9. Gastrointestinal Tract
Authors: Dahnert, Wolfgang
Title: Radiology Review Manual, 6th Edition
Copyright 2007 Lippincott Williams & Wilkins
> Table of Contents > Gastrointestinal Tract
function show_scrollbar() {}
Gastrointestinal Tract
Differential Diagnosis of Gastrointestinal Disorders
Acute Abdomen in Child
Intussusception
Appendicitis
Obstruction (previous surgery, hernia)
Acute gastroenteritis
Basilar pneumonia
Gastrointestinal Hemorrhage
| Mortality: | approx. 10% |
 Barium examination should be avoided in acute bleeders!
Barium examination should be avoided in acute bleeders!
Source:
UPPER GASTROINTESTINAL HEMORRHAGE
= bleeding site proximal to ligament of Treitz
@ Esophagogastric junction
Esophageal varices (17%): 50% mortality
Mallory-Weiss syndrome (7 14%): very low mortality
@ Stomach
Acute hemorrhagic gastritis (17 27%)
Gastric ulcer (10%)
Pyloroduodenal ulcer (17 25%)
Mortality: <10% if under age 60; >35% if over age 60 @ Other causes (14%):
visceral artery aneurysm, vascular malformation, neoplasm, vascular-enteric fistula
Average mortality: 8 10% Rx:
Transcatheter embolization (method of choice) abundant collaterals except for postoperative stomach
Intraarterial vasopressin infusion (0.2 0.4 U/min)
Prognosis: controls 73% of gastric mucosal bleeding; high recurrence rate
LOWER GASTROINTESTINAL HEMORRHAGE
= bleeding site distal to ligament of Treitz
@ Small intestine
tumor (eg, leiomyoma, hemangioma, metastases), ulcers, diverticula (eg, Meckel diverticulum), inflammatory bowel disease (eg, Crohn disease), vascular malformation, visceral artery aneurysm, aortoenteric fistula
@ Colorectal (70%)
massive bleeding
Diverticula (most common): hemorrhage in 25% of patients with diverticulosis; spontaneous cessation of bleeding in 80%; recurrent bleeding in 25%
Colonic angiodysplasia (2nd most common cause) = most common vascular lesion; self limiting
Biopsy
low-rate bleeding
Inflammatory bowel disease
Benign/malignant tumor
Mesenteric varices
Rx:
Intraarterial vasopressin infusion
Prognosis: 90% initial control rate; in 30% recurrent bleeding Transcatheter embolization
Requires superselective catheterization using microcatheters + microembolic agents
Cx: 25% risk of bowel infarction + stricture
Gastrointestinal Bleeding in Infant
Peptic ulcer
Varices
Ulcerated Meckel diverticulum
Gastrointestinal Bleeding in Child
Meckel diverticulum
Juvenile polyp
Inflammatory bowel disease
Clotting disorder
Arteriovenous malformation
Intramural Hemorrhage
VASCULITIS
Henoch-Sch nlein purpura
TRAUMA
COAGULATION DEFECT
Anticoagulant therapy
Thrombocytopenia
Disseminated intravascular coagulation
DISEASES WITH COAGULATION DEFECT
Hemophilia
Leukemia, lymphoma
Multiple myeloma
Metastatic carcinoma
Idiopathic thrombocytopenic purpura
ISCHEMIA (often fatal)
abdominal pain
melena
| Site: | submucosal/intramural/mesenteric |
 stacked coin / picket fence appearance of mucosal folds (due to symmetric infiltration of submucosal blood)
stacked coin / picket fence appearance of mucosal folds (due to symmetric infiltration of submucosal blood) thumbprinting = rounded polypoid filling defect (due to focal accumulation of hematoma in bowel wall)
thumbprinting = rounded polypoid filling defect (due to focal accumulation of hematoma in bowel wall) separation + uncoiling of bowel loops
separation + uncoiling of bowel loops narrowing of lumen + localized filling defects (asymmetric hematoma)
narrowing of lumen + localized filling defects (asymmetric hematoma) no spasm/irritability
no spasm/irritability mechanical obstruction + proximal distension of loops
mechanical obstruction + proximal distension of loops
| Prognosis: | resolution within 2 6 weeks |
GI Abnormalities In Chronic Renal Failure And Renal Transplantation
@ Esophagus
Esophagitis: candida, CMV, herpes
@ Stomach & duodenum
Gastritis
 thickened gastric folds (38%)
thickened gastric folds (38%) edema + erosions
edema + erosionsCause:
imbalance of gastrin levels + gastric acid secretion due to
reduced removal of gastrin from kidney with loss of cortical mass
impaired acid feedback mechanism
hypochlorhydria
opportunistic infection (eg, CMV)
Gastric ulcer (3.5%)
Duodenal ulcer (2.4%)
Duodenitis (47%)
@ Colon
More severely + frequently affected after renal transplantation
Progressive distention + pseudoobstruction
Contributing factors: dehydration, alteration of diet, inactivity, nonabsorbable antacids, high-dose steroids Ischemic colitis
primary disease responsible for end-stage renal disease (eg, diabetes, vasculitis)
trauma of renal transplantation
Diverticulitis
Contributing factors: chronic obstipation, steroids, autonomic nervous dysfunction Pseudomembranous colitis
Uremic colitis = nonspecific colitis
Spontaneous colonic perforation
Cause: nonocclusive ischemia, diverticula, duodenal + gastric ulcers
@ Pancreas
Pancreatitis
Cause: hypercalcemia, steroids, infection, immunosuppressive agents, trauma
@ General
GI hemorrhage
Cause: gastritis, ulcers, colonic diverticula, ischemic bowel, infectious colitis, pseudomembranous colitis, nonspecific cecal ulceration Bowel perforation (in 1 4% of transplant recipients)
Opportunistic infection
Organism: Candida, herpes, CMV, Strongyloides Malignancy
skin tumors
lymphoma
P.754
Enteropathy
Protein-Losing Enteropathy
DISEASE WITH MUCOSAL ULCERATION
Carcinoma
Lymphoma
Inflammatory bowel disease
Peptic ulcer disease
HYPERTROPHIED GASTRIC RUGAE
M n trier disease
NONULCERATIVE MUCOSAL DISEASE
Celiac disease
Tropical sprue
Whipple disease
Allergic gastroenteropathy
Gastrocolic fistula
Villous adenoma of colon
LYMPHATIC OBSTRUCTION
Intestinal lymphangiectasia
HEART DISEASE
Constrictive pericarditis
Tricuspid insufficiency
Malabsorption
= deficient absorption of any essential food materials within small bowel
PRIMARY MALABSORPTION
= the digestive abnormality is the only abnormality present
Celiac disease = nontropical sprue
Tropical sprue
Disaccharidase deficiencies
SECONDARY MALABSORPTION
= occurring during course of gastrointestinal disease
enteric
Whipple disease
Parasites: hookworm, Giardia, fish tapeworm
Mechanical defects: fistulas, blind loops, adhesions, volvulus, short circuits
Neurologic: diabetes, functional diarrhea
Inflammatory: enteritis (viral, bacterial, fungal, nonspecific)
Endocrine: Zollinger-Ellison syndrome
Drugs: neomycin, phenindione, cathartics
Collagen disease: scleroderma, lupus, polyarteritis
Lymphoma
Benign + malignant small bowel tumors
Vascular disease
CHF, agammaglobulinemia, amyloid, abetalipoproteinemia, intestinal lymphangiectasia
gastric
vagotomy, gastrectomy, pyloroplasty, gastric fistula (to jejunum, ileum, colon)
pancreatic
pancreatitis, pancreatectomy, pancreatic cancer, cystic fibrosis
hepatobiliary
intra- and extra-hepatic biliary obstruction, acute + chronic liver disease
Roentgenographic Signs in Malabsorption
 SMALL BOWEL WITH NORMAL FOLDS + FLUID
SMALL BOWEL WITH NORMAL FOLDS + FLUIDMaldigestion (deficiency of bile salt/pancreatic enzymes)
Gastric surgery
Alactasia
 SMALL BOWEL WITH NORMAL FOLDS + WET
SMALL BOWEL WITH NORMAL FOLDS + WETSprue
Dermatitis herpetiformis
 DILATED DRY SMALL BOWEL
DILATED DRY SMALL BOWELScleroderma
Dermatomyositis
Pseudoobstruction: no peristaltic activity
 DILATED WET SMALL BOWEL
DILATED WET SMALL BOWELSprue
Obstruction
Blind loop
 THICKENED STRAIGHT FOLDS + DRY SMALL BOWEL
THICKENED STRAIGHT FOLDS + DRY SMALL BOWELAmyloidosis (malabsorption is unusual)
Radiation
Ischemia
Lymphoma (rare)
Macroglobulinemia (rare)
 THICKENED STRAIGHT FOLDS + WET SMALL BOWEL
THICKENED STRAIGHT FOLDS + WET SMALL BOWELZollinger-Ellison syndrome
Abetalipoproteinemia: rare inherited disease characterized by CNS damage, retinal abnormalities, steatorrhea, acanthocytosis
 THICKENED NODULAR IRREGULAR FOLDS + DRY SMALL BOWEL
THICKENED NODULAR IRREGULAR FOLDS + DRY SMALL BOWELLymphoid hyperplasia
Lymphoma
Crohn disease
Whipple disease
Mastocytosis
 THICKENED NODULAR IRREGULAR FOLDS + WET SMALL BOWEL
THICKENED NODULAR IRREGULAR FOLDS + WET SMALL BOWELLymphangiectasia
Giardiasis
Whipple disease (rare)
P.755
Small Bowel Nodularity with Malabsorption
| mnemonic: | What is His Main Aim? Lay Eggs, By God |
W hipple disease
I ntestinal lymphangiectasia
H istiocytosis
M astocytosis
A myloidosis
L ymphoma, L ymph node hyperplasia
E dema
B lood
G iardiasis
Abdominal Mass
Abdominal Mass in Neonate
RENAL (55%)
Hydronephrosis (25%)
Multicystic dysplastic kidney (15%)
Polycystic kidney
Mesoblastic nephroma
Renal vein thrombosis
GENITAL (15%)
Ovarian cyst
Hydrometrocolpos
GASTROINTESTINAL (15%)
Duplication
Volvulus
Cystic meconium peritonitis
Mesenteric cyst
NONRENAL RETROPERITONEAL (10%)
Adrenal hemorrhage
Neuroblastoma
Teratoma
HEPATOBILIARY (5%)
Hemangioendothelioma
Choledochal cyst
Hydrops of gallbladder
Abdominal Mass in Infant &Child
RENAL (55%)
Wilms tumor (22%)
Hydronephrosis (20%)
Cystic renal mass
Congenital anomaly
NONRENAL RETROPERITONEAL (23%)
Neuroblastoma (21%)
Teratoma
GASTROINTESTINAL (18%)
Appendiceal abscess (10%)
Hepatobiliary (6%)
GENITAL (4%)
Ovarian cyst/teratoma
Hydrometrocolpos
Abnormal Intraabdominal Air
Abnormal Air Collection
Abnormally located bowel
Chilaiditi syndrome (= colon interposed between liver and chest wall), inguinal hernia
Pneumoperitoneum
Retropneumoperitoneum
perforation of duodenum/rectum/ascending + descending colon, diverticulitis, ulcerative disease, endoscopic procedure
Gas in bowel wall
gastric pneumatosis, phlegmonous gastritis, endoscopy, rupture of lung bulla
Gas within abscess
located in subphrenic, renal, perirenal, hepatic, pancreatic space, lesser sac
Gas in biliary system = pneumobilia
Gas in portal venous system
Pneumoperitoneum
Cause:
DISRUPTION OF WALL OF HOLLOW VISCUS
trauma
iatrogenic perforation
diseases of GI tract
Perforated gastric/duodenal ulcer
Perforated appendix
Ingested foreign-body perforation
Diverticulitis (ruptured Meckel diverticulum/sigmoid diverticulum, jejunal diverticulosis)
Necrotizing enterocolitis with perforation
Inflammatory bowel disease (eg, toxic megacolon)
Obstruction (gas traversing intact mucosa): neoplasm, imperforate anus, Hirschsprung disease, meconium ileus
Ruptured pneumatosis cystoides intestinalis with balanced pneumoperitoneum (= free intraperitoneal air acts as tamponade of pneumatosis cysts thus maintaining a balance between intracystic air + pneumoperitoneum)
Idiopathic gastric perforation = spontaneous perforation in premature infants (congenital gastric muscular wall defect)
P.756
THROUGH PERITONEAL SURFACE
transperitoneal manipulation
Abdominal needle biopsy/catheter placement
Mistaken thoracentesis/chest tube placement
Endoscopic biopsy
extension from chest
Dissection from pneumomediastinum (positive pressure breathing, rupture of bulla/bleb, chest surgery)
Bronchopleural fistula
rupture of urinary bladder
penetrating abdominal injury
THROUGH FEMALE GENITAL TRACT
iatrogenic
Perforation of uterus/vagina
Culdocentesis
Rubin test = tubal patency test
Pelvic examination
spontaneous
Intercourse, orogenital insufflation
Douching
Knee-chest exercise, water skiing, horseback riding
INTRAPERITONEAL
Gas-forming peritonitis
Rupture of abscess
| Note | = asymptomatic spontaneous pneumoperitoneum without peritonitis |
 air in lesser peritoneal sac
air in lesser peritoneal sac gas in scrotum (through open processus vaginalis)
gas in scrotum (through open processus vaginalis) Large collection of gas:
Large collection of gas: abdominal distension, no gastric air-fluid level
abdominal distension, no gastric air-fluid level football sign = large pneumoperitoneum outlining entire abdominal cavity
football sign = large pneumoperitoneum outlining entire abdominal cavity double wall sign = Rigler sign = bas-relief sign
double wall sign = Rigler sign = bas-relief sign  = air outlining the luminal + serosal surface of the bowel wall with patient in supine position (usually requires >1,000 mL of free intraperitoneal gas + intraperitoneal fluid)
= air outlining the luminal + serosal surface of the bowel wall with patient in supine position (usually requires >1,000 mL of free intraperitoneal gas + intraperitoneal fluid)[Leo Rigler (1896 1979), radiologist in Minneapolis, USA]
 telltale triangle sign = triangular air pocket between 3 loops of bowel
telltale triangle sign = triangular air pocket between 3 loops of bowel depiction of diaphragmatic muscle slips = two or three 6 13-cm long and 8 10-mm wide arcuate soft-tissue bands directed vertically inferiorly + arching parallel to diaphragmatic dome superiorly
depiction of diaphragmatic muscle slips = two or three 6 13-cm long and 8 10-mm wide arcuate soft-tissue bands directed vertically inferiorly + arching parallel to diaphragmatic dome superiorly outline of ligaments of anterior inferior abdominal wall:
outline of ligaments of anterior inferior abdominal wall: inverted V sign = outline of both lateral umbilical ligaments (containing inferior epigastric vessels)
inverted V sign = outline of both lateral umbilical ligaments (containing inferior epigastric vessels) outline of medial umbilical ligaments (obliterated umbilical arteries)
outline of medial umbilical ligaments (obliterated umbilical arteries) urachus sign = outline of middle umbilical ligament
urachus sign = outline of middle umbilical ligament
RUQ gas (best place to look for small collections):
 single large area of hyperlucency over the liver
single large area of hyperlucency over the liver oblique linear area of hyperlucency outlining the posteroinferior margin of liver
oblique linear area of hyperlucency outlining the posteroinferior margin of liver doge's cap sign = triangular collection of gas in Morison pouch (posterior hepatorenal space)
doge's cap sign = triangular collection of gas in Morison pouch (posterior hepatorenal space) outline of falciform ligament = long vertical line to the right of midline extending from ligamentum teres notch to umbilicus; most common structure outlined
outline of falciform ligament = long vertical line to the right of midline extending from ligamentum teres notch to umbilicus; most common structure outlined ligamentum teres sign = air outlining fissure of ligamentum teres hepatis (= posterior free edge of falciform ligament) seen as vertically oriented sharply defined slitlike/oval area of hyperlucency between 10th and 12th rib within 2.5 4.0 cm of right vertebral border 2 7 mm wide and 6 20 mm long
ligamentum teres sign = air outlining fissure of ligamentum teres hepatis (= posterior free edge of falciform ligament) seen as vertically oriented sharply defined slitlike/oval area of hyperlucency between 10th and 12th rib within 2.5 4.0 cm of right vertebral border 2 7 mm wide and 6 20 mm long ligamentum teres notch = inverted V-shaped area of hyperlucency along undersurface of liver
ligamentum teres notch = inverted V-shaped area of hyperlucency along undersurface of liver saddlebag/mustache/cupola sign = gas trapped below central tendon of diaphragm
saddlebag/mustache/cupola sign = gas trapped below central tendon of diaphragm parahepatic air = gas bubble lateral to right edge of liver
parahepatic air = gas bubble lateral to right edge of liver
Iatrogenic Pneumoperitoneum
Laparotomy/laparoscopy (58%)
absorbed in 1 24 days dependent on initial amount of air introduced and body habitus (80% in asthenic, 25% in obese patients)
 After 3 days free air should be followed with suspicion!
After 3 days free air should be followed with suspicion!
Leaking surgical anastomosis
Peritoneal dialysis
Feeding tube placement
Endoscopic perforation
Enema tip injury
Use of gynecologic instruments
Vigorous respiratory resuscitation
Diagnostic pneumoperitoneum
Spontaneous Pneumoperitoneum
Peptic perforation
Ischemia
Bowel obstruction
Toxic megacolon
Inflammation: appendicitis, tuberculosis, necrotizing enteroccolitis
Traumatic Pneumoperitoneum
Blunt trauma
Penetrating trauma:
Perforating foreign body (eg, thermometer injury to rectum, vaginal stimulator in rectum)
Compressor air directed toward anus
Miscellaneous Causes of Pneumoperitoneum
Drugs: steroids, NSAID
Pneumatosis coli/intestinalis
Entry through female genital tract: douching, sexual intercourse, insufflation
P.757
Pseudopneumoperitoneum
= process mimicking free air
ABDOMINAL GAS
gastrointestinal gas
Pseudo-wall sign = apposition of gas-distended bowel loops
Chilaiditi syndrome
Diaphragmatic hernia
Diverticulum of esophagus/stomach/duodenum
extraintestinal gas
Retroperitoneal air
Subdiaphragmatic abscess
CHEST
Pneumothorax
Empyema
Irregularity of diaphragm
FAT
Subdiaphragmatic intraperitoneal fat
Interposition of omental fat between liver + diaphragm
Pneumoretroperitoneum
Cause:
Traumatic rupture (usually duodenum)
Perforation of duodenal ulcer
Gas abscess of pancreas (usually extends into lesser sac)
Urinary tract gas (trauma, infection)
Dissected mediastinal air
 kidney outlined by gas
kidney outlined by gas outline of psoas margin gas streaks in muscle bundles
outline of psoas margin gas streaks in muscle bundles
Pneumatosis Intestinalis
= PNEUMATOSIS CYSTOIDES INTESTINALIS = BULLOUS EMPHYSEMA OF THE INTESTINE = INTESTINAL GAS CYSTS = PERITONEAL LYMPHOPNEUMATOSIS
Cause:
 Attributed to at least 58 causative factors!
Attributed to at least 58 causative factors!
BOWEL NECROSIS/GANGRENE
 Most common + life-threatening cause!
Most common + life-threatening cause!
Pathogenesis: damage + disruption of mucosa with entry of gas-forming bacteria into bowel wall (cysts contain 50% hydrogen = evidence of bacterial origin) necrotizing enterocolitis, ischemia + infarction (mesenteric thrombosis), neutropenic colitis, sepsis, volvulus, emphysematous gastritis, caustic ingestion
MUCOSAL DISRUPTION
Pathogenesis: increased intestinal gas pressure leads to overdistension and dissection of gas into bowel wall intestinal obstruction:
pyloric stenosis, annular pancreas, imperforate anus, Hirschsprung disease, meconium plug syndrome, obstructing neoplasm
intestinal trauma:
endoscopy biopsy, biliary stent perforation, sclerotherapy, bowel surgery, postoperative bowel anastomosis, penetrating/blunt abdominal trauma, trauma of child abuse, intracatheter jejunal feeding tube, barium enema
infection/inflammation:
peptic ulcer disease, intestinal parasites, tuberculosis, peritonitis, inflammatory bowel disease (Crohn disease, ulcerative colitis, pseudomembranous colitis), ruptured jejunal diverticula, Whipple disease, systemic amyloidosis
INCREASED MUCOSAL PERMEABILITY
Pathogenesis: defects in lymphoid tissue of bowel wall allows bacterial gas to enter bowel wall immunotherapy:
graft-versus-host disease, organ transplantation, bone marrow transplantation
others:
AIDS enterocolitides, steroid therapy, chemotherapy, radiation therapy, collagen vascular disease (scleroderma, systemic lupus erythematosus, periarteritis dermatomyositis), intestinal bypass enteropathy, diabetes mellitus
PULMONARY DISEASE
Pathogenesis: alveolar rupture with air dissecting interstitially along bronchovascular bundles to mediastinum + retroperitoneally along vascular supply of viscera Cause: Chronic obstructive pulmonary disease (chronic bronchitis, emphysema, bullous disease of lung), asthma, cystic fibrosis, chest trauma (barotrauma from artificial ventilation, chest tube), increased intrathoracic pressure associated with retching + vomiting
Path: (a) microvesicular type = 10 100-mm cysts/bubbles within lamina propria
(b) linear/curvilinear type = streaks of gas oriented parallel to bowel wallLocation: any part of GI tract; may be discontinuous with spread to distant sites along mesentery Site: subserosa > submucosa > muscularis > mesentery; mesenteric side >> antimesenteric side  radiolucent clusters of cysts along contour of bowel wall (best demonstrated on CT)
radiolucent clusters of cysts along contour of bowel wall (best demonstrated on CT) segmental mucosal nodularity (DDx: polyposis)
segmental mucosal nodularity (DDx: polyposis) pneumoperitoneum/pneumoretroperitoneum (asymptomatic large pneumoperitoneum may persist for months/years)
pneumoperitoneum/pneumoretroperitoneum (asymptomatic large pneumoperitoneum may persist for months/years) gas in mesenteric + portal vein
gas in mesenteric + portal veinPrognosis:
wide spectrum from innocuous to fatal; clinical outcome impossible to predict based on x-ray findings
 Linear gas collections probably have a more severe connotation
Linear gas collections probably have a more severe connotation Pneumatosis of the colon is likely clinically insignificant
Pneumatosis of the colon is likely clinically insignificant Extent of pneumatosis is inversely related to severity of disease
Extent of pneumatosis is inversely related to severity of disease
Soap-bubble Appearance in Abdomen of Neonate
Feces in infant fed by mouth
Meconium ileus:
gas mixed with meconium, usually RLQ
Meconium plug:
gas in and around plug, in distribution of colon
Necrotizing enterocolitis: submucosal pneumatosis
Atresia/severe stenosis: pneumatosis
Hirschsprung disease:
impacted stool, sometimes pneumatosis
P.758
Abdominal Calcifications & Opacities
Opaque Material in Bowel
| mnemonic: | CHIPS |
C hloral hydrate
H eavy metals (lead)
I ron
P henothiazines
S alicylates
Diffuse Abdominal Calcifications
Cystadenoma of ovary
 granular, sandlike psammomatous calcifications
granular, sandlike psammomatous calcifications
Pseudomyxoma peritonei
pseudomucinous adenoma of ovary
mucocele of appendix
Undifferentiated abdominal malignancy
Tuberculous peritonitis
 mottled calcifications simulating residual barium
mottled calcifications simulating residual barium
Meconium peritonitis
Oil granuloma
 annular/plaquelike calcifications
annular/plaquelike calcifications
Focal Alimentary Tract Calcifications
ENTEROLITHS
Appendicolith: in 10 15% of acute appendicitis
Stone in Meckel diverticulum
Diverticular stone
Rectal stone
Proximal to partial obstruction (eg, tuberculosis, Crohn disease)
MESENTERIC CALCIFICATIONS
Dystrophic calcification of omental fat deposits + appendices epiploicae (secondary to infarction/pancreatitis/TB)
Cysts: mesenteric cyst, hydatid cyst
Calcified mesenteric lipoma
INGESTED FOREIGN BODIES
trapped in appendix, diverticula, proximal to stricture
1. Calcified seeds + pits (bezoar)
2. Birdshot
Location of intraluminal lodgement:
esophagus (68%), stomach (11.6%), small bowel (3.3%), colon (11.6%)
TUMOR
Mucocele of appendix
 crescent-shaped/circular calcification
crescent-shaped/circular calcification
Mucinous adenocarcinoma of stomach/colon
= COLLOID CARCINOMA
 small mottled/punctate calcifications in primary site in regional lymph node metastases, adjacent omentum, metastatic liver foci
small mottled/punctate calcifications in primary site in regional lymph node metastases, adjacent omentum, metastatic liver foci
Gastric/esophageal leiomyoma: calcifies in 4%
Lipoma
Abdominal Wall Calcifications
IN SOFT TISSUES
Hypercalcemic states
Idiopathic calcinosis
IN MUSCLE
parasites:
Cysticercosis = Taenia solium
 round/slightly elongated calcifications
round/slightly elongated calcifications
Guinea worm = dracunculiasis
 stringlike calcifications up to 12 cm long
stringlike calcifications up to 12 cm long
injection sites
from quinine, bismuth, calcium gluconate, calcium penicillin
myositis ossificans
IN SKIN
Soft-tissue nodules: papilloma, neurofibroma, melanoma, nevi
Scar:
 linear density
linear density
Colostomy/ileostomy
Tattoo markings
Abdominal Vascular Calcifications
ARTERIES
Atheromatous plaques
Arterial calcifications in diabetes mellitus
VEINS
phleboliths = calcified thrombus, generally seen below interspinous line
Normal/varicose veins
Hemangioma
LYMPH NODES
Histoplasmosis/tuberculosis
Chronic granulomatous disease
Residual lymphographic contrast
Silicosis
Abnormal Intraabdominal Fluid
Ascites
Cause:
TRANSUDATE
Cirrhosis (75%): poor prognostic sign
Hypoproteinemia
CHF
Constrictive pericarditis
Chronic renal failure
Budd-Chiari syndrome
EXUDATE
Carcinomatosis
Polyserositis
TB peritonitis
Pancreatitis
Meigs syndrome
HEMORRHAGIC/CHYLOUS FLUID
Early signs (accumulation in pelvis):
 round central density in pelvis + ill-defined bladder top
round central density in pelvis + ill-defined bladder top thickening of peritoneal flank stripe
thickening of peritoneal flank stripe space between properitoneal fat and gut >3 mm
space between properitoneal fat and gut >3 mm
P.759
Late signs:
 Hellmer sign = medial displacement of lateral liver margins
Hellmer sign = medial displacement of lateral liver margins medial displacement of ascending + descending colon
medial displacement of ascending + descending colon obliteration of hepatic + splenic angles
obliteration of hepatic + splenic angles bulging flanks
bulging flanks gray abdomen
gray abdomen floating centralized loops
floating centralized loops separation of loops
separation of loops
High-density Ascites
Tuberculosis: 20 45 HU; may be lower
Ovarian tumor
Appendiceal tumor
Neonatal Ascites
GASTROINTESTINAL
perforation of hollow viscus
Meconium peritonitis
inflammatory lesions
Meckel diverticulum
Appendicitis
cyst rupture
Mesenteric cyst
Omental cyst
Choledochal cyst
bile leakage
Biliary obstruction
Biliary perforation
PORTOHEPATIC
extrahepatic portal vein obstruction
Atresia of veins
Compression by mass
intrahepatic portal vein obstruction
Portal cirrhosis (neonatal hepatitis)
Biliary cirrhosis (biliary atresia)
URINARY TRACT
 Urine ascites (most common cause) from lower urinary tract obstruction + upper urinary tract rupture: posterior/anterior urethral valves, ureterovesical/ureteropelvic junction obstruction, renal/bladder rupture, anterior urethral diverticulum, bladder diverticula, neurogenic bladder, extrinsic bladder mass
Urine ascites (most common cause) from lower urinary tract obstruction + upper urinary tract rupture: posterior/anterior urethral valves, ureterovesical/ureteropelvic junction obstruction, renal/bladder rupture, anterior urethral diverticulum, bladder diverticula, neurogenic bladder, extrinsic bladder mass
GENITAL
Ruptured ovarian cyst
Hydrometrocolpos
HYDROPS FETALIS
Immune hydrops
Nonimmune hydrops (usually cardiac causes)
MISCELLANEOUS
Chylous ascites
Lymphangiectasia
Congenital syphilis, trauma
Idiopathic
Chylous Ascites
| IN ADULTS: | 1. Inflammatory process | (35%) |
| 2. Tumor | (30%) | |
| 3. Idiopathic | (23%) | |
| 4. Trauma | (11%) | |
| 5. Congenital | (1%) | |
| IN CHILDREN: | 1. Congenital | (39%) |
| 2. Inflammatory process | (15%) | |
| 3. Trauma | (12%) | |
| 4. Tumor | (3%) | |
| 5. Idiopathic | (33%) |
Fluid Collections
| mnemonic: | BLUSCHINGS |
Biloma
Lymphocele, Lymphangioma, Lymphoma (almost anechoic by US)
Urinoma
Seroma
Cyst (pseudocyst, peritoneal inclusion cyst)
Hematoma (aneurysm, AVM)
Infection, Infestation (empyema, abscess, Echinococcus)
Neoplasm (necrotic)
GI tract (dilated loops, ileus, duplication)
Serosa (ascites, pleural fluid, pericardial effusion)
Intraabdominal Cyst in Childhood
Omental cyst (greater omentum/lesser sac, multilocular)
Mesenteric cyst (between leaves of small bowel mesentery)
Choledochal cyst
Intestinal duplication
Ovarian cyst
Pancreatic pseudocyst
Cystic renal tumor
Abscess
Meckel diverticulum (communicates with GI tract)
Lymphangioma
Mesenteric lymphoma
Intramural tumor
Mechanical Intestinal Obstruction
= occlusion/constriction of bowel lumen
| Prevalence: | 20% of acute abdominal admissions 80% small bowel obstruction 20% large bowel obstruction |
Air Progression in Neonates
| stomach | within minutes after birth |
| entire small bowel | within 3 hours |
| sigmoid colon | after 8 9 hours |
Cause of Absent Gas in Neonate
GI obstruction
Mechanical ventilation in severe respiratory distress
Continuous gastric suction
Cause of Delayed Passage of Gas in Neonate
Traumatic delivery
Septicemia
Hypoglycemia
Brain damage
Passage of Meconium
NORMAL
in 94% within 24 hours
in 99% within 48 hours
P.760
exceptions: prematurity, severely asphyxiated term infants DELAYED PASSAGE
Hirschsprung disease
Ileal/jejunal atresia
Meconium ileus
Meconium plug syndrome
Colon atresia
Imperforate anus
Common Causes of Obstruction in Children
Time of presentation:
| Nursery | Intestinal atresia, midgut volvulus, meconium ileus, Hirschsprung disease, small bowel atresia with meconium ileus, meconium plug syndrome, small left colon syndrome, imperforate anus, obstruction from duplication cyst |
| First 3 months | Hypertrophic pyloric stenosis, inguinal hernia, Hirschsprung disease, midgut volvulus |
| 6 24 months | Ileocolic intussusception |
| Childhood | Appendicitis |
Terminology:
High obstruction = proximal to midileum
 Rarely needs further radiologic evaluation
Rarely needs further radiologic evaluationbilious vomiting (after first feeding)
abdominal distention
 few dilated bowel loops
few dilated bowel loops
Low obstruction = distal ileum/colon
 More difficult to accurately localize
More difficult to accurately localize Requires contrast enema examination to diagnose microcolon, position of cecum, level of obstruction
Requires contrast enema examination to diagnose microcolon, position of cecum, level of obstructionabdominal distention + vomiting
failure to pass meconium
 many dilated intestinal loops
many dilated intestinal loops
Intestinal Obstruction in Neonate:
abdominal distension
vomiting
failure to pass meconium
Duodenal atresia (50%), stenosis (40%), web (10%)
Midgut volvulus
Jejunal/ileal atresia
Meconium ileus
Meconium plug syndrome
Hirschsprung disease
Necrotizing enterocolitis
NEONATAL OBSTRUCTION WITH MICROCOLON
Ileal atresia
Distal jejunal atresia
Meconium ileus
NEONATAL OBSTRUCTION WITH NORMAL COLON
Meconium plug
Hirschsprung disease
Intestinal Obstruction in Infant & Child
Hypertrophic pyloric stenosis
Appendicitis
Intussusception
Gastric Outlet Obstruction
CONGENITAL LESION
Antral mucosal diaphragm = antral web
Gastric duplication: usually along greater curvature, abdominal mass in infancy
Hypertrophic pyloric stenosis
INFLAMMATORY NARROWING
Peptic ulcer disease: cause in adults in 60 65%
Corrosive gastritis
Crohn disease, sarcoidosis, syphilis, tuberculosis
MALIGNANT NARROWING
Antral carcinoma: cause in adults in 30 35%
Scirrhous carcinoma of pyloric channel
OTHERS
Prolapsed antral polyp/mucosa
Bezoar
Gastric volvulus
Postoperative stomal edema
Abdominal plain film:
 large smoothly marginated homogeneous mass displacing transverse colon + small bowel inferiorly
large smoothly marginated homogeneous mass displacing transverse colon + small bowel inferiorly one/two air-fluid levels
one/two air-fluid levels
Duodenal Obstruction
Cause:
CONGENITAL
Annular pancreas
Peritoneal bands = Ladd bands
Aberrant vessel
INFLAMMATORY NARROWING
Chronic duodenal ulcer scar
Acute pancreatitis: phlegmon, abscess, pseudocyst
Acute cholecystitis: perforated gallstone
INTRAMURAL HEMATOMA
Blunt trauma (accident, child abuse)
Anticoagulant therapy
Blood dyscrasia
TUMORAL NARROWING
Primary duodenal tumors
Tumor invasion from pancreas, right kidney, lymph node enlargement
EXTRINSIC COMPRESSION
Aortic aneurysm
Pseudoaneurysm
OTHERS
Superior mesenteric artery syndrome from extensive burns, body cast, rapid weight loss, prolonged bed rest
Bezoar (in gastrectomized patient)
| mnemonic: | VA BADD TU BADD |
| child | adult |
|---|---|
| Volvulus | Tumor |
| Atresia | Ulcer |
| Bands | Bands |
| Annular pancreas | Annular pancreas |
| Duplication | Duplication |
| Diverticulum | Diverticulum |
P.761
Abdominal plain film:
 double-bubble sign = air-fluid levels in stomach + duodenum
double-bubble sign = air-fluid levels in stomach + duodenum frequently normal due to absence of gas from vomiting
frequently normal due to absence of gas from vomiting
Jejunal and Ileal Obstruction
= SMALL BOWEL OBSTRUCTION (SBO)
| Frequency: | accounts for 20% of all surgical admissions |
| Mortality: | 5.5% (dictum: Never let the sun rise or set on small-bowel obstruction ) |
Cause:
CONGENITAL
Jejunal atresia
Ileal atresia/stenosis
Enteric duplication: located on antimesenteric side, mostly in ileum
Midgut volvulus from arrest in rotation + fixation of small bowel during fetal life
Mesenteric cyst from meconium peritonitis:located on mesenteric side
Meckel diverticulum
EXTRINSIC BOWEL LESION
Fibrous adhesions (50 75%) from previous surgery (80%), peritonitis (15%), congenital/uncertain cause (5%)
Hernia (10%): internal/external
Volvulus
Masses: extrinsic neoplasm (most commonly advanced peritoneal carcinomatosis), abscess, aneurysm, hematoma, endometriosis
LUMINAL OCCLUSION
swallowed:
Foreign body: in children; mentally disturbed/disabled patients
Bezoar
Gallstone
Inspissated milk
Bolus of Ascaris lumbricoides
after birth:
Meconium ileus:
 microcolon in cystic fibrosis
microcolon in cystic fibrosis
Meconium ileus equivalent
other:
Intussusception
Tumor (rare): eg, lipoma
INTRINSIC BOWEL WALL LESION
neoplasm
Adenocarcinoma
Carcinoid tumor
Lymphoma
Gastrointestinal stromal tumor
inflammatory lesion
Crohn disease
Tuberculous enteritis
Eosinophilic gastroenteritis
Parasitic disease
vascular insufficiency
Ischemia (arterial/venous occlusion)
Radiation enteropathy
intramural hemorrhage
Blunt trauma
Henoch-Sch nlein purpura
Anticoagulants
strictures
Surgical anastomosis
Irradiation
Potassium chloride tablets
Massive deposition of amyloid
Plain abdominal radiograph (50 66% sensitive):
 candy cane appearance in erect position = >3 distended small bowel loops >3 cm with gas-fluid levels (>3 5 hours after onset of obstruction)
candy cane appearance in erect position = >3 distended small bowel loops >3 cm with gas-fluid levels (>3 5 hours after onset of obstruction) disparity in size between obstructed loops and contiguous small bowel loops of normal caliber beyond site of obstruction
disparity in size between obstructed loops and contiguous small bowel loops of normal caliber beyond site of obstruction small bowel positioned in center of abdomen
small bowel positioned in center of abdomen little/no gas + stool in colon with complete mechanical obstruction after 12 24 hours
little/no gas + stool in colon with complete mechanical obstruction after 12 24 hours stretch sign = erectile valvulae conniventes completely encircle bowel lumen
stretch sign = erectile valvulae conniventes completely encircle bowel lumen stepladder appearance in low obstruction (the greater the number of dilated bowel loops, the more distal the site of obstruction)
stepladder appearance in low obstruction (the greater the number of dilated bowel loops, the more distal the site of obstruction) string-of-beads indicate peristaltic hyperactivity to overcome mechanical obstruction
string-of-beads indicate peristaltic hyperactivity to overcome mechanical obstruction hyperactive peristalsis/aperistalsis = fatigued small bowel
hyperactive peristalsis/aperistalsis = fatigued small bowel snake head appearance = active peristalsis forms bulbous head of barium column in an attempt to overcome obstruction
snake head appearance = active peristalsis forms bulbous head of barium column in an attempt to overcome obstruction barium appears in colon >12 hours
barium appears in colon >12 hours
| CAVE: | little/no gas in small bowel from fluid-distended loops may lead one to overlook obstruction |
Location of obstruction:
valvulae conniventes high + frequent = jejunum
valvulae conniventes sparse/absent = ileum
Plain abdominal radiographic categories:
Normal
= absence of small intestinal gas/gas within 3 4 variably shaped loops <2.5 cm in diameter
Mild small bowel stasis
= single/multiple loops of 2.5 3 cm in diameter with 3 air-fluid levels
Probable SBO pattern
= dilated multiple gas-/fluid-filled loops with air-fluid levels + moderate amount of colonic gas
Definite SBO pattern
= clearly disproportionate gaseous/fluid distension of small bowel relative to colon
UGI:
 snake head appearance = active peristalsis forms bulbous head of barium column in an attempt to overcome obstruction
snake head appearance = active peristalsis forms bulbous head of barium column in an attempt to overcome obstruction barium appears in colon >12 hours
barium appears in colon >12 hours
Enteroclysis for adhesive obstruction:
 abrupt change in caliber of bowel with normal caliber/collapsed bowel distal to obstruction
abrupt change in caliber of bowel with normal caliber/collapsed bowel distal to obstruction stretched folds of normal pattern
stretched folds of normal pattern angulated + fixed bowel segment
angulated + fixed bowel segment
P.762
Enteroclysis categories of SBO (Shrake):
low-grade partial SBO
= sufficient flow of contrast material through point of obstruction so that fold pattern beyond obstruction is readily defined
high-grade partial SBO
= stasis + delay in arrival of contrast so that contrast material is diluted in distended prestenotic loop with minimal contrast in postobstructive loop leading to difficulty in defining fold pattern after transition point
complete SBO
= no passage of contrast material 3 24 hours after start of examination
CT (66% accurate, 78% specific, 63% sensitive, [81% sensitive for high-grade obstruction, 48% sensitive for low-grade partial obstruction]):
 small bowel dilatation >2.5 cm (not reliable to distinguish from adynamic ileus):
small bowel dilatation >2.5 cm (not reliable to distinguish from adynamic ileus): small bowel feces sign = gas bubbles mixed with particulate matter immediately proximal to obstruction (DDx: cystic fibrosis)
small bowel feces sign = gas bubbles mixed with particulate matter immediately proximal to obstruction (DDx: cystic fibrosis)
 discrepant caliber at transition zone from dilated to nondilated bowel:
discrepant caliber at transition zone from dilated to nondilated bowel: level of obstruction best determined by relative lengths of dilated versus collapsed bowel
level of obstruction best determined by relative lengths of dilated versus collapsed bowel passage of contrast material through transition zone indicates incomplete obstruction
passage of contrast material through transition zone indicates incomplete obstruction
 triangular beak immediately beyond dilated segment = point of transition
triangular beak immediately beyond dilated segment = point of transition
| DDx: | adynamic ileus (distension of entire small bowel) |
US:
 small bowel loops dilated >3 cm
small bowel loops dilated >3 cm length of dilated segment >10 cm
length of dilated segment >10 cm increased peristalsis of dilated segment (may become paralytic in prolonged obstruction)
increased peristalsis of dilated segment (may become paralytic in prolonged obstruction) colon collapsed
colon collapsed
Strangulated Obstruction:
= impaired circulation/ischemia of obstructed segment
| Prevalence: | 5 10 42% of patients with SBO |
| At risk: | patients with acute complete/high-grade SBO; risk increases over time |
TRIAD:
closed-loop obstruction of the involved segment (majority of cases)
mechanical obstruction proximal to the involved segment
venous congestion of the involved loop
CT (63 100% detection rate):
 slight circumferential thickening of bowel wall:
slight circumferential thickening of bowel wall: increased wall attenuation
increased wall attenuation target/halo sign
target/halo sign
 serrated beaklike narrowing at site of obstruction (32 100% specific) = closed loop with regional mesenteric vascular engorgement + bowel wall thickening at the obstructed segment
serrated beaklike narrowing at site of obstruction (32 100% specific) = closed loop with regional mesenteric vascular engorgement + bowel wall thickening at the obstructed segment unusual course of mesenteric vasculature
unusual course of mesenteric vasculature vascular compromise of affected bowel:
vascular compromise of affected bowel: poor/no enhancement of bowel wall (100% SPECIFIC)
poor/no enhancement of bowel wall (100% SPECIFIC) delayed prolonged enhancement of bowel wall
delayed prolonged enhancement of bowel wall mesenteric haziness due to edema (95% specific)
mesenteric haziness due to edema (95% specific) diffuse engorgement of mesenteric vasculature
diffuse engorgement of mesenteric vasculature localized mesenteric fluid/hemorrhage
localized mesenteric fluid/hemorrhage
 large amount of ascites
large amount of ascites pneumatosis intestinalis
pneumatosis intestinalis gas in portal vein
gas in portal vein
Prognosis:
20 37% mortality rate (compared with 5 8% for a recently reduced simple obstruction) due to delay in diagnosis: 8% for surgery performed in <36 hours, 25% mortality for surgery performed in >36 hours
CLOSED-LOOP OBSTRUCTION
= obstruction at two points along the course of the bowel at a single site usually with involvement of mesentery
| Pathophysiology: | impaired venous arterial flow |
 Most common cause of strangulation!
Most common cause of strangulation!
| Cause: | adhesion (75%), incarcerated hernia |
 fixation of bowel loop = no change in position:
fixation of bowel loop = no change in position: coffee bean sign = gas-filled loop
coffee bean sign = gas-filled loop pseudotumor = fluid-filled loop
pseudotumor = fluid-filled loop U- or C-shaped dilated bowel loop on CT
U- or C-shaped dilated bowel loop on CT
 increasing intraluminal fluid
increasing intraluminal fluid beak sign = point of obstruction on CT/UGI
beak sign = point of obstruction on CT/UGI whirl sign = twisting of bowel + mesentery on CT:
whirl sign = twisting of bowel + mesentery on CT: stretched engorged mesenteric vessels converging toward site of obstruction/torsion delayed enhancement
stretched engorged mesenteric vessels converging toward site of obstruction/torsion delayed enhancement
| Cx: | volvulus |
Acquired Small Bowel Obstruction in Childhood
| mnemonic: | AAIMM |
Adhesions
Appendicitis
Intussusception
Incarcerated hernia
Malrotation
Meckel diverticulum
Small Bowel Obstruction in Adulthood
| mnemonic: | SHAVIT |
Stone (gallstone ileus)
Hernia (21%)
Adhesion (49%)
Volvulus
Intussusception
Tumor (16%)
SBO IN VIRGIN ABDOMEN OF ADULTHOOD
Bowel ischemia including ischemic stricture
Primary small bowel neoplasm
Metastatic small bowel neoplasm
Extrinsic abdominal mass
Internal/abdominal wall hernia
Crohn disease
Colonic Obstruction
| Incidence: | 25% of all intestinal obstructions |
P.763
Cause:
NEONATAL COLONIC OBSTRUCTION
Meconium plug syndrome
Colonic atresia
Anorectal malformation: rectal atresia, imperforate anus
Hirschsprung disease
functional colonic immaturity (especially in premies + infants of mothers treated with magnesium or high doses of sedatives/opiates, children with septicemia, hypothyroidism, hypoglycemia, diabetic mothers)
small left colon syndrome
meconium plug syndrome
LUMINAL OBTURATION
Fecal impaction
 bubbly pattern of large mass of stool
bubbly pattern of large mass of stool
Fecaloma
Gallstone (in sigmoid narrowed by diverticulitis)
Intussusception
BOWEL WALL LESION
malignant (60 70% of obstructions) predominantly in sigmoid
inflammatory
Crohn disease
Ulcerative colitis
Mesenteric ischemia
Sigmoid diverticulitis (15%)
 stenotic segment >6 cm
stenotic segment >6 cm
Acute pancreatitis
infectious:
infectious granulomatous process
Actinomycosis
Tuberculosis
Lymphogranuloma venereum
parasitic disease
Amebiasis
Schistosomiasis
wall hematoma:
blunt trauma, coagulopathy
EXTRINSIC
mass impression
Endometriosis
Large tumor mass: prostate, bladder, uterus, tubes, ovaries
Pelvic abscess
Hugely distended bladder
Mesenteritis
Poorly formed colostomy
severe constriction
Volvulus (3rd most common cause): sigmoid colon, cecum, transverse colon, compound volvulus (= ileosigmoid knot)
Hernia: transverse colon in diaphragmatic hernia, sigmoid colon in left inguinal hernia
Adhesion
Abdominal plain-film patterns:
dilated colon only = competent ileocecal valve
dilated small bowel (25%) = incompetent ileocecal valve
dilated colon + dilated small bowel = ileocecal valve obstruction secondary to cecal overdistension
 gas-fluid levels distal to hepatic flexure (fluid is normal in cecum + ascending colon); sign not valid with diarrhea/saline catharsis/enema
gas-fluid levels distal to hepatic flexure (fluid is normal in cecum + ascending colon); sign not valid with diarrhea/saline catharsis/enema cecum most dilated portion (in 75% of cases); critical at 10 cm diameter (high probability for impending perforation)
cecum most dilated portion (in 75% of cases); critical at 10 cm diameter (high probability for impending perforation) The lower the obstruction, the more proximal the distension!
The lower the obstruction, the more proximal the distension!
| BE: | Emergency barium enema of unprepared colon in suspected obstruction! Contraindicated in toxic megacolon, pneumatosis intestinalis, portal vein gas, extraluminal gas |
Ileus
[ileus = stasis/inability to push fluid along (term does not distinguish between mechanical and nonmechanical causes)]
= ADYNAMIC/PARALYTIC/NONOBSTRUCTIVE ILEUS
= derangement impairing proper distal propulsion of intestinal contents
Cause:
in neonate:
Hyperbilirubinemia
Intracranial hemorrhage
Aspiration pneumonia
Necrotizing enterocolitis
Aganglionosis
in child/adult:
Postoperative ileus
usually resolves by 4th postoperative day
Visceral pain: obstructing ureteral stone, common bile duct stone, twisted ovarian cyst, blunt abdominal/chest trauma
Intraabdominal inflammation/infection: peritonitis, appendicitis, cholecystitis, pancreatitis, salpingitis, abdominal abscess, hemolytic-uremic syndrome, gastroenteritis
Ischemic bowel disease
Anticholinergic drugs: atropine, propantheline, morphine + derivatives, tricyclic antidepressants, dilantin, phenothiazines, hexamethonium bromide
Neuromuscular disorder: diabetes, hypothyroidism, porphyria, lead poisoning, uremia, hypokalemia, amyloidosis, urticaria, sprue, scleroderma, Chagas disease, vagotomy, myotonic dystrophy, CNS trauma, paraplegia, quadriplegia
Systemic disease: septic/hypovolemic shock, urticaria
Chest disease: lower lobe pneumonia, pleuritis, myocardial infarction, acute pericarditis, congestive heart failure
Retroperitoneal disease: hemorrhage (spine trauma), abscess
| mnemonic: | Remember the P's |
Pancreatitis
Pendicitis
Peptic ulcer
Perforation
Peritonitis
Pneumonia
Porphyria
Postoperative
Potassium paucity
Pregnancy
Pyelonephritis
P.764
intestinal sounds decreased/absent
abdominal distension
 large + small bowel gastric distension
large + small bowel gastric distension decreased small bowel distension on serial films
decreased small bowel distension on serial films delayed but free passage of contrast material
delayed but free passage of contrast material
| Rx: | not amenable to surgical correction |
Localized Ileus
= isolated distended loop of small/large bowel
= SENTINEL LOOP
| Often associated with: | adjacent acute inflammatory process |
Etiology:
| 1. Acute pancreatitis: | duodenum, jejunum, transverse colon |
| 2. Acute cholecystitis: | hepatic flexure of colon |
| 3. Acute appendicitis: | terminal ileum, cecum |
| 4. Acute diverticulitis: | descending colon |
| 5. Acute ureteral colic: | GI tract along course of ureter |
Intestinal Pseudoobstruction
TRANSIENT PSEUDOOBSTRUCTION
Electrolyte imbalance
Renal failure
Congestive heart failure
ACUTE COLONIC PSEUDOOBSTRUCTION (Ogilvie syndrome)
CHRONIC PSEUDOOBSTRUCTION
Scleroderma
Amyloidosis
IDIOPATHIC PSEUDOOBSTRUCTION
Chronic intestinal pseudoobstruction syndrome
Megacystis-microcolon-intestinal-hypoperistalsis syndrome
Esophagus
Esophageal Contractions
 Esophageal motor activity needs to be evaluated in recumbent position without influence of gravity!
Esophageal motor activity needs to be evaluated in recumbent position without influence of gravity!PERISTALTIC EVENT = coordinated contractions of esophagus
PERISTALTIC SEQUENCE = aboral stripping wave clearing esophagus
Primary Esophageal Peristalsis
= orderly peristaltic sequence with progressive aboral stripping traversing entire esophagus with complete clearance of barium; centrally mediated (medulla) swallow reflex via glossopharyngeal + vagal nerve; initiated by swallowing
 rapid wave of inhibition followed by slower wave of contraction
rapid wave of inhibition followed by slower wave of contraction Normal peristaltic sequence will be interrupted by repetitive swallowing before peristaltic sequence is complete!
Normal peristaltic sequence will be interrupted by repetitive swallowing before peristaltic sequence is complete!
Secondary Esophageal Peristalsis
= local peristaltic wave identical to primary peristalsis but elicited through esophageal distension = sensorimotor stretch reflex
 Esophageal motility can be evaluated with barium injection through nasoesophageal tube despite patient's inability to swallow!
Esophageal motility can be evaluated with barium injection through nasoesophageal tube despite patient's inability to swallow!
Tertiary Esophageal Contractions
= nonpropulsive esophageal motor event characterized by disordered up-and-down movement of bolus without clearing of esophagus
Cause:
Presbyesophagus
Diffuse esophageal spasm
Hyperactive achalasia
Neuromuscular disease:
@ diabetes mellitus, parkinsonism, amyotrophic lateral sclerosis, multiple sclerosis, thyrotoxic myopathy, myotonic dystrophy
Obstruction of cardia:
neoplasm, distal esophageal stricture, benign lesion, S/P repair of hiatal hernia
 Tertiary activity does not necessarily imply a significant motility disturbance!
Tertiary activity does not necessarily imply a significant motility disturbance!
| Age: | in 5 10% of normal adults during 4th 6th decade |
nonsegmental = partial luminal indentation
Location: in lower 2/3 of esophagus  spontaneous repetitive nonpropulsive contraction
spontaneous repetitive nonpropulsive contraction yo-yo motion of barium
yo-yo motion of barium corkscrew appearance = scalloped configuration of barium column
corkscrew appearance = scalloped configuration of barium column rosary bead / shish kebab configuration = compartmentalization of barium column
rosary bead / shish kebab configuration = compartmentalization of barium column no lumen-obliterating contractions
no lumen-obliterating contractions
segmental = luminal obliteration (rare)
 curling = erratic segmental contractions
curling = erratic segmental contractions rosary-bead appearance
rosary-bead appearance
Abnormal Esophageal Peristalsis
PRIMARY MOTILITY DISORDERS
Achalasia
Diffuse esophageal spasm
severe intermittent pain while swallowing
 compartmentalization of esophagus by numerous tertiary contractions
compartmentalization of esophagus by numerous tertiary contractions
Dx: extremely high pressures on manometry Presbyesophagus
Chalasia
Congenital TE fistula
Intestinal pseudoobstruction
SECONDARY MOTILITY DISORDERS
connective tissue disease
Scleroderma
SLE
Rheumatoid arthritis
Polymyositis
Dermatomyositis
Muscular dystrophy
chemical/physical injury
Reflux/peptic esophagitis
S/P vagotomy
Caustic esophagitis
Radiotherapy
infection
fungal: candidiasis parasitic: Chagas disease bacterial: TB, diphtheria viral: herpes simplex metabolic disease
Diabetes mellitus
Amyloidosis
Alcoholism
Electrolyte disturbances
endocrine disease
Myxedema
Thyrotoxicosis
neoplasm
drug-related: atropine, propantheline, curare
muscle disease
Myotonic dystrophy
Muscular dystrophy
Oculopharyngeal dystrophy
Myasthenia gravis (disturbed motility only in striated muscle of upper 1/3 of esophagus)
 persistent collection of barium in upper third of esophagus
persistent collection of barium in upper third of esophagus findings reversed by cholinesterase inhibitor edrophonium (Tensilon )
findings reversed by cholinesterase inhibitor edrophonium (Tensilon )
neurologic disease
Parkinsonism
Multiple sclerosis
CNS neoplasm
Amyotrophic lateral sclerosis
Bulbar poliomyelitis
Cerebrovascular disease
Huntington chorea
Ganglioneuromatosis
Wilson disease
Friedreich ataxia
Familial dysautonomia (Riley-Day)
Stiff-man syndrome
P.765
Diffuse Esophageal Dilatation
= ACHALASIA PATTERN = MEGAESOPHAGUS
ESOPHAGEAL MOTILITY DISORDER
Idiopathic achalasia
Chagas disease: patients commonly from South America; often associated with megacolon + cardiomegaly
Postvagotomy syndrome
Scleroderma
Systemic lupus erythematosus
Presbyesophagus
Ehlers-Danlos syndrome
Diabetic/alcoholic neuropathy
Anticholinergic drugs
Idiopathic intestinal pseudoobstruction
= degeneration of innervation
Amyloidosis: associated with macroglossia, thickened small bowel folds
Esophagitis
DISTAL OBSTRUCTION
Infiltrating lesion of distal esophagus/gastric cardia (eg, carcinoma) = pseudoachalasia
Benign stricture
Extrinsic compression
mnemonic: MA'S TACO in a SHell M uscular disorder (eg, myasthenia gravis)
A chalasia
S cleroderma
T rypanosomiasis (Chagas disease)
A myloidosis
C arcinoma
O bstruction
S tricture (lye, potassium, tetracycline)
H iatal hernia
Air Esophagogram
Normal variant
Scleroderma
Distal obstruction: tumor, stricture, achalasia
Thoracic surgery
Mediastinal inflammatory disease
S/P total laryngectomy (esophageal speech)
Endotracheal intubation + PEEP
Abnormal Esophageal Folds
TRANSVERSE FOLDS
Feline esophagus
frequently seen with gastroesophageal reflux; normally found in cats
 transient contraction of longitudinally oriented muscularis mucosae
transient contraction of longitudinally oriented muscularis mucosae
Fixed transverse folds
due to scarring from reflux esophagitis
 stepladder appearance in distal esophagus
stepladder appearance in distal esophagus
LONGITUDINAL FOLDS
normal: 1 2 mm wide, best seen in collapsed esophagus  >3 mm with submucosal edema/inflammation
>3 mm with submucosal edema/inflammation
Gastroesophageal reflux
Opportunistic infection
Caustic ingestion
Irradiation
| DDx: | (1) Varices tortuous/serpentine folds that can be effaced by esophageal distension (2) Varicoid carcinoma fixed rigid folds with abrupt demarcation due to submucosal spread |
Esophageal Inflammation
CONTACT INJURY
reflux related
Peptic ulcer disease
Barrett esophagus
Scleroderma (patulous LES)
Nasogastric intubation
caustic
Foreign body
Corrosives
thermic
habitual ingestion of excessively hot meals/liquids
P.766
RADIATION INJURY
INFECTION
Candidiasis
Herpes simplex virus/CMV
Diphtheria
SYSTEMIC DISEASE
dermatologic disorders
blistering of skin + mucous membranes in response to minor trauma
Epidermolysis bullosa dystrophica
Histo: intraepidermal bullae Benign mucous membrane pemphigoid
= rare disease of unknown cause
Histo: subepidermal bullae without acantholysis Age: 4th decade; M < F  esophageal lesions (in 2 13%) most frequent at sites of relative stasis (aortic knob, carina, GE junction):
esophageal lesions (in 2 13%) most frequent at sites of relative stasis (aortic knob, carina, GE junction): thin smooth webs arising from anterior aspect
thin smooth webs arising from anterior aspect stenoses of variable length
stenoses of variable length
Pemphigus vulgaris
others:
Crohn disease
Graft-versus-host disease
Beh et disease
Eosinophilic gastroenteritis
Esophageal Ulcer
PEPTIC
Reflux esophagitis: scleroderma
Barrett esophagus
Crohn disease
Dermatologic disorders: benign mucous membrane pemphigoid, epidermolysis bullosa dystrophica, Beh et disease
INFECTIOUS
Herpes
Cytomegalovirus
CONTACT INJURY/EXTERNAL INJURY
Corrosives: alkali, strictures in 50%
Alcohol-induced esophagitis
Drug-induced esophagitis
Radiotherapy: smooth stricture >4,500 rads
 shallow/deep ulcers conforming to radiation portal
shallow/deep ulcers conforming to radiation portal
Nasogastric tube
 elongated stricture in middle + distal 1/3
elongated stricture in middle + distal 1/3
Endoscopic sclerotherapy
MALIGNANT
Esophageal carcinoma
Location:
@ Upper esophagus
Barrett ulcer in islets of gastric mucosa
@ Midesophagus
Herpes esophagitis
CMV esophagitis
Drug-induced esophagitis
@ Distal esophagus
Reflux esophagitis
CMV esophagitis
DDx:
Sacculation
= outpouching in distal esophagus due to asymmetric scarring in reflux esophagitis
Esophageal intramural pseudodiverticula
Artifact
tiny precipitates of barium
transient mucosal crinkling in inadequate distension
irregular Z-line
Small Esophageal Ulcer (<1 cm)
Herpes simplex virus type I
Drug-induced
Reflux esophagitis
Beh et syndrome
Benign mucous membrane pemphigoid
Acute radiation change
Large Esophageal Ulcer (>1 cm)
Cytomegalovirus
Human immunodeficiency virus
Carcinoma
Drug-induced
Barrett esophagus
Sclerotherapy for varices
Double-barrel esophagus
Dissecting intramural hematoma from emetogenic injury
Mallory-Weiss tear trauma, esophagoscopy (in 0.25%), bougienage (in 0.5%), ingestion of foreign bodies, spontaneous (bleeding diathesis)
Intramural abscess
Intraluminal diverticulum
Esophageal duplication (if communication with esophageal lumen present)
Esophageal Diverticulum
Zenker diverticulum (pharyngoesophageal)
Interbronchial diverticulum
= traction diverticulum
= response to pull from fibrous adhesions following lymph node infection (TB), contains all 3 esophageal layers
Location: usually on right anterolateral wall of interbronchial segment  calcified mediastinal nodes
calcified mediastinal nodes
Interaorticobronchial diverticulum
= thoracic pulsion diverticulum
Location: on left anterolateral wall between inferior border of aortic arch + upper margin of left main bronchus Epiphrenic diverticulum (rare)
Location: usually on lateral esophageal wall, right > left, in distal 10 cm  often associated with hiatus hernia
often associated with hiatus hernia
Intramural esophageal pseudodiverticulosis
 outpouching from mucosal glands
outpouching from mucosal glands
P.767
Tracheobronchoesophageal Fistula
CONGENITAL
Congenital tracheoesophageal fistula
MALIGNANCY (in 60%)
Lung cancer
Metastases to mediastinal lymph nodes
Esophageal cancer
 In 5 10% of patients with advanced esophageal cancer
In 5 10% of patients with advanced esophageal cancer
Radiation treatment of mediastinal malignancy
TRAUMATIC
Instrumentation (esophagoscopy, bougienage, pneumatic dilatation)
Blunt ( crush injury )/penetrating chest trauma
Surgery
Foreign-body perforation
Corrosives
Postemetic rupture = Boerhaave syndrome
INFECTIOUS/INFLAMMATORY
TB, syphilis, histoplasmosis, actinomycosis, Crohn disease
Perforated diverticulum
Pulmonary sequestration/cyst
Long Smooth Esophageal Narrowing
Congenital esophageal stenosis
 at junction between middle + distal third
at junction between middle + distal third weblike/tubular stenosis of 1 cm in length
weblike/tubular stenosis of 1 cm in length
Surgical repair of esophageal atresia
 interruption of primary peristaltic wave at anastomosis
interruption of primary peristaltic wave at anastomosis secondary contractions may produce retrograde flow with aspiration
secondary contractions may produce retrograde flow with aspiration impaction of food
impaction of food
Caustic burns = alkaline burns
Alendronate (= inhibitor of osteoclastic activity)
Gastric acid: reflux, hyperemesis gravidarum
Intubation: reflux + compromise of circulation
Radiotherapy for esophageal carcinoma; tumor of lung, breast, or thymus; lymphoma; metastases to mediastinal lymph nodes
Onset of stricture: usually 4 8 months post Rx Dose: 3,000 5,000 rad Postinfectious: moniliasis (rare)
Lower Esophageal Narrowing
| mnemonic: | SPADE |
S cleroderma
P resbyesophagus
A chalasia; A nticholinergics
D iffuse esophageal spasm
E sophagitis
Focal Esophageal Narrowing
Esophageal web
= 1 2-mm thick (vertical length) area of complete/incomplete circumferential narrowing
Esophageal ring
= 5 10-mm thick (vertical length) area of complete/incomplete circumferential narrowing
Esophageal stricture
= >10 mm in vertical length
| mnemonic: | LETTERS MC |
Lye ingestion
Esophagitis
Tumor
Tube (prolonged nasogastric intubation)
Epidermolysis bullosa
Radiation
Surgery, S cleroderma
Moniliasis
Congenital
Midesophageal Stricture
Barrett esophagus
Radiation injury
Caustic esophagitis
Primary carcinoma: squamous cell carcinoma
Metastatic cancer (from subcarinal nodes/left mainstem bronchus)
Drug-induced stricture (esp. potassium chloride)
Esophageal intramural pseudodiverticulosis
Dermatologic disorder: benign mucous membrane pemphigoid, epidermolysis bullosa
Graft-versus-host disease
Long Distal Esophageal Stricture
SEVERE ACID EXPOSURE
Nasogastric intubation
Zollinger-Ellison syndrome
Alkaline reflux esophagitis
INFLAMMATION
Crohn disease
Short Distal Esophageal Stricture
Reflux esophagitis
Carcinoma (adenocarcinoma)
Crohn disease
Schatzki ring
Esophageal Filling Defect
BENIGN TUMORS
<1% of all esophageal tumors
Submucosal tumor (75%)
= nonepithelial, intramural
Leiomyoma (50% of all benign tumors)
 Most common submucosal mass in esophagus
Most common submucosal mass in esophagus
Granular cell myoblastoma
Lipoma, fibroma, lipoma, fibrolipoma, myxofibroma, hamartoma, hemangioma, lymphangioma, neurofibroma, schwannoma,
 primary wave stops at level of tumor
primary wave stops at level of tumor proximal esophageal dilatation + hypotonicity
proximal esophageal dilatation + hypotonicity rigid esophageal wall at site of tumoral implant
rigid esophageal wall at site of tumoral implant disorganized/altered/effaced mucosal folds around defect
disorganized/altered/effaced mucosal folds around defect tumor shadow on tangential view extending beyond esophageal margin
tumor shadow on tangential view extending beyond esophageal margin
Mucosal tumor (25%) = epithelial, intraluminal
Squamous papilloma
= most common benign mucosal tumor; rarely multiple (esophageal papillomatosis)
 small sessile slightly lobulated polyp
small sessile slightly lobulated polyp
Fibrovascular polyp
Path: fibrovascular + adipose tissue Location: cervical esophagus near cricopharyngeus  giant sausage-shaped intraluminal mass
giant sausage-shaped intraluminal mass
Cx: regurgitation into larynx causes sudden death Inflammatory esophagogastric polyp
= sentinel polyp = bulbous tip of thickened gastric fold
Cause: sequelae of chronic reflux esophagitis Prognosis: no malignant potential Adenoma
= originates in Barrett mucosa
 sessile/pedunculated polyp
sessile/pedunculated polyp
Cx: malignant degeneration Glycogen acanthosis
P.768
MALIGNANT TUMORS
Esophageal cancer
squamous/varicoid squamous cell carcinoma
adenocarcinoma
spindle cell carcinoma: leiomyosarcoma, carcinosarcoma, pseudosarcoma
Carcinoma of cardia (gastric cancer)
Metastases: malignant melanoma, lymphoma (<1% of gastrointestinal lymphomas), stomach, lung, breast
VASCULAR
Varices
INFECTION/INFLAMMATION
Candida/herpes esophagitis
Drug-induced inflammatory reaction
CONGENITAL/NORMAL VARIANT
Prolapsed gastric folds
Esophageal duplication cyst (0.5 2.5% of all esophageal tumors)
FOREIGN BODIES
Retained food particles (chicken bone, fish bone, pins, coins, small toys, meat)
Undissolved effervescent crystals
Air bubbles
Esophageal Mucosal Nodules/Plaques
| plaque | = discrete irregular/ovoid elevation barely protruding above mucosal surface |
| nodule | = small more rounded elevation |
Candida esophagitis
Reflux esophagitis (early stage)
Barrett esophagus
Glycogen acanthosis
Superficial spreading carcinoma
Artifacts (undissolved effervescent agent, air bubbles, debris)
Extrinsic Esophageal Impression
Cervical Causes of Esophageal Impression
OSSEOUS LESIONS
Anterior marginal osteophyte/DISH
Anterior disk herniation
Cervical trauma + hematoma
Osteomyelitis
Bone neoplasm
ESOPHAGEAL WALL LESIONS
muscle
Cricopharyngeus
Esophageal web
vessel
Pharyngeal venous plexus
Lymph node enlargement
ENDOCRINE ORGANS
Thyroid/parathyroid enlargement (benign/malignant)
Fibrotic traction after thyroidectomy
Retropharyngeal/mediastinal abscess
Thoracic Causes of Esophageal Impression
NORMAL INDENTATIONS
aortic arch, left mainstem bronchus, left inferior pulmonary vein, diaphragmatic hiatus
ABNORMAL VASCULATURE
right-sided aortic arch, cervical aortic arch, aortic unfolding, aortic tortuosity, aortic aneurysm, double aortic arch ( reverse S ), coarctation of aorta ( reverse figure 3 ), aberrant right subclavian artery
= arteria lusoria (semilunar/bayonet-shaped imprint upon posterior wall of esophagus), aberrant left pulmonary artery (between trachea + esophagus), anomalous pulmonary venous return (anterior), persistent truncus arteriosus (posterior)
CARDIAC CAUSES
enlargement of chambers
left atrial/left ventricular enlargement: mitral disease (esophageal displacement backward + to the right)
pericardial masses
pericardial tumor/cyst/effusion
MEDIASTINAL CAUSES
mediastinal tumor, lymphadenopathy (metastatic, tuberculous), inflammation, cyst
PULMONARY CAUSES
pulmonary tumor, bronchogenic cyst, atypical pulmonary fibrosis (retraction)
ESOPHAGEAL ABNORMALITIES
Esophageal diverticulum
Paraesophageal hernia
Esophageal duplication
Stomach
Gastric Tumor
Classification based on Biologic Behavior
MALIGNANT (10 15%)
Adenocarcinoma (>95%)
Lymphoma, mucosa-associated lymphoid tissue (MALT)
Sarcoma: leiomyosarcoma, Kaposi sarcoma
Carcinoid tumor
Metastasis
hematogenous: malignant melanoma, breast cancer
 one/more submucosal masses
one/more submucosal masses target/bull's-eye lesion if centrally ulcerated
target/bull's-eye lesion if centrally ulcerated giant cavitated lesion
giant cavitated lesion linitis plastica (usually in breast cancer)
linitis plastica (usually in breast cancer)
direct invasion
Barrett cancer: gastric fundus
Pancreatic cancer: stomach/duodenal sweep
Colonic cancer: greater gastric curvature
Omental cake: greater gastric curvature
P.769
BENIGN (85 90%)
epithelial/mucosal tumor (50%)
Hyperplastic polyp
Adenomatous polyp
Brunner gland hyperplasia
mesenchymal tumor (50%)
Leiomyoma
Ectopic pancreatic rest
Mesenchymal Tumors of GI Tract
SOMATIC SOFT TISSUE TUMOR
smooth muscle tumor
True leiomyoma
True leiomyosarcoma
neural tumor
 4% of all benign gastric tumors
4% of all benign gastric tumors
Schwannoma
Neurofibroma
Plexosarcoma
lipocytic tumor
Lipoma (2 3% of all benign gastric tumors)
Liposarcoma
vascular/perivascular tissue
 2% of all benign gastric tumors
2% of all benign gastric tumors
Glomus tumor (most common)
Hemangioma
Lymphangioma
GASTROINTESTINAL STROMAL TUMOR
Calcified Gastric Tumor
Mucinous adenocarcinoma: miliary/punctate
Stromal tumors: amorphous calcifications
Hemangioma: clusters of phleboliths
Congenital Gastric Obstruction
COMPLETE OBSTRUCTION
Gastric atresia
Frequency: <1% of all GI obstructions May be associated with: epidermolysis bullosa Site: antrum + pylorus regurgitation of bile-free vomitus within first few hours after birth
 single bubble appearance of air in stomach
single bubble appearance of air in stomach membranous mucosal diaphragm
membranous mucosal diaphragm
Congenital peritoneal bands
Annular pancreatic tissue
PARTIAL GASTRIC OUTLET OBSTRUCTION
cyclic transient postprandial vomiting
Incomplete prepyloric diaphragm
Antral stenosis
Aberrant pancreatic tissue in gastric antrum
Antral duplication cyst
Widened Retrogastric Space
PANCREATIC MASSES (most common cause)
Acute + chronic pancreatitis
Pancreatic pseudocyst
Pancreatic cystadenoma + carcinoma
OTHER RETROPERITONEAL MASSES
Sarcoma
Renal tumor, adrenal tumor
Lymph node enlargement
Abscess, hematoma
GASTRIC MASSES
Leiomyoma, leiomyosarcoma
OTHERS
Aortic aneurysm
Choledochal cyst
Obesity
Postsurgical disruptions + adhesions
Ascites
Gross hepatomegaly + enlarged caudate lobe
Hernia involving omentum
Gas within Stomach Wall
NONINFECTIOUS
Interstitial gastric emphysema
= gas accumulation in submucosa/subserosa/or both
Cause: air from an extrinsic source obstructive (due to raised intragastric pressure):
gastric outlet obstruction, volvulus, overinflation during gastroscopy, profuse severe vomiting
pulmonary (due to rupture + dissection of subpleural blebs in bullous emphysema along esophageal wall/mediastinum): pulmonary emphysema
traumatic (due to mucosal trauma):
instrumentation of stomach, recent gastroduodenal surgery, endoscopy (1.6%)
benign clinical course with spontaneous resolution
 linear lucency conforming to contour of a thinwalled distended stomach
linear lucency conforming to contour of a thinwalled distended stomach
Cystic pneumatosis
= PNEUMATOSIS CYSTOIDES INTESTINALIS
Cause: similar to interstitial gastric emphysema little/no gastrointestinal symptoms
 multiple 1 2-mm gas-filled cysts in wall of stomach and intestines
multiple 1 2-mm gas-filled cysts in wall of stomach and intestines
INFECTIOUS
Emphysematous gastritis
predisposing: corrosive gastritis, acid ingestion, severe necrotizing gastroenteritis, gastric ulcer disease with intramural perforation, gastric carcinoma, volvulus, gastric infarction
P.770
Gastric Atony
= gastric retention in the absence of mechanical obstruction
| Pathophysiology: | reflex paralysis |
 abdominal distension
abdominal distension vascular collapse (decreased venous return)
vascular collapse (decreased venous return) vomiting
vomiting large stomach filled with air + fluid (up to 7,500 mL)
large stomach filled with air + fluid (up to 7,500 mL) retention of barium
retention of barium absent/diminished peristaltic activity
absent/diminished peristaltic activity patulous pylorus
patulous pylorus frequently dilated duodenum
frequently dilated duodenum
| DDx: | gastric volvulus, pyloric stenosis |
Acute Gastric Atony
(may develop within 24 48 hours)
Acute gastric dilatation: secondary to decreased arterial perfusion (ischemia, congestive heart failure) in old patients, usually fatal
Postsurgical atony, ureteral catheterization
Immobilization: body cast, paraplegia, postoperative state
Abdominal trauma: especially back injury
Severe pain: renal/biliary colic, migraine headaches, severe burns
Infection: peritonitis, pancreatitis, appendicitis, subphrenic abscess, septicemia
Chronic Gastric Atony
Neurologic abnormalities: brain tumor, bulbar poliomyelitis, vagotomy, tabes
Muscular abnormalities: scleroderma, muscular dystrophy
Drug-induced atony: atropine, morphine, heroin, ganglionic blocking agents
Electrolyte imbalance: diabetic ketoacidosis, hypercalcemia, hypocalcemia, hypokalemia, hepatic coma, uremia, myxedema
Diabetes mellitus = gastroparesis diabeticorum (0.08% incidence)
Emotional distress
Lead poisoning
Porphyria
Narrowing of Stomach
= linitis plastica type of stenosis
MALIGNANCY
Scirrhous gastric carcinoma (involving portion/all of stomach)
Hodgkin lymphoma, NHL
Metastatic involvement (carcinoma of breast, pancreatic carcinoma, colonic carcinoma)
INFLAMMATION
Chronic gastric ulcer disease with intense spasm
Pseudo-Billroth-I pattern of Crohn disease
Sarcoidosis
 polypoid appearance, pyloric hypertrophy
polypoid appearance, pyloric hypertrophy gastric ulcers, duodenal deformity
gastric ulcers, duodenal deformity
Eosinophilic gastritis
Polyarteritis nodosa
Stenosing antral gastritis/hypertrophic pyloric stenosis
INFECTION
Tertiary stage of syphilis
 absent mucosal folds + peristalsis
absent mucosal folds + peristalsis no change over years
no change over years
Tuberculosis (rare)
 hyperplastic nodules/ulcerative lesion/annular lesion
hyperplastic nodules/ulcerative lesion/annular lesion pyloric obstruction, may cross into duodenum
pyloric obstruction, may cross into duodenum
Histoplasmosis
Actinomycosis
Strongyloidiasis
Phlegmonous gastritis
Toxoplasmosis
TRAUMA
Corrosive gastritis
Radiation injury
