15 - Hypertension
Editors: Schrier, Robert W.
Title: Manual of Nephrology, 6th Edition
Copyright 2005 Lippincott Williams & Wilkins
> Table of Contents > 15 - The Patient with Hypertension
function show_scrollbar() {}
15
The Patient with Hypertension
Charles R. Nolan
Definition and classification of hypertension. The definition of hypertension is somewhat arbitrary, because blood pressure (BP) is not distributed bimodally in the population. Instead, the distribution of BP readings in the population is unimodal, and an arbitrary level of BP must be defined as the threshold above which hypertension can be diagnosed. The correlation between the levels of systolic BP and diastolic BP and cardiovascular risk has long been recognized. It has become clear that in patients over age 50, systolic BP of more than 140 mm Hg is a much more important cardiovascular risk disease risk factor than is diastolic BP. Increasing BP clearly has an adverse effect on mortality over the entire range of recorded pressures, even those generally considered to be in the normal range. Lifespan and health are progressively reduced as BP rises. The goal of identifying and treating high BP is to reduce the risk of cardiovascular disease and associated morbidity and mortality. In this regard, classifying hypertension in adults is useful in identifying high-risk individuals and providing guidelines for follow-up and treatment of hypertension. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) has established criteria for the diagnosis and classification of BP in adult patients (Table 15-1). The optimal BP in an individual who is not acutely ill is lower than 120/80 mm Hg. Individuals with a systolic BP of 120 to 139 mm Hg or a diastolic BP of 80 to 89 mm Hg should be considered as prehypertensive; these patients require health-promoting lifestyle modifications to prevent cardiovascular disease. Patients with prehypertension are at twice the risk of developing hypertension as those with lower values. Although normotensive by definition, these prehypertensive patients should be rechecked annually to exclude the development of hypertension. Hypertension is arbitrarily defined as a systolic BP of 140 mm Hg or greater or a diastolic BP of 90 mm Hg or greater, or by virtue of the patient taking antihypertensive medications. The stage of hypertension (stage 1 or 2) is determined by the levels of both systolic BP and diastolic BP (Table 15-1). This classification should be based on the average of two or more blood pressure readings at each of two or more visits after the initial BP screening. When systolic BP and diastolic BP fall into different categories, the higher category should be selected to classify the individual's BP.
Table 15-1. Classification of Blood Pressure for Adultsa
BP classificationb Systolic BP (mm Hg)c Diastolic BP (mm Hg)c Normal < 120 and < 80 Prehypertension 120 139 or 80 89 Stage 1 hypertension 140 159 or 90 99 Stage 2 hypertension 160 or 100 aAdults aged 18 years and older. bClassification should be based on the mean of two or more properly measured seated blood pressure readings obtained on each of two or more office visits. cWhen systolic and diastolic BP fall into different categories, classify based on the higher category. (Adapted with permission from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.) Epidemiology of hypertension. The prevalence of hypertension ranges from 20% to 30% of the entire adult population of the United States. Hypertension affects approximately 50 million individuals in the United States and approximately 1 billion individuals worldwide. The prevalence increases with advancing age, so that approximately one-third of patients in their fifth decade meet the criteria for hypertension. Data from the Framingham Heart Study indicate that even individuals who are normotensive at 55 years of age have a 90% lifetime risk for developing hypertension. As the mean age in the general population increases, the prevalence of hypetension will no doubt increase further unless effective preventative measures are implemented. Many hypertensive patients have a positive family history of parental hypertension. The mode of inheritance is complex and probably polygenic in most instances. Black men and women have a twofold higher prevalence of hypertension (30%) than white men and women (15%) in a sampling of almost 18,000 American
P.243
adults aged 48 to 75 years in the National Health and Nutrition Examination Survey (NHANES). Prevalence appears to be equal in men and women in most surveys. Obese individuals have significantly more hypertension than nonobese individuals. In childhood, obesity is a major cause of hypertension. Proof of the significant relationship between body weight and blood pressure is found in the observation that BP falls with weight reduction. The intake of dietary salt (sodium chloride) has significant effects on BP, especially in patients with other factors predisposing to the development of hypertension, such as advancing age, obesity, adult onset diabetes, positive family history of hypertension, black race, or underlying renal disease. Numerous epidemiologic studies have shown that the dietary intake of salt correlates with the average BP in a population. Northern Japanese fisherman who ingest 450 mEq of sodium daily have a 40% prevalence of hypertension. In contrast, indigeneous Alaskan populations and the Yanomamo Indians in Brazil and Venezuela, who have dietary intakes of 1 mEq of sodium daily, do not develop hypertension at any age. Intersalt, an international epidemiologic study, examined the relation between dietary sodium intake (based on 24-hour urinary sodium excretion) and BP in more than 10,000 individuals aged 20 to 59 years from 52 countries around the world. The results demonstrate a significant correlation between median systolic BP and diastolic BP and dietary sodium intake. These observations can be explained based on the role of abnormal renal sodium handling in the pathogenesis of hypertension, which is discussed in section IV. The therapeutic implications of these observations include dietary sodium restriction as part of nonpharmacologic therapy and the recommendation of thiazide diuretics as first-line drug therapy for the treatment of hypertension in most patients. Despite the known cardiovascular risks of untreated hypertension and the widespread availability of effective pharmacologic treatment, the identification and effective control of hypertension remains a significant public health problem in the United States. From the 1976 1980 NHANES survey (NHANES II) to the 1991 1994 survey (NHANES III, phase 2), the percentage of hypertensive Americans who are aware that they have high BP increased from 51% to 68%. Among persons with hypertension, the prevalence of treatment increased from 31% to 54% during the same period. The number of persons with high BP controlled to below 140/90 mm Hg increased from 10% in NHANES II to 27% in NHANES III. Alarmingly, data computed for 1999 2000 reveal that more than 65% of patients with hypertension still have inadequate control of their BP. The continued high prevalence of hypertension and hypertension-related complications such as stroke, cardiovascular complications, heart failure, and end-stage renal disease (ESRD) represent a major public health challenge.Cardiovascular disease risk. The relationship of blood pressure to cardiovascular risk is continuous and independent of other cardiovascular risk factors.
P.244
Beginning at 115/75 mm Hg and across the entire BP range, each increment of 20/10 mm Hg doubles the risk of cardiovascular disease. The overall risk of cardiovascular morbidity and mortality in patients with hypertension is determined not only by the stage of hypertension, but also by the presence of other risk factors, such as smoking, hyperlipidemia, and diabetes, and by the existence of target-organ damage (Table 15-2). The major target organs affected by hypertension are the heart, peripheral vasculature, central nervous system, the kidney, and the eye. Most of the consequences of hypertension are the result of progressive vascular injury. Hypertension accelerates atherosclerotic vascular disease and aggravates the deleterious effects of diabetes, smoking, and hyperlipidemia on the aorta and its major branches. Atherosclerotic disease results in significant morbidity from myocardial infarction (MI), atherothrombotic cerebral infarction, peripheral vascular disease with claudication, and renal disease due to ischemia or cholesterol embolization. Hypertensive renal disease may result from hypertension-induced vasculitis in the setting of malignant hypertension or more insidious renal injury from long-standing essential hypertension with hypertensive nephrosclerosis. Hypertension is also an important cofactor in the progression of other renal diseases, especially diabetic nephropathy. Hypertension may also cause cerebrovascular disease in the form of lacunar infarction or intracerebral hemorrhage. Left ventricular hypertrophy (LVH) and congestive heart failure (CHF), often due to isolated diastolic dysfunction, are the result of the heightened peripheral vascular resistance (afterload) imposed by systemic hypertension. In clinical trials, antihypertensive therapy has been associated with significant reductions in the incidence of stroke (35% to 40%), MI (20% to 25%), and heart failure (50%). It has been estimated that in patients with stage 1 hypertension (systolic BPP.245
140 to 159 mm Hg and/or diastolic BP 90 to 99 mm Hg) and additional cardiovascular risk factors, achieving a sustained 12 mm Hg reduction in systolic BP for 10 years will prevent 1 death for every 11 patients treated. In the setting of pre-existing cardiovascular disease or target-organ damage, treatment of 9 patients would prevent 1 death.Table 15-2. Cardiovascular Risk Factors and Target-Organ Damage
Major Risk Factors Hypertensiona Cigarette smoking Obesity (BMI)b > 30)a Physical inactivity Dyslipidemiaa Diabetes mellitusa Microalbuminuria or estimated GFRc < 60 mL/min Age (> 55 years for men, > 65 years for women) Family history of premature cardiovascular disease (men < 55 years or women < 65 years) Target-Organ Damage Heart Left ventricular hypertrophy Angina or prior myocardial infarction Prior coronary revascularization Heart failure Brain Prior stroke or transient ischemic attack Chronic kidney disease Peripheral arterial disease Retinopathy (see Table 14-8) aComponents of the metabolic syndrome associated with insulin resistance and hyperinsulinemia. bBMI indicates body mass index calculated as weight in kilograms divided by the square of height in meters. cGFR indicates glomerular filtration rate. (Adapted with permission from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.) Pathogenesis of hypertension. Experiments with isolated, perfused kidneys demonstrate that the magnitude of urinary sodium excretion is a direct function of the renal arterial perfusion pressure. The level of perfusion pressure may alter sodium excretion by changing the peritubular hydrostatic pressure. Thus, an increase in perfusion pressure should increase peritubular hydrostatic pressure with a resultant decrease in sodium reabsorption. Micropuncture studies in the rat have shown an inverse relationship between renal perfusion pressure and proximal sodium reabsorption. It has been argued that if this pressure natriuresis mechanism was operating in a normal fashion, in the presence of hypertension, profound volume depletion would result. The fact that this does not occur suggests that in every hypertensive state, a shift in the pressure natriuresis curve must occur so that a higher perfusion pressure is required to achieve any given level of natriuresis. In this regard, Guyton and colleagues have postulated that this shift in the pressure natriuresis curve is the fundamental underlying pathophysiologic abnormality that leads to essential hypertension and virtually all secondary forms of hypertension (Fig. 15-1). If a primary renal defect in natriuresis does exist in hypertension, then, to avert disaster due to persistent positive sodium balance with inexorable fluid accumulation, compensatory mechanisms must be invoked that restore sodium balance. These compensatory processes restore sodium balance and normal extracellular fluid (ECF) volume but, in the process, cause systemic hypertension.
