1 - Acute Resuscitation
Editors: Susla, Gregory M.; Suffredini, Anthony F.; McAreavey, Dorothea; Solomon, Michael A.; Hoffman, William D.; Nyquist, Paul; Ognibene, Frederick P.; Shelhamer, James H.; Masur, Henry
Title: Handbook of Critical Care Drug Therapy, 3rd Edition
Copyright 2006 Lippincott Williams & Wilkins
> Table of Contents > Chapter 1 - Acute Resuscitation
Chapter 1
Acute Resuscitation
TABLE 1.1. Advanced Cardiac Life Support (ACLS) Drugs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
P.5
P.6
TABLE 1.2. Shock General Management | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
P.7
TABLE 1.3. Hypovolemic Shock | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
P.8
TABLE 1.4. Crystalloids and Colloids | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
P.9
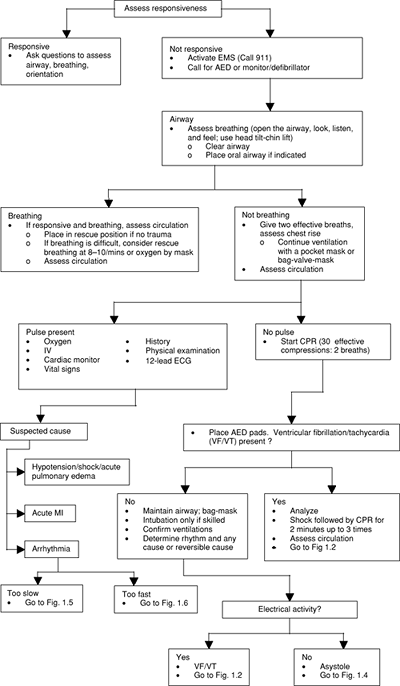 |
FIGURE 1.1. Universal Algorithm for Adult Emergency Cardiac Care AED, automatic external defibrillator; CPR, cardiopulmonary resuscitation; ECG, electro-cardiogram; EMS Emergency Management Service; IV, intravenous; MI, myocardial infarction ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Circulation 2000; 102: 8 Suppl I with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.10
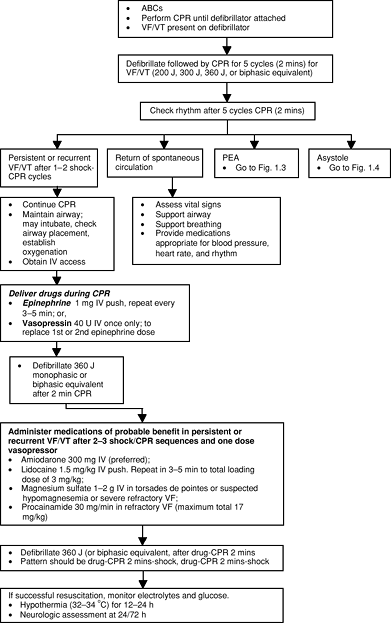 |
FIGURE 1.2. Algorithm for Ventricular Fibrillation (VF) and Pulseless Ventricular Tachycardia (VT) ABC, airway breathing circulation; CPR, cardiopulmonary resuscitation; IV, intravenous; PEA, pulseless electrical activity Give drugs typically at 3 5 minute intervals: Vasopressin 40 U IV single dose (wait 10 minutes before giving epinephrine) ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I, with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.11
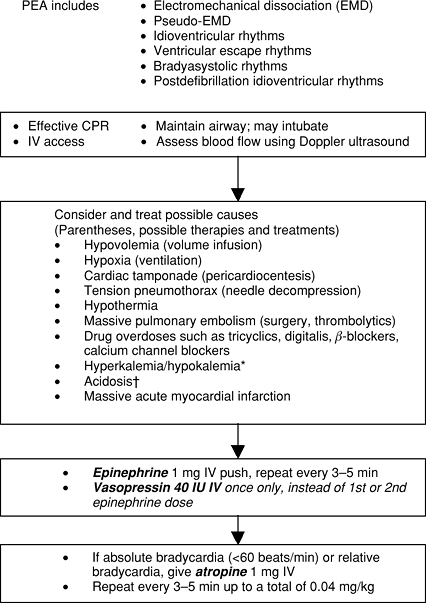 |
FIGURE 1.3. Algorithm for Pulseless Electrical Activity (PEA) CPR, cardiopulmonary resuscitation; EMD, electromechanical dissociation; IV, intravenous Class I: definitely helpful. Class IIa: acceptable, probably helpful. Class IIb: acceptable, possibly helpful. Class III: not indicated, may be harmful. *Sodium bicarbonate 1 mEq/kg: is Class I: if patient has known pre-existing hyperkalemia. Sodium bicarbonate 1 mEq/kg: Class IIa: if known pre-existing bicarbonate-responsive acidosis; if overdose with tricyclic antidepressants; to alkalinize the urine in drug overdoses. Class IIb: if intubated and long arrest interval; upon return to spontaneous circulation after long arrest interval. Class III: hypoxic lactic acidosis. ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.12
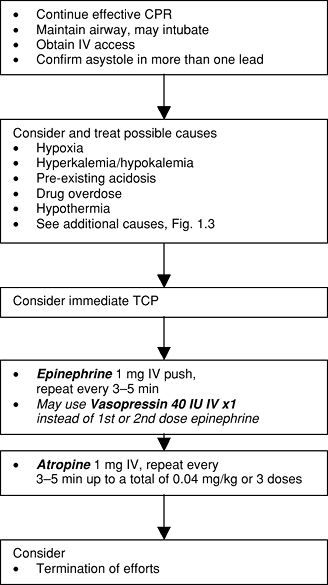 |