Gastric freezing
Hepatic arterial chemotherapy infusion
OTHERS
Perigastric adhesions (normal mucosa, no interval change, normal peristalsis)
Amyloidosis
Pseudolymphoma
Exogastric mass (hepatomegaly, pancreatic pseudocyst)
| mnemonic: | SLIMRAGE |
Scirrhous carcinoma of stomach
Lymphoma
Infiltration from adjacent neoplasm
Metastasis (breast carcinoma)
Radiation therapy
Acids (corrosive ingestion)
Granulomatous disease (TB, sarcoidosis, Crohn)
Eosinophilic gastroenteritis
Antral Narrowing
| mnemonic: | SPICER |
Sarcoidosis, Syphilis
Peptic ulcer disease
Infection (tuberculosis, chronic granulomatous disease of childhood)
Cancer (linitis plastica), Crohn disease, Caustic ingestion
Eosinophilic gastritis
Radiation
Antral Pad Sign
= extrinsic impression of the posteroinferior wall of antrum
Pancreatic cancer in head/body
Pancreatitis
Pancreatic pseudocyst
Normal/distended gallbladder (patient in RAO position)
Intramural-Extramucosal Lesions of Stomach
 sharply delineated marginal/contour defect
sharply delineated marginal/contour defect stretched folds over intact mucosa
stretched folds over intact mucosa acute angle at margins
acute angle at margins may ulcerate centrally
may ulcerate centrally may become pedunculated and acquire polypoid appearance over years
may become pedunculated and acquire polypoid appearance over years
P.771
NEOPLASTIC
1. Leiomyoma (48%) 2. Neurogenic tumors (14%) 3. Heterotopic pancreas (12%) 4. Fibrous tumor (11%) 5. Lipoma (7%) 6. Hemangioma (7%) 7. Glomus tumor (rare) 8. Carcinoid 9. Metastatic tumor INFLAMMATION/INFECTION
Granuloma
Foreign-body granuloma
Sarcoidosis
Crohn disease
Tuberculosis
Histoplasmosis
Eosinophilic gastritis
Tertiary syphilis: infiltrative/ulcerative/tumorous type
Echinococcal cyst
PANCREATIC ABNORMALITIES
Ectopic pancreas
Annular pancreas
Pancreatic pseudocyst
DEPOSITS
Amyloid
Endometriosis
Localized hematoma
OTHERS
Varices (ie, fundal)
Duplications (4% of all GI tract duplications)
Gastric Filling Defects
INTRINSIC WALL LESIONS
benign (most common)
Polyps: hyperplastic, adenomatous, villous, hamartomatous (Peutz-Jeghers syndrome, Cowden disease)
Leiomyoma
Granulomatous lesions
Eosinophilic granuloma
Crohn disease
Tuberculosis
Sarcoidosis
Pseudolymphoma = benign reactive proliferation of lymphoid tissue
Extramedullary hematopoiesis
Ectopic pancreas
Gastric duplication cyst
Intramural hematoma
Esophagogastric herniation
malignant
Gastric carcinoma, lymphoma
Gastric sarcoma: leiomyosarcoma, liposarcoma, leiomyoblastoma
Gastric metastases: melanoma, breast, pancreas, colon
EXTRINSIC IMPRESSIONS ON STOMACH
in 70% nonneoplastic (extrinsic pseudotumors in 20%)
normal organs: organomegaly, tortuous aorta, heart, cardiac aneurysm
benign masses:
cysts of pancreas, liver, spleen, adrenal, kidney; gastric duplication, postoperative deformity (eg, Nissen fundoplication)
malignant masses: enlarged celiac nodes
inflammatory lesion:
left subphrenic abscess/hematoma
lateral displacement: enlarged liver, aortic aneurysm, enlarged celiac nodes
medial displacement: splenomegaly, mass in colonic splenic flexure, cardiomegaly, subphrenic abscess
INTRALUMINAL GASTRIC MASSES
Bezoar
Foreign bodies: food, pills, blood clot, gallstone
TUMORS OF ADJACENT ORGANS
Pancreatic carcinoma + cystadenoma
Liver carcinoma
Carcinoma of gallbladder
Colonic carcinoma
Renal carcinoma
Adrenal carcinoma
Lymph node involvement
THICKENED GASTRIC FOLDS
Filling Defect of Gastric Remnant
IATROGENIC
surgical deformity/plication defect, suture granuloma
INFLAMMATORY
bile reflux gastritis, hyperplastic polyps
INTUSSUSCEPTION
Jejunogastric intussusception
(efferent loop in 75%, afferent loop in 25%)
(a) acute form: high intestinal obstruction, left hypochondriac mass, hematemesis
(b) chronic/intermittent form: may be self-reducing
 coiled spring appearance of gastric filling defect
coiled spring appearance of gastric filling defect
Gastrojejunal/gastroduodenal mucosal prolapse
often asymptomatic
bleeding partial obstruction
NEOPLASTIC
Gastric stump carcinoma: >5 years after resection for benign disease; 15% within 10 years; 20% after 20 years
Recurrent carcinoma (10%) secondary to incomplete removal of gastric cancer
Malignancy at anastomosis (incomplete resection)
INTRALUMINAL MATTER: bezoar
mnemonic: PUBLICS Polyp (hyperplastic polyp due to bile reflux)
Ulcer (anastomotic)
Bezoar, Blind loop syndrome
Loop (afferent loop syndrome)
Intussusception at gastrojejunostomy
Cancer (recurrent, residual, de novo)
Surgical deformity, Suture granuloma
P.772
Thickened Gastric Folds
INFLAMMATION/INFECTION
Inflammatory gastritis:
alcoholic, hypertrophic, antral, corrosive, postirradiation, gastric cooling
Crohn disease
Sarcoidosis
Infectious gastritis:
bacterial invasion, bacterial toxins from botulism, diphtheria, dysentery, typhoid fever, anisakiasis, TB, syphilis
Pseudolymphoma
MALIGNANCY
Lymphoma
Gastric carcinoma
INFILTRATIVE PROCESS
Eosinophilic gastritis
Amyloidosis
PANCREATIC DISEASE
Pancreatitis
Direct extension from pancreatic carcinoma
OTHERS
Zollinger-Ellison syndrome
M n trier disease
Gastric varices
mnemonic: ZEAL VOLUMES C3MP3 Zollinger-Ellison syndrome
Amyloidosis
Lymphoid hyperplasia
Varices
Operative defect
Lymphoma
Ulcer disease (peptic)
M n trier disease
Eosinophilic gastroenteritis
Syphilis
Crohn disease, Carcinoma, Corrosive gastritis
Pancreatitis, Pancreatic carcinoma,
Postradiation gastritis
Bull's-eye Lesions
PRIMARY NEOPLASMS
Leiomyoma, leiomyosarcoma
Lymphoma
Carcinoid
Primary carcinoma
HEMATOGENOUS METASTASES
Malignant melanoma
 usually spares large bowel
usually spares large bowel
Breast cancer (15%)
 scirrhous appearance in stomach
scirrhous appearance in stomach
Cancer of lung
Renal cell carcinoma
Kaposi sarcoma
Bladder carcinoma
ECTOPIC PANCREAS
in duodenum/stomach
EOSINOPHILIC GRANULOMA
most frequently in stomach
Complications of Postoperative Stomach
Filling defect of gastric remnant
Retained gastric antrum
Dumping syndrome
Afferent loop syndrome
Stomal obstruction
temporary reversible: edema of suture line, abscess/hematoma, potassium deficiency, inadequate electrolyte replacement, hypoproteinemia, hypoacidity
late mechanical: stomal ulcer (75%)
mnemonic: LOBULATING
Leaks (early)
Obstruction (early)
Bezoar
Ulcer (especially marginal)
Loop (afferent loop syndrome)
Anemia (macrocytic secondary to decreased intrinsic factor)
Tumor (? increased incidence)
Intussusception
Not feeling well after meals (dumping syndrome)
Gastritis (bile reflux)
Lesions Involving Stomach and Duodenum = Transpyloric Disease
Lymphoma: in up to 40% of patients with lymphoma
Gastric carcinoma: in 5 25%, but 50 more common than lymphoma
Peptic ulcer disease
Tuberculosis: in 10% of gastric TB
Crohn disease: pseudo-Billroth-I pattern
Strongyloidiasis
Eosinophilic gastroenteritis
Duodenum
Congenital Duodenal Obstruction
bile-stained vomiting delayed until after first feeding and increasing progressively
 double bubble sign
double bubble sign
Duodenal atresia/severe stenosis
Annular pancreas
Midgut volvulus
Duodenal web
Ladd bands
Preduodenal portal vein
Duodenal duplication cyst
Extrinsic Pressure Effect on Duodenum
BILE DUCTS
normal impression, dilated CBD, choledochal cyst
GALLBLADDER
normal impression, gallbladder hydrops, Courvoisier phenomenon, gallbladder carcinoma, pericholecystic abscess
LIVER
hepatomegaly, hypertrophied caudate lobe, anomalous hepatic lobe, hepatic cyst, hepatic tumor
RIGHT KIDNEY
bifid collecting system, hydronephrosis, multiple renal cysts, polycystic kidney disease, hypernephroma
RIGHT ADRENAL
adrenal carcinoma, enlargement in Addison disease
COLON
duodenocolic apposition due to anomalous peritoneal fixation, carcinoma of hepatic flexure
VESSELS
lymphadenopathy, duodenal varices, dilated arterial collaterals, aortic aneurysm, intramural/mesenteric hematoma
P.773
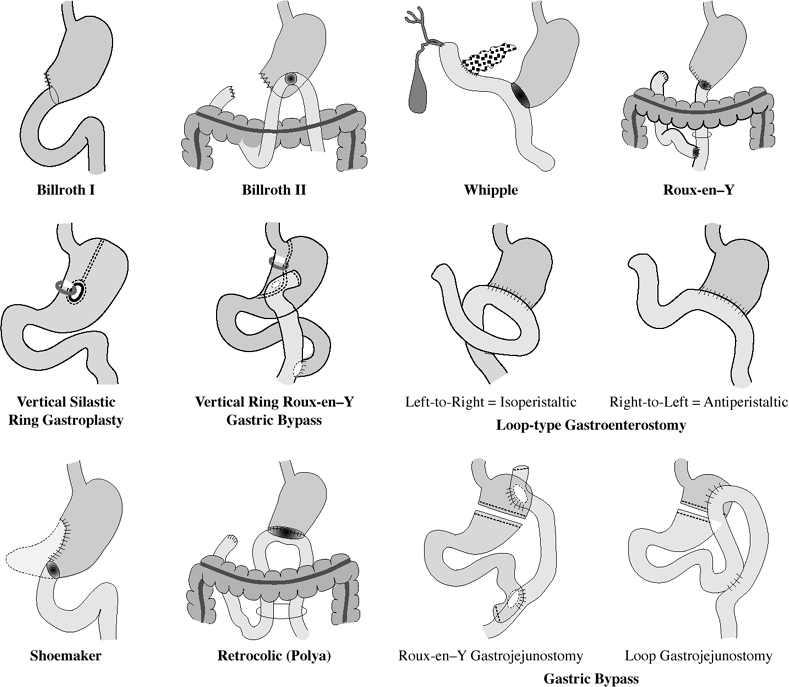 |
| Gastric Surgical Procedures |
Widened Duodenal Sweep
NORMAL VARIANT
PANCREATIC LESION
Acute pancreatitis
Chronic pancreatitis
Pancreatic pseudocyst
Pancreatic carcinoma
Metastasis to pancreas
Pancreatic cystadenoma
VASCULAR LESION
Lymph node enlargement: lymphoma, metastasis, inflammation
Cystic lymphangioma of the mesentery
RETROPERITONEAL MASS
Aortic aneurysm
Choledochal cyst
Thickened Duodenal Folds
INFLAMMATION
within bowel wall:
peptic ulcer disease, Zollinger-Ellison syndrome, regional enteritis, lymphoid hyperplasia, uremia
surrounding bowel wall:
pancreatitis, cholecystitis
INFECTION
giardiasis, TB, strongyloidiasis, celiac disease
NEOPLASIA
lymphoma, metastases to peripancreatic nodes
DIFFUSE INFILTRATIVE DISORDER
Whipple disease, amyloidosis, mastocytosis, eosinophilic enteritis, intestinal lymphangiectasia
VASCULAR DISORDER
duodenal varices, mesenteric arterial collaterals, intramural hemorrhage (trauma, Sch nlein-Henoch purpura), chronic duodenal congestion (congestive heart failure, portal venous hypertension); lymphangiectasia
HYPOPROTEINEMIA
nephrotic syndrome, M n trier disease, protein-losing enteropathy
GLANDULAR ENLARGEMENT
Brunner gland hyperplasia, cystic fibrosis
P.774
| mnemonic: | BAD HELP |
Brunner gland hyperplasia
Amyloidosis
Duodenitis (Z-E syndrome, peptic)
Hemorrhage
Edema, Ectopic pancreas
Lymphoma
Pancreatitis, Parasites
Duodenal Filling Defect
EXTRINSIC
gallbladder impression, CBD impression, gas-filled diverticulum
INTRINSIC TO WALL
benign neoplastic mass
Adenoma
Leiomyoma
Lipoma
Hamartoma (Peutz-Jeghers syndrome)
Prolapsed antral polyp
Brunner gland adenoma
Villous adenoma
Islet cell tumor
Gangliocytic paraganglioma
malignant neoplastic mass
Carcinoid tumor
Adenocarcinoma
Ampullary carcinoma
Lymphoma
Sarcoma
Metastasis (stomach, pancreas, gallbladder, colon, kidney, melanoma)
Retroperitoneal lymph node involvement
nonneoplastic mass
Papilla of Vater
Choledochocele
Duplication cyst
Pancreatic pseudocyst
Duodenal varix
Mesenteric artery collaterals
Intramural hematoma
Adjacent abscess, stitch abscess
Ectopic pancreas, heterotopic gastric mucosa
Prolapsed antral mucosa
Brunner gland hyperplasia
Benign lymphoid hyperplasia
INTRALUMINAL
Blood clot
Foreign body: fruit pit, gallstone, feeding tube
Duodenal Tumor
Benign Duodenal Tumors
Leiomyoma (27%)
Adenomatous polyp (21%)
Lipoma (21%)
Brunner gland adenoma (17%)
Angiomatous tumor (6%)
Ectopic pancreas (2%)
Duodenal cyst (2%)
Neurofibroma (2%)
Hamartoma (2%)
Malignant Duodenal Tumors
Adenocarcinoma (73%)
Location: 40% in duodenum, most often in 2nd + 3rd portion = periampullary neoplasm
(a) suprapapillary: apt to cause obstruction + bleeding
(b) peripapillary: extrahepatic jaundice
(c) intrapapillary: GI bleedingPredisposed: Gardner syndrome, celiac disease May be associated with: Peutz-Jeghers syndrome
annular/polypoid/ulcerativeMetastases: regional lymph nodes (2/3) DDx: (1) Primary bile duct carcinoma
(2) Ampullary carcinomaLeiomyosarcoma (14%)
most often beyond 1st portion of duodenum
 up to 20 cm in size
up to 20 cm in size frequently ulcerated exophytic mass
frequently ulcerated exophytic mass
Carcinoid (11%)
Lymphoma (2%)
 marked wall thickening
marked wall thickening bulky periduodenal lymphadenopathy
bulky periduodenal lymphadenopathy
Enlargement of Papilla of Vater
[Abraham Vater (1684 1751), anatomist in Wittenberg, Germany]
Normal variant
identified in 60% of UGI series; atypical location in 3rd portion of duodenum in 8%; 1.5 cm in diameter in 1% of normals
Papillary edema
Impacted stone
Pancreatitis (Poppel sign)
Acute duodenal ulcer disease
Papillitis
Perivaterian neoplasms
= tumor mass + lymphatic obstruction
1. Adenocarcinoma
2. Adenomatous polyp (premalignant lesion)
 irregular surface + erosions
irregular surface + erosions
Lesions simulating enlarged papilla
Benign spindle cell tumor
Ectopic pancreatic tissue
P.775
Duodenal Narrowing
DEVELOPMENTAL ANOMALIES
Duodenal atresia
Congenital web/duodenal diaphragm
Intraluminal diverticulum
Duodenal duplication cyst
Annular pancreas
Midgut volvulus, peritoneal bands (Ladd bands)
INTRINSIC DISORDERS
inflammation/infection
Postbulbar ulcer
Crohn disease
Sprue
Tuberculosis
Strongyloidiasis
tumor
duodenal/ampullary malignancy
DISEASE IN ADJACENT STRUCTURES
Pancreatitis, pseudocyst, pancreatic carcinoma
Cholecystitis
Contiguous abscess
Metastases to pancreaticoduodenal nodes (lymphoma, lung cancer, breast cancer)
TRAUMA
Duodenal rupture
Intramural hematoma
VASCULAR
Superior mesenteric artery syndrome
Aorticoduodenal fistula
Preduodenal portal vein (anterior to descending duodenum)
Dilated Duodenum
| Megaduodenum | = marked dilatation of entire C-loop |
| Megabulbus | = dilatation of duodenal bulb only |
VASCULAR COMPRESSION
superior mesenteric artery syndrome, abdominal aortic aneurysm, aorticoduodenal fistula
PRIMARY DUODENAL ATONY
scleroderma, dermatomyositis, SLE
Chagas disease, aganglionosis, neuropathy, surgical/chemical vagotomy
focal ileus: pancreatitis, cholecystitis, peptic ulcer disease, trauma
altered emotional status, chronic idiopathic intestinal pseudoobstruction
INFLAMMATORY/NEOPLASTIC INDURATION OF MESENTERIC ROOT
Crohn disease, tuberculous enteritis, pancreatitis, peptic ulcer disease, strongyloidiasis, metastatic disease
FLUID DISTENSION
celiac disease, Zollinger-Ellison syndrome
Postbulbar Ulceration
Benign postbulbar peptic ulcer
 medial aspect of upper 2nd portion
medial aspect of upper 2nd portion incisura pointing to ulcer
incisura pointing to ulcer occasionally barium reflux into common bile duct
occasionally barium reflux into common bile duct ring stricture
ring stricture stress- and drug-induced ulcers heal without deformity
stress- and drug-induced ulcers heal without deformity
Zollinger-Ellison syndrome
 multiple ulcers distal to duodenal bulb
multiple ulcers distal to duodenal bulb thickening of folds + hypersecretion
thickening of folds + hypersecretion
Leiomyoma
Malignant tumors:
primaries
adenocarcinoma, lymphoma, sarcoma
contiguous spread
pancreas, colon, kidney, gallbladder
hematogenous spread
melanoma, Kaposi sarcoma
lymphogenic spread
metastases to periduodenal lymph nodes
Granulomatous disease: Crohn disease, TB
Aorticoduodenal fistula
Mimickers: ectopic pancreas, diverticulum
Small Bowel
Anatomic Predilection for Intestinal Involvement
| @ proximal jejunum | diverticulosis, giardiasis, adenocarcinoma, Whipple disease, Z-E syndrome, celiac disease |
| @ distal ileum | Crohn disease, TB, infectious enteritis, lymphoma, carcinoid, metastases |
| @ mesenteric border | diverticulosis, Crohn disease, mesenteric hematoma, intraperitoneal spread of tumor |
| @ antimesenteric border | Meckel diverticulum, sacculations in scleroderma, hematogenous metastases |
Increased Fluid within Small Bowel
Ingestion
Resection/removal of stomach
Small-bowel obstruction
Enteritis
Malabsorption: celiac disease, Whipple disease
Peritoneal carcinomatosis
Small Bowel Diverticula
TRUE DIVERTICULA
Duodenal diverticula
Racemose diverticula: bizarre, lobulated
Giant diverticula
Intraluminal diverticula: result of congenital web/diaphragm
Jejunal diverticulosis
Meckel diverticulum
PSEUDODIVERTICULA
Scleroderma
Crohn disease
Lymphoma
Mesenteric ischemia
Communicating ileal duplication
Giant duodenal ulcer
P.776
Small Bowel Ulcer
Aphthous Ulcers of Small Bowel
INFECTION
Yersinia enterocolitis (25%)
Salmonellosis
Tuberculosis
Rickettsiosis
INFLAMMATION
Crohn disease (22%)
Beh et syndrome
Reiter syndrome
Ankylosing spondylitis
Large Nonstenotic Ulcers of Small Bowel
Primary nonspecific ulcer 47% incidence
Yersiniosis 33%
Crohn disease 30%
Tuberculosis 18%
Salmonellosis/shigellosis 7%
Meckel diverticulum 5%
Multiple Small Bowel Ulcers
DRUGS
Potassium tablets
Steroids
Nonsteroidal antiinflammatory drugs
INFECTION/INFLAMMATION
Bacillary dysentery
Ischemic enteritis
Ulcerative jejunoileitis as complication of celiac disease
TUMOR
Neoplasms
Intestinal lymphoma
Cavitary Small Bowel Lesion
PRIMARY TUMOR
Lymphoma (exoenteric form)
Leiomyosarcoma (exoenteric form)
Primary adenocarcinoma
METASTASIS
Malignant melanoma
Lung cancer
INFLAMMATION
Diverticulitis with abscess (Meckel, jejunal)
Communicating duplication cyst
Separation of Bowel Loops
INFILTRATION OF BOWEL WALL/MESENTERY
inflammation/infection
Crohn disease
TB
Radiation injury
Retractile mesenteritis
Intraperitoneal abscess
deposits
Intestinal hemorrhage/mesenteric vascular occlusion
Whipple disease
Amyloidosis
tumor
Carcinoid tumor: local release of serotonin responsible for muscular thickening + fibroplastic proliferation = desmoplastic reaction
Primary carcinoma of small bowel (unusual presentation)
Lymphoma
Neurofibromatosis
ASCITES/INTRAPERITONEAL BLEEDING
hepatic cirrhosis (75%), peritonitis, peritoneal carcinomatosis, congestive heart failure, constrictive pericarditis, primary/metastatic lymphatic disease
EXTRINSIC MASS
Intraperitoneal spread of tumor: peritoneal mesothelioma, mesenteric tumors (fibroma, lipoma, fibrosarcoma, leiomyosarcoma, malignant mesenteric lymphoid tumor, metastases)
Interloop abscesses/loculated fluid collection
Endometriosis
Retractile mesenteritis (fibrosis, fatty infiltration, panniculitis)
Mesenteric fat deposits
Fibrofatty proliferation: Crohn disease, mesenteric panniculitis
Normal Small Bowel Folds & Diarrhea
Pancreatic insufficiency
Lactase deficiency
Lymphoma/pseudolymphoma
Dilated Small Bowel & Normal Folds
| mnemonic: | SOS |
Sprue
Obstruction
Scleroderma
EXCESSIVE FLUID
mechanical obstruction
due to adhesion, hernia, neoplasm
 string-of-beads sign = air bubbles between mucosal folds in a fluid-filled small bowel
string-of-beads sign = air bubbles between mucosal folds in a fluid-filled small bowel pseudotumor sign = closed-loop obstruction
pseudotumor sign = closed-loop obstruction
malabsorption syndromes
Celiac disease, tropical + nontropical sprue
Lactase deficiency
BOWEL WALL PARALYSIS
= functional ileus = adynamic ileus
1. Surgical vagotomy
2. Chemical vagotomy from drug effects: atropine-like substances, morphine, L-dopa, glucagon
3. Chagas disease
4. Metabolic: hypokalemia, diabetes
5. Intrinsic + extrinsic intraabdominal inflammation
6. Chronic idiopathic pseudoobstruction
VASCULAR COMPROMISE
Mesenteric ischemia (atherosclerosis)
Acute radiation enteritis
Amyloidosis
SLE
BOWEL WALL DESTRUCTION
Lymphoma
Scleroderma (smooth muscle atrophy)
Dermatomyositis
P.777
Abnormal Small Bowel Folds
Abnormal Folds + Increased Intraluminal Fluid
Malabsorption syndrome
Crohn disease, infectious enteritis
Parasitic infestation/giardiasis
Ischemia proximal to an obstruction
Zollinger-Ellison syndrome
Lymphangiectasia, mesenteric lymphadenopathy
Thickened Folds of Stomach & Small Bowel
Lymphoma
Crohn disease
Eosinophilic gastroenteritis
Zollinger-Ellison syndrome
M n trier disease
Cirrhosis = gastric varices + hypoproteinemia
Amyloidosis
Whipple disease
Systemic sclerosis
Thickened Smooth Folds Dilatation
EDEMA
hypoproteinemia
Cirrhosis
Nephrotic syndrome
Protein-losing enteropathy (celiac disease, Whipple disease)
increased capillary permeability
Angioneurotic edema
Gastroenteritis
increased hydrostatic pressure
Portal venous hypertension
Zollinger-Ellison syndrome
HEMORRHAGE
vessel injury
Ischemia
Infarction
Trauma
vasculitis
Connective tissue disease
Henoch-Sch nlein purpura
Thrombangitis obliterans, irradiation
hypocoagulability
Hemophilia
Anticoagulant therapy
Hypofibrinogemia
Circulating anticoagulants
Fibrinolytic system activation
Idiopathic thrombocytopenic purpura
Coagulation defects (leukemia, lymphoma, multiple myeloma, metastatic carcinoma)
Hypoprothrombinembinema
LYMPHATIC BLOCKAGE
Tumor infiltration: lymphoma, pseudolymphoma
Irradiation
Mesenteric fibrosis
Intestinal lymphangiectasia
Whipple disease
DEPOSITS
Eosinophilic enteritis
Pneumatosis intestinalis
Amyloidosis
Abetalipoproteinemia
Crohn disease
Graft-versus-host disease
Immunologic deficiency: hypo-/dysgammaglobulinemia
Thickened Irregular Folds Dilatation
INFLAMMATION
Crohn disease
NEOPLASTIC
Lymphoma, pseudolymphoma
INFECTION
protozoan
giardiasis, strongyloidiasis, hookworm
bacterial
Yersinia enterocolitica, typhoid fever, tuberculosis
fungal: histoplasmosis
AIDS-related infection
IDIOPATHIC
lymphatic dilatation
Lymphangiectasia
Inflammatory process, tumor growth, irradiation fibrosis
Whipple disease
cellular infiltration
Eosinophilic enteritis
Mastocytosis
deposits
Zollinger-Ellison syndrome
Amyloidosis
Alpha chain disease: defective secretory IgA system
A- -lipoproteinemia: recessive, retinitis pigmentosa, neurologic disease
A- -lipoproteinemia
Fibrocystic disease of the pancreas
Polyposis syndrome
| mnemonic: | G. WILLIAMS |
Giardiasis
Whipple disease, Waldenstr m macroglobulinemia
Ischemia
Lymphangiectasia
Lymphoma
Inflammation
Amyloidosis, Agammaglobulinemia
Mastocytosis, Malabsorption
Soft-tissue neoplasm (carcinoid, lipoma)
Tethered Folds
= indicative of desmoplastic reaction
 kinking, angulation, tethering, separation of bowel loops
kinking, angulation, tethering, separation of bowel loops1. Carcinoid
2. Postoperative in Gardner syndrome
3. Retractile mesenteritis
4. Hodgkin disease
5. Peritoneal implants
6. Endometriosis
7. Tuberculous peritonitis
8. Mesothelioma
9. Postoperative adhesions
P.778
Atrophy of Small Bowel Folds
Chronic malabsorption: celiac disease
Chronic ischemic changes: radiation injury, amyloidosis
Crohn disease in burned-out stage
Parasitic infestation: strongyloidiasis
Graft-versus-host disease
Ribbonlike Small Bowel
= featureless/tubular nature of small bowel with effacement of folds
1. Graft-versus-host disease
2. Celiac disease
3. Small bowel infection (eg, viral enteritis)
4. Injury from radiation/corrosive medication
5. Allergy (eg, soybeans)
6. Ischemia
7. Amyloid, mastocytosis
8. Lymphoma, pseudolymphoma
9. Crohn disease
Delayed Small Bowel Transit
= transit time >6 hours
| mnemonic: | SPATS DID |
Scleroderma
Potassium (hypokalemia)
Anxiety
Thyroid (hypothyroidism)
Sprue
Diabetes (poorly controlled)
Idiopathic
Drugs (opiates, atropine, phenothiazine)
Constricting Lesion of Small Bowel
Primary adenocarcinoma (proximal jejunum)
Carcinoid (distal ileum)
Lymphoma, metastasis
Endometriosis
Adhesion, mucosal diaphragm
Strictures: Crohn disease, radiation enteritis, ischemia, potassium chloride tablets
Multiple Stenotic Lesions of Small Bowel
Crohn disease
End-stage radiation enteritis
Metastatic carcinoma
Endometriosis
Eosinophilic gastroenteritis
Tuberculosis
Drug-induced (eg, potassium chloride tablets, NSAIDs)
Small Bowel Filling Defects
Solitary Filling Defect of Small Bowel
INTRINSIC TO BOWEL WALL
benign neoplasm: leiomyoma (97%), adenoma, lipoma, hemangioma, neurofibroma
malignant primary: adenocarcinoma, lymphoma (desmoplastic response), sarcoma, carcinoid
metastases: from melanoma, lung, kidney, breast
inflammation: inflammatory pseudotumor
infection: parasites
EXTRINSIC TO BOWEL WALL
Duplication cyst
Endometrioma
INTRALUMINAL
Gallstone ileus
Parasites (ascariasis, strongyloidiasis)
Inverted Meckel diverticulum
Blood clot
Foreign body, bezoar, pills, seeds
Multiple Filling Defects of Small Bowel
POLYPOSIS SYNDROMES
Peutz-Jeghers syndrome
Gardner syndrome
Disseminated gastrointestinal polyposis
Generalized gastrointestinal juvenile polyposis
Cronkhite-Canada syndrome
BENIGN TUMORS
Multiple simple adenomatous polyps
Hemangioma, blue rubber bleb nevus syndrome
Leiomyoma, neurofibroma, lipoma
Nodular lymphoid hyperplasia
= normal terminal ileum in children + adolescents; may be associated with dysgammaglobulinemia
 symmetric fairly sharply demarcated filling defects
symmetric fairly sharply demarcated filling defects
Varices (= multiple phlebectasia in jejunum, oral mucosa, tongue, scrotum)
MALIGNANT TUMORS
Carcinoid tumor
Lymphoma
primary lymphoma (rarely multiple)
secondary lymphoma: gastrointestinal involvement in 63% of disseminated disease; 19% in small intestine
Kaposi sarcoma
Submucosal metastases: melanoma > lung > breast > choriocarcinoma > kidney > stomach, uterus, ovary, pancreas
INTRALUMINAL
Gallstones
Foreign bodies, food particles, seeds, pills
Parasites: ascariasis, strongyloidiasis, hookworm, tapeworm
Sandlike Lucencies of Small Bowel
Waldenstr m macroglobulinemia
Mastocytosis
Histoplasmosis
Nodular lymphoid hyperplasia
Intestinal lymphangiectasia
Eosinophilic gastroenteritis
Lymphoma
Crohn disease
Whipple disease
Yersinia enterocolitis
Cronkhite-Canada syndrome
Cystic fibrosis
Food particles/gas bubbles
Strongyloides stercoralis
P.779
P.780
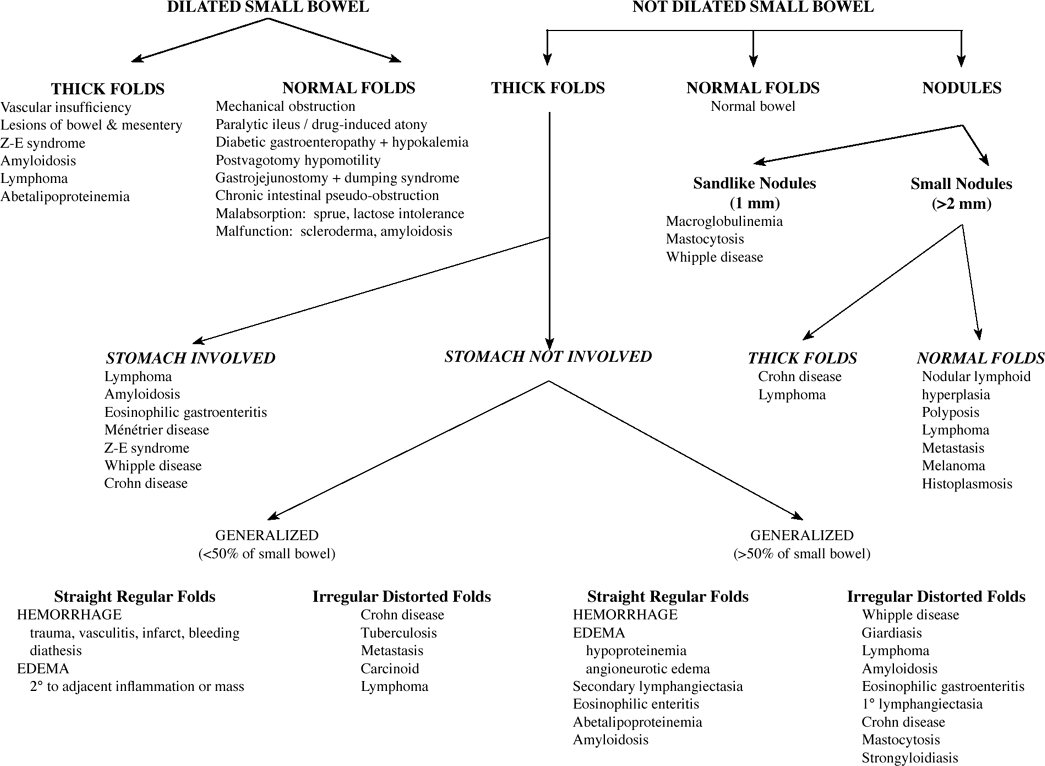 |
| ABNORMAL SMALL BOWEL CALIBER & CONTOUR |
Small Bowel Tumors
| Incidence: | 1:100,000; 1.5 6% of all GI neoplasms |
Malignant:benign = 1:1
Symptomatic malignant:symptomatic benign = 3:1
Location of small bowel primaries:
ileum (41%), jejunum (36%), duodenum (18%)
ROENTGENOGRAPHIC APPEARANCE:
pedunculated intraluminal tumor, usually originating from mucosa
 smooth/irregular surface without visible mucosal pattern
smooth/irregular surface without visible mucosal pattern moves within intestinal lumen twice the length of the stalk
moves within intestinal lumen twice the length of the stalk
sessile intraluminal tumor without stalk, usually from tissues outside mucosa
 smooth/irregular surface without visible mucosal pattern
smooth/irregular surface without visible mucosal pattern
intra-/extramural tumor
 base of tumor greater than any part projecting into the lumen
base of tumor greater than any part projecting into the lumen mucosal pattern visible, may be stretched
mucosal pattern visible, may be stretched
serosal tumor
 displacement of adjacent loops
displacement of adjacent loops small bowel obstruction (rare)
small bowel obstruction (rare) coil-spring pattern of intussusceptum
coil-spring pattern of intussusceptum
CT:
 small bowel wall >1.5 cm thick
small bowel wall >1.5 cm thick
| Cx: | small-bowel obstruction (in up to 10%) |
Benign Small Bowel Tumors
asymptomatic (80%)
melena, intermittent abdominal pain, weakness
palpable abdominal mass (20%)
Types:
Leiomyoma (36 49%)
Location: any segment Adenoma (15 20%)
Lipoma (14 16%)
Location: duodenum (32%), jejunum (17%), ileum (51%)
fat-density on CTHemangioma (13 16%)
Lymphangioma (5%)
Location: duodenum > jejunum > ileum Neurogenic tumor (1%)
Malignant Small Bowel Tumors
| At risk: | Crohn disease, celiac disease, polyposis syndromes, history of small-bowel diverting surgery |
asymptomatic (10 30%)
pain due to intermittent obstruction (80%)
weight loss (66%)
gastrointestinal blood loss (50%)
palpable abdominal mass (50%)
PRIMARY MALIGNANT SMALL BOWEL TUMOR
Carcinoid (25 41%)
 Most common primary small bowel tumor!
Most common primary small bowel tumor!Location: predominantly distal ileum  calcified mesenteric mass on CT
calcified mesenteric mass on CT
Adenocarcinoma (25 26%)
Location: duodenum (48%), jejunum (44%), ileum (8%) Non-Hodgkin lymphoma (16 17%)
 2nd most common location after stomach
2nd most common location after stomach aneurysmal dilatation
aneurysmal dilatation
Gastrointestinal stromal tumor (GIST)
= leiomyosarcoma (9 10%)
Location: ileum (50%) Vascular malignancy (1%)
Fibrosarcoma (0.3%)
Secondary Malignant Small Bowel Tumor
 Most common neoplasm of small intestines!
Most common neoplasm of small intestines!
Cecum
Primary Neoplasm of the Appendix
Mucinous adenoma (44%)/adenocarcinoma (23%)
Colonic-type adenocarcinoma (13%)
NHL
Carcinoid tumor
| Incidence: | 0.5 1.0% of appendectomy specimens |
appendicitis symptomatology (30 50%)
 appendiceal diameter increased >15 mm (86%)
appendiceal diameter increased >15 mm (86%) cystic dilatation of appendix (mucocele)
cystic dilatation of appendix (mucocele) soft-tissue mass
soft-tissue mass appendiceal wall thickening
appendiceal wall thickening periappendiceal fat stranding
periappendiceal fat stranding
Ileocecal Valve Abnormalities
Lipomatosis: >40 years of age, female
 stellate/rosette pattern
stellate/rosette pattern
NEOPLASM
Lipoma, adenomatous polyp, villous adenoma
Carcinoid tumor
Adenocarcinoma: 2% of all colonic cancers
Lymphoma: often involving terminal ileum
INFLAMMATION
Crohn disease
Ulcerative colitis
 patulous valve, fixed in open position
patulous valve, fixed in open position
Tuberculosis
Amebiasis
 terminal ileum not involved (in USA)
terminal ileum not involved (in USA)
Typhoid fever, anisakiasis, schistosomiasis, actinomycosis
Cathartic abuse
PROLAPSE
antegrade: indistinguishable from lipomatosis/prolapsing mucosa/neoplasm
retrograde
INTUSSUSCEPTION
LYMPHOID HYPERPLASIA
P.781
Coned Cecum
INFLAMMATION
Crohn disease
 involvement of ascending colon + terminal ileum
involvement of ascending colon + terminal ileum
Ulcerative colitis
 backwash ileitis (in 10%)
backwash ileitis (in 10%) gaping ileocecal valve
gaping ileocecal valve
Appendicitis
Typhlitis
Perforated cecal diverticulum
INFECTION
Tuberculosis
 colonic involvement more prominent than that of terminal ileum
colonic involvement more prominent than that of terminal ileum
Amebiasis
 involvement of cecum in 90% of amebiasis
involvement of cecum in 90% of amebiasis thickened ileocecal valve fixed in open position
thickened ileocecal valve fixed in open position reflux into normal terminal ileum
reflux into normal terminal ileum skip lesions in colon
skip lesions in colon
Actinomycosis
palpable abdominal mass
indolent sinus tracts in abdominal wall
Blastomycosis
Anisakiasis
Typhoid, Yersinia
TUMOR
Carcinoma of the cecum
Metastasis to cecum
Cecal Filling Defect
ABNORMALITIES OF THE APPENDIX
Acute appendicitis/appendiceal abscess
Crohn disease
Inverted appendiceal stump/appendiceal intussusception
Mucocele
Myxoglobulosis
Appendiceal neoplasm: carcinoid tumor (90%), leiomyoma, neuroma, lipoma, adenocarcinoma, metastasis
COLONIC LESION
Ameboma
Primary cecal neoplasm
Ileocolic intussusception
Lipomatosis of ileocecal valve
UNUSUAL ABNORMALITIES
Ileocecal diverticulitis (in 50% < age 30 years)
Solitary benign ulcer of the cecum
Adherent fecolith (eg, in cystic fibrosis)
Endometriosis
Burkitt lymphoma
| mnemonic: | CECUM TIP SALE |
Carcinoma
Enteritis
Carcinoid
Ulcerative colitis
Mucocele of appendix
Tuberculosis
Intussusception
Periappendiceal abscess
Stump of the appendix
Ameboma
Lymphoma
Endometriosis
Appendiceal Intussusception
Mucocele
Endometrioma
Fecolith
Foreign body
Polyp (juvenile, inflammatory)
Papilloma
Adenoma/adenocarcinoma
Carcinoid tumor
Postappendectomy stump
Pericecal Fat-Stranding on CT
Appendicitis
Crohn disease
Tuboovarian abscess
Cecal diverticulitis
Perforated cecal carcinoma
Colon
Colon Transit Time
Sitzmarks diagnostic test:
| Indication: | adults with severe constipation but otherwise normal GI examination |
1. Withhold laxatives/enemas/suppositories for 5 days
2. Patient takes 1 capsule (contains 24 radiopaque polyvinyl chloride markers of 1 4.5 mm)
3. Take KUB on day 3 and 5 to determine location + extent of marker elimination
19 markers (80%) expelled = grossly normal colonic transit time
markers scattered about the colon = colonic hypomotility/inertia
markers in rectum/rectosigmoid = functional outlet obstruction (eg, internal rectal prolapse/anismus)
5 markers (20%) retained need follow-up KUB on day 7
 All markers are usually in colon by 12 hours
All markers are usually in colon by 12 hours
Colon Cutoff Sign
= abrupt termination of colonic gas column at splenic flexure with decompression of the distal colon due to spasm + obstruction at the splenic flexure impinging on a paralytic transverse colon
IMPINGEMENT VIA PHRENICOCOLIC LIGAMENT
Acute pancreatitis/postpancreatitic stricture
Pancreatic/gastric carcinoma
Hemorrhage from rupture of splenic artery/abdominal aortic aneurysm
COLONIC DISEASE
Colon cancer
Mesenteric thrombosis
Ischemic colitis
Perforated appendicitis (in 20%)
N.B.: amputation of gas at the hepatic flexure due to spastic ascending colon
P.782
Colonic Thumbprinting
= sharply defined fingerlike marginal indentations at contours of wall
1. ISCHEMIA = Ischemic colitis
occlusive vascular disease, hypercoagulability state, hemorrhage into bowel wall (bleeding diathesis, anticoagulants), traumatic intramural hematoma
2. INFLAMMATION
ulcerative colitis, Crohn colitis
3. INFECTION
acute amebiasis, schistosomiasis, strongyloidiasis, cytomegalovirus (in renal transplant recipients), pseudomembranous colitis
4. MALIGNANT LESIONS
localized primary lymphoma, hematogenous metastases
5. MISCELLANEOUS
endometriosis, amyloidosis, pneumatosis intestinalis, diverticulosis, diverticulitis, hereditary angioneurotic edema
| mnemonic: | PSALM II |
Pseudomembranous colitis
Schistosomiasis
Amebic colitis
Lymphoma
Metastases (to colon)
Ischemic colitis
Inflammatory bowel disease
Colonic Urticaria Pattern
OBSTRUCTION
Obstructing carcinoma
Cecal volvulus
Colonic ileus
ISCHEMIA
INFECTION/INFLAMMATION
Yersinia enterocolitis
Herpes
Crohn disease
URTICARIA
Colonic Ulcers
IDIOPATHIC
Ulcerative colitis
Crohn colitis
ISCHEMIC
Ischemic colitis
TRAUMATIC
Radiation injury
Caustic colitis
NEOPLASTIC
Primary colonic carcinoma
Metastases (prostate, stomach, lymphoma, leukemia)
INFLAMMATORY
Pseudomembranous colitis
Pancreatitis
Diverticulitis
Beh et syndrome
Solitary rectal ulcer syndrome
Nonspecific benign ulceration
INFECTION
protozoan
Amebiasis
Schistosomiasis
Strongyloidiasis
bacterial
Shigellosis, salmonellosis
Staphylococcal colitis
Tuberculosis
Gonorrheal proctitis
Yersinia colitis
Campylobacter fetus colitis
fungal
histoplasmosis, mucormycosis, actinomycosis, candidiasis
viral
Lymphogranuloma venereum
Herpes proctocolitis
Cytomegalovirus (transplants)
Aphthous Ulcers of Colon
Crohn disease
Amebic colitis
Yersinia enterocolitis
Organism: gram-negative
fever, diarrhea, RLQ painLocation: terminal ileum
thickened folds + ulceration
lymphoid nodular hyperplasiaSalmonella, shigella infection
Herpes virus infection
Beh et syndrome
Lymphoma
Ischemia
Multiple Bull's-eye Lesions of Colonic Wall
| mnemonic: | MaCK CLaN |
Melanoma and
Carcinoma
Kaposi sarcoma
Carcinoid
Lymphoma and
Neurofibromatosis
Double-Tracking of Colon
= longitudinal extraluminal tracks paralleling the colon
1. Diverticulitis: generally 3 6 cm in length
2. Crohn disease: generally >10 cm
3. Ulcerative colitis
4. Primary carcinoma: wider + more irregular
Colonic Narrowing
CHRONIC STAGE OF ANY ULCERATING COLITIS
inflammatory:
Ulcerative colitis
Crohn colitis
Solitary rectal ulcer syndrome
Nonspecific benign ulcer
P.783
infectious:
Amebiasis
Schistosomiasis
Bacillary dysentery
Tuberculosis
Fungal disease
Lymphogranuloma venereum
Herpes zoster
Cytomegalovirus
Strongyloides
ischemic
Ischemic colitis
traumatic
Radiation injury
Cathartic colon
Caustic colitis
MALIGNANT LESION
primary
Colonic carcinoma (annular/scirrhous)
Complication of ulcerative colitis + Crohn colitis
metastatic:
from prostate, cervix, uterus, kidney, stomach, pancreas, primary intraperitoneal sarcoma
hematogenous (eg, breast)
lymphangitic spread
peritoneal seeding
EXTRINSIC PROCESS
inflammation
Retractile mesenteritis
Diverticulitis
Pancreatitis
deposits
Amyloidosis
Endometriosis
Pelvic lipomatosis
POSTSURGICAL
Adhesive bands
Surgical anastomosis
NORMAL
Cannon point
Localized Colonic Narrowing
| mnemonic: | SCARED CELL-MATE |
Schistosomiasis
Carcinoid
Actinomycosis
Radiation
Endometriosis
Diverticulitis
Colitis
Extrinsic lesion
Lymphoma
Lymphogranuloma venereum
Metastasis
Adenocarcinoma
Tuberculosis
Entamoeba histolytica
Microcolon
| mnemonic: | MI MCA |
Meconium ileus, Meconium peritonitis (cystic fibrosis)
Ileal/jejunal atresia
Megacystis-microcolon-hypoperistalsis syndrome
Colonic atresia (distal to atretic segment)
Aganglionosis (Hirschsprung disease)
Colonic Filling defects
Submucosal Tumor of Colon
Lipoma
Carcinoid
Leiomyoma
Lymphangioma, hemangioma
Single Colonic Filling Defect
BENIGN TUMOR
Polyp
(hyperplastic, adenomatous, villous adenoma, villoglandular); most common benign tumor
Lipoma
Most common intramural tumor; 2nd most common benign tumor; M < F
Location: ascending colon + cecum > left side of colon Carcinoid: 10% metastasize
Spindle cell tumor
(leiomyoma, fibroma, neurofibroma); 4th most common benign tumor; rectum > cecum
Lymphangioma, hemangioma
MALIGNANT TUMOR
primary tumor:
carcinoma, sarcoma
secondary tumor:
metastases (breast, stomach, lung, pancreas, kidney, female genital tract), lymphoma, invasion by adjacent tumors
INFECTION
Ameboma
Polypoid granuloma: schistosomiasis, TB
INFLAMMATION
Inflammatory pseudopolyp: ulcerative colitis, Crohn disease
Periappendiceal abscess
Diverticulitis
Foreign-body perforation
NONSESSILE INTRALUMINAL BODY
Fecal impaction
Foreign body
Gallstone
Bolus of Ascaris worms
MISCELLANEOUS
Endometriosis
3rd most common benign tumor
Location: sigmoid colon, rectosigmoid junction (at level of cul-de-sac)
may cause bleeding (after invasion of mucosa)Localized amyloid deposition
Suture granuloma
Intussusception
Pseudotumor (adhesions, fibrous bands)
Colitis cystica profunda
P.784
Multiple Colonic Filling Defects
NEOPLASMS
polyposis syndrome:
familial polyposis, Gardner syndrome, Peutz-Jeghers syndrome, Turcot syndrome, juvenile polyposis syndrome, disseminated gastrointestinal polyps, multiple adenomatous polyps
hematogenous metastases:
from breast, lung, stomach, ovary, pancreas, uterus
multiple tumors
benign:
neurofibromatosis, colonic lipomatosis, multiple hamartoma syndrome (Cowden disease)
malignant:
lymphoma, leukemia, adenocarcinoma
INFLAMMATORY PSEUDOPOLYPS
ulcerative colitis, Crohn colitis, ischemic colitis, amebiasis, schistosomiasis, strongyloidiasis, trichuriasis
ARTIFACTS
feces, air bubbles, oil bubbles, mucous strands, ingested foreign body (eg, corn kernels)
MISCELLANEOUS
nodular lymphoid hyperplasia, lymphoid follicular pattern, hemorrhoids, diverticula, pneumatosis intestinalis, colitis cystica profunda, colonic urticaria, submucosal colonic edema secondary to obstruction, cystic fibrosis, amyloidosis, ulcerative pseudopolyps, proximal to obstruction
| mnemonic: | MILL P3 |
Metastases (to colon)
Ischemia (thumbprinting)
Lymphoma
Lymphoid hyperplasia
Polyposis
Pseudopolyposis (with inflammatory bowel disease)
Pneumatosis cystoides
Carpet Lesions of Colon
= flat lobulated lesions with alteration of surface texture + little/no protrusion into lumen
| Location: | rectum > cecum > ascending colon |
Cause:
NEOPLASM
Tubular/tubulovillous/villous adenoma
Familial polyposis
Adenocarcinoma
Submucosal tumor spread (from adjacent carcinoma)
MISCELLANEOUS
Nonspecific follicular proctitis
Biopsy site
Endometriosis
Rectal varices
Colonic urticaria
Colonic Polyp
Terminology:
Polyp
= mass projecting into the lumen of a hollow viscus above the level of the mucosa; usually arises from mucosa, may derive from submucosa/muscularis propria
(a) neoplastic: adenoma/carcinoma
(b) nonneoplastic: hamartoma/inflammatory polyp
Pseudopolyp
= scattered island of inflamed edematous mucosa on a background of denuded mucosa
(a) pseudopolyposis of ulcerative colitis
(b) cobblestoning of Crohn disease
Postinflammatory (filiform) polyp
= fingerlike projection of submucosa covered by mucosa on all sides following healing + regeneration of inflammatory (most common in ulcerative colitis)/ischemic/infectious bowel disease
Histologic classification:
ADENOMATOUS POLYPS
= Familial adenomatous polyposis syndrome
Cause: abnormality on chromosome 5 Cx: adenomatous polyps are premalignant eventually leading to colorectal carcinoma 1. Familial (multiple) polyposis
2. Gardner syndrome
3. Turcot syndrome
HAMARTOMATOUS POLYPS
= Hamartomatous polyposis syndromes
1. Peutz-Jeghers syndrome (most in small bowel)*
2. Cowden disease*
3. Juvenile polyposis*
4. Cronkhite-Canada syndrome
5. Bannayan-Riley-Ruvalcaba syndrome
POLYPOSIS LOOK-ALIKES
Inflammatory polyposis
Lymphoid hyperplasia
Lymphoma
Metastases
Pneumatosis coli
Polyposis Syndromes
= more than 100 polyps in number
Mode of transmission:
HEREDITARY
autosomal dominant
Familial (multiple) polyposis
Gardner syndrome
Peutz-Jeghers syndrome
Juvenile polyposis coli
autosomal recessive
Turcot syndrome
NONHEREDITARY
Cronkhite-Canada syndrome
Juvenile polyposis
P.785
| Differential Diagnosis of Colonic polyps | ||
|---|---|---|
| Single Polyp | Multiple Polyps | |
| Neoplastic (10%) | ||
| epithelial (adenomatous) |
|
|
| nonepithelial |
| |
| Nonneoplastic (90%) | ||
| unclassified |
|
|
| hamartomatous |
|
|
| inflammatory |
|
|
Mural Stratification of Intestinal Tract
= bowel wall thickening with abnormal separation of bowel layers on cross-sectional imaging
CECT:
 double halo/target sign during arterial phase:
double halo/target sign during arterial phase: contrast enhancement of inner layer:
contrast enhancement of inner layer:(1) mucosa + (2) muscularis propria
 interposed edema (water)/hemorrhage (blood)/inflammatory cell infiltrate (pus, cells)/fatty proliferation:
interposed edema (water)/hemorrhage (blood)/inflammatory cell infiltrate (pus, cells)/fatty proliferation:(3) submucosa
 contrast enhancement of outer layer:
contrast enhancement of outer layer:(4) muscularis propria + (5) serosa
Cause:
 Tumor has not been reported to cause stratification!
Tumor has not been reported to cause stratification!
EDEMA
 low-density/water-density separation
low-density/water-density separation1. Ulcerative colitis (50%): rectum
2. Proximal to obstructing tumor/intussusception
INFLAMMATORY CELL INFILTRATE
Crohn disease (in up to 50%)
Mycobacterium tuberculosis
Eosinophilic enteritis
Cytomegalovirus
Clostridium difficile
Entamoeba histolytica
Vibrio cholerae
Shigella
Escherichia coli
ISCHEMIA/INFARCTION
Arterial obstruction: thromboembolism, plaque thrombus
Peripheral vasculopathy
Venous obstruction: thrombosis, bowel torsion, closed-loop obstruction
Hypoperfusion: proximal arterial stenosis potentiated by myocardial infarction, bradycardia, dehydration
N.B.: closed-loop obstruction with signs of bowel infarction is a surgical condition!  signs of bowel infarction:
signs of bowel infarction: free peritoneal fluid
free peritoneal fluid asymmetric bowel wall enhancement
asymmetric bowel wall enhancement persistent enhancement of bowel wall/segmental arteries
persistent enhancement of bowel wall/segmental arteries arterial/venous filling defects
arterial/venous filling defects increased density of mesentery
increased density of mesentery bowel obstruction
bowel obstruction
INTESTINAL WALL HEMORRHAGE
Anticoagulation
Blood dyscrasia: thrombocytopenic purpura
Blunt trauma
 snow-cone appearance of duodenum
snow-cone appearance of duodenum
Pseudomembranous Colitis
Clostridium difficile
Ischemic colitis: acute/subacute
Staphylococcus
Shigella
Pseudomonas aeruginosa
| 6. Drugs: | chlorpropamide, mercuric compounds, gold, NSAIDs |
Accordion Sign
= gross irregular polypoid thickening of colonic wall with wide separation of inner + outer walls
Radiation-induced colitis
Ischemic colitis
Infectious colitis: Clostridium difficile, tuberculosis
Typhlitis, neutropenic colitis
Inflammation: Crohn disease, ulcerative colitis
 The only 2 conditions with wall thickening >10 mm
The only 2 conditions with wall thickening >10 mm
Lymphangiectasia
Intramural hemorrhage
P.786
Rectum & Anus
Rectal Narrowing
Pelvic lipomatosis + fibrolipomatosis
Lymphogranuloma venereum
Radiation injury of rectum
Chronic ulcerative colitis
Enlarged Presacral Space
Normal width <5 mm in 95%; abnormal width >10 mm
RECTAL INFLAMMATION/INFECTION
ulcerative colitis, Crohn colitis, idiopathic proctosigmoiditis, radiation therapy
RECTAL INFECTION
Proctitis (TB, amebiasis, lymphogranuloma venereum, radiation, ischemia)
Diverticulitis
BENIGN RECTAL TUMOR
Developmental cyst (dermoid, enteric cyst, tailgut cyst)
Lipoma, neurofibroma, hemangioendothelioma
Epidermal cyst
Rectal duplication
MALIGNANT RECTAL TUMOR
Adenocarcinoma, cloacogenic carcinoma
Lymphoma, sarcoma, lymph node metastases
Prostatic carcinoma, bladder tumors, cervical cancer, ovarian cancer
BODY FLUIDS/DEPOSITS
Hematoma: surgery, sacral fracture
Pus: perforated appendix, presacral abscess
Serum: edema, venous thrombosis
Deposit of fat: pelvic lipomatosis, Cushing disease
Deposit of amyloid: amyloidosis
SACRAL TUMOR
Sacrococcygeal teratoma, anterior sacral meningocele
Chordoma, metastasis to sacrum
MISCELLANEOUS
Inguinal hernia containing segment of colon
Colitis cystica profunda
Pelvic lipomatosis
Lesions of Ischiorectal Fossa
Congenital and developmental anomalies
Gartner duct cyst
Klippel-Trenaunay syndrome
Tailgut cyst
Inflammatory and hemorrhagic lesions
Fistula in ano
Ischiorectal/perirectal abscess
Extraperitoneal pelvic hematoma
Rectal perforation
Secondary neoplasm
per direct extension/hematogenous spread:
anorectal/prostatic/pelvic/sacral tumor; lung cancer; melanoma; lymphoma
Primary neoplasm
Aggressive angiomyxoma
Lipoma
Plexiform neurofibroma
Anal adenocarcinoma
Squamous cell carcinoma
Peritoneum
Peritoneal Mass
SOLID MASS
Peritoneal mesothelioma
Peritoneal carcinomatosis
INFILTRATIVE PATTERN
Peritoneal mesothelioma
CYSTIC MASS
Cystic mesothelioma
Pseudomyxoma peritonei
Bacterial/mycobacterial infection
Multiple Peritoneal Masses
Metastases: RCC
Endometriosis
Abdominal lymphoma
Mesentery & Omentum
Short Mesentery
= shortened line of fixation
1. Malrotation + midgut volvulus
2. Omphalocele
3. Gastroschisis
4. Congenital diaphragmatic hernia
5. Asplenia + polysplenia
Apple peel Small Bowel
= distal small intestines spirals around its vascular supply resembling an apple peel resulting in a very short intestine
1. Proximal jejunal atresia
2. Absence of distal superior mesenteric artery
3. Shortening of small bowel distal to atresia
4. Absence of dorsal mesentery
| Cx: | propensity toward necrotizing enterocolitis |
| Prognosis: | high mortality |
Omental Mass
 33% of primary omental tumors are malignant!
33% of primary omental tumors are malignant! Secondary neoplasms are more frequent than primary!
Secondary neoplasms are more frequent than primary!
SOLID MASS
benign
Leiomyoma
Lipoma
Neurofibroma
malignant
Leiomyosarcoma
Liposarcoma
Fibrosarcoma
Lymphoma
Peritoneal mesothelioma
Hemangiopericytoma
Metastases
Infection: tuberculosis
CYSTIC MASS
Hematoma
Cystic mesothelioma
P.787
Omental Cake
= replacement of normal fat of the greater omentum by a soft-tissue density
Peritoneal metastases
mnemonic: COPS Colon
Ovary
Pancreas
Stomach
Lymphoma
Mesothelioma
Tuberculosis
Mesenteric Mass
ROUND SOLID MASSES
 Benign primary tumors are more common than malignant primary tumors!
Benign primary tumors are more common than malignant primary tumors! Secondary neoplasms more frequent than primary
Secondary neoplasms more frequent than primary Cystic tumors more common than solid tumors!
Cystic tumors more common than solid tumors! Malignant solid tumors have a tendency to be located near root of mesentery, benign solid tumors in periphery near bowel!
Malignant solid tumors have a tendency to be located near root of mesentery, benign solid tumors in periphery near bowel!1. Metastases especially from colon, ovary (most frequent neoplasm of mesentery)
2. Lymphoma
3. Leiomyosarcoma (more frequent than leiomyoma)
4. Neural tumor (neurofibroma, ganglioneuroma)
5. Lipoma (uncommon), lipomatosis, liposarcoma
6. Fibrous histiocytoma
7. Hemangioma
8. Desmoid tumor (most common primary)
9. Desmoplastic small round cell tumor of peritoneum
ILL-DEFINED MASSES
Metastases (ovary)
Lymphoma
Fibromatosis, fibrosing mesenteritis (associated with Gardner syndrome)
Lipodystrophy
Mesenteric panniculitis
STELLATE MASSES
1. Peritoneal mesothelioma
2. Retractile mesenteritis
3. Fibrotic reaction of carcinoid
4. Radiation therapy
5. Desmoid tumor
6. Hodgkin disease
7. Tuberculous peritonitis
8. Ovarian metastases
9. Diverticulitis
10. Pancreatitis
 A calcified mesenteric mass suggests carcinoid tumor!
A calcified mesenteric mass suggests carcinoid tumor!
LOCULATED CYSTIC MASSES (2/3)
Cystic lymphangioma (most common)
Pseudomyxoma peritonei
Cystic mesothelioma
Mesenteric cyst
Mesenteric hematoma
Benign cystic teratoma
Cystic spindle cell tumor (= centrally necrotic leiomyoma/leiomyosarcoma)
Mesenteric/Omental Cysts
= BUBBLES OF THE BELLY
 The first step is to determine the organ of origin!
The first step is to determine the organ of origin!1. Lymphangioma
2. Nonpancreatic pseudocyst
= sequelae of mesenteric/omental hematoma/abscess
Path: thick-walled, usually septated cystic mass with hemorrhagic/purulent contents 3. Duplication cyst
4. Mesothelial cyst
5. Enteric cyst
6. Cystic metastasis
7. Cystic mesothelioma
Mesenteric Edema/Congestion
 increase of mesenteric fat attenuation to 40 to 60 HU
increase of mesenteric fat attenuation to 40 to 60 HU loss of sharp interfaces between mesenteric vessels + fat
loss of sharp interfaces between mesenteric vessels + fat
SYSTEMIC FLUID OVERLOAD
Hypoalbuminemia
Liver cirrhosis
Nephrosis
Heart failure
LOCAL VESSEL DISEASE
Portal vein thrombosis
Mesenteric vein/artery thrombosis
Vasculitis
SMA dissection
CELL INFILTRATE
Malignant neoplasm
Inflammation
Trauma (small hemorrhage)
Comb Sign
= vascular dilatation of vasa recta + interconnected arterial arcades aligned as the teeth of a comb
 multiple tubular tortuous opacities on mesenteric side of ileum
multiple tubular tortuous opacities on mesenteric side of ileum1. Crohn disease
2. Ulcerative colitis
3. Vasculitis: Lupus, polyarteritis nodosa, Henoch-Sch nlein syndrome, microscopic polyangiitis, Beh et syndrome
4. Mesenteric thromboembolism
5. Strangulated bowel obstruction
Fat Ring Sign
= fat-stranding of the fat plane surrounding the root of mesenteric vessels
benign
Mesenteric panniculitis
Mesenteric lipodystrophy
Retractile mesenteritis
malignant
Carcinoid
Desmoid tumor
Lymphoma
P.788
Umbilical Tumor
PRIMARY (38%)
benign/malignant neoplasm, skin tumor
METASTASES (30%)
= Sister Joseph nodule
firm painful nodule
ulceration with serosanguinous/purulent discharge
Cause: gastrointestinal cancer (50%), undetermined (25%), ovarian cancer, pancreatic cancer, small cell carcinoma of lung (very rare) Spread:
direct extension from anterior peritoneal surface
extension along embryonic remnants: falciform, median umbilical, omphalomesenteric ligaments
hematogenous
retrograde lymphatic flow from inguinal, axillary, paraaortic nodes
iatrogenic: laparoscopic tract, tract of percutaneous needle biopsy
NONNEOPLASTIC
Endometriosis (32%)
Granuloma
Incarcerated hernia
Abdominal Lymphadenopathy
Regional Patterns of Lymphadenopathy
@ Retrocrural nodes
Abnormal size: >6 mm Common cause: lung carcinoma, mesothelioma, lymphoma @ Gastrohepatic ligament nodes
= superior portion of lesser omentum suspending stomach from liver
Abnormal size: >8 mm Common cause: carcinoma of lesser curvature of stomach, distal esophagus, lymphoma, pancreatic cancer, melanoma, colon + breast cancer DDx: coronary varices @ Porta hepatis nodes
= in porta hepatis extending down hepatoduodenal ligament, anterior + posterior to portal vein
Abnormal size: >6 mm Common cause: carcinoma of gallbladder + biliary tree, liver, stomach, pancreas, colon, lung, breast Cx: high extrahepatic biliary obstruction @ Pancreaticoduodenal nodes
= between duodenal sweep + pancreatic head anterior to IVC
Abnormal size: >10 mm Common cause: lymphoma, pancreatic head, colon, stomach, lung, breast cancer @ Perisplenic nodes
= in splenic hilum
Abnormal size: >10 mm Common cause: NHL, leukemia, small bowel neoplasm, ovarian cancer, carcinoma of right/transverse colon @ Retroperitoneal nodes
= periaortic, pericaval, interaortocaval
Abnormal size: >10 mm Common cause: lymphoma, renal cell, testicular, cervical, prostatic carcinomas @ Celiac and superior mesenteric artery nodes
= preaortic nodes
Abnormal size: >10 mm Common cause: any intraabdominal neoplasm @ Pelvic nodes
= along common, external + internal iliac vessels
Abnormal size: >15 mm Common cause: carcinoma of bladder, prostate, cervix, uterus, rectum
Low-Attenuation Abdominal Adenopathy
= ENLARGED LYMPH NODE WITH LOW-DENSITY CENTER
1. Mycobacterial infection (TB, M. avium-intracellulare)
2. Pyogenic infection
3. Whipple disease
4. Lymphoma
5. Metastatic disease after radiation + chemotherapy
6. Lymphangioleiomyomatosis
7. Neurofibromatosis type I
8. Cavitating mesenteric lymph node syndrome
P.789
Anatomy and Function of Gastrointestinal Tract
Gastrointestinal hormones
Cholecystokinin
= CCK = 33 amino acid residues (former name: Pancreozymin); the 5 C-terminal amino acids are identical to those of gastrin, causing similar effects as gastrin; 2.5-minute serum half-life
| Produced in: | duodenal + upper intestinal mucosa |
| Released by: | fatty acids, some amino acids (phenylalanine, methionine), hydrogen ions |
Effects:
@ Stomach
weakly stimulates HCl secretion
given alone: inhibits gastrin, which leads to decrease in HCl production
stimulates pepsin secretion
stimulates gastric motility
@ Pancreas
stimulates secretion of pancreatic enzymes (= Pancreozymin)
stimulates bicarbonate secretion (weakly by direct effect; strongly through potentiating effect on secretin)
stimulates insulin release
@ Liver
stimulates water + bicarbonate secretion
@ Intestine
stimulates secretion of Brunner glands
increases motility
@ Biliary tract
strong stimulator of gallbladder contraction with maximum effect within 5 15 minutes + return to basal size in 1 hour
relaxation of sphincter of Oddi
Medication:
sincalide (Kinevac ) = synthetic C-terminal octapeptide of the hormone cholecystokinin
Use: may be used to empty gallbladder about 30 minutes (to 4 hours) before tracer injection in patients on prolonged fasting (gallbladder atony + retained bile and sludge secondary to absence of endogenously produced CCK) Dose for hepatobiliary scintigraphy:
preferred: IV infusion of 0.01 g/kg Kinevac over 30 60 minutes;
package insert: with slow IV injection of 0.01 g/kg Kinevac over 3 minutes (concentration of 1 g/mL) the response is too variable
Useful in: - (a) patient fasting >24 hours/on total parenteral nutrition
- (b) acalculous cholecystitis
- (c) chronic GB dysfunction
- (d) GB ejection fraction
Side effect: increase in biliary-to-bowel transit time, dizziness, flushing, nausea, abdominal cramps, urge to defecate Contraindications:
acute pancreatitis, acute cholecystitis, obstruction of cystic duct/CBD, appendicitis, peritonitis, pyloric stenosis, peptic ulcer
Gastrin
= 17 amino acid peptide amide;
PENTAGASTRIN
= acyl derivative of the biologic active C-terminal tetrapeptide amide
| Produced in: | antral cells + G cells of pancreas |
| Released by: |
mediated by neuroendocrine cholinergic reflexes |
| Inhibited by: | drop in pH of antral mucosa to <3.5 |
Effects:
@ Stomach:
stimulation of gastric HCl secretion from parietal cells, which in turn:
increases pepsinogen production by chief cells through local reflex
increase in antral motility
trophic effect on gastric mucosa (parietal cell hyperplasia)
@ Pancreas
strong increase in enzyme output
weakly stimulates fluid + bicarbonate output
stimulates insulin release
@ Liver
water + bicarbonate secretion
@ Intestine
stimulates secretion of Brunner glands
increases motility
@ Gallbladder
stimulates contraction
@ Esophagus
increases resting pressure of LES
Glucagon
| Produced in: | cells (and cells) of pancreas |
| Released by: | low blood glucose levels |
Effects:
@ Intestines
lowers pressure of GE sphincter
hypotonic effect on duodenum > jejunum > stomach > colon
@ Hormones
releases catecholamines from the adrenal gland that paralyze intestinal smooth muscle
increases serum insulin + glucose levels (mobilization of hepatic glycogen)
@ Biliary tract
increases bile flow
relaxes gallbladder + sphincter of Oddi
P.790
| Dose for radiologic imaging: | 1 mg maximum |
 IV administration causes a quick response + rapid dissipation of action!
IV administration causes a quick response + rapid dissipation of action! IM administration prolongs onset + increases length of action!
IM administration prolongs onset + increases length of action!
| Half-life: | 3 6 minutes |
| Side effects: | nausea + vomiting, weakness, dizziness (delayed onset of 1.5 4 hours after IM administration) |
Contraindication:
hypersensitivity/allergy to glucagon: urticaria, periorbital edema, respiratory distress, hypotension, coronary artery spasm (?), circulatory arrest
known hypertensive response to glucagon
pheochromocytoma: glucagon stimulates release of catecholamines
insulinoma: insulin-releasing effect may result in hypoglycemia
glucagonoma
poorly controlled diabetes mellitus
Secretin
| Produced in: | duodenal mucosa |
| Released by: | hydrogen ions providing a pH <4.5 |
Effects:
@ Stomach
inhibits gastrin activity, which leads to decrease in HCl secretion
stimulates pepsinogen secretion by chief cells (potent pepsigogue)
decreases gastric and duodenal motility + contraction of pyloric sphincter
@ Pancreas
increases alkaline pancreatic secretions (NaHCO3)
weakly stimulates enzyme secretion
stimulates insulin release
@ Liver
stimulates water + bicarbonate secretion (most potent choleretic)
@ Intestine
stimulates secretion of Brunner glands
inhibits motility
@ Esophagus
opens LES
Embryology of alimentary tract
| Origin: | as a pouchlike extension of the yolk sac |
Development of GI tube:
continuous tubular structure by 6 weeks GA; divided into:
foregut (supplied by celiac artery)
midgut (supplied by superior mesenteric artery)
hindgut (supplied by inferior mesenteric artery)
Rotation about omphalomesenteric vessels by 270 :
<6 weeks GA
90 counterclockwise rotation of duodenojejunal segment toward the right of SMA
90 counterclockwise rotation of ileocolic segment toward the left of SMA
during 6th week GA
additional 90 counterclockwise rotation of duodenum posterior to SMA
remainder of midgut within umbilical cord
10 12 weeks GA
intestines slides back into peritoneal cavity
final 90 counterclockwise rotation of duodenum
final 180 counterclockwise rotation of cecum
Peritoneal fixation of small bowel:
broad-based mesentery extending from ligament of Treitz to ileocecal valve
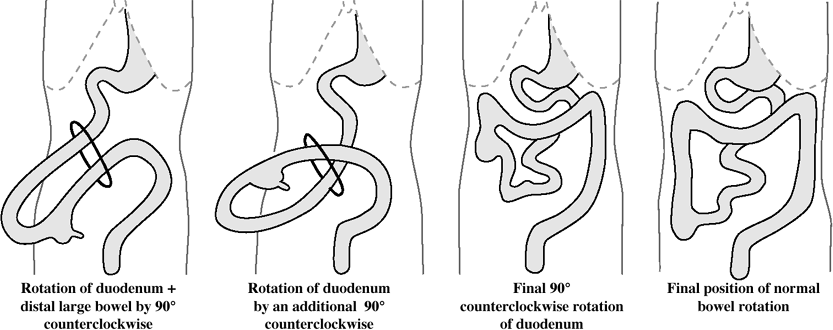 |
| Stages of Intestinal Rotation |
P.791
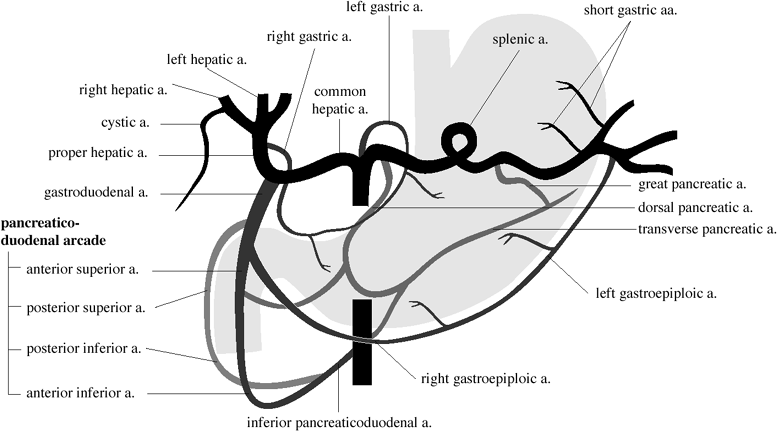 |
| Blood Supply of Stomach, Duodenum, and Pancreas |
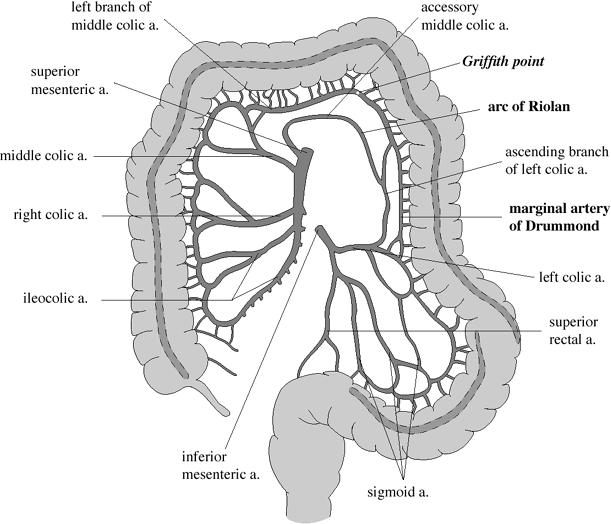 |
| Blood Supply of Large Intestine |
P.792
Vascular Supply of Bowel
 bowel receives 20% of resting cardiac output (2/3 for intestinal mucosa) which increases up to 35% in postprandial phase
bowel receives 20% of resting cardiac output (2/3 for intestinal mucosa) which increases up to 35% in postprandial phaseearliest + fast rise after intake of carbohydrates
slower + large rise after intake of fat + proteins
Celiac Trunk
| Supply for: | from distal esophagus to descending duodenum |
| Anastomosis: | to SMA via gastroduodenal artery as the 1st branch off the celiac trunk |
Superior Mesenteric Artery (SMA)
| Supply for: | transverse + descending duodenum, jejunum, ileum, large bowel to splenic flexure |
| Anastomosis: | to IMA via marginal artery of Drummond, arcade of Riolan |
Inferior Mesenteric Artery (IMA)
| Supply for: | colon from splenic flexure to rectum |
| Anastomoses: | to lumbar branches of abdominal aorta, sacral artery, internal iliac aa. |
Arcades
up to four arcades are formed by these arteries which continue toward the periphery as
Primary parallel circuits for
muscularis propria
submucosa
mucosa
Serial circuits of
resistance arterioles
precapillary sphincters
capillaries
postcapillary sphincters
venous capacitance vessels
Esophagus
Lower Esophageal Anatomy
Esophageal Vestibule
= saccular termination of lower esophagus with upper boundary at tubulovestibular junction + lower boundary at esophagogastric junction
 collapsed during resting state
collapsed during resting state assumes bulbous configuration with swallowing
assumes bulbous configuration with swallowing(a) tubulovestibular junction = A level = junction between tubular and saccular esophagus
(b) phrenic ampulla = bell-shaped part above diaphragm (term should be discarded because of dynamic changes of configuration)
(c) submerged segment = infrahiatal part of esophagus
 widening/disappearance is indicative of gastroesophageal reflux disease (GERD)
widening/disappearance is indicative of gastroesophageal reflux disease (GERD)
Gastroesophageal Junction
Site: at upper level of gastric sling fibers, straddles cardiac incisura demarcating the left lateral margin of GE junction Z-line = B level = zigzag-shaped squamocolumnar junction line
 Not acceptable criterion for locating GE junction
Not acceptable criterion for locating GE junction
Site: 1 2 cm above gastric sling fibers Lower Esophageal Sphincter
= physiologic 2 4-cm high pressure zone corresponding to esophageal vestibule
 tightly closed during resting state
tightly closed during resting state assumes bulbous configuration with swallowing
assumes bulbous configuration with swallowing
Muscular Rings of Esophagus
A Ring
= contracted/hypertrophied muscles in response to incompetent GE sphincter
rarely symptomatic/dysphagia
| Location: | at tubulovestibular junction = superior aspect of vestibule |
 usually 2 cm proximal to GE junction at upper end of vestibule
usually 2 cm proximal to GE junction at upper end of vestibule varies in caliber during the same examination, may disappear on maximum distension
varies in caliber during the same examination, may disappear on maximum distension broad smooth narrowing with thick rounded margins
broad smooth narrowing with thick rounded margins visible only if tubular esophagus above + vestibule below are distended
visible only if tubular esophagus above + vestibule below are distended
B Ring
= sling fibers representing a U-shaped thickening of inner muscle layers with open arm of U toward lesser curvature = inferior aspect of vestibule
| Location: | < 2 cm from hiatal margins |
 only visible when esophagogastric junction is above hiatus
only visible when esophagogastric junction is above hiatus thin ledge-like ring just below the mucosal junction (Z-line)
thin ledge-like ring just below the mucosal junction (Z-line)
Swallowing function
| Technique: | videofluoroscopy of a modified barium swallow study to assess handling of bolus (with consistency of nectar liquid, honey liquid, pureed food, soft solid food, hard solid food); preferably together with speech pathologist |
| Document patient behavior + reaction: | episode of refusal, cough, silent aspiration, apnea, bradycardia |
| CNS involved: | cranial nerves V, VII, IX, X, XII; 5 cervical nerves; cortical + subcortical pathways; midbrain; brainstem |
| Muscles involved: | 32 groups of muscles |
| Developmental: | swallowing as early as 11 weeks GA; suckling at 18 24 weeks GA; nonnutritive sucking at 27 28 weeks GA; single breath sucking at 35 36 weeks GA |
Phases:
Oral preparatory phase
 food chewed + mixed with saliva
food chewed + mixed with saliva
Oral phase
 bolus propelled posteriorly to tongue
bolus propelled posteriorly to tonguePath:
spillage from mouth
small bolus formation
tongue tremor
incomplete tongue elevation
early spillage into valleculae prior to initiation of swallow
Pharyngeal phase
 elevation of soft palate + valleculae (to seal nasopharynx)
elevation of soft palate + valleculae (to seal nasopharynx) elevation of larynx (to close vestibule)
elevation of larynx (to close vestibule) relaxation of cricopharyngeal muscle
relaxation of cricopharyngeal muscle contraction of lateral pharyngeal wall
contraction of lateral pharyngeal wallPath:
nasopharyngeal reflux
laryngeal penetration (= contrast material enters laryngeal vestibule
Cause: delayed elevation of larynx tracheal aspiration (= contrast material enters airway below vocal cord level)
Cause: delayed elevation of larynx, delayed pharyngeal transit time, decreased clearance of bolus with residual in vallecula + pyriform sinus spilling into larynx + trachea
Esophageal phase
 contraction of cricopharyngeal muscle
contraction of cricopharyngeal muscle bolus transfer into esophagus
bolus transfer into esophagus
Path: cricopharyngeal achalasia (with reflux of bolus into oropharynx/pooling in pyriform sinus)
P.793
Stomach
Gastric cells
Chief cells
= peptic/zymogenic cells
Location: body + fundus produce: pepsinogen Parietal cells
= oxyntic cells
Location: body + fundus produce: H+, Cl-, intrinsic factor, prostaglandins Mucous neck cells
produce: mucoprotein, mucopolysaccharide, aminopolysaccharide sulfate Argentaffine cells
= enteroendocrine cells
Location: body + fundus produce: glucagon-like substance (A-cells), somatostatin (D-cells), vasoactive intestinal polypeptide (D1-cells), 5-hydroxytryptamine (EC-cells) G-cells
Location: pylorus produce: gastrin
Effect of Bilateral Vagotomy
= cholinergic denervation
(1) decreased MOTILITY of stomach + intestines
(2) decreased GASTRIC SECRETION
(3) decreased TONE OF GALLBLADDER + bile ducts
(4) increased TONE OF SPHINCTERS (Oddi + lower esophageal sphincter)
Pylorus
= fan-shaped specialized circular muscle fibers with:
distal sphincteric loop = right canalis loop
 corresponds to radiologic pyloric sphincter
corresponds to radiologic pyloric sphincter
proximal sphincteric loop = left canalis loop
 2 cm proximal to distal sphincteric loop on greater curvature (seen during complete relaxation)
2 cm proximal to distal sphincteric loop on greater curvature (seen during complete relaxation)
torus
= fibers of both sphincters converge on the lesser curvature side to form a muscular prominence; prolapse of mucosa between sphincteric loops produces a niche simulating ulcer
 pyloric channel 5 10 mm long, wall thickness of 4 8 mm
pyloric channel 5 10 mm long, wall thickness of 4 8 mm concentric indentation of the base of the duodenal bulb
concentric indentation of the base of the duodenal bulb
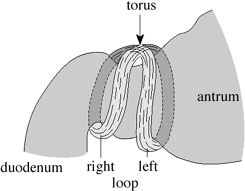 |
| Pyloric Muscular Anatomy |
Small Bowel
 Longest tubular organ in body measuring 550 600 cm (18 22 feet) in length
Longest tubular organ in body measuring 550 600 cm (18 22 feet) in length
| Segments: | duodenum of 25 30 cm in length jejunum of 10 12 feet in length (= proximal 60%) ileum of 6 8 feet in length (= distal 40%) |
| Mesentery: | 15 cm long between ligament of Treitz + ileocecal junction |
Duodenal Segments
duodenal bulb + short postbulbar segment:
intraperitoneal + freely movable
descending duodenum:
retroperitoneal attached to head of pancreas
horizontal = transverse segment:
retroperitoneal crossing the spine
ascending portion
retroperitoneal ascending to level of duodenojejunal junction
VARIATIONS:
mobile duodenum / water-trap duodenum
= long postbulbar segment with undulation/redundancy
duodenum inversum/duodenum reflexum
= distal duodenum ascends to the right of spine to the level of duodenal bulb + then crosses spine horizontally + fixated in normal location
Small Bowel Folds
 Circular small bowel folds = folds of Kerckring
Circular small bowel folds = folds of Kerckring= valvulae conniventes = two mucosal layers around a core of submucosa
NORMAL FOLD THICKNESS
@ jejunum 1.7 2.0 mm >2.5 mm pathologic @ ileum 1.4 1.7 mm >2.0 mm pathologic NORMAL NUMBER OF FOLDS
@ jejunum 4 7/inch @ ileum 2 4/inch NORMAL FOLD HEIGHT
@ jejunum 3.5 7.0 mm @ ileum 2.0 3.5 mm NORMAL LUMEN DIAMETER
@ upper jejunum 3.0 4.0 cm >4.5 cm pathologic @ lower jejunum 2.5 3.5 cm >4.0 cm pathologic @ ileum 2.0 2.8 cm >3.0 cm pathologic
P.794
RULE OF 3's:
 Wall thickness <3 mm
Wall thickness <3 mm Valvulae conniventes <3 mm
Valvulae conniventes <3 mm Diameter <3 cm
Diameter <3 cm Air-fluid levels <3
Air-fluid levels <3
Normal Bowel Caliber
| mnemonic: | 3-6-9-12 |
| 3 cm | maximal size of small bowel <25 mm on CT |
| 6 cm | maximal size of transverse colon |
| 9 cm | maximal size of cecum |
| 12 cm | maximal caliber of cecum before it may burst |
Small Bowel Peristalsis
INCREASED
Vagal stimulation
Acetylcholine
Anticholinesterase (eg, neostigmine)
Cholecystokinin
DECREASED
Atropine (eg, Pro-Banthine )
Bilateral vagotomy
Intestinal function
Intestinal Gas
INFLUX
- Aerophagia
- Liberation from intestinal tract
- neutralization of bicarbonate insecretions (CO2)
- bacterial fermentation (CO2, H2, CH4, H2S)
- Diffusion from blood (N2, O2, CO2)
2 L
8 L
15 LEFFLUX
- Diffusion from intestines into bloodand expulsion from lung
- Expulsion from anus
50 L
2 L
Intestinal Fluid
INFLUX
- Oral ingestion
- Intestinal secretions
saliva
bile
gastric secretions
pancreatic secretions
intestinal secretions
2.5 L
8.2 L
1.5 L
0.5 L
2.5 L
0.7 L
3.0 LEFFLUX
- Peranal
- Intestinal resorption (primarily in ileum+ ascending colon)
10.6 L
0.1 L
Intestinal Transit Time
(measured by pH telemetry); affected by type of diet
| Small bowel transit time: | 3 11 hours |
| Colonic transit time: | 20 71 hours |
Defecography/Evacuation Proctography
| evacuation time | = 15 (range 5 40) seconds | |
| anorectal angle | = angle formed between central axis of anal canal + line parallel to posterior wall of rectum 90 at rest and during voluntary contraction (squeeze maneuver) more obtuse during defecation straining (void) | |
| anorectal junction | = point of taper of distal rectal ampulla as it merges with the anal canal; position of anorectal junction referenced to plane of ischial tuberosities = 0 3.5 cm; elevation during squeeze of 0 4.5 cm; elevation during void of 3.0 0 cm | |
| rectovaginal space | = space between vagina and rectum | |
| perineum | = area between external genital organs and anal verge | |
| rectocele | = measurement of anteroposterior depth of convex wall protrusion extending beyond expected margin of normal rectal wall | |
| small | <2 cm; | |
| moderate | = 2 4 cm; | |
| large | >4 cm | |
| peritoneocele | = extension of rectouterine excavation to below upper third of vagina; containing liquid/bowel/omentum | |
| enterocele | = bowel present in peritoneocele | |
| rectal prolapse | = descent of entire thickness of rectal wall through anal verge | |
| rectal intussusception = | descent of the entire thickness of the rectal wall possibly extending into anal canal; starting 6 11 cm above anus; accompanied by formation of a circular indentation forming a ring pocket infolding of <3 mm in width/> 3 mm in width/intraluminal narrowing/descent into anal canal/external prolapse | |
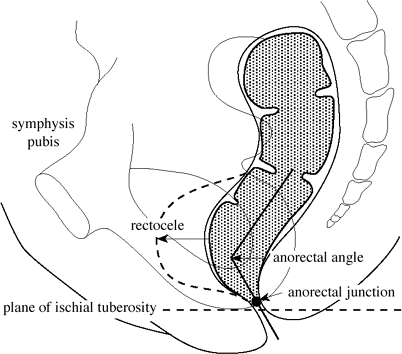 |
| Defecographic Measurements |
P.795
Peritoneum
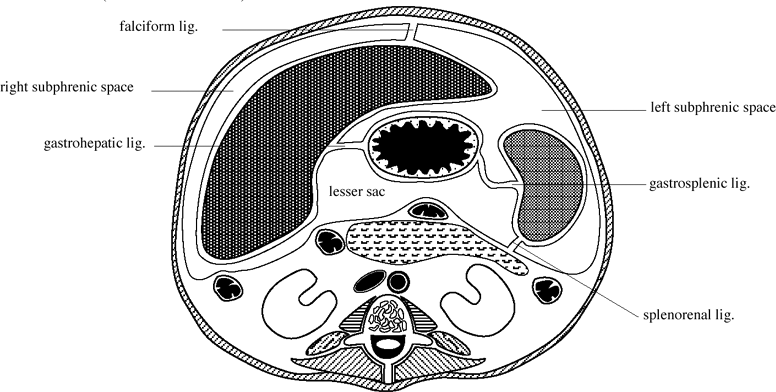 |
| Ligaments and Peritoneal Spaces in Upper Abdomen |
Peritoneal Spaces
Definitions:
Ligament = formed by two folds of peritoneum supporting a structure within the peritoneal cavity Omentum = specialized structure connecting stomach to an additional structure Mesentery = two peritoneal folds connecting a portion of bowel to the retroperitoneum Embryology:
above transverse mesocolon:
RIGHT PERITONEAL SPACE
forms perihepatic space + lesser sac:
Right subphrenic space:
located between right hepatic lobe + diaphragm
limited posteriorly by right superior reflection of coronary lig. + right triangular ligament
Right subhepatic space:
divided into
anterior right subhepatic space: located just posterior to porta hepatis, communicating with lesser sac via epiploic foramen (= foramen of Winslow)
posterior right subhepatic space
= Morison pouch = hepatorenal fossa
 Most dependent portion of the abdomen in supine patient!