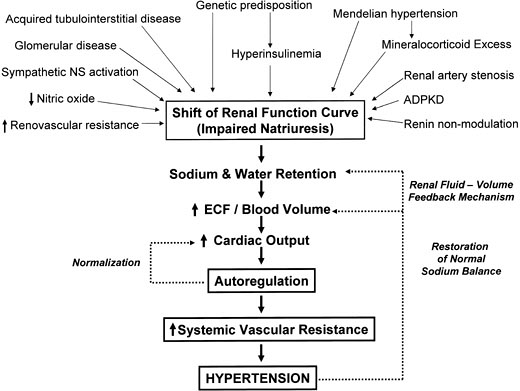
Figure 15-1. Abnormal renal sodium handling in the pathogenesis of hypertension (Guyton's hypothesis). In the setting of essential hypertension, primary renal disease, mineralocorticoid excess, or insulin resistance with hyperinsulinemia, a defect in the intrinsic natriuretic capacity of the kidney is present that prevents sodium balance from being maintained at a normal level of BP. Initially, this impairment in natriuresis leads to increases in extracellular fluid (ECF) volume and cardiac output. This hemodynamic state is short lived, however. Circulatory autoregulation occurs to maintain normal perfusion of the tissues, resulting in an increase in the systemic vascular resistance (SVR). The increase in SVR leads to systemic hypertension. With pressure-induced natriuresis, the renal fluid volume feedback mechanism returns sodium balance, ECF volume, and cardiac output to normal. Systemic hypertension can be conceptualized as an essentially protective mechanism that prevents life-threatening fluid overload in the setting of reduced renal natriuretic capacity. Normal salt balance and fluid volume are maintained, but at the expense of systemic hypertension. (AII, angiotensin II.) (Adapted with permission from Nolan CR, Schrier RW. The kidney in hypertension. In: Schrier RW, ed. Renal and electrolyte disorders, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2003.)
Guyton's hypothesis states that the most important and fundamental mechanism in determining the long-term control of BP is the renal fluid-volume feedback mechanism. In simple terms, through this basic mechanism, the kidneys regulate arterial pressure by altering renal excretion of sodium and water, thereby controlling circulatory volume and cardiac output. Changes in BP, in turn, directly influence the renal excretion of sodium and water, thus providing a negative feedback mechanism for the control of ECF volume, cardiac output, and BP. The hypothesis is that derangements in this renal fluid-volume pressure control mechanism are the fundamental cause of virtually all hypertensive states (Fig. 15-1). In every hypertensive state, an underlying abnormality exists in the intrinsic natriuretic capacity of the kidney, so that the daily salt intake cannot be excreted normally, and the development of hypertension is necessary to induce a pressure natriuresis that allows the kidney to excrete the daily salt intake. Normal sodium balance and ECF volume are maintained, but at the expense of systemic hypertension. The underlying cause for the abnormality in the natriuretic capacity depends on the etiology of hypertension. In essential hypertension, some underlying abnormality increases renal avidity for sodium. In patients with obesity and insulin resistance (metabolic syndrome), hyperinsulinemia increases proximal tubular sodium reabsorption. Increased angiotensin II levels and sympathetic nervous system activity also enhance sodium reabsorption. Mineralocorticoids enhance distal tubular sodium reabsorption. Renal parenchymal disease causes nephron loss, resulting in a natriuretic defect. Abnormalities in renal endothelin or nitric oxide (NO) levels may also impair natriuresis. To date, each of the genetic causes of hypertension that have been elucidated has been shown to relate to an abnormality of renal sodium handling. For example, Liddle's syndrome results from enhanced distal tubular sodium reabsorption due to an abnormality in sodium channels in the distal nephron. Cross-transplant experiments in hypertensive and normotensive rat strains validate the importance of the kidney in the pathogenesis of hypertension, because the presence or absence of hypertension depends on the donor source of the kidney. Guyton's hypothesis states that this decreased natriuretic capacity of the kidney initially leads to renal
P.246
salt and water retention, ECF volume expansion, and increased cardiac output with hypertension. This phase of volume expansion and high cardiac output is short lived. In the setting of high cardiac output, autoregulatory vasoconstriction of each vascular bed matches the blood flow to the metabolic requirements of the tissues. This phenomenon of circulatory autoregulation leads to an increase in systemic vascular resistance (SVR). Thus, hypertension that was initially caused by high cardiac output becomes high-SVR hypertension.The development of hypertension represents a protective mechanism, because it induces the kidney to undergo a pressure natriuresis and diuresis, thereby restoring normal salt balance and returning ECF volume to normal. This mechanism explains why an underlying problem with sodium excretion, as in salt-sensitive hypertension, is manifest as high-SVR hypertension
P.247
without evidence of overt fluid overload. Support for this hypothesis is found in animal models of mineralocorticoid-induced hypertension. To substantiate the role of direct pressure induced natriuresis in the regulation of sodium balance in mineralocorticoid hypertension, Hall and colleagues compared the systemic BP and natriuretic effect of aldosterone infusion in a dog model in which the renal perfusion pressure was either allowed to increase or mechanically servocontrolled to maintain renal artery pressure at normal levels. In the intact animal, continuous aldosterone infusion caused a transient period of sodium and water retention with a mild increase in BP. This sodium retention lasted only a few days, however, and was followed by an escape from the sodium-retaining effects of aldosterone and a restoration of normal sodium balance. In contrast, when the renal perfusion pressure was servocontrolled during aldosterone infusion, no aldosterone escape occurred, and a relentless increase in sodium and water retention occurred, accompanied by severe hypertension, edema, ascites, and pulmonary edema. When the servocontrol device was removed and the renal perfusion pressure was allowed to rise to the systemic level, a prompt natriuresis and diuresis ensued, with the restoration of sodium balance and a fall in BP. These observations highlight the pivotal role of BP in the regulation of renal sodium and water excretion. Moreover, the observation that abnormal renal sodium handling is central in the pathogenesis of all forms of hypertension provides a sound pathophysiologic rationale for the JNC 7 recommendation regarding thiazide-type diuretics as first-line antihypertensive therapy in most patients.Diagnostic evaluation of hypertension. Detection of hypertension begins with proper measurement of BP at each health care encounter. Repeated BP measurements are used to determine whether initial elevations persist and require prompt attention or have returned to normal values and require only periodic surveillance. BP measurement should be standardized as follows: After at least 5 minutes of rest, the patient should be seated in a chair with the back supported and one arm bared and supported at heart level. The patient should refrain from smoking or ingesting caffeine for 30 minutes before the examination. For an appropriately sized cuff, the bladder should encircle at least 80% of the arm. Many patients require a large adult cuff. Measurements should ideally be taken with a mercury sphygmomanometer. Alternatively, a recently calibrated aneroid manometer or a validated electronic device can be used. The first appearance of sound (phase 1) is used to define systolic BP. The disappearance of sound (phase 5) is used to define diastolic BP. The BP should be confirmed in the contralateral arm. Measurement of BP outside of the physician's office may provide some valuable information with regard to the diagnosis and treatment of hypertension. Self-measurement is useful in distinguishing sustained hypertension from white-coat hypertension, a condition in which the patient's pressure is consistently elevated in the clinician's office but normal at other times. Self-measurement may also be used to assess the response to antihypertensive medications and as a tool to improve patient adherence to treatment. Ambulatory monitoring is useful for the evaluation of suspected white-coat hypertension, patients with apparent drug resistance, hypotensive symptoms with antihypertensive medications, and episodic hypertension. However, ambulatory BP measurement is not appropriate for the routine evaluation of patients with suspected hypertension. In elderly patients, the possibility of pseudohypertension should always be considered in the diagnostic evaluation of possible hypertension. Pseudohypertension is a condition in which the indirect measurement of arterial pressure using a cuff sphygmomanometer is artificially high in comparison to direct intra-arterial pressure measurement. Failure to recognize pseudohypertension can result in unwarranted and sometimes frankly dangerous treatment. Pseudohypertension can result from Monckeberg's medial calcification (a clinically benign form of arterial calcification) or advanced atherosclerosis with widespread calcification of intimal plaques. In these entities, stiffening of the arterial wall may prevent its collapse by externally applied pressure, resulting
P.248
