Magnetic Resonance Imaging
Authors: Flaherty, Alice W.; Rost, Natalia S.
Title: Massachusetts General Hospital Handbook of Neurology, The, 2nd Edition
Copyright 2007 Lippincott Williams & Wilkins
> Table of Contents > Imaging > Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI)
A. Indications
Posterior fossa or small supratentorial lesions, telling new from old strokes, white matter dz, nonacute seizure workup, AVMs. In practice, MRI is privileged as a gold standard, even for unnecessary indications such as NPH. For the indications for specific sequences, see Table 50.
B. What MRI is bad for
Unstable pts., fresh blood (except with susceptibility sequence), bone or calcium, cost containment.
C. Contraindications
Cardiac pacemakers.
Old aneurysm clips: I.e., ferromagnetic ones, e.g., Drake, Heifetz, Mayfield, Scoville. Modern clips are usually MRI compatible, including Olivecrona, Sugita, McFadden, and Yasargil.
Some cochlear implants: Verify their compatibility.
Other ferromagnetic foreign bodies in head: E.g., bullets.
Other implants: Staples, pumps, penile implants, joint prosthetics, spine rods, etc., are usually safe but should be verified.
Unstable pts.: This includes pts. who cannot lie flat because of aspiration risk, increased ICP.
Agitation, claustrophobia, or back pain: Premedicate with a neuroleptic, benzodiazepine, or opiate, respectively or combine them. Severe cases may need conscious sedation or intubation.
Big pts.: Pts. over 300 lb or girth >50 in. may not fit. Open MRIs may help but have worse image quality, especially of spine.
Contrast allergy? Rarely a problem. Gadolinium is safe for pts. with renal failure or CT contrast allergies.
Wrong imaging goal: E.g., calcium, fresh small bleeds (except with susceptibility sequence), bone or other minerals, cost containment.
D. MRI findings by appearance
Ring-enhancing lesions: MAGIC DR : Metastases, Abscess or aneurysm, Glioblastoma, Inflammation (resolving stroke, infection), Contusion (resolving), Demyelination (active), Radiation necrosis.
Gray-white junction lesions: Metastases, septic emboli, thrombosis, vasculitis.
Periventricular white matter lesions: MS, hypertensive or diabetic microvascular dz, toxoplasmosis, CNS lymphoma, CMV, lacunar infarcts, glioma.
Cerebellopontine angle lesions: SAME : Schwannoma, Arachnoid cyst, Meningioma, Epidermoid.
Basal ganglia lesions: Bleed, stroke, carbon monoxide, lead, methanol, CJD, TORCH infection, glioma, Fahr's dz.
E. MRI findings by cause
Abscess: T2/FLAIR hyperintense ring of edema and hypointense capsule, enhances with gadolinium. Bright on DWI and ADC.
ADEM: Multiple lesions both supra- and infratentorially, cortical and subcortical, and fluffy in appearance.
Amyloid angiopathy: Iron susceptibility sequence shows dark regions at sites of old bleeds (microhemorrhages).
Arteriovenous malformations: Serpiginous hyper- and hypodensities on T2/FLAIR MRI; tangle of vessels on MRA.
P.184
Table 51. Standard MRI sequences. They correspond to images in Figure 25.
