic areas (mainly equatorial Africa and parts of South and Central America). The WHO certificate requires registration of the manufacturer and the batch number of the vaccine. Vaccination is available in the United States only at approved centers; the local health department should be contacted for available resources. Reimmunization is recommended at 10-year intervals if continued risk exists.
Because it is a live attenuated vaccine prepared in embryonated eggs, the yellow fever vaccine should not be given to immunosuppressed individuals or those with a history of anaphylaxis to eggs. Pregnancy is a relative contraindication to vaccination.
Since 2001, seven cases of fever, jaundice, and multiple organ system failure following yellow fever vaccination were reported (yellow fever vaccine–associated viscerotropic disease). As well, there have been nine cases of encephalitis (yellow fever vaccine–associated neurotropic disease). These reactions may have been the result of an aberrant host response to the vaccine rather than direct invasion of the vaccine virus. Because yellow fever is a severe disease and deaths have been reported in travelers, and these serious adverse reactions are rare (3–5 cases of viscerotropic disease and 4–6 cases of neurotropic disease per 1,000,000 doses of vaccine distributed), vaccination is still recommended but limited to those traveling to areas reporting epidemic or endemic yellow fever. (Current information about the vaccine and yellow fever activity can be found at http://www.cdc.gov/travel/yfever.htm.)
Japanese B Encephalitis
Japanese B encephalitis is a mosquito-borne viral encephalitis that affects primarily children and older adults (65 years and older) and usually occurs from May to September. It is the leading cause of encephalitis in Asia. Because the risk of infection is low and because adverse effects of the vaccine can be serious, not all travelers to Asia should be vaccinated. Vaccine should be given to travelers to endemic areas who will be staying at least 30 days and who are traveling during the transmission season, particularly if they are visiting rural areas. Travelers who spend less than 30 days in the region should be considered for vaccination if they intend to visit areas of epidemic transmission or if extensive outdoor activities are planned in rural rice-growing areas. The recommended primary immunization schedule is 1 mL of vaccine administered subcutaneously on days 0, 7, and 30. If time constraints are compelling, the last dose can be given on day 14. The last dose should be given at least 10 days before embarkation because urticaria and angioedema have been described, occurring from minutes up to 10 days after vaccination. Following vaccination, patients should be observed for 30 minutes and advised of the possibility of delayed reactions of angioedema and urticaria. In addition, local reactions have been reported in 20% of vaccinees and systemic reactions (fever, chills, malaise, headache) in 10%.
Craig AS et al: Prevention of hepatitis A with hepatitis A vaccine. N Engl J Med 2004;350:476.
Poland GA et al: Clinical practice: prevention of hepatitis B with the hepatitis B vaccine. N Engl J Med 2004;351:2832.
Vaccine recommendations—challenges and controversies. Infect Dis Clin North Am 2001;15(1).
Vaccinia (Smallpox) Vaccine. Recommendations of the advisory committee on immunization practices (ACIP) 2001. MMWR Recomm Rep 2001;50(RR-10):1.
Virk A: Medical advice for international travelers. Mayo Clinic Proc 2001;76:831.
HYPERSENSITIVITY TESTS & DESENSITIZATION
One should test for hypersensitivity before injecting antitoxin, materials derived from animal sources, or drugs (eg, penicillin) to which a patient has had a severe reaction in the past. If the test described below is negative, desensitization is not necessary, and a full dose of the material may be given. If the test is positive, alternative drugs should be strongly considered. If that is not feasible, desensitization is necessary.
Intradermal Test for Hypersensitivity
Penicillin is the drug that most frequently serves as an indication for sensitivity testing and desensitization. A clinical history of penicillin allergy has a positive predictive value of only 15%. In determining whether allergy testing should be performed, its nature should be determined. Immunoglobulin G-mediated delayed reactions such as erythematous or maculopapular skin rash or serum sickness should be distinguished from immediate-type immunoglobulin E-mediated reactions such as urticaria, angioedema, and anaphylaxis. Only patients with the latter history who require penicillin or a cephalosporin should undergo hypersensitivity testing. Skin testing requires two preparations: PPL (penicilloyl-polylysine) and a minor determinant mixture. Several points should be emphasized in performing and interpreting these tests. Whenever possible, both PPL and a minor determinant should be used, since 85% of skin test reactors are positive to PPL but 15% react only to the minor determinant mixture. In addition, if penicillin G is used instead of the minor determinant mixture, some allergic patients will be missed. About 25% of individuals who react to minor determinant mixture may not react to penicillin G, and such patients may still have an anaphylactic or accelerated reaction to penicillin. A pinprick test is performed with each solution at different sites by placing a small drop of solution on the skin and making small indentations of the skin with a needle. If there is no reaction within 10 minutes, 0.01–0.02 mL is injected intradermally, raising a small bleb. Development of a wheal greater than 5 mm in diameter is considered a
P.1316
positive test and an indication for desensitization. Even if the test is negative, about 1–2% of patients will have an immediate or accelerated reaction, but an anaphylactic reaction is rare. Thus, if the test is negative, the drug can be administered with relative safety, but the first dose should be medically supervised and the patient observed for 1 hour (serious reactions after 1 hour are rare).