Most dependent portion of the abdomen in supine patient!
Bare area of liver
situated between reflections of right + left coronary ligaments
continuous with right anterior pararenal space
Lesser sac:
superior recess:
 surrounds medial aspect of caudate lobe
surrounds medial aspect of caudate lobe separated from splenic recess by gastropancreatic fold
separated from splenic recess by gastropancreatic fold
splenic recess:
 extends across midline to splenic hilum
extends across midline to splenic hilum
inferior recess:
 separates stomach from pancreas + transverse mesocolon
separates stomach from pancreas + transverse mesocolon anteriorly covered by lesser omentum
anteriorly covered by lesser omentum
Lesser omentum = combination of gastrohepatic ligament + hepatoduodenal ligament
Right triangular ligament:
forms from coalescence of superior and inferior reflections of right coronary ligament
divides posterior aspect of right perihepatic space into right subphrenic space + posterior right subhepatic space
LEFT PERITONEAL SPACE
forms left subphrenic space
Left subphrenic space:
artificially divided into
immediate subphrenic space:
between diaphragm + gastric fundus
perisplenic space:
bounded inferiorly by phrenicocolic lig.
subhepatic space = gastrohepatic recess:
located between lateral segment of left hepatic lobe + stomach
P.796
separated from right subphrenic space by falciform ligament
Left triangular ligament:
forms from coalescence of superior and inferior reflections of left coronary ligament
located along superior aspect of left hepatic lobe
DORSAL MESENTERY gives rise to:
Gastrophrenic ligament
courses through immediate subphrenic space
suspends stomach from dome of diaphragm
Gastropancreatic ligament
formed by proximal left gastric artery
attaches posterior aspect of gastric fundus to retroperitoneum
partially separates superior recess of lesser sac from splenic recess
Phrenicocolic ligament
major suspensory ligament of spleen
attaches proximal descending colon to left hemidiaphragm
separates left subphrenic space from left paracolic gutter
Gastrosplenic ligament
remnant of dorsal mesentery
connects greater curvature of stomach with splenic hilum
contains short gastric vessels
Splenorenal ligament
connects posterior aspect of spleen to anterior pararenal space
contributes to left lateral + posterior border of lesser sac
encloses tail of pancreas + distal splenic artery + proximal splenic vein
Gastrocolic ligament
forms portion of anterior border of lesser sac
forms superior aspect of greater omentum
connects greater curvature of stomach with superior aspect of transverse colon
contains gastroepiploic vessels
VENTRAL MESENTERY gives rise to:
Falciform ligament
= sickle-shaped fold composed of two layers of peritoneum
attaches ventral surface of liver to anterior abdominal wall
its right layer continues into the superior layer of the coronary ligament, its left layer continues into the anterior layer of the left triangular ligament
contains ligamentum teres (= obliterated umbilical vein) in its free inferoposterior margin
continuous with fissure for ligamentum venosum
Gastrohepatic ligament:
arises in fissure of ligamentum venosum
connects medial aspect of liver to lesser curvature of stomach as part of lesser omentum
contains left gastric artery, coronary vein, lymph nodes
Hepatoduodenal ligament:
forms inferior edge of gastrohepatic ligament
forms anterior margin of epiploic foramen
extends from proximal duodenum to porta hepatis
contains common hepatic duct, common bile duct, hepatic artery, portal vein
below transverse mesocolon:
VENTRAL MESENTERY regresses
DORSAL MESENTERY forms:
Transverse mesocolon:
suspends transverse colon from retroperitoneum along anteroinferior edge of pancreas
forms posteroinferior border of lesser sac
contains middle colic vessels
Small bowel mesentery:
suspends small bowel from retroperitoneum
extends from ligament of Treitz to ileocecal valve
contains superior mesenteric vessels + lymph nodes
Sigmoid mesocolon:
attaches sigmoid colon to posterior pelvic wall
contains sigmoid + hemorrhoidal vessels
Greater omentum:
inferior continuation of gastrocolic ligament
formed by double reflection of dorsal mesogastrium thus composed of 4 layers of peritoneum
Superior + inferior ileocecal recesses:
located above + below terminal ileum
Retrocecal space:
present only if peritoneum reflects posterior to cecum
Right + left paracolic gutters:
located lateral to ascending + descending colon
Intersigmoid recess:
located along undersurface of sigmoid mesocolon
P.797
Gastrointestinal Disorders
Achalasia
= failure of organized peristalsis + relaxation at level of lower esophageal sphincter
| Etiology: | (a) idiopathic: abnormality of Auerbach plexus/medullary dorsal nucleus; neurotropic virus, gastrin hypersensitivity (b) Chagas disease |
 megaesophagus = dilatation of esophagus beginning in upper 1/3, ultimately entire length
megaesophagus = dilatation of esophagus beginning in upper 1/3, ultimately entire length absence of primary peristalsis below level of cricopharyngeus
absence of primary peristalsis below level of cricopharyngeus nonperistaltic contractions
nonperistaltic contractions bird-beak / rat tail deformity = V-shaped conical + symmetric tapering of stenotic segment with most marked narrowing at GE junction
bird-beak / rat tail deformity = V-shaped conical + symmetric tapering of stenotic segment with most marked narrowing at GE junction Hurst phenomenon = temporary transit through cardia when hydrostatic pressure of barium column is above tonic LES pressure
Hurst phenomenon = temporary transit through cardia when hydrostatic pressure of barium column is above tonic LES pressure sudden esophageal emptying after ingestion of carbonated beverage (eg, Coke)
sudden esophageal emptying after ingestion of carbonated beverage (eg, Coke) vigorous achalasia = numerous tertiary contractions in nondilated distal esophagus of early achalasia
vigorous achalasia = numerous tertiary contractions in nondilated distal esophagus of early achalasia prompt relaxation of LES upon amyl nitrate inhalation (smooth-muscle relaxant)
prompt relaxation of LES upon amyl nitrate inhalation (smooth-muscle relaxant)
CXR:
 right convex opacity behind right heart border; occasionally left convex opacity if thoracic aorta tortuous
right convex opacity behind right heart border; occasionally left convex opacity if thoracic aorta tortuous right convex opacity may be tethered by azygos arch allowing for greater dilatation above + below
right convex opacity may be tethered by azygos arch allowing for greater dilatation above + below air-fluid level (stasis in thoracic esophagus filled with retained secretions + alimentary residue)
air-fluid level (stasis in thoracic esophagus filled with retained secretions + alimentary residue) small/absent gastric air bubble
small/absent gastric air bubble anterior displacement + bowing of trachea (LAT view)
anterior displacement + bowing of trachea (LAT view) patchy bilateral alveolar opacities resembling acute/chronic aspiration pneumonia (M. fortuitum-chelonei infection)
patchy bilateral alveolar opacities resembling acute/chronic aspiration pneumonia (M. fortuitum-chelonei infection)
| Cx: | esophageal carcinoma in 2 7% (usually midesophagus) |
| Rx: | pneumatic dilatation/surgical myotomy |
| DDx: | (1) Neoplasm (separation of gastric fundus from diaphragm; normal peristalsis; asymmetric tapering) (2) Peptic stricture of esophagus |
Secondary Achalasia
= carcinoma of cardia/gastric fundus invading esophagus
Age: >50 years duration of symptoms for <6 months
 irregular/asymmetric narrowing
irregular/asymmetric narrowing abrupt transition
abrupt transition associated fundal lesion
associated fundal lesion
Adenoma of Small Bowel
| Location: | duodenum (21%), jejunum (36%), ileum (43%) esp. ileocecal valve |
Histo:
Hamartomatous polyp (77%), multiple in 47%, 1/3 of multiple lesions associated with Peutz-Jeghers syndrome
adenomatous polyp (13%), may have malignant potential
polypoid gastric heterotopic tumor (10%)
Adenomatous Colonic Polyp
= EPITHELIAL POLYP
Most common benign colonic tumor (68 79%)
| Predisposed: | previously detected polyp/cancer; family history of polyps/cancer; idiopathic inflammatory bowel disease; Peutz-Jeghers syndrome; Gardner syndrome; familial polyposis |
| Prevalence: | 3% in 3rd decade; 10% in 7th decade; 26% in 9th decade |
| Location: | rectum (21 34%); sigmoid (26 38%); descending colon (6 18%); transverse colon (12 13%); ascending colon (9 12%); multiple in 35 50% (usually <5 10 in number) |
Histo:
Tubular adenoma (75%)
= cylindrical glandular formation lined by stratified columnar epithelium + containing nests of epithelium within lamina propria
 usually <10 mm in diameter
usually <10 mm in diameter often pedunculated if >10 mm
often pedunculated if >10 mm
malignant potential: <10 mm in 1%; 10 20 mm in 10%; >20 mm in 35% Tubulovillous adenoma (15%)
= mixture between tubular + villous adenoma
malignant potential: <10 mm in 4%; 10 20 mm in 7%; >20 mm in 46% Villous adenoma (10%)
= thin frondlike surface projections ( villous fronds )
potassium depletion
 often >20 mm in diameter with papillary surface
often >20 mm in diameter with papillary surface often broad-based sessile lesion
often broad-based sessile lesion
malignant potential: <10 mm in 10%; 10 20 mm in 10%; >20 mm in 53%
Adenoma size & incidence of malignancy:
<5 mm in 0.5%; 5 9 mm in 1%; 10 20 mm in 5 10% >20 mm in 10 50% malignant
 Invasive carcinoma (= penetration of muscularis mucosa):
Invasive carcinoma (= penetration of muscularis mucosa):rare in a pedunculated adenoma of <15 mm
in 30% of villous adenomas of >50 mm
 All polyps >10 mm should be removed!
All polyps >10 mm should be removed! Time for adenoma-carcinoma sequence probably averages 10 15 years!
Time for adenoma-carcinoma sequence probably averages 10 15 years!
Probability of coexistent colonic growth:
synchronous adenoma in 50%
metachronous adenoma in 30 40%
synchronous adenocarcinoma in 1.5 5%
metachronous adenocarcinoma in 5 10%
asymptomatic (75%)
diarrhea, abdominal pain
peranal hemorrhage (67%)
Colonoscopy (incomplete in 16 43%)
BE:
Sensitivity of DCBE in detecting polyps:
<10 mm 80 83%; >10 mm 96 97%; all 84 88%; rate of detection of polyps <10 mm higher with DCBE than SCBE
P.798
 sessile flat/round polyp
sessile flat/round polyp pedunculated polyp: stalk >2 cm in length almost always indicative of a benign polyp
pedunculated polyp: stalk >2 cm in length almost always indicative of a benign polyp suggestive of malignancy: irregular lobulated surface, broad base = width of the base greater than height, retraction of colonic wall = dimpling/indentation/puckering at base of tumor, interval growth
suggestive of malignancy: irregular lobulated surface, broad base = width of the base greater than height, retraction of colonic wall = dimpling/indentation/puckering at base of tumor, interval growth lacelike/reticular surface pattern CHARACTERISTIC for villous adenoma (occasionally in tubular adenoma)
lacelike/reticular surface pattern CHARACTERISTIC for villous adenoma (occasionally in tubular adenoma)
| DDx: | (1) Nonneoplastic: hyperplastic polyp, inflammatory pseudopolyp, lymphoid tissue, ameboma, tuberculoma, foreign-body granuloma, malacoplakia, heterotopia, hamartoma (2) Neoplastic subepithelial: lipoma, leiomyoma, neurofibroma, hemangioma, lymphangioma, endothelioma, myeloblastoma, sarcoma, lymphoma, enteric cyst, duplication, varix, pneumatosis, hematoma, endometriosis |
Adenocarcinoma of Small Bowel
| Frequency: | 35% of primary malignant neoplasms of small bowel; about 50 less common than colonic carcinoma Most common primary malignancy of small bowel |
| Risk factors: | familial adenomatous polyposis (FAP), Crohn disease, sprue, Peutz-Jeghers syndrome, hereditary nonpolyposis colon cancer syndrome (Lynch syndrome), congenital bowel duplication, ileostomy, duodenal/jejunal bypass surgery |
| Histo: | mostly moderately to well differentiated; may arise in villous tumors/de novo; no correlation between size and invasiveness |
vague mild abdominal pain
anemia, weight loss
nausea, vomiting, anorexia
| Location: | duodenum (54%, especially near ampulla), jejunum (28%) > ileum (18%) in FAP: duodenum in celiac disease: jejunum in Crohn disease: ileum |
 annular stricture with overhanging edges (60%)
annular stricture with overhanging edges (60%) lobulated/ovoid polypoid sessile mass (41%)
lobulated/ovoid polypoid sessile mass (41%) Duodenal tumors tend to be papillary/polypoid!
Duodenal tumors tend to be papillary/polypoid! ulcerated mass (27%)
ulcerated mass (27%)
CT:
 soft-tissue mass with heterogeneous attenuation
soft-tissue mass with heterogeneous attenuation moderate contrast enhancement
moderate contrast enhancement
| Cx: | intussusception |
| Prognosis: | poor (often disseminated at time of presentation); 30% 5-year survival rate |
| DDx: | lymphoma (lymphadenopathy more bulky) |
Afferent Loop Syndrome
= PROXIMAL LOOP/BLIND LOOP SYNDROME
= partial intermittent obstruction of afferent loop leading to overdistension of loop by gastric juices after Billroth-II gastrojejunostomy
| Cause: | gastrojejunostomy with left-to-right anastomosis (= proximal jejunal loop attached to greater curvature instead of lesser curvature), mechanical factors (intussusception, adhesion, kinking), inflammatory disease, neoplastic infiltration of local mesentery or anastomosis, idiopathic motor dysfunction |
postprandial epigastric fullness relieved by bilious vomiting
vitamin B12 deficiency with megaloblastic anemia
afferent loop with abnormal bacterial flora (Gram negative, resembling colon in quality + quantity)
Abdominal plain film:
 normal in 85% (no air in lumen of afferent loop)
normal in 85% (no air in lumen of afferent loop)
UGI:
 preferential emptying of stomach into proximal loop
preferential emptying of stomach into proximal loop proximal loop stasis
proximal loop stasis regurgitation
regurgitation
CT:
 rounded water-density masses adjacent to head + tail of pancreas forming a U-shaped loop
rounded water-density masses adjacent to head + tail of pancreas forming a U-shaped loop oral contrast material may not enter loop
oral contrast material may not enter loop may result in biliary obstruction (increased pressure at ampulla)
may result in biliary obstruction (increased pressure at ampulla)
| Rx: | antibiotic therapy |
Aids
 Gastrointestinal involvement due to opportunistic infections + AIDS-associated neoplasms!
Gastrointestinal involvement due to opportunistic infections + AIDS-associated neoplasms! Pathologic abnormalities at multiple sites with single/several opportunistic organisms are frequent!
Pathologic abnormalities at multiple sites with single/several opportunistic organisms are frequent!A. VIRAL PATHOGENS
Cytomegalovirus infection
 Most common cause of life-threatening opportunistic viral infection in AIDS patients!
Most common cause of life-threatening opportunistic viral infection in AIDS patients!Organism: double-stranded DNA virus of the herpes family Infection: ubiquitous among humans occurring at an early age in populations with poor sanitation + crowded living conditions  Result of reactivation of latent virus in previously infected host!
Result of reactivation of latent virus in previously infected host!Prevalence: 13% of all gastrointestinal diseases in AIDS patients Path: infection of endothelial cells leads to small vessel vasculitis resulting in hemorrhage, ischemic necrosis, ulceration Histo: large mononuclear epithelial/endothelial cells that contain intranuclear/cytoplasmatic inclusions with surrounding inflammation Location: colon > small bowel (terminal ileum) > esophagus > stomach
@ Esophagus
 single/multiple large superficial ulcers
single/multiple large superficial ulcers
@ Small bowel
 luminal narrowing secondary to marked bowel wall thickening
luminal narrowing secondary to marked bowel wall thickening thickened irregular folds (vasculitis leading to thrombosis + ischemia)
thickened irregular folds (vasculitis leading to thrombosis + ischemia) penetrating ulcer perforation
penetrating ulcer perforation CMV pseudotumor (uncommon)
CMV pseudotumor (uncommon)
@ Colon (CMV colitis)
hematochezia, crampy abdominal pain, fever
 findings of toxic megacolon
findings of toxic megacolon discrete small well-defined nodules (similar to lymphoid nodular hyperplasia) throughout entire colon
discrete small well-defined nodules (similar to lymphoid nodular hyperplasia) throughout entire colon aphthous ulcers on background of normal mucosa
aphthous ulcers on background of normal mucosa marked bowel wall thickening
marked bowel wall thickening double-ring/target sign on CT (due to increased submucosal edema)
double-ring/target sign on CT (due to increased submucosal edema) ascites
ascites inflammation of pericolonic fat + fascia
inflammation of pericolonic fat + fascia
Rx: ganciclovir (effective in 75%)
P.799
Herpes simplex virus infection
 Result of reactivation of latent virus in previously infected host
Result of reactivation of latent virus in previously infected hostOrganism: neurotropic DNA virus of herpes family Prevalence: 70% for type 1, 16% for type 2 (endemic in United States); type 2 much more common in AIDS Infection: direct inoculation through mucous membrane contact; from dormant state in root ganglia reactivated + transported via efferent nerves to mucocutaneous surface Location: oral cavity, esophagus, rectum, anus  multiple small discrete ulcers
multiple small discrete ulcers
HIV infection
 Not an AIDS-defining illness!
Not an AIDS-defining illness!Infection: acute HIV-infection with transient immunosuppression/during AIDS  >2-cm large solitary ulcer in the mid- or distal esophagus (HIV-infected cells cause alterations in cytokines resulting in infiltration of inflammatory cells into submucosa + destruction of mucosa)
>2-cm large solitary ulcer in the mid- or distal esophagus (HIV-infected cells cause alterations in cytokines resulting in infiltration of inflammatory cells into submucosa + destruction of mucosa)
Rx: corticosteroids
B. FUNGAL PATHOGENS
Candidiasis
 The absence of thrush does not exclude the diagnosis of candida esophagitis!
The absence of thrush does not exclude the diagnosis of candida esophagitis!Organism: commensal fungus Candida albicans Prevalence: 10 20% (in United States); up to 80% in developing countries Location: oral cavity, esophagus  discrete linear/irregular longitudinally oriented filling defects in esophagus
discrete linear/irregular longitudinally oriented filling defects in esophagus
Cx: disseminated systemic candidiasis (rare + indicative of granulocytopenia from chemotherapy/direct inoculation via catheter) Histoplasmosis
Organism: dimorphic opportunistic fungus Prevalence: 10% GI involvement with disseminated histoplasmosis in AIDS patients Location: colon > terminal ileum  segmental inflammation/apple core lesion/bowel stricture
segmental inflammation/apple core lesion/bowel stricture hepatosplenomegaly
hepatosplenomegaly mesenteric lymphadenopathy
mesenteric lymphadenopathy diffuse hypoattenuation of spleen
diffuse hypoattenuation of spleen
C. PROTOZOAN PATHOGENS
Cryptosporidiosis
 One of the most common causes of enteric + biliary disease in AIDS patients!
One of the most common causes of enteric + biliary disease in AIDS patients!Organism: intracellular parasite Cryptosporidium Prevalence: isolated in 6% of all patients with AIDS; in 16% (in United States) + in up to 48% (in developing countries) in patients with diarrhea severe choleralike debilitating diarrhea with fluid loss of 10-17 L/day
Location: jejunum > other small bowel > stomach > colon  Cryptosporidium antritis (= area of focal gastric thickening + ulceration)
Cryptosporidium antritis (= area of focal gastric thickening + ulceration) small bowel dilatation (increased secretions)
small bowel dilatation (increased secretions) regular fold thickening + effacement (atrophy, blunting, fusion, loss of villi)
regular fold thickening + effacement (atrophy, blunting, fusion, loss of villi) toothpaste appearance of small bowel (mimicking sprue)
toothpaste appearance of small bowel (mimicking sprue) dilution of barium (hypersecretion)
dilution of barium (hypersecretion) marked antral narrowing (extensive inflammation)
marked antral narrowing (extensive inflammation) AIDS-related cholangitis
AIDS-related cholangitis
Dx: microscopic identification in stool/biopsy Pneumocystosis
 Likely to occur in patients treated with aerosolized pentamidine!
Likely to occur in patients treated with aerosolized pentamidine!Organism: eukaryotic microbe Pneumocystis carinii Prevalence: pulmonary infection in 75% of AIDS patients; in <1% dissemination Location: liver, spleen, lymph nodes  hepatic + splenic + nodal punctate calcifications
hepatic + splenic + nodal punctate calcifications multiple tiny echogenic foci in spleen
multiple tiny echogenic foci in spleen multiple low-attenuation lesions of varying size in spleen (foamy eosinophilic material) with subsequently progressive rimlike/punctate calcifications
multiple low-attenuation lesions of varying size in spleen (foamy eosinophilic material) with subsequently progressive rimlike/punctate calcifications
D. BACTERIAL PATHOGENS
1. tuberculosis
 Most common cause of serious HIV-related infection worldwide with tendency to occur earlier than other AIDS-defining opportunistic infections!
Most common cause of serious HIV-related infection worldwide with tendency to occur earlier than other AIDS-defining opportunistic infections!Prevalence: 4% (in United States) + 43% (in developing countries) of HIV-infected persons Infection: swallowing of infected sputum; hematogenous spread from pulmonary focus; direct extension from lymph node Location: lymph nodes, liver, spleen, peritoneum, GI tract (especially ileum, colon, ileocecal valve)  low-attenuation mesenteric lymphadenopathy (suggestive of necrosis)
low-attenuation mesenteric lymphadenopathy (suggestive of necrosis) segmental ulceration
segmental ulceration inflammatory stricture
inflammatory stricture hypertrophic lesion resembling polyp or mass
hypertrophic lesion resembling polyp or mass
2.Mycobacterium avium complex infection
= PSEUDO-WHIPPLE DISEASE in AIDS
 Most common opportunistic infection of bacterial origin in AIDS patients!
Most common opportunistic infection of bacterial origin in AIDS patients! Most common nontuberculous mycobacterial infection in AIDS patients!
Most common nontuberculous mycobacterial infection in AIDS patients!Organism: facultative intracellular acid-fast bacillus M. avium/M. intracellulare Infection: invasion of Peyer patches + adjacent mesenteric lymph nodes Histo: true granulomas with Langhans giant cells and caseous necrosis are rare because infection occurs in patients with advanced disease and a CD4 cell count of <100/ L diarrhea, malabsorption (similar clinical picture as in Whipple disease caused by Mycobacterium avium-intracellulare)
Location: jejunum (most common)  mild dilatation of middle + distal small bowel
mild dilatation of middle + distal small bowel wall thickening of small bowel loops
wall thickening of small bowel loops diffuse irregular mucosal fold thickening and nodularity without ulceration
diffuse irregular mucosal fold thickening and nodularity without ulceration mesenteric + retroperitoneal lymphadenopathy (1.0 1.5 cm in size) with homogeneous soft-tissue attenuation causing segmental separation of small bowel loops
mesenteric + retroperitoneal lymphadenopathy (1.0 1.5 cm in size) with homogeneous soft-tissue attenuation causing segmental separation of small bowel loops hepatosplenomegaly
hepatosplenomegaly multiple tiny echogenic foci in liver + spleen (occasionally large hypoechoic/low-attenuation lesions)
multiple tiny echogenic foci in liver + spleen (occasionally large hypoechoic/low-attenuation lesions)
P.800
Dx: (1) Visualization of large numbers of intracellular acid-fast bacilli in foamy histiocytes of tissue specimens
(2) Tissue cultureDDx: Whipple disease (positive with periodic acid-Schiff stain just like M. avium, but not with acid-fast stain, responsive to tetracyclines) E. OTHER INFECTIONS
Bacillary angiomatosis
Organism: Rickettsiales Bartonella henselae Histo: characteristic pattern of vascular proliferation with bacilli Location: cutis (mimicking Kaposi sarcoma), liver, spleen, lymph nodes  peliosis (blood-filled cystic spaces) of liver/spleen
peliosis (blood-filled cystic spaces) of liver/spleen abdominal lymphadenopathy with contrast enhancement
abdominal lymphadenopathy with contrast enhancement
Isospora belli
 Infection resembles cryptosporidiosis
Infection resembles cryptosporidiosisOrganism: protozoan pathogen Histo: oval oocysts within bowel lumen/epithelial cells; localized inflammation; fold atrophy Location: small intestine severe watery diarrhea
 fold thickening
fold thickening
F. AIDS-ASSOCIATED NEOPLASMS
Kaposi sarcoma
Non-Hodgkin lymphoma
 2nd most common AIDS-associated neoplasm
2nd most common AIDS-associated neoplasmPrevalence: in 4 10% of AIDS patients (60 times higher risk compared with general population); occurs in all AIDS risk groups Histo: multiclonal B-cell lymphoma of high or intermediate grade at initial presentation widely disseminated disease often with extranodal involvement
Location: CNS, bone marrow, GI tract (stomach, small bowel)
@ Stomach
 circumferential/focal wall thickening
circumferential/focal wall thickening mural mass ulceration
mural mass ulceration
@ Small bowel
 diffuse/focal wall thickening
diffuse/focal wall thickening excavated mass
excavated mass solitary/multiple liver lesions
solitary/multiple liver lesions
Differential diagnostic considerations:
Splenomegaly (31 45%)
Cause: nonspecific (most), lymphoma, infection (M. avium-intracellulare, P. carinii) Lymphadenopathy (21 60%)
Cause: reactive hyperplasia (most), Kaposi sarcoma, lymphoma, infections Size: <3 cm in diameter (in 95%) Hepatomegaly (20%)
Cause: nonspecific, hepatitis, fatty infiltration, lymphoma, Kaposi sarcoma AIDS-related cholangiopathy:
Organism: CMV, Cryptosporidium  papillary stenosis of CBD
papillary stenosis of CBD dilatation of extra- and intrahepatic bile ducts
dilatation of extra- and intrahepatic bile ducts periductal fibrosis
periductal fibrosis strictures + irregularities of bile ducts resembling primary sclerosing cholangitis
strictures + irregularities of bile ducts resembling primary sclerosing cholangitis intraluminal polypoid filling defects
intraluminal polypoid filling defects
AIDS-related esophagitis:
Organism: Candida, herpes simplex, CMV  giant esophageal ulcer: HIV (76%), CMV (14%)
giant esophageal ulcer: HIV (76%), CMV (14%) esophageal fistula/perforation: tuberculosis, actinomycosis
esophageal fistula/perforation: tuberculosis, actinomycosis
Gastritis
Organism: CMV (GE junction + prepyloric antrum), Cryptosporidium (antrum) AIDS enteritis
Organism: Cryptosporidium, M. avium complex AIDS colitis
ischemic bowel
acute appendicitis
neutropenic colitis
pseudomembranous colitis
infectious colitis/ileitis
Bowel obstruction
infection
intussusception: Kaposi sarcoma, lymphoma
Amebiasis
= primary infection of the colon by protozoan Entamoeba histolytica
| Countries: | worldwide distribution, most common in warm climates; South Africa, Egypt, India, Asia, Central + South America (20%); United States (5%) |
| Route: | contaminated food/water (human cyst carriers); cyst dissolves in small bowel; trophozoites settle in colon; proteolytic enzymes + hyaluronidase lyse intestinal epithelium; may embolize into portal venous + systemic blood system |
| Histo: | amebic invasion of mucosa + submucosa causing tiny ulcers, which spread beneath mucosa + merge into larger areas of necrosis; mucosal sloughing; secondary bacterial infection |
P.801
asymptomatic for months/years
acute attacks of diarrhea (loose mucoid bloodstained stools)
fever, headache, nausea
Location: (areas of relative stasis) right colon + cecum (90%) > hepatic + splenic flexures > rectosigmoid  loss of normal haustral pattern with granular appearance (edema, punctate ulcers)
loss of normal haustral pattern with granular appearance (edema, punctate ulcers) collarbutton ulcers
collarbutton ulcers cone-shaped cecum
cone-shaped cecum several cm long stenosis of bowel lumen in transverse colon, sigmoid colon, flexures (result of healing + fibrosis); in multiple segments
several cm long stenosis of bowel lumen in transverse colon, sigmoid colon, flexures (result of healing + fibrosis); in multiple segments ameboma = hyperplastic granuloma with bacterial invasion of amebic abscess; usually annular + constricting/intramural mass/cavity continuous with bowel lumen; shrinkage under therapy in 3 4 weeks
ameboma = hyperplastic granuloma with bacterial invasion of amebic abscess; usually annular + constricting/intramural mass/cavity continuous with bowel lumen; shrinkage under therapy in 3 4 weeks ileocecal valve thickened + fixed in open position with reflux
ileocecal valve thickened + fixed in open position with reflux involvement of distal ileum (10%)
involvement of distal ileum (10%)
| Dx: | stool examination/rectal biopsy |
| Cx: | (1) Toxic megacolon with perforation (2) Amebic abscess in liver (2%), brain, lung (transdiaphragmatic spread of infection), pericolic, ischiorectal, subphrenic space (3) Intussusception in children (due to ameboma) (4) Fistula formation (colovesical, rectovesical, rectovaginal, enterocolic) |
Amyloidosis
= group of heterogeneous disorders caused by interstitial deposits of a protein-polysaccharide in various organs leading to hypoxia, mucosal edema, hemorrhage, ulceration, mucosal atrophy, muscle atrophy
| Cause: | (a) prolonged antigenic stimulation of RES by chronic infection (b) disorder of immunoincompetence (c) aging (d) idiopathic |
| Histo: | amorphous eosinophilic hyaline material deposited around terminal blood vessels, stains with Congo red + crystal violet; green birefringence under polarizing light; amyloid fibrils have -pleated sheet structure (= fibrilloses) |
Biochemical classification (1979):
AL amyloidosis
(A = amyloidosis, L = light chain immunoglobulin)
monoclonal protein in serum + urine
occurs in primary amyloidosis + myeloma-associated amyloidosis
Histo: massive deposits in muscularis mucosae + submucosa  thickening of folds with polyps/large nodules
thickening of folds with polyps/large nodules
SAA amyloidosis (S = serum, AA = amyloid A)
occurs in secondary = reactive amyloidosis
Histo: expansion of lamina propria  coarse mucosal pattern + innumerable fine granular elevations
coarse mucosal pattern + innumerable fine granular elevations
AF amyloidosis (A = amyloid, F = familial)
AF prealbumin as precursor of fibrils
occurs in familial amyloidosis
AS amyloidosis (A = amyloid, S = senile)
AS prealbumin as precursor of fibrils
occurs in senile amyloidosis
 massive amyloid deposition
massive amyloid deposition
AH amyloidosis (A = amyloid, H = hemodialysis)
2 microglobulin as precursor of fibrils
AE amyloidosis (A = amyloid, E = endocrine)
calcitonin produced by medullary thyroid carcinoma is precursor of fibrils
Reimann classification (1935):
Primary = idiopathic amyloidosis
= probably autosomal dominant inheritance with immunologically determined dysfunction of plasma cells
absence of discernible preceding/concurrent disease
Location: (predominant involvement of connective tissues + mesenchymal organs) heart (90%), lung (30 70%), liver (35%), spleen (40%), kidneys (35%), adrenals, tongue (40%), GI tract (70%), skin + subcutis (25%)  tendency to nodular deposition
tendency to nodular deposition
2.Secondary amyloidosis (most common form)
following/coexistent with prolonged infectious/inflammatory processes
Cause: rheumatoid arthritis (in 20%), Still disease, tuberculosis, osteomyelitis, leprosy, chronic pyelonephritis, bronchiectasis, ulcerative colitis, Waldenstr m macro-globulinemia, familial Mediterranean fever, lymphoreticular malignancy, paraplegia Location: spleen, liver, kidneys (>80%), breast, tongue, GI tract, connective tissue  small amyloid deposits
small amyloid deposits
3.Amyloidosis associated with multiple myeloma
may precede development of multiple myeloma
Incidence: 10 15%  primary amyloidosis with osteolytic lesions in myelomatous disease
primary amyloidosis with osteolytic lesions in myelomatous disease
4.Tumor-forming/organ-limited amyloidosis
related to primary type
(a) hereditary = familial amyloidosis
(b) senile amyloidosis (limited to heart/brain/pancreas/spleen)
 large localized masses
large localized masses
 GI involvement in primary more common than in secondary amyloidosis!
GI involvement in primary more common than in secondary amyloidosis!malabsorption (diarrhea, protein loss)
occult GI bleeding
obstruction
macroglossia
@ Esophagus (11%)
 loss of peristalsis
loss of peristalsis megaesophagus
megaesophagus
P.802
@ Stomach (37%)
postprandial epigastric pain + heartburn
acute erosive hemorrhagic gastritis
(a) diffuse infiltrative form
 small-sized stomach with rigidity + loss of distensibility simulating linitis plastica (from thickening of gastric wall)
small-sized stomach with rigidity + loss of distensibility simulating linitis plastica (from thickening of gastric wall) effaced rugal pattern
effaced rugal pattern diminished/absent peristalsis
diminished/absent peristalsis marked retention of food
marked retention of food
(b) localized infiltration (often located in antrum)
 irregularly narrowed + rigid antrum
irregularly narrowed + rigid antrum thickened rugae
thickened rugae superficial erosions/ulcerations
superficial erosions/ulcerations
(c) amyloidoma = well-defined submucosal mass
@ Small bowel (74%)
diffuse form (more common)
 diffuse uniform thickening of valvulae conniventes in entire small bowel
diffuse uniform thickening of valvulae conniventes in entire small bowel broadened flat undulated mucosal folds (mucosal atrophy)
broadened flat undulated mucosal folds (mucosal atrophy) jejunalization of ileum
jejunalization of ileum impaired intestinal motility
impaired intestinal motility small bowel dilatation
small bowel dilatation
localized form (less common)
 multiple pea-/marble-sized deposits
multiple pea-/marble-sized deposits pseudoobstruction = physical + plain-film findings suggesting mechanical obstruction with patent large + small bowel on barium examination (involvement of myenteric plexus)
pseudoobstruction = physical + plain-film findings suggesting mechanical obstruction with patent large + small bowel on barium examination (involvement of myenteric plexus)
Cx: small bowel infarction @ Colon (27%):
 pseudopolyps in colon
pseudopolyps in colon
@ Bone:
 bone cysts
bone cysts
@ Liver:
Path: extracellular deposition of amyloid in the spaces of Disse (= narrow gaps between endothelial linings of sinusoids and hepatocytes of hepatic lamina) with progressive encroachment on hepatic parenchymal cells + sinusoids hepatic function usually preserved
CT:
 hepatomegaly
hepatomegaly regions of low attenuation with decreased contrast enhancement
regions of low attenuation with decreased contrast enhancement
@ Spleen:
Histo: (a) nodular form involving lymph follicles
(b) diffuse form infiltrating red pulp discrete masses
discrete masses splenomegaly (4 13%)
splenomegaly (4 13%)
MR:
 T2 values significantly lower than normal
T2 values significantly lower than normal
| Cx: | spontaneous splenic rupture (from vascular fragility + acquired coagulopathy) |
| Dx: | by rectal/gingival biopsy |
| DDx: | Whipple disease, intestinal lymphangiectasia, lymphosarcoma |
Angiodysplasia of Colon
= VASCULAR ECTASIA = ARTERIOVENOUS MALFORMATION (not a true AVM)
Cause: age-related degenerative dilatation of normal vessels in submucosa of bowel wall Theory: colonic contractions result in dilatation of colonic veins, venules and capillaries forging multiple small arteriovenous communications Associated with: aortic stenosis (20%); NOT related to extraintestinal angiomatous lesions Prevalence: most common vascular lesion of GI tract! at autopsy: 2% at colonoscopy: 0.8% (age >50 years) Age: majority > 55 years; M = F Location: (a) cecum + ascending colon (74%)
(b) jejunum, ileum (15%)
(c) descending + sigmoid colon ( 25%)Site: usually at antimesenteric border chronic intermittent low-grade bleeding
occasionally massive bleeding
NUC (Tc-99m labeled RBCs):
 focus of tracer accumulation at site of bowel hemorrhage migrating with peristalsis
focus of tracer accumulation at site of bowel hemorrhage migrating with peristalsis
BE:
 no abnormality (due to soft submucosal lesion)
no abnormality (due to soft submucosal lesion)
NUC:
 increased tracer accumulation of Tc-99m labeled RBC
increased tracer accumulation of Tc-99m labeled RBC
Angio:
 arterial tuft = cluster/tangle of vessels during arterial phase along antimesenteric border
arterial tuft = cluster/tangle of vessels during arterial phase along antimesenteric border early opacification of draining ileocolic vein
early opacification of draining ileocolic vein densely opacified dilated tortuous ileocolic vein into late venous phase
densely opacified dilated tortuous ileocolic vein into late venous phase contrast extravasation into bowel lumen (unusual)
contrast extravasation into bowel lumen (unusual)
| Rx: | surgical excision |
Anisakiasis
= parasitic disease of GI tract
Cause: ingestion of Anisakis larvae present in raw/undercooked fish (mackerel, cod, pollack, herring, whiting, bonito, squid) consumed as sashimi, sushi, ceviche, lomi-lomi Organism: worm with straight/serpentine/circular threadlike appearance  Site of penetration by larvae determines clinical form!
Site of penetration by larvae determines clinical form!@ Gastric anisakiasis
acute gastric pain, nausea, vomiting a few hours after ingestion (DDx: acute gastritis, peptic ulcer, food poisoning, neoplasia)
eosinophilia
 mucosal edema
mucosal edema about 3-cm-long threadlike filling defects (= larvae)
about 3-cm-long threadlike filling defects (= larvae)
@ Intestinal anisakiasis
diffuse abdominal tenderness/colicky abdominal pain, nausea, vomiting (DDx: acute appendicitis, regional enteritis, intussusception, ileus, diverticulitis, neoplasia)
leukocytosis without eosinophilia (frequent)
Histo: marked edema, eosinophilic infiltrates, granuloma formation  thickened folds
thickened folds disappearance of Kerckring folds
disappearance of Kerckring folds thumbprinting/saw-tooth appearance
thumbprinting/saw-tooth appearance irregular luminal narrowing
irregular luminal narrowing eosinophilic ascites (DDx: eosinophilic gastroenteritis, hypereosinophilic syndrome)
eosinophilic ascites (DDx: eosinophilic gastroenteritis, hypereosinophilic syndrome)Cx: ileus
P.803
@ Colonic anisakiasis (rare)
DDx: colonic tumor
Anorectal Malformation
Rectal atresia
= open anus + atretic rectal segment superior to anus + no fistula
Ectopic anus
= fistulous opening of bowel due to failure of terminal bowel to descend normally
Site of arrest: high/low colon arrest = above/below puborectal sling most common anomaly of anorectal segment
anal dimple + external sphincter in normal position
Location of fistula: perineum, vestibule, vagina, urethra, bladder, cloaca  low small bowel/colonic obstruction
low small bowel/colonic obstruction M line accurately represents level of puborectal muscle = line drawn horizontally through junction of lower 1/3 + upper 2/3 of ischium on lateral radiograph
M line accurately represents level of puborectal muscle = line drawn horizontally through junction of lower 1/3 + upper 2/3 of ischium on lateral radiograph
Imperforate anus
= blind ending of terminal bowel + no fistula
Cloacal malformation
Cloacal exstrophy
Embryology:
during weeks 3 and 4 the dorsal part of the yolk sac folds are incorporated into embryo forming the primitive hindgut consisting of distal part of transverse + descending + sigmoid colon, rectum, superior portion of anal canal, epithelium of urinary bladder, and most of the urethra; at 4 weeks the transverse rectovesical septum descends caudally between allantois and hindgut dividing the cloaca into urogenital sinus ventrally + anorectal canal dorsally; by 7th week the rectovaginal septum fuses with cloacal membrane creating a urogenital membrane ventrally + anal membrane dorsally; perineum is formed by fusion of rectovesical septum + cloacal membrane; anal membrane ruptures by 9th week
| In 48% associated with: | (part of VACTERL syndrome) |
GU anomalies (20%):
renal agenesis/ectopia, vesicoureteral reflux, obstruction, hypospadia (3.1%); M > F
Lumbosacral segmentation anomalies (30%):
dysplasia, agenesis, hemivertebrae
GI anomalies (11%):
esophageal atresia tracheoesophageal fistula (4%), duodenal atresia/stenosis
Cardiovascular anomalies (8%)
Abdominal wall (2%)
Cleft lip cleft palate (1.6%)
Down syndrome (1.5%)
Meningomyelocele (0.5%) + occult myelodysplasia
Others (8%)
Antral Mucosal Diaphragm
= ANTRAL WEB
Age range: 3 months to 80 years Associated with: gastric ulcer (30 50%) symptomatic if opening <1 cm
Location: usually 1.5 cm from pylorus (range 0 7 cm)  constant symmetric band of 2 3 mm thickness traversing the antrum perpendicular to long axis of stomach
constant symmetric band of 2 3 mm thickness traversing the antrum perpendicular to long axis of stomach double bulb appearance (in profile)
double bulb appearance (in profile) concentric/eccentric orifice
concentric/eccentric orifice normal peristaltic activity
normal peristaltic activity
Appendicitis
| Prevalence: | 1 4% in children with acute abdominal pain |
| Lifetime risk: | 7 9% in Western world population |
| Etiology: | obstruction of appendiceal lumen by lymphoid hyperplasia (60%), fecolith (33%), foreign bodies (4%), stricture, tumor, parasite; Crohn disease (in 25%) |
| Cause: | luminal obstruction from |
fecolith (11 52%) = hard crushable concretions from inspissation of fecal material + inorganic salts
appendiceal calculus = hard noncrushable calcified stone (7 15%)
lymphoid hyperplasia
foreign body
parasite
primary tumor: carcinoid, adenocarcinoma, Kaposi sarcoma, lymphoma
metastatic tumor: colon cancer, breast cancer
Pathogenesis:
continued secretion of mucus in appendiceal obstruction elevates intraluminal pressure + distends lumen; venous engorgement + arterial compromise + tissue ischemia ensues after intraluminal pressure exceeds capillary perfusion pressure
| Peak age: | 2nd decade; thereafter declining incidence; M:F = 3:2 (in teens/young adults, thereafter 1:1) Rare under the age of 2 years! |
80% clinical accuracy (78 92% in males, 58 85% in females):
Diagnostic dilemma (20 35%):
in elderly, ovulating women, infants/young children
 32 45% rate of misdiagnosis in women between ages 20 40!
32 45% rate of misdiagnosis in women between ages 20 40! 5 25% false-negative appendectomy rate for pediatric population!
5 25% false-negative appendectomy rate for pediatric population!
pain
mild poorly localized visceral pain of 4 6 hours duration referred to epigastrium + periumbilical region
crampy pain migrates into RLQ pain over appendix = McBurney sign (72%) and becomes continuous + more severe (somatic pain)
anorexia, nausea, vomiting (40%)
afebrile/low-grade fever (56%)
 Suspect perforation with temperature >38.3
Suspect perforation with temperature >38.3
leukocytosis with left shift (88%)
| Clinical scoring system: | MANTRELS score of 10 |
| Migration of pain to RLQ | 1 |
| Anorexia | 1 |
| Nausea and vomiting | 1 |
| Tenderness in RLQ | 2 |
| Rebound pain | 1 |
| Elevated temperature | 1 |
| Leukocytosis | 2 |
| Shift of WBC count to left | 1 |
P.804
Location:
base of appendix: posteromedial wall of cecum + 3 cm below ileocecal valve
 The appendix is on the same side of the cecum as the ileocecal valve!
The appendix is on the same side of the cecum as the ileocecal valve!
tip of appendix: retrocecal, subcecal, retroileal, preileal, within pelvis (30%), extraperitoneal (5%)
Abdominal plain film (abnormalities seen in <50%):
 Plain-film findings become more distinctive after perforation, while clinical findings subside/simulate other diseases!
Plain-film findings become more distinctive after perforation, while clinical findings subside/simulate other diseases! usually laminated calcified appendicolith in RLQ (in 7 15%):
usually laminated calcified appendicolith in RLQ (in 7 15%): Appendicolith + abdominal pain = 90% probability of acute appendicitis!
Appendicolith + abdominal pain = 90% probability of acute appendicitis! Appendicolith in acute appendicitis means a high probability for gangrene/perforation!
Appendicolith in acute appendicitis means a high probability for gangrene/perforation!
 cecal changes:
cecal changes: thickening of cecal wall
thickening of cecal wall water-density mass + paucity/absence of intestinal gas in RLQ (in 24% of perforations)
water-density mass + paucity/absence of intestinal gas in RLQ (in 24% of perforations) cecal ileus = gas-fluid level in cecum in gangrene (= local paralysis)
cecal ileus = gas-fluid level in cecum in gangrene (= local paralysis) colon cutoff sign = amputation of gas at the hepatic flexure (in 20% of perforations) due to spastic ascending colon
colon cutoff sign = amputation of gas at the hepatic flexure (in 20% of perforations) due to spastic ascending colon
 small bowel obstruction pattern = small bowel dilatation with air-fluid levels (in 43% of perforations)
small bowel obstruction pattern = small bowel dilatation with air-fluid levels (in 43% of perforations) extraluminal gas (in 33% of perforations):
extraluminal gas (in 33% of perforations): gas loculation
gas loculation mottled bacteriogenic gas
mottled bacteriogenic gas pneumoperitoneum (rare)
pneumoperitoneum (rare)
 loss of fat planes:
loss of fat planes: focal increase in thickness of lateral abdominal wall in 32% (= edema between properitoneal fat line + cecum)
focal increase in thickness of lateral abdominal wall in 32% (= edema between properitoneal fat line + cecum) loss of properitoneal fat line
loss of properitoneal fat line loss of pelvic fat planes around the bladder/right obturator (= fluid/pus in cul-de-sac)
loss of pelvic fat planes around the bladder/right obturator (= fluid/pus in cul-de-sac) loss of definition of right inferior hepatic outline (= free peritoneal fluid)
loss of definition of right inferior hepatic outline (= free peritoneal fluid) distortion of psoas margin + flank stripes
distortion of psoas margin + flank stripes
 scoliosis (due to muscle irritation)
scoliosis (due to muscle irritation)
BE/UGI (accuracy 50 84%):
 failure to fill appendix with barium (normal finding in up to 35%)
failure to fill appendix with barium (normal finding in up to 35%) indentation along medial wall of cecum (= edema at base of appendix/matted omentum/periappendiceal abscess)
indentation along medial wall of cecum (= edema at base of appendix/matted omentum/periappendiceal abscess)
Graded-compression US (85% sensitive, 92% specific, 78 96% accurate, 91 94% PPV, 89 97% NPV):
 Nondiagnostic study in 4% due to inadequate compression of RLQ
Nondiagnostic study in 4% due to inadequate compression of RLQ Useful in ovulating women (false-negative appendectomy rate in males 15%, in females 35%) + infants/children
Useful in ovulating women (false-negative appendectomy rate in males 15%, in females 35%) + infants/children visualization of noncompressible appendix as a blind-ending tubular aperistaltic structure (seen only in 2% of normal adults, but in 50% of normal children)
visualization of noncompressible appendix as a blind-ending tubular aperistaltic structure (seen only in 2% of normal adults, but in 50% of normal children) laminated wall with target appearance of 6 mm in total diameter on cross section (81% SPECIFIC)/mural wall thickness 2 mm
laminated wall with target appearance of 6 mm in total diameter on cross section (81% SPECIFIC)/mural wall thickness 2 mm lumen may be distended with anechoic/hyperechoic material
lumen may be distended with anechoic/hyperechoic material pericecal/periappendiceal fluid
pericecal/periappendiceal fluid increased periappendiceal echogenicity (= infiltration of mesoappendix/pericecal fat)
increased periappendiceal echogenicity (= infiltration of mesoappendix/pericecal fat) enlarged mesenteric lymph nodes
enlarged mesenteric lymph nodes loss of wall layers = gangrenous appendix
loss of wall layers = gangrenous appendix perforated appendix (23 73%):
perforated appendix (23 73%): loss of echogenic submucosal layer
loss of echogenic submucosal layer appendix no longer visualized (40 60%)
appendix no longer visualized (40 60%) loculated periappendiceal/pelvic fluid collection gas bubbles (= abscess)
loculated periappendiceal/pelvic fluid collection gas bubbles (= abscess) prominent hyperechoic mesoappendix/pericecal fat
prominent hyperechoic mesoappendix/pericecal fat visualization of appendicolith (6%) = bright echogenic focus with clean distal acoustic shadowing
visualization of appendicolith (6%) = bright echogenic focus with clean distal acoustic shadowing gas bubbles localized to perforation site
gas bubbles localized to perforation site
 hypoechoic zones with poor margination within inflamed fat (= phlegmonous appendicitis)
hypoechoic zones with poor margination within inflamed fat (= phlegmonous appendicitis) sympathetic thickening of adjacent terminal ileum + ascending colon
sympathetic thickening of adjacent terminal ileum + ascending colon
False-negative US:
failure to visualize appendix
inability of adequate compression
aberrant location of appendix (eg, retrocecal)
appendiceal perforation
early inflammation limited to appendiceal tip
False-positive US:
normal appendix mistaken for appendicitis
alternate diagnosis: Crohn disease, pelvic inflammatory disease, inflamed Meckel diverticulum
spontaneous resolution of acute appendicitis
Color Doppler US:
 increased conspicuity (= increase in size + number) of circumferential vessels in and around the wall of the appendix (= hyperemia)
increased conspicuity (= increase in size + number) of circumferential vessels in and around the wall of the appendix (= hyperemia) decreased resistance of arterial waveforms
decreased resistance of arterial waveforms continuous/pulsatile venous flow
continuous/pulsatile venous flow decreased/no perfusion = gangrenous appendicitis
decreased/no perfusion = gangrenous appendicitis
CT (87 100% sensitive, 89 98% specific, 93 98% accurate, 92 98% PPV, 95 100% NPV):
 normal appendix visualized in 67 100%:
normal appendix visualized in 67 100%: 1 2 cm below ileocecal junction from posteromedial aspect of cecum with a diameter of up to 10 mm
1 2 cm below ileocecal junction from posteromedial aspect of cecum with a diameter of up to 10 mm
 abnormal appendix:
abnormal appendix: distended lumen (appendix >7 mm in diameter)
distended lumen (appendix >7 mm in diameter) circumferential wall thickening
circumferential wall thickening homogeneously enhancing wall mural stratification ( target sign )
homogeneously enhancing wall mural stratification ( target sign ) appendicolith = homogeneous/ringlike calcification (25%)
appendicolith = homogeneous/ringlike calcification (25%) distal appendicitis = abnormal tip of appendix + normal proximal appendix and normal cecal apex
distal appendicitis = abnormal tip of appendix + normal proximal appendix and normal cecal apex
 periappendicular inflammation (98%):
periappendicular inflammation (98%): linear streaky densities in periappendicular/pericecal/mesenteric/pelvic fat
linear streaky densities in periappendicular/pericecal/mesenteric/pelvic fat subtle clouding of mesentery
subtle clouding of mesentery local fascial thickening
local fascial thickening free peritoneal fluid
free peritoneal fluid mesenteric lymphadenopathy
mesenteric lymphadenopathy marked terminal ileal wall thickening
marked terminal ileal wall thickening localized lymphadenopathy
localized lymphadenopathy peritonitis
peritonitis small-bowel obstruction
small-bowel obstruction
P.805
 circumferential/focal cecal apical thickening (80%):
circumferential/focal cecal apical thickening (80%): arrowhead sign = funnel of contrast medium in cecum symmetrically centering about occluded orifice of appendix (30% sensitive, 100% specific)
arrowhead sign = funnel of contrast medium in cecum symmetrically centering about occluded orifice of appendix (30% sensitive, 100% specific)
 perforated appendix:
perforated appendix: defect in the enhancing appendiceal wall
defect in the enhancing appendiceal wall nonvisualization of appendix (due to fragmentation)
nonvisualization of appendix (due to fragmentation) phlegmon = diffuse substantial inflammation of periappendiceal fat with ill-defined fluid collections(DDx: ileocolitis with secondary inflammation of appendix)
phlegmon = diffuse substantial inflammation of periappendiceal fat with ill-defined fluid collections(DDx: ileocolitis with secondary inflammation of appendix) pericecal/mesenteric/interloop/pelvic abscess = poorly encapsulated single/multiple fluid collection with air/extravasated contrast material
pericecal/mesenteric/interloop/pelvic abscess = poorly encapsulated single/multiple fluid collection with air/extravasated contrast material extraluminal appendicolith
extraluminal appendicolith extraluminal air
extraluminal air
False-negative CT:
overlapping range in maximal appendiceal diameter between inflamed + uninflamed appendix
appendix mistaken for unopacified bowel
inflammation limited to appendiceal tip
Prognosis:
mild acute appendicitis may resolve spontaneously (after relief of inciting obstruction)
recurrent appendicitis (10%) = repeated similar episodic attacks of RLQ pain leading to appendectomy + showing acute inflammation
chronic appendicitis (1%) = RLQ pain of >3 weeks + no alternative diagnosis + chronic active inflammation on histology + relief of symptoms after appendectomy
Mortality rate of 1% (associated with perforation)
| Cx: | perforation (13 30 73%), abscess formation, peritonitis, wound infection, sepsis, infertility, adhesions, bowel obstruction, death |
| Rx: | finding of appendicolith is sufficient evidence to perform prophylactic appendectomy in asymptomatic patients (50% have perforation/abscess formation at surgery) |
| DDx: | colitis, diverticulitis, epiploic appendagitis, small bowel obstruction, infectious enteritis, duodenal ulcer, pancreatitis, intussusception, Crohn disease, mesenteric lymphadenitis, ovarian torsion, pelvic inflammatory disease; primary neoplasm of appendix Only 22 38% of children referred for suspected appendicitis actually have appendicitis |
Ascariasis
= most common parasitic infection in world; cosmopolitan occurrence; endemic along Gulf Coast, Ozark Mountains, Nigeria, Southeast Asia
| Organism: | Ascaris lumbricoides = roundworm parasite, 15 35 cm in length; production of 200,000 eggs daily |
| Cycle: | infection by contaminated soil, eggs hatch in duodenum, larvae penetrate into venules/lymphatics, carried to lungs, migrate to alveoli and up the bronchial tree, swallowed, maturation in jejunum within 2.5 months |
| Age: | children age 1 10 years |
colic
eosinophilia
appendicitis
hematemesis/pneumonitis
jaundice (if bile ducts infested)
Location: jejunum > ileum (99%), duodenum, stomach, CBD, pancreatic duct  15-35-cm-long tubular filling defects
15-35-cm-long tubular filling defects barium-filled enteric canal outlined within Ascaris
barium-filled enteric canal outlined within Ascaris whirled appearance, occasionally in coiled clusters ( bolus of worms )
whirled appearance, occasionally in coiled clusters ( bolus of worms )
| Cx: | (1) Perforation of bowel (2) Mechanical obstruction |
Bannayan-Riley-Ruvalcaba Syndrome
= RUVALCABA-MYHRE-SMITH SYNDROME
Cause: autosomal dominant transmission pigmented genital lesions
 hamartomatous intestinal polyps (in 45%): usually in distal ileum + colon
hamartomatous intestinal polyps (in 45%): usually in distal ileum + colon macrocephaly
macrocephaly subcutaneous and visceral lipomas + hemangiomas
subcutaneous and visceral lipomas + hemangiomas
Barrett Esophagus
= BARRETT SYNDROME
= replacement of stratified squamous epithelium by metaplastic columnar epithelium (Barrett epithelium) containing goblet cells but no parietal cells
| Cause: | chronic gastroesophageal reflux with epithelial injury from esophagitis |
Contributing factors:
genetic influence, reduced LES pressure, transient LES relaxation, hiatal hernia, delayed acid clearance, reduced acid sensitivity, duodenogastroesophageal reflux, alcohol, tobacco, chemotherapy, scleroderma (37%), S/P repair of esophageal atresia/esophagogastric resection/Heller esophagomyotomy
| Histo: | (1) specialized columnar epithelium (proximal) (2) junctional-type epithelium (distal to above) (3) fundic-type epithelium (most distally) |
| Prevalence: | in general 0.3-4%; 7-10% of patients with advanced chronic reflux esophagitis |
| Associated with: | moderate + severe esophagitis (94%), no/mild esophagitis (6%) |
| Age: | 0-15 years and 40-88 years (mean of 55 years); M > F; mainly among Whites |
dysphagia (due to esophageal stricture)
signs of reflux esophagitis: heartburn, substernal chest pain, regurgitation
low-grade upper intestinal bleeding
asymptomatic
| Location: | middle to lower esophagus |
| N.B.: | the squamocolumnar junction does not coincide with the GE junction, is irregular and lies > 2-3 cm orad from the gastroesophageal junction |
| Distribution: | circumferential/focal |
P.806
 several-cm-long stricture (71%) in midesophagus (40%) or lower esophagus (60%) [DDx: peptic stricture without Barrett esophagus]
several-cm-long stricture (71%) in midesophagus (40%) or lower esophagus (60%) [DDx: peptic stricture without Barrett esophagus] large deep wide-mouthed peptic ulcer (= Barrett ulcer) at upwardly displaced squamocolumnar junction/within columnar epithelium
large deep wide-mouthed peptic ulcer (= Barrett ulcer) at upwardly displaced squamocolumnar junction/within columnar epithelium fine reticular mucosal pattern (3-30%) resembling areae gastricae of the stomach = netlike web of barium-filled grooves surrounding small tufts of mucosa; located distally from stricture (DDx: gastroesophageal reflux, monilial + viral esophagitis, superficial spreading carcinoma)
fine reticular mucosal pattern (3-30%) resembling areae gastricae of the stomach = netlike web of barium-filled grooves surrounding small tufts of mucosa; located distally from stricture (DDx: gastroesophageal reflux, monilial + viral esophagitis, superficial spreading carcinoma) thickened irregular mucosal folds (28 86%)
thickened irregular mucosal folds (28 86%) fine granular mucosal pattern (DDx: reflux esophagitis, acanthosis, leukoplakia, superficial spreading carcinoma, moniliasis/herpes simplex/CMV esophagitis)
fine granular mucosal pattern (DDx: reflux esophagitis, acanthosis, leukoplakia, superficial spreading carcinoma, moniliasis/herpes simplex/CMV esophagitis) gastroesophageal reflux (45 63%)
gastroesophageal reflux (45 63%) distal esophageal widening (34 66%; due to abnormal motility)
distal esophageal widening (34 66%; due to abnormal motility) hiatal hernia (75 94%)
hiatal hernia (75 94%) uptake of Tc-99m pertechnetate by columnar epithelium
uptake of Tc-99m pertechnetate by columnar epithelium
| Dx: | velvety pinkish red appearance of gastric-type mucosa extending from gastric mucosa into distal esophagus (endoscopy with biopsy) |
| Cx: | (1) Ulceration penetration into mediastinum (2) Stricture 3. Adenocarcinoma (0 10 46%;) 40-fold higher risk than general population plaquelike/focal irregularity/nodularity/sessile polyps |
| Rx: | (1) stop smoking, avoid bedtime snacks + foods that lower LES pressure, lose excess weight (2) suppress gastric acidity: antacids, H2-receptor antagonists (cimetidine, ranitidine, famotidine), H+K+-adenosintriphosphatase inhibitor (omeprazole) (3) improve LES pressure: metoclopramide, bethanechol (4) esophageal resection in high-grade dysplasia |
Beh et Syndrome
[Hulusi Beh et (1889 1948), dermatologist in Istanbul, Turkey]
= uncommon chronic multisystem inflammatory disorder of unknown etiology with relapsing course characterized by mucocutaneous-ocular symptoms as a triad of aphthous stomatitis, genital ulcers, ocular inflammation
Countries: worldwide, most common in eastern Mediterranean countries, eastern rim of Asia Histo: nonspecific necrotizing vasculitis with deposition of immune complexes in walls of small blood vessels Age at onset: 3rd decade; M:F = 2:1 Major criteria: buccal + genital ulceration, ocular inflammation, skin lesions Minor criteria: thrombophlebitis, GI + CNS lesions, arthritis, family history abdominal pain + diarrhea (50%)
| @ Mucocutaneous: | aphthous stomatitis, papules, pustules, vesicles, folliculitis, erythema nodosum-like lesions |
| @ | Genital: ulcers on penis + scrotum/vulva + vagina |
| @ Ocular: | relapsing iridocyclitis, hypopyon, choroiditis, papillitis, retinal vasculitis |
| @Articular: | mild nondestructive arthritis |
| @ | Vascular: migratory thrombophlebitis |
| @CNS: | chronic meningoencephalitis |
| DDx: | Reiter syndrome, Stevens-Johnson syndrome, SLE, ulcerative colitis, ankylosing spondylitis |
Intestinal Beh et Disease
= large deeply penetrating intestinal ulcers (HALLMARK)
Incidence: 10 40% Location: terminal ileum, cecum, ascending colon, transverse colon  deep round ulcers similar in appearance to peptic ulcers of stomach/duodenum
deep round ulcers similar in appearance to peptic ulcers of stomach/duodenum multiple shallow/longitudinal/aphthoid ulcers
multiple shallow/longitudinal/aphthoid ulcers
CT:
 polypoid lesion/thickened bowel wall (mural edema associated with deep ulcer penetration)
polypoid lesion/thickened bowel wall (mural edema associated with deep ulcer penetration) contrast enhancement (71%)
contrast enhancement (71%) minimal lymphadenopathy, mostly <10 mm
minimal lymphadenopathy, mostly <10 mm
| Cx (56%): | panperitonitis with high mortality due to tendency for perforation at multiple sites; fistula; hemorrhage |
| Prognosis: | recurrence in 40 45% adjacent to surgical anastomosis |
| DDx: | ulcerative colitis, Crohn disease |
Bezoar
[padzahr, Persian = antidote, counterpoison]
= persistent concretions of foreign matter composed of accumulated ingested material in intestines
| Incidence: | 0.4% (large endoscopic series) |
| Etiology: | material unable to exit stomach because of large size, indigestibility, gastric outlet obstruction, poor gastric motility (diabetes, mixed connective tissue disease, myotonic dystrophy, hypothyroidism) |
Predisposition:
previous gastric surgery (vagotomy, pyloroplasty, antrectomy, partial gastrectomy), inadequate chewing, missing teeth, dentures, massive overindulgence of food with high fiber contents
anorexia, bloating, early satiety/may be asymptomatic
Phytobezoar
= poorly digested fibers, skin + seeds of fruits and vegetables usually forming in stomach, may become impacted in small bowel
Incidence: 55% of all bezoars history of recent ingestion of pulpy foods
| Food: | oranges, persimmons (most common, unripe persimmons contain the tannin shibuol that forms a gluelike coagulum after contact with dilute acid) |
| Site of impaction: | stomach, jejunum, ileum |
 intraluminal filling defect without constant site of attachment to bowel wall
intraluminal filling defect without constant site of attachment to bowel wall interstices filled with barium
interstices filled with barium coiled-spring appearance (rare)
coiled-spring appearance (rare) partial/complete obstruction
partial/complete obstruction
| Cx: | decubitus ulceration + pressure necrosis of bowel wall, perforation, peritonitis |
| DDx: | lobulated/villous adenoma, leiomyosarcoma, metastatic melanoma, intussusception |
P.807
Trichobezoar
[trikho-, thrix, Greek = hair]
80% are < age 30, almost exclusively in females;
| Associated with: | gastric ulcer in 24 70% |
Blue Rubber Bleb Nevus Syndrome
= rare disorder characterized by vascular hamartomas of skin + visceral hemangiomas predominantly afflicting the GI tract (but also liver, spleen, heart, skeletal muscle, lung, kidney, thyroid, eyes, CNS)
Etiology: sporadic/autosomal dominant Path: thin layer of connective tissue + single layer of endothelial cells surrounding blood-filled ectatic vessels red to deep blue soft painless cutaneous lesions evacuating under pressure + slow refilling (commonly present at birth increase in size and number with age)
iron deficiency anemia (due to spontaneous hemorrhage)
 nodular filling defects throughout small bowel
nodular filling defects throughout small bowel
MR:
 hyperintense lesions on T2WI (due to slow flow/thrombosis)
hyperintense lesions on T2WI (due to slow flow/thrombosis)
| Cx: | intussusception, volvulus; pressure erosion of bone, osseous + soft-tissue hypertrophy (secondary to hypervascularity) |
DDx:
Maffucci syndrome (dyschondroplasia + osteochondromas + vascular malformations)
Klippel-Trenaunay-Weber syndrome (port wine stain, vascular malformations, limb hypertrophy)
Kasabach-Merritt syndrome (large vascular malformations + consumptive coagulopathy)
Kaposi sarcoma
Peutz-Jeghers syndrome (congenital polyposis + melanotic cutaneous lesions)
Gardner syndrome (soft-tissue tumors + sebaceous cysts)
Blunt Abdominal Trauma
CT is imaging method of choice for evaluation of stable patients
US imaging in the detection of intraabdominal injury:
86% sensitive, 99% specific, 98% accurate
Hemoperitoneum
| Frequency: | 29 34% of patients with abdominal visceral injury have no hemoperitoneum |
| Location: | paracolic gutters, pelvis |
CT (negative predictive value of 99.6%):
Attenuation values of blood:
during IV contrast administration and assuming an initially normal hematocrit without significant dilution from intraperitoneal fluid (ascites, urine, succus, lavage fluid)
serum (after hematocrit effect) 0 20 HU fresh unclotted blood 30 45 HU clotted blood 60 100 HU active arterial extravasation >180 HU  sentinel clot sign = the highest attenuation value of blood clot marks the anatomic site of visceral injury
sentinel clot sign = the highest attenuation value of blood clot marks the anatomic site of visceral injury high-density active arterial extravasation always surrounded by lower-density hematoma (DDx: extravasated oral contrast is not surrounded by lower-density material)
high-density active arterial extravasation always surrounded by lower-density hematoma (DDx: extravasated oral contrast is not surrounded by lower-density material)
US:
 usually anechoic fluid accumulation in subhepatic space (= Morison pouch) > pouch of Douglas/paravesical space > between bowel loops
usually anechoic fluid accumulation in subhepatic space (= Morison pouch) > pouch of Douglas/paravesical space > between bowel loopsDDx: bowel contents, urine, bile, ascites  hemoperitoneum score = depth of largest fluid collection in cm + 1 point for each additional site with fluid (score of 2 managed conservatively)
hemoperitoneum score = depth of largest fluid collection in cm + 1 point for each additional site with fluid (score of 2 managed conservatively) hyperechoic/occasionally isoechoic masses (= intraperitoneal clot)
hyperechoic/occasionally isoechoic masses (= intraperitoneal clot)
| Prognosis: | 17% of patients without hemoperitoneum require surgical/angiographic intervention |
 Peritoneal lavage cannot quantify amount of hemoperitoneum + results in a 19 39% rate of nontherapeutic surgeries
Peritoneal lavage cannot quantify amount of hemoperitoneum + results in a 19 39% rate of nontherapeutic surgeries
Hypovolemia = Hypoperfusion complex
 collapsed cava sign = persistent flattening of IVC (due to decreased venous return)
collapsed cava sign = persistent flattening of IVC (due to decreased venous return)N.B.: abort CT examination as shock is imminent!  small hypodense spleen (decreased enhancement)
small hypodense spleen (decreased enhancement) small aorta + mesenteric arteries (due to intense vasoconstriction)
small aorta + mesenteric arteries (due to intense vasoconstriction) shock nephrogram = lack of renal contrast excretion
shock nephrogram = lack of renal contrast excretion shock bowel = dilatation of fluid-filled intestines + generalized thickening of small bowel folds + increased enhancement (due to vasoconstriction of mesenteric vessels)
shock bowel = dilatation of fluid-filled intestines + generalized thickening of small bowel folds + increased enhancement (due to vasoconstriction of mesenteric vessels) marked enhancement of adrenal gland
marked enhancement of adrenal gland intense pancreatic enhancement
intense pancreatic enhancement
| Categories of Splenic Injury | ||
|---|---|---|
| Grade | Injury | Description |
| I | hematoma | subcapsular <25% of surface area |
| laceration | capsular tear <1 cm of parenchymal depth | |
| II | hematoma | subcapsular 25-50% of surface area; intraparenchymal <5 cm in diameter |
| laceration | 1-3 cm deep without involvement of trabecular vessel | |
| III | hematoma | subcapsular >50% of surface area; ruptured subcapsular/parenchymal; intraparenchymal >10 cm/expanding |
| laceration | >3 cm parenchymal depth/involvement of trabecular vessels | |
| IV | laceration | involving segmental/hilar vessels with devascularization of >25% |
| V | laceration | completely shattered spleen |
| vascular | total splenic devascularization | |
Blunt Trauma To Spleen
 Most frequently injured intraperitoneal organ in blunt abdominal trauma
Most frequently injured intraperitoneal organ in blunt abdominal trauma
| Associated with: | other solid visceral/bowel injuries (29%); lower rib fractures in 44%, injury to left kidney in 10%, injury to left diaphragm in 2% |
P.808
 20% of left rib fractures have splenic injury!