in artificially high indirect BP readings affecting both systolic and diastolic measurements. The presence of a positive Osler's maneuver, in which the radial or brachial artery remains palpable despite being made pulseless by proximal inflation of a cuff above systolic pressure, is an important physical examination finding that should suggest the diagnosis. Roentgenograms of the extremities frequently reveal calcified vessels. The diagnosis can only be made definitely by a direct measurement of intra-arterial pressure. Patients with pseudohypertension are often elderly and therefore may have a critical limitation of blood flow to the brain or heart, such that inappropriate BP treatment may precipitate life-threatening ischemic events.The initial history and physical examination of patients with documented hypertension should be designed to assess lifestyle, identify other cardiovascular risk factors, and identify the presence of target-organ damage that may affect prognosis and impact treatment decisions (Table 15-2). Although the vast majority of hypertensive patients have essential (primary) hypertension without a clearly definable etiology, the initial evaluation is also designed to screen for identifiable causes of secondary hypertension (Table 15-3). A medical history should include information about prior BP measurements, to assess the duration of hypertension, and details about adverse effects from any prior antihypertensive therapy. History or symptoms of coronary heart disease, CHF, cerebrovascular disease, peripheral vascular disease, or renal disease should be carefully evaluated. Symptoms suggesting unusual secondary causes of hypertension should be queried, such as weakness (hyperaldosteronism) or episodic anxiety, headache, diaphoresis, and palpitations (pheochromocytoma). Information regarding other risk factors, such as diabetes, tobacco use, hyperlipidemia, physical activity, and any recent weight gain, should be obtained. Dietary assessment regarding the intake of salt, alcohol, and saturated fat is also important. Detailed information should be sought regarding all prescription and over-the-counter medication use, including herbal remedies and illicit drugs, some of which may raise BP or interfere with the effectiveness of antihypertensive therapy. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) impair the response to virtually all antihypertensive agents and increase the risk of hyperkalemia or renal insufficiency with ACE inhibitor therapy. Stimulants such as cocaine, ephedra, amphetamines, and anabolic steroids can raise BP. A family history of hypertension, diabetes, premature cardiovascular disease, or renal disease should be sought. A psychosocial history is important to identify family situation, working conditions, employment status, educational level, and sexual dysfunction that may influence adherence to antihypertensive treatment.
Table 15-3. Identifiable Causes of Hypertension
Metabolic syndrome (obesity, insulin resistance, impaired glucose tolerance, dyslipidemia, hypertension) Obstructive sleep apnea Drug-induced hypertension (see Table 14-7) Chronic kidney disease Primary hyperaldosteronism Renovascular disease Chronic steroid use or Cushing syndrome Pheochromocytoma Coarctation of the aorta Thyroid or parathyroid disease (Adapted with permission from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.) P.249
Physical examination should include the measurement of height, weight, and calculation of body mass index (weight in kg divided by the square of height in meters). Funduscopic examination is important to identify striate hemorrhages, cotton-wool spots, and papilledema, the characteristic findings of hypertensive neuroretinopathy, which are indicative of the presence of malignant hypertension. Documentation of the presence of arteriosclerotic retinopathy (e.g., arteriolar narrowing, arteriovenous crossing changes, changes in light reflexes) is less important, given its lack of prognostic significance with regard to the potential long-term cardiovascular complications of hypertension. Examination of the neck for carotid bruits, distended neck veins, and thyromegaly is important. Cardiac examination should include investigation for abnormalities of rate or rhythm, murmurs, and third or fourth heart sounds. The lungs should be examined for rales and evidence of bronchospasm. Abdominal examination should include auscultation for bruits (an epigastric bruit present in both systole and diastole suggests renal artery stenosis), abdominal or flank masses (polycystic kidney disease), or increased aortic pulsation (abdominal aortic aneurysm). Peripheral pulses should be examined for quality and bruits. The lower extremities should be examined for edema. A neurologic screening examination is used to identify prior cerebrovascular events. Routine laboratory tests are recommended before the initiation of antihypertensive therapy to identify other risk factors and screen for the presence of target-organ damage. These routine tests include blood chemistry (sodium, potassium, creatinine, fasting glucose), lipid profile (total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol), and a complete blood cell count. Creatinine clearance should be estimated using either the Cockcroft-Gault or the Modification of Diet in Renal Disease (MDRD) study forumulae. A urinalysis is used to identify proteinuria or hematuria that would suggest the presence of underlying primary renal disease. A 12-lead electrocardiogram (ECG) is used to identify left atrial enlargement, LVH, or prior MI. Optional tests, depending on the clinical situation, include 24-hour creatinine clearance, 24-hour urine protein or urine protein to creatinine ratio, serum uric acid, glycosylated hemoglobin, and thyroid function tests. A limited ECG to identify the presence of LVH may be useful in selected patients to determine the clinical significance of labile hypertension. The majority of patients with hypertension have primary (essential) hypertension in which no clearly definable underlying etiology is apparent.
In contrast, a wide variety of uncommon conditions can lead to so-called secondary hypertension, some of which are potentially amenable to surgical correction (Table 15-3). Secondary causes of hypertension include underlying chronic kidney disease (CKD), primary hyperaldosteronism, pheochromocytoma, renovascular hypertension due to fibromuscular dysplasia or atherosclerotic renal artery stenosis, coarctation of the aorta, and Cushing's syndrome. Secondary causes of hypertension amenable to surgical intervention are so unusual that extensive diagnostic testing is not warranted. More extensive laboratory and radiographic testing for identifiable causes of hypertension is not indicated unless adequate control of BP cannot be achieved with a multidrug antihypertensive regimen that includes a diuretic. The initial history, physical examination, and routine laboratory tests are usually all that is required to evaluate for the possibility of secondary hypertension. A normal estimated creatinine clearance and urinalysis are usually sufficient to exclude underlying renal disease as a secondary cause of hypertension. Examination for abdominal or flank masses is used to screen for polycystic kidney disease, which can be confirmed by ultrasound examination. Because most patients with primary hyperaldosteronism have unprovoked hypokalemia while not on diuretic therapy, a measurement of serum potassium is a suitable screening test, and routine measurement of aldosterone levels is not necessary. Assessment for any delay or diminution of pulses in the lower extremities, or a discrepancy between arm and leg BP can be used to screen for coarctation
P.250
of the aorta. A careful assessment for a history of episodic hypertension, associated with headache, palpitations, diaphoresis, and pallor, is all that is usually required to screen for pheochromocytoma. The routine measurement of serum or urine catecholamines is not warranted. Likewise, evaluation for truncal obesity and abdominal purple striae is all that is usually required to screen for Cushing's syndrome; therefore, routine measurement of serum cortisol or cortisol suppression testing is unnecessary. Several tests are notably absent from the recommended list of routine screening tests for secondary hypertension. Hypertensive intravenous pyelography, renal scanning, captopril renography, and arterial digital subtraction angiography all lack sufficient specificity to be of any value as routine screening tests for renovascular hypertension. In this regard, the prevalence of renovascular hypertension in the general hypertensive population is so low that the predictive value of a positive test from any of these procedures is abysmal when used as a general screening test.
Treatment of hypertension
Goals of treatment. The goal of treating hypertension is the reduction of cardiovascular and renal morbidity and mortality. Because systolic BP correlates best with target-organ damage and mortality, the primary focus should be on achieving the systolic BP goal. The goal of treatment is a systolic BP less than 140 mm Hg and a diastolic BP less than 90 mm Hg. In hypertensive patients with diabetes or underlying chronic kidney disease, a BP goal of less than 130/80 mm Hg is recommended.