Sequence Good For What's Bright What's Dark Comments T1-weighted Anatomy Fat, subacute bleed, protein, calcium, melanomas CSF, edema, bone, acute bleed; most T1 lesions are dark Most useful when compared with T1-gado T1 with gadolinium Highly perfused lesions Gado and T1-bright structures T1-dark structures except those with high perfusion To tell if scan is gado enhanced, look at cerebral veins or nasal mucosa T2-weighted Infarcts, inflamma- tion, tumors CSF, fluid, CVA, edema; most T2 lesions are bright Solids, calcium, intact RBCs, fer-ritin, he-mosiderin, muci-nous mets Good for CSF spaces FLAIR (fluid attenuated inversion recovery) Edema, gliosis, small WM lesions, anatomy Edema, gliosis, old strokes, subacute bleed CSF, hyperacute bleed Like T2 but dark CSF; also good for delineating small lesions near CSF spaces DWI (diffusion weighted) Acute ischemia (~30 min to 7 days) Acute stroke, abscess CSF-filled spaces Bright artifact at air-bone interface. T2 shine through : T2-bright signal mimics CVA ADC (apparent diffusion coefficient) Acute ischemia Edema, gliosis (including old strokes), CSF-filled spaces Acute ischemia (allows to differentiate T2 shine through) Calculated from DWI maps; ischemia seen from 30 min to 3-7 days P.185
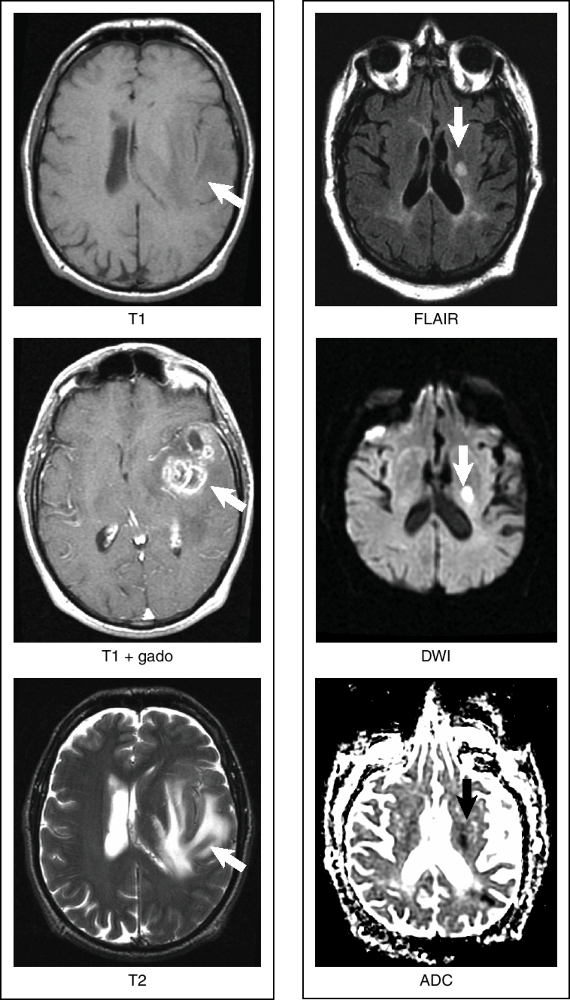
Figure 25. Standard MRI sequences. They correspond to row entries in Table 50; arrows point to pathology. Left: T1, T1+gado, and T2 scans of a tumor. Right: FLAIR, DWI, and ADC of an acute stroke.
P.186
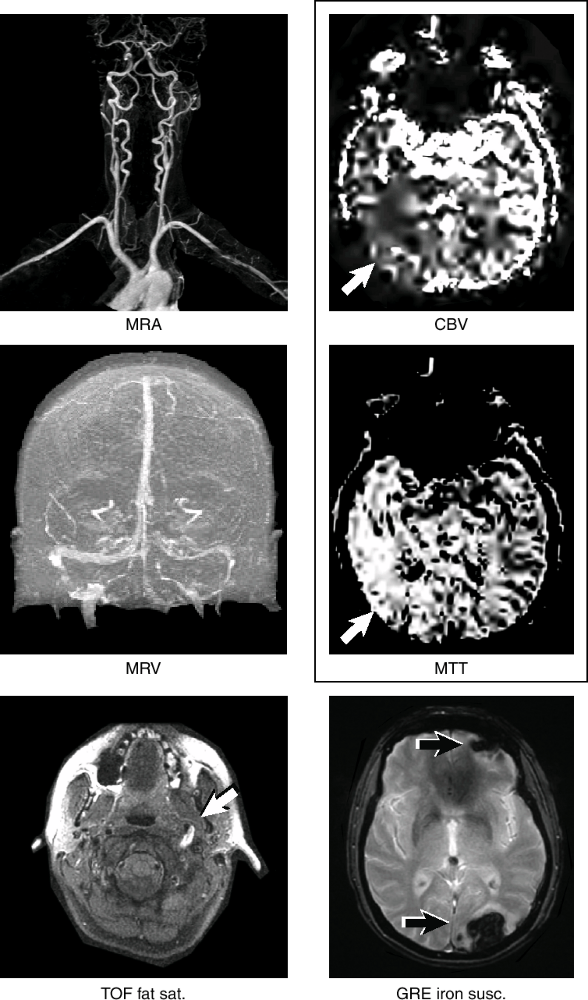
Figure 26. Additional MRI sequences. They correspond to row entries in Table 52. The MRA and MRV are gadolinium enhanced. The arrow in the fat sat sequence points to a carotid dissection. The grouped CBV and MTT sequences are from the same brain, and white arrows point to ischemia. The GRE iron sequence arrows point to hemorrhages.