20% of left rib fractures have splenic injury! 25% of left renal injury have splenic injury!
25% of left renal injury have splenic injury!
| Technique: | scanning delay of 60 70 seconds to avoid heterogeneous splenic enhancement |
CECT (95% accurate):
 CT not reliable to determine need for surgical intervention!
CT not reliable to determine need for surgical intervention! hemoperitoneum (indicates disruption of splenic capsule)
hemoperitoneum (indicates disruption of splenic capsule) sentinel clot (= area of >60 HU adjacent to spleen) sensitive predictor of splenic injury =perisplenic hematoma
sentinel clot (= area of >60 HU adjacent to spleen) sensitive predictor of splenic injury =perisplenic hematoma high-attenuation area (80 370 HU) =active extravasation/pseudoaneurysm:
high-attenuation area (80 370 HU) =active extravasation/pseudoaneurysm:N.B.: active extravasation of contrast material usually requires surgery  mottled parenchymal enhancement =contusion
mottled parenchymal enhancement =contusion hypoattenuating line connecting opposing visceral surfaces = linear parenchymal defect =splenic laceration:
hypoattenuating line connecting opposing visceral surfaces = linear parenchymal defect =splenic laceration: almost always associated with hemoperitoneum
almost always associated with hemoperitoneum
 crescentic region of low attenuation along splenic margin flattening/indenting/compressing the normal parenchyma =subcapsular hematoma
crescentic region of low attenuation along splenic margin flattening/indenting/compressing the normal parenchyma =subcapsular hematoma round hypodense inhomogeneous region hyperdense clot =intrasplenic hematoma
round hypodense inhomogeneous region hyperdense clot =intrasplenic hematoma hypoattenuating hematoma with complete separation of splenic fragments = laceration traversing two capsular surfaces =splenic fracture
hypoattenuating hematoma with complete separation of splenic fragments = laceration traversing two capsular surfaces =splenic fracture multiple lacerations = shattered spleen
multiple lacerations = shattered spleen
US:
 hyperechoic intraparenchymal region (= acute hematoma/laceration)
hyperechoic intraparenchymal region (= acute hematoma/laceration) anechoic intralesional collection (= brisk hemorrhage)
anechoic intralesional collection (= brisk hemorrhage) diffusely heterogeneous parenchymal pattern containing hyper- and hypo-echoic areas (= extensive splenic injury)
diffusely heterogeneous parenchymal pattern containing hyper- and hypo-echoic areas (= extensive splenic injury) loss of normal organ contour (= perisplenic clot)
loss of normal organ contour (= perisplenic clot)
Sequelae:
scar/fibrosis
splenic pseudocyst (20 30 HU)
pseudoaneurysm formation
delayed splenic rupture
= hemorrhage >48 hours after trauma
Cause: subcapsular hematoma Prevalence: 0.3 20% of blunt splenic injuries Time of onset: in 70% within 2 weeks of injury, in 90% within 4 weeks of injury Prognosis: 52% surgery (splenectomy [8%], splenorrhaphy), 48% nonsurgical management Rx: up to 91% of stable patients can be treated conservatively with observation; transcatheter embolization DDx: (1) Normal lobulation/splenic cleft (smoothly contoured, medially located)
(2) Adjacent unopacified jejunum simulating splenic tissue
(3) Early differential enhancement of red and white pulp (scan obtained within 20 50 seconds)
(4) Perisplenic fluid from ascites/urine/succus/bile/lavage
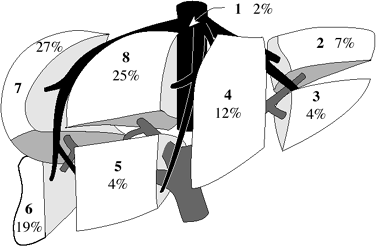 |
| Distribution of Traumatic Hepatic Lesions |
Blunt Trauma To Liver (20%)
 Second most frequently injured intraabdominal viscus
Second most frequently injured intraabdominal viscusAssociated with: splenic injury in 45% clinical manifestation often delayed by days/weeks
| Location: | R > L lobe |
| Site: | perivascular, paralleling right + middle hepatic arteries + posterior branches of right portal vein, avulsion of right hepatic vein from IVC (13%) Left lobe injury more often associated with damage to duodenum, pancreas, transverse colon |
| Categories of Splenic Injury | ||
|---|---|---|
| Grade | Injury | Description |
| I | hematoma | subcapsular <10% of surface area |
| laceration | capsular tear <1 cm of parenchymal depth | |
| II | hematoma | subcapsular 10-50% of surface area; intraparenchymal <10 cm in diameter |
| laceration | 1-3 cm deep and <10 cm long | |
| III | hematoma | subcapsular >50% of surface area; ruptured subcapsular/parenchymal; intraparenchymal >10 cm/expanding |
| laceration | >3 cm parenchymal depth | |
| IV | laceration | parenchymal disruption 25-75% of lobe; 1-3 Couinaud segments in single lobe |
| V | laceration | disruption >75% of single lobe; >3 Couinaud segments in single lobe |
| vascular | juxtahepatic venous injury (HV, IVC) | |
| VI | vascular | hepatic avulsion |
CECT:
 hypoattenuating hematoma:
hypoattenuating hematoma: lenticular configuration (= subcapsular hematoma) usually resolving within 6-8 weeks
lenticular configuration (= subcapsular hematoma) usually resolving within 6-8 weeks irregular linear branching/round regions of low attenuation = laceration
irregular linear branching/round regions of low attenuation = laceration focal/diffuse periportal tracking (in up to 22%) due to dissecting hemorrhage/bile/dilated periportal lymphatics (secondary to elevated central venous pressure/injury to lymphatics)
focal/diffuse periportal tracking (in up to 22%) due to dissecting hemorrhage/bile/dilated periportal lymphatics (secondary to elevated central venous pressure/injury to lymphatics) alteration in distribution of vessels + ducts
alteration in distribution of vessels + ducts
P.809
 hypodense wedge extending to liver surface = focal hepatic devascularization
hypodense wedge extending to liver surface = focal hepatic devascularization focal hyperdense (80-350 HU) area = active hemorrhage/pseudoaneurysm
focal hyperdense (80-350 HU) area = active hemorrhage/pseudoaneurysm hemoperitoneum (inability of liver veins to contract)
hemoperitoneum (inability of liver veins to contract) intrahepatic/subcapsular gas (usually due to necrosis)
intrahepatic/subcapsular gas (usually due to necrosis)
US:
 localized area of increased intraparenchymal echogenicity (= acute hematoma/laceration)
localized area of increased intraparenchymal echogenicity (= acute hematoma/laceration) widespread heterogeneous liver echogenicity + absence of normal vascular pattern (= global parenchymal injury)
widespread heterogeneous liver echogenicity + absence of normal vascular pattern (= global parenchymal injury)
| Cx: | in up to 20% (1) delayed rupture (rare) (2) hemobilia (3) arteriovenous fistula/pseudoaneurysm (4) biloma infection (5) superinfection of hematoma/devascularized hepatic parenchyma |
| Rx: | conservative treatment in up to 80% in adults + 97% in children; transcatheter embolization |
| Healing: | 1-6-15 months |
| DDx: | (1) beam-hardening artifact from adjacent ribs/from air-contrast level in stomach (2) Focal fatty infiltration |
Blunt Trauma to Gallbladder (2%)
| Associated with: | injury to liver, duodenum |
 pericholecystic fluid (extraperitoneal location of GB)
pericholecystic fluid (extraperitoneal location of GB) free intraperitoneal fluid
free intraperitoneal fluid
CECT:
 blurred contour of GB
blurred contour of GB focal thickening/discontinuity of GB wall
focal thickening/discontinuity of GB wall intraluminal enhancing mucosal flap
intraluminal enhancing mucosal flap hyperattenuating blood within GB lumen
hyperattenuating blood within GB lumen mass effect on adjacent duodenum
mass effect on adjacent duodenum collapsed GB = GB rupture
collapsed GB = GB rupture focal periportal tracking = GB rupture
focal periportal tracking = GB rupture
US:
 focal hypoechoic thickening
focal hypoechoic thickening echogenic mass within GB lumen
echogenic mass within GB lumen
Blunt Trauma to GI Tract (5%)
| Cause in children: | MVA (lap belts), bicycle handle bar, child abuse |
| May be associated with: | Chance fracture; traumatic hernia (disruption of the rectus abdominis muscle) |
| Location: | jejunum distal to ligament of Treitz > duodenum > ascending colon at ileocecal valve > descending colon |
abdominal tenderness (100% sensitive)
increased temperature + heart rate
decreased urine output over 24 hours
lap belt ecchymosis
NECT:
 pneumoperitoneum (15 32%):
pneumoperitoneum (15 32%): small gas bubbles anteriorly near liver/trapped within leaves of mesentery (with small bowel perforation)
small gas bubbles anteriorly near liver/trapped within leaves of mesentery (with small bowel perforation) retroperitoneal air (with disruption of duodenum/colon)
retroperitoneal air (with disruption of duodenum/colon) hypodense free fluid (58 85%), particularly in interloop location due to perforation
hypodense free fluid (58 85%), particularly in interloop location due to perforationDDx: parenchymal organ injury/osseous injury/large vessel injury/bladder perforation  sentinel clot sign adjacent to bowel
sentinel clot sign adjacent to bowel
CECT (88 92% sensitive):
 focal discontinuity of bowel wall = direct evidence
focal discontinuity of bowel wall = direct evidence focal bowel wall thickening > 3 mm (= intramural hematoma (75%)/vascular compromise and inflammation due to spilling of bowel contents):
focal bowel wall thickening > 3 mm (= intramural hematoma (75%)/vascular compromise and inflammation due to spilling of bowel contents): intestinal obstruction
intestinal obstruction
 hyperdense contrast enhancement of injured bowel wall = delayed venous transit time (20%)
hyperdense contrast enhancement of injured bowel wall = delayed venous transit time (20%) stranding of mesentery = streaky hyperattenuating infiltration/fluid at mesenteric root (due to hemorrhage + inflammatory response)
stranding of mesentery = streaky hyperattenuating infiltration/fluid at mesenteric root (due to hemorrhage + inflammatory response) mesenteric hematoma (39%)
mesenteric hematoma (39%) extravasation of oral contrast material (uncommon), most dense near perforation
extravasation of oral contrast material (uncommon), most dense near perforationDDx: hyperattenuating blood, extravasating vascular contrast material, leak of contrast material from urinary tract  mesenteric pseudoaneurysm
mesenteric pseudoaneurysm
US:
 nonspecific free fluid (98% sensitive)
nonspecific free fluid (98% sensitive)
| N.B.: | clinical signs + symptoms may be delayed for 24 hours (increasing mortality to 65%) |
Blunt Trauma to Pancreas (3%)
| Mechanism: | compression against vertebral column with shear across pancreatic neck |
| Incidence: | <10% of childhood trauma |
| Cause: | motor vehicle accident, fall onto handle bars of a bicycle, child abuse |
| Associated with: | injury to liver, duodenum |
Classification:
| I | minor contusion/hematoma, capsule + major duct intact |
| II | parenchymal injury without major duct injury |
| III | major ductal injury |
| IV | severe crush injury |
| Location: | junction of body + tail |
 posttraumatic pancreatitis:
posttraumatic pancreatitis: edema/fluid in peripancreatic fat
edema/fluid in peripancreatic fat focal/diffuse pancreatic enlargement
focal/diffuse pancreatic enlargement irregularity of pancreatic contour
irregularity of pancreatic contour
 area of low-attenuation = contusion/laceration (actual site of laceration difficult to visualize)
area of low-attenuation = contusion/laceration (actual site of laceration difficult to visualize) fluid around superior mesenteric artery
fluid around superior mesenteric artery fluid in transverse mesocolon/lesser sac
fluid in transverse mesocolon/lesser sac fluid between pancreas and splenic vein
fluid between pancreas and splenic vein thickening of anterior pararenal fascia
thickening of anterior pararenal fascia
| N.B.: | 24 48-hour delayed scans uncover findings not present earlier |
| Rx: | I + II conservative management; III + IV need surgery within 24 hours |
| Cx: | recurrent pancreatitis, pseudocyst, pseudoaneurysm, fistula, abscess (attendant mortality of 20%) |
P.810
Boerhaave Syndrome
= complete transmural disruption of esophageal wall with extrusion of gastric content into mediastinum/pleural space secondary to food bolus impaction
forceful vomiting with sudden onset of pain (substernal, left chest, in neck, pleuritic, abdominal)
dyspnea
NO hematemesis (blood escapes outside esophageal lumen)
 rent of 2 5 cm in length, 2 3 cm above GE junction, predominantly on left posterolateral wall
rent of 2 5 cm in length, 2 3 cm above GE junction, predominantly on left posterolateral wall pleural effusion on left >> right side/hydropneumothorax
pleural effusion on left >> right side/hydropneumothorax pneumomediastinum (single most important plain-film finding), pneumopericardium, subcutaneous air
pneumomediastinum (single most important plain-film finding), pneumopericardium, subcutaneous air V sign of Naclerio = localized mediastinal emphysema with air between lower thoracic aorta + diaphragm
V sign of Naclerio = localized mediastinal emphysema with air between lower thoracic aorta + diaphragm mediastinal widening
mediastinal widening air-fluid level within mediastinum
air-fluid level within mediastinum extravasation of contrast medium into mediastinum/pleura
extravasation of contrast medium into mediastinum/pleura
Brunner Gland Hyperplasia
= BRUNNER GLAND HAMARTOMA
| Incidence: | 1.2% of all gastric polyps |
| Etiology: | response to increased acid secretion |
| Histo: | diffusely enlarged hyperplastic glands with Swiss cheese appearance |
| Physiology: | secrete a clear viscous alkaline mucus into crypts of Lieberk hn |
MORPHOLOGIC TYPES:
Diffuse nodular hyperplasia
Circumscribed nodular hyperplasia: in suprapapillary portion
Single adenomatous hyperplastic polyp: in duodenal bulb
| Location: | duodenum, prepyloric region (duodenal glands begin in vicinity of pylorus extending distally within proximal 2/3 of duodenum) |
 multiple nodular filling defects (usually limited to 1st portion of duodenum) with cobblestone appearance (most common finding)
multiple nodular filling defects (usually limited to 1st portion of duodenum) with cobblestone appearance (most common finding)DDx: polyposis syndromes, lymphoid hyperplasia, heterotopic gastric mucosa, nodular duodenitis  occasionally single mass up to 5 cm central ulceration
occasionally single mass up to 5 cm central ulcerationDDx: adenomatous polyp, various submucosal tumors Cx: GI bleeding, obstruction, intussusception
Burkitt Lymphoma
= most common type of pediatric non-Hodgkin lymphoma; initially described in a 7-year old Ugandan child in 1958 by Dennis Burkitt, a British surgeon
Etiology: tumor from undifferentiated small noncleaved B-cell derived lymphocytes Path: resemblance to Hodgkin disease Histo: characteristic starry sky pattern fastest growing tumor in humans with a potential doubling time of 24 hours
paraplegia
NO peripheral leukemia
 conspicuous absence of lymph node disease
conspicuous absence of lymph node disease tendency to permeate/destroy bone
tendency to permeate/destroy bone
MR:
 isointense to muscle on T1WI + T2WI
isointense to muscle on T1WI + T2WI intense homogeneous enhancement
intense homogeneous enhancement
| Rx: | dramatic response to chemotherapy |
| Prognosis: | long-term survival in 50% |
Endemic Form of Burkitt Lymphoma
Endemic in areas with malaria:
sub-Saharan Africa, New Guinea (exposure to Plasmodium falciparum has a synergistic effect causing a marked decrease in T-cell surveillance)
Incidence in central Africa:
50 80% of all childhood neoplasms
| Associated with: | Epstein-Barr virus infection in 95% (implicated as a B-cell mitogen in the oncogenesis) |
| Age: | 3 10 years |
@ Mandible (first)/maxilla/facial bones
jaw mass
exophthalmos (orbital extension)
 grossly destructive lesion, spicules of bone growing at right angles
grossly destructive lesion, spicules of bone growing at right angles large soft-tissue mass
large soft-tissue mass
@ Other skeleton (multifocal in 10%)
 reminiscent of Ewing tumor/reticulum cell sarcoma
reminiscent of Ewing tumor/reticulum cell sarcoma lamellated periosteal reaction around major long bones
lamellated periosteal reaction around major long bones
Sporadic Form of Burkitt Lymphoma
= NONENDEMIC FORM OF BURKITT LYMPHOMA
Incidence in Europe + North America:
35 45% of all pediatric NHL; 3% of all childhood tumors
| Age: | 6 15 years |
Epstein-Barr virus genome found in only a minority
@ Abdomen (69%)
tumors of small bowel (Peyer patches of terminal ileum), mesentery
abdominal mass
intestinal obstruction
 usually intraabdominal extranodal involvement with sparing of spleen
usually intraabdominal extranodal involvement with sparing of spleen well-defined sharply marginated homogeneous tumors (75%)
well-defined sharply marginated homogeneous tumors (75%) ascites (13%)
ascites (13%)
@ Genitourinary tract (20%)
ovary, uterus, kidneys, retroperitoneum
 renal masses/diffuse enlargement (5%)
renal masses/diffuse enlargement (5%) hydronephrosis (28%)
hydronephrosis (28%)
@ Chest
 pleural effusion (most common chest abnormality)
pleural effusion (most common chest abnormality)
@ CNS
 meningeal infiltration (most commonly)
meningeal infiltration (most commonly) cavernous sinus invasion
cavernous sinus invasion supra- and parasellar tumor
supra- and parasellar tumor epidural spinal mass spinal cord compression
epidural spinal mass spinal cord compression
@ Others
salivary glands, thyroid, bone marrow
P.811
Carcinoid
= most common primary tumor of small bowel + appendix (>95% of all carcinoids); belongs to APUDomas (like pheochromocytoma, medullary carcinoma of thyroid, islet cell tumors of pancreas)
| Age: | 5th 6th decade; M:F = 2:1 |
| Path: | firm yellow submucosal nodule arising from argentophil Kulchitsky cells in the crypts of Lieberk hn (= argentaffinoma due to affinity for silver stain); invasion into mesentery incites an intense fibrotic reaction |
| Histo: | low-grade malignancy = resemble adeno-carcinomas but do not have their aggressive behavior; malignant through invasion of muscularis |
Biochemistry:
tumor elaborates (1) ACTH, (2) histamine, (3) bradykinin (4) kallikrein, (5) prostaglandin, (6) serotonin = 5-hydroxytryptamine (from tryptophan over 5-hydroxytryptophan), which is metabolized in liver by monamine oxidase into 5-hydroxyindole acetic acid (5-HIAA) and excreted in urine; 5-hydroxytryptophan is destroyed in pulmonary circulation
| Associated with: | other synchronous/metachronous malignancies (36% at necropsy); neurofibromatosis type 1 |
asymptomatic (66%)
abdominal pain/obstruction (19%)
nausea, weight loss (16%)
palpable mass (14%)
GI bleeding
Carcinoid syndrome (in 7% of small bowel carcinoids):
= constellation of clinical findings related to hormone secretion by tumor
Cause: excess serotonin levels when the metabolic pathway to 5-HIAA (in liver) is bypassed
(a) with liver metastases
(b) with primary pulmonary/ovarian carcinoidsrecurrent diarrhea (70%)
right-sided endocardial fibroelastosis (35%) resulting in tricuspid regurgitation + pulmonary valve stenosis + right heart failure
attacks precipitated by ingestion of food/alcohol
asthmatic wheezing from bronchospasm (15%)
desquamative skin lesions (5%)
pellagra (7%) from niacin deficiency as a result of preferential conversion of dietary tryptophan to serotonin rather than niacin
multiple telangiectasias (25%)
nausea & vomiting, fever
hypotension (vasomotor instability)
cutaneous facial flushing (rare)
excess 5-HIAA in urine
| Prognosis: | carcinoid syndrome has a higher morbidity & mortality than does the tumor itself! |
| RULE OF 1/3: | 1/3 occur in small bowel 1/3 have metastases 1/3 are multiple 1/3 have a second malignancy |
Metastases:
to mesenteric lymph nodes, liver (in 90% of patients with carcinoid syndrome), lung, bone (osteoblastic), peritoneum
incidence versus tumor size
tumor of <1 cm (in 75%) metastasizes in 2% tumor of 1 2 cm (in 20%) metastasizes in 50% tumor of >2 cm (in 5%) metastasizes in 85% incidence versus location
tumor in ileum (in 28%) metastasizes in 35% tumor in appendix (in 46%) metastasizes in 3% tumor in rectum (in 17%) metastasizes in 1%
| Liver metastases seen: | best/ | (only) on: |
| (a) NECT | 35% | (3%) |
| (b) CECT in HAP | 35% | (14%) |
| (c) CECT in PVP | 30% | (3%) |
HAP = hepatic arterial-dominant phase of triple phase CT
PVP = portal venous-dominant phase of triple phase CT
| Location: | between gastric cardia and anus (85% in GI tract; 15% in lungs + bronchi) |
@ Appendix (30 45%)
Commonly benign: slow growth, rarely metastasizing Incidence at surgery: 0.03 0.7% Site: tip (70%), middle (20%), base (10%) of appendix symptoms of appendicitis
 invasion of mesoappendix (11%)
invasion of mesoappendix (11%)
@ Small bowel (25 35%)
Incidence: 25% of all small bowel tumors Location: ileum (91%); jejunum (7%), duodenum (2%); multiple in 15 29 41%  75% of patients with symptomatic spread have midgut carcinoids
75% of patients with symptomatic spread have midgut carcinoids 30% have a second primary malignancy of GI tract
30% have a second primary malignancy of GI tract Duodenal carcinoids are associated with multiple endocrine neoplasia
Duodenal carcinoids are associated with multiple endocrine neoplasia Periampullary carcinoids are associated with neurofibromatosis type 1 + often contain somatostatin-producing cells
Periampullary carcinoids are associated with neurofibromatosis type 1 + often contain somatostatin-producing cells
@ Rectum (10 15%): metastasize in 10%
@ Colon (5%): ascending colon, often malignant
@ Stomach (<3%): lesser curvature of distal antrum
 one/more 1 4-cm submucosal masses:
one/more 1 4-cm submucosal masses: bull's eye appearance when ulcerated
bull's eye appearance when ulcerated
 one/more sessile/pedunculated polyps
one/more sessile/pedunculated polyps
@ Other organs (5%): bronchus, thyroid, pancreas, biliary tract, teratomas (ovarian, sacrococcygeal, testicular)
@ may be multicentric
UGI:
 small smooth submucosal mass (usually <2 cm) impinging eccentrically on lumen
small smooth submucosal mass (usually <2 cm) impinging eccentrically on lumen desmoplastic response of mesentery from locally high levels of serotonin causes:
desmoplastic response of mesentery from locally high levels of serotonin causes: angulation + kinking of loops leading to obstruction (DIAGNOSTIC)
angulation + kinking of loops leading to obstruction (DIAGNOSTIC) spiculated/tethered appearance of mucosal folds
spiculated/tethered appearance of mucosal folds matting of multiple loops
matting of multiple loops
 separation of loops due to large mesenteric metastases
separation of loops due to large mesenteric metastases
CT:
 submucosal vascular lesion (dual-phase imaging with water as oral contrast)
submucosal vascular lesion (dual-phase imaging with water as oral contrast) focal calcified mesenteric mass surrounded by thickened mesentery:
focal calcified mesenteric mass surrounded by thickened mesentery: stellate radiating pattern + beading of mesenteric neurovascular bundles (desmoplastic reaction)
stellate radiating pattern + beading of mesenteric neurovascular bundles (desmoplastic reaction) retraction + shortening of mesentery
retraction + shortening of mesentery displacement + kinking + separation of adjacent bowel loops
displacement + kinking + separation of adjacent bowel loops segmental thickening of adjacent bowel loops (encasement of mesenteric vessels leads to chronic ischemia)
segmental thickening of adjacent bowel loops (encasement of mesenteric vessels leads to chronic ischemia)
P.812
 low-density lymphadenopathy (due to necrosis)
low-density lymphadenopathy (due to necrosis) characteristically hyperattenuating liver metastases in early arterial phase
characteristically hyperattenuating liver metastases in early arterial phase may become isodense after slow contrast infusion/in portal-venous phase
may become isodense after slow contrast infusion/in portal-venous phase
Angio:
 sunburst appearance:
sunburst appearance: kinking of small- and medium-sized vessels with a stellate configuration
kinking of small- and medium-sized vessels with a stellate configuration simulated hypervascularity with thickening + foreshortening of mesenteric vessels secondary to fibrotic retraction
simulated hypervascularity with thickening + foreshortening of mesenteric vessels secondary to fibrotic retraction
 mesenteric ischemia:
mesenteric ischemia: arterial branch stenoses from encasement of mediumsized vessels (due to elastic vascular sclerosis with locally elevated serotonin levels)
arterial branch stenoses from encasement of mediumsized vessels (due to elastic vascular sclerosis with locally elevated serotonin levels) venous occlusion/mesenteric varices
venous occlusion/mesenteric varices
 tumor may be identified as hypervascular mass
tumor may be identified as hypervascular mass
NUC (I-123 MIBG imaging):
 uptake in 44-63% (higher frequency of radiotracer uptake in midgut carcinoids + with elevated serotonin levels)
uptake in 44-63% (higher frequency of radiotracer uptake in midgut carcinoids + with elevated serotonin levels)
US:
 persistent fluid-distended appendix without typical signs of appendicitis
persistent fluid-distended appendix without typical signs of appendicitis
| Prognosis: | slow progression with average survival time of 3.2 years after diagnosis of liver metastases; 5-year survival of 65% for localized disease + 36% for distant metastatic disease |
| Rx: | resection; somatostatin/SMS 201-995; chemoembolization of hepatic arteries |
| DDx: | oat-cell carcinoma, pancreatic carcinoma, medullary thyroid carcinoma, retractile mesenteritis, desmoplastic carcinoma/lymphoma |
Cathartic Colon
= prolonged use of stimulant-irritant cathartics (>15 years) resulting in neuromuscular incoordination from chronically increased muscular activity + tonus
Agents: castor oil, senna, phenolphthalein, cascara, podophyllum, aloin Location: involvement of colon proximal to splenic flexure  effaced mucosa with flattened smooth surface
effaced mucosa with flattened smooth surface diminished/absent haustrations
diminished/absent haustrations pseudostrictures = smoothly tapered areas of narrowing are typical (sustained tonus of circular muscles)
pseudostrictures = smoothly tapered areas of narrowing are typical (sustained tonus of circular muscles) poor evacuation of barium
poor evacuation of barium flattened + gaping ileocecal valve
flattened + gaping ileocecal valve shortened but distensible ascending colon
shortened but distensible ascending colon
| DDx: | burned-out ulcerative colitis with right-sided predominance (very similar) |
Chagas Disease
[Carlos Chagas (1879-1934), physician in Rio de Janeiro, Brazil]
= damage of ganglion cells by neurotoxin liberated from protozoa Trypanosoma cruzi resulting in aperistalsis of GI tract + dilatation
Endemic to Central + South America (esp. eastern Brazil)
| Histo: | decreased number of cells in medullary dorsal motor nucleus + Wallerian degeneration of vagus + decrease/loss of argyrophilic cells in myenteric plexus of Auerbach |
| Peak age: | 30 50 years; M:F = 1:1 |
intermittent/persistent dysphagia
odynophagia (= fear of swallowing)
foul breath, regurgitation, aspiration
Mecholyl test: abnormal response indicative of deficient innervation; 2.5 10 mg methacholine subcutaneously followed by severe tetanic nonperistaltic contraction 2 5 minutes after injection, commonly in distal half of esophagus, accompanied by severe pain
@ Dilatative cardiomyopathy (myocarditis)
@ Megacolon (bowels move at intervals of 8 days to 5 months)
Cx: impacted feces, sigmoid volvulus @ Esophagus: changes as in achalasia
Chalasia
= continuously relaxed sphincter with free reflux in the absence of a sliding hernia
Etiology: elevated submerged segment
Causes:
Delayed development of esophagogastric region in newborns
Scleroderma, Raynaud disease
S/P forceful dilatation/myotomy for achalasia
 free/easily induced reflux
free/easily induced reflux
Colitis Cystica Profunda
= rare benign condition characterized by submucosal mucus-containing cysts lined by normal colonic epithelium
Etiology: probably related to chronic inflammation Associated with: solitary rectal ulcer syndrome (in localized form) Age: primarily disease of young adults brief periods of bright red rectal bleeding
mucous/bloody discharge
intermittent diarrhea
Location:
(a) localized to rectum (most commonly)/sigmoid
(b) generalized colonic process (less common)
 nodular polypoid/cauliflower-like lesions <2 cm in size, containing no gas
nodular polypoid/cauliflower-like lesions <2 cm in size, containing no gas spiculations mimicking ulcers (barium-filled clefts between nodules)
spiculations mimicking ulcers (barium-filled clefts between nodules)
| DDx: | pneumatosis (rarely affects rectum) |
Colonic Atresia
| Incidence: | less common than ileal atresia |
Plain radiograph:
 massive dilatation of colon proximal to obstruction
massive dilatation of colon proximal to obstruction mottled pattern of gas + feces proximal to point of atresia
mottled pattern of gas + feces proximal to point of atresia
| DDx: | often indistinguishable from obstruction of distal ileum |
BE:
 functional microcolon
functional microcolon obstruction to retrograde flow of barium
obstruction to retrograde flow of barium
P.813
US:
 dilated hyperechoic distal small bowel + proximal colon (from retained meconium)
dilated hyperechoic distal small bowel + proximal colon (from retained meconium)
Colorectal Carcinoma
Most common cancer of GI tract; 3rd most commonly diagnosed malignancy in developed countries in men (after lung + prostate cancer) and women (after lung + breast cancer); 2nd leading cause of cancer deaths
| Incidence: | 11% of all newly diagnosed cancers; 13% of all cancer deaths; 150,000 new cases/year with 57,000 deaths in United States (1999); 6% lifetime probability of any White person to develop colorectal cancer; 3:100,000 in 30 34-year-olds; 532:100,000 for >85-year-olds |
| Lifetime probability: | 4% |
Risk factors:
Personal history of colonic adenoma/carcinoma
malignancy in 5% of tubular adenomas
malignancy in 30 40% of villous adenomas
Proof of adenoma-carcinoma sequence:
frequent coexistence of adenoma + carcinoma
similar distribution within colon
consistent proportional prevalence in population having varied magnitudes of colon cancer risk
increased frequency of carcinoma in patients with adenomas
reduction of cancer incidence following endoscopic removal of polyps
all patients with familial adenomatous polyposis syndrome develop colon carcinoma if colon not removed
similarity of DNA + chromosomal constitution
 93% of colorectal carcinomas arise from adenomatous polyp!
93% of colorectal carcinomas arise from adenomatous polyp! A patient with one adenoma has a 9% chance of having a colorectal carcinoma in next 15 years!
A patient with one adenoma has a 9% chance of having a colorectal carcinoma in next 15 years! It takes about 7 years for a 1-cm adenoma to become an invasive cancer!
It takes about 7 years for a 1-cm adenoma to become an invasive cancer! 5% of adenomas 5 mm in size develop into invasive cancers (5 mm is considered critical mass of intraepithelial neoplasia)!
5% of adenomas 5 mm in size develop into invasive cancers (5 mm is considered critical mass of intraepithelial neoplasia)!
Family history of benign/malignant colorectal tumors in first-degree relatives (3 5 risk)
Personal history of ovarian/endometrial/breast cancer
Dysplasia of colon within flat mucosa
Inflammatory bowel disease:
Ulcerative colitis (3 5% incidence; cumulative incidence of 26% after 25 years of colitic symptoms)
Crohn disease affecting the colon + rectum (particularly in bypassed loops/in vicinity of chronic fistula)
Time delay: >8 10 years of colitis Underlying lesion: dysplasia within flat mucosa Prominent lymphoid follicular pattern
Pelvic irradiation
Ureterosigmoidostomy
Environmental risk factors:
low fiber diet: prevents rapid transit time thus increasing contact time between potential toxins and colonic mucosa
increased ingestion of fat + animal protein
obesity
asbestos worker
Genetic risk factors (6% of colorectal carcinomas):
familial adenomatous polyposis syndrome: familial polyposis, Gardner syndrome, Turcot syndrome
Age: approximately at 40 years certain hamartomatous polyposis syndromes:Peutz-Jeghers syndrome, juvenile polyposis, Cowden disease
hereditary nonpolyposis colon cancer syndrome
= Lynch syndrome (see below)
Screening recommendations (American Cancer Society):
as/more effective than mammographic screening
(a) for persons >50 years of age: annual fecal occult-blood test + sigmoidoscopy/BE every 3 5 years
(b) for first-degree relatives of patients with colon cancer screening should start at age 40
| Age: | median age of 71 years for colon cancer; median age of 69 years for rectal cancer; M:F = 3:2 |
Histo:
Adenocarcinoma with varied degrees of differentiation
Mucinous carcinoma (uncommon)
Squamous cell carcinoma + adenoacanthoma (rare)
Metastases (lymphatic/hematogenous venous):
Liver (75%; 15 20% at time of surgery) due to portal venous drainage route
Mesentery + mesenteric nodes (10 15%)
Adrenal (10 14%)
Lung (5 50%)
Ovary (3 8%) = Krukenberg tumor
Psoas muscle tumor deposit
Peritoneal metastases:
malignant ascites: usually associated with poorly differentiated colonic carcinoma
pseudomyxoma peritonei (<5%): low-grade colonic adenocarcinoma
Bone (5%)
Brain (5%)
 Because of absence of lymphatics in lamina propria colon cancer will not metastasize until it penetrates the muscularis mucosa!
Because of absence of lymphatics in lamina propria colon cancer will not metastasize until it penetrates the muscularis mucosa!
rectal bleeding, iron deficiency anemia
change in bowel habits/caliber of stools
obstruction (poor prognostic indicator)
hydronephrosis (13%)
positive fecal occult blood testing (2 6% positive-result rate; 5 10% positive predictive value; fails to detect 30 50% of colorectal carcinomas + up to 75% of adenomas):
Hemoccult (hematein), HemoQuant (porphyrins), Haemselect (hemoglobin)
progressive elevation of carcinoembryonic antigen (CEA) >10 g/L indicative of recurrent/metastatic disease
watery diarrhea + potassium depletion/excessive secretion of mucus + hypoalbuminemia (in large mucin-secreting villous tumor)
| Location: | aging gut = number of right-sided lesions increasing with age ( changing distribution ) |
P.814
left colon (52 61%):
rectum (15 33 41%), sigmoid (20 37%), descending colon (10 11%)
 commonly annular strictures with obstruction
commonly annular strictures with obstruction
right colon:
transverse colon (12%), ascending colon (8 16%), cecum (8 10%)
 commonly polypoid lesions with chronic bleeding + intussusception
commonly polypoid lesions with chronic bleeding + intussusception
| Colonoscopy: | cecum not visualized in 10 36%; fails to detect 12% of colonic polyps (10% in areas never reached by colonoscope) |
| Cx: | perforation in 0.2% (0.02% for BE); death in 1:5,000 (1:50,000 for BE) |
BE (sensitivities in detection of polyps >1 cm: SCBE 77 94%, DCBE 82 97%; for polyps <1 cm: SCBE 18 72%, DCBE 61 83%):
 fungating polypoid carcinoma:
fungating polypoid carcinoma:chronic bleeding, intussusception
 annular ulcerating carcinoma = apple core lesion
annular ulcerating carcinoma = apple core lesion = annular constriction is a result of tumor growing along the lymphatic channels, which parallel the circular muscle fibers of the inner layer of the muscularis propria; longitudinal growth is limited with abrupt transition to normal mucosa
colonic obstruction
 saddle lesion = growth characteristics between polypoid mass + annular constricting lesion
saddle lesion = growth characteristics between polypoid mass + annular constricting lesion scirrhous carcinoma (signet-ring type)
scirrhous carcinoma (signet-ring type)= long-segment stricture without significant mucosal abnormality similar to linitis plastica due to diffuse circumferential + longitudinal tumor infiltration within the loose submucosal tissue between muscularis mucosa + muscularis propria
often seen in ulcerative colitis
 curvilinear/mottled calcifications (rare) are CHARACTERISTIC of mucinous adenocarcinoma
curvilinear/mottled calcifications (rare) are CHARACTERISTIC of mucinous adenocarcinoma
CT (48 90% staging accuracy, 25 73% for lymph node metastases):
CT staging (poor accuracy compared with Astler-Coller classification):
Stage 1 intramural polypoid mass Stage 2 thickening of bowel wall Stage 3 slight invasion of surrounding tissues Stage 4 massive invasion of surrounding tissue + adjacent organs/distant metastases Staging of colorectal cancer
(modified Dukes = Astler-Coller classification):Stage Findings A limited to mucosa B involvement of muscularis propria B1 extension into muscularis propria B2 extension through muscularis propria into serosa/mesenteric fat (35%) C lymph node metastases (50%) C1 + growth limited to bowel wall C2 + growth extending into adipose tissue D distant metastases Staging of Colorectal Cancer
(UICC-AJCC Colorectal Cancer Staging System)Stage Grouping 5-year Survival 0 Tis N0 M0 >95% I T1 N0 M0 75-100% T2 N0 M0 II T3 N0 M0 50-75% T4 N0 M0 III any T N1 M0 30-50% any T N2,3 M0 IV any T any N M1 <10% Legend: Tis carcinoma in situ T1 invasion of submucosa T2 invasion of muscularis propria T3 invasion of subserosa/pericolic tissue T4 invasion of visceral peritoneum/other organs N1 1 3 pericolic Lnn N2 >4 pericolic Lnn N3 any Lnn along course of a vascular trunk  low-density mass + low-density lymph nodes in mucinous adenocarcinoma (= >50% of tumor composed of extracellular mucin)
low-density mass + low-density lymph nodes in mucinous adenocarcinoma (= >50% of tumor composed of extracellular mucin) psammomatous calcifications in mucinous adenocarcinoma
psammomatous calcifications in mucinous adenocarcinoma signs of Lnn involvement: single lymph node >1 cm in diameter/cluster of 3 nodes <1 cm/node of any size within mesentery
signs of Lnn involvement: single lymph node >1 cm in diameter/cluster of 3 nodes <1 cm/node of any size within mesentery
MR (staging accuracy of 73%, 40% sensitivity for lymph node metastases)
Prognosis:
Survival rate of 40 50% overall in 5 years (unchanged over past 40 years); 80 90% with Duke A; 70% with Duke B; 33% with Duke C; 5% with Duke D
Recurrence in 1/3 of patients:
local recurrence at line of anastomosis (60%) within 1 year after resection in 50%, within 2 years after resection in 70 80%
distant metastases (26%)
local recurrence + metastases (14%)
Risk after detection of colon cancer:
5% for synchronous colon cancer 14% for synchronous cancer with sentinel polyp 35% for additional adenomatous polyp 3% for metachronous colon cancer 4% for extracolonic malignancy
| Cx: | (1) Obstruction (frequently in descending + sigmoid colon) (2) Perforation (3) Intussusception (4) Abscess formation (5) Fistula formation (6) Pneumatosis cystoides intestinalis (7) Pseudomyxoma peritonei (from low-grade adenocarcinoma of colon) |
| Rx: | (1) Local surgical excision/polypectomy for stage I disease (2) Right/left hemicolectomy with eventual anastomosis of proximal + distal excision sites (3) Low anterior resection: >2 cm of rectum must remain to anastomose the colon (4) Abdominoperineal resection with colostomy for low rectal carcinoma (5) Adjuvant chemotherapy for stage II disease (fluorouracil/levamisole) |
| DDx: | (1) Prolapsing ileocecal valve (change on palpation) (2) Spasm (intact mucosa, released by propantheline bromide) (3) Diverticulitis |
P.815
Lynch Syndrome
= HEREDITARY NONPOLYPOSIS COLORECTAL CANCER SYNDROME
= families with high incidence of colorectal cancers + increased incidence of synchronous and metachronous colorectal cancers
Amsterdam criteria:
3 family members of whom 2 are 1st degree relatives of the third
family members in 2 generations
one family member diagnosed <50 years of age
| Lynch I | = no associated extracolonic cancer |
| Lynch II | = associated with extracolonic malignancy: transitional cell carcinoma of ureter + renal pelvis; adenocarcinoma of endometrium, stomach, small bowel, pancreas, biliary tract, brain; hematologic malignancy; carcinoma of skin + larynx |
| Etiology: | autosomal dominant abnormality of chromosome 2 with defect in DNA replication-repair process (a) accelerated adenoma-carcinoma sequence (b) dysplasia in flat mucosa of colon |
| Prevalence: | 5-10% of patients with colon cancer; 5 more common than familial adenomatous polyposis syndrome |
| Mean age: | 45 years |
| Location: | 70% proximal to splenic flexure |
| Prognosis: | better stage for stage than in other cancers (5-year survival rate of 65% versus 44% in sporadic cases) |
| Surveillance: | colonoscopy every 1-2 years from ages 22-35 years |
| Pathologic staging of rectal cancer | |||
|---|---|---|---|
| Astler-Coller/TNM | Description | 5-year Survival | |
| A | T1,N0,M0 | limited to submucosa | 80% |
| B1 | T2,N0,M0 | limited to muscularis propria | 70% |
| B2 | T3,N0,M0 | transmural extension | 60-65% |
| C1 | T2,N1,M0 | nodes (+), into muscularis | 35-45% |
| C2 | T3,N1,M0 | nodes (+), transmural | 25% |
| T4 | invasion of adjacent organs | ||
| D | M1 | distant metastasis | <25% |
Rectal Cancer
| Incidence: | 45,000 rectal cancers/year in United States |
Hematogenous metastasis:
dual venous drainage into portal + systemic veins
 may have lung without liver metastases
may have lung without liver metastases
Risk of recurrence:
| 5% | for T1 | |
| 10% | for T2 | 33% for T1, N1 + T2N1 |
| 25% | for T3 | 66% for T3N1 |
| 50% | for T4 |
Staging accuracy:
Digital rectal examination: 68-75-83%; limited to lesions within 10 cm of anal verge
CT: 48-72-92%, better for more extensive regional spread; 25-73% for lymph node involvement
MR: 74-84-93% with tendency for overstaging
Transrectal ultrasound: 64-77-94% with tendency for overstaging; limited to lesions <14 cm from anal verge + nonstenotic lesions; 50-83% sensitivity for lymph node involvement
Transrectal US (81% accuracy):
Normal layers:
hyperechoic interface of balloon + mucosa
hypoechoic mucosa + muscularis mucosa
hyperechoic submucosa
hypoechoic muscularis propria
hyperechoic serosa
 hypoechoic mass disrupting rectal wall:
hypoechoic mass disrupting rectal wall: no interruption of hyperechoic submucosa = tumor confined to mucosa + submucosa
no interruption of hyperechoic submucosa = tumor confined to mucosa + submucosa no interruption of hyperechoic serosa = tumor confined to rectal wall
no interruption of hyperechoic serosa = tumor confined to rectal wall break in outermost hyperechoic layer = tumor penetrates into perirectal fat
break in outermost hyperechoic layer = tumor penetrates into perirectal fat irregular serrated outer border of muscularis propria (pseudopodia through serosa)
irregular serrated outer border of muscularis propria (pseudopodia through serosa)
 hypoechoic perirectal lymph nodes (= tumor involvement)
hypoechoic perirectal lymph nodes (= tumor involvement)
Colonic Volvulus
= most common form of volvulus
| Incidence: | 10% of large-bowel obstruction |
Cecal Volvulus
= VOLVULUS OF CECUM
| Incidence: | 40% of colonic volvulus |
| Cause: | sudden distension by trauma, pressure, constipation, distal colonic obstruction |
| Associated with: | malrotation + long mesentery resulting in poor fixation of right colon (10-25% of population) |
Pathophysiology of vascular compromise:
Acute mesenteric torsion + strangulation causes arterial + venous obstruction
Gradual distension + increase in intraluminal pressure interferes with blood supply; perforation in 65%
| Age peak: | 20 40 years; M > F |
 cecal gaseous distension:
cecal gaseous distension: cecum rotates anterior to ascending colon =cecal bascule [French = seesaw] (type I cecal volvulus)
cecum rotates anterior to ascending colon =cecal bascule [French = seesaw] (type I cecal volvulus) kidney-shaped distended cecum rotates into left upper quadrant (type II cecal volvulus)
kidney-shaped distended cecum rotates into left upper quadrant (type II cecal volvulus)
 tapered end of barium column points toward torsion
tapered end of barium column points toward torsion
| Cx: | (1) cecal distension >10 12 cm means risk of bowel perforation/infarction (2) Abdominal compartment syndrome= increase in abdominal pressure diminishes respiratory function + cardiac output |
P.816
Sigmoid Volvulus
= VOLVULUS OF SIGMOID
| Cause: | sigmoid twists on mesenteric axis |
| Age: | usually in elderly/psychiatrically disturbed |
| Degree of torsion: | 360 (50%), 180 (35%), 540 (10%) |
 greatly distended paralyzed loop with fluid-fluid levels, mainly on left side, extending toward diaphragm (erect film)
greatly distended paralyzed loop with fluid-fluid levels, mainly on left side, extending toward diaphragm (erect film) coffee-bean sign = distinct midline crease corresponding to mesenteric root in largely gas-distended loop (supine)
coffee-bean sign = distinct midline crease corresponding to mesenteric root in largely gas-distended loop (supine) bird-of-prey sign = tapered hooklike end of barium column
bird-of-prey sign = tapered hooklike end of barium column
CT:
 whirl sign = tightly torsioned mesentery formed by twisted afferent + efferent loop
whirl sign = tightly torsioned mesentery formed by twisted afferent + efferent loop
Congenital Esophageal Atresia & Tracheoesophageal Fistula
= complex of congenital anomalies characterized by failed/incomplete formation of the tubular esophagus or an abnormal communication between esophagus + trachea
| Cause: | developmental disorder in formation and separation of primitive foregut into trachea + esophagus/vascular compromise |
Embryology:
primitive foregut tube develops lateral wall folds that may incompletely connect at any point leaving a fistulous communication; occurs at 3rd 5th week of intrauterine life
| Incidence: | 1:2,000 4,000 livebirths; most common sporadic congenital anomaly diagnosed in childhood |
| Risk of recurrence in sibling: | 1% |
Associated anomalies (17 56 70%):
Gastrointestinal (20 25%): imperforate anus, pyloric stenosis, duodenal atresia, annular pancreas
Cardiac (15 39%): patent ductus arteriosus, ASD, VSD, right-sided aortic arch (5%)
Musculoskeletal (24%): radial ray hypoplasia, vertebral anomalies
Genitourinary (12%): unilateral renal agenesis
Chromosomal (3 19%): trisomy 18, 21, 13
 Trisomy 18 is present in 75 100% of fetuses + in 3 4% of neonates with esophageal atresia!
Trisomy 18 is present in 75 100% of fetuses + in 3 4% of neonates with esophageal atresia!
| mnemonic: | ARTICLES |
Anal atresia
Renal anomalies
TE fistula
Intestinal atresia/malrotation
Cardiac anomaly (PDA, VSD)
Limb anomalies (radial ray hypoplasia, polydactyly)
Esophageal atresia
Spinal anomalies
| mnemonic: | VACTERL |
Vertebral anomalies
Anorectal anomaly
Cardiovascular anomalies
Tracheo-
Esophageal fistula
Renal anomalies
Limb anomalies
drooling from excessive accumulation of pharyngeal secretions (esophageal atresia = EA)
obligatory regurgitation of ingested fluids (EA)
aspiration with coughing + choking during feeding (TEF)
recurrent pneumonia + progressive respiratory distress of variable severity (tracheoesophageal fistula = TEF) in neonate
| Location: | between upper 1/3 + lower 1/3 of esophagus just above carina |
@ Mediastinum
 coiled tube = inability to pass feeding tube into stomach (esophageal atresia)
coiled tube = inability to pass feeding tube into stomach (esophageal atresia) retrotracheal air-distended pouch of proximal esophagus causing compression/displacement of trachea
retrotracheal air-distended pouch of proximal esophagus causing compression/displacement of trachea non-/hypoperistaltic esophageal segment (6 15 cm) in midesophagus
non-/hypoperistaltic esophageal segment (6 15 cm) in midesophagus food impaction
food impaction
@ Abdomen
 gasless abdomen (esophageal atresia proximal TE fistula = types A + B)
gasless abdomen (esophageal atresia proximal TE fistula = types A + B) abdomen distended by bowel gas in 90% (distal TE fistula/H-type fistula = types C + D)
abdomen distended by bowel gas in 90% (distal TE fistula/H-type fistula = types C + D)
@ Chest
 bronchopneumonia with patchy airspace opacity, esp. in dependent upper lobes (in 50%)
bronchopneumonia with patchy airspace opacity, esp. in dependent upper lobes (in 50%)
OB-US (anomalies not identified before 24 weeks GA):
 polyhydramnios in 33 60%:
polyhydramnios in 33 60%: TE-fistula with esophageal atresia is cause of polyhydramnios in only 3%!
TE-fistula with esophageal atresia is cause of polyhydramnios in only 3%!
 absence of fluid-distended stomach (in 10 41%; in remaining cases TE-fistula/gastric secretions allow some gastric distension)
absence of fluid-distended stomach (in 10 41%; in remaining cases TE-fistula/gastric secretions allow some gastric distension) reduced intraluminal fluid in fetal gut
reduced intraluminal fluid in fetal gut small abdomen (birth weight <10th percentile in 40%)
small abdomen (birth weight <10th percentile in 40%) distended proximal pouch of atretic esophagus
distended proximal pouch of atretic esophagus
Cx after repair:
Anastomotic leak
Recurrent TE fistula
Aspiration pneumonia secondary to
esophageal stricture
disordered esophageal motility distal to TE fistula
gastroesophageal reflux
| DDx: | pharyngeal pseudodiverticulum (traumatic perforation of posterior pharynx from finger insertion into oropharynx during delivery/tube insertion) |
Esophageal Atresia without Fistula = Type A
| Frequency: | 8 10% |
Associated anomalies in 17% (mostly Down syndrome + other atresias of GI tract)
Esophageal Atresia with Fistula
Associated anomalies in 30% (mostly cardiovascular)
| Type B | = esophageal atresia + proximal TE fistula |
| Frequency: | 0.9 1% |
| Type C | = esophageal atresia + distal TE fistula |
| Frequency: | 53 86% |
| Type D | = esophageal atresia + proximal and distal TE fistula |
| Frequency: | 1 2.1% |
P.817
Tracheoesophageal Fistula without Atresia
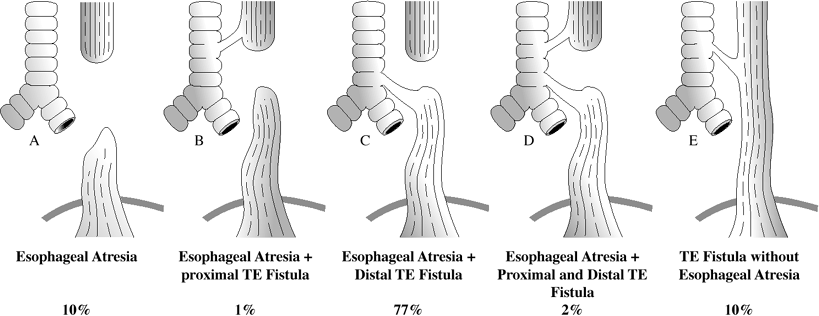 |
| Esophageal Atresia With Tracheo-esophageal Fistula |
= H-shaped fistula =Type E
| Frequency: | 6 10% |
Associated anomalies in 23% (mostly cardiovascular)
feeding difficulties with choking
diagnosis may not be made for several years
 fistula courses forward and upward from esophagus
fistula courses forward and upward from esophagus
| mnemonic: | NO PD, P+D No | ||
| type A | =esophageal atresia | NO fistula | = 10% |
| type B | = esophageal atresia | Prox fistula | = 1% |
| type C | = esophageal atresia | Dist fistula | = 80% |
| type D | = esophageal atresia | Prox + Dist | = 1% |
| type E | = H-type fistula | NO atresia | = 10% |
Congenital Intestinal Atresia
| Incidence: | 1:300 livebirths |
| Cause: | usually sporadic vascular accidents (primary/secondary to volvulus or gastroschisis) |
| Location: | jejunum + ileum (70%), duodenum (25%), colon (5%); may involve multiple sites |
 triple bubble sign = intraluminal gas in stomach + duodenal bulb + proximal jejunum as pathognomonic sign for jejunal atresia
triple bubble sign = intraluminal gas in stomach + duodenal bulb + proximal jejunum as pathognomonic sign for jejunal atresia bulbous bowel segment sign = dilated loop of bowel just proximal to site of atresia (due to prolonged impaction of intestinal contents) with curvilinear termination
bulbous bowel segment sign = dilated loop of bowel just proximal to site of atresia (due to prolonged impaction of intestinal contents) with curvilinear termination gasless lower abdomen (gut usually air-filled by 4 hours after birth)
gasless lower abdomen (gut usually air-filled by 4 hours after birth) meconium peritonitis (6%)
meconium peritonitis (6%) polyhydramnios (in 50% with duodenal/proximal jejunal atresia; rarely in ileal/colonic atresia)
polyhydramnios (in 50% with duodenal/proximal jejunal atresia; rarely in ileal/colonic atresia)
| Prognosis: | 88% survival for isolated atresia |
Cricopharyngeal Achalasia
= hypertrophy of cricopharyngeus muscle (= upper esophageal sphincter) with failure of complete relaxation
Etiology:
Normal variant without symptoms: seen in 5 10% of adults
Compensatory mechanism to gastroesophageal reflux
Neuromuscular dysfunction of deglutition
primary neural disorders: brainstem disorder (bulbar poliomyelitis, syringomyelia, multiple sclerosis, amyotrophic lateral sclerosis); central/peripheral nerve palsy; cerebrovascular occlusive disease; Huntington chorea
primary muscle disorder: myotonic dystrophy; polymyositis; dermatomyositis; sarcoidosis; myopathies secondary to steroids/thyroid dysfunction; oculopharyngeal myopathy
myoneural junction disorder: myasthenia gravis; diphtheria; tetanus
mostly asymptomatic
dysphagia
 Cineradiography/videotape recording required for demonstration!
Cineradiography/videotape recording required for demonstration! distension of proximal esophagus + pharynx
distension of proximal esophagus + pharynx smoothly outlined shelf-/liplike projection posteriorly at level of cricoid (= pharyngoesophageal junction) = level of C5-6
smoothly outlined shelf-/liplike projection posteriorly at level of cricoid (= pharyngoesophageal junction) = level of C5-6 barium may overflow into larynx + trachea
barium may overflow into larynx + trachea
| Cx: | Zenker diverticula |
| Rx: | cricopharyngeal myotomy |
Cowden Disease
= MULTIPLE HAMARTOMA SYNDROME
= autosomal dominant disease with high penetrance characterized by multiple hamartomas + neoplasms of endodermal, ectodermal, mesodermal origin
| Incidence: | 160 cases reported |
| Cause: | susceptibility gene on long arm of chromosome 10 (10q23) |
| Age: | 2nd decade |
@ Mucocutaneous tumors
facial papules
oral papillomas (lips, gingiva, tongue)
palmoplantar keratosis, acral keratosis
@ CNS neoplasia
meningioma; glioma
Associated with: dysplastic cerebellar gangliocytoma macrocephaly
@ Breast lesions (in 50%):
 fibrocystic disease + fibroadenomas
fibrocystic disease + fibroadenomas breast cancer (20 30%): often bilateral + ductal
breast cancer (20 30%): often bilateral + ductal
@ GI tract
 multiple hamartomatous polyps (in 30 60%, commonly in rectosigmoid)
multiple hamartomatous polyps (in 30 60%, commonly in rectosigmoid)
@ Thyroid abnormalities (in 60 70%):
 adenomas + goiter
adenomas + goiter follicular thyroid adenocarcinoma (3 4%)
follicular thyroid adenocarcinoma (3 4%)
@ Genitourinary lesions
@ Skeletal abnormalities
P.818
Crohn Disease
[Burrill Crohn (1884 1983), gastroenterologist in New York, USA]
= REGIONAL ENTERITIS
= disease with prolonged + unpredictable course characterized by discontinuous + asymmetric involvement of entire GI tract
Genetic susceptibility:
homozygosity for Nod-2 gene (intracellular protein in lymphocytes) responsible for binding bacterial endotoxins + initiating a cascade that produces TNF-alpha;(tumor necrosis factor-alpha)
increased mucosal permeability for enteric bacteria
| Prevalence: | 2 3:100,000 white adults |
| Path: | transmural inflammation (noncaseating granuloma with Langhans giant cells and epithelioid cells, edema, fibrosis); obstructive lymphedema + enlargement of submucosal lymphoid follicles; ulceration of mucosa overlying lymphoid follicles |
| Age: | onset between 15 and 30 years; M:F = 1:1 |
recurrent episodes of diarrhea
colicky/steady abdominal pain
low-grade fever
weight loss, anorexia
occult blood + anemia
perianal abscess/fistula (40%)
malabsorption (30%)
| Associated with: | erythema nodosum, pyoderma gangrenosum |
| Rx: | probiotics + antibiotics (modulation of enteric flora); purine synthesis inhibitors like azathioprine + 6-mercaptopurine (downregulation of inflammatory response); infliximab (chimeric antibody binding to TNF- ) |
Intestinal Manifestations of Crohn Disease
@ Esophagus (3%)
 aphthous ulcers (early)
aphthous ulcers (early) esophagitis, stricture, fistula (late)
esophagitis, stricture, fistula (late)
@ Stomach (1 2%) = granulomatous gastritis
 aphthous ulcers (= pinpoint erosions)
aphthous ulcers (= pinpoint erosions) pseudo post Billroth-I appearance
pseudo post Billroth-I appearance ram's horn sign = poorly distensible smooth tubular narrowed antrum + widened pylorus + narrow duodenal bulb
ram's horn sign = poorly distensible smooth tubular narrowed antrum + widened pylorus + narrow duodenal bulb cobblestone appearance of mucosa
cobblestone appearance of mucosa antral-duodenal fistula
antral-duodenal fistula
@ Duodenum (4 10%)
almost always associated with gastric involvement
Location: duodenal bulb + proximal half of duodenum  superficial erosions/aphthoid ulcers (early lesion)
superficial erosions/aphthoid ulcers (early lesion) thickened duodenal folds
thickened duodenal folds
@ Small bowel (80%) = REGIONAL ENTERITIS
terminal ileum (alone/in combination in 95%); jejunum/ileum (15 55%)
 thickening + slight nodularity of circular folds
thickening + slight nodularity of circular folds aphthous ulcers
aphthous ulcers cobblestone mucosa/ulceration
cobblestone mucosa/ulceration commonly associated with medial cecal defect
commonly associated with medial cecal defect
@ Colon (22 55%) = GRANULOMATOUS COLITIS
Location: particularly on right side with rectum + sigmoid frequently spared  tiny 1 2-mm nodular filling defects (lymphoid follicular pattern)
tiny 1 2-mm nodular filling defects (lymphoid follicular pattern) aphthous ulcers with target/bull's-eye appearance
aphthous ulcers with target/bull's-eye appearance transverse stripe sign = 1-cm-long straight stripes representing contrast medium within deep grooves of coarse mucosal folds
transverse stripe sign = 1-cm-long straight stripes representing contrast medium within deep grooves of coarse mucosal folds long fistulous tracts parallel to bowel lumen
long fistulous tracts parallel to bowel lumen
@ Appendicitis (20%)
@ Rectum (14 50%)
 deep/collarbutton ulcers
deep/collarbutton ulcers rectal sinus tracts
rectal sinus tracts
Phases:
Earliest changes
 nodular enlargement of lymphoid follicles
nodular enlargement of lymphoid follicles blunting/flattening/distortion/straightening/thickening of valvulae conniventes (obstructive lymphedema, usually first seen in terminal ileum)
blunting/flattening/distortion/straightening/thickening of valvulae conniventes (obstructive lymphedema, usually first seen in terminal ileum) aphthous ulcers = nodules with shallow central barium collection up to 5 mm in diameter
aphthous ulcers = nodules with shallow central barium collection up to 5 mm in diameter
Location: duodenal bulb, second portion of duodenum, terminal ileum Advanced nonstenotic phase
 skip lesions (90%) = discontinuous involvement with intervening normal areas
skip lesions (90%) = discontinuous involvement with intervening normal areas cobblestone appearance = serpiginous longitudinal + transverse ulcers separated by areas of edema
cobblestone appearance = serpiginous longitudinal + transverse ulcers separated by areas of edema thick + blunted small bowel folds (inflammatory infiltration of lamina propria + submucosa)
thick + blunted small bowel folds (inflammatory infiltration of lamina propria + submucosa) straightening + rigidity of small bowel loops with luminal narrowing (spasm + submucosal edema)
straightening + rigidity of small bowel loops with luminal narrowing (spasm + submucosal edema) separation + displacement of small bowel loops (from lymphedematous wall thickening/increase in mesenteric fat/enlarged mesenteric lymph nodes/perforation with abscess formation)
separation + displacement of small bowel loops (from lymphedematous wall thickening/increase in mesenteric fat/enlarged mesenteric lymph nodes/perforation with abscess formation) pseudopolyps = islands of hyperplastic mucosa between denuded mucosa
pseudopolyps = islands of hyperplastic mucosa between denuded mucosa inflammatory polypoid masses
inflammatory polypoid masses sessile/pedunculated/filiform postinflammatory polyps
sessile/pedunculated/filiform postinflammatory polyps diffuse mucosal granularity due to 0.5 1-mm round lucencies (= blunted + fused villi seen en face)
diffuse mucosal granularity due to 0.5 1-mm round lucencies (= blunted + fused villi seen en face) linear ulcers on mesenteric border (nearly PATHOGNOMONIC)
linear ulcers on mesenteric border (nearly PATHOGNOMONIC)pseudodiverticula = pseudosacculations = bulging area of normal wall opposite affected scarred wall on antimesenteric side
P.819
Stenotic phase
 string sign = strictures (in 21%, most frequently in terminal ileum)/marked narrowing of rigid loops
string sign = strictures (in 21%, most frequently in terminal ileum)/marked narrowing of rigid loops normal proximal loops may be dilated with stasis ulcers + fecoliths
normal proximal loops may be dilated with stasis ulcers + fecoliths
CT:
@ bowel wall:
 mucosal hyperenhancement (best seen with bowel lumen distended by negative contrast material):
mucosal hyperenhancement (best seen with bowel lumen distended by negative contrast material): target sign of active inflammation = mural stratification = hyperenhancement of mucosa + muscularis propria sandwiching an edematous/fatty submucosa of decreased attenuation
target sign of active inflammation = mural stratification = hyperenhancement of mucosa + muscularis propria sandwiching an edematous/fatty submucosa of decreased attenuation comb sign = hyperemic engorged tortuous vasa recta leading to actively inflamed bowel segment
comb sign = hyperemic engorged tortuous vasa recta leading to actively inflamed bowel segment
 homogeneous density of thickened bowel wall (DDx: ulcerative colitis with heterogeneous attenuation):
homogeneous density of thickened bowel wall (DDx: ulcerative colitis with heterogeneous attenuation): double halo configuration (50%) = intestinal lumen surrounded by inner ring of low attenuation (= edematous mucosa) + outer ring of soft-tissue density (= thickened fibrotic muscularis + serosa) (DDx: radiation enteritis, ischemia, mesenteric venous thrombosis, acute pancreatitis)
double halo configuration (50%) = intestinal lumen surrounded by inner ring of low attenuation (= edematous mucosa) + outer ring of soft-tissue density (= thickened fibrotic muscularis + serosa) (DDx: radiation enteritis, ischemia, mesenteric venous thrombosis, acute pancreatitis) skip areas of asymmetric bowel wall thickening of 11 (range 10 20) mm in 82% (DDx: ulcerative colitis with a mean thickness of 8 mm)
skip areas of asymmetric bowel wall thickening of 11 (range 10 20) mm in 82% (DDx: ulcerative colitis with a mean thickness of 8 mm)
 luminal narrowing + proximal dilatation
luminal narrowing + proximal dilatation
@ paraenteric findings
 creeping fat = massive proliferation of mesenteric fat along mesenteric border (40%):
creeping fat = massive proliferation of mesenteric fat along mesenteric border (40%): fat attenuation elevated by 20 60 HU
fat attenuation elevated by 20 60 HU separation of small bowel loops (mass effect)
separation of small bowel loops (mass effect)
 mild mesenteric adenopathy (18%) with lymph nodes 3 8 mm small
mild mesenteric adenopathy (18%) with lymph nodes 3 8 mm small Consider lymphoma/carcinoma with lymph nodes >10 mm!
Consider lymphoma/carcinoma with lymph nodes >10 mm!
 fistula/sinus tract (15 40%)
fistula/sinus tract (15 40%) mesenteric phlegmon/abscess in 15 20% (DDx: postoperative blind loop)
mesenteric phlegmon/abscess in 15 20% (DDx: postoperative blind loop)
US:
 pseudokidney /target sign = thickening of bowel wall (22 65 89%) of 5 20 mm (DDx: ulcerative colitis)
pseudokidney /target sign = thickening of bowel wall (22 65 89%) of 5 20 mm (DDx: ulcerative colitis) circumferential diffusely hypoechoic bowel wall with loss of normal layering (due to transmural edema, inflammation, fibrosis)
circumferential diffusely hypoechoic bowel wall with loss of normal layering (due to transmural edema, inflammation, fibrosis) rigid + noncompressible bowel segment with reduction/loss of peristalsis
rigid + noncompressible bowel segment with reduction/loss of peristalsis hyperemia of gut wall + adjacent fat on color Doppler
hyperemia of gut wall + adjacent fat on color Doppler inflammatory mass = phlegmon (14%), abscess (4%)
inflammatory mass = phlegmon (14%), abscess (4%) distended fluid-filled loops (12%)
distended fluid-filled loops (12%) hypoechoic fistulous tract
hypoechoic fistulous tract
| Prognosis: | recurrence rate of up to 39% after resection (commonly at the site of the new terminal ileum, most frequently during first 2 years after resection); mortality rate of 7% at 5 years, 12% at 10 years after 1st resection |
| Cx: | (1) Fistula (2) Intramural sinus tracts (3) Abscess in up to 20% (DDx: acute appendicitis) (4) Free perforation (1 2%) (5) Toxic megacolon (6) Small bowel obstruction (15%) (7) Hydronephrosis (from ureteric compression, generally on right side) (8) Adenocarcinoma in ileum/colon (particularly in bypassed loops/in vicinity of chronic fistula) 4 20 increased risk of colonic adeno-carcinoma compared with general population with a latency period of 25 30 years! (9) Lymphoma in large + small bowel |
| DDx: | (1) Yersinia (in terminal ileum, resolution within 3 4 months) (2) Tuberculosis (more severe involvement of cecum, pulmonary TB) (3) Actinomycosis, histoplasmosis, blastomycosis, anisakiasis (4) Segmental infarction (acute onset, elderly patient) (5) Radiation ileitis (appropriate history) (6) Lymphoma (no spasm, luminal narrowing is uncommon, tumor nodules) (7) Carcinoid tumor (tumor nodules) (8) Eosinophilic gastroenteritis (9) Potassium stricture |
Fistulizing Crohn Disease
| Incidence: | 33% |
 Crohn disease is 3rd most common cause of fistula/sinus tracts (DDx: iatrogenic [most common cause], diverticula [2nd most common cause])!
Crohn disease is 3rd most common cause of fistula/sinus tracts (DDx: iatrogenic [most common cause], diverticula [2nd most common cause])!
Types:
enterocolic:
most frequently between ileum and cecum
enterocutaneous (8 21%):
rectum-to-skin; rectum-to-vagina
perineal fistula + sinus tracts
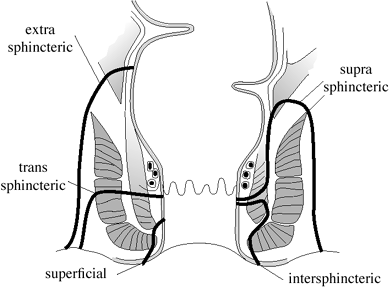 |
| Park's Classification Of Perianal Fistulas |
P.820
Extraintestinal Manifestations of Crohn Disease
@ Hepatobiliary
Fatty infiltration of liver (steroid therapy, hyperalimentation)
Hepatic abscess (rare): M:F = 3:1
Gallstones (15 34%): predominantly cholesterol;
Risk: 3 5 higher risk than expected; risk correlates with length of diseased ileum/resected ileum/duration of disease Cause: interrupted enterohepatic circulation with malabsorption of bile salts in terminal ileum Acute cholecystitis
Primary sclerosing cholangitis (1%) + hepatoma
Bile duct + gallbladder carcinoma
Pancreatitis
@ Genitourinary
Urolithiasis (5 10%): oxalate (steatorrhea leads to excess colonic absorption of oxalate)/urate stones
Hydronephrosis
Renal amyloidosis
Focal cystitis
Ileoureteral/ileovesical fistula (5 20%)
@ Musculoskeletal
digital clubbing (11 40%)
mild self-limiting seronegative peripheral migratory arthritis (15 22%): may precede bowel disease in 10%; severity + course correlates well with severity of intestinal disease; resection of diseased bowel leads to regression of symptoms
Hypertrophic osteoarthropathy
Ankylosing spondylitis (in 3 16%)
 Axial skeletal involvement usually precedes onset of GI symptoms!
Axial skeletal involvement usually precedes onset of GI symptoms!unrelated in severity/course to activity level of bowel disease
 symmetric bilateral sacroiliitis
symmetric bilateral sacroiliitis spondylitis with syndesmophytes
spondylitis with syndesmophytes
Peripheral erosive arthritis
 small marginal erosions
small marginal erosions periostitis
periostitis propensity for osseous ankylosis
propensity for osseous ankylosis
Avascular necrosis of femoral head (steroid Rx)
Pelvic osteomyelitis (contiguous involvement)
Septic arthritis
Muscle abscess
Retarded skeletal growth + maturation
@ Erythema nodosum, uveitis
Cronkhite-Canada Syndrome
= nonneoplastic nonhereditary polyps (as in juvenile polyposis) associated with ectodermal abnormalities; no familial predisposition
| Incidence: | >100 cases described |
| Histo: | hamartomatous polyps resembling juvenile/retention polyps = multiple cystic spaces filled with mucin secondary to degenerative changes; expansion + inflammation of lamina propria |
| Age: | 62 years (range 42 75 years); M < F |
exudative protein-losing enteropathy
diarrhea (disaccharidase deficiency, bacterial overgrowth in small intestine)
severe weight loss, anorexia
abdominal pain
nail atrophy
brownish macules of hand + feet
alopecia
 multiple polyps
multiple polyps thickened gastric rugae
thickened gastric rugae
| Location: | stomach (100%); small bowel (>50%); colon (100%) |
| Prognosis: | rapidly fatal in women within 6 18 months (cachexia); tendency toward remission in men |
Desmoplastic Small Round Cell Tumor
= INTRAABDOMINAL DESMOPLASTIC SMALL ROUND CELL TUMOR OF PERITONEUM
= highly malignant tumor belonging to a generic group of small round blue cell tumors (Ewing sarcoma, neuroblastoma, Wilms tumor, rhabdomyosarcoma, primitive neuroendocrine tumor)
| Incidence: | <50 cases in literature |
| Median age: | 21 years; affects children + young adults; up to 6th decade; M:F = 4:1 |
| Origin: | mesothelial/submesothelial/subserosal mesenchyme of the abdominal cavity |
| Histo: | islands of small blue cells surrounded by fibrous stroma; immunohistochemically positive for epithelial, neural, muscular markers (cytoplasmic keratin + desmin); abnormal chromosome 11 |
gastrointestinal/genitourinary discomfort/pain
abdominal distension
palpable abdominal mass
| Location: | mesentery (spread to omentum), retroperitoneum, paratesticular, posterior mediastinum, pleura, meninges |
 multiple scattered necrotic tumor masses in abdomen + pelvis with no definite visceral organ of origin:
multiple scattered necrotic tumor masses in abdomen + pelvis with no definite visceral organ of origin: nodular peritoneal thickening
nodular peritoneal thickening serosal hepatic metastases
serosal hepatic metastases punctate peritoneal calcifications
punctate peritoneal calcifications
 enlarged lymph nodes
enlarged lymph nodes scant ascites
scant ascites
| Cx: | hydronephrosis, bowel obstruction |
| Prognosis: | mean survival time of 17 months |
DDx:
in infants/adolescents: rhabdomyosarcoma; neuroblastoma; mesenteric carcinoid; Burkitt lymphoma
in adults: diffuse omental/peritoneal carcinomatosis (carcinoma of stomach, colon, ovary, pancreas); melanoma; leiomyosarcoma; lymphoma; desmoid tumor; mesothelioma; tumefactive tuberculosis; actinomycosis; Castleman disease
Diaphragm Disease
= small bowel webs due to NSAIDs
| Effect of NSAID: | gastric irritation, ulceration of small intestines |
| Frequency: | in 10% of patients receiving long-term NSAID therapy |
| Path: | foci of submucosal fibrosis with interruption of adjacent muscularis mucosae |
blood + protein loss
intermittent intestinal obstruction
| Location: | ileum > jejunum |
P.821
Enteroclysis:
 multiple concentric diaphragm-like strictures
multiple concentric diaphragm-like strictures
| DDx: | Crohn disease |
Disaccharidase Deficiency
= enzyme deficiencies for any of the disaccharides (maltose, lactose, etc.)