Nonpharmacologic treatment. Lifestyle modification is recommended in the management of all individuals with hypertension, even in those who require antihypertensive drug treatment. All patients should be encouraged to adopt the lifestyle modificationis outlined in Table 15-4, especially if they have additional cardiovascular risk factors such as hyperlipidemia or diabetes. Modest weight reduction of as little as 4 kg (10 lbs) significantly reduces BP. Anorectic agents should be avoided because they may contain stimulants that raise BP. Obstructive sleep apnea (OSA) is now recognized as an important treatable cause of hypertension. Clues to the presence of OSA include morbid obesity, daytime hypersomnolence, headache, snoring, or fitful sleep. The diagnosis can be confirmed with a sleep study to document apneic episodes. Appropriate treatment with a continuous positive airway pressure (CPAP) device may result in a significant reduction in BP. Dietary sodium intake in the form of sodium chloride (NaCl; table salt) has a strong epidemiologic link to hypertension. Meta-analysis of clinical trials indicates that the limitation of dietary sodium intake to 75 to 100 mEq per day lowers BP over a period of several weeks to a few years. The restriction of sodium intake has been shown to reduce the need for antihypertensive medication, reduce diuretic-induced renal potassium wasting, lead to regression of LVH, and prevent renal stones through a reduction in renal calcium excretion. Average American dietary sodium intake is in excess of 150 mEq per day, most of which (75%) is derived from processed foods. Moderation of sodium intake to a level of less than 100 mEq per day (2.4 g of sodium or 6 g of sodium chloride) is recommended for the nonpharmacologic treatment of hypertension.
Table 15-4. Lifestyle Modifications to Manage Hypertension
Modification Recommendation Approximate SBP reduction Weight loss Maintain normal weight (BMIa 18.5 24.9) 5 20 mm Hg/10 kg Dietary sodium restriction Limit dietary sodium intake to less than 100 mEq/day (2.4 gm sodium or 6 gm sodium chloride) 2 8 mm Hg Adopt DASH diet Consume diet rich in fruits, vegetables, and low-fat dairy products with a reduced content of saturated and total fat 8 14 mm Hg Increase physical activity Engage in regular aerobic physical activity such as brisk walking (at least 30 minutes per day, most days of the week) 4 9 mm Hg Moderate alcohol consumption Limit consumption to no more than two drinks per day (1 oz or 30 mL ethanol per day; e.g., 24 oz beer, 10 oz wine, 3 oz 80-proof whiskey) in most men, and no more than one drink per day in women and lighterweight men 2 4 mm Hg aBMI indicates body mass index calculated as weight in kilograms divided by the square of height in meters. (Adapted with permission from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.) Excessive intake of ethanol is an important risk factor for high BP, and it can lead to resistant hypertension. Ethanol intake should be limited to not more than 30 mL (1 oz) per day in men and 15 mL (0.5 oz) per day in women and lighter-weight men. This type of moderate ethanol intake may be associated with a reduction in risk of coronary heart disease.
Regular aerobic exercise can enhance weight loss and reduce the risk for cardiovascular disease and all-cause mortality.
Inadequate potassium intake may increase BP, whereas high dietary potassium intake may improve BP control in patients with hypertension. An intake of 90 mEq per day in the form of fresh fruits and vegetables should be recommended.
P.251
An increase in dietary calcium may lower blood pressure in some patients with hypertension, but the effect is negligible. Nonetheless, adequate calcium intake is recommended for general health and osteoporosis prophylaxis.
Smoking cessation and reductions in dietary fat and cholesterol are also recommended to reduce overall cardiovascular risk. Although caffeine may acutely raise BP, tolerance to this effect develops quickly. Most epidemiologic studies have found no direct relationship between caffeine intake and BP.
Pharmacologic treatment of hypertension. The decision to treat hypertension with medications after the failure of lifestyle modifications to adequately control BP or initially, as an adjunct to lifestyle modifications, is based on the severity (stage) of hypertension and an assessment of the risk of cardiovascular morbidity, given the presence of other cardiovascular risk factors and pre-existing target organ damage or cardiovascular disease (see Table 15-2). Reducing BP with drugs clearly decreases cardiovascular morbidity and mortality regardless of age, gender, race, stage of hypertension, or socioeconomic status. Benefit has been demonstrated for stroke, coronary events, heart failure, progression of primary renal disease, prevention of progression to malignant hypertension, and all-cause mortality. Numerous clinical trials have demonstrated that lowering BP with several classes of drugs, including thiazide-type diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs), beta-blockers, and
P.252
calcium channel blockers (CCBs), reduces all the complications of hypertension. Thiazide-type diuretics have been the treatment regimen employed in most large-scale outcome trials. In these trials, including the recently published Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), thiazide diuretics are unsurpassed in antihypertensive efficacy and for prevention of the cardiovascular complications of hypertension. In ALLHAT, stage 1 or 2 hypertensive patients older than age 55, with at least one other cardiovascular risk factor, received first-line treatment with chlorthalidone (thiazide-type diuretic), doxazocin (selective alpha-blocker), amlodipine (CCB), or lisinopril (ACE inhibitor). In this study, 47% of patients were women, 35% were black, 19% were Hispanic, 36% were diabetic, and the mean body mass index (BMI) was nearly 30. The doxazocin arm was terminated prematurely because of an excess of CHF. After a mean follow-up of 4.9 years, neither the primary clinical outcome (fatal coronary heart disease or nonfatal MI), nor the secondary outcomes of all-cause mortality, combined coronary heart disease, peripheral arterial disease, cancer, or ESRD had occurred more often in the clorthalidone group than in the amlodipine or lisinopril groups. Furthermore, event rates were signficantly lower in the chlorthalidone group than in one or both of the other groups for some of the secondary outcomes (Table 15-5). As expected, patients in the chlorthalidone group developed higher cholesterol levels, lower serum potassium levels, and higher fasting blood glucose levels than patients in other groups. The mean cholesterol was 216 mg per dL at baseline, falling at 4 years to 197 mg per dL in the chlorthalidone group, to 196 mg per dL in the amlodipine group (p = 0.009 versus chlorthalidone), and to 195 mg per dL in the lisinopril group (p < 0.001 versus chlorthalidone). At 4 years, 8.5% of the chlorthalidone group had developed hypokalemiaP.253
(serum potassium less than 3.5 mEq per L), compared with 1.9% in the amlodipine group (p < 0.001) and 0.8% in the lisinopril group (p < 0.001). The incidence of new-onset diabetes (fasting blood glucose greater than 126 mg per dL) was 11.6% with chlorthalidone, compared with 9.8% in the amlodipine group (p = 0.04) and 8.1% in the lisinopril group (p < 0.001). Nontheless, the presence of these metabolic abnormalities did not translate into more cardiovascular events or deaths in the chlorthalidone group. The public health implications of ALLHAT are enormous. The 2002 Drug Topics Red Book indicates that generic chlorthalidone costs $15.95 for 100 tablets, compared with $97.96 for Prinavil (lisinopril) 10 mg, $102.76 for Zestril (lisinopril) 10 mg, and $145.13 for Norvasc (amlodipine) 5 mg. Using the less expensive generic diuretic to treat the more than 50 million hypertensive patients in the United States could lead to a cost savings of billions of dollars annually. Based on the results of the ALLHAT and other trials, the JNC 7 report has recommended that thiazide-type diuretics should be used as initial therapy for most patients with hypertension, either alone or in combination with one of the other classes of drugs (ACE inhibitors, ARBs, beta-blockers, or CCBs). An algorithm outlining the approach to treatment of hypertension is shown in Fig. 15-2. Diuretic therapy potentiates the antihypertensive effect of most other antihypertensive drugs. For this reason, the drug treatment algorithm outlined in JNC 7 recommends the addition of diuretic as a second-step agent if BP is inadequately controlled with any other drug chosen as a first-line agent. The mechanism of action of thiazide diuretics is to block sodium reabsorption by inhibiting the thiazide-sensitive NaCl cotransporter in the distal tubule. The sustained antihypertensive effect of thiazides however, is mediated through a reduction in systemic vascular resistance rather than through chronic volume depletion and a reduction of cardiac output, as one might predict. In fact, thiazides do not cause a large, sustained decrease in intravascular volume or sodium balance when used for the treatment of hypertension. Within a few days to weeks of the initiation of therapy with thiazide diuretics, salt balance returns toward normal, and total-body sodium and intravascular volume returns toward pretreatment levels. This seeming paradox can be understood in the context of Guyton's hypothesis regarding the pathogenesis of hypertension, whereby the development of systemic hypertension is conceptualized as an essential protective mechanism to maintain normal fluid volume in various disease states in which an underlying renal impairment exists with regard to excreting the daily sodium load at a normal BP (Fig. 15-2). In this context, diuretics lower BP by addressing the primary renal defect in salt excretion, so that systemic hypertension (high SVR) is no longer a prerequisite for maintaining sodium balance. It should be noted that in ALLHAT and most clinical trials, achievement of the desired BP goal often requires treatment with two or more antihypertensive agents. Addition of a second drug from a different class should be implemented when use of a single drug in optimal doses fails to adequately control BP. When the BP is more than 20 mm Hg systolic or 10 mm Hg diastolic above goal, treatment may be initiated with two drugs (usually including a thizide-type diuretic), either as separate prescriptions or in fixed-dose combinations.Table 15-5. Results of the Antihypertensive Lipid-Lowering to Prevent Heart Attack Trial