FIGURE 1.4. Asystole Treatment Algorithm CPR, cardiopulmonary resuscitation; IV, intravenous; TCP, transcutaneous pacing ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I, with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.13
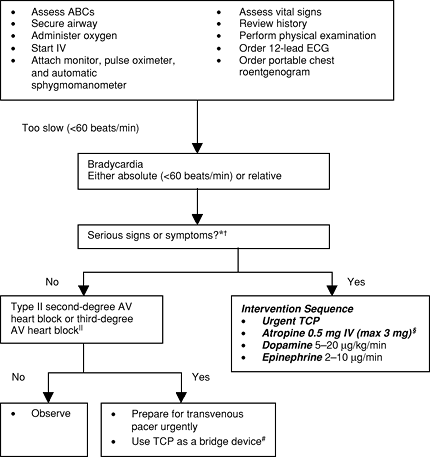 |
FIGURE 1.5. Bradycardia Algorithm (Patient not in Cardiac Arrest) ABC, airway breathing circulation; AV, atrioventricular; BP, blood pressure; ECG, electrocardiogram; HF, heart failure; IV, intravenous; MI, myocardial infarction; TCP, transcutaneous pacemaker *Serious signs or symptoms must be related to the slow rate. Clinical manifestations include: symptoms (chest pain, shortness of breath, decreased level of consciousness) and signs (low BP, shock, pulmonary congestion, HF, acute MI). Do not delay TCP while awaiting IV access or for atropine to take effect if patient is symptomatic. Atropine should be given in repeat doses in 3 5 minutes up to total of 0.04 mg/kg. Never treat third-degree heart block plus ventricular escape beats with lidocaine. #Verify patient tolerance and mechanical capture. Use analgesia and sedation as needed. ( The American Heart Association in Collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I, with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.14
P.15
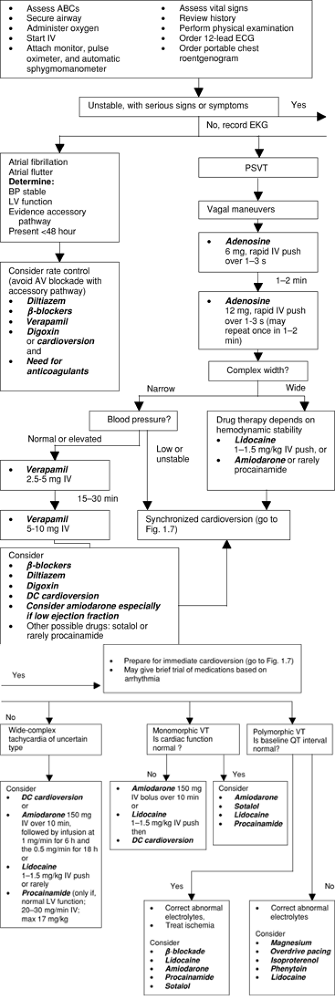 |
FIGURE 1.6. Tachycardia Algorithm ABC, airway breathing circulation; AV, atrioventricular; BP, blood pressure; DC, direct current; ECG, electrocardiogram; LV, left ventricular; PSVT, paroxysmal supraventricular tachycardia; VT, ventricular tachycardia ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I, with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
P.16
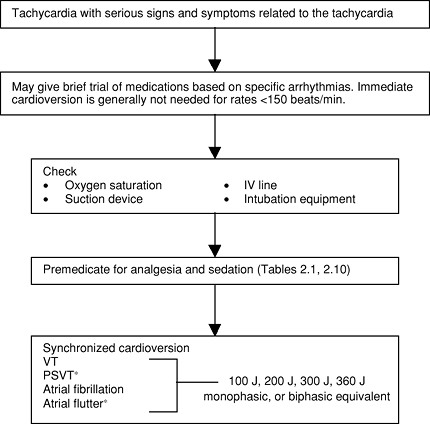 |
FIGURE 1.7. Electrical Cardioversion Algorithm (Patient not in Cardiac Arrest) IV, intravenous; VT, ventricular tachycardia *PSVT (paroxysmal supraventricular tachycardia) and atrial flutter often respond to lower energy levels (start with 50 J) ( The American Heart Association in collaboration with the International Liaison Committee on Resuscitation: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2000; 102: 8 Suppl I, with permission; also adapted from Circulation 2005;Suppl III:1 130. ) |
EAN: 2147483647
Pages: 19
- Chapter I e-Search: A Conceptual Framework of Online Consumer Behavior
- Chapter II Information Search on the Internet: A Causal Model
- Chapter X Converting Browsers to Buyers: Key Considerations in Designing Business-to-Consumer Web Sites
- Chapter XI User Satisfaction with Web Portals: An Empirical Study
- Chapter XII Web Design and E-Commerce