PRIMARY
SECONDARY to other diseases (eg, Crohn disease)
Pathophysiology:
unabsorbed disaccharides produce osmotic diarrhea
bacterial fermentation produces short-chain volatile fatty acids causing further osmotic + irritant diarrhea
 normal small bowel series without added lactose
normal small bowel series without added lactose abnormal small bowel series done with lactose (50 g added to 600 cm3 of barium suspension)
abnormal small bowel series done with lactose (50 g added to 600 cm3 of barium suspension) small + large bowel distension
small + large bowel distension dilution of barium
dilution of barium shortening of transit time
shortening of transit time
Distal Intestinal Obstruction Syndrome
= MECONIUM ILEUS EQUIVALENT
= impaction of inspissated stool in distal part of ileum + proximal part of colon
| Prevalence: | 7 15 41% of children/adolescents with cystic fibrosis; 2% in patients <5 years of age |
| Cause: | tenacious intestinal mucus, steatorrhea due to pancreatic insufficiency, undigested food residue, disordered intestinal motility with increase in intestinal transit time, fecal stasis, dehydration |
| Age: | 2nd 3rd decade of life |
recurrent bouts of colicky abdominal pain (from fecal impaction/constipation) in RLQ
palpable cecal mass
 bubbly granular ileocecal soft-tissue mass in RLQ
bubbly granular ileocecal soft-tissue mass in RLQ partial/complete small bowel obstruction (due to puttylike fecal material in terminal ileum/right colon)
partial/complete small bowel obstruction (due to puttylike fecal material in terminal ileum/right colon) thickening of mucosal folds
thickening of mucosal folds cystic fibrosis of lung
cystic fibrosis of lung
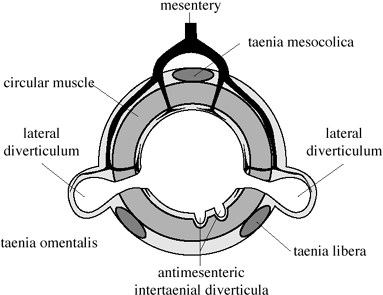 |
| Cross Section Through Colon |
CT:
| Location: | cecum > ascending colon > transverse colon > descending colon (contiguous involvement) |
 diffuse colonic thickening
diffuse colonic thickening mural striation (50%)
mural striation (50%) mesenteric soft-tissue infiltration (100%)
mesenteric soft-tissue infiltration (100%) increased pericolonic fat (60%)
increased pericolonic fat (60%)
| Cx: | intussusception, volvulus |
| Rx: | stool softeners, oral polyethylene glycol-electrolyte solution (Golytely ), increasing dose of pancreatic enzyme supplements, mucolytic agents (N-acetylcysteine) orally/with Gastrografin enema |
| DDx: | appendicitis, partial intestinal obstruction (adhesion/stricture from previous bowel surgery) |
Diverticular Disease of Colon
= overactivity of smooth muscle causing herniation of mucosa + submucosa through muscle layers
| Incidence: | 5 10% in 5th decade; 33 48% over age 50; 50 65% past 7th decade; M:F = 1:1; most common affliction of colon in developed countries |
| Cause: | decreased fecal bulk (diet high in refined fiber + low in roughage) |
| Location: | in 80% in sigmoid (= narrowest colonic segment with highest pressure); in 17% distributed over entire colon; in 4 12% isolated to cecum/ascending colon |
Prediverticular Disease of Colon
= longitudinal + circular smooth muscle thickening with redundancy of folds secondary to myostatic contracture
 saw-tooth sign = crowding + thickening of haustral folds (shortening of colonic segment)
saw-tooth sign = crowding + thickening of haustral folds (shortening of colonic segment) plump marginal indentations
plump marginal indentations superimposed muscle spasm (relieved by antispasmodics)
superimposed muscle spasm (relieved by antispasmodics)
| DDx: | hemorrhage; ischemia; radiation changes; pseudomembranous colitis |
Colonic Diverticulosis
= acquired herniations of mucosa + muscularis mucosae through the muscularis propria with wall components of mucosa, submucosa, serosa = false diverticula of pulsion type
| Location: | predominantly left-sided colon |
Site:
lateral diverticula arise between mesenteric + antimesenteric teniae on opposite sides
antimesenteric intertaenial diverticula opposite of mesenteric side
Intramural type vasa recta (= nutrient arteries) pass through the circular muscle (weakness in muscular wall) and are carried over the fundus of the diverticula as it enlarges
 size: initially tiny (3 10-mm) V-shaped protrusions increasing up to several cm in diameter
size: initially tiny (3 10-mm) V-shaped protrusions increasing up to several cm in diameter bubbly appearance of air-containing diverticula
bubbly appearance of air-containing diverticula residual barium within diverticula from previous study
residual barium within diverticula from previous study spiky irregular outline (antimesenteric intertaenial ridge is typical site for intramural diverticula)
spiky irregular outline (antimesenteric intertaenial ridge is typical site for intramural diverticula) smooth dome-shaped appendages with a short neck
smooth dome-shaped appendages with a short neck may be pointed, attenuated, irregular with variable filling
may be pointed, attenuated, irregular with variable filling circular line with sharp outer edge + fuzzy blurred inner edge (en face view in double contrast BE)
circular line with sharp outer edge + fuzzy blurred inner edge (en face view in double contrast BE) Giant sigmoid diverticulum = large gas-containing cyst (air entrapment secondary to ball-valve mechanism) arising in left iliac fossa
Giant sigmoid diverticulum = large gas-containing cyst (air entrapment secondary to ball-valve mechanism) arising in left iliac fossa
P.822
CT:
 rounded outpouchings containing air contrast material (= diverticula)
rounded outpouchings containing air contrast material (= diverticula) circumferential sawtooth-like thickening of colonic haustra + distorted luminal contour (= muscular hypertrophy)
circumferential sawtooth-like thickening of colonic haustra + distorted luminal contour (= muscular hypertrophy)
| Cx: | bleeding (usually right colon), diverticulitis (usually sigmoid colon) |
Colonic Diverticulitis
= perforation of diverticulum with intramural/localized pericolic inflammatory mass
| Incidence: | 5% of population; in 10 35% of diverticular disease; increasing frequency with age (in 5 10% >45 years of age, in 80% >85 years of age) |
| Pathogenesis: | mucosal abrasion from inspissated fecal material leads to perforation of thin wall |
pain + local tenderness + mass in LLQ
fever (25%), leukocytosis (36%)
clinical misdiagnosis rate of 34 67%
| Location: | sigmoid colon (95%), cecum (4%) |
 localized ileus
localized ileus pattern of small bowel obstruction (kinking/edema if small bowel adheres to abscess)
pattern of small bowel obstruction (kinking/edema if small bowel adheres to abscess) extraluminal gas in abscess/fistula
extraluminal gas in abscess/fistula pneumoperitoneum (rare)
pneumoperitoneum (rare)
BE (77 86% sensitive):
 focal area of eccentric luminal narrowing caused by pericolic/intramural inflammatory mass:
focal area of eccentric luminal narrowing caused by pericolic/intramural inflammatory mass: annular lesion mimicking carcinoma
annular lesion mimicking carcinoma
 marked thickening + distortion of mucosal folds
marked thickening + distortion of mucosal folds tethered spiculated mucosal folds
tethered spiculated mucosal folds centrally amputated diverticulum
centrally amputated diverticulum extraluminal contrast = peridiverticulitis:
extraluminal contrast = peridiverticulitis: double-tracking = pericolonic longitudinal sinus tract
double-tracking = pericolonic longitudinal sinus tract pericolonic collection = peridiverticular abscess
pericolonic collection = peridiverticular abscess fistula to bladder/small bowel/vagina
fistula to bladder/small bowel/vagina
CT (79 93% sensitive, 77% specific):
 inflamed diverticulum:
inflamed diverticulum: pericolic fat stranding = poorly marginated hazy area of increased attenuation fine linear strands within pericolic fat (98%)
pericolic fat stranding = poorly marginated hazy area of increased attenuation fine linear strands within pericolic fat (98%) diverticula (84%) = flask-shaped structures projecting through colonic wall + filled with air/barium/fecal material
diverticula (84%) = flask-shaped structures projecting through colonic wall + filled with air/barium/fecal material centipede sign = hyperemic engorged vasa recta
centipede sign = hyperemic engorged vasa recta
 bowel wall thickening:
bowel wall thickening: circumferential bowel wall thickening of >4 mm (70%)
circumferential bowel wall thickening of >4 mm (70%) focally thickened + inflamed colonic wall
focally thickened + inflamed colonic wall arrowhead sign = funnel of intraluminal contrast medium/air in focally thickened colonic wall centering about occluded orifice of inflamed diverticulum (27%)
arrowhead sign = funnel of intraluminal contrast medium/air in focally thickened colonic wall centering about occluded orifice of inflamed diverticulum (27%)
 fluid collection:
fluid collection: frank abscess (47%) = central liquid/gas
frank abscess (47%) = central liquid/gas fluid air of peritonitis (16%)
fluid air of peritonitis (16%) fluid at root of sigmoid mesentery
fluid at root of sigmoid mesentery
 tract formation:
tract formation: fistula formation (14%): most commonly colovesical, also colovaginal, coloenteric, colocutaneous
fistula formation (14%): most commonly colovesical, also colovaginal, coloenteric, colocutaneous intramural sinus tracts (9%)
intramural sinus tracts (9%)
 fecolith
fecolith colonic obstruction (12%)
colonic obstruction (12%) ureteral obstruction (7%)
ureteral obstruction (7%)
US (85 98% sensitive, 80 97% specific):
 thickening of bowel wall = >4 mm distance between echogenic lumen interface and serosa
thickening of bowel wall = >4 mm distance between echogenic lumen interface and serosa diverticula = round/oval hypo-/hyperechoic foci protruding from colonic wall with focal disruption of normal layer continuity internal acoustic shadowing
diverticula = round/oval hypo-/hyperechoic foci protruding from colonic wall with focal disruption of normal layer continuity internal acoustic shadowing inflammatory pericolic fat = regionally increased echogenicity adjacent to colonic wall ill-defined hypoechoic zones
inflammatory pericolic fat = regionally increased echogenicity adjacent to colonic wall ill-defined hypoechoic zones pericolic abscess
pericolic abscess
| Prognosis: | (a) self-limiting (usually) (b) transmural perforation (c) superficial ulceration (d) chronic abscess |
| Cx: | (1) Colonic obstruction (2) Fistula to bladder/vagina/small bowel (3) Free perforation (rare) |
| DDx: | (1) Colonic neoplasm (shorter segment, heaped-up margins, ulcerated mucosa) (2) Crohn colitis (double-tracking longer than 10 cm) |
| Rx: | antibiotics, surgery (in 25%), percutaneous abscess drainage |
Right Colonic Diverticulitis
= congenital true diverticulum
| Frequency: | 1:34 1:300 appendectomies |
| Age: | any; peak prevalence at 35 45 years of age |
protracted mild pain; palpable mass in 33%
 solitary diverticulum containing a 12-mm fecolith surrounded by inflamed fat
solitary diverticulum containing a 12-mm fecolith surrounded by inflamed fat marked circumferential colonic wall thickening
marked circumferential colonic wall thickening
| Cx: | pericolonic abscess |
| Prognosis: | spontaneous evacuation into colonic lumen |
| Rx: | conservative |
| DDx: | appendicitis |
Colonic Diverticular Hemorrhage
Not related to diverticulitis
| Incidence: | in 3 47% of diverticulosis |
| Location: | 75% located in ascending colon (larger neck + dome of diverticula) |
massive rectal hemorrhage without pain
 extravasation of radionuclide tracers
extravasation of radionuclide tracers angiographic contrast pooling in bowel lumen
angiographic contrast pooling in bowel lumen
| Rx: | (1) transcatheter infusion of vasoconstrictive agents (Pitressin ) (2) embolization with Gelfoam |
P.823
Dumping Syndrome
= early postprandial vascular symptomatology of sweating, flushing, palpitation, feeling of weakness and dizziness
| Pathophysiology: | rapid entering of hypertonic solution into jejunum resulting in fluid shift from blood compartment into small bowel |
| Incidence: | 1 5%; M:F = 2:1 |
 Roentgenologic findings not diagnostic!
Roentgenologic findings not diagnostic! rapid emptying of barium into small bowel (= loss of gastric reservoir function)
rapid emptying of barium into small bowel (= loss of gastric reservoir function)
| Rx: | lying down, diet |
| DDx: | late postprandial hypoglycemia (90 120 minutes after eating) |
Duodenal Atresia
= most common cause of congenital duodenal obstruction; second most common site of gastrointestinal atresias after ileum
| Incidence: | 1:10,000; M:F = 1:1 |
| Etiology: | defective vacuolization of duodenum between 6th and 11th weeks of fetal life; rarely from vascular insult (extent of obstruction usually involves larger regions with vascular insult) |
| Age at presentation: | first few days of life |
persistent bilious vomiting a few hours after birth/following 1st feeding (75%)
rapid deterioration secondary to loss of fluids + electrolytes
Isolated sporadic anomaly (30 52%)
Associated anomalies (in 50 60%):
Down syndrome (20 33%);
 25% of fetuses with duodenal atresia have Down syndrome!
25% of fetuses with duodenal atresia have Down syndrome! <5% of fetuses with Down syndrome have duodenal atresia!
<5% of fetuses with Down syndrome have duodenal atresia!
CHD (8 30 50%): endocardial cushion defect, VSD
Gastrointestinal anomalies (26%):
esophageal atresia, biliary atresia, duodenal duplication, imperforate anus, small bowel atresia, malrotation, Ladd bands, Meckel diverticulum, transposed liver, annular pancreas (20%), preduodenal portal vein
Urinary tract anomalies (8%)
Vertebral + rib anomalies (37%)
| Location: | (a) usually distal to ampulla of Vater (80%) (b) proximal duodenum (20%) |
 double bubble sign = gas-fluid levels in duodenal bulb + gastric fundus
double bubble sign = gas-fluid levels in duodenal bulb + gastric fundus total absence of intestinal gas in small/large bowel
total absence of intestinal gas in small/large bowel colon of normal caliber
colon of normal caliber
OB-US (usually not identified prior to 24 weeks GA):
elevated AFP
 double bubble sign = simultaneous distension of stomach + 1st portion of duodenum, continuity of fluid between stomach + duodenum must be demonstrated
double bubble sign = simultaneous distension of stomach + 1st portion of duodenum, continuity of fluid between stomach + duodenum must be demonstrated increased gastric peristalsis
increased gastric peristalsis polyhydramnios in 3rd trimester (100%)
polyhydramnios in 3rd trimester (100%)
| Prognosis: | 36% mortality in neonates |
| DDx: | (1) Prominent incisura angularis causing bidissection of stomach (2) Choledochal cyst (3) Annular pancreas (4) Peritoneal bands (5) Intestinal duplication |
| Cx: | prematurity (40%) secondary to preterm labor related to polyhydramnios |
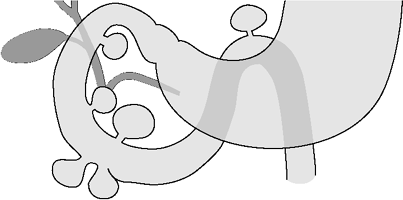 |
| Duodenal Diverticula |
Duodenal Diverticulum
| Incidence: | 1 5% of GI studies; 22% of autopsies |
PRIMARY DIVERTICULUM
= mucosal prolapse through muscularis propria
posteriorly (8%), lateral wall (4%)
SECONDARY DIVERTICULUM
= all layers of duodenal wall = true diverticulum as complication of duodenal/periduodenal inflammation
| Location: | almost invariably in 1st portion of duodenum |
mostly asymptomatic
| Cx: | (1) Perforation + peritonitis (2) Bowel obstruction (3) Biliary obstruction (4) Bleeding (5) Diverticulitis |
Duodenal Ulcer
| Incidence: | 200,000 cases/year; 2 3 more frequent than gastric ulcers; M:F = 3:1 |
| Pathophysiology: | too much acid in duodenum from (a) abnormally high gastric secretion (b) inadequate neutralization |
| Predisposed: | cortisone therapy, severe cerebral injury, after surgery, chronic obstructive pulmonary disease |
Location:
bulbar (95%):
anterior wall (50%), posterior wall (23%), inferior wall (22%), superior wall (5%)
 bulbar deformity in 85%
bulbar deformity in 85%
postbulbar (3 5%):
M:F = 7:1; majority on medial wall above papilla
hemorrhage in 66%
 edema + spasm may obscure ulcer
edema + spasm may obscure ulcer smooth rounded indentation of lateral wall
smooth rounded indentation of lateral wall
 frequently <1 cm round/ovoid (5% linear) ulcer niche
frequently <1 cm round/ovoid (5% linear) ulcer niche kissing ulcers = ulcers opposite from each other on anterior + posterior wall
kissing ulcers = ulcers opposite from each other on anterior + posterior wall giant duodenal ulcer >2 cm (rare) with higher morbidity + mortality; may be overlooked by simulating a normal/deformed scarred duodenal bulb
giant duodenal ulcer >2 cm (rare) with higher morbidity + mortality; may be overlooked by simulating a normal/deformed scarred duodenal bulb cloverleaf deformity, hourglass stenosis (healed stage) with prestenotic dilatation of recesses
cloverleaf deformity, hourglass stenosis (healed stage) with prestenotic dilatation of recesses
P.824
| Cx: | (1) Obstruction (5%) (2) Perforation (<10%): anterior > posterior wall; fistula to gallbladder (3) Penetration (<5%) = sealed perforation (4) Hemorrhage (15%): melena > hematemesis |
| Rx: | antral resection (Billroth I) + vagotomy |
Duodenal Varices
= dilated collateral veins secondary to portal hypertension (posterior superior pancreaticoduodenal vein)
 lobulated filling defects (best demonstrated in prone position, maximal luminal distension will obliterate them)
lobulated filling defects (best demonstrated in prone position, maximal luminal distension will obliterate them) commonly associated with fundal + esophageal varices
commonly associated with fundal + esophageal varices
Duplication Cyst
= uncommon congenital anomaly found anywhere along alimentary tract from tongue to anus
| Incidence: | 15% of pediatric abdominal masses are gastrointestinal duplication cysts |
Theories of formation:
Abortive twinning
Persistent embryologic diverticula
Split notochord
Aberrant luminal recanalization (Bremer): foregut epithelium grows and obliterates lumen (solid stage for esophagus, small bowel, colon); later produces secretions that form vacuoles in the intercellular space; vacuoles line up longitudinally and coalesce to form new lumen; failure of an aberrant vacuole to coalesce creates a wall cyst
Intrauterine vascular accident (Favara) associated with alimentary tract atresia in 9%
| Age: | presentation often in infancy/early childhood |
| Path: | spherical cyst/tubular structure located in/immediately adjacent to gastrointestinal tract; shares a common muscle wall + blood supply; has a separate mucosal lining; cyst contents are usually serous |
| Histo: | smooth muscle wall + lined with alimentary tract mucosa; ectopic mucosa; squamous, transitional, ciliated mucosa; lymphoid aggregates; ganglion cells Gastric mucosa + pancreatic tissue are the only ectopic tissues of clinical importance! |
respiratory distress (with esophageal duplication)
palpable abdominal mass
nausea, emesis (due to partial/complete obstruction)
| Location: | ileum (30 33%), esophagus (17 20%), colon (13 30%), jejunum (10 13%), stomach (7%), pylorus (4%), duodenum (4 5%), ileocecal junction (4%), rectum (4%) In 7 15% concomitant duplications elsewhere in the alimentary tract! |
| Site: | on mesenteric aspect of alimentary canal |
Morphology:
large spherical/saccular cyst (82%)
small intramural cyst
tubular sausage-shaped cyst (18%): commonly along small + large bowel; frequently communicates with lumen of adjacent gut
BE:
 mass extrinsic to bowel lumen
mass extrinsic to bowel lumen
US:
 elongated tubular/spherical cystic mass:
elongated tubular/spherical cystic mass: sonolucent mass with good through transmission (due to clear fluid content)
sonolucent mass with good through transmission (due to clear fluid content) echogenic mass (due to hemorrhage + inspissated material)
echogenic mass (due to hemorrhage + inspissated material)
 muscular rim sign (= echogenic inner mucosal lining + hypoechoic outer rim) in 47%
muscular rim sign (= echogenic inner mucosal lining + hypoechoic outer rim) in 47% cyst paralleling normal bowel lumen
cyst paralleling normal bowel lumen
CT:
 smoothly rounded fluid-filled cyst/tubular structure
smoothly rounded fluid-filled cyst/tubular structure thin slightly enhancing wall
thin slightly enhancing wall
MR:
 heterogeneous signal intensity of intracystic fluid on T1WI + homogeneous high signal intensity on T2WI
heterogeneous signal intensity of intracystic fluid on T1WI + homogeneous high signal intensity on T2WI
| Cx: | bowel obstruction, intussusception (due to cyst at ileocecal junction), small bowel volvulus (due to weight of duplication), bleeding (due to presence of gastric mucosa/pressure necrosis of adjacent mucosa by cyst expansion/from intussusception) |
DDx:
Omental cyst (greater omentum/lesser sac, multilocular)
Mesenteric cyst (between leaves of small bowel mesentery)
Choledochal cyst
Ovarian cyst
Pancreatic pseudocyst
Cystic renal tumor
Abscess
Meckel diverticulum (communicates with GI tract)
Lymphangioma
Mesenteric lymphoma
Intramural tumor
Colonic Duplication Cyst
| Incidence: | 13% of all alimentary tract duplications |
Cystic Colonic Duplication (7%)
| Path: | closed spherical cyst; contains gastric mucosa in 2% + ectopic pancreatic tissue in 5% |
abdominal mass, bowel obstruction/constipation
GI hemorrhage
| Location: | cecum (40%) intussusception |
 air/intestinal matter can enter cyst (20%)
air/intestinal matter can enter cyst (20%)
Colorectal Tubular Duplication (6%)
= DUPLICATION OF THE HINDGUT
= double-barreled duplication involving part/all of large bowel with twin segment on mesenteric/antimesenteric side
| Symptomatic age: | neonatal period/infancy; M:F = 1:2 |
May be associated with:
rectogenital/rectourinary fistula, duplication of internal/external genitalia, vertebral anomalies, multisystem congenital anomaly complex
bowel obstruction/constipation
passage of feces through vagina
 simultaneous opacification of true + twin colon
simultaneous opacification of true + twin colon duplication may terminate at
duplication may terminate at2nd functional anus
imperforate perineal orifice
fistulous communication with GU tract
P.825
Double Appendix
Duodenal Duplication Cyst
| Incidence: | 5% of all alimentary tract duplications |
| Path: | noncommunicating spherical cyst; may contain ectopic gastric mucosa in 21%, small bowel mucosa, pancreatic tissue |
obstructive symptoms, palpable abdominal mass
hemorrhage (due to peptic ulceration)
jaundice (due to biliary obstruction)
pancreatitis (due to ectopic pancreatic tissue)
| Site: | on mesenteric side of anterior wall of 1st + 2nd portion of duodenum |
 mass in concavity of duodenal C-loop
mass in concavity of duodenal C-loop compression + displacement of 1st/2nd portion of duodenum superiorly + anteriorly
compression + displacement of 1st/2nd portion of duodenum superiorly + anteriorly
Cholangiography:
 may communicate with pancreatic ductal system through the aberrant duct of an accessory lobe
may communicate with pancreatic ductal system through the aberrant duct of an accessory lobe
| Cx: | pancreatitis from perforation of duplication cyst |
| DDx: | pancreatic cyst, pancreatic pseudocyst, choledochal cyst, choledochocele, duodenal intramural tumor, pancreatic tumor |
Esophageal Duplication Cyst
arises from foregut
| Incidence: | 10 20% of all alimentary tract duplications; 0.5 2.5% of all esophageal masses; M:F = 2:1 |
| Path: | contains ectopic gastric mucosa in 43% |
| Histo: | contains no cartilage, lined by alimentary tract mucosa |
| Associated with: | vertebral anomalies (spina bifida, hemivertebra, fusion defects), esophageal atresia, small bowel duplication (18%) |
| Location: | adjacent to esophagus/within esophageal musculature at any level, paraspinal position; R:L = 2:1; in right pleural space detached from esophagus (rare) |
CERVICAL ESOPHAGUS (23%)
asymptomatic enlarging lateral neck mass
upper airway obstruction in newborn
DDx: thyroglossal duct cyst, branchial cleft cyst, cystic hygroma, cervical tumor, cervical lymphadenopathy MIDESOPHAGUS (17%)
severe upper airway obstruction in early infancy
DDx: bronchogenic cyst, neurenteric cyst, intramural esophageal tumor DISTAL ESOPHAGUS (60%)
frequently asymptomatic
Location: paraspinal DDx: bronchogenic cyst, neurenteric cyst, intramural esophageal tumor  thick-walled closed spherical cyst, almost never communicating
thick-walled closed spherical cyst, almost never communicating
CXR:
 posterior mediastinal mass air-fluid level
posterior mediastinal mass air-fluid level lobar consolidation + central cavitation (from autodigestion of lung tissue by gastric secretions)
lobar consolidation + central cavitation (from autodigestion of lung tissue by gastric secretions) thoracic vertebral anomalies
thoracic vertebral anomalies
UGI:
 displacement of esophagus by paraesophageal mass
displacement of esophagus by paraesophageal mass intramural extramucosal mass
intramural extramucosal mass
US:
 hypoechoic fluid-filled cyst + inner mucosal lining
hypoechoic fluid-filled cyst + inner mucosal lining
CT:
 sharply marginated homogeneous near-water density mass without enhancement
sharply marginated homogeneous near-water density mass without enhancement
| Cx: | (1) Peptic ulceration (secondary to gastric mucosa) (2) Perforation (secondary to penetrating ulcer) (3) Hematemesis (from erosion into esophagus) (4) Hemoptysis + autodigestion of pulmonary tissue (from erosion into tracheobronchial tree) |
Gastric Duplication Cyst
= intramural gastric cyst lined with secretory epithelium
| Incidence: | 7% of all alimentary tract duplications |
| Path: | noncommunicating spherical cyst (majority); may communicate with aberrant pancreatic duct; ectopic pancreatic tissue found in 37% |
| Symptomatic age: | infancy; in 75% detected before age 12; M:F = 1:2 |
pain (from overdistension of cyst, rupture with peritonitis, peptic ulcer formation, internal pancreatitis)
vomiting, anemia, fever
symptoms mimicking congenital hypertrophic pyloric stenosis (if duplication in antrum/pylorus)
| Most common site: | greater curvature (65%) |
 paragastric cystic mass up to 12 cm in size, indenting greater curvature
paragastric cystic mass up to 12 cm in size, indenting greater curvature seldom communicates with main gastric lumen at one or both ends
seldom communicates with main gastric lumen at one or both ends may enlarge + ulcerate
may enlarge + ulcerate Tc-99m uptake
Tc-99m uptake
US:
 cyst with two wall layers: inner echogenic layer of mucosa + outer hypoechoic layer of muscle
cyst with two wall layers: inner echogenic layer of mucosa + outer hypoechoic layer of muscle clear/debris-containing fluid
clear/debris-containing fluid
| Cx: | (1) Partial/complete small bowel obstruction (2) Relapsing pancreatitis (with ductal communication) (3) Ulceration, perforation, fistula formation |
| DDx: | pancreatic cyst, pancreatic pseudocyst, mesenteric cyst, leiomyoma, adenomatous polyp, hamartoma, lipoma, neurofibroma, teratoma |
Rectal Duplication Cyst
| Incidence: | 4% of all alimentary tract duplications |
| Path: | spherical fluid-filled cyst; may contain duodenal/gastric mucosa + pancreatic tissue |
| Site: | posterior to rectum/anus |
 communication with rectum/perianal fistula (in 20%)
communication with rectum/perianal fistula (in 20%)
| Symptomatic age: | childhood |
P.826
constipation + fecal soiling
palpable retrorectal/retroanal mass
intractable excoriation of perianal skin (with chronic perianal fistula)
 cystic mass; may be echogenic (due to solid material gas from communication with rectum)
cystic mass; may be echogenic (due to solid material gas from communication with rectum)
| DDx: | anterior meningocele, sacrococcygeal teratoma, retrorectal abscess, pilonidal cyst, sacral bone tumor |
Small Bowel Duplication Cyst
| Incidence: | most common of all alimentary tract duplications |
| Symptomatic age: | neonatal period (1/3); <2 years of age (in 72%) |
| Path: | contains ectopic gastric mucosa in 24%; ectopic pancreatic tissue in jejunum (8%) |
| May be associated with: | small bowel atresia |
neonatal bowel obstruction
intussusception, palpable mass
acute abdominal pain
GI hemorrhage (may be painless)
| Location: | ileum (33%), jejunum (10%), ileocecal (4%) |
| Site: | on mesenteric side |
 low small bowel obstruction soft-tissue mass
low small bowel obstruction soft-tissue mass cyst may serve as lead point for intussusception
cyst may serve as lead point for intussusception
| DDx: | mesenteric cyst, pancreatic pseudocyst, omental cyst, exophytic hepatic cyst, ovarian cyst |
Thoracoabdominal Duplication
= FOREGUT DUPLICATION
= long tubular cyst closed at its cranial end, passing through diaphragm through its own hiatus, in 60% communicating with normal duodenum/jejunum/ileum
| Incidence: | 2% of all alimentary tract duplications |
| Associated with: | thoracic vertebral anomalies |
| Histo: | gastric mucosa in 29% |
| Symptomatic age: | 50% during neonatal period; 80% within 1st year of life |
severe respiratory distress
chest pain, GI bleeding, anemia
 tubular right posterior mediastinal mass air
tubular right posterior mediastinal mass air thoracic vertebral anomaly
thoracic vertebral anomaly contrast material may enter through distal connection
contrast material may enter through distal connection
Ectopic Pancreas
= PANCREATIC REST = MYOEPITHELIAL HAMARTOMA
| Incidence: | 2 10% of autopsies; M:F = 2:1 |
asymptomatic
| Location: | lesions may be multiple (a) greater curvature of antrum 1 6 cm from pylorus, pylorus, duodenal bulb, proximal jejunum (in 80%) (b) ileum, Meckel diverticulum |
 smooth cone-/nipple-shaped submucosal nodule 1 5 cm in size
smooth cone-/nipple-shaped submucosal nodule 1 5 cm in size central umbilication representing orifice of filiform duct
central umbilication representing orifice of filiform duct
Enteric Cyst
= cyst lined by gastrointestinal mucosa without bowel wall
| Etiology: | migration of small bowel/colonic diverticulum into mesentery/mesocolon |
| Path: | unilocular thin smooth-walled cyst with serous contents lined by enteric epithelium + thin fibrous wall |
US:
 hypoechoic cystic mass, occasionally with septations
hypoechoic cystic mass, occasionally with septations
| DDx: | duplication cyst (reduplication of bowel wall) |
Eosinophilic Gastroenteritis
= uncommon self-limited form of gastroenteritis with remissions + exacerbations characterized by infiltration of eosinophilic leukocytes into stomach/small bowel wall + usually marked peripheral eosinophilia
| Cause: | unknown |
| Histo: | fibrous tissue + eosinophilic infiltrate of gastrointestinal mucosa |
| Age: | in children + young adults with allergy + eosinophilia |
EOSINOPHILIC GRANULOMA
= FIBROUS POLYPOID LESION
= INFLAMMATORY PSEUDOTUMOR
= localized form/circumscribed type
Location: almost exclusively in stomach (most common in antrum + pylorus)  submucosal polypoid mass/pedunculated polyp
submucosal polypoid mass/pedunculated polyp
EOSINOPHILIC GASTROENTERITIS
= diffuse type
= eosinophilic infiltration of mucosa, submucosa, and muscular layers of small intestine stomach by mature eosinophils ( gastric pendant to L ffler syndrome)
recurrent episodes of abdominal pain, diarrhea, vomiting
weight loss
hematemesis (from ulceration)
peripheral eosinophilia, anemia
history of systemic allergy/food allergy
| Location: | entire small bowel (particularly jejunum), distal stomach, omentum, mesentery |
| Site: | (a) mucosal (b) muscular (c) serosal (rare) |
@ Stomach (almost always limited to antrum)
 wet stomach
wet stomach  ulcers are rare
ulcers are rare
mucosal type
 enlarged gastric rugae/cobblestone nodules/polyps
enlarged gastric rugae/cobblestone nodules/polyps
muscular type
 thickened + rigid wall with narrowed gastric antrum/pylorus
thickened + rigid wall with narrowed gastric antrum/pylorus bulky intraluminal mass up to 9 cm in size
bulky intraluminal mass up to 9 cm in size
Cx: pyloric obstruction DDx: hypertrophic gastritis, lymphoma, carcinoma
@ Small bowel (involved in 50%)
 separation of small bowel loops
separation of small bowel loops
mucosal type
malabsorption + hypoproteinemia
 thickening + distortion of folds predominantly in jejunum
thickening + distortion of folds predominantly in jejunum
submucosal/muscular type
 motility disturbance
motility disturbance small-bowel obstruction
small-bowel obstruction effacement of mucosal pattern + narrowing of lumen
effacement of mucosal pattern + narrowing of lumen
serosal type
 ascites
ascites
P.827
| Prognosis: | tendency toward spontaneous remission |
| Rx: | steroids/removal of sensitizing agent |
Epiploic Appendagitis
= rare inflammation of one of the 100 epiploic/omental appendages, between 5 and 50 mm long, arising from serosal surface of colon
| Cause: | (a) primary: torsion (exercise), venous thrombosis (b) secondary: inflammation of adjacent organ (eg, diverticulitis, appendicitis) |
| Associated with: | obesity, hernia, unaccustomed exercise |
| Age: | 4th 5th decade; M>F |
| Histo: | acute infarction with fat necrosis, inflammation, thrombosed vessels with hemorrhagic suffusion |
abrupt onset of localized abdominal pain (RLQ in 50%), gradually resolving over 3 7 days
palpable mass (10 30%)
peritoneal signs
normal/mildly increased WBCs; NO fever
 Almost never suspected preoperatively!
Almost never suspected preoperatively!
| Location: | anterolaterally/(occasionally) anteromedially to sigmoid > descending > ascending colon |
US:
 solid hyperechoic noncompressible oval mass at site of maximal tenderness
solid hyperechoic noncompressible oval mass at site of maximal tenderness hypoechoic margin (93%)
hypoechoic margin (93%) absence of central blood flow
absence of central blood flow
CT:
 pericolic oval-shaped pedunculated mass, 1 5 cm in diameter, with fat attenuation (approx. 60 HU):
pericolic oval-shaped pedunculated mass, 1 5 cm in diameter, with fat attenuation (approx. 60 HU): hyperattenuating peripheral rim
hyperattenuating peripheral rim internal fat stranding
internal fat stranding
 periappendigeal fat infiltration
periappendigeal fat infiltration thickening of adjacent visceral peritoneal lining (93%)
thickening of adjacent visceral peritoneal lining (93%)
MR:
 foal lesion with signal intensity of fat
foal lesion with signal intensity of fat enhancing rim
enhancing rim
| Cx: | adhesion, bowel obstruction, intussusception, intraperitoneal loose body, peritonitis, abscess |
| Prognosis: | spontaneous resolution within 2 weeks clinically + within 6 months on CT |
| Rx: | conservative management with NSAID |
| DDx: | torsion/infarction of greater omentum, sclerosing mesenteritis, diverticulitis, appendicitis, primary tumor of mesocolon |
Esophageal Cancer
| Incidence: | <1% of all cancers; 4 10% of all GI malignancies; 11,000 cases/year (USA in 1994); M:F = 4:1; Blacks:Whites = 2:1 |
| High-risk regions: | Iran, parts of Africa, Italy, China |
Predisposing factors:
achalasia (risk factor of 1,000 x), asbestosis, Barrett esophagus, celiac disease, radiation exposure, caustic stricture (risk factor of 1,000 x), Plummer-Vinson syndrome, tannins, alcohol, tobacco, history of oral/pharyngeal cancer, tylosis palmaris et plantaris
| mnemonic: | BELCH SPAT |
Barrett esophagus
EtOH abuse
Lye stricture
Celiac disease
Head and neck tumor
Smoking
Plummer-Vinson syndrome
Achalasia, Asbestosis
Tylosis
Cancer Staging:
TNM system:
T1 tumor invades lamina propria/submucosa T2 tumor invades muscularis propria T3 tumor invades adventitia T4 tumor invades adjacent structures Stage I = T1,N0,M0 Stage IIA = T2/3,N0,M0 Stage IIB = T1/2,N1,M0 Stage III = T3,N1,M0
or T4,N0/1,M0Stage IV = T1-4,N0/1,M1 CT staging (Moss):
Stage 1 intraluminal tumor/localized wall thickening of 3 5 mm Stage 2 localized/circumferential wall thickening >5 mm Stage 3 contiguous spread into adjacent mediastinum (trachea, bronchi, aorta, pericardium)
loss of fat planes (nonspecific due to cachexia, often still resectable)
mass in contact with aorta >90 arc (in 20 70% still resectable)
displacement/compression of airway (90 100% accuracy for invasion)
esophagotracheal/-bronchial fistula (unresectable)Stage 4 distant metastases
enlarged abdominal lymph nodes >10 mm (12 85% accuracy)
hepatic, pulmonary, adrenal metastases direct erosion of vertebral body
tumor >3 cm wide = high frequency of extraesophageal spread
Histo:
Squamous cell carcinoma (50 70%)
Adenocarcinoma (30 50%) arising from mucosal/submucosal glands or heterotopic gastric mucosa or columnar-lined epithelium (Barrett)
in 70% from Barrett esophagus
gastric adenocarcinoma involving GE junction
in submucosal/deep esophageal glands
ectopic gastric mucosa in esophagus
 2,500 new cases each year; M:F = 7:1
2,500 new cases each year; M:F = 7:1 tendency to invade gastric cardia + fundus
tendency to invade gastric cardia + fundus
Spindle-cell squamous carcinoma = carcinosarcoma = pseudosarcoma
Histo: squamous + sarcomatous elements Age: in men >45 years Location: usually middle third of esophagus  large bulky polypoid smooth, lobulated, scalloped intraluminal mass; may be pedunculated
large bulky polypoid smooth, lobulated, scalloped intraluminal mass; may be pedunculated
DDx: lymphoma, other sarcomas Mucoepidermoid ca., adenoid cystic carcinoma
Leiomyosarcoma, rhabdomyosarcoma, fibrosarcoma, malignant lymphoma
Secondary tumor involvement from: thyroid, larynx
Metastasis from: breast, melanoma, GI tract
P.828
dysphagia (87 95%) of <6 months' duration
weight loss (71%)
retrosternal pain (46%)
regurgitation (29%)
| Location: | upper 1/3 (15 20%); middle 1/3 (37 44%); lower 1/3 (38 43%) |
Radiologic types:
Polypoid/fungating form (most common)
 sessile/pedunculated tumor with lobulated surface
sessile/pedunculated tumor with lobulated surface protruding, irregular, polycyclic, overhanging, steplike apple core lesion
protruding, irregular, polycyclic, overhanging, steplike apple core lesion
Ulcerating form
 large ulcer niche within bulging mass
large ulcer niche within bulging mass
Infiltrating form
 gradual narrowing with smooth transition
gradual narrowing with smooth transition(DDx: benign stricture)
Varicoid form = superficial spreading carcinoma
Histo: longitudinal extension confined to mucosa/submucosa  focal area of confluent mucosal nodules/plaques
focal area of confluent mucosal nodules/plaques
DDx: Candida esophagitis
Metastases:
lymphogenic: anterior jugular chain + supraclavicular nodes (primary in upper 1/3); paraesophageal + subdiaphragmatic nodes (primary in middle 1/3); mediastinal + paracardial + celiac trunk nodes (primary in lower 1/3)
hematogenous: lung, liver, adrenal gland
CXR:
 widened azygoesophageal recess with convexity toward right lung (in 30% of distal + midesophageal cancers)
widened azygoesophageal recess with convexity toward right lung (in 30% of distal + midesophageal cancers) thickening of posterior tracheal stripe + right paratracheal stripe >4 mm (if tumor located in upper third of esophagus)
thickening of posterior tracheal stripe + right paratracheal stripe >4 mm (if tumor located in upper third of esophagus) widened mediastinum
widened mediastinum tracheal deviation
tracheal deviation posterior tracheal indentation/mass
posterior tracheal indentation/mass retrocardiac mass
retrocardiac mass esophageal air-fluid level
esophageal air-fluid level lobulated mass extending into gastric air bubble
lobulated mass extending into gastric air bubble repeated aspiration pneumonia (with tracheoesophageal fistula)
repeated aspiration pneumonia (with tracheoesophageal fistula)
| Cx: | fistula formation to trachea (5 10%)/bronchi/mediastinum |
| Prognosis: | 3 5 20% 5-year survival rate; 0% 5-year survival rate for cancer of cervical esophagus |
Mean survival time:
90 days with subdiaphragmatic lymphadenopathy
180 days with local invasion + abdominal metastases
480 days without evidence of invasion/metastases
| Rx: | (1) chemotherapy (fluorouracil, cisplatin, bleomycin sulfate, mitomycin) + surgery (2) chemotherapy + irradiation (~4,000 cGy) (3) chemotherapy + irradiation + surgery |
| Operative mortality: | 3 8% |
Esophageal Intramural Pseudodiverticulosis
= dilated excretory ducts of deep mucous glands
| Etiology: | uncertain |
| Incidence: | about 100 cases in world literature |
In 90% associated with:
diabetes, alcoholism, any severe esophagitis (most often reflux/Candida), esophageal stricture
| Site: | diffuse/segmental involvement |
 multiple tiny rounded/flask-shaped barium collections in longitudinal rows parallel to long axis of esophagus:
multiple tiny rounded/flask-shaped barium collections in longitudinal rows parallel to long axis of esophagus: appear to float outside esophagus without apparent communication with lumen
appear to float outside esophagus without apparent communication with lumen
 esophageal stricture:
esophageal stricture: short stricture in distal esophagus (common)
short stricture in distal esophagus (common) long stricture in cervical/upper thoracic esophagus (classic)
long stricture in cervical/upper thoracic esophagus (classic)
Esophageal Perforation
= ESOPHAGEAL RUPTURE
Cause:
Iatrogenic injury (most common cause, 55%): complication of endoscopy, dilatation of stricture, bougie, disruption of suture line following surgical anastomosis, attempted intubation
Spontaneous rupture = Boerhaave syndrome (15%): emetogenic injury of the esophagus from sudden increase in intraabdominal pressure + relaxation of distal esophageal sphincter in the presence of a moderate to large amount of gastric contents
Closed chest trauma (10%)
Incidence: 1% of all blunt chest trauma Location:
cervical/upper thoracic esophagus (82%)
just above gastroesophageal junction along posterolateral wall on the left side
Esophageal carcinoma
Retained foreign body (14%): coin, aluminum pop-tops, metallic button, safety pin, invisible plastic toy) leading to perforation (in pediatric age group)
Barrett ulcer
pain, dysphagia, odynophagia
rapid onset of overwhelming sepsis: fever, tachycardia, hypotension, shock
Plain film (normal in 9 12%):
 extensive pneumomediastinum
extensive pneumomediastinum V sign of Naclerio = extrapleural air within lower mediastinum between parietal pleura + diaphragm (usually on left)
V sign of Naclerio = extrapleural air within lower mediastinum between parietal pleura + diaphragm (usually on left) subcutaneous emphysema of the neck
subcutaneous emphysema of the neck delayed widening of the mediastinum (secondary to mediastinitis)
delayed widening of the mediastinum (secondary to mediastinitis) hydrothorax (after rupture into pleural cavity), usually unilateral on left side
hydrothorax (after rupture into pleural cavity), usually unilateral on left side hydropneumothorax (often not initially seen)
hydropneumothorax (often not initially seen) left lower lobe atelectasis
left lower lobe atelectasis confirmation with contrast study (90% of contrast esophagograms are positive)
confirmation with contrast study (90% of contrast esophagograms are positive)
CT:
 focal extraluminal air collection at site of tear (92%; most useful sign)
focal extraluminal air collection at site of tear (92%; most useful sign) periesophageal/mediastinal hematoma/fluid (92%)
periesophageal/mediastinal hematoma/fluid (92%) pleural effusion (75%)
pleural effusion (75%) esophageal wall thickening
esophageal wall thickening extravasation of oral contrast material
extravasation of oral contrast material
P.829
Esophagography with:
water-soluble contrast material (10% false-negative results)
barium (if result with water-soluble material negative)
| Cx: | (1) Acute mediastinitis (2) Obstruction of SVC (3) Mediastinal abscess |
| Prognosis: | 20 60% mortality |
Upper/Midesophageal Perforation
| Location: | at level of cricopharyngeus muscle (most frequent) |
 widening of upper mediastinum
widening of upper mediastinum right-sided hydrothorax
right-sided hydrothorax
Distal Esophageal Perforation
| Incidence: | more common (but not in blunt chest trauma) |
| Cause: | biopsy, dilatation of stricture, Boerhaave syndrome |
 left-sided hydrothorax
left-sided hydrothorax little mediastinal changes
little mediastinal changes
Esophageal Varices
= plexuses formed by dilated subepithelial veins + submucosal veins + dilated venae commitantes of the vagus nerves outside the tunica muscularis
Anatomy:
anterior branch connected to left gastric vein
posterior branch connected to azygos + hemiazygos system
Examination Technique:
small amount of barium (not to obscure varices)
relaxation of esophagus (not to compress varices): refrain from swallowing because succeeding swallow initiates a primary peristaltic wave that lasts for 10 30 seconds; sustained Valsalva maneuver precludes from swallowing
in LAO projection with patient recumbent/in Trendelenburg position Valsalva maneuver/deep inspiration
Plain film:
 lobulated masses in posterior mediastinum (visible in 5 8% of patients with varices)
lobulated masses in posterior mediastinum (visible in 5 8% of patients with varices) silhouetting of descending aorta
silhouetting of descending aorta abnormal convex contour of azygoesophageal recess at level of gastroesophageal junction
abnormal convex contour of azygoesophageal recess at level of gastroesophageal junction
UGI:
 thickened sinuous interrupted mucosal folds (earliest sign)
thickened sinuous interrupted mucosal folds (earliest sign) tortuous radiolucencies of variable size + location
tortuous radiolucencies of variable size + location worm-eaten smooth lobulated filling defects
worm-eaten smooth lobulated filling defects findings may be accentuated after sclerotherapy
findings may be accentuated after sclerotherapy
CT:
 thickened esophageal wall + lobulated outer contour
thickened esophageal wall + lobulated outer contour scalloped esophageal luminal masses
scalloped esophageal luminal masses right-/left-sided soft-tissue masses (= paraesophageal varices)
right-/left-sided soft-tissue masses (= paraesophageal varices) marked enhancement following dynamic CT
marked enhancement following dynamic CT
| Cx: | bleeding in 28% within 3 years; exsanguination in 10 15% |
| DDx: | varicoid carcinoma of esophagus |
Uphill Esophageal Varices
= collateral blood flow from portal vein via azygos vein into SVC (usually lower esophagus drains via left gastric vein into portal vein)
Cause:
intrahepatic obstruction from cirrhosis
 In <5% of patients with portal hypertension
In <5% of patients with portal hypertension
splenic vein thrombosis (usually gastric varices)
obstruction of hepatic veins
IVC obstruction below hepatic veins
IVC obstruction above hepatic vein entrance/CHF
marked splenomegaly/splenic hemangiomatosis (rare)
 varices in lower half of esophagus
varices in lower half of esophagus
Downhill Esophageal Varices
= collateral blood flow from SVC via azygos vein into IVC/portal venous system (upper esophagus usually drains via azygos vein into SVC)
| Cause: | obstruction of superior vena cava distal to entry of azygos vein (= superior vena cava syndrome) most commonly due to lung cancer, lymphoma, retrosternal goiter, thymoma, mediastinal fibrosis |
 varices in upper 1/3 of esophagus
varices in upper 1/3 of esophagus
Esophageal Web
= complete/incomplete circumferential narrowing caused by 1 2-mm thick (vertical length) mucosal membrane projecting into esophageal lumen; covered by squamous epithelium on superior + inferior surfaces
| Age: | middle-aged females |
Association with:
Plummer-Vinson syndrome = Paterson-Kelly syndrome (iron deficiency anemia, stomatitis, glossitis, dysphagia, thyroid disorder, spoon-shaped nails)
Cause:
| mnemonic: | BIEP |
B-ring (Schatzki ring)
Idiopathic (= transverse mucosal fold)
Epidermolysis bullosa
Plummer-Vinson disease
| Path: | hyperkeratosis + chronic inflammation of submucosa |
mostly asymptomatic (unless severely stenosing)
| Location: | in cervical esophagus near cricopharyngeus (most common) > thoracic esophagus; occasionally multiple |
 visualized during maximal distension (in one-tenth of a second)
visualized during maximal distension (in one-tenth of a second) arises at right angles from anterior esophageal wall
arises at right angles from anterior esophageal wall thin delicate membrane of uniform thickness of <3 mm
thin delicate membrane of uniform thickness of <3 mm
| Cx: | high risk of upper esophageal + hypopharyngeal carcinoma |
| Rx: | (1) balloon dilatation (2) bougienage during esophagoscopy |
| DDx: | stricture (circumferential + thicker = 1 2-mm thick [vertical length] area of complete/incomplete circumferential narrowing |
P.830
Esophagitis
Acute Esophagitis
Cause:
| mnemonic: | CRIER |
Corrosives, Crohn disease
Reflux
Infection, Intubation
Epidermolysis bullosa
Radiation therapy
 thickened >3-mm-wide folds with irregular lobulated contour
thickened >3-mm-wide folds with irregular lobulated contour mucosal nodularity (= multiple ulcerations + intervening edema)
mucosal nodularity (= multiple ulcerations + intervening edema) erosions
erosions vertically oriented ulcers usually 3 10 mm in length
vertically oriented ulcers usually 3 10 mm in length inflammatory esophagogastric polyp = proximal gastric fold extending across esophagogastric junction (rare)
inflammatory esophagogastric polyp = proximal gastric fold extending across esophagogastric junction (rare) abnormal motility
abnormal motility
Candida Esophagitis
= MONILIASIS = CANDIDIASIS
 Most common cause of infectious esophagitis!
Most common cause of infectious esophagitis!
| Organism: | C. albicans, C. tropicalis; endogenous (majority)/transmitted by another human/animal; often discovered in diseased skin, GI tract, sputum, female genital tract, urine with an indwelling Foley catheter |
Predisposed:
individuals with depressed immunity: hematologic disease, renal transplant, leukemia, chronic debilitating disease, diabetes mellitus, steroids, chemotherapy, radiotherapy, AIDS
 Most common type of fungi found with opportunistic infections!
Most common type of fungi found with opportunistic infections!
delayed esophageal emptying: scleroderma, strictures, achalasia, S/P fundoplication
antibiotics
| Path: | patchy, creamy-white plaques covering a friable erythematous mucosa |
| Histo: | mucosal plaques = necrotic epithelial debris + fungal colonies |
dysphagia (= difficulty swallowing)
severe odynophagia (= painful swallowing from segmental spasm)
intense retro-/substernal pain
associated with thrush (= oropharyngeal moniliasis) in 20 50 80%
| Location: | predilection for upper 1/2 of esophagus |
 involvement of long esophageal segments:
involvement of long esophageal segments: cobblestone appearance = mucosal nodularity in early stage (from growth of colonies on surface)
cobblestone appearance = mucosal nodularity in early stage (from growth of colonies on surface) longitudinal plaques = grouping of tiny 1 2-mm nodular filling defects with linear orientation (= heaped-up areas of mucosal plaques)
longitudinal plaques = grouping of tiny 1 2-mm nodular filling defects with linear orientation (= heaped-up areas of mucosal plaques) shaggy/fuzzy/serrated contour (from coalescent plaques, pseudomembranes, erosions, ulcerations, intramural hemorrhage) in fulminant candidiasis of AIDS
shaggy/fuzzy/serrated contour (from coalescent plaques, pseudomembranes, erosions, ulcerations, intramural hemorrhage) in fulminant candidiasis of AIDS
 narrowed lumen (from spasm, pseudomembranes, marked edema)
narrowed lumen (from spasm, pseudomembranes, marked edema) intramural diverticulosis = multiple tiny indentations + protrusions
intramural diverticulosis = multiple tiny indentations + protrusions sluggish/absent primary peristalsis
sluggish/absent primary peristalsis strictures (rare)
strictures (rare) mycetoma resembling large intraluminal tumor (rare)
mycetoma resembling large intraluminal tumor (rare)
| Diagnostic sensitivity: | endoscopy (97%), double contrast (88%), single contrast (55%) |
| Cx: | (1) Systemic candidiasis ( microabscesses in liver, spleen, kidney) (2) Gastric bezoar due to large fungus ball (after long-standing esophageal candidiasis) |
| Rx: | ketoconazole/fluconazole |
| DDx: | glycogen acanthosis, reflux esophagitis, superficial spreading carcinoma, artifacts (undissolved effervescent crystals, air bubbles, retained food particles), herpes esophagitis, acute caustic ingestion, intramural pseudo-diverticulosis, squamous papillomatosis, Barrett esophagus, epidermolysis bullosa, varices |
Caustic Esophagitis
= CORROSIVE ESOPHAGITIS
Corrosive agents:
lye (sodium hydroxide), washing soda (sodium carbonate), household cleaners, iodine, silver nitrate, household bleaches, Clinitest tablets (tend to be neutralized by gastric acid)
 Severity of injury dependent on contact time + concentration of corrosive material!
Severity of injury dependent on contact time + concentration of corrosive material!
| Associated with: | injury to pharynx + stomach (7 8%): antral burns more common with acid (buffering effect of gastric acid on alkali) |
| Location: | middle + lower thirds of esophagus |
| Stage I: | acute necrosis from protein coagulation mucosal blurring (edema) diffusely atonic + dilated esophagus tertiary contractions/spasm |
| Stage II: | frank ulceration in 3 5 days ulceration + pseudomembranes |
| Stage III: | scarring + stricture from fibroblastic activity long segmental stricture after 10 days when acute edema subsides (7 30%) |
| Cx: | (1) Esophageal/gastric perforation during ulcerative stage (2) Squamous cell carcinoma in injured segment |
| Rx: | dilatation procedure/esophageal replacement surgery |
Chronic Esophagitis
 luminal narrowing with tapered transition to normal + proximal dilatation
luminal narrowing with tapered transition to normal + proximal dilatation circumferential/eccentric stricture
circumferential/eccentric stricture sacculations = pseudodiverticula
sacculations = pseudodiverticula
Drug-induced Esophagitis
= contact esophagitis due to oral medications = pill esophagitis
| Agents: | antibiotics (tetracycline, doxycycline), quinidine, potassium chloride, nonsteroidal antiinflammatory agents (aspirin), ascorbic acid, alprenolol chloride, emepronium bromide, alendronate (= inhibitor of osteoclastic activity) |
P.831
severe odynophagia
history of taking medication with little/no water immediately before going to bed
rapid clinical improvement after withdrawal of offending agent
| Location: | midesophagus at site of normal extrinsic impressions by aortic arch/left mainstem bronchus/left atrium |
 localized cluster of tiny ulcers distributed circumferentially (most commonly)
localized cluster of tiny ulcers distributed circumferentially (most commonly) superficial solitary/several discrete ulcers
superficial solitary/several discrete ulcers
| Prognosis: | ulcers heal within 7 10 days after cessation of offending medication |
| DDx: | herpes esophagitis (immunosuppressed patient, less localized); reflux esophagitis (heartburn, distal esophagus near esophagogastric junction) |
Reflux Esophagitis
= esophageal inflammation secondary to reflux of acid-peptic contents of the stomach; reflux occurs if resting pressure of LES <5 mm Hg (may be normal event if followed by rapid clearing)
| Prevalence: | in 20% of gastroesophageal reflux |
| Histo: | basal cell hyperplasia with wall thickening + thinning of epithelium, mucosal edema + erosions, inflammatory infiltrate |
| Determinants: | (1) Frequency of reflux (2) Adequacy of clearing mechanism (3) Volume of refluxed material (4) Potency of refluxed material (5) Tissue resistance |
Reflux preventing features:
Lower esophageal sphincter
Phrenoesophageal membrane
Length of subdiaphragmatic esophagus
Gastroesophageal angle of His (70 110 )
| May be associated with: | sliding hiatal hernia (in most patients), scleroderma, nasogastric intubation |
heartburn, epigastric discomfort
choking, globus hystericus
retrosternal pain
thoracic/cervical dysphagia
| Site: | usually lower 1/3/lower 1/2 with continuous disease extending proximally from GE junction |
 segmental esophageal narrowing (edema/spasm/stricture)
segmental esophageal narrowing (edema/spasm/stricture) poorly defined tiny mucosal elevations ( mucosal granularity ) on thickened/nodular longitudinal folds (mucosal edema + inflammation) in early stages
poorly defined tiny mucosal elevations ( mucosal granularity ) on thickened/nodular longitudinal folds (mucosal edema + inflammation) in early stages single marginal ulcer/erosion at or adjacent to gastroesophageal junction
single marginal ulcer/erosion at or adjacent to gastroesophageal junction multiple areas of superficial ulceration in distal esophagus
multiple areas of superficial ulceration in distal esophagus prominent mucosal fold ending in polypoid protuberance within hiatal hernia/cardia
prominent mucosal fold ending in polypoid protuberance within hiatal hernia/cardia interruption of primary peristalsis at inflamed segment
interruption of primary peristalsis at inflamed segment nonperistaltic waves in distal esophagus following deglutition (85%)
nonperistaltic waves in distal esophagus following deglutition (85%) incomplete relaxation of LES (75%), incompetent sphincter (33%)
incomplete relaxation of LES (75%), incompetent sphincter (33%) acid test = abnormal motility elicited by acid barium (pH 1.7)
acid test = abnormal motility elicited by acid barium (pH 1.7) felinization = transverse ridges of esophagus secondary to contraction of muscularis mucosae (similar to cat esophagus)
felinization = transverse ridges of esophagus secondary to contraction of muscularis mucosae (similar to cat esophagus)
NUC (pertechnetate):
 esophageal activity (Barrett esophagus similar to ectopic gastric mucosa)
esophageal activity (Barrett esophagus similar to ectopic gastric mucosa)
Reflux tests:
Reflux of barium in RPO position, may be elicited by coughing/deep respiratory movements/swallowing of saliva + water/anteflexion in erect position: only in 50% accurate
Water-siphon test: in 5% false negative; large number of false positives
Tuttle test = measurement of esophageal pH: 96% accurate
Radionuclide gastroesophageal reflux test (typically combined with gastric emptying test):
Technique: ROI drawn over distal esophagus + compared with time-activity curve over stomach, scaled to 4%  esophageal activity >4% stomach activity
esophageal activity >4% stomach activity
Cx of reflux:
from acid + pepsin acting on esophageal mucosa:
Motility disturbance
Stricture
Schatzki ring
Barrett esophagus
Iron-deficiency anemia
Reflux/peptic esophagitis
from aspiration of gastric contents
Acute aspiration pneumonia
Mendelson syndrome
Pulmonary fibrosis
Viral Esophagitis
| Predisposed: | immunocompromised, eg, underlying malignancy, debilitating illness, radiation treatment, steroids, chemotherapy, AIDS |
Cytomegalovirus Esophagitis
| Organism: | member of herpesvirus group |
| Associated with: | AIDS |
severe odynophagia
 diffusely normal mucosal background
diffusely normal mucosal background one/more giant ovoid flat ulcers (up to several cm in size) near gastroesophageal junction
one/more giant ovoid flat ulcers (up to several cm in size) near gastroesophageal junction discrete small superficial ulcers indistinguishable from herpes esophagitis (uncommon)
discrete small superficial ulcers indistinguishable from herpes esophagitis (uncommon)
| Rx: | ganciclovir (relatively toxic) |
| Dx: | endoscopic brushings, biopsy specimen, cultures |
Herpes Esophagitis
 2nd most common cause of opportunistic infection!
2nd most common cause of opportunistic infection!
| Organism: | Herpes simplex virus type I (DNA core virus) secreted in saliva of 2% of healthy population |
| Age: | 15 30 years; usually males |
| Predisposed: | immunosuppressed patient |
history of recent exposure to sexual partners with herpetic lesions on lips/buccal mucosa
flulike prodrome of 3 10 days (headaches, fever, sore throat, upper respiratory symptoms, myalgia)
severe acute dysphagia/odynophagia
P.832
| May be associated with: | oropharyngeal herpetic lesions/oropharyngeal candidiasis |
| Location: | midesophagus (level of left main bronchus) |
 initially vesicles/blisters that subsequently rupture
initially vesicles/blisters that subsequently rupture multiple small discrete superficial punctate/round/linear/serpentine/stellate (often diamond-shaped ) ulcers surrounded by radiolucent halos of edematous mucosa (in >50%)
multiple small discrete superficial punctate/round/linear/serpentine/stellate (often diamond-shaped ) ulcers surrounded by radiolucent halos of edematous mucosa (in >50%) intervening mucosa normal (without plaques)
intervening mucosa normal (without plaques) multiple plaquelike lesions (only with severe infection)
multiple plaquelike lesions (only with severe infection)
| Dx: | rising serum titer for HSV type I, viral culture, biopsy (immunofluorescent staining for HSV antigen, demonstration of intranuclear inclusions) |
| Rx: | oral/intravenous acyclovir |
| Prognosis: | resolution of symptoms in 3 14 days |
| DDx: | drug-induced esophagitis, Crohn disease, esophageal intramural pseudodiverticulosis |
Human Immunodeficiency Virus Esophagitis
maculopapular rash + ulcers of soft palate (occasionally)
recent seroconversion/known AIDS
 one/more giant (>1 cm) flat ovoid/diamond-shaped ulcers (at time of seroconversion) indistinguishable from CMV esophagitis
one/more giant (>1 cm) flat ovoid/diamond-shaped ulcers (at time of seroconversion) indistinguishable from CMV esophagitis
| Dx: | per exclusion (brushings, biopsies, cultures negative for CMV) |
| Rx: | oral steroids |
| DDx: | CMV esophagitis, mycobacterial esophagitis, actinomycosis, potassium chloride, quinidine, caustic ingestion, nasogastric intubation, radiation therapy, endoscopic sclerotherapy |
Familial Adenomatous Polyposis
= FAMILIAL MULTIPLE POLYPOSIS
= autosomal dominant disease with 80% penetrance (gene for familial polyposis localized on chromosome 5); sporadic occurrence in 1/3
| Incidence: | 1:7,000 to 1:24,000 live births |
| Histo: | tubular/villotubular adenomatous polyps; usually about 1,000 adenomas |
| Age: | polyps appear around puberty |
family history of colonic polyps (66%)
 Screening of family members after puberty!
Screening of family members after puberty!
clinical symptoms begin during 3rd 4th decade (range 5 55 years)
vague abdominal pain, weight loss
diarrhea, bloody stools
protein-losing enteropathy (occasionally)
| Associated with: | (1) Hamartomas of stomach in 49% (2) Adenomas of duodenum in 25% (3) Periampullary carcinoma |
 carpet of polyps = myriad of 2 3 mm (up to 2 cm) polypoid lesions
carpet of polyps = myriad of 2 3 mm (up to 2 cm) polypoid lesions@ Colon (100%): more numerous in distal colon; always affecting rectum
 normal haustral pattern
normal haustral pattern
@ Stomach (5%)
@ Small bowel (<5%)
| Cx: | malignant transformation of adenomas in: colon > stomach > small bowel (in 12% by 5 years; in 30% by 10 years; in 100% by 20 years after diagnosis; age at carcinomatous development usually 20 40 years; multiple carcinomas in 48%) 331-fold increased risk of small bowel adenocarcinoma compared to general population after colectomy Periampullary carcinoma is the most common cause of death after prophylactic colectomy! |
| Rx: | prophylactic total colectomy in late teens/early twenties before symptoms develop (1) Permanent ileostomy (2) Continent endorectal pull-through pouch (3) Kock pouch (= distal ileum formed into a one-way valve by invaginating the bowel at skin site) |
| DDx: | other polyposes, lymphoid hyperplasia, lymphosarcoma, ulcerative colitis with inflammatory pseudopolyps |
Gallstone Ileus
| Incidence: | 0.4 5% of all intestinal obstructions (20% of obstruction in patients >65 years; 24% of obstructions in patients >70 years); develops in <1% of patients with cholelithiasis; in 1 of 6 perforations; risk increases with age |
| Etiology: | biliary disease (90%), peptic ulcer disease, cancer, trauma |
| Age: | average 65 75 years; M:F = 1:4 1:7 |
previous history of gallbladder disease
intermittent episodes of acute colicky abdominal pain (20 30%)
nausea, vomiting, fever, distension, obstipation
 Rigler triad on plain film (in 10%):
Rigler triad on plain film (in 10%):Partial/complete intestinal obstruction (usually small bowel), string of rosary beads = multiple small amounts of air trapped between dilated + stretched valvulae conniventes (in 86%)
Gas in biliary tree (in 69%)
Ectopic calcified gallstone (in 25%): stones are commonly >2.5 cm in diameter
 change in position of previously identified gallstone
change in position of previously identified gallstone
UGI/BE:
 well-contained localized barium collection lateral to first portion of duodenum (barium-filled collapsed GB + possibly biliary ducts)
well-contained localized barium collection lateral to first portion of duodenum (barium-filled collapsed GB + possibly biliary ducts)Fistulous communication:
cholecystoduodenal (60%), choledochoduodenal, cholecystocolic, choledochocolic, cholecystogastric
 identification of site of obstruction: terminal ileum (60 70%), proximal ileum (25%), distal ileum (10%), pylorus, sigmoid, duodenum (Bouveret syndrome)
identification of site of obstruction: terminal ileum (60 70%), proximal ileum (25%), distal ileum (10%), pylorus, sigmoid, duodenum (Bouveret syndrome)
| Cx: | recurrent gallstone ileus in 5 10% (additional silent calculi more proximally) |
| Prognosis: | high mortality |
Gangliocytic Paraganglioma
= rare benign tumor of the GI tract
| Frequency: | <100 cases reported |
| Origin: | pancreatic endocrine rest that remained when the ventral primordium rotated around the duodenum |
| Age: | 50 60 years of age; M:F = 2:1 |
| Location: | almost exclusively in 2nd portion of duodenum near the ampulla of Vater on the medial/lateral wall of duodenum |
P.833
GI hemorrhage, abdominal pain
 polypoid smooth-surfaced intraluminal mass
polypoid smooth-surfaced intraluminal mass homogeneously enhancing mural/extrinsic solid mass of soft-tissue attenuation
homogeneously enhancing mural/extrinsic solid mass of soft-tissue attenuation well-circumscribed hypoechoic mass contiguous with bowel
well-circumscribed hypoechoic mass contiguous with bowel no biliary duct dilatation
no biliary duct dilatation
| DDx: | adenocarcinoma (biliary duct dilatation, hypovascular), leiomyosarcoma (cystic internal hemorrhage/necrosis), hemangioma, duplication cyst, choledochal cyst, lipoma, hamartoma, inflammatory fibroid polyp (distal small bowel), lymphoma (isolated in stomach and ileum) |
Gardner Syndrome
= autosomal dominant disease ( variant of familial polyposis) characterized by a triad of
colonic polyposis
osteomas
soft-tissue tumors
| Cause: | adenomatous polyposis gene on chromosome 5-q21; in 20% new mutations Familial polyposis + Gardner syndrome may occur in the same family! |
| Histo: | adenomatous polyps |
| Age: | 15 30 years (2 months 70 years) |
| Associated with: | MEA complex |
periampullary/duodenal carcinoma (12%)
papillary thyroid carcinoma (often multicentric)
adrenal adenoma/carcinoma
parathyroid adenoma
pituitary chromophobe adenoma
carcinoid, adenoma of small bowel
retroperitoneal leiomyoma
 Extraintestinal manifestations occur usually earlier than in intestinal polyposis!
Extraintestinal manifestations occur usually earlier than in intestinal polyposis!skin pigmentation
cramping abdominal pain
weight loss, diarrhea
@ Polyposis
Location: colon (100%), stomach (5 68%), duodenum (90%), small bowel (<5%)  multiple colonic polyps appearing during puberty, increasing in number during 3rd 4th decade
multiple colonic polyps appearing during puberty, increasing in number during 3rd 4th decade lymphoid hyperplasia of terminal ileum
lymphoid hyperplasia of terminal ileum hamartomas of stomach
hamartomas of stomach intussusception
intussusception
Cx: small bowel/colonic obstruction @ Soft-tissue tumors
sebaceous/epidermoid inclusion cysts (scalp, back, face, extremities)
fibroma, lipoma, leiomyoma, neurofibroma
desmoid tumors (3 29%); peritoneal adhesions (desmoplastic tendency); mesenteric fibrosis, retroperitoneal fibrosis
urinary tract obstruction
mammary fibromatosis
marked keloid formation, hypertrophied scars (anterior abdominal wall) arise 1 3 years after surgery
@ Osteomatosis of membranous bone (50%)
Location: calvarium, mandible (81%), maxilla, ribs, long bones @ Long bones
 localized wavy cortical thickening/exostoses
localized wavy cortical thickening/exostoses slight shortening + bowing
slight shortening + bowing
@ Teeth
 odontoma, unerupted/supernumerary teeth, hypercementosis
odontoma, unerupted/supernumerary teeth, hypercementosis tendency toward numerous caries (dental prosthesis at early age)
tendency toward numerous caries (dental prosthesis at early age)
| Cx: | malignant transformation of colonic polyps in 100% (average age at death is 41 years if untreated) |
| Prophylaxis: | gastrointestinal surveillance, thyroid screening, ophthalmologic evaluation for retinal pigmentation anomalies; screening of family members starting at age 15 |
| Rx: | prophylactic total colectomy at about 20 years of age |
Gastric Carcinoma
 3rd most common GI malignancy after colorectal + pancreatic cancer, 6th leading cause of cancer deaths
3rd most common GI malignancy after colorectal + pancreatic cancer, 6th leading cause of cancer deaths
| Prevalence: | declining; 24,000 cases/year in USA |
| Risk factors: | smoking, nitrites, nitrates, pickled vegetables |
Predisposing factors:
H. pylori gastritis, chronic atrophic gastritis, adenomatous + villous polyp (7 27% are malignant), gastrojejunostomy, partial gastrectomy (Billroth II > Billroth I), pernicious anemia (risk factor of 2), M n trier disease ( )
| Histo: | adenocarcinoma (95%); rarely squamous cell carcinoma/adenoacanthoma |
Staging:
| T1 | tumor limited to mucosa/submucosa |
| T2 | tumor involves muscle/serosa |
| T3 | tumor penetrates through serosa |
| T4a | invasion of adjacent contiguous tissues |
| T4b | invasion of adjacent organs, diaphragm, abdominal wall |
| N1 | involvement of perigastric nodes within 3 cm of primary along greater/lesser curvature |
| N2 | involvement of regional nodes >3 cm from primary along branches of celiac axis |
| N3 | paraaortic, hepatoduodenal, retropancreatic, mesenteric nodes |
| M1 | distant metastases |
| Location: | mostly distal third of stomach + cardia; 60% on lesser curvature, 10% on greater curvature; esophagogastric junction in 30%; transpyloric spread in 5 25% (for lymphoma 40%) |
Probability of malignancy of an ulcer:
at lesser curvature 10 15%, at greater curvature 70%, in fundus 90%
Morphology:
Polypoid/fungating carcinoma
Ulcerating/penetrating carcinoma (70%)
Infiltrating/scirrhous carcinoma (5 15%)
= linitis plastica
Histo: frequently signet ring cell type + increase in fibrous tissue Location: antrum, fundus + body (38%) P.834
 firmness, rigidity, reduced capacity of stomach, aperistalsis in involved area
firmness, rigidity, reduced capacity of stomach, aperistalsis in involved area granular/polypoid folds with encircling growth
granular/polypoid folds with encircling growth
Superficial spreading carcinoma
= confined to mucosa/submucosa; 5-year survival of 90%
 patch of nodularity
patch of nodularity little loss of elasticity
little loss of elasticity
Advanced bulky carcinoma
GI bleeding, abdominal pain, weight loss
UGI:
 rigidity
rigidity filling defect
filling defect amputation of folds ulceration stenosis
amputation of folds ulceration stenosis miliary/punctate calcifications (mucinous adenocarcinoma)
miliary/punctate calcifications (mucinous adenocarcinoma)
CT:
 irregular nodular luminal surface
irregular nodular luminal surface asymmetric thickening of folds
asymmetric thickening of folds mass of uniform density/varying attenuation
mass of uniform density/varying attenuation wall thickness >6 mm with gas distension + 13 mm with positive contrast material distension:
wall thickness >6 mm with gas distension + 13 mm with positive contrast material distension: diffuse low attenuation in mucinous carcinoma
diffuse low attenuation in mucinous carcinoma
 increased density in perigastric fat
increased density in perigastric fat enhancement exclusively in linitis plastica type
enhancement exclusively in linitis plastica type nodules of serosal surface (= dilated surface lymphatics)
nodules of serosal surface (= dilated surface lymphatics) diameter of esophagus at gastroesophageal junction larger than adjacent aorta (DDx: hiatal hernia)
diameter of esophagus at gastroesophageal junction larger than adjacent aorta (DDx: hiatal hernia) lymphadenopathy below level of renal pedicle (3%)
lymphadenopathy below level of renal pedicle (3%)
Metastases:
along peritoneal ligaments
gastrocolic lig.: transverse colon, pancreas
gastrohepatic + hepatoduodenal lig.: liver
local lymph nodes
hematogenous: liver (most common), adrenals, ovaries, bone (1.8%), lymphangitic carcinomatosis of lung (rare)
peritoneal seeding:
on rectal wall = Blumer shelf on ovaries = Krukenberg tumor left supraclavicular lymph node = Virchow node
Prognosis:
overall 5-year survival rate of 5 18%, mean survival time of 7 8 months;
| 85% | 5-year survival in stage T1 |
| 52% | 5-year survival in stage T2 |
| 47% | 5-year survival in stage T3 |
| 17% | 5-year survival in stage N1-2 |
| 5% | 5-year survival in stage N3 |
Early Gastric Cancer (20%)
= invasion limited to mucosa + submucosa (T1 lesion) regardless of lymph node involvement
Classification of Japan Research Society for Gastric Cancer:
| Type I | protruded type = >5 mm in height with protrusion into gastric lumen (10 20%) |
| Type II | superficial type = <5 mm in height |
| IIa | slightly elevated surface (10 20%) |
| IIb | flat/almost unrecognizable (2%) |
| IIc | slightly depressed surface (50 60%) |
| Type III | excavated/ulcerated type (5 10%) |
Advanced Gastric Cancer (T2 lesion and higher)
Bormann classification:
| Type 1 | broad-based elevated polypoid lesion |
| Type 2 | elevated lesion + ulceration + well-demarcated margin |
| Type 3 | elevated lesion + ulceration + ill-defined margin |
| Type 4 | ill-defined flat lesion |
| Type 5 | unclassified, no apparent elevation |
Gastric Diverticulum
 Stomach is least common site of diverticula
Stomach is least common site of diverticula
| Incidence: | 1:600 2,400 of UGI studies |
| Etiology: | (a) traction secondary to scarring/periantral inflammation = true diverticulum (b) pulsion (less common) = false diverticulum |
| Age: | beyond 40 years |
| Often associated with: | aberrant pancreas in antral location |
| Location: | juxtacardiac on posterior wall (75%), prepyloric (15 22%), greater curve (3%) |
 pliability + varying degrees of distension
pliability + varying degrees of distension NO mass, edema or rigidity of adjacent folds
NO mass, edema or rigidity of adjacent folds
| DDx: | small ulcer in intramural-extramucosal mass |
Gastric Polyp
| Incidence: | 1.5 5%, most common benign gastric tumor |
| Associated with: | hyperacidity + ulcers, chronic atrophic gastritis, gastric carcinoma |
NONNEOPLASTIC
Inflammatory polyp of stomach (75 90%)
= HYPERPLASTIC POLYP = REGENERATIVE POLYP
Histo: cystically dilated glands lined by gastric epithelium + acute and chronic inflammatory infiltrates in lamina propria Associated with: chronic atrophic gastritis, pernicious anemia Location: predominantly in fundus + body; usually multiple  sharply delineated polyp with smooth circular border
sharply delineated polyp with smooth circular border Mexican hat sign = stalk seen en face overlying the head of polyp
Mexican hat sign = stalk seen en face overlying the head of polyp sessile/pedunculated
sessile/pedunculated usually <2 cm in diameter without progression
usually <2 cm in diameter without progression no contour defect of stomach
no contour defect of stomach
Prognosis: no malignant potential Hamartomatous polyp of stomach (rare)
Histo: densely packed gastric glands + bundles of smooth muscle Associated with: Peutz-Jeghers syndrome  sessile/pedunculated
sessile/pedunculated usually <2 cm in diameter
usually <2 cm in diameter
Retention polyp of stomach (rare)
Histo: dilated cystic glands + stroma Associated with: Cronkhite-Canada syndrome
NEOPLASTIC
Adenomatous polyp of stomach (10 20%)
= true neoplasm with malignant potential (10 80%, increasing with size)
Age: increasing incidence with age; M:F = 2:1 Histo: intestinal metaplasia (common) + marked cellular atypism Associated with: Gardner syndrome; coexistent with gastric carcinoma in 35% Location: more commonly in antrum (antrum spared in Gardner syndrome) P.835
 broad-based elliptical/mushroom-shaped polyp pedicle; usually solitary
broad-based elliptical/mushroom-shaped polyp pedicle; usually solitary usually >2 cm in diameter (in 80%)
usually >2 cm in diameter (in 80%) smooth/irregular lobulated contour
smooth/irregular lobulated contour
Villous polyp of stomach (rare)
 trabeculated/lobulated slightly irregular contour
trabeculated/lobulated slightly irregular contour
Cx: malignant transformation
| DDx: | (1) M n trier disease (antrum spared) (2) Eosinophilic polyp (peripheral eosinophilia, linitis plastica appearance, small bowel changes) (3) Lymphoma (4) Carcinoma |
Gastric Ulcer
Benign Gastric Ulcer
95% of all gastric ulcers
Cause:
HORMONAL
Zollinger-Ellison syndrome
Hyperparathyroidism (in 1.3 24%)
duodenum:stomach = 4:1; M:F = 3:1
 Duodenal ulcers predominate in females!
Duodenal ulcers predominate in females! Gastric ulcers predominate in males!