6-Year Incidence (%) Outcome Chlorthalidone Amlodipine Lisinopril Primary outcome Coronary heart diseasea 11.5 11.3 11.4 Secondary outcomes All-cause mortality 17.3 16.8 17.2 Stroke 5.6 5.4 6.3b Combined coronary heart diseasec 19.9 19.9 20.8 Combined cardiovascular diseased 30.9 32.0 33.3b Angina 12.1 12.6 13.6b Coronary revascularization 9.2 10.0 10.2b Heart failure 7.7 10.2b 8.7b ;End-stage renal disease 1.8 2.1 2.0 Cancer 9.7 10.0 9.9 aFatal coronary heart disease or nonfatal myocardial infarction. bp 0.05. cCombined coronary heart disease death, nonfatal myocardial infarction, coronary revascularization, and hospitalized angina. dCombined coronary heart disease death, nonfatal myocardial infarction, coronary revascularization, angina, heart failure, and peripheral arterial disease. (Adapted with permission from The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981 2997.) 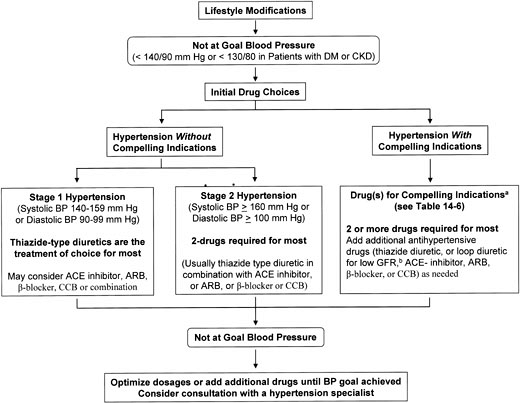
Figure 15-2. Algorithm for treatment of hypertension. aCompelling indications are special high-risk conditions for which clinical trials demonstrate benefit of specific classes of antihypertensive drugs: treatment of hypertension in the setting of diabetes, chronic kidney disease, heart failure, high coronary disease risk, post-MI, and for recurrent stroke prevention. bIn the setting of advanced chronic kidney disease with GFR less than 30 mL per minute or in patients with fluid overload unresponsive to thiazide diuretics, more potent loop diuretic therapy may be requried. (BP, blood pressure; DM, diabetes mellitus; CKD, chronic kidney disease; ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blocker; and CCB, calcium channel blocker.) (Adapted with permission from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.)
Treatment of hypertension in special populations. The presence of certain comorbidities or target-organ damage in the individual hypertensive patient may provide a compelling indication for treatment with a certain class of antihypertensive agent, based on favorable outcome data from clinical trials (Table 15-6). In hypertensive patients with diabetes mellitus, thiazide diuretics, beta-blockers, ACE inhibitors, ARBs, and CCBs have been shown to reduce cardiovascular disease and the incidence of stroke. In patients with evidence of diabetic nephropathy, ACE inhibitor- or ARB-based treatment regimens have been shown to retard the progression of nephropathy, reduce urine albumin excretion, and slow progression from
P.254
microalbuminuria to overt proteinuria. Chronic kidney disease (CKD) is present in patients with estimated glomerular filtration rate less than 60 mL per minute or if albuminuria (greater than 300 mg per day or 200 mg albumin per gram creatinine on spot urine specimen) is present. ACE inhibitors and ARBs have been shown to slow the progression of both diabetic and nondiabetic CKD. Thus, these agents should be included as part of the multidrug regimen often required for adequate BP control in CKD. Potent loop diuretics are usually needed in combination with other classes of drugs when the estimated GFR falls below 30 mL per minute. LVH is an independent risk factor for subsequent cardiovascular disease. Regression of LVH occurs with aggressive BP management using all classes of drugs except the direct-acting vasodilators such as hydralazine and minoxidil. Ischemic heart disease is a common form of target-organ damage in hypertension. In patients with hypertension and stable angina pectoris, the treatment regimen should include a beta-blocker or, alternatively, a long-acting CCB.P.255
P.256
In patients with acute coronary syndromes (unstable angina or acute MI), hypertension should be treated initially with beta-blockers and ACE inhibitors, with the addition of other agents such as thiazide diuretics as needed for BP control. In the chronic BP management of post-MI patients, beta-blockers, ACE inhibitors, and aldosterone receptor antagonists have proven to be of highest benefit. In patients with ischemic heart disease, low-dose aspirin therapy and intensive lipid lowering therapy are also indicated. Heart failure represents another special hypertensive patient population; it can occur in the setting of either systolic or diastolic dysfunction. In asymptomatic patients with LV dysfunction, ACE inhibitors and beta-blockers are recommended. In patients with symptomatic heart failure or end-stage heart disease, ACE inhibitors, beta-blockers, ARBs, and aldosterone receptor blockers (spironolactone or eplerenone) are recommended, along with potent loop diuretics as needed for fluid overload. Treatment of hypertension in patients with cerebrovascular disease requires special consideration. Lowering of BP during the acute phase of an ischemic stroke may worsen ischemia and extend the infarct. However, treatment of chronic hypertension following a cerebrovascular accident with ACE inhibitors and thiazide-type diuretics may reduce the rate of recurrent stroke. The treatment of elderly patients with predominant systolic hypertension should follow the same treatment algorithm. In the Systolic Hypertension in the Elderly Program (SHEP) trial, a double-blind placebo-controlled trial of low-dose chlorthalidone in patients over age 60 with isolated systolic hypertension (systolic BP greater than 160 mm Hg with diastolic BP less than 90 mm Hg), the relative risks of stroke, left ventricular failure, nonfatal MI or fatal coronary heart disease, and the requirement for coronary artery bypass grafting were all significantly reduced in the active treatment group. Because of the risks of orthostatic hypotension and falls, selective alpha-blockers should be avoided in the treatment of older individuals with hypertension.Table 15-6. Clinical Trial and Guideline Basis for Compelling Indications for Treatment with Individual Drug Classes
High-risk condition with compelling Indication Diuretic Beta-blocker ACE inhibitor ARB CCB Aldosterone antagonist Clinical trial basisa Diabetes mellitus ALLHAT, UKPDS, NKF Guideline, ADA Guideline Chronic kidney disease Captopril Trial, RENAAL, IDNT, REIN, AASK, NKF Guideline Heart failure ACC/AHA Heart Failure Guideline, MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, ValHEFT, RALES High coronary disease risk ALLHAT, HOPE, ANBP2, Life, CONVINCE Post-myocardial infarction ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS Recurrent stroke prevention PROGRESS aCompelling indications for certain classes of antihypertensive drugs are based on proven benefit from outcome studies or existing clinical practice guidelines. The compelling indication must be managed in parallel with blood pressure. Patients with these high-risk conditions usually require combination treatment with two to three additional antihypertensive drugs from different classes in order to achieve the recommended blood pressure treatment goal. AASK, African American Study of Kidney Disease and Hypertension; ACC/AHA, American College of Cardiology/American Heart Association; ACE, angiotensin-converting enzyme; AIRE, Acute Infarction Ramipril Efficacy; ALLHAT, Antihypertensive and Lipid-Lowering to Prevent Heart Attack Trial; ANBP2, Second Australian National Blood Pressure Study; ARB, angiotensin-receptor blocker; BHAT, Beta-Blocker Heart Attack Trial; CCB, calcium channel blocker; CIBIS, Cardiac Insufficiency Bisoprolol Study; CONVINCE, Controlled Onset Verapamil Investigation of Cardiovascular Endpoints; COPERNICUS, Carvedilol Prospective Randomized Cumulative Survival Study; EPHESUS, Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study; HOPE, Heart Outcomes Prevention Evaluation Study; INDT, Irbesartan Diabetic Nephropathy Trial; LIFE, Losartan Intervention for Endpoint Reduction in Hypertension Study; MERIT-HT, Metoprolol CR/SL Randomized Intervention Trial in Congestive Heart Failure; NKF, National Kidney Foundation; PROGRESS, Perindopril Protection against Recurrent Stroke Study; RALES, Randomized Aldactone Evaluation Study; EEIN, Ramipril Efficacy in Nephropathy Study; RENAAL, Reduction of Endpoints in Non-Insulin Dependent Diabetes Mellitus with the Angiotensin II Antagonist Losartan Study; SAVE, Survival and Ventricular Enlargement Study; SOLVD, Studies of Left Ventricular Dysfunction; TRACE, Trandolapril Cardiac Evaluation Study; USPDS, United Kingdom Prospective Diabetes Study; ValHEFT, Valsartan Heart Failure Trial. (Adapted from Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The JNC 7 Report. JAMA 2003;289:2560 2572.) Treatment of the patient with resistant hypertension. Resistant hypertension is defined as a failure to reach BP less than 140/90 mm Hg in an adherent patient treated with a three-drug regimen including a diuretic. Truly resistant hypertension should prompt an investigation for underlying potentially treatable forms of secondary hypertension (Table 15-3). Table 15-7 outlines other causes of resistant hypertension. Consultation with a hypertension specialist should be considered if the BP goal cannot be achieved.