Patients with a history of allergy to penicillin are also at an increased risk for having a reaction to cephalosporins. A common approach to these patients is to assess the severity of the reaction. If an IgE-mediated reaction can be excluded by history, a cephalosporin can be administered. When the history justifies concern about an immediate-type reaction, penicillin skin testing should be performed. If the test is negative, a cephalosporin can be given. If the test is positive, cephalosporin desensitization should be performed.
Desensitization
A. PRECAUTIONS
The desensitization procedure is not innocuous— deaths from anaphylaxis have been reported. If extreme hypersensitivity is suspected, it is advisable to use an alternative structurally unrelated drug and to reserve desensitization for situations when treatment cannot be withheld and no alternative drug is available.
An antihistaminic drug (25–50 mg of hydroxyzine or diphenhydramine intramuscularly or orally) should be administered before desensitization is begun in order to lessen any reaction that occurs.
Desensitization should be conducted in an intensive care unit where cardiac monitoring and emergency endotracheal intubation can be performed.
Epinephrine, 1 mL of 1:1000 solution, must be ready for immediate administration.
B. DESENSITIZATION METHOD
Several methods of desensitization have been described for penicillin, including use of both oral and intravenous preparations. All methods start with very small doses of drug and gradually increase the dose until therapeutic doses are achieved. For penicillin, 1 unit of drug is given intravenously and the patient observed for 15–30 minutes. If there is no reaction, some recommend doubling the dose while others recommend increasing it tenfold every 15–30 minutes until a dosage of 2 million units is reached; then give the remainder of the desired dose.
For recommendations on skin testing and desensitization for other preparations (botulism antitoxin, diphtheria antitoxin, etc), one should consult the manufacturer's package inserts.
Treatment of Reactions
A. MILD REACTIONS
If a mild reaction occurs, drop back to the next lower dose and continue with desensitization. If a severe reaction occurs, administer epinephrine (see below) and discontinue the drug unless treatment is urgently needed. If desensitization is imperative, continue slowly, increasing the dosage of the drug more gradually.
B. SEVERE REACTIONS
If bronchospasm occurs, epinephrine, 0.3–0.5 mL of 1:1000 dilution, should be given subcutaneously every 10–20 minutes. The following can also be given if symptoms persist: inhaled metaproterenol (0.3 mL of a 5% solution in 2.5 mL of saline), intravenous aminophylline (0.3–0.9 mL/kg/h maintenance after a 6 mg/kg loading dose over 30 minutes), or corticosteroids (250 mg of hydrocortisone or 50 mg of methylprednisolone intravenously every 6 hours for two to four doses). Hypotension should be treated with intravenous fluids (saline or colloid), epinephrine (1 mL of 1:1000 dilution in 500 mL of D5W intravenously at a rate of 0.5–5 mcg/min), and antihistamines (25–50 mg of hydroxyzine or diphenhydramine intramuscularly or orally every 6–8 hours as needed). Cutaneous reactions, manifested as urticaria or angioedema, respond to epinephrine subcutaneously and antihistamines in the doses set forth above.
Arroliga ME et al: Penicillin allergy: consider trying penicillin again. Cleve Clin J Med 2003;70:313.
Kelkar PS et al: Cephalosporin allergy. N Engl J Med 2001; 345:804.
Robinson JL et al: Practical aspects of choosing an antibiotic for patients with a reported allergy to an antibiotic. Clin Infect Dis 2002;35:26.
Salkind AR et al: The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA 2001;288:2998.
Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR-6):1
Footnote
*Reportable to public health authorities.
EAN: 2147483647
Pages: 71