Gastric ulcers predominate in males!absence of gastric hypersecretion
Steroid-induced ulcer
gastric > duodenal location;
frequently multiple + deep ulcers;
commonly associated with erosions
bleeding (in 1/3)
Stress, severe prolonged illness
Cerebral disease = Cushing ulcer
Curling ulcer (burns) (in 0.09 2.6%)
Retained gastric antrum
Uremia
INFLAMMATION
Peptic ulcer disease
Gastritis
Radiation-induced ulcer
Intubation
Stasis ulcer proximal to pyloric/duodenal obstruction
BENIGN MASS
Leiomyoma
Granulomatous disease
Pseudolymphoma (lymphoid hyperplasia)
DRUGS
ASA: greater curvature
Pathophysiology:
disrupted mucosal barrier (Helicobacter pylori) with vulnerability to acid + secretion of large volume of gastric juice containing little acid
| Incidence: | 5:10,000; 100,000/year (United States) |
| Age peak: | 55 65 years; M:F = 1:1 |
Multiplicity:
multiple in 2 8% (17 24% at autopsy), especially in patients on aspirin
coexistent duodenal ulcer in 5 64%; gastric:duodenal = 1:3 (adults) = 1:7 (children)
abdominal pain: in 30% at night, in 25% precipitated by food
| Location: | lesser curvature at junction of corpus + antrum within 7 cm from pylorus; proximal half of stomach in older patients (geriatric ulcer); adjacent to GE junction within hiatal hernia |
 ulcer size usually <2 cm (range 1 250 mm); in 4% >40 mm
ulcer size usually <2 cm (range 1 250 mm); in 4% >40 mm round/ovoid/linear shape
round/ovoid/linear shape Haudek niche = conical/collar button-shaped barium collection projecting outside gastric contour (profile view)
Haudek niche = conical/collar button-shaped barium collection projecting outside gastric contour (profile view) Hampton line = 1-mm thin straight lucent line traversing the orifice of the ulcer niche (seen on profile view + with little gastric distension) = ledge of touching overhanging gastric mucosa of undermined benign ulcer
Hampton line = 1-mm thin straight lucent line traversing the orifice of the ulcer niche (seen on profile view + with little gastric distension) = ledge of touching overhanging gastric mucosa of undermined benign ulcer ulcer collar = smooth thick lucent band interposed between the niche and gastric lumen (thickened rim of edematous gastric wall) in well-distended stomach
ulcer collar = smooth thick lucent band interposed between the niche and gastric lumen (thickened rim of edematous gastric wall) in well-distended stomach ulcer mound = smooth, sharply delineated, gently sloping extensive tissue mass surrounding a benign ulcer (edema + lack of wall distensibility) in well-distended stomach
ulcer mound = smooth, sharply delineated, gently sloping extensive tissue mass surrounding a benign ulcer (edema + lack of wall distensibility) in well-distended stomach ulcer crater = round/oval barium collection with smooth border on dependent side (en face view)
ulcer crater = round/oval barium collection with smooth border on dependent side (en face view) halo defect = wide lucent band symmetrically surrounding ulcer resembling extensive ulcer mound (viewed en face)
halo defect = wide lucent band symmetrically surrounding ulcer resembling extensive ulcer mound (viewed en face) ring shadow: ulcer on nondependent side (en face view)
ring shadow: ulcer on nondependent side (en face view) radiating thick folds extending directly to crater edge fusing with the effaced marginal fold of the ulcer collar/halo of ulcer mound
radiating thick folds extending directly to crater edge fusing with the effaced marginal fold of the ulcer collar/halo of ulcer mound incisura defect = smooth, deep, narrow, sharp indentation on greater curvature opposite a niche on lesser curvature at/slightly below the level of the ulcer (spastic contraction of circular muscle fibers)
incisura defect = smooth, deep, narrow, sharp indentation on greater curvature opposite a niche on lesser curvature at/slightly below the level of the ulcer (spastic contraction of circular muscle fibers)
| Prognosis: | healing in 50% by 3 weeks, in 100% by 6 8 weeks; slower healing in older patients; only complete healing proves benignancy |
| Cx: | bleeding, perforation, fistula Most common cause of gastrocolic fistula! |
| Gastric Ulcer | ||
|---|---|---|
| Sign | Benign | Malignant |
| Crater | round, ovoid | irregular |
| Radiating folds | symmetric | nodular, clubbed, fused |
| Areae gastricae | preserved | destroyed |
| Projection | outside lumen | inside lumen |
| Ulcer mound | smooth | rolled edge |
Malignant Gastric Ulcer
| Incidence: | 5% of ulcers are malignant |
Cause:
Gastric carcinoma
Lymphoma (2% of all gastric neoplasms)
 multiple ulcers with aneurysmal appearance
multiple ulcers with aneurysmal appearance
Leiomyosarcoma, neurogenic sarcoma, fibrosarcoma, liposarcoma
Metastases
hematogenic: malignant melanoma, breast cancer, lung cancer
per continuum: pancreas, colon, kidney
P.836
| Prognosis: | partial healing may occur |
| Location: | anywhere within stomach; fundal ulcers above level of cardia are usually malignant |
 ulcer location within gastric lumen, ie, not projecting beyond expected margin of stomach (profile view)
ulcer location within gastric lumen, ie, not projecting beyond expected margin of stomach (profile view) eccentrically located ulcer within the tumor
eccentrically located ulcer within the tumor irregularly shaped ulcer
irregularly shaped ulcer shallow ulcer with width greater than depth
shallow ulcer with width greater than depth nodular ulcer floor
nodular ulcer floor abrupt transition between normal mucosa + abnormal tissue at some distance (usually 2 4 cm) from ulcer edge
abrupt transition between normal mucosa + abnormal tissue at some distance (usually 2 4 cm) from ulcer edge rolled/rounded/shouldered edges surrounding ulcer
rolled/rounded/shouldered edges surrounding ulcer nodular irregular folds approaching ulcer with fused/clubbed/amputated tips
nodular irregular folds approaching ulcer with fused/clubbed/amputated tips rigidity/lack of distensibility
rigidity/lack of distensibility associated large irregular mass
associated large irregular mass Carman meniscus sign = curvilinear lens-shaped intraluminal form of crater with convexity of crescent toward gastric wall and concavity toward gastric lumen (profile view, usually under compression) found in specific type of ulcerating carcinoma, seen only infrequently; wall aspect can also be concave/flat
Carman meniscus sign = curvilinear lens-shaped intraluminal form of crater with convexity of crescent toward gastric wall and concavity toward gastric lumen (profile view, usually under compression) found in specific type of ulcerating carcinoma, seen only infrequently; wall aspect can also be concave/flat Kirklin meniscus complex = Carman sign (appearance of crater) + radiolucent slightly elevated rolled border
Kirklin meniscus complex = Carman sign (appearance of crater) + radiolucent slightly elevated rolled border
Gastric Varices
| Cause: | portal hypertension (varices seen in 2 78%); splenic vein obstruction (from pancreatitis, pancreatic carcinoma, pseudocyst) |
| Location: | (a) esophagogastric junction (most common) (b) along lesser curvature (in 11 75% of patients with portal hypertension/cirrhosis) |
Feeding vessels:
Left gastric vein (between splenic vein + stomach)
Short gastric veins (between spleen + fundus)
Retrogastric vein (between splenic vein + esophagogastric junction)
increased prevalence of portosystemic encephalopathy
 barium study: 65 89% rate of detection:
barium study: 65 89% rate of detection: lobulated folds/polypoid masses in fundus
lobulated folds/polypoid masses in fundus
 endoscopy: most practical method
endoscopy: most practical method splenic portography
splenic portography hepatofugal blood flow along SMV into left gastric + splenic vein
hepatofugal blood flow along SMV into left gastric + splenic vein
| Cx: | variceal bleeding in 3 10 36% Gastric varices bleed less frequently but more severely than esophageal varices! |
Gastric Volvulus
 SURGICAL EMERGENCY
SURGICAL EMERGENCY= abnormal degree of rotation of one part of stomach around another part, usually requires >180 twisting to produce complete obstruction
Degrees of rotation:
Partial Volvulus
= rotation of stomach <180 degrees without vascular compromise
Complete volvulus
= rotation of stomach >180 degrees
Etiology:
abnormality of suspensory ligaments
unusually long gastrohepatic + gastrocolic mesenteries
Anatomy of ligaments:
gastrohepatic at lesser curvature; gastrosplenic + gastrocolic at greater curvature; gastrophrenic at posterior fundus; attachment to esophagus at gastroesophageal junction; attachment to duodenum at pylorus
Predisposing factors:
sliding/paraesophageal hernia (33%), ligamentous laxity, eventration of diaphragm, phrenic nerve paralysis, splenic abnormalities (asplenia, polysplenia, splenomegaly, prior splenectomy)
| Age: | 40 50 years (in 20% in infants <1 year of age); M:F = 1:1 |
Types:
ORGANOAXIAL VOLVULUS (more common)
= rotation around a line from cardia to pylorus
more common in elderly
high correlation with hiatal hernia
 mirror-image stomach:
mirror-image stomach: reversal of locations of greater + lesser curvatures (in transversely oriented stomach)
reversal of locations of greater + lesser curvatures (in transversely oriented stomach) greater curvature to right of lesser curvature (in vertically oriented stomach)
greater curvature to right of lesser curvature (in vertically oriented stomach)
MESENTEROAXIAL VOLVULUS (less common)
= rotation around an axis from lesser to greater curvature coinciding with axis of mesenteric attachments
associated with severe obstruction + strangulation
 upside-down stomach (= antrum + pylorus superior to fundus + proximal body)
upside-down stomach (= antrum + pylorus superior to fundus + proximal body)
COMBINATION (rare)
Borchordt triad:
sudden onset of severe epigastric pain
intractable retching (= vigorous attempts to vomit) without production of vomitus
inability to pass nasogastric tube into stomach
chronic volvulus: asymptomatic/postprandial pain, belching, bloating, vomiting, early satiety
 massively distended stomach in LUQ extending into chest
massively distended stomach in LUQ extending into chest unexpected location of stomach gas bubble
unexpected location of stomach gas bubble air-fluid levels in mediastinum/upper abdomen
air-fluid levels in mediastinum/upper abdomen incomplete/absent entrance of barium into stomach
incomplete/absent entrance of barium into stomach displaced gastroesophageal junction
displaced gastroesophageal junction barium demonstrates area of twist
barium demonstrates area of twist
| Cx: | intramural emphysema, gastric ischemia, necrosis, perforation, peritonitis, shock, gastric ulceration, hemorrhage, pancreatic necrosis, omental avulsion, splenic rupture |
| Mortality: | 42 80% in acute volvulus; 10 13% in chronic volvulus |
| Rx: | open/laparoscopic gastropexy |
| DDx: | gastric atony, acute gastric dilatation, pyloric obstruction |
P.837
Gastritis
Corrosive Gastritis
Agents:
acid, formaldehyde
clinically usually silent
Location: esophagus usually unharmed, severe gastric damage, duodenum may be involved (newer potent materials cause atypical distribution) alkaline
Location: pylorus + antrum most frequently involved
ACUTE CHANGES (edema + mucosal sloughing)
 marked enlargement of gastric rugae + erosions/ulceration
marked enlargement of gastric rugae + erosions/ulceration complete cessation of motor activity
complete cessation of motor activity gas in portal venous system
gas in portal venous system
Cx: perforation CHRONIC CHANGES
 firm thick nonpliable wall
firm thick nonpliable wall stenotic/incontinent pylorus (if involved)
stenotic/incontinent pylorus (if involved) gastric outlet obstruction (cicatrization) after 3 10 weeks
gastric outlet obstruction (cicatrization) after 3 10 weeks
Emphysematous Gastritis
= rare but severe form of widespread phlegmonous gastritis subsequent to mucosal disruption characterized by gas in wall of stomach
Cause of mucosal disruption:
ingestion of toxic/corrosive substances (37%), alcohol abuse (22%), gastroenteritis (15%), recent abdominal surgery (15%), gastric infarction, necrotizing enterocolitis, ulcer, acute pancreatitis, adenocarcinoma of stomach, phytobezoar, leukemia, diabetes mellitus, disseminated strongyloidiasis, gastric mucormycosis, after ingestion of large amounts of carbonated beverages
| Histo: | bacterial invasion of submucosa + subserosa |
| Organism: | hemolytic streptococcus, Clostridium welchii, Clostridium perfringens, E. coli, S. aureus, enterobacter, P. aeruginosa |
explosive onset of severe abdominal pain
nausea, diarrhea, chills, fever, leukocytosis
bloody foul-smelling emesis PATHOGNOMONIC vomiting of a necrotic cast of stomach (due to dissection along plane of muscularis mucosae)
CT:
 gastric wall thickening (DDx: emphysematous gastritis)
gastric wall thickening (DDx: emphysematous gastritis)
Plain radiographs:
 innumerable small gas bubbles silhouetting the stomach in a mottled fashion without positional change
innumerable small gas bubbles silhouetting the stomach in a mottled fashion without positional change thickening of rugal folds
thickening of rugal folds portal venous gas
portal venous gas
GI:
 cobblestone appearance of mucosa on upper GI
cobblestone appearance of mucosa on upper GI intramural penetration of contrast material
intramural penetration of contrast material
| Cx: | cicatricial stenosis (21%), sinus tract formation |
| Prognosis: | 60 80% mortality |
| Rx: | broad-spectrum antibiotics + intravenous fluids; emergent surgery for acute perforation |
Erosive Gastritis
= HEMORRHAGIC GASTRITIS
| Incidence: | 0.5 10% of GI studies |
Etiology (in 50% without causative factors):
Peptic disease: emotional stress, alcohol, acid, corrosives, severe burns, anti-inflammatory agents (aspirin, steroids, phenylbutazone, indomethacin)
Infection: herpes simplex virus, CMV, Candida
Crohn disease: aphthoid ulcers identical in appearance to varioliform erosions
| Histo: | epithelial defect not penetrating beyond muscularis mucosae |
10 20% of all GI hemorrhages (usually without significant blood loss)
vague dyspepsia, ulcerlike symptoms
| Location: | antrum, rarely extending into fundus; aligned on surface of gastric rugal folds |
 varioliform complete erosion (95%) = tiny fleck of barium surrounded by radiolucent halo ( target lesion ) <5 mm, usually multiple
varioliform complete erosion (95%) = tiny fleck of barium surrounded by radiolucent halo ( target lesion ) <5 mm, usually multiple incomplete erosion (5%) = linear streaks/dots of barium without surrounding mound of edema/inflammation
incomplete erosion (5%) = linear streaks/dots of barium without surrounding mound of edema/inflammation nodularity/scalloping of prominent antral folds
nodularity/scalloping of prominent antral folds contiguous duodenal disease may be present
contiguous duodenal disease may be present limited distensibility, poor peristalsis/atony, delayed gastric emptying
limited distensibility, poor peristalsis/atony, delayed gastric emptying
Phlegmonous Gastritis
| Etiology: | septicemia, local abscess, postoperative stomach, complication of gastric ulcer/cancer |
| Organism: | Streptococcus |
| Path: | multiple gastric wall abscesses, which may communicate with lumen |
severe fulminating illness
patient may vomit pus
| Location: | usually limited to stomach not extending beyond pylorus; submucosa is the most severely affected gastric layer |
 barium dissection into submucosa + serosa
barium dissection into submucosa + serosa
Gastrointestinal stromal tumor
= GIST = SPINDLE CELL/EPITHELOID TUMOR
| Origin: | KIT-positive gut pacemaker cell = precursor of the interstitial cell of Cajal of myenteric plexus |
 Most common mesenchymal neoplasm of GI tract
Most common mesenchymal neoplasm of GI tract
| Incidence: | 4500 6000 new cases per year (USA) |
| Age: | >50 years |
| Histo: | spindle cell (70 80%)/epithelioid (20 30%) morphology/mixture of both |
Location:
GI tract anywhere between esophagus and anus:
stomach (37 70%), small intestine (20 33%), duodenum (9%), anorectum (5 7%) > colon (4%) > esophagus (2%)
 75% of mesenchymal tumors in the esophagus are leiomyomas, 25% GIST
75% of mesenchymal tumors in the esophagus are leiomyomas, 25% GIST Stomach is the most common location of GIST = 2 3% of all gastric tumors
Stomach is the most common location of GIST = 2 3% of all gastric tumors
peritoneum (4%), omentum; mesentery; retroperitoneum
| Site: | muscularis propria (leiomyomas arise from muscularis mucosae) |
P.838
early satiety, indigestion, bloating, vague abdominal pain
 often not detected until late in their progression
often not detected until late in their progressiongastrointestinal bleeding (from mucosal ulceration)
expresses transmembrane receptor tyrosine kinase encoded by KIT gene (CD117) in 95%; 70% of GISTs coexpress CD34
| Associated with: | neurofibromatosis type 1 |
| Spread: | (in 50% at presentation) |
adjacent organ invasion, ascites, omentum, peritoneum, liver metastasis
 Lymphadenopathy is NOT a feature!
Lymphadenopathy is NOT a feature! large hypervascular enhancing mass in prominent extraluminal location
large hypervascular enhancing mass in prominent extraluminal location heterogeneous texture due to necrosis, hemorrhage, cystic degeneration
heterogeneous texture due to necrosis, hemorrhage, cystic degeneration ulceration + fistulization to GI lumen (common)
ulceration + fistulization to GI lumen (common) tumor vessels visible within tumor
tumor vessels visible within tumor displacement of adjacent organs + vessels
displacement of adjacent organs + vessels@ Stomach
 well-circumscribed mass up to 30 cm in size
well-circumscribed mass up to 30 cm in size features of submucosal mass:
features of submucosal mass: lesion margin obtuse/at right angle with gastric wall (in profile)
lesion margin obtuse/at right angle with gastric wall (in profile) smoothly circumscribed (en face)
smoothly circumscribed (en face)
 smooth mucosal surface (common)
smooth mucosal surface (common) mucosal ulceration (in up to 60%)
mucosal ulceration (in up to 60%) polypoid intraluminal mass (in 14%
polypoid intraluminal mass (in 14%
CT:
 extragastric extension into gastrohepatic/gastrosplenic ligament/lesser sac (in 86%)
extragastric extension into gastrohepatic/gastrosplenic ligament/lesser sac (in 86%) peripheral enhancement in 92% (corresponding to viable tumor)
peripheral enhancement in 92% (corresponding to viable tumor) central areas of low attenuation (corresponding to hemorrhage, necrosis, cyst formation)
central areas of low attenuation (corresponding to hemorrhage, necrosis, cyst formation) cavity containing air/air-fluid level/oral contrast medium communicates with gastric lumen
cavity containing air/air-fluid level/oral contrast medium communicates with gastric lumen calcified in 3%
calcified in 3%
MR:
 solid tumor portion hypointense on T1WI + hyperintense on T2WI + enhancement
solid tumor portion hypointense on T1WI + hyperintense on T2WI + enhancement tumoral hemorrhage varies from high to low signal intensity on T1WI + T2WI depending on age
tumoral hemorrhage varies from high to low signal intensity on T1WI + T2WI depending on age
| DDx: | leiomyoma, leiomyosarcoma, schwannoma, neurofibroma, carcinoid |
@ Small intestine
@ Anorectum
| Cx: | bowel obstruction (rare) |
| Rx: | (1) surgery for localized primary (2) imatinib (= tyrosine kinase inhibitor) inhibits growth of GIST (paradoxical enlargement due to tumor hemorrhage/necrosis) |
Giardiasis
= overgrowth of commensal parasite Giardia lamblia
Organism:
Giardia lamblia (flagellated protozoan); often harmless contaminant of duodenum + jejunum in motile form (= trophozoite) attached to mucosa by suction disk, nonmotile form (= cyst) shed in feces; capable of pathogenic behavior with invasion of gut wall
| Incidence: | 1.5 2% of population in United States, infests 4 16% of inhabitants of tropical countries, found in 3 20% of children in parts of southern USA |
| Predisposed: | altered immune mechanism (dysgammaglobulinemia, nodular lymphoid hyperplasia of ileum) |
| Histo: | blunted villi (may be misdiagnosed as celiac disease especially in children), cellular infiltrate of acute + chronic inflammation in lamina propria |
abdominal pain, weight loss, failure to thrive (especially in children)
spectrum from asymptomatic to severe debilitating diarrhea, steatorrhea (related to number of organisms)
reduced fat absorption (simulating celiac disease)
| Location: | most pronounced in duodenum + jejunum |
 thickened distorted mucosal folds in duodenum + jejunum (mucosal edema) with normal ileum
thickened distorted mucosal folds in duodenum + jejunum (mucosal edema) with normal ileum marked spasm + irritability with rapid change in direction + configuration of folds
marked spasm + irritability with rapid change in direction + configuration of folds hypersecretion with blurring + indistinctness of folds
hypersecretion with blurring + indistinctness of folds hyperperistalsis with rapid transit time
hyperperistalsis with rapid transit time segmentation of barium (from motility disturbance + excess intraluminal fluid)
segmentation of barium (from motility disturbance + excess intraluminal fluid) lymphoid hyperplasia (associated with immunoglobulin deficiency state)
lymphoid hyperplasia (associated with immunoglobulin deficiency state)
| Dx: | (1) Detection of Giardia lamblia cysts in formed feces or trophozoites in diarrheal stools (2) Trophozoites in duodenal aspirate/jejunal biopsy |
| DDx: | Strongyloides/hookworm infection |
| Rx: | quinacrine (Atabrine ) |
Glomus Tumor of Stomach
 Most common benign vascular gastric tumor
Most common benign vascular gastric tumor
| Histo: | dilated irregularly shaped thin-walled vessels (= modified capillaries) covered by nests/strands/sheets of glomus cells |
asymptomatic/upper GI bleeding
| Location: | gastric antrum |
 single smooth submucosal mass ulceration
single smooth submucosal mass ulceration tiny flecks of calcification (occasionally)
tiny flecks of calcification (occasionally) strong enhancement in early arterial phase
strong enhancement in early arterial phase
Glycogen Acanthosis
= benign degenerative condition with accumulation of cellular glycogen within squamous epithelial lining of esophagus
| Incidence: | in up to 15% of endoscoped patients |
| Etiology: | unknown |
| Age: | middle-aged/elderly individuals |
| Histo: | hyperplasia + hypertrophy of squamous mucosal cells secondary to increased glycogen; no malignant potential |
asymptomatic
white oval mucosal plaques of 2 15 mm in diameter on otherwise normal appearing mucosa
| Location: | middle (common)/upper esophagus, in random distribution |
 multiple 1 3-mm rounded nodules/plaques
multiple 1 3-mm rounded nodules/plaques
| Dx: | biopsy |
| DDx: | candida esophagitis (lesions disappear under treatment in contrast to glycogen acanthosis), reflux esophagitis |
P.839
Graft-Versus-Host Disease
= T lymphocytes from donor bone marrow cause selected epithelial damage of recipient target organs
Bone marrow transplantation for treatment of:
leukemia, lymphoma, aplastic anemia, immunologic deficit, metabolic disorders of hematopoietic system, some metastatic disease
| Incidence: | 30 70% of patients with allogeneic (= donor genetically different from host) transplant |
| Target organs: | GI tract (small bowel), skin, liver |
@ Skin
maculopapular rash on face, trunk, extremities
@ Liver
elevation of hepatic enzymes liver failure
@ GI tract
profuse secretory diarrhea
abdominal cramping, fever, nausea, vomiting
| Path: | severe mucosal atrophy/destruction |
 shaggy fold thickening
shaggy fold thickening ribbon bowel = small bowel fold effacement with tubular appearance (DDx: viral enteritis, ischemia, celiac disease, radiation, soybean allergy)
ribbon bowel = small bowel fold effacement with tubular appearance (DDx: viral enteritis, ischemia, celiac disease, radiation, soybean allergy) loss of haustration, spasm, edema, ulceration, granular mucosal pattern of colon (simulating ulcerative colitis)
loss of haustration, spasm, edema, ulceration, granular mucosal pattern of colon (simulating ulcerative colitis) small bowel cast = prolonged coating of abnormal bowel for hours to days
small bowel cast = prolonged coating of abnormal bowel for hours to days circular collections of contrast material on cross section + parallel tracks on longitudinal section
circular collections of contrast material on cross section + parallel tracks on longitudinal section severely decreased transit time
severely decreased transit time
CT:
 abnormally enhancing thin layer of mucosa diffusely involving small + large bowel
abnormally enhancing thin layer of mucosa diffusely involving small + large bowel fluid-filled distended poorly opacified bowel (oral contrast material not given!)
fluid-filled distended poorly opacified bowel (oral contrast material not given!) barium (from previous contrast enema) may become incorporated into bowel wall
barium (from previous contrast enema) may become incorporated into bowel wall
| Cx: | infection with opportunistic organisms, eg, Candida albicans, herpes virus, invasive fungal organisms, CMV, Varicella-zoster virus, Epstein-Barr virus, hepatitis viruses, Rotavirus, Adenovirus, Coxsackie virus A and B, P. carinii, pneumococcus |
| Prognosis: | fatal in up to 15% (due to opportunistic infections) |
| Rx: | steroids + cyclosporine |
| DDx: | superinfection with enteroviruses |
Helicobacter Pylori Infection
| Organism: | worldwide gram-negative spiral-shaped bacillus [formerly Campylobacter pylori] |
| Prevalence: | increasing with age; >50% of Americans >60 years of age |
| Path: | surface epithelial damage + inflammation with mucosal infiltration by neutrophils, plasma cells, and lymphoid nodules |
| Location: | gastric antrum > proximal half of stomach |
| Site: | beneath mucus layer on surface epithelial cells |
asymptomatic (vast majority)
dyspepsia, epigastric pain
 gastritis (75% prevalence of H. pylori):
gastritis (75% prevalence of H. pylori): thickened gastric folds
thickened gastric folds polypoid gastritis mimicking malignant tumor
polypoid gastritis mimicking malignant tumor enlarged areae gastricae
enlarged areae gastricae
 gastric ulcer (60 80% prevalence of H. pylori)
gastric ulcer (60 80% prevalence of H. pylori) duodenal ulcer (90 100% prevalence of H. pylori)
duodenal ulcer (90 100% prevalence of H. pylori)
| Dx: | (1) Endoscopic brushings + biopsy (2) Breath test measuring urease activity after ingestion of carbon-14 labeled urea (3) Serologic test for IgG antibodies |
| Rx: | triple therapy (= bismuth + metronidazole + tetracycline/amoxicillin) results in 95% cure rate after 2 weeks of therapy |
Hemangioma of Small Bowel
| Incidence: | 7 10% of all benign small bowel tumors |
| Increased incidence in: | Turner syndrome, tuberous sclerosis, Osler-Weber-Rendu disease |
symptomatic (80%):
acute intermittent severe bleeding (melena)
acute/chronic life-threatening anemia
intestinal obstruction, intussusception, perforation
| Path: | submucosal soft infiltrative polypoid mass |
| Location: | jejunum (55%), ileum (42%), duodenum (2%) |
 multiple sessile compressible intraluminal filling defects
multiple sessile compressible intraluminal filling defects nodular segmental mucosal abnormality
nodular segmental mucosal abnormality phleboliths in intestinal wall
phleboliths in intestinal wall
CT:
 well-circumscribed lobulated mass of mixed attenuation supplied by large artery
well-circumscribed lobulated mass of mixed attenuation supplied by large artery
Henoch-Sch nlein Purpura
= most common systemic allergic hypersensitivity-related acute small-vessel vasculitis in children
| Precipitated by: | bacterial/viral infection, allergies, insect sting, drugs (eg, penicillin, sulfonamides, aspirin), certain foods |
| Cause: | deposition of IgA-dominant immune complexes in venules, capillaries, and arterioles |
| Age: | children (peak age of 5, range 3 10 years) + adults >20 years (in up to 30%) |
most frequent manifestations:
purpuric skin rash on legs + extensor surfaces on arms
colicky abdominal pain + GI bleeding
microscopic hematuria + proteinuria in 50% (from proliferative glomerulonephritis with IgA deposits demonstrated by immunofluorescence)
often begins as an upper respiratory tract infection
arthralgias of large joints
 multifocal bowel wall thickening (due to intramural hemorrhage + edema)
multifocal bowel wall thickening (due to intramural hemorrhage + edema)
| Cx: | (1) Bowel infarct/perforation/irreducible intussusception (3 5%) (2) Renal insufficiency (10 20%), end-stage renal disease (5%) |
| Rx: | high doses of corticosteroids + azathioprine |
Hernia
| Prevalence: | 10% of SBO; 2nd most common cause of small bowel obstruction! |
| Nomenclature: | according to anatomic site of its orifice |
P.840
External Hernia
= bowel extending outside the abdominal cavity
| Incidence: | 95% of all hernias |
Location:
@ Ventral
Postoperative hernia
Trocar site hernia
Incidence: 1 3.6%  often Richter type hernia
often Richter type hernia
Umbilical hernia
see below
Paraumbilical hernia
 large defect through linea alba from diastasis of rectus abdominis muscle at umbilicus
large defect through linea alba from diastasis of rectus abdominis muscle at umbilicus
Epigastric/hypogastric hernia
 in linea alba above/below umbilicus
in linea alba above/below umbilicus
Spigelian hernia
Frequency: 2% of anterior abdominal hernias = acquired ventrolateral hernia through defect in aponeurosis between transverse and rectus muscle of abdomen at junction of semilunar + arcuate lines below umbilicus
 hernia sac dissects laterally to rectus abdominis muscle through a fibrous groove (= semicircular/spigelian line)
hernia sac dissects laterally to rectus abdominis muscle through a fibrous groove (= semicircular/spigelian line) hernia sac lies beneath an intact external oblique aponeurosis
hernia sac lies beneath an intact external oblique aponeurosis
@ Diaphragm
Bochdalek hernia
Morgagni hernia
@ Lumbar
Location: defect in lumbar muscles below 12th rib + above iliac cest Grynflett-Lesshaft (upper)
Borders: internal oblique m. (anteriorly), 12th rib (superiorly), erector spinae m. (posteriorly) Inferior lumbar triangle (Petit) (lower)
Borders: external oblique m. (anteriorly), iliac crest (inferiorly), latissimus dorsi m. (posteriorly)
@ Pelvic floor
Obturator foramen
 hernia between pectineus + external obturator muscles
hernia between pectineus + external obturator muscles
Sciatic notch
Perineal hernia (rare)
(a) anterior perineal hernia = defect of urogenital diaphragm anterior to superficial transverse perineal m. + lateral to bulbocavernosus m. + medial to ischiocavernosus m. (only in females)
(b) posterior perineal hernia = defect in levator ani m./between levator ani m. and coccygeus m. posterior to superficial transverse perineal m.
 defecating proctography
defecating proctography
@ Groin
Inguinal hernia
 Most common type of abdominal wall hernia, M>F
Most common type of abdominal wall hernia, M>F
direct inguinal hernia
= defect in Hesselbach triangle (bounded by inguinal ligament inferiorly, inferior epigastric artery superolaterally, fused aponeuroses of internal oblique + transverse abdominal muscles medially)
 medial to inferior epigastric vessels
medial to inferior epigastric vessels hernia contains bowel, mesenteric fat, vessels
hernia contains bowel, mesenteric fat, vessels
indirect inguinal hernia
 Most common hernia in children due to failure of obliteration of processus vaginalis accompanying the testis
Most common hernia in children due to failure of obliteration of processus vaginalis accompanying the testis lateral to inferior epigastric vessels originating at deep inguinal ring
lateral to inferior epigastric vessels originating at deep inguinal ring
Littre hernia = inguinal hernia containing Meckel diverticulum
Femoral hernia
M<F
 medial to femoral vein within femoral canal
medial to femoral vein within femoral canal posterior to inguinal ligament
posterior to inguinal ligament
Cx: high probability of incarceration Richter hernia = entrapment of antimesenteric border of bowel in hernia orifice, usually seen in older women with femoral hernias
no palpable mass = difficult to diagnose
 partial obstruction with patent bowel lumen
partial obstruction with patent bowel lumen
Internal Hernia
= herniation of bowel through a developmental/surgically created defect of the peritoneum, omentum, mesentery or through an adhesive band
| Incidence: | 5% of all hernias, responsible for <1% of mechanical small bowel obstruction |
Classification of internal hernias:
retroperitoneal: usually congenital containing a hernia sac
paraduodenal (ligament of Treitz)
foramen of Winslow
intersigmoid
pericecal/ileocolic
supravesical
anteperitoneal:
small group of hernias without a peritoneal sac
transmesenteric (transverse/sigmoid mesocolon)
transomental
pelvic (including broad ligament)
intermittent nausea, abdominal pain, distension (made worse by eating + standing and relieved by fasting + assuming a recumbent position)
 signs of bowel obstruction (only during symptomatic period)
signs of bowel obstruction (only during symptomatic period) mass effect with displacement of other abdominal organs
mass effect with displacement of other abdominal organs
| Cx: | volvulus |
Paraduodenal Hernia (53%)
= congenital defect in descending mesocolon
frequently asymptomatic
P.841
LEFT through fossa of Landzert (75%)
Location: to the left of 4th portion of duodenum at duodenojejunal junction (paraduodenal fossa = confluent zone of descending mesocolon + transverse mesocolon + small bowel mesentery  cluster of dilated small-bowel loops between pancreas + stomach
cluster of dilated small-bowel loops between pancreas + stomach displacement of gastric wall anteriorly
displacement of gastric wall anteriorly displacement of duodenojejunal flexure + transverse colon inferiorly
displacement of duodenojejunal flexure + transverse colon inferiorly engorged crowded vessels at entrance of hernia sac
engorged crowded vessels at entrance of hernia sacCT:
 encapsulated bowel loop displacing the inferior mesenteric vein (= landmark of the right margin of the descending mesocolon) anterolaterally
encapsulated bowel loop displacing the inferior mesenteric vein (= landmark of the right margin of the descending mesocolon) anterolaterally
RIGHT through mesentericoparietal fossa of Waldeyer (25%)
Predisposed: nonrotation of small bowel Location: behind the root of small bowel mesentery caudal to SMA and inferior to 3rd portion of duodenum on right side CT:
 encapsulated bowel loop displacing the right colic vein (= landmark of left margin of the ascending mesocolon) anteriorly
encapsulated bowel loop displacing the right colic vein (= landmark of left margin of the ascending mesocolon) anteriorly looping of small intestine behind SMA + SMV below transverse portion of duodenum
looping of small intestine behind SMA + SMV below transverse portion of duodenum SMV located ventral + to left of SMA
SMV located ventral + to left of SMA absence of normal horizontal duodenum
absence of normal horizontal duodenum
| Cx: | partial/complete obstruction of small intestine (in 50%) |
Lesser Sac Hernia (<10%)
through foramen of Winslow in retrogastric location
Invaginated gut:
ileum > jejunum, cecum, appendix, ascending colon, Meckel diverticulum, gallbladder, greater omentum
 gas-containing bowel loops in center of upper abdomen
gas-containing bowel loops in center of upper abdomen distended small bowel loops occupying space between stomach + liver
distended small bowel loops occupying space between stomach + liver
Iatrogenic Hernia
Transmesenteric Hernia
Cause: fenestration of transverse mesocolon in construction of Roux-en-Y loop  cluster of small-bowel loops (70%)
cluster of small-bowel loops (70%) clustered small bowel outside colon compressed against abdominal wall without overlying omental fat (85%)
clustered small bowel outside colon compressed against abdominal wall without overlying omental fat (85%) central displacement of colon (92%)
central displacement of colon (92%) displacement of mesenteric trunk (85%)
displacement of mesenteric trunk (85%) engorged mesenteric vessels (85%)
engorged mesenteric vessels (85%)
Hernia through Broad Ligament (very rare)
after laceration/fenestration during surgery or during pregnancy
Hiatal Hernia
| Associated with: | diverticulosis (25%), reflux esophagitis (25%), duodenal ulcer (20%), gallstones (18%) |
Sliding Hiatal Hernia (99%)
= AXIAL HERNIA = CONCENTRIC HERNIA
= esophagogastric junction (= termination point of converging gastric folds) >1.5 cm above diaphragmatic hiatus (= pinched appearance of gastric folds) with portion of peritoneal sac forming part of wall of hernia
| Etiology: | rupture of phrenicoesophageal membrane due to repetitive stretching with swallowing |
| Incidence: | increasing with age |
 reducible in erect position
reducible in erect position epiphrenic bulge = entire vestibule + sleeve of stomach are intrathoracic
epiphrenic bulge = entire vestibule + sleeve of stomach are intrathoracic distance between B ring (if visible) and hiatal margin >2 cm
distance between B ring (if visible) and hiatal margin >2 cm peristalsis ceases above hiatus (end of peristaltic wave delineates esophagogastric junction)
peristalsis ceases above hiatus (end of peristaltic wave delineates esophagogastric junction) tortuous esophagus having an eccentric junction with hernia
tortuous esophagus having an eccentric junction with hernia numerous coarse thick gastric folds within suprahiatal pouch (>6 longitudinal folds)
numerous coarse thick gastric folds within suprahiatal pouch (>6 longitudinal folds) gastroesophageal reflux
gastroesophageal refluxCT:
 dehiscence of diaphragmatic crura >15 mm
dehiscence of diaphragmatic crura >15 mm pseudomass within/above esophageal hiatus
pseudomass within/above esophageal hiatus increase in fat surrounding distal esophagus (= herniation of omentum through phrenicoesophageal ligament)
increase in fat surrounding distal esophagus (= herniation of omentum through phrenicoesophageal ligament)
| DDx: | normal temporary cephalad motion of esophagogastric junction by 1 2 cm into chest due to contraction of longitudinal muscle during esophageal peristalsis |
Paraesophageal Hernia (1%)
= ROLLING HIATAL HERNIA = parahiatal HERNIA
= portion of stomach superiorly displaced into thorax with esophagogastric junction remaining in subdiaphragmatic position
 cardia in normal position
cardia in normal position herniation of portion of stomach anterior to esophagus
herniation of portion of stomach anterior to esophagus frequently nonreducible
frequently nonreducible may be associated with gastric ulcer of lesser curvature at level of diaphragmatic hiatus
may be associated with gastric ulcer of lesser curvature at level of diaphragmatic hiatus
Totally Intrathoracic Stomach
= defect in central tendon of diaphragm in combination with slight volvulus in transverse axis of stomach behind heart (organoaxial rotation)
 cardia may be intrathoracic (usually)/subdiaphragmatic
cardia may be intrathoracic (usually)/subdiaphragmatic great gastric curvature either on right/left side
great gastric curvature either on right/left side
Congenitally Short Esophagus
(not true hernia, very rare)
= gastric ectopy by lack of lengthening of esophagus
 nonreducible intrathoracic gastric segment (in erect/supine position)
nonreducible intrathoracic gastric segment (in erect/supine position) cylindrical/round intrathoracic segment with large sinuous folds
cylindrical/round intrathoracic segment with large sinuous folds short straight esophagus
short straight esophagus circular narrowing at gastroesophageal junction, frequently with ulcer
circular narrowing at gastroesophageal junction, frequently with ulcer gastroesophageal reflux
gastroesophageal reflux
P.842
Umbilical Hernia
= protrusion of abdominal contents/fat into anterior abdominal wall via umbilical ring
| Prevalence: | 4% of all hernias; M < F |
| Cause: | failed closure of umbilical ring, obesity, multiple pregnancies, intraabdominal masses, liver failure, increased intraabdominal pressure, weak abdominal wall |
 may contain fat/small bowel/colon
may contain fat/small bowel/colon
| Cx: | strangulation, incarceration |
| DDx: | paraumbilical, spigelian, epigastric, incisional hernia |
Hirschsprung Disease
= AGANGLIONOSIS OF THE COLON = AGANGLIONIC MEGACOLON
= absence of parasympathetic ganglia in muscle (Meissner plexus) + submucosal layers (Auerbach plexus) secondary to an arrest of craniocaudal migration of neuroblasts along vagal trunks before 12th week leading to relaxation failure of the aganglionic segment
| Incidence: | 1:5,000 8,000 live births; 15 20% of all neonatal bowel obstructions; usually sporadic; familial in 4% |
| Age: | during first 6 weeks of life of a full-term infant (70 80%); M:F = 4 9:1; extremely rare in premature infants |
| Associated with: | trisomy 21 (in 2%) |
| Location: | at varying distances proximal to anus, usually rectosigmoid (in 80%) |
| (a) ultrashort segment (= internal sphincter) | (very rare) |
| (b) short segment disease | (80%) |
| (c) long segment disease | (15%) |
| (d) total colonic aganglionosis | (5%) |
| (e) skip aganglionosis = sparing of rectum | (very rare) |
failure to pass meconium within first 48 hours of life
intermittent constipation + paradoxical diarrhea (25%)
bilious vomiting, abdominal distention
rectal manometry with absence of spike activity
 generalized gaseous distention of bowel loops
generalized gaseous distention of bowel loopsBE:
 short patent colon usually of normal caliber
short patent colon usually of normal caliber inverted cone shape at transition between abnormal
inverted cone shape at transition between abnormal+ normal bowel (MOST CHARACTERISTIC):
 transition zone = aganglionic segment appearing normal in size (seen in 50% during 1st week of life)
transition zone = aganglionic segment appearing normal in size (seen in 50% during 1st week of life) dilatation of large + small bowel aborally from transition zone
dilatation of large + small bowel aborally from transition zone
 normal-appearing rectum in 33%
normal-appearing rectum in 33% marked retention of barium on delayed postevacuation films after 12 24 hours
marked retention of barium on delayed postevacuation films after 12 24 hours 10 15-cm segment of persistent corrugated/convoluted rectum (= abnormal uncoordinated contractions of the aganglionic portion of colon) in 31% (DDx: colitis, milk allergy, normal intermittent spasm of rectum)
10 15-cm segment of persistent corrugated/convoluted rectum (= abnormal uncoordinated contractions of the aganglionic portion of colon) in 31% (DDx: colitis, milk allergy, normal intermittent spasm of rectum)
N.B.: avoid digital exam/cleansing enema prior to radiographic studies! OB-US:
 dilated small bowel/dilated colon
dilated small bowel/dilated colon
| Cx: |
|
| Dx: | suction mucosal biopsy of rectum (increased acetylcholinesterase activity) |
| Rx: |
|
Hyperplastic Polyp of Colon
= intestinal metaplasia consisting of mucous glands lined by a single layer of columnar epithelium; NO malignant potential
| Path: | infolding of epithelium into the glandular lumen |
| Location: | rectosigmoid |
 smooth rounded sessile elevation
smooth rounded sessile elevation usually <5 mm in diameter
usually <5 mm in diameter
Hypertrophic Pyloric Stenosis
= idiopathic hypertrophy and hyperplasia of circular muscle fibers of pylorus with proximal extension into gastric antrum
| Incidence: | 3:1,000; M:F = 4 5:1 |
| Etiology: | inherited as a dominant polygenic trait; increased incidence in firstborn boys; acquired rather than congenital condition |
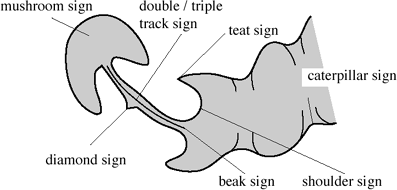 |
| Hypertrophic Pyloric Stenosis |
Infantile Form of Hypertrophic Pyloric Stenosis
| Age: | manifestation between 2 8 weeks of life |
nonbilious projectile vomiting (sour formula/clear gastric contents) with progression over a period of several weeks after birth (15 20%)
positive family history
palpable olive-shaped mass (80% sensitive in experienced hands, up to 14% false positive)
nasogastric aspirate >10 mL (92% sensitive, 86% specific)
UGI (95% sensitivity):
Precautions: - empty stomach via nasogastric tube before study
- remove contrast at end of study
 elongation + narrowing of pyloric canal (2 4 cm in length):
elongation + narrowing of pyloric canal (2 4 cm in length): double/triple track sign = crowding of mucosal folds in pyloric channel
double/triple track sign = crowding of mucosal folds in pyloric channel string sign = passing of small barium streak through pyloric channel
string sign = passing of small barium streak through pyloric channel Twining recess = diamond sign = transient triangular tentlike cleft/niche in midportion of pyloric canal with apex pointing inferiorly secondary to mucosal bulging between two separated hypertrophied muscle bundles on the greater curvature side within pyloric channel
Twining recess = diamond sign = transient triangular tentlike cleft/niche in midportion of pyloric canal with apex pointing inferiorly secondary to mucosal bulging between two separated hypertrophied muscle bundles on the greater curvature side within pyloric channel
P.843
 abnormal configuration of antrum:
abnormal configuration of antrum: pyloric teat = outpouching along lesser curvature due to disruption of antral peristalsis
pyloric teat = outpouching along lesser curvature due to disruption of antral peristalsis antral beaking = mass impression upon antrum with streak of barium pointing toward pyloric channel
antral beaking = mass impression upon antrum with streak of barium pointing toward pyloric channel Kirklin sign = mushroom sign = indentation of base of bulb (in 50%)
Kirklin sign = mushroom sign = indentation of base of bulb (in 50%)
 gastric distension with fluid
gastric distension with fluid active gastric hyperperistalsis:
active gastric hyperperistalsis: caterpillar sign = gastric hyperperistaltic waves
caterpillar sign = gastric hyperperistaltic waves
US:
 target sign = hypoechoic ring of hypertrophied pyloric muscle around echogenic mucosa centrally on cross-section
target sign = hypoechoic ring of hypertrophied pyloric muscle around echogenic mucosa centrally on cross-section elongated pylorus with thickened muscle:
elongated pylorus with thickened muscle: pyloric muscle wall thickness 3 mm
pyloric muscle wall thickness 3 mm pyloric volume >1.4 cm3 (= 1/4 [maximum pyloric diameter]2 pyloric length); most criteria independent of contracted or relaxed state (33% false negative)
pyloric volume >1.4 cm3 (= 1/4 [maximum pyloric diameter]2 pyloric length); most criteria independent of contracted or relaxed state (33% false negative) pyloric length (mm) + 3.64 muscle thickness (mm) > 25
pyloric length (mm) + 3.64 muscle thickness (mm) > 25 pyloric transverse diameter 13 mm with pyloric channel closed
pyloric transverse diameter 13 mm with pyloric channel closed elongated pyloric canal 17 mm in length
elongated pyloric canal 17 mm in length
 cervix sign = indentation of muscle mass on fluid-filled antrum on longitudinal section
cervix sign = indentation of muscle mass on fluid-filled antrum on longitudinal section antral nipple sign = redundant pyloric channel mucosa protruding into gastric antrum
antral nipple sign = redundant pyloric channel mucosa protruding into gastric antrum exaggerated peristaltic waves
exaggerated peristaltic waves delayed gastric emptying of fluid into duodenum
delayed gastric emptying of fluid into duodenum
Cx: hypochloremic metabolic alkalosis DDx:
infantile pylorospasm
 muscle thickness between 1.5 and 2 mm
muscle thickness between 1.5 and 2 mm variable caliber of antral narrowing
variable caliber of antral narrowing antral peristalsis
antral peristalsis delayed gastric emptying
delayed gastric emptying elongation of pylorus
elongation of pylorus
Prognosis: resolves in several days/ early stage of evolving pyloric stenosis Rx: effective with metoclopramide/bentyl Gastritis/milk allergy
 circumferential/eccentric thickening of antral mucosa >2 3 mm
circumferential/eccentric thickening of antral mucosa >2 3 mm
Duodenal obstruction from midgut volvulus
 distended descending duodenum
distended descending duodenum reversal of SMA and SMV relationship
reversal of SMA and SMV relationship whirlpool sign = twisting of small bowel mesentery
whirlpool sign = twisting of small bowel mesentery
Gastric diaphragm
Adult Form of Hypertrophic Pyloric Stenosis
| Cause: | secondary to mild infantile form |
acute obstructive symptoms uncommon
nausea, intermittent vomiting
postprandial distress, heartburn
Associated with:
peptic ulcer disease (in 50 74%) (prolonged gastrin production secondary to stasis of food)
chronic gastritis (54%)
 persistent elongation (2 4 cm) + concentric narrowing of pyloric channel
persistent elongation (2 4 cm) + concentric narrowing of pyloric channel parallel + preserved mucosal folds
parallel + preserved mucosal folds antispasmodics show no effect on narrowing
antispasmodics show no effect on narrowing proximal benign ulcer (74%), usually near incisura
proximal benign ulcer (74%), usually near incisura
Focal Pyloric hypertrophy
= TORUS HYPERPLASIA
= localized muscle hypertrophy on the lesser curvature
= milder atypical form of HPS
 flattening of distal lesser curvature
flattening of distal lesser curvature
Imperforate Anus
| Prevalence: | 1:5,000 live births |
LOW ANOMALY (55%)
= bowel has passed through levator sling
fistula to perineum/vulva
Rx: readily reparable INTERMEDIATE DEFECT (least common)
= bowel ends within levator muscle as a result of abnormality in posterior migration of rectum
fistula opening low in vagina/vestibule
Rx: 2-/3-stage operation HIGH ANOMALY
= bowel ends above levator sling; M > F
fistulous connection to perineum/vagina/posterior urethra (air in bladder in males; air in vagina in females)
Cx: associated malformations more common + more severe Rx: multiple surgical procedures
 distance between rectal air and skin will not accurately outline the extent of atretic rectum and anus (varying length during crying with increase in abdominal pressure + contraction of levator ani muscle)
distance between rectal air and skin will not accurately outline the extent of atretic rectum and anus (varying length during crying with increase in abdominal pressure + contraction of levator ani muscle)US:
 15 mm distance between anal dimple + distal rectal pouch on transperineal images indicates low lesion
15 mm distance between anal dimple + distal rectal pouch on transperineal images indicates low lesion
OB-US (earliest detection by 20 29 weeks GA):
absent/low disaccharidase level in amniotic fluid
 dilated colon in lower pelvis with U-/S-shaped configuration intraluminal calcifications
dilated colon in lower pelvis with U-/S-shaped configuration intraluminal calcifications normal amniotic fluid (unless also TE fistula)
normal amniotic fluid (unless also TE fistula) absence of anal characteristics (= hypoechoic circular rim with central echogenic stripe)
absence of anal characteristics (= hypoechoic circular rim with central echogenic stripe)
Infectious Colitis
Cause:
bacterium: Shigella, Salmonella, Yersinia, Campylobacter, Staphylococcus, Chlamydia trachomatis, amebiasis, tuberculosis
fungus: histoplasmosis, mucormycosis, actinomycosis
virus: herpesvirus, CMV, rotavirus
Location:
diffuse involvement = CMV, E. coli
limited to right colon = Shigella, Salmonella
descending + sigmoid colon = schistosomiasis
rectosigmoid = gonorrhea, herpesvirus, C. trachomatis (lymphogranuloma venereum)
P.844
CT:
 wall thickening + low attenuation
wall thickening + low attenuation homogeneous wall enhancement
homogeneous wall enhancement multiple air-fluid levels
multiple air-fluid levels inflammation of pericolic fat
inflammation of pericolic fat ascites
ascites
| Dx: | clinical |
Intestinal Lymphangiectasia
CONGENITAL LYMPHANGIECTASIA
= PRIMARY PROTEIN-LOSING ENTEROPATHY
= generalized congenital malformation of lymphatic system with atresia of the thoracic duct + gross dilatation of small bowel lymphatics; usually sporadic; may be inherited
Age: presentation before 30 years asymmetric generalized lymphedema (due to protein-losing enteropathy with hypoproteinemia)
chylous pleural effusions (45%)
diarrhea (60%), steatorrhea (20%)
vomiting (15%)
abdominal pain (15%) + distension
decreased albumin + globulin
lymphocytopenia (90%)
decreased serum fibrinogen, transferrin, ceruloplasmin
ACQUIRED LYMPHANGIECTASIA
Causes leading to dilatation of intestinal lymphatics:
Mesenteric adenitis
Retroperitoneal fibrosis
Diffuse small bowel lymphoma
Pancreatitis
Pericardial effusion with obstruction of thoracic duct
peripheral edema/anasarca (KEY SYMPTOM)
chylous + serous effusion
diarrhea, vomiting, abdominal pain, malabsorption, steatorrhea
hypoproteinemia secondary to protein loss into intestinal lumen
| Path: | dilatation of lymph vessels in mucosa + submucosa + abundance of foamy fat-staining macrophages (negative for PAS) |
 diffuse symmetric marked enlargement of folds in jejunum
diffuse symmetric marked enlargement of folds in jejunum+ ileum (due to dilated intestinal lymphatics
+ hypoproteinemic edema)
 slight separation + rigidity of folds
slight separation + rigidity of folds dilution of barium column (considerable increase in intestinal secretions from malabsorption)
dilution of barium column (considerable increase in intestinal secretions from malabsorption) no/mild dilatation of bowel
no/mild dilatation of bowelLymphangiogram (not always diagnostic):
 hypoplasia of lower extremity lymphatics
hypoplasia of lower extremity lymphatics occlusion of thoracic duct/large tortuous thoracic duct
occlusion of thoracic duct/large tortuous thoracic duct obstruction of cisterna chyli with backflow into mesenteric + intestinal lymphatics
obstruction of cisterna chyli with backflow into mesenteric + intestinal lymphatics hypoplastic lymph nodes
hypoplastic lymph nodes
| Dx: | small bowel biopsy (dilated lymphatics in lamina propria + vascular core) |
| Rx: | low-fat diet with medium-chain triglycerides (direct absorption into portal venous system) |
| DDx: |
|
Intestinal Pseudoobstruction
Acute Colonic Pseudoobstruction
= Ogilvie syndrome
[Sir William Heanage Ogilvie (1887 1971), English surgeon at Guy's Hospital, London]
= rare clinical disorder with signs & symptoms & radiographic appearance of an acute large bowel obstruction but without mechanical obstruction
| Pathogenesis: | imbalance in autonomic nervous system (sympathetic overactivity + parasympathetic suppression) after recent significant medical illness/surgical procedure |
| Cause: | retroperitoneal trauma, especially fracture (11 52%), pelvic/abdominal/cardiothoracic surgery (20%), infection (10%), cardiac disease [MI, CHF] (10%) |
In 50% associated with:
metabolic imbalance (hypokalemia, hypocalcemia, hypomagnesemia), drugs (narcotic analgesics, antidepressants, antipsychotic, calcium channel blockers, narcoleptics)
| Age: | >60 years/younger patient with spinal disorder; M > F |
abdominal pain (80%), abdominal distension
nausea & vomiting (80%)
obstipation (40%), diarrhea
fever (37%)
bowel sounds present
 massively dilated colon, especially cecum + right hemicolon (occasionally extending to rectum)
massively dilated colon, especially cecum + right hemicolon (occasionally extending to rectum) normal haustral markings
normal haustral markings colon cut-off sign (= lack of gas in distal colon)
colon cut-off sign (= lack of gas in distal colon) small bowel air-fluid levels
small bowel air-fluid levels absence of obstructive lesion on enema
absence of obstructive lesion on enema
| Cx: | cecal perforation |
| Prognosis: | 15 45% mortality |
| Rx: | nasogastric + rectal suctioning; neostigmine; colonic decompression (if cecum exceeds 10 cm) |
| DDx: | toxic megacolon, mechanical obstruction |
Chronic Intestinal Pseudoobstruction Syndrome
= nonpropulsive intestine characterized by impaired response to intestinal dilatation without definable cause; autosomal dominant
Cause:
reduced density of interstitial cells of Cajal in colon (= intestinal pacemaker cells)
neuropathic disorder: amyloidosis, diabetes, multiple sclerosis, brainstem tumor, stroke, spinal cord injury, Parkinsonism, paraneoplastic syndromes (antineuronal nuclear antibodies)
myopathy: scleroderma
Medication: anticholinergic antidepressant, calcium channel blocker, alpha-2 adrenergic agonists
P.845
| Age: | neonatal period/delayed for months + years, M:F = 1:1 |
recurrent attacks of nausea & vomiting (83%)
abdominal pain (74%)
abdominal distension (57%)
constipation (36%), diarrhea (29%)
persistently decreased peristalsis
 esophageal dilation + hypoperistalsis (lower third)
esophageal dilation + hypoperistalsis (lower third) excessive duodenal dilation (DDx: megaduodenum, superior mesenteric artery syndrome)
excessive duodenal dilation (DDx: megaduodenum, superior mesenteric artery syndrome) mild to marked gaseous distension of proximal small bowel
mild to marked gaseous distension of proximal small bowel ligament of Treitz may be placed lower than usual
ligament of Treitz may be placed lower than usual delayed transit of barium through affected segments
delayed transit of barium through affected segments disordered motor activity (fluoroscopy)
disordered motor activity (fluoroscopy) small bowel air-fluid levels + distension
small bowel air-fluid levels + distension disturbed intestinal transit
disturbed intestinal transit
Intraluminal Duodenal Diverticulum
= congenital lesion secondary to elongation of an incomplete duodenal diaphragm
| Age at presentation: | in young adult |
easy satiety
vomiting
upper abdominal cramping pain
| Location: | 2nd 3rd portion of duodenum |
 barium-filled sac within duodenal lumen (pathognomonic picture) = windsock, comma, teardrop appearance
barium-filled sac within duodenal lumen (pathognomonic picture) = windsock, comma, teardrop appearance anchored to the lateral wall of the duodenum
anchored to the lateral wall of the duodenum halo sign = duodenal mucosa covers outer + inner wall of diverticulum
halo sign = duodenal mucosa covers outer + inner wall of diverticulum
Intramural Esophageal Rupture
= DISSECTING INTRAMURAL HEMATOMA
= mucosal tear with dissecting hemorrhage into submucosa and involvement of venous plexus
hematemesis
 intramural hematoma simulates retained solid material within lumen
intramural hematoma simulates retained solid material within lumen mucosal stripe sign = dissected mucosa floating within lumen
mucosal stripe sign = dissected mucosa floating within lumen
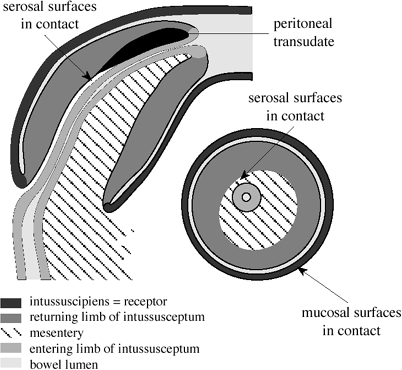 |
| Anatomy of Intussusception |
Intussusception
= telescope-like invagination or prolapse of a segment of intestinal tract (= intussusceptum = donor loop) into the lumen of the adjacent intestine (= intussuscipiens = receiving loop)
 The intussuscipiens contains the folded intussusceptum with entering limb + returning limb + their mesentery
The intussuscipiens contains the folded intussusceptum with entering limb + returning limb + their mesentery
IN CHILDREN (94%)
Incidence: 2 4:1,000 live births; most common abdominal emergency of early childhood  Leading cause of acquired bowel obstruction in childhood!
Leading cause of acquired bowel obstruction in childhood!Etiology:
idiopathic (over 95%): mucosal edema + lymphoid hyperplasia following viral gastroenteritis; predominantly at ileocecal valve
lead point (5%):
infants <3 months: Meckel diverticulum (most common), duplication cyst
children >3 years of age: Burkitt lymphoma, polyp in Peutz-Jeghers syndrome, polypoid hemangioma, enterogenous cyst, ectopic pancreas, suture granuloma, periappendicitis, Henoch-Sch nlein purpura, coagulopathy, inspissated meconium
mnemonic: H DIMPL Henoch-Sch nlein purpura
Duplication
Idiopathic
Meckel diverticulum
Polyp
Lymphosarcoma
Age: peak incidence between 6 months and 2 years; 3 9 months (40%); <1 year (50%); <2 years (75%); >3 years (<10%); M:F = 2:1 abrupt onset of violent crampy pain (94%)
vomiting (91%)
red currant jelly stools/hematochezia (66%) usually only after >48 hours duration
palpable abdominal mass (59%)
diarrhea
restlessness, pallor, fever
Types: ileocolic (75 95%) > ileoileocolic (9%) > ileoileal (4%) > colocolic Location: transverse colon + hepatic flexure + ascending colon (90%) Cx: vascular compromise secondary to incorporation of mesentery (hemorrhage, infarction, acute inflammation) IN ADULTS (6%)
Incidence: accounts for <16% of all bowel obstructions; 0.05% of CT exams P.846
Etiology:
specific cause (80%):
Tumor: benign (1/3), malignant (1/5)
Postsurgical changes (1/3): adhesions adjacent to sutures/submucosal bowel edema/discoordinated motility
Invaginated (= inverted) Meckel diverticulum
Prolapsed gastric mucosa
Aberrant pancreas
Foreign body, feeding tube
Chronic ulcer (TB, typhoid)
Prior gastroenteritis
Gastroenterostomy, trauma
spontaneous without anatomic lead point:
celiac disease, scleroderma, Whipple disease, fasting, anxiety, agonal state
idiopathic (20%)
recurrent episodes of colicky pain, nausea, vomiting
abdominal tenderness, distention
change in bowel habits
palpable mass (in up to 50%)
bloody stool (in majority)
Location: ileoileal (40%) > ileocolic (15%) small bowel (55%): benign neoplasm (40%), malignant neoplasm (17%), nonneoplastic (43%) colon (45%): malignant neoplasm (48%), benign neoplasm (21%), nonneoplastic (31%) Prognosis: self-limiting if intussusception <3.5 cm in length
Plain film (40 90% accuracy):
 no abnormality in 25%
no abnormality in 25% abdominal soft-tissue mass (50 60%), usually in RUQ:
abdominal soft-tissue mass (50 60%), usually in RUQ: target sign = soft-tissue mass with concentric circular areas of lucency (due to mesenteric fat of intussusceptum)
target sign = soft-tissue mass with concentric circular areas of lucency (due to mesenteric fat of intussusceptum) meniscus sign = crescent of gas within colonic lumen that outlines the apex of the intussusceptum
meniscus sign = crescent of gas within colonic lumen that outlines the apex of the intussusceptum loss of inferior hepatic margin
loss of inferior hepatic margin
 little air in small intestine/gasless abdomen
little air in small intestine/gasless abdomen air in displaced appendix
air in displaced appendix small bowel obstruction (25%)
small bowel obstruction (25%)
Antegrade barium study:
 coiled spring appearance
coiled spring appearance beaklike abrupt narrowing of barium column demonstrating a central channel
beaklike abrupt narrowing of barium column demonstrating a central channel
Diagnostic enema:
| Indication: | unusual age of child (<2 months, >4 years), high fever, peritoneal signs |
| Contraindication: | free air |
 meniscus sign = convex intracolic mass = rounded apex of intussusceptum protrudes into contrast column
meniscus sign = convex intracolic mass = rounded apex of intussusceptum protrudes into contrast column coiled spring sign = edematous mucosal folds of returning limb of intussusceptum outlined by contrast material within lumen of colon
coiled spring sign = edematous mucosal folds of returning limb of intussusceptum outlined by contrast material within lumen of colon
US (98 100% sensitive, 88 100% specific):
 readily detectable mass over 5.0 2.5 cm
readily detectable mass over 5.0 2.5 cm crescent-in-doughnut/target/bull's eye sign (on transverse scan) = concentric rings of alternating hypoechoic + hyperechoic layers (= intussuscipiens) with central hyperechoic portion (= mesentery of intussusceptum)
crescent-in-doughnut/target/bull's eye sign (on transverse scan) = concentric rings of alternating hypoechoic + hyperechoic layers (= intussuscipiens) with central hyperechoic portion (= mesentery of intussusceptum) pseudokidney/sandwich/hay fork sign (on longitudinal scan) = hypoechoic layers on each side of echogenic center of mesenteric fat
pseudokidney/sandwich/hay fork sign (on longitudinal scan) = hypoechoic layers on each side of echogenic center of mesenteric fat peritoneal fluid trapped inside intussusception in <15% (associated with irreducibility + ischemia)
peritoneal fluid trapped inside intussusception in <15% (associated with irreducibility + ischemia) echogenic mesentery contains lymph nodes + cecoappendiceal complex close to base of intussusception
echogenic mesentery contains lymph nodes + cecoappendiceal complex close to base of intussusception color Doppler demonstrates mesenteric vessels dragged between entering + returning wall of intussusceptum
color Doppler demonstrates mesenteric vessels dragged between entering + returning wall of intussusceptum Absence of blood flow within the intussusceptum suggests bowel necrosis (47%)!
Absence of blood flow within the intussusceptum suggests bowel necrosis (47%)! Presence of blood flow within the intussusceptum is a good predictor of reducibility!
Presence of blood flow within the intussusceptum is a good predictor of reducibility!
CT:
 multiple concentric rings = 3 concentric cylinders (central cylinder = canal + wall of intussusceptum; middle cylinder = crescent of mesenteric fat; outer cylinder = returning intussusceptum + intussuscipiens)
multiple concentric rings = 3 concentric cylinders (central cylinder = canal + wall of intussusceptum; middle cylinder = crescent of mesenteric fat; outer cylinder = returning intussusceptum + intussuscipiens) proximal obstruction
proximal obstruction
Hydrostatic/Pneumatic Reduction
<1% mortality if reduction occurs <24 hours after onset!
| Overall success rate: | 70 85% |
| Contraindications: | pneumoperitoneum, peritonitis, hypovolemic shock Obtain abdominal radiograph to document absence of perforation before reduction! |
Technique:
Sedation (debated) with morphine sulfate (0.2 mg/kg IM)/fentanyl citrate IV (straining increases intraluminal pressure of distended colon)
Anal seal with 24-F Foley catheter + balloon inflation to size equal to interpediculate distance of L5; balloon pulled down to levator sling; taped to buttocks; both buttocks firmly taped together
60% wt/vol barium sulfate with container between 24 36 inches above level of anus
Maximally 3 attempts for 3 minutes each
Manual manipulation increases colonic pressure
Reduction should be accomplished within 10 minutes
Extensive reflux into small bowel desirable to exclude residual ileoileal intussusception
rule of 3s :
3.5 feet (105 cm) above table (= 120 mm Hg)
3 attempts
3 minutes between attempts (delay allows venous congestion + edema to subside)
Alternative medium:
1:4 Gastrografin -water solution raised to a height of 5 feet (150 cm)
air: delivers higher intracolonic pressures, faster, less fluoroscopic time, smaller tears, less contamination of peritoneal cavity
Ultrasound-guided saline enema: no limit to procedure time, low perforation rate
P.847
| Cx: | perforation (0.4 3%; colonic bursting pressure ~200 mm Hg); reduction of nonviable bowel; incomplete reduction; missed lead point |
| Prognosis: | 3.5 10% rate of recurrence |
Ischemic Colitis
= nonocclusive ischemic disease (major mesenteric vessels usually patent) characterized by acute onset + rapid clinical and radiographic evolutionary changes
| Etiology: | decrease in blood flow to 20% of normal flow associated with small vessel disease (hypoxia) + reperfusion injury when blood flow is reestablished; injury more severe if terminal vascular branches obstructed rather than proximal mesenteric arcades |
Path:
mucosal congestion, patchy necrosis, ulcerations + submucosal edema and hemorrhage (mucosa + submucosa most sensitive to ischemia)
 Early mucosal injury is reversible
Early mucosal injury is reversible
injury of muscularis propria (after severe + prolonged ischemia) can lead to transmural necrosis
 Fibrotic stricture, perforation, severe sepsis
Fibrotic stricture, perforation, severe sepsis
Precipitating factors:
bowel obstruction: volvulus, carcinoma (proximal dilatation with increased intraluminal pressure and reduced blood flow)
thrombosis: cardiovascular disease, myocardial infarction, digitalis treatment, arrhythmia, oral contraceptives, hypotensive episode, collagen vascular disease, sickle cell disease, hemolytic-uremic syndrome
trauma: aortoiliac reconstruction (2%) with ligation of IMA, cardiac surgery
idiopathic/spontaneous: mainly in elderly
| mnemonic: | VINTS |
Vasculitis
Incarceration (hernia, volvulus)
Nonocclusive ischemia (shock, CHF)
Thrombosis (atherosclerosis, emboli, polycythemia vera, hyperviscosity)
Spontaneous
| Age: | usually >50 years; M = F |
abrupt onset of lower abdominal pain + rectal bleeding
abdominal tenderness, diarrhea
lack of sepsis
negative stool cultures
| Location: | segmental involvement of any part of colon; entire colon (11%); right colon (30%); transverse colon (9%); left colon (46 90%); sigmoid colon (4%); rectum spared; most commonly affected segments:
|
Mean length of segmental involvement: 19 cm
Plain film (usually normal):
 segmental thumbprinting = marginal indentations on mesenteric side (rare finding on plain film)
segmental thumbprinting = marginal indentations on mesenteric side (rare finding on plain film)
BE (in 90% abnormal):
 Single contrast may efface thumbprinting, but double contrast overall is more sensitive!
Single contrast may efface thumbprinting, but double contrast overall is more sensitive! thumbprinting (75%) due to submucosal hemorrhage + edema
thumbprinting (75%) due to submucosal hemorrhage + edema transverse ridging = markedly enlarged mucosal folds (spasm), some wall pliability is preserved
transverse ridging = markedly enlarged mucosal folds (spasm), some wall pliability is preserved serrated mucosa = inflammatory edema + superficial longitudinal/circumferential ulceration
serrated mucosa = inflammatory edema + superficial longitudinal/circumferential ulceration deep penetrating ulcers (late)
deep penetrating ulcers (late)
CT (detection rate of 26 39%):
 symmetric/lobulated segmental thickening of colonic wall between 2 and 20 (mean 8) mm:
symmetric/lobulated segmental thickening of colonic wall between 2 and 20 (mean 8) mm: shaggy configuration + alternate layers of high and low attenuation (double halo sign) + marked pericolic streakiness of edema (wet appearance in 61%)
shaggy configuration + alternate layers of high and low attenuation (double halo sign) + marked pericolic streakiness of edema (wet appearance in 61%) sharply defined homogeneously enhancing wall + mild mural thickening (dry appearance in 33%)
sharply defined homogeneously enhancing wall + mild mural thickening (dry appearance in 33%)
 loss of haustral markings
loss of haustral markings irregular narrowed atonic lumen (= thumbprinting)
irregular narrowed atonic lumen (= thumbprinting) curvilinear collection of intramural gas (6%) suggests bowel infarction
curvilinear collection of intramural gas (6%) suggests bowel infarction portal + mesenteric venous air
portal + mesenteric venous air blood clot in SMA/SMV
blood clot in SMA/SMV
US:
 absence/barely visible color flow
absence/barely visible color flow absence of arterial signals
absence of arterial signals nonstratified (= indistinct layers) thickened bowel wall >3 mm
nonstratified (= indistinct layers) thickened bowel wall >3 mm
Angio (findings similar to inflammatory disease):
 normal/slightly attenuated arterial supply
normal/slightly attenuated arterial supply mild acceleration of arteriovenous transit time
mild acceleration of arteriovenous transit time small tortuous ectatic draining veins
small tortuous ectatic draining veins
Prognosis:
Transient ischemia = complete resolution within 1 3 months (76%)
Stricturing ischemia = incomplete delayed healing
 narrowed foldless segment of several cm in length with smooth tapering margins
narrowed foldless segment of several cm in length with smooth tapering margins
Gangrene with necrosis + perforation (extremely uncommon)
Mortality rate of 11 36%
| DDx: |
|
Jejunal Atresia
 Air may be injected through nasogastric tube
Air may be injected through nasogastric tube BE to exclude 2nd and 3rd areas of atresia
BE to exclude 2nd and 3rd areas of atresia
| Cause: | intrauterine ischemic injury to developing gut |
| Age: | majority presenting during 1st day of life |
| In 25% associated with: | malrotation, volvulus, gastroschisis, omphalocele |
bilious vomiting, abdominal distension, failure to pass meconium
Plain film:
| N.B.: | difficult to tell colon from small bowel in neonate |
 2 3 dilated bowel loops
2 3 dilated bowel loops absence of gas in lower portion of abdomen
absence of gas in lower portion of abdomen
P.848
BE:
| Purpose: | to exclude large-bowel causes of obstruction, show anatomical size of colon, demonstrate meconium ileus |
 microcolon/small colon/colon of normal caliber (due to sufficient intestinal secretions in remaining small bowel)
microcolon/small colon/colon of normal caliber (due to sufficient intestinal secretions in remaining small bowel)
| Cx: | meconium peritonitis (5%) |
Jejunoileal Diverticular Disease
= JEJUNAL DIVERTICULOSIS
= rarest form of gastrointestinal diverticular disease
| Cause: | disordered contractions of smooth muscle results in increased intraluminal pressure and mucosal herniation (= pulsion diverticula = false diverticula) |
| Incidence: | 0.5 1.1 2.3% on UGI; 0.3 4.5% of autopsy series; M > F |
| Age: | 6th 7th decades |
| Location: | 80% in jejunum, 15% in ileum (usually solitary), 5% in jejunum + ileum |
| Site: | on mesenteric border near entrance of vasa recti intermittent upper abdominal pain, flatulence, episodes of diarrhea (30%) |
| Size: | a few millimeters to >10 cm |
Plain film:
 air-fluid levels in multiple diverticula
air-fluid levels in multiple diverticula slight dilatation of intestinal loops in area of diverticula
slight dilatation of intestinal loops in area of diverticula
BE:
 may not fill (narrow neck/stagnant secretions)
may not fill (narrow neck/stagnant secretions) trapped barium on delayed film after 24 hours
trapped barium on delayed film after 24 hours
Cx:
Blind loop syndrome with bacterial overgrowth
steatorrhea, diarrhea, malabsorption, weight loss
megaloblastic anemia (overgrowth of coliform bacteria leads to deconjugation of bile acids + intraluminal metabolism of vitamin B12)
Free perforation = leading cause of pneumo-peritoneum without peritonitis (21 40% mortality)
Hemorrhage (few cases)
Diverticulitis
Intestinal obstruction (enterolith ileus)
Juvenile Polyposis
= rare autosomal dominant disease with variable penetrance characterized by development of multiple (>5) juvenile polyps in GI tract
 Most common familial/nonfamilial colonic polyp in children (75%)!
Most common familial/nonfamilial colonic polyp in children (75%)!Categories:
Juvenile polyposis of infancy
Age: 4 6 years (range 1 10 years); M:F = 3:2 protein-losing enteropathy, diarrhea, hemorrhage
rectal prolapse
 intussusception
intussusception
Colonic & generalized juvenile polyposis
Age: in 85% manifested by 20 years of age prolapse of polyp/rectum
rectal bleeding, anemia
| Path: | hamartomatous polyps; adenomas may coexist |
| Histo: | little/no smooth muscle; hyperplasia of mucous glands; retention cysts develop with obstruction of gland orifices (multiple mucin-filled spaces); edematous inflamed expanded lamina propria |
| DDx: | familial adenomatous polyposis, Peutz-Jeghers syndrome |
rectal bleeding (95%) most commonly as intermittent bright red hematochezia
anemia, pain
diarrhea, constipation
abdominal pain (from intussusception)
rectal prolapse (rare)
| Location: | rectosigmoid (80%); rare in small bowel + stomach; not in esophagus |
 solitary polyp (75%); multiple polyps (1/3) of smooth round contour
solitary polyp (75%); multiple polyps (1/3) of smooth round contour lesion of pinpoint size/up to several cm in diameter
lesion of pinpoint size/up to several cm in diameter invariably on stalk of variable length
invariably on stalk of variable length
| Dx: |
|
| Cx: | colorectal cancer by 35 years of age (in 15%) |
| DDx: | solitary juvenile polyps (<5 polyps, 1% prevalence in children) |
Kaposi Sarcoma
[Moritz Kaposi (1837 1902), dermatologist in Vienna, Austria]
= multicentric malignant neoplasm originating from endothelial cells of lymphatic/blood vessels
| Cause: | HIV regulatory protein (trans-activator target [TAT]) important for viral replication is thought to cause proliferation of Kaposi sarcoma cells |
| Incidence: | most common AIDS-related neoplasm (10 20 34%); in 51% of homosexual/bisexual men with AIDS; rare in hemophiliacs; M:F = 50:1 |
| Histo: | proliferation of spindle cells with numerous extra-vasated RBCs located in clefts between stromal cells |
Types:
Classic Kaposi sarcoma
affecting men of Mediterranean origin in 7th decade
Central African Kaposi sarcoma
AIDS-related Kaposi sarcoma
@ Skin (most frequent site)
multiple bluish red slightly elevated skin lesions
@ Lymph nodes (2nd most frequent site):
 abdominal + pelvic lymphadenopathy with high contrast-enhancement (secondary to vascularity)
abdominal + pelvic lymphadenopathy with high contrast-enhancement (secondary to vascularity)Associated with high frequency of GI tract involvement
@ GI tract (40 50%, 3rd most frequent site):
usually clinically silent
concurrent with/after cutaneous disease
 GI tract is the only site of involvement in <5%!
GI tract is the only site of involvement in <5%!
Location: anywhere within GI tract; often multifocal  thickened nodular folds
thickened nodular folds multiple submucosal nodules central umbilication
multiple submucosal nodules central umbilication polypoidal mass
polypoidal mass infiltrating linitis plastica lesion (rare)
infiltrating linitis plastica lesion (rare)
@ Liver (34% at autopsy)
infrequently contributes to morbidity + mortality
 multiple 5 12-mm nodules hyperechoic on US, hypoattenuating on NECT/CECT indistinguishable from multiple hemangiomas
multiple 5 12-mm nodules hyperechoic on US, hypoattenuating on NECT/CECT indistinguishable from multiple hemangiomas
P.849
DDx: metastatic disease, fungal microabscesses, multiple areas of bacillary angiomatosis (= swollen venous lakes in liver) @ Lung (18 47% of patients with cutaneous sarcoma):
= late complication of AIDS
Site: peribronchial + perivascular axial interstitium (91%); middle/lower lung zones (92%)  coarsening of bronchovascular bundles:
coarsening of bronchovascular bundles: tram track opacities
tram track opacities peribronchial cuffing
peribronchial cuffing septal lines (38 71%)
septal lines (38 71%)
 central perihilar coalescent consolidation air bronchograms in 45% (= confluent tumor)
central perihilar coalescent consolidation air bronchograms in 45% (= confluent tumor) small (50%)/large (28%) pulmonary nodules (= tumor proliferation extending into parenchyma)
small (50%)/large (28%) pulmonary nodules (= tumor proliferation extending into parenchyma) pleural effusion (33 67%), chylothorax (rare)
pleural effusion (33 67%), chylothorax (rare) moderate lymphadenopathy (16%)
moderate lymphadenopathy (16%)
@ Lower extremities
 lytic cortical lesion
lytic cortical lesion subcutaneous nodules
subcutaneous nodules
| Dx: | visualization + biopsy of mass with red-purple color |
Ladd Bands
= congenital peritoneal bands extending from cecum/hepatic flexure over anterior surface of 2nd/3rd portion of duodenum causing duodenal obstruction at its 2nd portion (even without volvulus)
| Associated with: | malrotation |
 oblique termination of duodenal contrast column
oblique termination of duodenal contrast column
Leiomyoma
| Location: | 2/3 occur in stomach |
| Path: | arising from muscularis propria/submucosa/muscularis mucosae/smooth muscle of blood vessels within wall of viscus |
| Histo: | intersecting bands of muscle + fibrous tissue in a well-defined capsule difficult to differentiate from leiomyosarcoma |
| DDx: | fibroma, neurofibroma, hemangioma |
Esophageal Leiomyomatosis
| Age: | 6 18 (mean of 11) years; M > F |
| Cause: |
|
| Site: | distal third/half of esophagus extension into proximal stomach |
slowly progressive dysphagia over years
 smooth tapered narrowing of distal esophagus over an average length of 6 cm
smooth tapered narrowing of distal esophagus over an average length of 6 cm decreased/absent esophageal peristalsis
decreased/absent esophageal peristalsis smooth relatively symmetric defect at cardia (from thickened muscle bulging into gastric fundus)
smooth relatively symmetric defect at cardia (from thickened muscle bulging into gastric fundus)CT:
 marked circumferential wall thickening of up to 4 cm from mass with relatively low soft-tissue attenuation
marked circumferential wall thickening of up to 4 cm from mass with relatively low soft-tissue attenuation
DDx: - Primary achalasia (shorter narrowed segment)
- Secondary achalasia (older individual, recent onset of dysphagia)
- Stricture from reflux esophagitis
- Idiopathic muscular hypertrophy of the esophagus (in late adulthood, corkscrew appearance of esophagus with nonperistaltic contractions, cardia rarely involved)
Leiomyoma of Esophagus
 Most common benign submucosal tumor of esophagus
Most common benign submucosal tumor of esophagus
| Incidence: | 1:1,119 (autopsy study); 50% of all benign esophageal tumors |
| Age: | young adults; 3% in children; M > F |
usually asymptomatic (due to slow growth)
dysphagia, odynophagia, dyspepsia
hematemesis if large (rare)
| Site: | frequently lower + mid 1/3 of esophagus; intramural; multiple leiomyomas in 3 4% |
 2 15-cm large smooth well-defined intramural mass
2 15-cm large smooth well-defined intramural masscausing eccentric thickening of wall + deformity of lumen
 may have coarse calcifications:
may have coarse calcifications: Leiomyoma is the only calcifying esophageal tumor!