Table 15-7. Causes of resistant hypertension
Improper blood pressure measurement (use of inadequately sized BP cuff in obese patients) Pseudohypertension in elderly individuals White coat (office) hypertension Volume overload or pseudotolerance Excess dietary sodium intake Fluid retention from underlying renal disease Inadequate diuretic therapy (failure to use loop diuretic with advanced CKD) Noncompliance Patient nonadherence with therapy due to ignorance, cost, or side-effects Physician noncompliance (inadequate drug dosage or failure to include diuretic in regimen) Drug-induced Nonsteroidal anti-inflammatory agents (NSAIDs) or cyclooxygenase 2 (Cox 2) inhibitors Cocaine, amphetamines, or other illicit drugs Sympathomimetics (decongestants or anoretic agents) Oral contraceptives Adrenal steroids Erythropoietin Licorice Over-the-counter dietary supplements (ephedra, ma huang, bitter orange) Excessive alcohol consumption Identifiable secondary causes of hypertension (see Table 15-3)
Benign versus malignant hypertension. The classification of hypertension as benign or malignant is based on funduscopic examination. The finding of hypertensive neuroretinopathy (HNR) is the clinical sine qua non for the diagnosis of malignant hypertension (Fig. 15-3). In the absence of HNR, malignant hypertension cannot be diagnosed, regardless of the severity of the hypertension. Hypertensive neuroretinopathy is defined by the presence of striate hemorrhages and cotton-wool spots with or without papilledema (Table 15-8). The clinical importance of the finding of HNR is that it signifies the presence of a systemic hypertensive vasculopathy with fibrinoid necrosis and obliterative arteriopathy that, left untreated, will lead to ESRD or death within 1 year. Fortunately, malignant hypertension is a relatively rare disorder, occurring in less than 1% of hypertensive patients. The term benign hypertension is clearly a misnomer, because although the clinical course is less dramatic and precipitous than that seen in patients with malignant hypertension, the eventual cerebrovascular and cardiovascular complications are quite devastating, and they represent a major cause of morbidity and mortality in the general population. Benign hypertension is defined based on the absence of hypertensive neuroretinopathy. Retinal arteriosclerosis and arteriosclerotic retinopathy (see Table 15-8), which are the characteristic funduscopic findings in benign hypertension, are of little clinical utility, because they may be found in elderly normotensive individuals. These findings have no predictive value with regard to the risk of cardiovascular or cerebrovascular complications.
Table 15-8. Classification of hypertensive retinopathy
Retinal arteriosclerosis and arteriosclerotic retinopathy (characteristic of benign hypertension) Arteriolar narrowing (focal or diffuse) Arteriovenous crossing changes Broadening of the arteriolar light reflex Copper or silver wiring changes Perivasculitis Solitary round retinal hemorrhages Hard exudates Central or branch venous occlusion Hypertensive neuroretinopathy (sine qua non of malignant hypertension) Generalized arteriolar narrowing Striate (flame-shaped hemorrhages)a Cotton-wool spots (soft exudates)a Bilateral papilledemaa Star figure at the macula aThese features distinguish retinal arteriosclerosis (benign hypertension) from hypertensive neuroretinopathy (malignant hypertension). (Adapted with permission from Nolan CR. Malignant hypertension and other hypertensive crises. In: RW Schrier, (ed.) Diseases of the kidney and urinary tract, 7th ed. Boston: Lippincott Williams & Wilkins, 2000;1513 1592.) 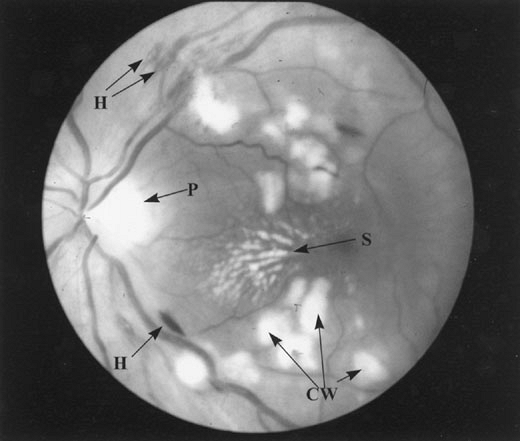
Figure 15-3. Hypertensive neuroretinopathy in malignant hypertension. Fundus photograph in a 30-year-old man with malignant hypertension demonstrates all the characteristic features of hypertensive neuroretinopathy, including striate hemorrhages (H), cotton-wool spots (CW), papilledema (P), and a star figure at the macula (S).
P.257
Definition of hypertensive crises. The vast majority of hypertensive patients are asymptomatic for many years until complications due to atherosclerosis, cerebrovascular disease, or CHF supervene. In a minority of patients, this benign course is punctuated by a hypertensive crisis. A hypertensive crisis is defined as the turning point in the course of an illness at which acute management of the elevated BP plays a decisive role in the eventual outcome. The haste with which the BP must be controlled varies with the type of hypertensive crisis. However, the crucial role of hypertension in the disease process must be identified and a plan for managing the BP successfully implemented if the patient's outcome is to be optimal. The absolute level of the BP is clearly not the most important factor in determining the existence of a hypertensive crisis. For example, in children, pregnant women, and other previously normotensive individuals in whom mild to moderate hypertension develops suddenly, a hypertensive crisis can occur at a BP level that is normally well tolerated by adults with chronic hypertension. Furthermore, in adults with mild to moderate hypertension, a crisis can occur with the onset of acute end-organ dysfunction involving the heart or brain. Table 15-9 outlines the spectrum of hypertensive crises.