P.187
Table 52. Additional MRI sequences.
Sequence Good For What's Bright What's Dark Comments MRA, MRV (either time of flight [TOF] or with gado) Extra- and intracranial flow Blood vessels (arteries or veins) Air, CSF TOF shows flow but may exaggerate stenosis; gado-enhanced flow gives better view TOF fat saturation ( fat sats ) Acute blood Vessel wall clot, e.g., dissection Fat, CSF (looks like a T1) Test of choice for carotid/ vertebral dissection Iron susceptibility (gradient echo [GRE]) Iron products, calcium CSF, gliosis, old strokes Blood products, calcium Helps tell blood from CT contrast; vessel cross-sections can look like tiny bleeds MR perfusion Diffusion-perfusion mismatch Ischemia on MTT and TTP maps Ischemia on CBV or CBF maps Watch for asymmetry on all maps to identify mismatch Functional MRI (not shown) Preoperative lesion localization High blood flow areas Low blood flow areas Shows blood flow's focal changes as area's activity changes MR spectroscopy (not shown) Tumors, metabolic disorders, strokes N/A N/A Spectrum reads R L: lipid, lactate, NAA, creatinine, choline, myoinositol Brainstem lesion: Request thin cuts through the brainstem.
Carotid or vertebral artery lesion:
Stenosis: MRA of neck and head. Few false negatives but frequent false positives.
Dissection: Get TOF fat saturation and MRA. 90% sensitive.
Chiasm/optic nerve/middle fossa problem: Order gadolinium and fat suppression, with coronal cuts through orbit and middle fossa.
Edema: Bright T2 and FLAIR.
Hemorrhage dating: Complicated. CT is better for fresh blood. Dating uses hemoglobin's oxidation. The clot oxidizes from the outside in, giving a ring appearance at some stages.
Table 53. Intracerebral hemorrhage dating by MRI: principle, sequences, and the world's most famous mnemonic on MR blood aging.
Blood Age Oxidation T1 T2 Mnemonic 1-3 days DeoxyHb (i) Isodense Dark Iddy 3-7 days MetHb (i) Bright Dark Biddy 7-14 days MetHb (e) Bright Bright BaBy >14 days Hemosiderin (e) Dark Dark Doodoo 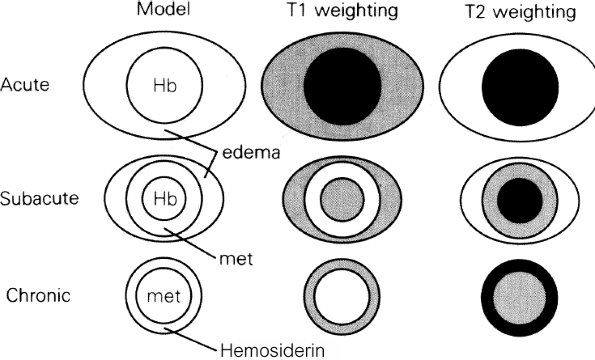
Figure 27. Variation with age of bleed appearance on MRI. (From Berlit P. Memorix Neurology. London: Chapman and Hall, 1996, with permission.)
Infarct: See also Figure 5, p. 27.