Leiomyoma is the only calcifying esophageal tumor!
 ulceration extremely uncommon
ulceration extremely uncommonCT:
 uniform soft-tissue density
uniform soft-tissue density diffuse contrast enhancement
diffuse contrast enhancement
| CAVE: | high percentage misdiagnosed as extrinsic lesion! |
Leiomyoma of Small Bowel
Most common benign tumor of small bowel
| Location: | duodenum (21%), jejunum (48%), ileum (31%); single in 97% |
| Site: | mainly serosal (50%), mainly intraluminal (20%), intramural (10%) |
| Size: | <5 cm (50%), 5 10 cm (25%), >10 cm (25%) |
 small ulcer + large barium-filled cavity (central necrosis + communication with lumen)
small ulcer + large barium-filled cavity (central necrosis + communication with lumen) hypervascular
hypervascular
Leiomyoma of Stomach
 2nd most common benign gastric tumor (after gastric polyp), most common of calcified benign tumors
2nd most common benign gastric tumor (after gastric polyp), most common of calcified benign tumors
| Location: | pars media (39%), antrum (26%), pylorus (12%), fundus (12%), cardia (10%) |
| Site: | intraluminal submucosal (60%), exophytic subserosal (35%), combined intramural-extramural dumbbell type mass (5%) 90% of all submucosal tumors! |
 average size of 4.5 cm
average size of 4.5 cm ovoid mass with smooth margin + smooth surface (most frequently)
ovoid mass with smooth margin + smooth surface (most frequently) forms right angle with gastric wall
forms right angle with gastric wall ulcerated in 50%
ulcerated in 50% pedunculated intraluminal tumor in submucosal growth (rare)
pedunculated intraluminal tumor in submucosal growth (rare) iceberg phenomenon = large extraluminal component in subserosal growth
iceberg phenomenon = large extraluminal component in subserosal growth calcifies in 4%
calcifies in 4%
P.850
| Cx: |
|
Leiomyosarcoma
Leiomyosarcoma of Small Bowel
| Location: | duodenum (26%), jejunum (34%), ileum (40%) |
 usually >6 cm in size
usually >6 cm in size nodular mass: intraluminal (10%), intraluminal pedunculated (5%), intramural (15%), chiefly extrinsic (66%)
nodular mass: intraluminal (10%), intraluminal pedunculated (5%), intramural (15%), chiefly extrinsic (66%) mucosa may be stretched + ulcerated (50%)
mucosa may be stretched + ulcerated (50%) may show central ulcer pit/fistula communicating with a large necrotic center
may show central ulcer pit/fistula communicating with a large necrotic center intussusception
intussusception
Leiomyosarcoma of Stomach
| Incidence: | 0.1 3% of all gastric malignancies |
| Age: | 10 73 years; M > F |
| Histo: | pleomorphism, hypercellularity, mitotic figures, cystic degeneration, necrosis |
GI bleeding (from ulceration)
obstruction
Metastases:
hematogenous to liver, lung, peritoneum; rarely to bone + soft tissue
direct extension into omentum, retroperitoneum
lymph nodes (rare)
| Location: | 90% in fundus/body of stomach |
| Site: | anterior/posterior wall; endo-/exogastric |
 average size of 12 cm
average size of 12 cm intramural mass
intramural mass may be pedunculated
may be pedunculated large masses tend to be exogastric
large masses tend to be exogastric very frequently ulcerated
very frequently ulceratedCT:
 lobulated irregular outline
lobulated irregular outline heterogeneous exogastric mass with central zones of low density (necrosis with liquefaction)
heterogeneous exogastric mass with central zones of low density (necrosis with liquefaction) air/positive contrast within tumor (= ulceration)
air/positive contrast within tumor (= ulceration) dystrophic calcifications
dystrophic calcifications
Carney Triad
| Triad of |
|
| Incidence: | 24 patients reported; M:F = 1:11 |
Lipoma
= benign submucosal tumor composed of mature adipose tissue
 Most common submucosal tumor in colon
Most common submucosal tumor in colon
| Incidence: | in colon in 0.25% (autopsy); 2 3% of benign gastric tumors |
| Location: | colon (particularly cecum + ascending colon) > duodenum > ileum > stomach (gastric antrum) > jejunum > esophagus |
asymptomatic
crampy pain, hemorrhage (rare)
 smooth, sharply outlined, round/ovoid globular mass of 1 3 cm in diameter
smooth, sharply outlined, round/ovoid globular mass of 1 3 cm in diameter short thick pedicle in 1/3 caused by repeated peristaltic activity (prone to intussuscept)
short thick pedicle in 1/3 caused by repeated peristaltic activity (prone to intussuscept) marked radiolucency
marked radiolucency change in shape + size on compression due to softness:
change in shape + size on compression due to softness: squeeze sign = sausage-shaped mass on postevacuation radiographs
squeeze sign = sausage-shaped mass on postevacuation radiographs
CT:
 well-circumscribed submucosal mass of uniform fat density
well-circumscribed submucosal mass of uniform fat density
| Cx: |
|
| Prognosis: | NO liposarcomatous degeneration |
Lymphangioma
= congenital malformation of lymphatic vessels
| Path: | usually multiloculated large thin-walled cystic mass with chylous/serous/hemorrhagic fluid contents |
| Location: | mesentery; rarely affecting GI tract |
 proximal bowel dilatation (in partial bowel obstruction)
proximal bowel dilatation (in partial bowel obstruction)US:
 multiseptated cystic mass with lobules
multiseptated cystic mass with lobules fluid anechoic/with internal echoes/sedimentation
fluid anechoic/with internal echoes/sedimentation
CT:
 cystic mass with contents of water- to fat-density
cystic mass with contents of water- to fat-density
MR:
 serous contents: hypointense on T1WI + hyperintense on T2WI
serous contents: hypointense on T1WI + hyperintense on T2WI hemorrhage/fat: hyperintense on T1WI + T2WI
hemorrhage/fat: hyperintense on T1WI + T2WI
| Rx: | surgery (difficult due to intimate attachment to bowel wall) |
Lymphogranuloma Venereum
= LGV = sexually transmitted disease caused by virus Chlamydia trachomatis producing a nonspecific granulomatous inflammatory response in infected mucosa (mononuclear cells + macrophages), perirectal lymphatic invasion
| Location: | rectum, extension to sigmoid + descending colon M:F = 3.4:1 |
 narrowing + shortening + straightening of rectosigmoid
narrowing + shortening + straightening of rectosigmoid widening of retrorectal space
widening of retrorectal space irregularity of mucosa + ulcerations
irregularity of mucosa + ulcerations paracolic abscess
paracolic abscess fistula to pericolic area, rectum, vagina (common)
fistula to pericolic area, rectum, vagina (common)
| Rx: | tetracyclines effective in acute phase before scarring has occurred |
Lymphoid Hyperplasia
| Incidence: | normal variant in 13% of BE examinations |
| Histo: | hyperplastic lymph follicles in lamina propria (Peyer patches), probably compensatory attempt for immunoglobulin deficiency |
Etiology:
Normal in child/young adult
Self-limiting local/systemic inflammation/infection/allergy
May be related to immunodeficiency/dysgammaglobulinemia with small bowel involvement
P.851
| Age: |
|
| Associated with: | splenomegaly, large tonsils, eczematous dermatitis, achlorhydria, pernicious anemia, acute pancreatitis, colonic carcinoma |
At risk for:
Good syndrome (10%)
= gastric carcinoma + benign thymoma + lymphoid hyperplasia
Respiratory infections
Giardia lamblia infection (90%)
Functional thyroid abnormalities
| Location: | primarily jejunum, may involve entire small bowel, ascending colon + hepatic flexure, seldom in sigmoid/rectum |
malabsorption (diarrhea + steatorrhea)
low serum concentrations of IgA, IgG, IgM
 mucosa studded with innumerable 1 3-mm small uniform polypoid lesions
mucosa studded with innumerable 1 3-mm small uniform polypoid lesions lesions may be umbilicated (uncommon)
lesions may be umbilicated (uncommon)
Lymphoma of Gastrointestinal Tract
Classification:
PRIMARY LYMPHOMA OF BOWEL
localized
diffuse
Predisposed: Arabs + Middle Eastern Jews Associated with: celiac disease SECONDARY INTESTINAL LYMPHOMA
as part of generalized systemic process
| Incidence: | 4 20% of all NHL; 10% of patients with abdominal lymphoma have bowel involvement |
| At risk: | long-standing celiac disease, AIDS, systemic lupus erythematosus, Crohn disease, history of chemotherapy |
| Median age: | 60 years |
Histo:
B-cell lymphoma (most common)
T-cell lymphoma (in celiac disease/peripheral T-cell lymphoma)
Immunoproliferative small intestinal disease
(= Mediterranean/Middle Eastern lymphoma) in young patients of poor socioeconomic status
Low-grade B-cell lymphoma (= low-grade mucosa-associated lymphoid tissue = MALT lymphoma)
50 72% of all primary gastric lymphomas;
Associated with: Helicobacter pylori gastritis in 90% (may regress completely after antibiotic therapy) Follicular lymphoma
Burkitt lymphoma (in children)
Mantle cell lymphoma
Hodgkin disease (<15%)
| May be associated with: | enlargement of extraabdominal lymph nodes, malabsorption |
Radiographic types:
Polypoid/nodular (47%)
 enlarged nodular folds
enlarged nodular folds
Ulcerative (42%)
 ulcerative lesions, may be complicated by perforation
ulcerative lesions, may be complicated by perforation aneurysmal configuration
aneurysmal configuration
Diffusely infiltrating (11%)
 diffuse hoselike thickening of bowel wall
diffuse hoselike thickening of bowel wall decreased/absent peristalsis
decreased/absent peristalsis
CT staging:
| Stage I | tumor confined to bowel wall |
| Stage II | limited to local nodes |
| Stage III | widespread nodal disease |
| Stage IV | disseminated to bone marrow, liver, other organs |
| Location: | 10 25% of NHL are extranodal; stomach (50%) > small bowel > colon > esophagus; multicentric in 10 50% |
 enlargement of spleen
enlargement of spleen bulky enlargement of regional lymph nodes
bulky enlargement of regional lymph nodes@ Esophagus
least common site of GI involvement (in <1%)
@ Stomach
1 5% of all gastric malignancies; most common site of extranodal lymphoma (25%); most frequent site of involvement by NHL (50%); isolated primary gastric malignancy in 10%
Location: no predilection for any particular region of stomach Site: arises in lymphoid tissue of lamina propria that forms secondary to chronic Helicobacter pylori gastritis (normally gastric mucosa has no lymphoid tissue!) Direct extension into: pancreas, spleen, transverse colon, liver  pliant gastric wall
pliant gastric wall duodenum often affected when antrum involved
duodenum often affected when antrum involved circumscribed mass with endogastric/exogastric (25%) growth
circumscribed mass with endogastric/exogastric (25%) growth broad tortuous mucosal folds over large portions of stomach (diffuse form):
broad tortuous mucosal folds over large portions of stomach (diffuse form): polypoid/nodular
polypoid/nodular
 large irregular ulcer
large irregular ulcer rarely luminal narrowing
rarely luminal narrowingCT:
 diffuse involvement of entire stomach (50%), typically more than half of gastric circumference
diffuse involvement of entire stomach (50%), typically more than half of gastric circumference segmental involvement (15%)
segmental involvement (15%) ulcerated mass (8%)
ulcerated mass (8%) average wall thickness of 4 5 cm
average wall thickness of 4 5 cm luminal irregularity (66%)
luminal irregularity (66%) hyperrugosity (58%)
hyperrugosity (58%)
Prognosis: 55% 5-year survival rate after resection DDx: gastric adenocarcinoma (wall thickening less pronounced, perigastric fat plane not likely preserved, luminal narrowing, rigid wall, smaller lymph nodes above the level of renal veins) @ Small bowel
1/5 of all small bowel malignancies; most common malignant small bowel tumor; multiple sites of involvement in 1/5; most common cause of intussusception in children >6 years
P.852
Location: ileum (51%), jejunum (47%), duodenum (2%) Site: arising from lymphoid patches of Peyer Radiographic types:
Nodular pattern
 cobblestone defects due to lymphomatous polyps
cobblestone defects due to lymphomatous polyps mucosal/submucosal nodules may ulcerate
mucosal/submucosal nodules may ulcerate may cause intussusception
may cause intussusception sprue pattern
sprue pattern
Single mass
 intussusception
intussusception obstruction unusual (soft + pliable tumor
obstruction unusual (soft + pliable tumor
Infiltrating pattern
 plaquelike thickening of wall >5 cm in length (80%)/>10 cm in length (20%) (DDx: Crohn disease)
plaquelike thickening of wall >5 cm in length (80%)/>10 cm in length (20%) (DDx: Crohn disease) ulceration (considerable excavation)
ulceration (considerable excavation) desmoplastic response
desmoplastic response thickened valvulae with corrugated appearance
thickened valvulae with corrugated appearance aneurysmal dilatation in up to 50% (secondary to destruction of autonomic nerve plexus + muscle/tumor necrosis)
aneurysmal dilatation in up to 50% (secondary to destruction of autonomic nerve plexus + muscle/tumor necrosis) obstruction unusual (soft + pliable tumor
obstruction unusual (soft + pliable tumor
Exophytic = endoexoenteric mass
 large mass with only small intramural component
large mass with only small intramural component ulcer + fistulas + aneurysmatic dilatation
ulcer + fistulas + aneurysmatic dilatation
DDx: adenocarcinoma, GIST Mesenteric/retroperitoneal adenopathy
 single/multiple extraluminal masses displacing bowel
single/multiple extraluminal masses displacing bowel ill-defined confluent mass engulfing + encasing multiple loops of adjacent bowel
ill-defined confluent mass engulfing + encasing multiple loops of adjacent bowel sandwich configuration = mass surrounding mesenteric vessels that are separated by perivascular fat
sandwich configuration = mass surrounding mesenteric vessels that are separated by perivascular fat conglomerate mantle of retroperitoneal + mesenteric mass
conglomerate mantle of retroperitoneal + mesenteric mass
@ Colon
Less commonly involved than stomach/small bowel; 1.5% of all abdominal lymphomas
Location: cecum most commonly involved (85%)  single mass > diffuse infiltration > polypoid lesion
single mass > diffuse infiltration > polypoid lesion paradoxical dilatation
paradoxical dilatation gross mural circumferential/focal soft-tissue thickening (average size of 5 cm)
gross mural circumferential/focal soft-tissue thickening (average size of 5 cm) slight enhancement
slight enhancement massive regional + distant mesenteric + retroperitoneal adenopathy
massive regional + distant mesenteric + retroperitoneal adenopathy
| DDx: | frequently resembles inflammatory disease/polyposis |
| Prognosis: |
|
| Cx during chemotherapy: | perforation (9 40%), hemorrhage |
Peripheral T-Cell Lymphoma
| Incidence: | 5 30% of all NHL |
| Age: | middle age + elderly |
| Histo: | mature T-cell phenotype |
| Location: | bone marrow, skin, lung, liver, GI tract (4 6%) |
| Site: | small intestine (64%, esp. duodenum + jejunum) |
malabsorption
 multifocal bowel involvement (50 72% compared with 10 25% in B-cell lymphoma)
multifocal bowel involvement (50 72% compared with 10 25% in B-cell lymphoma) bowel perforation with pneumoperitoneum (41 50% compared with <30% in B-cell lymphoma)
bowel perforation with pneumoperitoneum (41 50% compared with <30% in B-cell lymphoma) mild (<1 cm)/moderate (1 2 cm) gastric/bowel thickening
mild (<1 cm)/moderate (1 2 cm) gastric/bowel thickening polypoid mass (rare; common in B-cell lymphoma)
polypoid mass (rare; common in B-cell lymphoma) thickened plaques, ulcers, strictures (compared with exophytic/annular masses in B-cell lymphoma)
thickened plaques, ulcers, strictures (compared with exophytic/annular masses in B-cell lymphoma) nonbulky lymphadenopathy (compared with bulky lymphadenopathy in B-cell lymphoma)
nonbulky lymphadenopathy (compared with bulky lymphadenopathy in B-cell lymphoma) hepatosplenomegaly
hepatosplenomegaly
Malignant Melanoma
= develops from melanocytes derived from neural crest cells, arising in preexisting benign nevi (in 20%)
| Incidence: | 1% of all cancers; increasing at 3.9% per year |
| Peak prevalence: | 40 60 years of age |
| Risk factors: | dysplastic mole, atypical melanocytic hyperplasia, xeroderma pigmentosum, melanoma in first-degree relative, sun-sensitive phenotype, excessive sun exposure |
| Sites: | skin, mucous membranes, leptomeninges, eye |
areas of red/white/blue in addition to brown and black colors of benign nevi
irregular borders with notching + striking protrusions
@ Skin primary
Clark staging: Level I all tumor cells above basement membrane (in situ lesion) Level II tumor extends to papillary dermis Level III tumor extends to interface between papillary + reticular dermis Level IV tumor extends between bundles of collagen of reticular dermis Level V tumor invasion of subcutaneous tissue (in 87% metastatic) Breslow staging: thin <0.75 mm depth of invasion intermediate 0.76 3.99 mm depth of invasion thick >4 mm depth of invasion METASTASES:
latent period of 2 20 years after initial diagnosis (most commonly 2 5 years)
Primary site: head + neck (79%), eye (77%), GU system (67%), GI tract (in up to 60%) @ Lymphadenopathy
in 23% with level II + IV
in 75% with level V
sentinel node biopsy:
 intraoperative intradermal injection of dye
intraoperative intradermal injection of dye preoperative lymphoscintigraphy
preoperative lymphoscintigraphy
@ Bone (7 17%)
Prevalence: 30 40% at autopsy often initial manifestation of recurrence
poor prognosis
 predominantly osteolytic
predominantly osteolytic
Location: axial skeleton (80%), ribs (38%) @ Lung (70% at autopsy)
most common site of relapse; respiratory failure most common cause of death
@ Liver (17 23%; 58 66% at autopsy)
 single/multiple lesions 0.5 15 cm in size
single/multiple lesions 0.5 15 cm in size larger lesion often necrotic
larger lesion often necrotic may be partially calcified
may be partially calcified
@ Spleen (1 5%; 33% at autopsy)
 single/multiple lesions of variable size
single/multiple lesions of variable size solid/cystic
solid/cystic
@ GI tract + mesentery (4 8%)
abdominal pain, GI bleeding
Location: small intestine (35 50%), colon (14 20%), stomach (7 20%)  multiple submucosal nodules bull's-eye/target appearance = central ulceration
multiple submucosal nodules bull's-eye/target appearance = central ulceration irregular amorphous cavity (exoenteric growth)
irregular amorphous cavity (exoenteric growth) intussusception (10 20%)
intussusception (10 20%)
@ Kidney (up to 35% at autopsy)
@ Adrenal (11%, up to 50% at autopsy)
@ Subcutis
MR of melanotic melanoma:
 hypo-/isointense on T1WI + T2WI + STIR images (most commonly)
hypo-/isointense on T1WI + T2WI + STIR images (most commonly) hyperintense on T1WI + hypointense on T2WI (due to T1-shortening effect of the paramagnetic metals iron + copper bound to melanin)
hyperintense on T1WI + hypointense on T2WI (due to T1-shortening effect of the paramagnetic metals iron + copper bound to melanin)
P.853
| DDx: | melanotic/amelanotic hemorrhagic tumor (hyperintense on T1WI + iso-/hyperintense on T2WI) |
| Prognosis: | 30 40% eventually die from this tumor |
Mallory-Weiss Syndrome
= mucosal + submucosal tear with involvement of venous plexus
| Pathophysiology: | violent projection of gastric contents against lower esophagus |
| Age: | 30 60 years; M > F |
| Predisposed: | alcoholics |
history of repeated vomiting prior to hematemesis
massive painless hematemesis
| Location: | at/above/below (76%) esophagogastric junction |
 longitudinal single tear in 77%, in 23% multiple tears
longitudinal single tear in 77%, in 23% multiple tears extravasation of barium
extravasation of bariumAngio:
 bleeding site at gastric cardia
bleeding site at gastric cardia
| DDx: | peptic ulcer/ulcerative gastritis |
Malrotation
abnormal position of gut secondary to a narrow mesenteric attachment as a result of arrest in the embryologic development of gut rotation + fixation
Embryology:
duodenojejunal + ileocolic segments of primitive digestive tube rotate by 270 in a counterclockwise direction about the omphalomesenteric vessels to cross beneath the vessels (future SMA + SMV); normally LUQ fixation at ligament of Treitz (an extension of the right crus of diaphragm) + fibrous tissue around celiac artery, located to left of L2) + RLQ fixation of cecum
Abnormal fixation of mesentery: shorter than usual, its upper point below the normal position of ligament of Treitz, its lower point superior + medial to normal cecal position
| Associated with: | urinary pseudoobstruction, prune-belly syndrome, cloacal exstrophy |
symptoms of partial/complete proximal bowel obstruction:
vomiting (77% of neonates; in 39% within 1st week of life)
recurrent attacks of vomiting + distension (in older children)
Barium meal & barium enema:
Purpose: guess the location of abnormal peritoneal fixation from position of bowel!  clearly abnormal position of duodenum (81%):
clearly abnormal position of duodenum (81%): duodenum + jejunum to the right of spine (30%)
duodenum + jejunum to the right of spine (30%) corkscrew duodenum + jejunum (29%)
corkscrew duodenum + jejunum (29%) duodenojejunal junction low + in midline (22%)
duodenojejunal junction low + in midline (22%)
 unusual abnormal position of duodenum (16%):
unusual abnormal position of duodenum (16%): duodenojejunal junction over right pedicle
duodenojejunal junction over right pedicle duodenojejunal junction to left of spine but low
duodenojejunal junction to left of spine but low duodenal redundancy to right of spine
duodenal redundancy to right of spine Z-shape configuration of duodenum + jejunum
Z-shape configuration of duodenum + jejunum
 small bowel on right + colon on left side of abdomen (in 0.2% incidental finding in adults)
small bowel on right + colon on left side of abdomen (in 0.2% incidental finding in adults) abnormal position of duodenum + cecum (84%)
abnormal position of duodenum + cecum (84%) normal position of duodenum (3%)
normal position of duodenum (3%) normal position of cecum (in 5 20%)
normal position of cecum (in 5 20%)DDx: mobile cecum (15%)
CT:
 SMV positioned to left of SMA (80%)
SMV positioned to left of SMA (80%) aplastic/hypoplastic uncinate process of pancreas
aplastic/hypoplastic uncinate process of pancreas
| Cx: | midintestinal/midgut volvulus, duodenal obstruction, Ladd bands, internal herniation |
Nonrotation
= midgut loop returns to peritoneal cavity without rotation resulting in weak peritoneal fixation
| Frequency: | common |
generally asymptomatic: often incidental finding in older children + adults
 SMA to right of SMV
SMA to right of SMV large intestine on left + small intestine on right
large intestine on left + small intestine on right
| Cx: | volvulus (as a result of local clockwise rotation) with whirl sign around SMA |
Incomplete Rotation
= failure of midgut loop to complete final 90 of rotation
prearterial segment of midgut reenters abdomen first toward left side
 cecum just inferior to pylorus
cecum just inferior to pylorus
| Cx: | duodenal obstruction (peritoneal bands pass over duodenum) |
Reversed Rotation
| Frequency: | rare |
postarterial segment of midgut reenters abdomen first
= cecum migrates first passing behind SMA toward right thus unwinding the normal counterclockwise rotation of the first stage with additional final 90 clockwise rotation
 duodenum anterior to SMA
duodenum anterior to SMA transverse colon behind duodenum + SMA
transverse colon behind duodenum + SMA
P.854
| Cx: | obstruction of transverse colon by pressure from SMA |
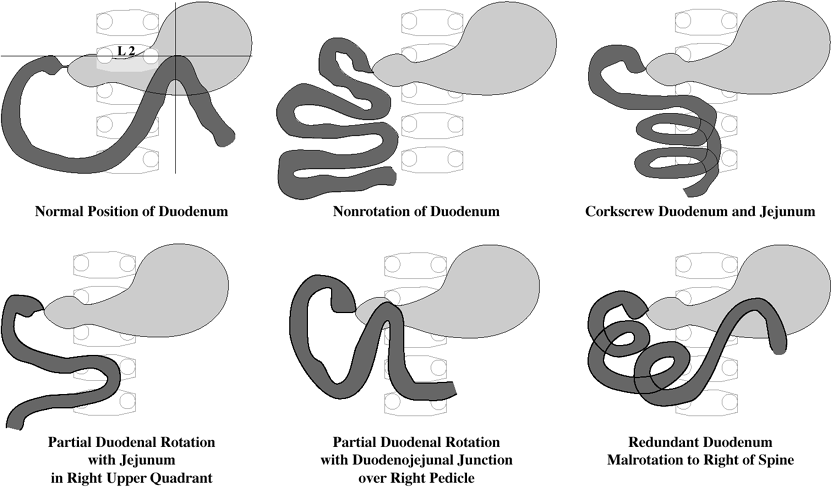 |
| Malrotation |
Mastocytosis
= URTICARIA PIGMENTOSA
= systemic disease with mast cell proliferation in skin and RES (lamina propria of small bowel; bone; lymph nodes; liver; spleen) associated with eosinophils + lymphocytes
| Age: | <6 months old (in 50%) |
| Associated with: | myeloproliferative disorders, acute nonlymphatic leukemia, malignant lymphoma, mast cell leukemia |
Categories:
| I | indolent mastocytosis (most frequent) |
| II | mastocytosis associated with myeloproliferative/myelodysplastic hematologic disorder |
| III | aggressive/lymphadenopathic mastocytosis with eosinophilia |
| IV | mast cell leukemia (rare) |
diarrhea, malabsorption, steatorrhea, anorexia
urticaria pigmentosa = cutaneous form (in 80 90%):
hyperpigmented skin lesions exhibiting wheal and flare phenomenon when disturbed
abdominal pain, nausea, vomiting
tachycardia, asthma, flushing, gastrointestinal upset, headache, pruritus (due to liberation of histamine/prostaglandin D2)
caused by: physical exertion, heat, certain foods, alcohol, nonsteroidal antiinflammatory drugs pancytopenia (chronic neutropenia)
@ Skeletal involvement (70%)
bone and joint pain
 osteoporosis (due to release of heparin + prostaglandin by mast cells activating osteoclasts)
osteoporosis (due to release of heparin + prostaglandin by mast cells activating osteoclasts) scattered well-defined sclerotic foci with focal/diffuse involvement (due to release of histamine by mast cells promoting osteoblastic activity); often alternating with areas of bone rarefaction
scattered well-defined sclerotic foci with focal/diffuse involvement (due to release of histamine by mast cells promoting osteoblastic activity); often alternating with areas of bone rarefaction
Predilected sites: skull, spine, ribs, pelvis, humerus, femur @ Reticuloendothelial system
 hepatomegaly
hepatomegaly splenomegaly (43 61%)
splenomegaly (43 61%) lymphadenopathy: retroperitoneal, periportal, mesenteric
lymphadenopathy: retroperitoneal, periportal, mesenteric Budd-Chiari hepatic venoocclusive disease
Budd-Chiari hepatic venoocclusive disease reversed portal venous flow
reversed portal venous flow cavernous transformation of portal vein
cavernous transformation of portal vein
@ Abdomen
nausea, vomiting, diarrhea
 thickening of omentum, + mesentery
thickening of omentum, + mesentery ascites:
ascites:transudative secondary to liver disease
exudative from mast cell proliferation of peritoneum
@ Small bowel
 generalized irregular distorted nodular thickened folds wall thickening (due to infiltration by mast cells, lymphocytes, plasma cells)
generalized irregular distorted nodular thickened folds wall thickening (due to infiltration by mast cells, lymphocytes, plasma cells) diffuse pattern of 2 3-mm sandlike mucosal nodules
diffuse pattern of 2 3-mm sandlike mucosal nodules urticaria-like lesions of gastric + intestinal mucosa
urticaria-like lesions of gastric + intestinal mucosa
| Dx: | skin/bone marrow biopsy; jejunal biopsy demonstrates an excess of mast cells |
| Cx: |
|
| Rx: | antihistamines, histamine decarboxylase inhibitors, sodium chromoglycase; steroids; splenectomy (for symptomatic splenomegaly/hypersplenism) |
| DDx: | carcinoid, pheochromocytoma |
P.855
Meckel Diverticulum
= persistence of the omphalomesenteric duct (= vitelline duct), which usually obliterates by 5th embryonic week
 Most common congenital abnormality of the GI tract!
Most common congenital abnormality of the GI tract!
| Incidence: | 0.3 2 3% of population (at autopsy) |
| Age: | majority in children <10 years of age; M:F = 3:1 |
| Histo: | contains ectopic mucosa in 50%: gastric/pancreatic/colonic mucosa Frequency of heterotopic gastric mucosa: 15 34% overall; 50% in symptomatic patients; in >95% with GI hemorrhage |
| Location: | within terminal 6 feet of ileum (= 30 100 cm from ileocecal valve); in 94% on antimesenteric border asymptomatic (20 40%) |
| RULE OF 2s: |
|
NUC = Meckel scan (>85% sensitive, >95% specific, >83 88% accurate):
 Tc-99m pertechnetate is excreted by mucoid cells of gastric mucosa, excretion is not dependent on presence of parietal cells
Tc-99m pertechnetate is excreted by mucoid cells of gastric mucosa, excretion is not dependent on presence of parietal cells
N.B.: sensitivity drops after adolescence, because patients asymptomatic throughout childhood are less likely to have ectopic gastric mucosa Preparation:
No irritative measures for 48 hours (contrast studies, endoscopy, cathartics, enemas, drugs irritating GI tract)
Fasting for 3 6 hours (results in decreased gastric secretion + diminished bowel peristalsis)
Evacuation of bowel + bladder prior to study
Dose: 5 10 20 mCi (100 Ci/kg) Tc-99m pertechnetate (adult dose!) Radiation dose: 0.54 rad/2 mCi for thyroid;
0.3 rad/2 mCi for large intestine;
0.2 rad/2 mCi for stomachImaging: immediate continuous anterior imaging for 30 45 minutes/serial images in 5 10-minute intervals for up to 1 hour  small focal collection of tracer in RLQ appearing at the same time/shortly after gastric activity
small focal collection of tracer in RLQ appearing at the same time/shortly after gastric activity tracer activity increases in intensity with time parallel to that of stomach
tracer activity increases in intensity with time parallel to that of stomach improved visualization through
improved visualization throughpentagastrin = stimulates uptake (6 g/kg SC 20 minutes prior to pertechnetate)
cimetidine = inhibits secretion (maximum 300 mg/dose IV 1 hour prior)
glucagon = decreases peristalsis (50 g/kg IM 5 10 minutes prior)
 poor visualization with use of perchlorate + atropine (= depressed uptake)
poor visualization with use of perchlorate + atropine (= depressed uptake)False-positive results:
Ectopic gastric mucosa in gastrogenic cyst, enteric duplication, normal small bowel, Barrett esophagus
Increased blood pool in AVM, hemangioma, hypervascular tumor, aneurysm
Duodenal ulcer, ulcerative colitis, Crohn disease, appendicitis, laxative abuse
Intussusception, intestinal obstruction, volvulus
Urinary tract obstruction, caliceal diverticulum
Anterior meningomyelocele
Poor technique
mnemonic: HA GUIDI Hemangioma
Appendicitis
Gastric ectopia
Urinary obstruction
Intussusception
Duplication of bowel
Inflammatory bowel disease
False-negative results:
Insufficient mass of ectopic gastric mucosa
Dilution of intraluminal activity (hemorrhage/hypersecretion)
mnemonic: MIS Malrotation of ileum
Irritable bowel in RLQ (rapid transit)
Small amount of ectopic gastric mucosa
Enteroclysis:
 elongated, smoothly marginated, clublike, intraluminal mass parallel to long axis of distal ileum = inverted Meckel diverticulum (20%)
elongated, smoothly marginated, clublike, intraluminal mass parallel to long axis of distal ileum = inverted Meckel diverticulum (20%) 0.5 20-cm-long blind pouch on the antimesenteric border of ileum with junctional fold pattern
0.5 20-cm-long blind pouch on the antimesenteric border of ileum with junctional fold pattern
Angio (59% accuracy):
 presence of vitelline artery (= anomalous end branch of superior mesenteric artery) is PATHOGNOMONIC
presence of vitelline artery (= anomalous end branch of superior mesenteric artery) is PATHOGNOMONIC
Cx (in 4 20 40%):
painless GI bleeding secondary to ulceration (in 95% due to heterotopic gastric mucosa) in children <5 years of age
Acute diverticulitis
Intestinal obstruction secondary to intussusception (diverticulum acts as lead point)/volvulus (when omphalomesenteric diverticulum attached to umbilicus by fibrous band) in older children/adults
Malignant tumor (rare): carcinoma, sarcoma, carcinoid
Chronic abdominal pain
Meconium Ileus
= small bowel obstruction secondary to desiccated meconium pellets impacted in distal ileum
| Age: | may develop in utero (in 15%) |
Associated with:
cystic fibrosis with tenacious + sticky meconium due to deficiency of pancreatic secretions (in almost 100%)
 Virtually all infants with meconium ileus prove to have cystic fibrosis
Virtually all infants with meconium ileus prove to have cystic fibrosis 10 15% of infants with cystic fibrosis present with meconium ileus!
10 15% of infants with cystic fibrosis present with meconium ileus!P.856
Earliest clinical manifestation of cystic fibrosis!
abdominal distension, bilious emesis
failure to pass meconium within 48 hours
 numerous dilated small bowel loops without air-fluid levels (fluid not present)
numerous dilated small bowel loops without air-fluid levels (fluid not present) bubbly / frothy appearance of intestinal contents
bubbly / frothy appearance of intestinal contents soap-bubble / applesauce appearance in RLQ (in 50 66%) due to admixture of gas with meconium
soap-bubble / applesauce appearance in RLQ (in 50 66%) due to admixture of gas with meconium multiple round/oval filling defects in distal ileum + colon
multiple round/oval filling defects in distal ileum + colon functional microcolon (unused colon in antenatal obstruction)
functional microcolon (unused colon in antenatal obstruction)
OB-US:
 unusual echogenic intraluminal areas in small bowel (DDx: normal transient inspissated meconium)
unusual echogenic intraluminal areas in small bowel (DDx: normal transient inspissated meconium) usually polyhydramnios
usually polyhydramnios fluid-filled dilated small bowel
fluid-filled dilated small bowel
| Cx (in 40 50%): | volvulus, ischemia, necrosis, stenosis, atresia, perforation, meconium peritonitis, pseudocyst |
| Rx: | (1) Nonionic contrast media enema (because of risk of bowel perforation) (2) 17% Hypaque/Conray enema mixed with acetylcysteine (MucomystR) (3) GastrografinR enema with Tween 80 (attention to fluid + electrolyte balance) |
| DDx: | Hirschsprung disease, small bowel atresia with meconium ileus, meconium plug syndrome, small left colon syndrome, imperforate anus, obstruction from duplication cyst |
Meconium Peritonitis
= sterile chemical peritonitis secondary to perforation of bowel proximal to high-grade/complete obstruction that seals in utero due to inflammatory response
| Incidence: | 1:35,000 livebirths |
| Age: | antenatal perforation after 3rd month of gestation |
Cause:
Atresia (secondary to ischemic event) (50%)
of small bowel (usually ileum or jejunum)
of colon (uncommon)
Bowel obstruction (46%)
meconium ileus
volvulus, internal hernia
intussusception, congenital bands, Meckel diverticulum
microcolon
Hydrometrocolpos
 Meconium peritonitis due to cystic fibrosis diagnosed in utero in 8% + at birth in 15 40%!
Meconium peritonitis due to cystic fibrosis diagnosed in utero in 8% + at birth in 15 40%! Intraperitoneal meconium may calcify within 24 hours!
Intraperitoneal meconium may calcify within 24 hours!
Types:
fibroadhesive type (most common):
= intense chemical reaction of peritoneum, which seals off the perforation
no evidence for active leak at birth
 dense mass with calcium deposits
dense mass with calcium deposits calcific plaques scattered throughout peritoneal cavity
calcific plaques scattered throughout peritoneal cavity
cystic type:
= cystic cavity formed by fixation of bowel loops surrounding the perforation site, which continues to leak meconium
 cyst outlined by calcific rim
cyst outlined by calcific rim
generalized type:
perforation occurs immediately antenatally
active leakage of bowel contents
 complicated ascites
complicated ascites
 intraabdominal calcifications (conspicuously absent in cystic fibrosis):
intraabdominal calcifications (conspicuously absent in cystic fibrosis): peripherally calcified pseudocysts
peripherally calcified pseudocysts small flecks of calcifications scattered throughout abdomen
small flecks of calcifications scattered throughout abdomen larger aggregates of calcifications along inferior surface of liver/flank/processus vaginalis/scrotum
larger aggregates of calcifications along inferior surface of liver/flank/processus vaginalis/scrotum
 obstructive roentgen signs following birth
obstructive roentgen signs following birth separation of bowel loops by fluid
separation of bowel loops by fluid microcolon = unused colon
microcolon = unused colon  meconium hydrocele producing labial mass
meconium hydrocele producing labial mass
US:
 highly echogenic linear/clumped foci with posterior acoustic shadowing in scrotum
highly echogenic linear/clumped foci with posterior acoustic shadowing in scrotum snowstorm appearance = highly echogenic material throughout abdomen in between bowel loops
snowstorm appearance = highly echogenic material throughout abdomen in between bowel loops ill-/well-defined homo-/heterogeneous encysted collections of meconium
ill-/well-defined homo-/heterogeneous encysted collections of meconium
OB-US (>18 weeks EGA):
 polyhydramnios (64 71%)
polyhydramnios (64 71%) fetal ascites (54 57%)
fetal ascites (54 57%) bowel dilatation (27 29%)
bowel dilatation (27 29%) intraabdominal bright echogenic mass
intraabdominal bright echogenic mass multiple linear/clumped foci of scattered calcifications (85%); may develop within 12 hours to 8 days after perforation
multiple linear/clumped foci of scattered calcifications (85%); may develop within 12 hours to 8 days after perforation meconium pseudocyst = well-defined hypoechoic mass surrounded by an echogenic calcified wall (= contained perforation)
meconium pseudocyst = well-defined hypoechoic mass surrounded by an echogenic calcified wall (= contained perforation)
| DDx: | (1) Intraabdominal teratoma (2) Fetal gallstones (3) Isolated liver calcifications |
| Mortality: | up to 62% |
| Prognosis: | generally good; surgery may not be required when perforation site is completely healed |
Meconium Plug Syndrome
= local inspissation of meconium leading to low colonic obstruction; probably related to small left colon syndrome as part of same spectrum of functional immaturity
| Age: | newborn infant (symptomatic within first 24 hours of life) |
| Cause: | cystic fibrosis (25%), Hirschsprung disease, prematurity, maternal magnesium sulfate treatment |
abdominal distension
vomiting
failure to pass meconium
 distended transverse + ascending colon + dilated small bowel (proximal to obstruction)
distended transverse + ascending colon + dilated small bowel (proximal to obstruction) small left colon with change in caliber at splenic flexure
small left colon with change in caliber at splenic flexure occasionally bubbly appearance in colon (DDx: submucosal air in necrotizing enterocolitis)
occasionally bubbly appearance in colon (DDx: submucosal air in necrotizing enterocolitis) presacral pseudotumor (no gas in rectum)
presacral pseudotumor (no gas in rectum)
BE:
 double-contrast effect = barium between meconium plug + colonic wall
double-contrast effect = barium between meconium plug + colonic wall
| Rx: | water-soluble enema |
| DDx: | Hirschsprung disease |
P.857
Melanosis Coli
= benign brown-black discoloration of colonic mucosa
| Incidence: | 10% of autopsies |
| Cause: | chronic anthracene cathartic usage |
asymptomatic
| Prognosis: | no malignant potential |
M n trier Disease
= GIANT HYPERTROPHIC GASTRITIS = HYPERPLASTIC GASTROPATHY
= characterized by excessive mucus production and
| TRIAD of | (1) Giant mucosal hypertrophy (2) Hypoproteinemia (3) Hypochlorhydria |
| Path: | mucosal thickness up to 6 mm (normal range: 0.6 1.0 mm) |
| Histo: | hyperplasia of glandular tissue + microcyst formation |
| Age: | 20 70 years; M:F = 2:1 |
| Associated with: | benign gastric ulcer (13 72%) |
epigastric pain, vomiting, weight loss
gastrointestinal bleeding
protein-losing enteropathy with hypoproteinemia + peripheral edema
absent/decreased acid secretion (>50%)
| Location: | throughout fundus + body, particularly prominent along greater curvature, antrum usually spared (DDx to lymphoma: usually in antrum) |
 markedly enlarged + tortuous gastric rugae in spite of adequate gastric distension:
markedly enlarged + tortuous gastric rugae in spite of adequate gastric distension: relatively abrupt demarcation between normal antrum + abnormal fundus + body
relatively abrupt demarcation between normal antrum + abnormal fundus + body
 marked hypersecretion (mucus)
marked hypersecretion (mucus) preserved pliability of stomach
preserved pliability of stomach
CT:
 wall thickening of proximal stomach
wall thickening of proximal stomach nodular symmetric folds
nodular symmetric folds
| Cx: | development of gastric cancer reported |
| DDx: | lymphoma, polypoid variety of gastric carcinoma, acute gastritis, chronic gastritis, gastric varices |
Mesenteric Lymphadenitis
= clinical entity whose symptoms relate to benign inflammation of lymph nodes in the bowel mesentery
| Cause: | Yersinia enterocolitica, Y. pseudotuberculosis, viral infection |
| Age: | children, young adults |
nausea, vomiting, diarrhea, fever
diffuse/RLQ pain + tenderness
| Location: | usually RLQ (immediately anterior to right psoas muscle in 78%, small bowel mesentery in 56%) |
 enlarged mesenteric lymph nodes
enlarged mesenteric lymph nodes isolated ileal wall thickening (33%)
isolated ileal wall thickening (33%) colonic wall thickening (18%)
colonic wall thickening (18%)
| N.B.: | visualization of entire normal appendix is necessary to differentiate from acute appendicitis! |
| DDx: | appendicitis (enlarged nodes immediately anterior to right psoas muscle in 40 82%, nodes less numerous + smaller), Crohn disease |
Mesenteric Ischemia
= BOWEL ISCHEMIA
Etiology:
arterial occlusion: atheromatous disease, thromboembolic disease, dissecting aortic aneurysm, fibromuscular hyperplasia, arteritis, endotoxin shock, hypoperfusion (shock, hypovolemia), disseminated intravascular coagulation, direct trauma, aortic surgery, stent placement, therapeutic embolization, radiation, antiphospholipid antibody syndrome
occlusive mesenteric infarction (90% mortality)
Embolus (40 50%) just distal to middle colic a.
SMA thrombosis (20 40%) at origin + site of atherosclerotic narrowing (ostium stenosis)
nonocclusive mesenteric ischemia (10% mortality)
Preexisting atherosclerosis with systemic low-flow state, cardiac failure/arrhythmia, intraoperative hypotension
Bowel vasoconstriction = vasospasm (reflex hypotension, digitalis, ergot preparation, vasopressin, amphetamine, cocaine), pheochromocytoma, familial dysautonomia
Shock bowel = diffuse small bowel ischemia in hypovolemia and hemorrhagic/cardiogenic/septic shock (due to increased bowel permeability to macromolecules + albumin)
 diffuse bowel wall thickening
diffuse bowel wall thickening persistent increased enhancement on CT (due to slowed perfusion and washout + interstitial leakage of contrast material)
persistent increased enhancement on CT (due to slowed perfusion and washout + interstitial leakage of contrast material) accumulation of intraluminal fluid (due to failed resorption capacity)
accumulation of intraluminal fluid (due to failed resorption capacity)
venous occlusion (<10%): young patient, often following abdominal surgery
Location: superior mesenteric vein > inferior mesenteric vein > portal vein bowel obstruction: strangulation by adhesions or bands mesenteric vein thrombosis, incarceration of hernia, volvulus, intussusception, pronounced overdistension (prestenotic, distension colitis), ischemic colitis due to endoscopy/enemas/colonic carcinoma (1 7%)
vasculitis: polyarteritis nodosa (50 70%)
 relatively long segment of bowel involved
relatively long segment of bowel involved multiple skip areas in nonsegmental distribution
multiple skip areas in nonsegmental distribution involvement of duodenum is indicative
involvement of duodenum is indicative
abdominal inflammation: pancreatitis, appendicitis, diverticulitis, diffuse peritonitis, parasitic infestation
cytotoxic drugs: long-term immunosuppressive drugs for rejection, chemotherapy for leukemia/lymphoma
radiation: >4,500 cGy
| Prevalence: | 5% for SMA; 4% for celiac artery; 11% for inferior mesenteric artery |
Pathophysiology:
ischemia leads to
inflammatory response (cytokines, platelet-activating factor, tumor necrosis factor released from activated neutrophils, platelets, mast cells, endothelial cells)
breakdown of mucosal barrier from
mild superficial necrosis limited to mucosa (mucosal ulcer) = partial mural bowel ischemia, to
life-threatening continuous necrosis of all bowel wall layers = transmural bowel infarction
P.858
invasion of bacteria with bacteremia + sepsis
strictures
Acute Mesenteric Ischemia
Cause:
acute occlusive SMA embolus (in >50%): usually lodges at bifurcation of middle colic artery + SMA
SMA thrombosis (4 18%; nonocclusive in 25%): frequently involves the proximal SMA
SMA dissection (due to cystic medial necrosis, fibromuscular dysplasia)
venous occlusion in 5 10 15% (due to hypercoagulability, trauma, portal hypertension, infection, carcinoma, oral contraceptives)
first crampy, then continuous abdominal pain with acute event
cardiac disease predisposing to embolization
gut emptying (vomiting/diarrhea)
WBC >12,000/ l with left shift (80%)
gross rectal bleeding
| Location: | (a) any segment of small bowel (b) distal transverse colon, splenic flexure, cecum (most common) |
Consequences:
dependent on magnitude of insult, duration of process, adequacy of collaterals
reversible ischemia
Complete restitution of bowel wall secondary to abundant collaterals
Healing with fibrosis + stricture formation
irreversible ischemia
Transmural infarction with bowel perforation
Plain film:
 gasless abdomen (= fluid-filled loops from exudation) in 21%
gasless abdomen (= fluid-filled loops from exudation) in 21% bowel distension to splenic flexure (= perfusion territory of SMA) in 43%
bowel distension to splenic flexure (= perfusion territory of SMA) in 43% thumbprinting (36%) = thickening of bowel wall + valvulae (edema)
thumbprinting (36%) = thickening of bowel wall + valvulae (edema) small bowel pseudoobstruction (most frequently in thrombosis)
small bowel pseudoobstruction (most frequently in thrombosis) pneumatosis = dissection of luminal gas into bowel wall (28%)
pneumatosis = dissection of luminal gas into bowel wall (28%) mesenteric + portal vein gas (14%)
mesenteric + portal vein gas (14%) ascites (14%)
ascites (14%)
Barium:
 scalloping/thumbprinting = thickening of wall + valvulae
scalloping/thumbprinting = thickening of wall + valvulae picket fencing
picket fencing  separation + uncoiling of loops
separation + uncoiling of loops narrowed lumen
narrowed lumen circumferential ulcer
circumferential ulcer
CT (26 73 82% sensitive):
 circumferential bowel wall thickening (28 52 96%) >3 5 mm depending on degree of distention:
circumferential bowel wall thickening (28 52 96%) >3 5 mm depending on degree of distention: target sign = alternating layers of high and low attenuation (from submucosal edema hemorrhage superinfection) in
target sign = alternating layers of high and low attenuation (from submucosal edema hemorrhage superinfection) inischemic colitis (94%)
reversible mesenteric ischemia (80%)
mesenteric infarction (26 38%)
 spastic contractions of colon in mild mucosal ischemia
spastic contractions of colon in mild mucosal ischemia Least specific sign
Least specific sign No correlation with the severity of ischemic damage
No correlation with the severity of ischemic damage
 thinning of bowel wall (in acute arterio-occlusive transmural infarction) if it becomes gangrenous
thinning of bowel wall (in acute arterio-occlusive transmural infarction) if it becomes gangrenous focal/diffuse bowel dilatation (10 56 91%) with gas (43%)/fluid (29%) due to interruption of peristaltic activity (destruction of intramural nerves + intestinal musculature)/irreversible transmural ischemic damage
focal/diffuse bowel dilatation (10 56 91%) with gas (43%)/fluid (29%) due to interruption of peristaltic activity (destruction of intramural nerves + intestinal musculature)/irreversible transmural ischemic damage bowel wall attenuation:
bowel wall attenuation: decreased, usually homogeneously (due to edema)
decreased, usually homogeneously (due to edema) increased (due to hemorrhage)
increased (due to hemorrhage)
 variable enhancement pattern:
variable enhancement pattern: diminished enhancement of bowel wall (due to compromised blood flow)
diminished enhancement of bowel wall (due to compromised blood flow) absent enhancement of bowel wall (in 18%, 62% sensitive, 96% specific)
absent enhancement of bowel wall (in 18%, 62% sensitive, 96% specific) engorgement of mesenteric vessels = venous congestion secondary to stasis
engorgement of mesenteric vessels = venous congestion secondary to stasis increased wall enhancement (due to hyperemia in outflow obstruction from mesenteric venous occlusion/during reperfusion after arteriogenic bowel ischemia/in shock bowel) is a good prognostic indicator (33% sensitive, 71% specific)
increased wall enhancement (due to hyperemia in outflow obstruction from mesenteric venous occlusion/during reperfusion after arteriogenic bowel ischemia/in shock bowel) is a good prognostic indicator (33% sensitive, 71% specific) delayed + persistent enhancement (due to delayed venous return and arteriospasm)
delayed + persistent enhancement (due to delayed venous return and arteriospasm)
 increased attenuation of mesenteric fat from mesenteric edema (in 68%, 58% sensitive, 79% specific)
increased attenuation of mesenteric fat from mesenteric edema (in 68%, 58% sensitive, 79% specific) mesenteric fluid (88% sensitive, 90% specific)
mesenteric fluid (88% sensitive, 90% specific) ascites (in 43 88%, 75% sensitive, 76% specific)
ascites (in 43 88%, 75% sensitive, 76% specific) pneumatosis intestinalis (in 6 28%, 3 14% specific) = dissection of luminal gas into bowel wall across compromised mucosa signaling irreversible disease:
pneumatosis intestinalis (in 6 28%, 3 14% specific) = dissection of luminal gas into bowel wall across compromised mucosa signaling irreversible disease: small isolated gas bubbles within wall
small isolated gas bubbles within wall broad rims of air dissecting the entire bowel wall into two layers
broad rims of air dissecting the entire bowel wall into two layers
 portal venous gas (5 13 36%)/mesenteric vein gas (28%) = propagation of intramural gas into mesenteric venous system
portal venous gas (5 13 36%)/mesenteric vein gas (28%) = propagation of intramural gas into mesenteric venous system pneumoperitoneum (7%) = perforation of infarcted bowel segment
pneumoperitoneum (7%) = perforation of infarcted bowel segment
arterial occlusion:
 hyperattenuating SMA on NECT
hyperattenuating SMA on NECT filling defect with ring enhancement on CECT
filling defect with ring enhancement on CECT thumbprinting (26%) = thickening of bowel wall
thumbprinting (26%) = thickening of bowel wall lack of bowel wall enhancement with arterial occlusion
lack of bowel wall enhancement with arterial occlusion concurrent embolic infarction of kidney/spleen
concurrent embolic infarction of kidney/spleen
venous thrombosis (15%):
 enlarged diameter + increased attenuation of SMV on NECT
enlarged diameter + increased attenuation of SMV on NECT filling defect in SMV/portal vein thrombosis on CECT
filling defect in SMV/portal vein thrombosis on CECT thickened intestinal wall (64%) due to edema
thickened intestinal wall (64%) due to edema waterlogging with marked contrast enhancement of mesentery + bowel wall
waterlogging with marked contrast enhancement of mesentery + bowel wall
P.859
| Cx: | bowel necrosis (with occlusion of small vasa recta disallowing collateral flow) |
Common pitfalls:
Spastic colon misinterpreted a s simple contraction, issue resolved by repeat CT with enema)
Widely distended colonic segment with a wall thickness of 3 5 mm misinterpreted as normal
Small bowel dilatation + air-fluid levels misinterpreted as ileus/pseudoobstruction
Angio (AP and LAT views):
 occlusion/vasoconstriction/vascular beading
occlusion/vasoconstriction/vascular beading embolus lodged at major branching points distal to first 3 cm of SMA
embolus lodged at major branching points distal to first 3 cm of SMA
Rx for nonocclusive mesenteric ischemia:
via SMA catheter 60 mg papaverin slowly injected followed by papaverin infusion of 1 mg/min
NUC:
IV/IA Tc-99m sulfur colloid/labeled leukocytes, Gacitrate, Tc-99m pyrophosphate:
 tracer accumulation 5 hours after onset of ischemia (more intense uptake with transmural infarcts)
tracer accumulation 5 hours after onset of ischemia (more intense uptake with transmural infarcts)
intraperitoneal injection of Xe-133 in saline is absorbed by intestine:
 decreased washout with abnormal perfusion of strangulated bowel
decreased washout with abnormal perfusion of strangulated bowel
Prognosis:
Massive infarction of small + large bowel if mesenteric embolization occurs proximal to middle colic artery (= limited collateral flow)
Focal segments of intestinal ischemia if mesenteric embolization occurs distal to middle colic artery (= good collateral flow)
| Local Cx: | bleeding, intestinal perforation, abscess formation, peritonitis |
| Systemic Cx: | hemoconcentration, acidosis, DIC, bone marrow suppression, multiple organ failure (including heart + kidneys) |
| Mortality: | 70 80 92% for intestinal infarction |
| DDx: | typhlitis, Crohn disease, infectious/ulcerative colitis, proctosigmoiditis, sigmoid diverticulitis, other causes of pneumatosis intestinalis/portal venous gas |
Chronic Mesenteric Ischemia
= ABDOMINAL ANGINA
= intermittent mesenteric ischemia in severe arterial stenosis with inadequate collateralization provoked by food ingestion
postprandial abdominal pain 15 20 minutes after food intake (due to gastric steal diverting blood flow away from intestine)
fear of eating large meals
weight loss, malabsorption
reflex emptying of bowel after eating
Barium:
Subacute:
 flattening of one border
flattening of one border pseudosacculation/pseudodiverticula on antimesenteric border
pseudosacculation/pseudodiverticula on antimesenteric border
Chronic:
 7 10-cm-long smooth pliable strictures
7 10-cm-long smooth pliable strictures dilatation of gut between strictures
dilatation of gut between strictures thinned + atrophic valvulae
thinned + atrophic valvulae
Cx: obstruction
Duplex US:
 celiac trunk occlusion + retrograde perfusion of hepatic artery through SMA
celiac trunk occlusion + retrograde perfusion of hepatic artery through SMA PSV >300 cm/sec and EDV >45 cm/sec in SMA
PSV >300 cm/sec and EDV >45 cm/sec in SMA peak systolic velocity >160 cm/sec in celiac trunk for >50% stenosis (57% sensitivity, 100% specificity) during fasting state
peak systolic velocity >160 cm/sec in celiac trunk for >50% stenosis (57% sensitivity, 100% specificity) during fasting state
Mesenteric Venous Thrombosis
Cause:
Infection: sepsis, diverticulitis, appendicitis, Crohn disease, peritonitis, abdominal abscess
Hypercoagulable state: antithrombin III/protein C or S deficiency, oral contraceptives
Trauma
Mechanical: volvulus, bowel obstruction, postoperative state
| Location: | SMV > IMV (6%) |
subacute symptomatology over 1 4 weeks
severe abdominal pain with rebound/guarding
nausea, vomiting, diarrhea
hematemesis, hematochezia (after bowel necrosis)
 ileus
ileus ascites
ascites bowel wall thickening with thumbprinting (bowel wall thickening usually more pronounced compared to arterio-occlusive disease)
bowel wall thickening with thumbprinting (bowel wall thickening usually more pronounced compared to arterio-occlusive disease) dilated vein with echogenic thrombus
dilated vein with echogenic thrombus
Mesothelial Cyst
= MESENTERIC/OMENTAL CYST
| Etiology: | failure of mesothelial peritoneal surfaces to coalesce |
| Path: | unilocular thin-walled cyst usually with serous, occasionally chylous/hemorrhagic fluid contents |
| Histo: | lined by mesothelial cells + surrounded by thin layer of fibrous tissue |
| Location: | small bowel, mesentery (78%), mesocolon |
asymptomatic
 single cyst up to several cm in size
single cyst up to several cm in size omental cysts may be pedunculated
omental cysts may be pedunculated
CT:
 near-water density/soft-tissue density
near-water density/soft-tissue density fluid levels related to fat + water components
fluid levels related to fat + water components
| Cx: | torsion, hemorrhage, intestinal obstruction |
| DDx: | lymphangioma (septations) |
Metastases to Colon
Spread:
Hematogenous
 submucosal masses/bull's-eye lesions
submucosal masses/bull's-eye lesions diffusely infiltrating lesions mimicking inflammatory bowel disease
diffusely infiltrating lesions mimicking inflammatory bowel disease
Direct invasion by contiguous tumor
ovary inferior border of sigmoid left kidney splenic flexure pancreatic tail splenic flexure pelvis (uterus, bladder) anterior border of rectum prostate rectosigmoid Direct invasion along mesenteric reflections
stomach transverse colon superior margin pancreas transverse colon inferior margin omental cake transverse colon superior margin Intraperitoneal seeding
Origin: ovarian, gastric, colonic, pancreatic cancers (most commonly) Classic sites of seeding:
pouch of Douglas (50%):
anterior border of rectosigmoid
lower small bowel mesentery (40%):
medial border of cecum
sigmoid mesocolon (20%):
superior border of sigmoid colon
right paracolic gutter (10%):
lateral border of ascending colon
P.860
Metastases to Small Bowel
| Origin: | colon > stomach > breast > ovary > uterine cervix > melanoma > lung > pancreas |
Spread:
Intraperitoneal seeding: primary mucinous tumor of ovary, appendix, colon; breast cancer
Hematogenous dissemination with submucosal deposits: malignant melanoma, breast carcinoma, lung carcinoma, Kaposi sarcoma
Direct extension from adjacent neoplasm:
ovary, uterus, prostate, pancreas, colon, kidney
 fixation + tenting + transverse stretching (= across long axis) of folds secondary to mesenteric + peritoneal infiltration (most common form)
fixation + tenting + transverse stretching (= across long axis) of folds secondary to mesenteric + peritoneal infiltration (most common form)
UGI:
 single mass protruding into lumen resembling annular carcinoma
single mass protruding into lumen resembling annular carcinoma bull's-eye lesions = multiple polypoid masses with sizable ulcer craters
bull's-eye lesions = multiple polypoid masses with sizable ulcer craters obstruction from kinking/annular constriction/large intraluminal mass
obstruction from kinking/annular constriction/large intraluminal mass compression by direct extension of primary tumor/involved nodes
compression by direct extension of primary tumor/involved nodes
CT:
 soft-tissue density nodules/masses
soft-tissue density nodules/masses sheets of tissue causing thickening of bowel wall + mesenteric leaves
sheets of tissue causing thickening of bowel wall + mesenteric leaves fixation + angulation of bowel loops (in tumors with desmoplastic response)
fixation + angulation of bowel loops (in tumors with desmoplastic response) ascites
ascites
Metastases to Stomach
| Organ of origin: | malignant melanoma, breast, lung, colon, prostate, leukemia, secondary lymphoma |
GI bleeding + anemia (40%)
epigastric pain
 solitary mass (50%)
solitary mass (50%) multiple nodules (30%)
multiple nodules (30%) linitis plastica (20%): especially breast
linitis plastica (20%): especially breast multiple umbilicated nodules: melanoma
multiple umbilicated nodules: melanoma
Midgut Volvulus
= torsion of entire gut around SMA due to a short mesenteric attachment of small intestine in malrotation
| Age: | neonate/young infant (= acute intestinal obstruction); occasionally older child/adult (= chronic intestinal obstruction) In 20% associated with: (1) Duodenal atresia (2) Duodenal diaphragm (3) Duodenal stenosis (4) Annular pancreas |
Pathophysiology:
degree of twisting can change due to natural movement of bowel + determines symptomatology; severe volvulus (= twist of 3 and a half turns) causes bowel necrosis
acute symptoms within first 3 weeks of life in 75% (MEDICAL EMERGENCY): bilious vomiting (postprandial, intermittent, projectile) is HALLMARK; abdominal distension; shock
intermittent obstructive symptoms in older child: recurring attacks of nausea, vomiting, and abdominal pain
failure to thrive (hypoproteinemic gastroenteropathy as a result of lymphatic + venous obstruction)
currant jelly stools/melena (implying vascular compromise)
Plain film:
 dilated air-filled duodenal bulb + paucity of gas distally
dilated air-filled duodenal bulb + paucity of gas distally double bubble sign = air-fluid levels in stomach + duodenum
double bubble sign = air-fluid levels in stomach + duodenum isolated collection of gas-containing bowel loops distal to obstructed duodenum = gas-filled volvulus = closed-loop obstruction (from nonresorption of intestinal gas secondary to obstruction of mesenteric veins)
isolated collection of gas-containing bowel loops distal to obstructed duodenum = gas-filled volvulus = closed-loop obstruction (from nonresorption of intestinal gas secondary to obstruction of mesenteric veins)
UGI:
| N.B.: | exclude perforation on plain films! |
 dilated proximal duodenum terminating in a distinctive conical shape
dilated proximal duodenum terminating in a distinctive conical shape duodenal-fold thickening + thumbprinting (mucosal edema + hemorrhage)
duodenal-fold thickening + thumbprinting (mucosal edema + hemorrhage) duodenojejunal junction (ligament of Treitz) located lower than duodenal bulb + to the right of expected position
duodenojejunal junction (ligament of Treitz) located lower than duodenal bulb + to the right of expected position spiral course of midgut loops beyond point of obstruction = apple-peel/twisted ribbon/corkscrew appearance (in 81%)
spiral course of midgut loops beyond point of obstruction = apple-peel/twisted ribbon/corkscrew appearance (in 81%) abnormally high position of cecum (on barium enema)
abnormally high position of cecum (on barium enema)
CT:
 whirl-like pattern of small bowel loops + adjacent mesenteric fat converging to the point of torsion (during volvulus)
whirl-like pattern of small bowel loops + adjacent mesenteric fat converging to the point of torsion (during volvulus) transposition of SMA/SMV = SMV to the left of SMA (NO volvulus)
transposition of SMA/SMV = SMV to the left of SMA (NO volvulus) chylous mesenteric cyst (from interference with lymphatic drainage)
chylous mesenteric cyst (from interference with lymphatic drainage)
US:
 clockwise whirlpool sign = color Doppler depiction of superior mesenteric vein wrapping clockwise around superior mesenteric artery
clockwise whirlpool sign = color Doppler depiction of superior mesenteric vein wrapping clockwise around superior mesenteric artery distended proximal duodenum with arrowhead-type compression over spine
distended proximal duodenum with arrowhead-type compression over spine superior mesenteric vein to the left of SMA
superior mesenteric vein to the left of SMA thick-walled bowel loops below duodenum + to the right of spine associated with free intraperitoneal fluid
thick-walled bowel loops below duodenum + to the right of spine associated with free intraperitoneal fluid
P.861
Angio:
 barber pole sign = spiraling of SMA
barber pole sign = spiraling of SMA tapering/abrupt termination of mesenteric vessels
tapering/abrupt termination of mesenteric vessels marked vasoconstriction + prolonged contrast transit time
marked vasoconstriction + prolonged contrast transit time absent venous opacification/dilated tortuous superior mesenteric vein
absent venous opacification/dilated tortuous superior mesenteric vein
| Cx: | intestinal ischemia + necrosis in distribution of SMA with occlusion of lymphatics, SMV + SMA (bloody diarrhea, ileus, abdominal distension) |
| DDx: | pyloric stenosis (same age group, no bilious vomiting) |
Mucocele of Appendix
Mucocele
= distension of appendix with sterile mucus
Etiology:
(perhaps) cystic dilatation of lumen secondary to obstruction by fecolith, foreign body, carcinoid, endometriosis, adhesions, volvulus
mucosal hyperplasia (25%)
mucinous cystadenoma due to hyperplasia with epithelial atypia (63%)
mucinous cystadenocarcinoma with stromal invasion (12%)
accumulation of thick mucus in cystic fibrosis
| Incidence: | 0.07 0.3% of appendectomy specimens |
| Mean age: | 55 years; M:F = 1:4 |
| Associated with: | colonic adenocarcinoma (6-fold risk), mucin-secreting tumor of ovary |
asymptomatic (25%)
palpable mass (in up to 50%)
acute/chronic right lower quadrant pain
 globular, smooth-walled, broad-based mass invaginating into cecum
globular, smooth-walled, broad-based mass invaginating into cecum nonfilling of the appendix on BE
nonfilling of the appendix on BE peripheral punctate/rimlike calcifications frequent
peripheral punctate/rimlike calcifications frequent
CT:
 round sharply defined paracecal mass with homogeneous content of near-water/soft-tissue attenuation (depending on amount of mucin)
round sharply defined paracecal mass with homogeneous content of near-water/soft-tissue attenuation (depending on amount of mucin)
US:
 purely cystic/cystic with fine internal echoes/complex cystic mass with high-level echoes
purely cystic/cystic with fine internal echoes/complex cystic mass with high-level echoes gravity-dependent echoes = layering of protein macroaggregates/inspissated mucoid material
gravity-dependent echoes = layering of protein macroaggregates/inspissated mucoid material acoustic shadowing if calcifications present
acoustic shadowing if calcifications present
NUC:
 intense early gallium uptake (affinity to acid mucopolysaccharides of mucus)
intense early gallium uptake (affinity to acid mucopolysaccharides of mucus)
| Cx: | (1) Rupture with pseudomyxoma peritonei (2) Torsion with gangrene + hemorrhage (3) Herniation into cecum with bowel obstruction (4) Intussusception |
Myxoglobulosis
= rare variant of mucocele of the appendix characterized by clusters of pearly white mucous balls intermixed with mucus
usually asymptomatic
may appear as acute appendicitis
 multiple 1 10-mm small rounded annular, nonlaminated calcified spherules (PATHOGNOMONIC)
multiple 1 10-mm small rounded annular, nonlaminated calcified spherules (PATHOGNOMONIC)
| DDx: | inverted appendiceal stump, acute appendicitis, carcinoma of the cecum |
Necrotizing Enterocolitis
= NEC = ischemic bowel disease secondary to hypoxia, perinatal stress, infection (endotoxin), congenital heart disease
| Incidence: | most common GI emergency in premature infants |
| Age: | develops 2 3 days after birth; in 90% within first 10 days of life |
| Path: | acute inflammation + mucosal ulceration + widespread transmural necrosis |
| Organism: | not yet isolated; often occurs in miniepidemics within nursery |
| Predisposed: | premature infant (50 80%), Hirschsprung disease, bowel obstruction (small bowel atresia, pyloric stenosis, meconium ileus, meconium plug syndrome) |
abdominal distension, bilious emesis
blood-streaked stools (in 50%); explosive diarrhea
mild respiratory distress
generalized sepsis
| Location: | usually in terminal ileum (most commonly involved), cecum, right colon; rarely in stomach, upper bowel |
 distension of small bowel and colon (loops wider than vertebral body L1) air-fluid levels, commonly in RLQ (1st sign)
distension of small bowel and colon (loops wider than vertebral body L1) air-fluid levels, commonly in RLQ (1st sign) disarrayed bowel gas pattern (no longer normal array of polygons)
disarrayed bowel gas pattern (no longer normal array of polygons) tubular loops of bowel
tubular loops of bowel bowel wall thickening + thumbprinting
bowel wall thickening + thumbprinting  fixed bowel = persistent abnormal loop of bowel without change on supine vs. prone films/for >24 hours
fixed bowel = persistent abnormal loop of bowel without change on supine vs. prone films/for >24 hours pneumatosis intestinalis (80%):
pneumatosis intestinalis (80%):in curvilinear shape (= subserosal) or
bubbly/cystic (= submucosal gas collection from gas-forming organisms/dissection of intraluminal gas)
 bubbly appearance of bowel due to gas in wall/intraluminal gas/fecal matter (intraluminal contents are composed of blood, sloughed colonic mucosa, intraluminal gas, some fecal material)
bubbly appearance of bowel due to gas in wall/intraluminal gas/fecal matter (intraluminal contents are composed of blood, sloughed colonic mucosa, intraluminal gas, some fecal material) gas in portal venous system (frequently transient, does not imply hopeless outcome)
gas in portal venous system (frequently transient, does not imply hopeless outcome) ascites
ascites pneumoperitoneum (immediate surgery required)
pneumoperitoneum (immediate surgery required)
| N.B.: | barium enema is contraindicated! May be used judiciously in selected cases with radiologic + clinical doubt! |
| Cx: | (1) Inflammatory stricture after healing in 10 30%, in 30% multiple, in 80% in left colon (BE follow-up in survivors) (2) Bowel perforation in 12 32% |
Pelvic Lipomatosis + Fibrolipomatosis
= nonmalignant overgrowth of adipose tissue with minimal fibrotic + inflammatory components compressing soft-tissue structures within pelvis
| Incidence: | 0.6 1.7:100,000 |
| Cause: | unknown; UTIs, obesity, endocrine dysfunction |
| Age: | 9 80 years (peak 25 60 years); M:F = 10:1; NO racial predominance for Blacks ( ); obesity NOT contributing factor |
P.862
often incidental finding
urinary frequency, dysuria, nocturia, hematuria
flank pain, suprapubic tenderness
recurrent urinary tract infections
low back pain, fever
constipation, tenesmus, rectal bleeding, ribbonlike stools with mucus
edema of lower extremities
 elongation + narrowing of rectum
elongation + narrowing of rectum elevation of rectosigmoid + sigmoid colon out of pelvis
elevation of rectosigmoid + sigmoid colon out of pelvis increase in sacrorectal space >10 mm
increase in sacrorectal space >10 mm stretching of sigmoid colon
stretching of sigmoid colon elongation + elevation of urinary bladder with symmetric inverted pear shape
elongation + elevation of urinary bladder with symmetric inverted pear shape elongation of posterior urethra
elongation of posterior urethra pelvic lucency; CT confirmatory
pelvic lucency; CT confirmatory medial/lateral displacement of ureters
medial/lateral displacement of ureters
Cx of fibrolipomatosis:
Ureteral obstruction (40% within 5 years)
IVC obstruction
| Rx: | urinary diversion to prevent end stage renal disease |
Peritoneal Mesothelioma
= only primary tumor of peritoneum arising from mesothelial cells lining peritoneal cavity
| Age: | 55 66 years; M > F |
| Associated with: | asbestos exposure |
| Spread: | intraperitoneal along serosal surfaces; direct invasion of liver, pancreas, bladder, bowel |
| Location: | pleura (67%), peritoneum (30 40%), pericardium (2.5%), processus vaginalis (0.5%) |
 thickening of mesentery, omentum, peritoneum, bowel wall
thickening of mesentery, omentum, peritoneum, bowel wall nodular masses in anterior parietal peritoneum becoming confluent and cakelike
nodular masses in anterior parietal peritoneum becoming confluent and cakelike disproportionately small amount of ascites
disproportionately small amount of ascites areas of calcification (rare)
areas of calcification (rare)
CT:
 nodular irregular thickening of peritoneal surfaces
nodular irregular thickening of peritoneal surfaces localized masses
localized masses infiltrating sheets of tissue
infiltrating sheets of tissue foci of calcifications
foci of calcifications ascites of near-water density
ascites of near-water density stellate configuration of neurovascular bundles
stellate configuration of neurovascular bundles pleated thickening of mesenteric leaves
pleated thickening of mesenteric leaves
NUC:
 diffuse uptake of gallium-67
diffuse uptake of gallium-67
| Prognosis: | extremely poor due to advanced disease at presentation (most patients die within 1 year) |
Cystic Mesothelioma
= rare benign neoplasm without metastatic potential but tendency for local recurrence (in 27 50%)
| Path: | multiple thin-walled cysts lined by mesothelial cells + filled with watery fluid; intermediate form between benign adenomatoid tumor + malignant peritoneal mesothelioma |
 Not associated with asbestos exposure!