Table 15-9. Spectrum of Hypertensive Crises
Malignant hypertension (hypertensive neuroretinopathy present) Hypertensive encephalopathy (occurs with either malignant or severe benign hypertension) Nonmalignant ( benign ) hypertensin with acute complications (acute end-organ dysfunction in the absence of hypertensive neuroretinopathy) Acute hypertensive heart failure (pulmonary edema due to acute diastolic dysfunction) Acute coronary syndromes Acute myocardial infarction Unstable angina Acute aortic dissection Central nervous system catastrophe Hypertensive encephalopathy Intracerebral hemorrhage Subarachnoid hemorrhage Severe head trauma Catecholamine excess states Pheochromocytoma crisis Monoamine oxidase inhibitor tyramine interactions Antihypertensive drug withdrawal syndromes Phenylpropanolamine overdose Preeclampsia and eclampsia Active bleeding (including postoperative bleeding) Poorly controlled hypertension in patients requiring emergency surgery Severe postoperative hypertension Postcoronary artery bypass hypertension Postcarotid endarterectomy hypertension Scleroderma renal crisis Autonomic hyperreflexia in quadriplegic patients (Adapted from Nolan CR. Malignant hypertension and other hypertensive crises. In: Schrier RW, ed. Diseases of the kidney and urinary tract, 7th ed. Boston: Lippincott Williams & Wilkins, 2001. Malignant hypertension is a clinical syndrome characterized by a marked elevation of BP with widespread acute arteriolar injury (hypertensive vasculopathy). Funduscopy reveals HNR with flame-shaped hemorrhages, cotton-wool spots (soft exudates), and sometimes papilledema (Fig. 15-3). Regardless of the severity of BP elevation, in the absence of HNR, malignant hypertension cannot be diagnosed. HNR is thus an extremely important clinical finding, indicating the presence of a hypertension-induced arteriolitis that may involve the kidneys, heart, and central nervous system. With malignant hypertension, a rapid and relentless progression to ESRD occurs if effective BP control is not implemented. Mortality can result from
P.258
acute hypertensive heart failure, intracerebral hemorrhage, hypertensive encephalopathy, or complications of uremia. Malignant hypertension represents a hypertensive crisis; adequate control of BP clearly prevents these morbid complications.Hypertensive crises due to nonmalignant hypertension with acute complications. Even in patients with benign hypertension, in whom HNR is absent, a hypertensive crisis may be diagnosed based on the presence of concomitant acute end-organ dysfunction (Table 15-9). Hypertensive crises due to nonmalignant hypertension with acute complications include hypertension accompanied by hypertensive encephalopathy, acute hypertensive heart failure, acute aortic dissection, intracerebral hemorrhage, subarachnoid hemorrhage, severe head trauma, acute MI or unstable angina, and active bleeding. Poorly controlled hypertension in a patient requiring surgery increases the risk of intraoperative cerebral or myocardial ischemia and postoperative acute renal failure. Severe postoperative hypertension, including post coronary artery bypass hypertension and post carotid endarterectomy hypertension, increases the risk of postoperative bleeding, hypertensive encephalopathy, pulmonary edema, and myocardial ischemia. The various catecholamine-excess states can cause a hypertensive crisis with hypertensive encephalopathy or acute hypertensive heart failure. Preeclampsia and eclampsia represent hypertensive crises that are unique
P.259
P.260
to pregnancy. Scleroderma renal crisis is a hypertensive crisis in which failure to adequately control BP with a regimen that includes an ACE inhibitor results in rapid irreversible loss of renal function. Hypertensive crises can also occur in quadriplegic patients due to autonomic hyperreflexia induced by bowel or bladder distention. The sudden onset of hypertension in this setting can lead to hypertensive encephalopathy or acute pulmonary edema.Treatment of malignant hypertension. Malignant hypertension must be treated expeditiously to prevent complications such as hypertensive encephalopathy, acute hypertensive heart failure, and renal failure. The traditional approach to patients with malignant hypertension has been the initiation of potent parenteral agents. In general, parenteral therapy should be used in patients with evidence of acute end-organ dysfunction (hypertensive encephalopathy or pulmonary edema) or those unable to tolerate oral medications. Nitroprusside is the treatment of choice for patients requiring parenteral therapy. In general, reducing the mean arterial pressure by 20% or to a level of 160 to 170/100 to 110 mm Hg is safe. The use of a short-acting agent such as nitroprusside has obvious advantages, because BP can quickly be stabilized at a higher level if complications develop during rapid BP reduction. If no evidence of vital organ hypoperfusion is apparent during the initial reduction, the diastolic BP can gradually be lowered to 90 mm Hg over a period of 12 to 36 hours. Oral antihypertensive agents should be initiated as soon as possible to minimize the duration of parenteral therapy. The nitroprusside infusion can be weaned as the oral agents become effective. The cornerstone of initial oral therapy should be arteriolar vasodilators such as hydralazine or minoxidil. Beta-blockers are required to control reflex tachycardia, and a diuretic must be initiated within a few days to prevent salt and water retention in response to vasodilatator therapy when the patient's dietary salt intake increases. Diuretics may not be necessary as a part of initial parenteral therapy, because patients with malignant hypertension often present with volume depletion due to pressure-induced natriuresis. Although many patients with malignant hypertension definitely require initial parenteral therapy, some patients may not yet have evidence of cerebral or cardiac dysfunction or rapidly deteriorating renal function and therefore do not require instantaneous control of BP. These patients can often be managed with an intensive oral regimen, often with a beta-blocker and minoxidil, designed to bring the BP under control within 12 to 24 hours. After the immediate crisis has resolved and the hypertension has been controlled with initial parenteral therapy, oral therapy, or both, lifelong surveillance of BP is mandatory. If control lapses, malignant hypertension can recur even after years of successful antihypertensive therapy. Triple therapy with a diuretic, a beta-blocker, and a vasodilator is often required to maintain satisfactory long-term BP control.
Treatment of other hypertensive crises. Sodium nitroprusside is the drug of choice for the management of virtually all hypertensive crises outlined in Table 15-9, including malignant hypertension, hypertensive encephalopathy, acute hypertensive heart failure, intracerebral hemorrhage, perioperative hypertension, catecholamine-related hypertensive crises, and acute aortic dissection (in combination with beta-blockers). Intravenous nitroglycerin may also be useful in patients with concomitant myocardial ischemia, because it dilatates intracoronary collaterals.
Sodium nitroprusside is a potent intravenous hypotensive agent with an immediate onset and brief duration of action. The site of action is the vascular smooth muscle. It has no direct action on the myocardium, although it may indirectly affect cardiac performance through alterations in systemic hemodynamics. Nitroprusside is an iron-coordination complex with five cyanide moieties and a nitroso group. The nitroso group combines with cysteine to form nitrosocysteine, a potent activator of guanylate cyclase that causes cyclic guanosine monophosphate (cGMP) accumulation and the relaxation of vascular smooth muscle. Nitroprusside causes vasodilation of
P.261
both arteriolar resistance vessels and venous capacitance vessels. Its hypotensive action is a result of a decrease in SVR. The combined decrease in preload and afterload reduces myocardial wall tension and myocardial oxygen demand. The net effect of nitroprusside on cardiac output and heart rate depends on the intrinsic state of the myocardium. In patients with left ventricular systolic dysfunction and elevated left ventricular end-diastolic pressure, it causes an increase in stroke volume and cardiac output as a result of afterload reduction. Heart rate may actually decrease in response to improved cardiac performance. In contrast, in the absence of left ventricular dysfunction, venodilation and preload reduction can result in a reflex increase in sympathetic tone and heart rate. For this reason, nitroprusside must be used in conjunction with a beta-blocker in acute aortic dissection.The hypotensive action of nitroprusside appears within seconds and is immediately reversible when the infusion is stopped. The cGMP in vascular smooth muscle is rapidly degraded by cGMP-specific phosphodiesterases. Nitroprusside is rapidly metabolized, with a half-life of 3 to 4 minutes. Cyanide is formed, as a short-lived intermediate product, by direct combination with sulfhydryl groups in red blood cells and tissues. The cyanide groups are rapidly converted to thiocyanate by the liver, in a reaction in which thiosulfate acts as a sulfur donor. Thiocyanate is excreted by the kidney, with a half-life of 1 week in patients with normal renal function. Thiocyanate accumulation and toxicity can occur when a high dose or prolonged infusion is required, especially in patients with renal insufficiency. When these risk factors are present, thiocyanate levels should be monitored and the infusion stopped if the level is over 10 mg per dL. Thiocyanate toxicity is rare in patients with normal renal function requiring less than 3 g per kg per minute for less than 72 hours. Cyanide poisoning is a very rare complication, unless hepatic clearance of cyanide is impaired by severe liver disease, or massive doses of nitroprusside (more than 10 g per kg per minute) are used to induce deliberate hypotension during surgery. Once the hypertensive crisis has resolved and the BP is adequately controlled, oral antihypertensive therapy should be initiated. The nitroprusside infusion is weaned as the oral antihypertensive agents become effective.
Treatment of severe uncomplicated hypertension in the acute care setting. The benefits of acute reduction in blood pressure in the setting of true hypertensive crisis are obvious (Fig. 15-4). Fortunately, true hypertensive crises are relatively rare events that never affect the vast majority of hypertensive patients. Much more common than true hypertensive crisis is the patient who presents with markedly elevated BP (greater than 180/100 mm Hg) in the absence of HNR (malignant hypertension) or acute end-organ damage that would signify a true crisis. This entity, known as severe uncomplicated hypertension, is very common in the emergency department or other acute-care settings. Of patients with severe uncomplicated hypertension, 60% are entirely asymptomatic and present for prescription refills or routine blood pressure checks, or are found to have elevated pressure during routine physical examinations. The other 40% present with nonspecific findings such as headache, dizziness, or weakness in the absence of evidence of acute end-organ dysfunction.
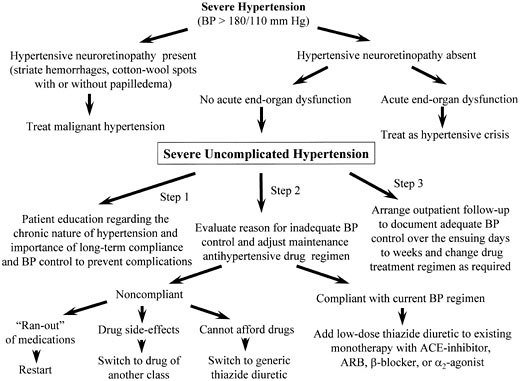
Figure 15-4. Algorithm for treatment of severe uncomplicated hypertension. ACE, angiotensin-converting enzyme; BP, blood pressure; CCB, calcium channel blocker. (Adapted with permission from Nolan CR. Hypertensive crises. In: Schrier RW, ed. Atlas of diseases of the kidney, vol. 3. Philadelphia: Current Medicine, 1999.)