Acute and subacute infarcts: Diffusion-weighted image (DWI) is bright and ADC is dark within 30 min and for 2 wk post stroke. ADC dark signal resolves by 2-7 days. After 4-12 h, see bright T2, bright FLAIR, bright proton density, dark T1. There may be edema or punctate hemorrhage associated with subacute infarcts.
Chronic infarcts: Similar to subacute infarcts except that they are not bright on DWI/or dark on ADC, and may show tissue loss or cavitation rather than edema or hemorrhagic conversion.
Multiple sclerosis: T2-bright white matter lesions, usually periventricular, with long axis perpendicular to ventricles (Dawson's fingers). Acute plaques may ring enhance.
Spinal vertebral disc herniation: See Figure 28. On T2 images, compressed discs are darker. They bulge into CSF (bright) and sometimes spinal cord (grey). Axial cuts show nerve root impingement best.
P.189
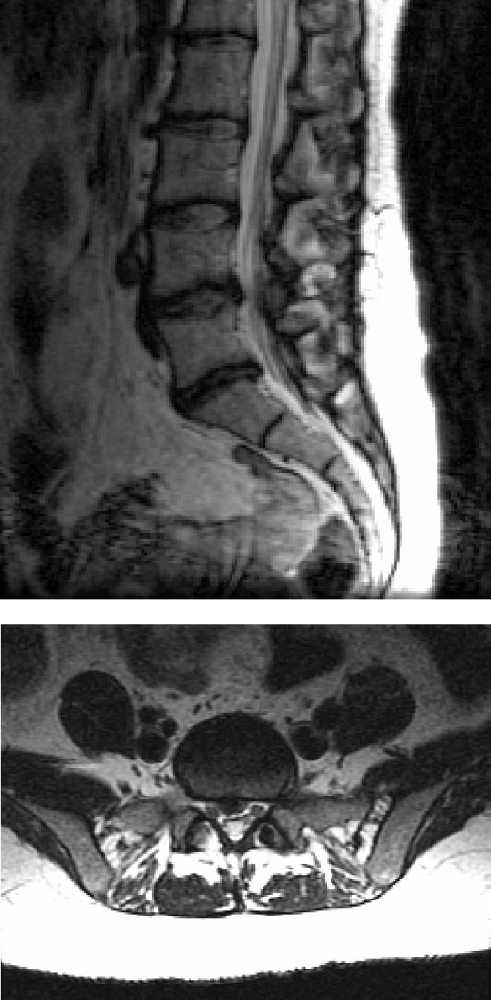
Figure 28. Parasagittal and axial T2-weighted MRI images show a right paracentral disc herniation towards the proximal right S1 nerve root.
Spinal tumor: Multiple lesions are common, so order a longitudinal scout of entire spine. Consider gadolinium.
Intramedullary: Astrocytoma, ependymoma.
Intradural: Nerve sheath tumor, meningioma, lymphoma.
Extradural: Metastases, bone tumor.
Tumor, brain: T1 and T2 density will vary with tumor type, presence of hemorrhage, etc. Look for hydrocephalus, shift, necrosis, enhancement, edema. See also Tumors of Brain, p. 120.
Gray-white junction mass: Usually metastasis.
Hemorrhagic mass: suggests GBM, metastasis (renal cell CA, melanoma, thyroid, choriocarcinoma).
Calcification: suggests oligodendroglioma, meningioma, AVM.
Lymphoma: Little edema, often subcortical, often travels across corpus callosum ( butterfly appearance ). Enhancement is usually homogeneous, but in AIDS, may ring enhance and look like toxoplasmosis.
Glioma: May have heterogeneous appearance, surrounded by significant edema with mass effect. May travel across corpus callosum. Gadolinium enhancing. Rarely multifocal.
Meningioma: Extra-axial, usually dark on T2, enhances uniformly ( light bulb sign ).
Pituitary tumor: Get MRI with thin cuts thru sella. To see microadenoma, scan must be done within 5 min of gadolinium (normal pituitary enhances immediately, but microadenoma takes about 30 min).
Post-op scans: Do within 48 h to see residual tumor before inflammation begins. Post-op pituitary scans are rarely helpful.
P.188
P.190
EAN: 2147483647
Pages: 109