Not associated with asbestos exposure!
| Median age: | 37 years; M F |
| Location: | any peritoneal/omental surface, most frequently in pelvis |
contains watery fluid
 uni-/multilocular cystic tumor (cysts of 1 mm to 6 cm) without calcifications
uni-/multilocular cystic tumor (cysts of 1 mm to 6 cm) without calcifications
| DDx: | lymphangioma, ovarian carcinoma |
Peritoneal Metastases
= PERITONEAL CARCINOMATOSIS
= intraabdominal spread of malignant tumors
| Origin: | (a) common: ovary, stomach, colon (b) less common: pancreas, uterus, bladder |
 massive ascites
massive ascites desmoplastic reaction at (a) anterior border of rectum (Blumer shelf), (b) mesenteric side of terminal ileum
desmoplastic reaction at (a) anterior border of rectum (Blumer shelf), (b) mesenteric side of terminal ileum
CT:
 increased density of linear network in mesenteric fat
increased density of linear network in mesenteric fat loculated fluid collections in peritoneal cavity
loculated fluid collections in peritoneal cavity apparent thickening of mesenteric vessels (= fluid within leaves of mesentery)
apparent thickening of mesenteric vessels (= fluid within leaves of mesentery) adnexal mass of cystic/soft-tissue density (= Krukenberg tumor)
adnexal mass of cystic/soft-tissue density (= Krukenberg tumor) small nodular densities on peritoneal surface
small nodular densities on peritoneal surface omental cake = thickening of greater omentum
omental cake = thickening of greater omentum lobulated mass in pouch of Douglas
lobulated mass in pouch of Douglas calcified peritoneal implants in serous cystadenocarcinoma of ovary (in up to 40% with stage III/IV disease)
calcified peritoneal implants in serous cystadenocarcinoma of ovary (in up to 40% with stage III/IV disease)
Peutz-Jeghers Syndrome
[Johannes Peutz (1886 1957), internist in Den Haag, Holland]
[Harold Jeghers (1904 1990), internist in Boston, USA]
= rare autosomal dominant disease with incomplete penetrance characterized by intestinal polyposis + mucocutaneous pigmentation (= hamartomatosis); often spontaneous mutation
| Incidence: | 1:7,000 live births; in 50% familial, in 50% sporadic; most frequent of polyposis syndromes to involve small intestines |
| Age: | 25 years at presentation (range 10 30 years); M:F = 1:1 |
| Path: | multiple small sessile/large pedunculated polyps |
| Histo: | benign hamartomatous polyp with smooth muscle core arising from muscularis mucosae + extending treelike into lamina propria of polyp; misplaced epithelium in submucosa, muscularis propria, sub-serosa frequently surrounding mucin-filled spaces |
mucocutaneous pigmentation (similar to freckles):
= 1 5-mm small elongated melanin spots on mucous membranes (lower lips, gums, palate) + facial skin (nose, cheeks, around eyes) + volar aspects of toes and fingers (100%), becoming noticeable in first few years of life
cramping abdominal pain (small bowel intussusception in 47%)
rectal bleeding, melena (30%)
prolapse of polyp through anus
chronic hypochromic microcytic anemia
| Location: | small bowel (jejunum + ileum > duodenum) > colon > stomach; mouth + esophagus spared |
@ Small bowel (>95%)
 multiple usually broad-based polyps separated by wide areas of intervening flat mucosa
multiple usually broad-based polyps separated by wide areas of intervening flat mucosa multilobulated surface of larger polyps
multilobulated surface of larger polyps myriad of 1 2-mm nodules of up to several cm = carpet of polyps
myriad of 1 2-mm nodules of up to several cm = carpet of polyps intussusception usually confined to small bowel
intussusception usually confined to small bowel
P.863
@ Colon + rectum (30%)
 multiple scattered 1 30-mm polyps; NO carpeting
multiple scattered 1 30-mm polyps; NO carpeting
@ Stomach + duodenum (25%)
 diffuse involvement with multiple polyps
diffuse involvement with multiple polyps
@ Respiratory + urinary tract
 adenoma of bronchus + bladder
adenoma of bronchus + bladder
Cx:
Transient intussusception (pedunculated polyp)
Carcinoma of GI tract (2 3%)
Carcinoma of pancreas (13%)
Carcinoma of breast (commonly bilateral + ductal)
Ovarian tumor (5%), commonly bilateral: sex cord-stromal tumor of ovary (almost in 100% of patients), mucinous cystic tumor, cystadenoma, granulosa cell tumor
Endometrial cancer: adenoma malignum of cervix
(= minimal deviation adenocarcinoma = low-grade mucinous tumor of cervix)
Testicular tumor: feminizing Sertoli cell tumor
| Rx: | (1) Endoscopic removal of all polyps >5 mm (2) Surgery is reserved for obstruction, severe bleeding, malignancy |
| Prognosis: | decreased life expectancy (risk of cancer approaching 40% by 40 years of age) |
| DDx: | familial adenomatous polyposis, juvenile polyposis (similar age), Cowden syndrome, Cronkhite-Canada syndrome |
Postcricoid Defect
= variable defect seen commonly in the fully distended cervical esophagus; no pathologic value
| Etiology: | redundancy of mucosa over rich postcricoid submucosal venous plexus |
| Incidence: | in 80% of normal adults |
| Location: | anterior aspect of esophagus at level of cricoid cartilage |
 tumor-/weblike lesion with variable configuration during swallowing
tumor-/weblike lesion with variable configuration during swallowing
| DDx: | submucosal tumor, esophageal web (persistent configuration) |
Postinflammatory Polyposis
= PSEUDOPOLYPOSIS
= reepithelialized inflammatory polyps as sequelae of mucosal ulceration
| Etiology: | ulcerative colitis (10 20%); granulomatous colitis (less frequent); schistosomiasis (endemic); amebic colitis (occasionally); toxic megacolon |
| Pathogenesis: | ulcerative undermining of strips of mucosa with reepitheliazation of denuded surfaces of tags + bowel wall |
| Location: | most common in left hemicolon, may occur in stomach/small intestine |
 sessile + frondlike appearance (often)
sessile + frondlike appearance (often) filiform polyposis = multiple wormlike projections only attached at their bases (CHARACTERISTIC)
filiform polyposis = multiple wormlike projections only attached at their bases (CHARACTERISTIC)
| Prognosis: | NO malignant potential |
| DDx: | familial polyposis (polyps terminate in bulbous heads) |
Presbyesophagus
= defect in primary peristalsis + LES relaxation associated with aging
| Incidence: | 15% in 7th decade; 50% in 8th decade; 85% in 9th decade |
| Associated with: | hiatus hernia, reflux |
usually asymptomatic
 impaired/no primary peristalsis
impaired/no primary peristalsis often repetitive nonperistaltic tertiary contractions in distal esophagus
often repetitive nonperistaltic tertiary contractions in distal esophagus mild/moderate esophageal dilatation
mild/moderate esophageal dilatation poor LES relaxation
poor LES relaxation
| DDx: | diabetes, diffuse esophageal spasm, scleroderma, esophagitis, achalasia, benign stricture, carcinoma |
Progressive Systemic Sclerosis
= PSS = multisystem connective tissue disorder (collagen-vascular disease) of unknown etiology characterized by widespread disorder of the microvasculature and overproduction of collagen causing exuberant interstitial fibrosis with atrophy + sclerosis of many organ systems
= SCLERODERMA = variety of skin disorders associated with hardening of skin;
by extent of cutaneous involvement divided into:
DIFFUSE SCLERODERMA
tends to involve older women;
interstitial pulmonary fibrosis more severe;
organ failure more likely
SYSTEMIC SCLEROSIS WITH LIMITED SCLERODERMA (formerly CREST syndrome)
CREST features more common; pulmonary arterial hypertension more common + more severe)
May be associated with:
other connective tissue diseases (especially SLE and polymyositis/dermatomyositis)
| Cause: | autoimmune condition with genetic predisposition, may be initiated by environmental antigen (eg, toxic oil syndrome in Spain through ingestion of adulterated rape seed oil/ingestion of L-tryptophan) |
| Peak age: | 30 50 years; M:F = 1:3 |
| Histo: | vasculitis + submucosal fibrosis extending into muscularis, smooth muscle atrophy (initially hypertrophy and finally atrophy of collagen fibers) |
| CREST: | Calcinosis of skin Raynaud phenomenon Esophageal dysmotility Sclerodactyly Telangiectasia |
antinuclear antibodies (30 80%):
centromere antibody (ACA) specific for limited disease
anti topoisomerase-1 (= antiScl-70) identifies patients with diffuse cutaneous disease
antibodies to extracellular matrix proteins and type I + IV collagen
rheumatoid factor (35%)
LE cells (5%)
weakness, generalized debility
| Prognosis: | 50 67% 5-year survival rate |
P.864
Gastrointestinal Scleroderma (in 40 45%)
 Third most common manifestation of scleroderma (after skin changes + Raynaud phenomenon)
Third most common manifestation of scleroderma (after skin changes + Raynaud phenomenon) May precede other manifestations!
May precede other manifestations!abdominal pain, diarrhea
multiple episodes of pseudoobstruction
 hepatomegaly
hepatomegaly@ Esophagus (in 42 95%)
 First GI tract location to be involved!
First GI tract location to be involved!dysphagia (50%), heartburn (30%)
 normal peristalsis above aortic arch (striated muscle in proximal 1/3 of esophagus)
normal peristalsis above aortic arch (striated muscle in proximal 1/3 of esophagus) hypotonia/atony + hypokinesia/aperistalsis in lower 2/3 of esophagus (>50%)
hypotonia/atony + hypokinesia/aperistalsis in lower 2/3 of esophagus (>50%) deficient emptying in recumbent position
deficient emptying in recumbent position thin/vanished longitudinal folds
thin/vanished longitudinal folds mild to moderate dilatation of esophagus
mild to moderate dilatation of esophagus chalasia (= patulous lower esophageal sphincter)
chalasia (= patulous lower esophageal sphincter) gastroesophageal reflux (70%)
gastroesophageal reflux (70%) erosions + superficial ulcers (from asymptomatic reflux esophagitis: NO protective esophageal contraction)
erosions + superficial ulcers (from asymptomatic reflux esophagitis: NO protective esophageal contraction) fusiform stricture usually 4 5 cm above gastroesophageal junction (from reflux esophagitis)
fusiform stricture usually 4 5 cm above gastroesophageal junction (from reflux esophagitis) esophageal shortening + sliding hiatal hernia
esophageal shortening + sliding hiatal hernia
Cx: peptic stricture, aspiration, Barrett esophagus, adenocarcinoma @ Stomach (less frequent involvement)
 gastric dilatation
gastric dilatation decreased motor activity + delayed emptying
decreased motor activity + delayed emptying
@ Small bowel (in up to 45%)
 PSS is rapidly progressing once small intestine is involved!
PSS is rapidly progressing once small intestine is involved!malabsorption (delayed intestinal transit time + bacterial overgrowth)
 marked dilatation of small bowel (in particular duodenum = megaduodenum, jejunum) simulating small bowel obstruction
marked dilatation of small bowel (in particular duodenum = megaduodenum, jejunum) simulating small bowel obstructionCAVE: misdiagnosis of obstruction may lead to exploratory surgery!  abrupt cutoff at SMA level (atrophy of neural cells with hypoperistalsis)
abrupt cutoff at SMA level (atrophy of neural cells with hypoperistalsis) prolonged transit time with barium retention in duodenum up to 24 hours
prolonged transit time with barium retention in duodenum up to 24 hours hidebound/accordion pattern (60%) = sharply defined folds of normal thickness with decreased intervalvular distance (tightly packed folds) within dilated segment (due to predominant involvement of circular muscle)
hidebound/accordion pattern (60%) = sharply defined folds of normal thickness with decreased intervalvular distance (tightly packed folds) within dilated segment (due to predominant involvement of circular muscle) pseudodiverticula (10 40%) = asymmetric sacculations with squared tops + broad bases on mesenteric side (due to eccentric smooth muscle atrophy)
pseudodiverticula (10 40%) = asymmetric sacculations with squared tops + broad bases on mesenteric side (due to eccentric smooth muscle atrophy) pneumatosis cystoides intestinalis + pneumoperitoneum (occasionally)
pneumatosis cystoides intestinalis + pneumoperitoneum (occasionally) excess fluid with bacterial overgrowth (= pseudo blind loop syndrome )
excess fluid with bacterial overgrowth (= pseudo blind loop syndrome ) normal mucosal fold pattern
normal mucosal fold pattern
Cx: intussusception without anatomic lead point @ Colon (up to 40 50%)
constipation (common), may alternate with diarrhea
 pseudosacculations + wide-mouthed diverticula on antimesenteric side (formed by repetitive bulging through atrophic areas) in transverse + descending colon
pseudosacculations + wide-mouthed diverticula on antimesenteric side (formed by repetitive bulging through atrophic areas) in transverse + descending colon eventually complete loss of haustrations (simulating cathartic colon)
eventually complete loss of haustrations (simulating cathartic colon) marked dilatation (may simulate Hirschsprung disease)
marked dilatation (may simulate Hirschsprung disease) stercoral ulceration (from retained fecal material)
stercoral ulceration (from retained fecal material)
| Cx: | life-threatening barium impaction |
| DDx: | (1) Dermatomyositis (similar radiographic findings) (2) Sprue (increased secretions, segmentation, fragmentation, dilatation most significant in midjejunum, normal motility) (3) Obstruction (no esophageal changes, no pseudodiverticula) (4) Idiopathic intestinal pseudoobstruction (usually in young people) |
Pulmonary Scleroderma (in 10 66%)
| Path: | almost 100% involvement in autopsy series |
| Histo: | thickening of basement membrane of alveoli + small arteries and veins; pattern of usual interstitial pneumonia/nonspecific interstitial pneumonitis |
slightly productive, mostly dry cough
exertional progressive dyspnea
hematemesis
pulmonary function abnormalities in the absence of frank roentgenographic changes (typical dissociation of clinical, functional, and radiologic evidence)
pericarditis
| Location: | peripherally, most prominent at both lung bases (where blood flow greatest) |
 bibasilar pulmonary fibrosis:
bibasilar pulmonary fibrosis:Prevalence: 20 65% on CXR, up to 90% on HRCT  fine/coarse reticulations/diffuse interstitial infiltrates
fine/coarse reticulations/diffuse interstitial infiltrates subpleural fibrocystic spaces (honeycombing)
subpleural fibrocystic spaces (honeycombing)
 low lung volumes from progressive volume loss
low lung volumes from progressive volume loss alveolar changes (secondary to aspiration of refluxed gastric contents with disturbed esophageal motility/mineral oil taken to combat constipation)
alveolar changes (secondary to aspiration of refluxed gastric contents with disturbed esophageal motility/mineral oil taken to combat constipation) dilated esophagus with air esophagogram (DDx: achalasia, mediastinitis) with increased frequency of aspiration pneumonia
dilated esophagus with air esophagogram (DDx: achalasia, mediastinitis) with increased frequency of aspiration pneumonia pleural reaction/effusion distinctly uncommon
pleural reaction/effusion distinctly uncommon
HRCT:
 areas of ground-glass attenuation
areas of ground-glass attenuation poorly defined subpleural nodules
poorly defined subpleural nodules reticular pattern of attenuation
reticular pattern of attenuation traction bronchiectasis
traction bronchiectasis honeycombing
honeycombing
| Cx: | (1) Pulmonary arterial hypertension (6 60%) (2) Aspiration pneumonia (3) Increased incidence of lung cancer |
@ Heart: sclerosis of cardiac muscle cor pulmonale
Renal Scleroderma (25%)
| Onset: | common within 3 years |
| Histo: | fibrinoid necrosis of afferent arterioles (also seen in malignant hypertension) |
 renal cortical necrosis
renal cortical necrosis spotty inhomogeneous nephrogram (constriction + occlusion of arteries)
spotty inhomogeneous nephrogram (constriction + occlusion of arteries) concomitant arterial ectasia
concomitant arterial ectasia
P.865
| Cx: | renal failure (from nephrosclerosis) |
Musculoskeletal Scleroderma
edema of distal portion of extremities
thickened inelastic waxy skin most prominent about face + extremities
symmetrical polyarthralgias (50 80%)
Raynaud phenomenon (may precede other symptoms by months/years)
atrophy + thickening of skin and musculature (78%)
@ Fingers
sausage digit = edema of digits associated with loss of transverse skin folds + lack of definition of subcutaneous fat
 tapered fingers = sclerodactyly = atrophy + resorption of soft tissues of fingertips + soft-tissue calcifications
tapered fingers = sclerodactyly = atrophy + resorption of soft tissues of fingertips + soft-tissue calcifications acroosteolysis = penciling / autoamputation
acroosteolysis = penciling / autoamputation = resorption of distal phalanges of hand (63%) beginning at volar aspect of terminal tufts with proximal progression
 calcinosis (25%) = punctate soft-tissue calcifications of fingertips, axilla, ischial tuberosity, forearm, elbow (over pressure area), lower leg, face
calcinosis (25%) = punctate soft-tissue calcifications of fingertips, axilla, ischial tuberosity, forearm, elbow (over pressure area), lower leg, face calcifications around tendons. bursae, within joints
calcifications around tendons. bursae, within joints
@ Arthritis
stiffness in small joints, occasionally in knee, shoulder, wrist
lack of motility, eventually contractures
 arthritis of interphalangeal joints of hands (25%)
arthritis of interphalangeal joints of hands (25%)Location: 1st CMC, MCP, DIP, PIP  central/marginal erosions (50%):
central/marginal erosions (50%): resorption of palmar aspect of terminal phalanges (most frequent sign)
resorption of palmar aspect of terminal phalanges (most frequent sign) bony erosions of carpal bones (trapezium), distal radius + ulna, mandible, ribs, lateral aspect of clavicle, humerus, acromion, mandible, cervical spine
bony erosions of carpal bones (trapezium), distal radius + ulna, mandible, ribs, lateral aspect of clavicle, humerus, acromion, mandible, cervical spine
 joint-space narrowing (late)
joint-space narrowing (late)DDx: rheumatoid, psoriatic, erosive arthritis  soft-tissue swelling periarticular osteoporosis
soft-tissue swelling periarticular osteoporosis NO significant osteoporosis
NO significant osteoporosis flexion contractures of fingers (from tendon sheath inflammation + fibrosis)
flexion contractures of fingers (from tendon sheath inflammation + fibrosis)
@ Ribs
 erosion of superior aspect of ribs
erosion of superior aspect of ribs
@ Teeth
 widening of periodontal membrane
widening of periodontal membrane
Prolapsed Antral Mucosa
= prolapse of hypertrophic + inflammatory mucosa of gastric antrum into duodenum resulting in pyloric obstruction
 mushroom-/umbrella-/cauliflower-shaped filling defect at duodenal base
mushroom-/umbrella-/cauliflower-shaped filling defect at duodenal base filling defect varies in size + shape
filling defect varies in size + shape redundant gastric rugae can be traced from pyloric antrum through pyloric channel
redundant gastric rugae can be traced from pyloric antrum through pyloric channel gastric hyperperistalsis
gastric hyperperistalsis
Pseudomembranous Colitis
= CLOSTRIDIUM DIFFICILE DISEASE
= nosocomial epidemic/endemic acute infectious colitis due to Clostridium difficile toxins
| Cause: | unopposed proliferation of gram-positive Clostridium difficile in response to a decrease in normal intestinal flora |
| Etiologic agent: | toxin A (enterotoxin) + toxin B (cytotoxin) produced by C. difficile |
Predisposed:
complication of antibiotic therapy with tetracycline, penicillin, ampicillin, clindamycin, lincomycin, amoxicillin, chloramphenicol, cephalosporins
complication of some chemotherapeutic agents: methotrexate, fluorouracil
following abdominal surgery/renal transplantation/irradiation
prolonged hypotension/hypoperfusion of bowel
shock, uremia
proximal to colonic obstruction
debilitating diseases: lymphosarcoma, leukemia, advanced HIV infection
immunosuppressive therapy with actinomycin D
| Histo: | pseudomembranes (exudate composed of leukocytes, fibrin, mucin, sloughed necrotic epithelium held in columns by strands of mucus) on a partially denuded colonic edematous mucosa (mucosa generally intact); reactive edema in lamina propria, submucosa, and eventually subserosa |
Clinical manifestations of C. difficile infection:
absence of symptoms (majority)
antibiotic-associated colitis without pseudomembrane formation
pseudomembranous colitis
fulminant colitis
profuse watery diarrhea, abdominal cramps, tenderness
fever, fecal blood, leukocytosis
less common: chronic diarrhea, dehydration, toxic megacolon, hyperpyrexia, leukemoid reaction, hypoalbuminemia with anasarca
| Location: | rectum (95%); confined to right + transverse colon (5 27 40%) |
 Radiographic abnormalities in 32% with a positive stool toxin assay!
Radiographic abnormalities in 32% with a positive stool toxin assay!
Plain film:
 adynamic ileus pattern = moderate gaseous distension of small bowel + colon:
adynamic ileus pattern = moderate gaseous distension of small bowel + colon: small bowel ileus (20%)
small bowel ileus (20%) colonic ileus (32%)
colonic ileus (32%)
 nodular haustral thickening (18%):
nodular haustral thickening (18%): thumbprinting = transverse banding = marked thickening + distortion of haustral folds most prominent in transverse colon
thumbprinting = transverse banding = marked thickening + distortion of haustral folds most prominent in transverse colon diffusely shaggy + irregular surface (confluent pseudomembranes)
diffusely shaggy + irregular surface (confluent pseudomembranes)
 ascites (7%)
ascites (7%)
BE (CONTRAINDICATED in severe cases):
 pseudoulcerations = barium filling clefts between pseudomembranes
pseudoulcerations = barium filling clefts between pseudomembranes irregular ragged polypoid contour of colonic wall
irregular ragged polypoid contour of colonic wall discrete multiple plaquelike lesions of 2 4 mm in size (DDx: polyposis, nodular form of lymphoma)
discrete multiple plaquelike lesions of 2 4 mm in size (DDx: polyposis, nodular form of lymphoma)
P.866
| N.B.: | risk of colonic perforation in toxic megacolon! |
CT (85% sensitive, 48% specific):
 NO colonic abnormality (12 39%)
NO colonic abnormality (12 39%) colonic wall thickening of 3 32 (mean of 14.7) mm in 61 88%:
colonic wall thickening of 3 32 (mean of 14.7) mm in 61 88%: circumferential/eccentric
circumferential/eccentric smooth (44%)/irregular/polypoid (17%)
smooth (44%)/irregular/polypoid (17%) target sign = submucosal edema + mucosal hyperemia (best seen during arterial enhancement)
target sign = submucosal edema + mucosal hyperemia (best seen during arterial enhancement)
DDx: wall thickening is greater than in any other colitis except Crohn disease!  accordion sign (51 70%) = orally administered intraluminal contrast material trapped between distorted thickened closely spaced transverse edematous folds of low attenuation (simulating intramural tracts), TYPICAL but only in severe cases
accordion sign (51 70%) = orally administered intraluminal contrast material trapped between distorted thickened closely spaced transverse edematous folds of low attenuation (simulating intramural tracts), TYPICAL but only in severe cases colonic dilatation frequent due to transmural inflammation
colonic dilatation frequent due to transmural inflammation homogeneous enhancement due to hyperemia
homogeneous enhancement due to hyperemia usually disproportionately mild pericolonic stranding (42%) relative to marked wall thickening
usually disproportionately mild pericolonic stranding (42%) relative to marked wall thickening ascites in severe cases (15 35%)
ascites in severe cases (15 35%) pneumatosis coli portal vein gas in severe cases
pneumatosis coli portal vein gas in severe cases
| Dx: | (1) Stool assay for Clostridium difficile cytotoxin (detects toxin B): cumbersome to perform (2) Enzyme immunoassay test (up to 33% false-negative results): detects toxin A + B (3) Stool culture (95% sensitive): not available for 2 days (4) Pseudomembranes of adherent yellow plaques 2 10 mm in diameter on proctosigmoidoscopy |
| Cx: | peritonitis, toxic megacolon, perforation |
| Prognosis: | 1.1 3.5% overall mortality; most patients recover within 2 weeks |
| Rx: | (1) Discontinuation of suspected antibiotic (2) Administration of vancomycin/metronidazole (response within 3 4 days) (3) Attention to fluid and electrolyte balance (4) Life-saving partial colectomy required in <1% |
| DDx: | acute stage of ulcerative/granulomatous colitis, inflammatory colitis, ischemic colitis, colonic wall hemorrhage, colonic lymphangiectasia, leukemic infiltration, diverticulitis |
Pseudomyxoma Peritonei
= jelly belly = gelatinous ascites
= slow insidious accumulation of large amounts of intraperitoneal gelatinous material
| Etiology: | spillage of mucin from ruptured mucocele with foreign body peritonitis; spread of cystadeno-carcinoma of appendix (male)/ovary (female) |
| Rarely associated with: | malignancy of colon (<5%), stomach, uterus, pancreas, common bile duct, urachal duct, omphalomesenteric duct |
slowly progressive massive abdominal distension
recurrent abdominal pain
 thickening of peritoneal + omental surfaces
thickening of peritoneal + omental surfaces omental cake
omental cake posterior fixation of bowel loops + mesentery
posterior fixation of bowel loops + mesentery voluminous septated/loculated pseudoascites
voluminous septated/loculated pseudoascites several thin-walled cystic masses of different size throughout abdominal cavity
several thin-walled cystic masses of different size throughout abdominal cavity scalloped contour of liver + splenic margins
scalloped contour of liver + splenic margins annular/semicircular calcifications (rare but highly suggestive)
annular/semicircular calcifications (rare but highly suggestive)
CT:
 intraperitoneal collection of very low attenuation (common)/soft-tissue density (rare)
intraperitoneal collection of very low attenuation (common)/soft-tissue density (rare) may contain enhancing septa calcifications
may contain enhancing septa calcifications discrete hypoattenuating masses (infrequent)
discrete hypoattenuating masses (infrequent)
US:
 hypoechoic collection (common)/more solid appearance (rare)
hypoechoic collection (common)/more solid appearance (rare)
| Prognosis: | bowel obstruction with need for multiple surgical debulkings |
| DDx: | peritoneal metastases, pancreatitis with pseudocysts, pyogenic peritonitis, widespread echinococcal disease, ascites |
| Prognosis: | 50% 5-year survival rate |
| Rx: | often requires repeated laparotomies for drainage |
Radiation Injury
= obliterative endarteritis with irradiation in excess of 4,000 4,500 rads
| Incidence: | 5%; increased risk after pelvic surgery |
 radiographic changes within field of radiation only
radiographic changes within field of radiation only
Radiation Gastritis
 Permanent radiographic findings of radiation injury appear 1 month to 2 years after therapy
Permanent radiographic findings of radiation injury appear 1 month to 2 years after therapy gastric ulceration + deformity (pylorus)
gastric ulceration + deformity (pylorus) enlargement + effacement of gastric folds
enlargement + effacement of gastric folds antral narrowing + rigidity (similar to linitis plastica)
antral narrowing + rigidity (similar to linitis plastica)
Radiation Enteritis
 Permanent radiographic findings of radiation injury appear >1 2 years following irradiation
Permanent radiographic findings of radiation injury appear >1 2 years following irradiation
| Predisposed: | women (cancer of cervix, endometrium, ovary), patients with bladder cancer |
crampy abdominal pain (from intermittent obstruction)
persistent diarrhea
occult intestinal hemorrhage
| Location: | ileum; concomitant radiation damage to colon/rectum |
 irregular nodular thickening of folds with straight transverse course ulcerations
irregular nodular thickening of folds with straight transverse course ulcerations serrated bowel margin
serrated bowel margin thickened bowel wall with luminal narrowing
thickened bowel wall with luminal narrowing multiple strictures + partial mechanical obstruction
multiple strictures + partial mechanical obstruction separation of adjacent bowel loops by >2 mm
separation of adjacent bowel loops by >2 mm shortening of small bowel
shortening of small bowel fixation + immobilization of bowel loops with similar radiographic appearance between examinations (from dense desmoplastic response to irradiation)
fixation + immobilization of bowel loops with similar radiographic appearance between examinations (from dense desmoplastic response to irradiation)
CT:
 increased attenuation of mesentery
increased attenuation of mesentery
| DDx: | Crohn disease, lymphoma, ischemia, hemorrhage |
P.867
Radiation Injury of Rectum
 Manifestation of radiation colitis can occur up to 15 years following irradiation
Manifestation of radiation colitis can occur up to 15 years following irradiation
| Predisposed: | 90% in women (carcinoma of cervix) |
tenesmus, diarrhea, bleeding, constipation
 ridgelike appearance of mucosa (submucosal fibrosis)
ridgelike appearance of mucosa (submucosal fibrosis) irregularly outlined ulcerations (rare)
irregularly outlined ulcerations (rare)
CT:
 narrowed partially distensible rectum
narrowed partially distensible rectum thick homogeneous rectal wall
thick homogeneous rectal wall target sign = submucosal circumferential lucency
target sign = submucosal circumferential lucency proliferation of perirectal fat >10 mm
proliferation of perirectal fat >10 mm thickening of perirectal fascia
thickening of perirectal fascia halo sign = increase in pararectal fibrosis
halo sign = increase in pararectal fibrosis
| Cx: | (1) Obstruction (2) Colovaginal/coloenteric fistula formation |
Retained Gastric Antrum
| Cause: | retention of endocrinologically active gastric antrum in continuity with pylorus + duodenum |
| Pathophysiology: | bathing of antrum in alkaline duodenal juice stimulates secretion of gastrin |
| Associated with: | gastric ulcers in 30 50% |
 duodenogastric reflux of barium through pylorus (diagnostic)
duodenogastric reflux of barium through pylorus (diagnostic) giant marginal ulcer/several marginal ulcers usually on jejunal side of anastomosis (large false-negative + false-positive rates; correct-positive rate of 28 60%)
giant marginal ulcer/several marginal ulcers usually on jejunal side of anastomosis (large false-negative + false-positive rates; correct-positive rate of 28 60%) large amount of secretions
large amount of secretions edematous mucosa of jejunal anastomotic segment
edematous mucosa of jejunal anastomotic segment lacy/cobweblike small bowel pattern (hypersecretion)
lacy/cobweblike small bowel pattern (hypersecretion)
| Cx: | gastrojejunocolic fistula |
Retractile Mesenteritis
= CHRONIC FIBROSING MESENTERITIS = CHRONIC SUBPERITONEAL SCLEROSIS = MESENTERIC PANNICULITIS = LIPOSCLEROTIC MESENTERITIS
= LIPOGRANULOMA OF THE MESENTERY = MESENTERIC
LIPODYSTROPHY = ISOLATED LIPODYSTROPHY
= RETROPERITONEAL XANTHOGRANULOMA
= MESENTERIC WEBER-CHRISTIAN DISEASE
= rare benign disorder of unknown etiology characterized by fibrofatty thickening of small bowel mesentery
| Etiology: | trauma, previous surgery, ischemia |
| Age: | most common in 6th decade; M:F = 2 3:1 |
Associated with:
Gardner syndrome, familial polyposis
Fibrosing mediastinitis, retroperitoneal fibrosis
Lymphoma, lymphosarcoma (in 15%)
Carcinoid tumor
Metastatic gastric/colonic carcinoma
Whipple lipodystrophy
Weber-Christian disease
| Location: | root of mesentery extending toward mesenteric border of bowel |
| Site: | small bowel mesentery; occasionally mesocolon, sigmoid mesentery, omentum, retroperitoneum |
Plain film:
 soft-tissue mass with calcifications
soft-tissue mass with calcifications thumbprinting (from vascular congestion)
thumbprinting (from vascular congestion)
UGI:
 compression/distortion of duodenum near ligament of Treitz
compression/distortion of duodenum near ligament of Treitz separation of small bowel loops with fixation, kinking, and angulation
separation of small bowel loops with fixation, kinking, and angulation
CT:
 mass of fat density interspersed with soft-tissue density (fibrous tissue) + calcifications
mass of fat density interspersed with soft-tissue density (fibrous tissue) + calcifications mesenteric thickening with fine stellate pattern extending to bowel border
mesenteric thickening with fine stellate pattern extending to bowel border retraction of small bowel loops
retraction of small bowel loops single mesenteric soft-tissue mass (fibroma)
single mesenteric soft-tissue mass (fibroma) multiple nodules throughout mesentery (fibromatosis)
multiple nodules throughout mesentery (fibromatosis)
| Dx: | supported by absence of pancreatitis/inflammatory bowel disease |
| Prognosis: | usually benign course with spontaneous resolution |
| Rx: | steroids |
| DDx: | pseudomyxoma peritonei (from metastatic gastric/colonic adenocarcinoma); carcinoid/desmoid tumor; mesenteric lymphoma, lymphosarcoma; liposarcoma of mesentery; pyogenic peritonitis |
Mesenteric Lipodystrophy (1st stage)
= degeneration of mesenteric fat
| Path: | diffuse mesenteric thickening (42%); solitary (32%)/multiple (26%) discrete mesenteric masses |
| Histo: | sheets of foamy macrophages with scattered lymphocytic infiltration replacing mesenteric fat |
asymptomatic
 chylous ascites
chylous ascites
| Prognosis: | spontaneous recovery |
Mesenteric Panniculitis (2nd stage)
= inflammatory changes in mesenteric adipose tissue
| Path: | diffuse mesenteric thickening with puckering of mesenteric surface due to desmoplastic reaction; adherent mass(es) in root of mesentery; fat necrosis |
| Histo: | infiltrate of plasma cells, foreign body giant cells, foamy macrophages |
crampy abdominal pain; bowel disturbances
nausea + vomiting; malaise; mild weight loss
poorly defined mass (50%)/abdominal fullness
low-grade fever
Retractile Mesenteritis (3rd stage)
= fibrosis of adipose tissue
| Histo: | collagen deposition, fibrosis, inflammation; calcifications |
 intestinal obstruction
intestinal obstruction
Schatzki Ring
= LOWER ESOPHAGEAL MUCOSAL RING
= constant lower esophageal ring (mucosal thickening) presumed to result from reflux esophagitis = thin annular peptic stricture
| Incidence: | 6 14% of population; old age > young age; M > F |
| Histo: | usually squamous epithelium on upper surface + columnar epithelium on undersurface; may be covered totally by squamous epithelium or columnar epithelium |
P.868
asymptomatic (if ring >20 mm)
dysphagia (if ring <12 mm)
| Location: | near the squamocolumnar junction; in region of B ring at inferior margin of lower esophageal sphincter |
 permanently present nondistensible transverse ring with constant shape + size (range of 3 18 mm)
permanently present nondistensible transverse ring with constant shape + size (range of 3 18 mm) 2 4-mm-thick shelflike projection into lumen with smooth symmetric margins
2 4-mm-thick shelflike projection into lumen with smooth symmetric margins visible only with adequate distension of esophagogastric region and when located above the esophageal hiatus of the diaphragm
visible only with adequate distension of esophagogastric region and when located above the esophageal hiatus of the diaphragm best demonstrated in prone position during arrested deep inspiration with Valsalva maneuver while solid barium column passes through esophagogastric region
best demonstrated in prone position during arrested deep inspiration with Valsalva maneuver while solid barium column passes through esophagogastric region short esophagus + intrahiatal/intrathoracic gastric segment
short esophagus + intrahiatal/intrathoracic gastric segment= sliding hiatal hernia if Schatzki ring located 1 2 cm above diaphragmatic hiatus
| Prognosis: | decrease in caliber over 5 years (in 25 33%) |
| Cx: | impaction of food bolus (associated with severe chest pain) |
| Rx: | (1) Proper mastication of food (2) Endoscopic rupture (3) Esophageal dilatation (radiographically often lack of caliber change after successful dilatation) |
| DDx: | annular peptic stricture (usually thicker, asymmetric, irregular surface, associated with thickened esophageal folds, serration of esophageal margins) |
Schwannoma
= rare neurogenic tumor
| Incidence: | 4% of all benign gastric tumors are neurogenic tumors |
| Location: | stomach |
 discrete submucosal mass
discrete submucosal mass
| Cx: | (1) Ulceration (pressure necrosis of overlying mucosa) (2) Central necrosis (after outgrowing its blood supply) |
Small Bowel Volvulus
= rare life-threatening surgical emergency
| Cause: | adhesive bands, internal hernia, external hernia |
Pathophysiology:
closed-loop obstruction bacterial overgrowth accelerated fluid sequestration + gas production increased intraluminal pressure + dilatation compromise of vascular supply to intestinal wall hemorrhagic infarction necrosis perforation
 poor/absent enhancement of bowel wall
poor/absent enhancement of bowel wall spoke wheel sign = radial peripheral distribution of distended fluid-filled small-bowel loops around central engorged thickened mesenteric vessels (75%)
spoke wheel sign = radial peripheral distribution of distended fluid-filled small-bowel loops around central engorged thickened mesenteric vessels (75%) two collapsed adjacent bowel loops = site of constriction (35%)
two collapsed adjacent bowel loops = site of constriction (35%) U-shaped configuration of distended fluid-filled small-bowel loops = radial arrangement of incarcerated fluid-filled dilated loop at periphery of tightly twisted mesentery (30%)
U-shaped configuration of distended fluid-filled small-bowel loops = radial arrangement of incarcerated fluid-filled dilated loop at periphery of tightly twisted mesentery (30%) triangular sign = fusiform tapering of collapsed loop at site of constriction on longitudinal section through loop (15%)
triangular sign = fusiform tapering of collapsed loop at site of constriction on longitudinal section through loop (15%) whirl sign = swirling appearance of twisted mesentery (10%)
whirl sign = swirling appearance of twisted mesentery (10%)
| Cx: | (1) bowel ischemia in 46% due to closed-loop obstruction + torsion of mesenteric vessels (2) bowel necrosis |
| Mortality: | 9% |
Small Left Colon Syndrome
| Cause: | transient functional colonic obstruction due to immaturity of mesenteric plexus |
| Age: | newborn infant |
| Associated with: | maternal diabetes mellitus (most common), maternal substance abuse; NOT related to cystic fibrosis |
 colonic caliber becomes abruptly diminutive distal to splenic flexure
colonic caliber becomes abruptly diminutive distal to splenic flexure bowel dilatation proximal to splenic flexure
bowel dilatation proximal to splenic flexure meconium plug (as a result and not the cause of obstruction)
meconium plug (as a result and not the cause of obstruction)
| Prognosis: | gradual resolution of functional immaturity over days to weeks |
Solitary Rectal Ulcer Syndrome
= MUCOSAL PROLAPSE SYNDROME
Related disorders with common pathogenesis:
hamartomatous inverted polyp, colitis cystica profunda
| Cause: | prolapse of anterior rectal wall resulting in mucosal ischemia due to traumatization of rectal mucosa by anal sphincter during defecation (rectal straining/prolapse) |
| Age: | young patients (especially women) |
| Path: | small/large, single/multiple shallow ulcers; 25% broad-based, 18% patchy granular/velvety hyperemic mucosa; rectal stenosis through confluent circumferential lesion |
| Histo: | obliteration of lamina propria mucosae by fibromuscular proliferation of muscularis mucosae, streaming of fibroblasts + muscle fibers between crypts, misplaced mucosal glands deep to muscularis mucosae; diffuse increase in mucosal collagen |
chronic rectal bleeding
passage of mucus
disordered defecation
tenesmus
BE:
 ulcer (ulcerative type) on anterior rectal wall
ulcer (ulcerative type) on anterior rectal wall polypoid lesion/nodules (polypoid type)
polypoid lesion/nodules (polypoid type) flat granular mucosa (flat type)
flat granular mucosa (flat type) thickened valves of Houston without ulcer
thickened valves of Houston without ulcer stricture
stricture
Evacuation proctography:
 failure of anorectal angle to open while straining
failure of anorectal angle to open while straining excessive perineal descent
excessive perineal descent
Prognosis:
Little change over time
Considerable change in appearance of lesion
Transfusions necessitated by massive blood loss
| Dx: | rectal biopsy |
| DDx: | invasive rectal carcinoma, Crohn disease |
Sprue
= classic disease of malabsorption
P.869
| Path: | villous atrophy (truncation) + elongation of crypts of Lieberk hn (crypt hyperplasia) + round cell infiltration of lamina propria and epithelium (plasma cells, mast cells, lymphocytes, eosinophils) |
severe diarrhea, steatorrhea (CLASSIC but found only in minority of patients); flatulence
crampy abdominal pain (from intussusception)
lassitude, fatigue, weight loss, failure to thrive
recurrent oral aphthous ulcers, dental enamel defects (10 40%)
peripheral neuropathy, ataxia, dementia, seizures
bleeding diathesis
infertility
idiopathic osteopenia with bone pain
dermatitis herpetiformis (= pruritic bullous skin rash)
anemia from iron/folate/vitamin B12deficiency
low serum levels of cholesterol, calcium, albumin
elevated alkaline phosphatase + liver enzymes
prolonged prothrombin time
Serologic testing for antibodies to gliadin + endomysium in screening + monitoring compliance
| Location: | patchy involvement of duodenum + jejunum > remainder of small bowel |
Small bowel follow-through:
 small bowel dilatation is HALLMARK in untreated celiac disease (70 95%), best seen in mid + distal jejunum (due to intestinal hypomotility); degree of dilatation related to severity of disease
small bowel dilatation is HALLMARK in untreated celiac disease (70 95%), best seen in mid + distal jejunum (due to intestinal hypomotility); degree of dilatation related to severity of disease hypersecretion-related artifacts:
hypersecretion-related artifacts: air-fluid levels in small bowel (rare)
air-fluid levels in small bowel (rare) segmentation = breakup of normal continual column of barium creating large masses of barium in dilated segments separated by stringlike strands from adjacent clumps due to excessive fluid; best seen on delayed films
segmentation = breakup of normal continual column of barium creating large masses of barium in dilated segments separated by stringlike strands from adjacent clumps due to excessive fluid; best seen on delayed films flocculation = coarse granular appearance of small clumps of disintegrated barium due to excess fluid best seen at periphery of intestinal segment; occurs especially with steatorrhea
flocculation = coarse granular appearance of small clumps of disintegrated barium due to excess fluid best seen at periphery of intestinal segment; occurs especially with steatorrhea fragmentation = scattering = faint irregular stippling of residual barium resembling snowflakes associated with segmentation due to excessive fluid
fragmentation = scattering = faint irregular stippling of residual barium resembling snowflakes associated with segmentation due to excessive fluid
 moulage sign (50%) = smooth contour with effaced featureless folds resembling tubular wax mold (due to atrophy of the folds of Kerckring); CHARACTERISTIC of sprue if seen in duodenum + jejunum
moulage sign (50%) = smooth contour with effaced featureless folds resembling tubular wax mold (due to atrophy of the folds of Kerckring); CHARACTERISTIC of sprue if seen in duodenum + jejunum long/normal/short transit time
long/normal/short transit time nonpropulsive peristalsis (flaccid + poorly contracting loops)
nonpropulsive peristalsis (flaccid + poorly contracting loops) normal/thickened/effaced mucosal folds (depending on degree of hypoproteinemia)
normal/thickened/effaced mucosal folds (depending on degree of hypoproteinemia) colonlike haustrations in well-filled jejunum (secondary to spasm + cicatrization from transverse ulcers)
colonlike haustrations in well-filled jejunum (secondary to spasm + cicatrization from transverse ulcers) jejunization of ileal loops (= adaptive response to decreased jejunal mucosal surface) = SPECIFIC
jejunization of ileal loops (= adaptive response to decreased jejunal mucosal surface) = SPECIFIC transient nonobstructive intussusception (20%) without anatomic lead point
transient nonobstructive intussusception (20%) without anatomic lead point bubbly bulb = peptic duodenitis = mucosal inflammation, gastric metaplasia, Brunner gland hyperplasia
bubbly bulb = peptic duodenitis = mucosal inflammation, gastric metaplasia, Brunner gland hyperplasia
Enteroclysis:
 decreased number of folds in proximal jejunum ( 3 folds per inch)
decreased number of folds in proximal jejunum ( 3 folds per inch) increased number of folds in distal ileum (>5 folds per inch)
increased number of folds in distal ileum (>5 folds per inch) tubular featureless lumen
tubular featureless lumen mosaic pattern = 1 2-mm polygonal islands of mucosa surrounded by barium-filled distinct grooves (10%)
mosaic pattern = 1 2-mm polygonal islands of mucosa surrounded by barium-filled distinct grooves (10%)
CT:
 small bowel dilatation + increased fluid content mucosal fold thickening
small bowel dilatation + increased fluid content mucosal fold thickening mild to moderate lymphadenopathy in mesentery/retroperitoneum (up to 12%)
mild to moderate lymphadenopathy in mesentery/retroperitoneum (up to 12%)
US:
 moderately dilated fluid-filled small intestine
moderately dilated fluid-filled small intestine thickening of small bowel wall
thickening of small bowel wall hyperperistalsis (82%)
hyperperistalsis (82%) dilated superior mesenteric artery + portal vein
dilated superior mesenteric artery + portal vein liver steatosis (metabolic derangement from malabsorption)
liver steatosis (metabolic derangement from malabsorption) mesenteric + retroperitoneal lymphadenopathy (12%)
mesenteric + retroperitoneal lymphadenopathy (12%) slight ascites (76%)
slight ascites (76%)
| Dx: | (1) Clinical presentation (2) Jejunal/duodenal biopsy with typical histopathologic features (3) Improvement of small bowel abnormalities after a few months of a gluten-free diet |
| Cause for relapse: | hidden dietary gluten, diabetes, bacterial overgrowth, intestinal ulceration, development of lymphoma |
Cx:
Ulcerative jejunoileitis
= multiple chronic benign ulcers (sausage appearance of small bowel) with hemorrhage, perforation + obstruction
Age: 5th 6th decade Location: jejunum > ileum > colon response to gluten-free diet ceases
Prognosis: frequently fatal Rx: small bowel resection Hyposplenism (30 50%)
 small atrophic spleen
small atrophic spleen
Cavitating mesenteric lymph node syndrome
Path: multiple pseudocystic lymph nodes containing chylous fluid (thin milky fluid/thick creamy material) + thin peripheral rim of fibrous material and scant elements of atrophic lymph node structures refractory weight loss, fatigue, diarrhea
target cells + Howell-Jolly bodies in peripheral blood smear (signs of hyposplenism)
Location: confined to jejunoileal mesentery  multiple 2 7-cm large lymph nodes with a central cavity of low attenuation fat-fluid levels
multiple 2 7-cm large lymph nodes with a central cavity of low attenuation fat-fluid levels splenic atrophy
splenic atrophy villous atrophy of small intestinal mucosa
villous atrophy of small intestinal mucosa
Prognosis: usually fatal disorder Malignant tumors (up to 14%)
lymphoma (in 8%):
Type: enteropathy-associated T-cell lymphoma (85 90%) + extraintestinal lymphoma (mostly Hodgkin lymphoma) Peak prevalence: 7th decade  enlarged nodular folds, ulcers, extrinsic mass effect
enlarged nodular folds, ulcers, extrinsic mass effect
adenocarcinoma of small bowel (7%), rectum, stomach
squamous cell carcinoma of esophagus (in 4%) during 6th 7th decade
malignancies of oropharynx, ovaries, testicles, thyroid, breast, lungs
P.870
Generalized lymphadenopathy with lymphocytosis (mimicking lymphoma)
Sigmoid volvulus (rare)
DDx:
Esophageal hypoperistalsis: scleroderma, idiopathic pseudoobstruction
Gastric abnormalities: Zollinger-Ellison syndrome, chronic granulomatous disease, eosinophilic enteritis, amyloidosis, malignancy
Tiny nodular defects on thickened folds: Whipple disease, intestinal lymphangiectasia, Waldenstr m macroglobulinemia
Small 1 3-mm nodules: lymphoid hyperplasia associated with giardiasis and immunoglobulin deficiency disease, diffuse lymphoma
Small nodules of varying sizes: systemic mastocytosis, amyloidosis, eosinophilic enteritis, Cronkhite-Canada syndrome
Bowel wall narrowing, kinking, scarring, ulceration: regional enteritis, bacterial/parasitic infection, carcinoid, vasculitis, ischemia, irradiation
Celiac Disease
= CELIAC SPRUE = NONTROPICAL SPRUE = GLUTEN-SENSITIVE ENTEROPATHY
| Cause: | genetically based immunologic intolerance to ingested grain glutens causing inflammation + damage of small intestinal villi; detected in 15% of 1st-degree relatives |
| Irritating agent: | gliadin polypeptides in wheat, rye, barley, oats |
| Countries: | North America, Europe, Australia, India, Pakistan, Middle East, Cuba |
| Incidence: | 1:200 to 1:500 |
| Age: | childhood by age 2 years; 30 40 years with M < F; 40 60 years with M > F |
| Rx: | gluten-free diet: corn, rice, tapioca, soya, millet, vitamin supplements |
Tropical Sprue
| Etiology: | infectious agent cured with antibiotics; geographic distribution (India, Far East, Puerto Rico) |
| Age: | any age group |
glossitis
hepatosplenomegaly
macrocytic anemia + leukopenia
| Prognosis: | spontaneous resolution after months/years |
| Rx: | responds well to folic acid + broad-spectrum antibiotics |
Strongyloidiasis
| Organism: | helminthic parasite Strongyloides stercoralis (2.2 mm long, 50 m in diameter); capable of reproducing within human host |
| Prevalence: | 100 million cases globally; 0.4 4% in USA |
| Country: | tropical + subtropical regions, parts of Europe, southeastern USA (eastern Kentucky, rural Tennessee), Puerto Rico |
| Primary host: | humans |
| Infection: | filiform larva enters body through skin/mucous membranes (from contaminated soil) |
| Cycle: | filariform larva penetrates skin and passes from subcutaneous/submucosal sites via lymphatic + venous circulation to lung; larva breaks into alveolar spaces and ascends bronchi + trachea; larva swallowed; settles in duodenum + upper jejunum (lives in tunnels between enterocytes); larva matures into parasitic adult female worm; worm deposits eggs into the intestinal lumen; ova hatch immediately into nonmigratory rhabditiform larvae, which are excreted in feces Autoinfection (endogenous reinfection) rhabditiform larva may remain in intestines long enough to metamorphose into infective filariform larva, which penetrates intestinal mucosa/perianal skin and reenters venous system repeating life cycle in same host |
| Path: | edema + inflammation of intestinal wall secondary to invasion by larvae; flattening of villi; ova in mucosal crypts |
| Histo: | intact larvae with Gomori methenamine silver stain |
asymptomatic for many years (in majority)
midepigastric pain mimicking peptic ulcer disease
weight loss
severe malnutrition (malabsorption, steatorrhea)
larva currens = recurrent allergic pruritic cutaneous skin reaction at site of larval penetration within 24 hours in area of buttocks + upper thighs in patients with autoinfection
worms, larvae, eggs in stool
blood eosinophilia (extremely common)
elevated levels of immunoglobulin E
 paralytic ileus (due to massive intestinal infestation):
paralytic ileus (due to massive intestinal infestation): mild to moderate dilatation of proximal 2/3 of duodenum + jejunum
mild to moderate dilatation of proximal 2/3 of duodenum + jejunum edematous irregular mucosal folds
edematous irregular mucosal folds
 ulcerations
ulcerations stricture of 3rd + 4th part of duodenum
stricture of 3rd + 4th part of duodenum rigid pipestem appearance + irregular narrowing of duodenum (in advanced cases)
rigid pipestem appearance + irregular narrowing of duodenum (in advanced cases)
| Rx: | thiabendazole (90% efficacy rate) |
| Prognosis: | high mortality in undernourished patients |
Strongyloides Hyperinfection Syndrome
= widespread dissemination + extensive tissue invasion in immunocompromised host with malignancy, autoimmune disease, malnutrition
gram-negative bacteremia, septicemia (due to spillage of gut organisms into bloodstream at time of larval penetration of intestinal wall)
crampy abdominal pain, nausea, diarrhea
persistent vomiting, hematemesis
 thickened colonic wall (due to florid transmural granulomatous inflammatory colitis caused by invasive larvae)
thickened colonic wall (due to florid transmural granulomatous inflammatory colitis caused by invasive larvae)@ Heart, skeletal muscle, lymph nodes, liver
endocarditis, peritonitis
@ CNS
meningitis due to larvae in pia arachnoid
global ischemia, atrophy, microinfarcts (from capillary obstruction)
@ Lung
P.871
| Histo: | foreign body reaction resulting in inflammatory pneumonitis + pulmonary hemorrhage |
dyspnea, cough, sputum production, wheezing
hemoptysis
 fine miliary nodules
fine miliary nodules diffuse reticulonodular interstitial opacities
diffuse reticulonodular interstitial opacities fleeting bilateral patchy alveolar/segmental/lobar opacities (with heavy infestation)
fleeting bilateral patchy alveolar/segmental/lobar opacities (with heavy infestation) adult ARDS may develop
adult ARDS may develop
| Dx: | filariform larvae in stool (single stool sample in 70% negative), sputum samples/bronchial washings/bronchial/lung biopsy specimens, CNS samples |
Superior Mesenteric Artery Syndrome
= VASCULAR COMPRESSION OF DUODENUM = WILKIE SYNDROME = CHRONIC DUODENAL ILEUS = BODY CAST SYNDROME
= vascular compression of 3rd portion of duodenum within aortomesenteric compartment; probably representing a functional reflex dilatation
| Pathophysiology: | narrowing of angle between SMA + aorta to 10 22 (normal 45 65 ) |
| Cause: | congenital, weight loss, visceroptosis due to loss of abdominal muscle tone (as in pregnancy), asthenic build, exaggerated lumbar lordosis, prolonged bed rest in supine position (body cast, whole-body burns, surgery) |
repetitive vomiting
abdominal cramping
 megaduodenum = pronounced dilatation of 1st + 2nd portion of duodenum + frequently stomach, best seen in supine position
megaduodenum = pronounced dilatation of 1st + 2nd portion of duodenum + frequently stomach, best seen in supine position vertical linear compression defect in transverse portion of duodenum overlying spine
vertical linear compression defect in transverse portion of duodenum overlying spine abrupt change in caliber distal to compression defect
abrupt change in caliber distal to compression defect relief of compression by postural change into prone knee elbow position
relief of compression by postural change into prone knee elbow position
Tailgut Cyst
= RETRORECTAL CYSTIC HAMARTOMA
| Cause: | incomplete regression of embryonic tailgut (= the portion distal to future anus) |
| Average age: | 35 years; M < F |
| Histo: | several types of epithelia + elements of intestinal epithelium, smooth muscle within cyst wall |
asymptomatic/perirectal pain, rectal bleeding, urinary frequency
| Location: | retrorectal/presacral space extension into ischiorectal fossa |
 thin-walled multicystic/unilocular cyst adhering to sacrum/rectum
thin-walled multicystic/unilocular cyst adhering to sacrum/rectum clear fluid/mucoid fluid with internal echoes
clear fluid/mucoid fluid with internal echoes
| Cx: | (1) Repeated perirectal abscesses, recurring anorectal fistula (2) Degeneration into mucinous adenocarcinoma |
Toxic Megacolon
= acute transmural fulminant colitis with neurogenic loss of motor tone + rapid development of extensive colonic dilatation >5.5 cm in transverse colon (damage to entire colonic wall + neuromuscular degeneration)
Etiology:
Ulcerative colitis (most common)
Crohn disease
Amebiasis, salmonellosis
Pseudomembranous colitis
Ischemic colitis
| Histo: | widespread sloughing of mucosa + thinning of frequently necrotic muscle layers |
systemic toxicity
profuse bloody diarrhea
 colonic ileus with marked dilatation of transverse colon
colonic ileus with marked dilatation of transverse colon few air-fluid levels
few air-fluid levels increasing caliber of colon on serial radiographs without redundancy
increasing caliber of colon on serial radiographs without redundancy loss of normal colonic haustra + interhaustral folds
loss of normal colonic haustra + interhaustral folds coarsely irregular mucosal surface
coarsely irregular mucosal surface pseudopolyposis = mucosal islands in denuded ulcerated colonic wall
pseudopolyposis = mucosal islands in denuded ulcerated colonic wall pneumatosis coli pneumoperitoneum
pneumatosis coli pneumoperitoneum
CT:
 distended colon filled with large amounts of fluid + air
distended colon filled with large amounts of fluid + air distorted haustral pattern
distorted haustral pattern irregular nodular contour of thin wall
irregular nodular contour of thin wall intramural air/small collections
intramural air/small collections
| BE: | CONTRAINDICATED due to risk of perforation |
| Prognosis: | 20% mortality |
Tuberculosis
Rarely encountered in Western Hemisphere, increased incidence in AIDS; usually associated with pulmonary tuberculosis (in 6 38%)
Etiology:
Ingestion of tuberculous sputum
Hematogenous spread from tuberculous focus in lung to submucosal lymph nodes
 Radiographic evidence of pulmonary TB in <50%
Radiographic evidence of pulmonary TB in <50%
Primary infection by cow milk (Mycobacterium bovis)
Path:
ulcerative form (most frequent): ulcers with their long axis perpendicular to axis of intestine, undermining + pseudopolyps
hypertrophic form: thickening of bowel wall (transmural granulomatous process)
| Organism: | M. tuberculosis, M. bovis, M. avium-intracellulare |
| Age: | 20 40 years |
weight loss, abdominal pain (80 90%)
nausea, vomiting
tuberculin skin test negative in most patients with primary intestinal TB
| Location: | ileocecal area > ascending colon > jejunum > appendix > duodenum > stomach > sigmoid > rectum |
P.872
@ Tuberculous peritonitis (in 1/3)
 Most common presentation associated with widespread abdominal disease!
Most common presentation associated with widespread abdominal disease!
Cause: hematogenous spread/rupture of mesenteric node Types:
wet type (most common) = exudative ascites with high protein contents + leukocytes
large amount of freely distributed/loculated viscous fluid
 high-density ascites of 20 45 HU (due to high protein + cellular content)
high-density ascites of 20 45 HU (due to high protein + cellular content)
dry/plastic type = caseous adenopathy + adhesions
 caseous nodules, fibrous peritoneal reaction, dense adhesions
caseous nodules, fibrous peritoneal reaction, dense adhesions
fibrotic-fixed type = omental cakelike mass with separation + fixation of bowel loops
 irregular masses of soft-tissue density in omentum + mesentery (common)
irregular masses of soft-tissue density in omentum + mesentery (common) matted loops of bowel and mesentery
matted loops of bowel and mesentery loculated ascites (occasionally)
loculated ascites (occasionally)
CT:
 enlarged lymph nodes (90%) with low-density centers in 40% (due to caseous necrosis)
enlarged lymph nodes (90%) with low-density centers in 40% (due to caseous necrosis)Location: peripancreatic, mesenteric, omental, retroperitoneal Lnn
 infiltration of mesentery
infiltration of mesentery
Cx: small bowel obstruction (adhesions from serosal tubercles) @ Ileocecal area (80 90%)
 Most commonly affected bowel segment!
Most commonly affected bowel segment!
Cause: relative stagnation of intestinal contents + abundance of lymphoid tissue (Peyer patches)  Stierlin sign = rapid emptying (hypermotility) of narrowed terminal ileum (spasm) into shortened rigid obliterated cecum on BE
Stierlin sign = rapid emptying (hypermotility) of narrowed terminal ileum (spasm) into shortened rigid obliterated cecum on BE thickened ileocecal valve (mass effect)
thickened ileocecal valve (mass effect) Fleischner sign = inverted umbrella defect = wide gaping patulous ileocecal valve associated with narrowing of the immediately adjacent terminal ileum
Fleischner sign = inverted umbrella defect = wide gaping patulous ileocecal valve associated with narrowing of the immediately adjacent terminal ileum deep fissures + large shallow linear/stellate ulcers with CHARACTERISTIC elevated margins following the orientation of lymphoid follicles (ie, longitudinal in terminal ileum and transverse in colon)
deep fissures + large shallow linear/stellate ulcers with CHARACTERISTIC elevated margins following the orientation of lymphoid follicles (ie, longitudinal in terminal ileum and transverse in colon) sinus tracts (rare)/enterocutaneous fistulas/perforation
sinus tracts (rare)/enterocutaneous fistulas/perforation symmetric annular napkin ring stenoses
symmetric annular napkin ring stenosesCT:
 circumferential wall thickening of cecum + terminal ileum
circumferential wall thickening of cecum + terminal ileum asymmetric thickening of ileocecal valve + medial wall of cecum
asymmetric thickening of ileocecal valve + medial wall of cecum exophytic extension engulfing terminal ileum
exophytic extension engulfing terminal ileum adjacent massive mesenteric lymphadenopathy with central areas of low attenuation
adjacent massive mesenteric lymphadenopathy with central areas of low attenuation
DDx: Crohn disease, amebiasis, cecal carcinoma @ Colon
Site: segmental colonic involvement, esp. on right side  rigid contracted cone-shaped cecum (spasm/transmural fibrosis)
rigid contracted cone-shaped cecum (spasm/transmural fibrosis) spiculations + wall thickening
spiculations + wall thickening diffuse ulcerating colitis + pseudopolyps
diffuse ulcerating colitis + pseudopolyps short hourglass strictures
short hourglass strictures shortened amputated cecum secondary to retraction of cecum out of the iliac fossa (due to fibrosis of mesocolon)
shortened amputated cecum secondary to retraction of cecum out of the iliac fossa (due to fibrosis of mesocolon)
DDx: ulcerative colitis, Crohn disease, amebiasis (spares terminal ileum), colitis of bacillary dysentery, ischemic colitis, pseudomembranous colitis @ Gastroduodenal
Site: simultaneous involvement of pylorus + duodenum  stenotic pylorus with gastric outlet obstruction
stenotic pylorus with gastric outlet obstruction narrowed antrum (linitis plastica appearance)
narrowed antrum (linitis plastica appearance) antral fistula
antral fistula multiple large and deep ulcerations on lesser curvature
multiple large and deep ulcerations on lesser curvature thickened duodenal folds with irregular contour/dilatation
thickened duodenal folds with irregular contour/dilatation
DDx: carcinoma, lymphoma, syphilis @ Esophagus
 Least common GI tract manifestation
Least common GI tract manifestation
Cause: secondary involvement from adjacent tuberculous lymphadenitis/primary TB  deep ulceration
deep ulceration stricture
stricture mass
mass intramural dissection/fistula formation = sinus tract formation
intramural dissection/fistula formation = sinus tract formation
Turcot Syndrome
= autosomal recessive disease with
colonic polyposis
CNS tumors (especially supratentorial glioblastoma, occasionally medulloblastoma)
| Age: | symptomatic during 2nd decade |
| Histo: | adenomatous polyps |
diarrhea
seizures
 multiple 1 30-mm polyps in colon + rectum
multiple 1 30-mm polyps in colon + rectum
| Cx: | malignant transformation of colonic polyps in 100% |
| Prognosis: | death from brain tumor in 2nd + 3rd decade |
Typhlitis
= ILEOCECAL SYNDROME = NEUTROPENIC COLITIS
= acute inflammation of cecum, appendix, and occasionally terminal ileum; initially described in children with leukemia + severe neutropenia;
[typhlos, Greek = blind sac = cecum]
| Cause: | leukemic/lymphomatous infiltrate, ischemia, focal pseudomembranous colitis, infection (CMV) |
| Histo: | edema + ulceration of entire bowel wall; transmural necrosis with perforation possible |
| Organism: | CMV, Pseudomonas, Candida, Klebsiella, E. coli, B. fragilis, Enterobacter |
| Predisposed: | common in childhood leukemia, aplastic anemia, lymphoma, immunosuppressive therapy (eg, renal transplant), cyclic neutropenia, myelodysplastic syndrome, clinical AIDS |
abdominal pain, may be localized to RLQ
watery/bloody diarrhea
fullness/palpable mass in RLQ
fever, neutropenia
hematochezia/occult blood
P.873
| Location: | cecum + ascending colon, appendix + distal ileum may become secondarily involved |
 fluid-filled masslike density in RLQ
fluid-filled masslike density in RLQ distension of nearby small bowel loops
distension of nearby small bowel loops thumbprinting of ascending colon
thumbprinting of ascending colon circumferential thickening of cecal wall >4 mm
circumferential thickening of cecal wall >4 mm occasionally pneumatosis
occasionally pneumatosisCT (preferable examination due to risk of perforation):
 circumferential wall thickening (>1 3 mm) of cecum terminal ileum
circumferential wall thickening (>1 3 mm) of cecum terminal ileum decreased bowel wall attenuation (edema)
decreased bowel wall attenuation (edema) increased attenuation of adjacent fat + thickening of fascial planes (pericolonic inflammation)
increased attenuation of adjacent fat + thickening of fascial planes (pericolonic inflammation) pericolonic fluid + intramural pneumatosis
pericolonic fluid + intramural pneumatosis
| Cx: |
|
| Rx: |
|
| DDx: |
|
| DDx between Crohn Disease and Ulcerative Colitis | ||
|---|---|---|
| Crohn Disease | Ulcerative Colitis | |
| mnemonic: | LUCIFER M | |
| Location | right side | left side |
| Ulcers | deep | shallow |
| Contraction | no | yes |
| Ileocecal valve | thickened | gaping |
| Fistulae | yes | no |
| Eccentricity | yes | no |
| Rate of carcinoma | slight increase | marked increase |
| Megacolon | unusual | yes |
Ulcerative Colitis
= common idiopathic inflammatory bowel disease with continuous concentric + symmetric colonic involvement
| Etiology: | hypersensitivity/autoimmune disease |
| Prevalence: | 50 80:100,000 In high incidence areas of North America, Northern Europe, Australia |
| Path: | predominantly mucosal + submucosal disease with exudate + edema + crypt abscesses (HALLMARK) resulting in shallow ulceration |
| Age peak: | 20 40 years + 60 70 years; M:F = 1:1 |
alternating periods of remission + exacerbation
bloody diarrhea
electrolyte depletion, fever, systemic toxicity
abdominal cramps
Extracolonic manifestations:
iritis, erythema nodosum, pyoderma gangrenosum
pericholangitis, chronic active hepatitis, primary sclerosing cholangitis, fatty liver
spondylitis, peripheral arthritis, coincidental rheumatoid arthritis (10 20%)
thrombotic complications
Location: begins in rectum with proximal progression (rectum spared in 4%); relatively uniform symmetric involvement of bowel rectosigmoid in 95% (diagnosed by rectal biopsy); continuous circumferential involvement often limited to left side of colon
colitis extending proximally to splenic flexure = universal colitis
terminal ileum in 10 25% ( backwash ileitis )
Plain film:
 hyperplastic mucosa, polypoid mucosa, deep ulcers
hyperplastic mucosa, polypoid mucosa, deep ulcers diffuse dilatation with loss of haustral markings
diffuse dilatation with loss of haustral markings toxic megacolon
toxic megacolon free intraperitoneal gas
free intraperitoneal gas complete absence of fecal residue (due to inflammation)
complete absence of fecal residue (due to inflammation)
BE:
acute stage
 narrowing + incomplete filling (spasm + irritability)
narrowing + incomplete filling (spasm + irritability) fine mucosal granularity = stippling of barium coat (from diffuse mucosal edema + hyperemia + superficial erosions)
fine mucosal granularity = stippling of barium coat (from diffuse mucosal edema + hyperemia + superficial erosions) spicules + serrated bowel margins (tiny superficial ulcers)
spicules + serrated bowel margins (tiny superficial ulcers) collar button ulcers (= undermining of ulcers)
collar button ulcers (= undermining of ulcers) double-tracking = longitudinal submucosal ulceration over several cm
double-tracking = longitudinal submucosal ulceration over several cm hazy/fuzzy quality of bowel contour (excessive secretions)
hazy/fuzzy quality of bowel contour (excessive secretions) thumbprinting = symmetric thickening of colonic folds
thumbprinting = symmetric thickening of colonic folds pseudopolyps = scattered islands of edematous mucosa + reepithelialized granulation tissue within areas of denuded mucosa
pseudopolyps = scattered islands of edematous mucosa + reepithelialized granulation tissue within areas of denuded mucosa widening of presacral space
widening of presacral space obliterated rectal folds = valves of Houston (43%)
obliterated rectal folds = valves of Houston (43%)
subacute stage
 distorted irregular haustra
distorted irregular haustra inflammatory polyps = sessile frondlike/rarely pedunculated lesions (= localized mucosal inflammation resulting in polypoid protuberance)
inflammatory polyps = sessile frondlike/rarely pedunculated lesions (= localized mucosal inflammation resulting in polypoid protuberance) coarse granular mucosa (= mucosal replacement by granulation tissue)
coarse granular mucosa (= mucosal replacement by granulation tissue)
chronic stage
 shortening of colon (= reversible spasm of longitudinal muscle) with depression of flexures
shortening of colon (= reversible spasm of longitudinal muscle) with depression of flexures leadpipe colon = rigidity + symmetric narrowing of lumen
leadpipe colon = rigidity + symmetric narrowing of lumen widening of haustral clefts/complete loss of haustrations (DDx: cathartic colon)
widening of haustral clefts/complete loss of haustrations (DDx: cathartic colon) burnt-out colon = fairly distensible colon without haustral markings + without mucosal pattern
burnt-out colon = fairly distensible colon without haustral markings + without mucosal pattern hazy/fuzzy quality of bowel contour (excessive secretions)
hazy/fuzzy quality of bowel contour (excessive secretions) postinflammatory polyps (12 19%) = small sessile nodules/long wormlike branching + bridging outgrowths (= filiform polyposis)
postinflammatory polyps (12 19%) = small sessile nodules/long wormlike branching + bridging outgrowths (= filiform polyposis) backwash ileitis (5 30%) involving 4 25 cm of terminal ileum with patulous ileocecal valve + absent peristalsis + granularity
backwash ileitis (5 30%) involving 4 25 cm of terminal ileum with patulous ileocecal valve + absent peristalsis + granularity
P.874
CT:
 wall thickening <10 mm
wall thickening <10 mm
Cx:
Toxic megacolon perforation in 5 10%
(DDx: granulomatous/ischemic/amebic colitis)
 Most common cause of death in ulcerative colitis!
Most common cause of death in ulcerative colitis!
Colonic adenocarcinoma (3 5%):
risk starts after 8 10 years of onset of disease; risk progresses at 0.5%/year for 10 20 years + at 0.9%/year thereafter; higher risk with pancolitis + onset of disease in <15 years of age
Usually associated with: total colitis Location: rectosigmoid > descending colon, distal transverse colon  narrowed segment of 2 6 cm in length with eccentric lumen + irregular contour + flattened rigid tapered margins = scirrhous carcinoma
narrowed segment of 2 6 cm in length with eccentric lumen + irregular contour + flattened rigid tapered margins = scirrhous carcinoma annular/polypoid carcinoma
annular/polypoid carcinoma
Prognosis: synchronous lesions in 35% Colonic strictures (10%)
smooth contour with fusiform pliable tapering margins, usually short + single stricture; commonly in sigmoid/rectum/transverse colon; usually after minimum of 5 years of disease; rarely cause for obstruction (DDx: colonic carcinoma)
Perforation
| DDx: |
|
Villous Adenoma
Villous Adenoma of Colon
| Incidence: | 7% of all colonic tumors |
| Age: | presentation late in life; M = F |
| Location: | rectum + sigmoid (75%), cecum, ileocecal valve; 2% of all tumors in rectum + colon |
| Associated with: | other GI tumors (25%) |
sensation of incomplete evacuation
rectal bleeding
excretion of copious amounts of thick mucus
fatigability, weakness
diarrhea + electrolyte depletion syndrome in 4% (dehydration, hypokalemia, hyponatremia)
 may completely encircle the colon
may completely encircle the colon broad-based sessile bulky tumor often >20 mm in diameter:
broad-based sessile bulky tumor often >20 mm in diameter: innumerable papillary mucosal projections ( villous fronds ) with reticular/granular surface pattern (if villous elements constitute >75% of tumor, diagnosis can be made on BE):
innumerable papillary mucosal projections ( villous fronds ) with reticular/granular surface pattern (if villous elements constitute >75% of tumor, diagnosis can be made on BE): spongelike corrugated appearance (barium within interstices)
spongelike corrugated appearance (barium within interstices) striated brushlike surface
striated brushlike surface
 soft pliable tumor with change in shape:
soft pliable tumor with change in shape: apparent decrease in size on postevacuation films
apparent decrease in size on postevacuation films
CT:
 heterogeneous low attenuation on CT (due to capacious mucin becoming trapped within papillary projections + crevices)
heterogeneous low attenuation on CT (due to capacious mucin becoming trapped within papillary projections + crevices)
| Prognosis: | higher malignant potential than tubular adenoma |
| Cx: | malignant transformation/invasion (in 36%) related to size of tumor <5 cm (9%); >5 cm (55%); >10 cm (100%) |
Villous Adenoma of Duodenum
More common in colon + rectum; fewer than 50 cases in world literature
 sessile, soft nonobstructive mass
sessile, soft nonobstructive mass lace / soap bubble pattern
lace / soap bubble pattern preservation of peristaltic activity + bowel distensibility
preservation of peristaltic activity + bowel distensibility
Waldenstr m Macroglobulinemia
= low-grade lymphoid malignancy composed of mature plasmacytoid lymphocytes with production of abnormal monoclonal IgM protein
| Incidence: | 0.53/100,000 annually; frequency 10 15% that of multiple myeloma |
| Histo: | macroglobulin proteinaceous hyaline material fills lacteals in lamina propria of small bowel villi with secondary lymphatic distension + edema |
| Mean age: | 63 years; M > F |
fatigue, weight loss
diarrhea, steatorrhea, malabsorption
anemia, bleeding diathesis
IgM elevation
hyperviscosity syndrome (20%) = bleeding, visual changes, neurologic abnormalities
@ Small bowel (rarely involved)
 small bowel dilatation
small bowel dilatation uniform diffuse thickening of valvulae conniventes with spikelike configuration (jejunum + proximal ileum)
uniform diffuse thickening of valvulae conniventes with spikelike configuration (jejunum + proximal ileum) granular surface of punctate filling defects (distended villi)
granular surface of punctate filling defects (distended villi)
@ Bone marrow involvement (91 98%)
(a) diffuse replacement of bone marrow (56%)
(b) variegated replacement of bone marrow (35%)
 compression fractures of spine (48%)
compression fractures of spine (48%) diffuse demineralization of spine
diffuse demineralization of spine lytic lesions on bone surveys (in up to 20%)
lytic lesions on bone surveys (in up to 20%)MR (pre- and post-contrast T1WI preferred):
 marrow iso-/hypointense to muscle on T1WI
marrow iso-/hypointense to muscle on T1WI enhancement of abnormal marrow on T1WI
enhancement of abnormal marrow on T1WI
@ Lymph nodes
 lymphadenopathy (43%)
lymphadenopathy (43%)
@ Liver & spleen
 hepatosplenomegaly
hepatosplenomegaly
| Dx: |
|
| DDx: | multiple myeloma (lymphadenopathy rare, lytic lesions in 31%) |
Whipple Disease
[George Whipple (1878 1976), pathologist in Rochester, USA]
= INTESTINAL LIPODYSTROPHY
= sporadically occurring chronic multisystem disease
P.875
| Etiology: | thought to be caused by infection with a gram-positive bacterium (Tropheryma whippelii) closely related to actinobacteria |
| Histo: | PAS-positive material (periodic acid Schiff) = glycoprotein (from bacterial cell wall) within foamy macrophages in the submucosa of the jejunum + fat deposits within intestinal submucosa and lymph nodes causing lymphatic obstruction + dilatation |
| Age: | 4th 6th decade (mean age of onset, 50 years); M:F = 8:1; Caucasians |
recurrent and migratory arthralgias/nondeforming arthritis (65 95%); arthritis may precede Whipple disease in 10% up to 10 years
malabsorption, steatorrhea, abdominal pain
weight loss, low-grade fever
polyserositis
generalized peripheral lymphadenopathy (50%)
hyperpigmentation of skin similar to Addison disease
pale shaggy yellow plaques/erosions in postbulbar duodenum on endoscopy
Organ involvement: liver, intestines, joints, heart, lung, CNS, eyes, skin (virtually every organ system)  moderate thickening of jejunal + duodenal folds (from mucosal + submucosal infiltration by PAS-positive macrophages combined with lymphatic obstruction)
moderate thickening of jejunal + duodenal folds (from mucosal + submucosal infiltration by PAS-positive macrophages combined with lymphatic obstruction) micronodularity (= swollen villi) and wild mucosal pattern
micronodularity (= swollen villi) and wild mucosal pattern hypersecretion, segmentation, fragmentation (occasionally if accompanied by hyperproteinemia)
hypersecretion, segmentation, fragmentation (occasionally if accompanied by hyperproteinemia) NO/minimal dilatation of small bowel
NO/minimal dilatation of small bowel NO rigidity of folds, NO ulcerations
NO rigidity of folds, NO ulcerations normal transit time (approximately 3 hours)
normal transit time (approximately 3 hours) hepatosplenomegaly
hepatosplenomegalyCT:
 bulky 3 4-cm large low-density lymph nodes in mesenteric root + retroperitoneum (due to extracellular neutral fat + fatty acids)
bulky 3 4-cm large low-density lymph nodes in mesenteric root + retroperitoneum (due to extracellular neutral fat + fatty acids) thickening of bowel wall
thickening of bowel wall splenomegaly
splenomegaly ascites
ascites pleuropericarditis
pleuropericarditis sacroiliitis
sacroiliitis
US:
 echogenic lymph nodes
echogenic lymph nodes
| Dx: | endoscopically guided biopsy of small bowel mucosa, abdominal/peripheral lymph node biopsy |
| Rx: | long-term broad-spectrum antibiotics (tetracycline) |
| DDx: |
|
Zenker Diverticulum
= PHARYNGOESOPHAGEAL DIVERTICULUM
= outpouching of posterior hypopharyngeal wall = pulsion diverticulum with herniation of mucosa + submucosa through oblique + transverse muscle bundles (pseudodiverticulum) of the cricopharyngeal muscle
| Prevalence: | 0.01 0.11% (overall); higher in elderly women (50% occur in 7th 8th decade) |
| Etiology: | cricopharyngeal dysfunction (cricopharyngeal achalasia/premature closure) results in increased intraluminal pressure |
| Associated with: | hiatal hernia, gastroduodenal ulcer, midesophageal diverticulum, esophageal spasm, achalasia |
compressible neck mass
upper esophageal dysphagia (98%)
regurgitation + aspiration of undigested food
noisy deglutition
halitosis (= foul breath)
Location: at pharyngoesophageal junction in midline of Killian dehiscence/triangle of Laimer, at level of C5-6  posterior barium extension in upper half of semilunar depression on the posterior wall of esophagus (cricopharyngeal muscle)
posterior barium extension in upper half of semilunar depression on the posterior wall of esophagus (cricopharyngeal muscle) barium-filled sac extending caudally behind + usually to left of esophagus
barium-filled sac extending caudally behind + usually to left of esophagus partial/complete obstruction of esophagus from external pressure of sac contents
partial/complete obstruction of esophagus from external pressure of sac contents partial barium reflux from diverticulum into hypopharynx
partial barium reflux from diverticulum into hypopharynx continual growth with successive enlargement
continual growth with successive enlargementCXR:
 air-fluid level in superior mediastinum
air-fluid level in superior mediastinum
| Cx: | aspiration pneumonia (30%); esophageal perforation; carcinoma (0.48%) |
| Rx: | surgical excision |
Zollinger-Ellison Syndrome
= peptic ulcer diathesis associated with marked hypersecretion of gastric acid + gastrin-producing non- islet cell tumor of pancreas
Cause:
GASTRINOMA (90%)
= non- islet cell tumor with continuous gastrin production
PSEUDO Z-E SYNDROME = Cowley SYNDROME
= antral G-cell hyperplasia (10%) = increase in number of G-cells in gastric antrum
lack of gastrin elevation after secretin injection
exaggerated gastrin elevation after protein meal
| Age: | middle age; M > F |
Clinical tetrad:
Gastric hypersecretion: refractory response to histamine stimulation test concerning HCl concentration; increased basal secretion (>60% of augmented secretion is diagnostic)
Hypergastrinemia >1000 ng/L (during fasting)
Hyperacidity with basal acid output >15 mEq/h
Diarrhea (30%), steatorrhea (40%): may be sole complaint in 10%, frequently nocturnal; secondary to inactivation of pancreatic enzymes by large volumes of HCl/excessive delivery of acid to small bowel
severe intractable pain (90%)
ulcer perforation (30%)
positive secretin test = increase in serum gastrin level by >200 ng/L after administration of 2 IU/kg of secretin
 ulcers (atypical location + course should suggest diagnosis):
ulcers (atypical location + course should suggest diagnosis):Location: duodenal bulb (65%) + stomach (20%), near ligament of Treitz (25%), duodenal C-loop (5%), distal esophagus (5%) Multiplicity: solitary ulcer (90%), multiple ulcers (10%)  recurrent/intractable ulcers
recurrent/intractable ulcers marginal ulcers in postgastrectomy patient
marginal ulcers in postgastrectomy patienton gastric side of anastomosis
on mesenteric border of efferent loop
 prominence of area gastricae (hyperplasia of parietal cell mass)
prominence of area gastricae (hyperplasia of parietal cell mass) enlargement of rugal folds
enlargement of rugal folds sluggish gastric peristalsis ( hypokalemia)
sluggish gastric peristalsis ( hypokalemia) wet stomach = dilution of barium by excess secretions in nondilated nonobstructed stomach
wet stomach = dilution of barium by excess secretions in nondilated nonobstructed stomach gastroesophageal reflux (common) + esophagitis
gastroesophageal reflux (common) + esophagitis dilatation of duodenum + upper small bowel (fluid overload)
dilatation of duodenum + upper small bowel (fluid overload) thickened folds in duodenum + jejunum (edema)
thickened folds in duodenum + jejunum (edema) rapid small-bowel transit time
rapid small-bowel transit time
P.876
| mnemonic: | FUSED |
Folds (thickened, gastric folds)
Ulcers (often multiple, postbulbar)
Secretions increased (refractory to histamine)
Edema (of proximal small bowel)
Diarrhea
| Cx: |
|
| Rx: |
|
EAN: 2147483647
Pages: 24