In the past, this entity was referred to as urgent hypertension, reflecting the erroneous notion that an acute reduction of BP over a few hours before discharge from the acute care facility was essential to minimize the risk of short-term complications from severe hypertension. Commonly used treatment regimens included oral clonidine loading or sublingual nifedipine. However, the practice of acute BP reduction in severe uncomplicated hypertension is no longer considered the standard of care. The Veterans Administration Cooperative Study of patients with severe hypertension included 70 placebo-treated patients who had an average diastolic BP of 121 mm Hg at entry. Among these untreated patients, 27 experienced morbid events at a mean of 11 (plus or minus 2) months of follow-up. However, the earliest
P.262
morbid event occurred after 2 months. These data suggest that in patients with severe uncomplicated hypertension in which severe hypertension is not accompanied by evidence of malignant hypertension or acute end-organ dysfunction, eventual complications due to stroke, MI, or heart failure tend to occur over a time frame of months to years rather than hours to days. Although the long-term control of BP can clearly prevent these eventual complications, a hypertensive crisis cannot be diagnosed, because no evidence indicates that the acute reduction of BP results in an improvement in short- or long-term prognosis. Although the acute reduction of BP in patients with severe uncomplicated hypertension using sublingual nifedipine or oral clonidine loading was once the de facto standard of care, this practice was often an emotional response on the part of the treating physician to the dramatic elevation of BP, or it was motivated by the fear of medicolegal repercussions in the unlikely event of a hypertensive complication occurring within hours to days. Observing and documenting the dramatic fall in BP is a satisfying therapeutic maneuver, but no scientific basis for this approach exists. No literature supports the notion that some goal level of BP reduction must be achieved before the patient with severe uncomplicated hypertension leaves the acute care setting. In fact, the acute reduction of BP is often counterproductive, because it can produce untoward side effects that render the patient less likely to comply with long-term drug therapy. Instead, the acute therapeutic intervention should focus on tailoring an effective, well-tolerated maintenance antihypertensive regimen, with patient education regarding the chronic nature of the disease process and the importance of long-term compliance and medical follow-up. If the patientP.263
has simply run out of medicines, reinstitution of the previously effective drug regimen should suffice. If the patient is thought to be compliant with an existing drug regimen, a sensible change in the regimen, such as an increase in a suboptimal dosage of an existing drug or the addition of a drug of another class, is appropriate. In this regard, the addition of a low dose of a thiazide diuretic as a second-step agent to existing monotherapy with ACE inhibitor, ARB, CCB, beta-blocker, or central alpha-agonist is often remarkably effective. Another essential goal of the acute intervention should be to arrange suitable outpatient follow-up within a few days. A gradual reduction of BP to normotensive levels over a few days to a week should be accomplished in conjunction with frequent outpatient visits to modify the drug regimen and reinforce the importance of lifelong compliance with therapy. Although less dramatic than the acute reduction of BP in the acute care setting, this type of approach to the treatment of chronic hypertension is more likely to prevent long-term hypertensive complications and recurrent episodes of severe uncomplicated hypertension.
Suggested Readings
Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effects of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993;342:821 828.
ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomized to doxazosin vs. chlorthalidone: the antihypertensive and lipid-lowering to prevent heart attack trial (ALLHAT). JAMA 2000;238:1967 1975.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor, calcium channel blocker vs. diuretic. JAMA 2002;288:2981 2997.
American Diabetes Association. Treatment of hypertension in adults with diabetes. Diabetes Care 2003;26(Suppl 1):S80 S82.
-blocker Heart Attack Trial Research Group. A randomized trial of propranolol in patients with acute myocardial infarction, I: mortality results (BHAT). JAMA 1982;247:1707 1714.
Black HR, Elliott JW, Grandits G, et al. Principal results of the Controlled Onset Verapamil Investigation of Cardiovasculaar End Points (CONVINCE) trial. JAMA 2003;289:2073 2082.
Braunwald E, Antgman EM, Beasley JW, et al. AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction (ACC/AHA Post MI Guideline). J Am Coll Cardiol 2002;40:1366 1374.
Brenner BM, Copper ME de Zeeuq D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy (RENAAL). N Engl J Med 2001;345:861 869.
Capricorn Investigators. Effect of varvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: The CAPRICORN randomized trial. Lancet 2001;357:1358 1390.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of Hypertension. The JNC 7 report. JAMA 2003;289:2560 2572.
CIBIS Investigators and Committees. A randomized trial of beta-blockade in heart failure: the Cardiac Insufficiency Bisprolol Study (CIBIS). Circulation 1994;90:1765 1773.
Cohn J, Tognoni G. A randomized trial of the angiotensin receptor blocker valsartan in chronic heart failure (ValHEFT). N Engl J Med 2001;345:1667 1675.
Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint Reduction in Hypertension Study (LIFE). Lancet 2002;359:995 1003.
GISEN (Cruppo Italiano di Studi Epidemiologici in Nefrologia) Group. Randomized placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy (REIN). Lancet 1997;349:1857 1863.
P.264
Guyton AC, Manning RD, Norman RA, et al. Current concepts and perspectives of renal volume regulation in relationship to hypertension. J Hypertens 1986;4(Suppl 4):S49 S56.
Hager WD, Davis BR, Riba A, et al., for the Survival and Ventricular Enlargement (SAVE) Investigators. Absence of a deleterious effect of calcium channel blockers in patients with left ventricular dysfunction after myocardial infarction: the SAVE Study Experience. Am Heart J 1998;135:406 423.
Hall JE, Granger JP, Smith MJ, et al. Role of renal hemodynamics and arterial pressure in aldosterone escape. Hypertension 1984;6(Suppl 1):I183 I192.
Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril on cardiovascular events in high-risk patients (HOPE). N Engl J Med 2000;342:145 153.
Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult. J Am Coll Cardiol 2001;38:2101 2113.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Br Med J 1988;297:319 330.
Kober L, Torp-Pedersen C, Carlsen JE, et al., for Trandolapril Cardiac Evaluation (TRACE) Study Group. A clinical trial of the angiotensin-converting enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 1995;333:1670 1676.
Lewis EJ, Hunsicker LG, Bain RP, et al. The effect of angiotensin-converting enzyme inhibitor on diabetic nephropathy: the Collaborative Study Group (Captopril Trial). N Engl J Med 1993;329:1456 1462.
Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes (INDT). N Engl J Med 2001;345:851 860.
Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell 2001;104:545 556.
National Kidney Foundation Guideline. K/DOQI clinical practice guidelines for chronic kidney disease: Kidney Disease Outcome Quality Initiative. Am J Kidney Dis 2002;39(suppl 2):S1 S246.
Nolan CR. Hypertensive crises. In: RW Schrier, ed. Atlas of diseases of the kidney, Vol. 3. Philadelphia: Current Medicine, 1999.
Nolan CR. Malignant hypertension and other hypertensive crises. In: RW Schrier, ed. Diseases of the kidney and urinary tract, 7th ed. Boston: Lippincott Williams & Wilkins, 2001:1513 1592.
Nolan CR, Schrier RW. The kidney in hypertension. In: RW Schrier, ed. Renal and electrolyte disorders, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2003.
Packer M, Coats AJ, Fowler MB, et al. Effect of carvedolo on survival in severe chronic heart failure (COPERNICUS). N Engl J Med 2001;344:1651 1658.
Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction (EPHESUS). N Engl J Med 2003;348:1309 1321.
Pitt B, Zannad F, Remme WJ, et al., for Randomized Aldactone Evaluation Study Investigators. The effect of spironolactone on morbidity and mortality in patients with severe heart failure (RALES). N Engl J Med 1999;341:709 717.
PROGRESS Collaborative Study Group. Randomised trial of perindopril-based blood pressure lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet 2001;358:1033 1041.
Pstay BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. JAMA 1997;277:739 745.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991;265:3255 3264.
P.265
SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293 302.
Tepper D. Frontiers in congestive heart failure: effect of metoprolol CR/XL in chronic heart failure (MERIT-HF). Congest Heart Fail 1999;5:184 185.
UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 1998;317:713 720.
Wing LMH, Reid CM, Ryan P, et al., for Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly (ANBP2). N Engl J Med 2003;348:583 592.
Wright JT Jr., Agadoa L, Contreras G, et al. Successful blood pressure control in African American Study of Kidney Disease and Hypertension (AASK). Arch Intern Med 2002;162:1636 1643.